Академический Документы
Профессиональный Документы
Культура Документы
CH 17
Загружено:
Ungureanu DaniaИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
CH 17
Загружено:
Ungureanu DaniaАвторское право:
Доступные форматы
Treatment of pulpally inamed primary and perma-
nent teeth in children presents a unique challenge to
the dental clinician. Pulp diagnosis in the child is
imprecise as clinical symptoms do not correlate well
with histologic pulpal status. Age and behavior can
compromise the reliability of pain as an indicator of
the extent of pulp inammation. Furthermore, treat-
ment goals are developmentally oriented and may be
relatively short term by comparison to the long-term
restorative permanence of adult endodontics.
Because of this latter fact, a major focus in pediatric
pulp therapy is vital pulp treatment, that capitalizes
on the healing potential of the noninamed remain-
ing portions of the pulp. With instances of irre-
versibly inamed and necrotic radicular pulps, con-
ventional concepts of nonvital pulp treatment are
indicated. However, they must be modied to accom-
modate physiologic root resorption in primary teeth
and continued root development in young perma-
nent teeth.
Lewis and Law succinctly stated the ultimate objec-
tive of pediatric pulp therapy: The successful treat-
ment of the pulpally involved tooth is to retain that
tooth in a healthy condition so it may fulll its role as a
useful component of the primary and young perma-
nent dentition.
1
Premature loss of primary teeth from
dental caries and infection may result in the following
sequelae:
Loss of arch length
Insufficient space for erupting permanent teeth
Ectopic eruption and impaction of premolars
Mesial tipping of molar teeth adjacent to primary
molar loss
Extrusion of opposing permanent teeth
Shift of the midline with a possibility of crossbite
occlusion
Development of certain abnormal tongue positions
It is for this reason that maximum attempts must be
made to preserve primary teeth in a healthy state until
normal exfoliation occurs. A major contention in con-
temporary research involving vital pulp treatment is
the denition of healthy pulp status ascribed to many
of the treatment outcomes. This issue will be addressed
in more detail later in this chapter.
Vital pulp therapy is based on the premise that pulp
tissue has the capacity to heal. In addition to the bio-
logic basis for the healing capacity of the pulp, differ-
ences between primary and permanent teeth exist from
a morphologic and histologic standpoint. These differ-
ences must be addressed by the clinician to successful-
ly treat pulpally inamed teeth in children.
PULP MORPHOLOGY
Anatomic Differences Between Primary and
Permanent Teeth
Anatomic differences between the pulp chambers and
root canals of primary teeth and those of young perma-
nent teeth have been described
2
(Figure 17-1): (1) Pulp
chamber anatomy in primary teeth approximates the
surface shape of the crown more closely than in perma-
nent teeth. (2) The pulps of primary teeth are propor-
tionately larger and the pulp horns extend closer to the
outer surfaces of the cusps than in permanent teeth. (3)
The pulp-protecting dentin thickness between the pulp
chamber and the dentinoenamel junction is less than in
permanent teeth. These three factors increase the poten-
tial for pulp exposure from mechanical preparation,
dental caries, and trauma. (4) An increased number of
accessory canals and foramina, as well as porosity in pul-
pal oors of primary teeth, has been noted in compari-
son with permanent teeth.
3
This is thought to account
for the consistent pulp necrosis response of furcation
radiolucency in primary teeth versus periapical radiolu-
cency in permanent teeth.
46
Chapter 17
PEDIATRIC ENDODONTICS
Clifton O. Dummett Jr and Hugh M. Kopel
A comparison of root canals in primary teeth with
those of young permanent teeth reveals the following
characteristics: (1) the roots of primary teeth are pro-
portionately longer and more slender; (2) primary root
canals are more ribbon-like and have multiple pulp l-
aments within their more numerous accessory canals;
(3) the roots of primary molars are outward from the
cervical part of the tooth to a greater degree than per-
manent teeth and continue to are apically to accom-
modate the underlying succedaneous tooth follicle; (4)
the roots of primary anterior teeth are narrower
mesiodistally than permanent anterior tooth roots; and
(5) in contrast to permanent teeth, the roots of primary
teeth undergo physiologic root resorption. These fac-
tors make complete extirpation of pulp remnants
almost impossible and increase the potential of root
perforation during canal instrumentation. As a result,
the requirements of primary root canal lling materials
must encompass germicidal action, good obturation,
and resorptive capability.
3
Histologic Considerations
Numerous descriptions of pulp histology exist that
identify the various cell components of pulp tissue.
7,8
Consistently, the pulp is primarily connective tissue
and has considerable healing potential. Features that
862 Endodontics
distinguish pulp tissue from other connective tissue
include the presence of odontoblasts, absence of hista-
mine-releasing mast cells, tissue connement in a hard
cavity with little collateral circulation, and vascular
access limited to the root apex.
7,8
Pulp healing capabil-
ity is affected by endogenous factors of coronal cellu-
larity and apical vascularity. Both are increased in pri-
mary and young permanent teeth.
8
Pulps become more
brous, less cellular, and less vascular with age.
8
Exogenous factors affecting pulp healing include bacte-
rial invasion and chemical/thermal insult. Current
research in pulp biology and restorative materials
strongly substantiates the need for bacterial microleak-
age control in maximizing pulp survival.
9
Fox and Heeley concluded that, histologically, no
structural differences exist between primary pulp tissue
and young permanent pulp tissue with the exception of
the presence of a cap-like zone of reticular and collage-
nous bers in the primary coronal pulp.
10
However,
many clinicians have noted different pulp responses
between primary and young permanent teeth to trau-
ma, bacterial invasion, irritation, and medication.
Anatomic differences may contribute to these respons-
es. Primary roots have an enlarged apical foramen, in
contrast to the foramen of permanent roots, which is
constricted. The resultant reduced blood supply in
mature permanent teeth favors a calcic response and
healing by calcic scarring.
11
This hypothesis is
exemplied in older pulps, in which more calcied
nodules and ground substance are found than in young
pulps. Primary teeth, with their abundant blood sup-
ply, demonstrate a more typical inammatory
response than that seen in mature permanent teeth.
The exaggerated inammatory response in primary
teeth may account for increased internal and external
root resorption from calcium hydroxide pulpotomies.
The alkalinity of calcium hydroxide can produce severe
pulp inammation and subsequent metaplasia with
resultant internal primary root resorption. It has been
shown that the greater the inammation, the more
severe the resorption (Figure 17-2). Although it is sus-
pected that pulps of primary teeth have a different
function from those of permanent teeth, no supporting
data are available.
Some clinicians believe that primary teeth are less
sensitive to pain than permanent teeth, probably
because of differences in the number and/or distribu-
tion of neural elements. When comparing primary and
permanent teeth, Bernick found differences in the nal
distribution of pulp nerve bers.
12
In permanent teeth,
these bers terminate mainly among the odontoblasts
and even beyond the predentin. In primary teeth, pulp
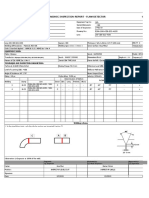
Figure 17-1 Comparative anatomy between primary (left) and
permanent (right) molars. Primary teeth are smaller in all dimen-
sions; their enamel cap is thinner, with less tooth structure protect-
ing the pulp. Primary pulp horns are higher, particularly mesial.
The roots of primary molars are longer and more slender, are
pinched in at the cervical part of the tooth, and are more toward
the apex to accommodate permanent tooth buds. All of these fac-
tors tend to increase the incidence of pulp involvement from caries
or complicate canal preparation and obturation. Reproduced with
permission from Finn SB.
2
Pediatric Endodontics 863
nerve bers pass to the odontoblastic area, where they
terminate as free nerve endings. Bernick postulated
that if primary teeth were not so short-lived in the oral
cavity, their nerve endings might terminate among the
odontoblasts and in the predentin as in permanent
teeth
12
(Figure 17-3).
Rapp and associates concurred with Bernicks
hypothesis and also stated that the density of the inner-
vation of the primary tooth is not as great as that of the
permanent tooth and may be the reason why primary
teeth are less sensitive to operative procedures.
13
They
agree, however, that as the primary teeth resorb, there is
a degeneration of the neural elements as with other
pulp cells. Neural tissue is the rst to degenerate when
root resorption begins, just as it is the last tissue to
mature when the pulp develops.
Primary and permanent teeth also differ in their cel-
lular responses to irritation, trauma, and medication. It
has been shown, for example, that the incidence of
reparative dentin formation beneath carious lesions is
more extensive in primary than in permanent
teeth.
1417
McDonald reported that the localization of
infection and inammation is poorer in the primary
pulp than in the pulp of permanent teeth.
18
MANAGEMENT OF DEEP CARIOUS LESIONS
AND PULP INFLAMMATION IN PRIMARY
AND YOUNG PERMANENT TEETH
Pulp therapy for primary and young permanent teeth
has historically been subject to change and controversy.
Pulp medicaments, such as zinc oxideeugenol (ZOE)
cement, calcium hydroxide, and formocresol, have been
the basis for much of this controversy. A better under-
standing of the reactions of the pulp and dentin to these
medicaments has developed over time, primarily
through improvements in histologic techniques.
Anderson and colleagues felt that the pulp and dentin
should be considered as one organ.
19
Frankl determined
that this pulpodentinal system reaction is proportional
to the intensity and duration of the offending agents of
caries, trauma, medicaments, or restorative materials.
20
A correct diagnosis of pulp conditions in primary
teeth is important for treatment planning. McDonald
and Avery have outlined several diagnostic aids in select-
Figure 17-2 Internal resorption triggered by inammation. A,
Advanced caries in a 5-year-old child. Note calcication (arrow) in
the rst primary molar (contraindication for pulp therapy). B,
Same patient 6 months later. Marked internal resorption, forecast in
the earlier radiograph, indicates advanced degenerative changes.
Reproduced with permission from Law DB, Lewis TM, Davis JM.
An atlas of pedodontics. Philadelphia: WB Saunders; 1969.
Figure 17-3 Section of pulp from a human primary molar. Note
that the majority of nerves terminate at the pulp-odontoblastic
(PO) border. Only isolated nerve ber penetrates the P-O border to
terminate in the zone of Weil. D = dentin; N = nerve ber;
O = odontoblasts; Pr = predentin; PO = pulp-odontoblast border.
Reproduced with permission from Bernick S.
12
A
B
ing teeth for vital pulp therapy.
3
Eidelman et al.
21
and
Prophet and Miller
22
have emphasized that no single
diagnostic means can be relied on for determining a
diagnosis of pulp conditions. Rayner and Southam have
stated that the inammation response to the effects of
dentin caries in the deciduous pulp is more rapid than in
the permanent pulp.
23
Yet Taylor concluded that in spite
of being inamed and infected by the carious process,
primary molars are still capable of marked defense reac-
tions similar to those observed in permanent teeth.
24
The goal in managing the deep carious lesion is
preservation of pulp vitality before arbitrarily institut-
ing endodontic therapy. A suggested outline for deter-
mining the pulpal status of cariously involved teeth in
children involves the following:
1. Visual and tactile examination of carious dentin and
associated periodontium
2. Radiographic examination of
a. periradicular and furcation areas
b. pulp canals
c. periodontal space
d. developing succedaneous teeth
3. History of spontaneous unprovoked pain
4. Pain from percussion
5. Pain from mastication
6. Degree of mobility
7. Palpation of surrounding soft tissues
8. Size, appearance, and amount of hemorrhage associ-
ated with pulp exposures
Pediatric pulp therapy for primary and young per-
manent teeth involves the following techniques:
1. Indirect pulp capping
2. Direct pulp capping
3. Coronal pulpotomy
4. Pulpectomy
The rst three methods are vital techniques that
involve conservative management of portions of
inamed pulp tissue with the preservation of the
remaining vital pulp. The pulpectomy procedure is a
nonvital technique and involves the complete extirpa-
tion of the irreversibly inamed and/or necrotic pulp
followed by canal obturation with a resorbable medica-
ment in primary teeth and conventional root canal ll-
ing in permanent teeth.
INDIRECT PULP CAPPING
Indirect pulp capping is dened as the application of a
medicament over a thin layer of remaining carious
864 Endodontics
dentin, after deep excavation, with no exposure of the
pulp. In 1961, Damele described the purpose of indi-
rect pulp capping as the use of reconstructed dentin
to prevent pulp exposure.
25
The treatment objective is
to avoid pulp exposure and the necessity of more inva-
sive measures of pulp therapy by stimulating the pulp
to generate reparative dentin beneath the carious
lesion. This results in the arrest of caries progression
and preservation of the vitality of the nonexposed
pulp.
26
This technique can be used as a one-sitting pro-
cedure or the more classic two-sitting procedure. The
latter involves re-entry after a 6 to 8-week interval to
remove any remaining carious dentin and place the
nal restoration
3,27
(Figure 17-4).
DiMaggio found, in a histologic evaluation of teeth
selected for indirect treatment, that 75% would have
been pulp exposures if all of the caries had initially
been removed. Using clinical criteria, this same study
showed a failure rate of only 1%for indirect pulp caps
compared with 25% failure for direct caps.
28
A histo-
logic examination, however, raised these failure rates to
12% and 33%, respectively. Trowbridge and Berger
stated that complete removal of softened dentin, with
ensuing pulp exposure, may contribute nothing of
diagnostic value in estimating the extent of existing
pulp disease.
29
In fact, other studies have shown that
the true picture of pulp disease cannot be assessed on
the basis of such diagnostic criteria as history of pain,
response to temperature change, percussion, and elec-
tric pulp testing.
30,31
Figure 17-4 Indirect pulp-capping technique. A, Medicament,
either zinc oxideeugenol cement, calcium hydroxide, or both,
against remaining caries. B, Lasting temporary restoration.
Following repair, both materials are removed along with softened
caries, and nal restorations are placed.
Pediatric Endodontics 865
Historical Review
The concept of indirect pulp capping was rst
described by Pierre Fauchard as reported by John
Tomes in the mid-18th century, who recommended
that all caries should not be removed in deep, sensitive
cavities for fear of exposing the nerve and making the
cure worse than the disease.
32
John Tomes, in his mid-
19th century textbook, stated, It is better that a layer
of discolored dentin should be allowed to remain for
the protection of the pulp rather than run the risk of
sacricing the tooth.
32
Although neither of these den-
tal pioneers referred to any specic medication for the
softened dentin, they recognized the healing capacity
of the pulp.
In 1891, W. D. Miller discussed various antisep-
tics that should be used for sterilizing dentin.
34
In
contrast to these early reports advocating conservative
management of deep lesions, G. V. Black felt that in the
interest of scientic dental practice, no decayed or soft-
ened material should be left in a cavity preparation,
whether or not the pulp was exposed.
35
Rationale
Indirect pulp capping is based on the knowledge that
decalcication of the dentin precedes bacterial invasion
within the dentin.
3638
This technique is predicated on
removing the outer layers of the carious dentin, that
contain the majority of the microorganisms, reducing
the continued demineralization of the deeper dentin
layers from bacterial toxins, and sealing the lesion to
allow the pulp to generate reparative dentin. Fusayama
and colleagues demonstrated that in acute caries,
dentin discoloration occurred far in advance of the
microorganisms, and as much as 2 mm of softened or
discolored dentin was not infected.
38
In a later study,
Fusayama found that carious dentin actually consists of
two distinct layers having different ultramicroscopic
and chemical structures.
39
The outer carious layer is
irreversibly denatured, infected, and incapable of being
remineralized and should be removed. The inner cari-
ous layer is reversibly denatured, not infected, and
capable of being remineralized and should be pre-
served. The two layers can be differentiated clinically by
a solution of basic fuchsin.
39
Whitehead and colleagues compared deep excava-
tions in primary and permanent teeth.
40
After all soft-
ened dentin had been removed from the cavity oor,
they found that 51.5% of the permanent teeth were
free from all signs of organisms, and a further 34%
had only 1 to 20 infected dentinal tubules in any one
section.
40
Primary teeth, however, showed a much
higher percentage of bacteria in the cavity oor after
all softened dentin was removed. These results were
further supported by Shovelton, who found that
although the deepest demineralized layers of dentin
were generally free from infection, the possibility of a
few dentinal tubules containing organisms did exist,
especially in primary teeth.
41
This nding was sup-
ported by Seltzer and Bender.
42
Thus, complete clini-
cal removal of carious dentin does not necessarily
ensure that all infected tubules have been eradicated.
Conversely, the presence of softened dentin does not
necessarily indicate infection.
A number of investigators have provided evidence
that the pulp can readily cope with minute contami-
nation. Reeves and Stanley
43
and Shovelton
44
showed
that when the carious lesion proximity to the pulp was
greater than 0.8 mm (including reparative dentin
when present), no signicant disturbance occurred
within the pulp of permanent teeth. Rayner and
Southam, in studying carious primary teeth, found the
mean depth of pulp inammatory changes from bac-
terial dentin penetration to be 0.6 mm in proximity to
the pulp, with some changes occurring within a
1.8 mm pulp proximity.
23
Massler considered that
pulp reactions under deep carious lesions result from
bacterial toxins rather than the bacteria themselves.
45
Massler and Pawlak used the terms affected and
infected to describe pulp reaction to deep carious
attack.
46
This histologic study showed that the affect-
ed pulp, beneath a deep carious lesion with a thin
layer of dentin between the pulp and the bacterial
front, was often inamed and painful but contained
no demonstrable bacteria. However, when signicant
numbers of bacteria were found within the infected
pulp, a microscopic exposure in the carious dentin was
seen. Canby and Bernier concluded that the deeper
layers of carious dentin tend to impede the bacterial
invasion of the pulp because of the acid nature of the
affected dentin.
47
The results of these studies indicate the presence of
three dentinal layers in a carious lesion: (1) a necrotic,
soft, brown dentin outer layer, teeming with bacteria
and not painful to remove; (2) a rmer, discolored
dentin layer with fewer bacteria but painful to remove,
suggesting the presence of viable odontoblastic exten-
sions from the pulp; and (3) a hard, discolored dentin
deep layer with a minimal amount of bacterial invasion
that is painful to instrumentation.
Response to Treatment
Sayegh found three distinct types of new dentin in
response to indirect pulp capping: (1) cellular brillar
dentin at 2 months post-treatment, (2) presence of
globular dentin during the rst 3 months, and (3)
tubular dentin in a more uniformly mineralized pat-
tern.
17
In this study of 30 primary and permanent
teeth, Sayegh concluded that new dentin forms fastest
in teeth with the thinnest dentin remaining after cavity
preparation. He also found that the longer treatment
times enhanced dentin formation.
17
Diagnosis of the type of caries inuences the treat-
ment planning for indirect pulp capping. In the active
lesion, most of the caries-related organisms are found in
the outer layers of decay, whereas the deeper decalcied
layers are fairly free of bacteria. In the arrested lesion, the
surface layers are not always contaminated, especially
where the surface is hard and leathery. The deepest lay-
ers are quite sclerotic and free of microorganisms.
48
Deep carious dentin is even more resistant to decompo-
sition by acids and proteolysis than is normal dentin.
This was especially true in arrested caries.
49,50
Procedures for Indirect Pulp Capping
Case selection based on clinical and radiographic assess-
ment to substantiate the health of the pulp is critical for
success. Only those teeth free from irreversible signs
and symptoms should be considered for indirect pulp
capping. The following measures should be employed
for those teeth appropriate for this technique.
Indications. The decision to undertake the indi-
rect pulp capping procedure should be based on the
following ndings:
1. History
a. Mild discomfort from chemical and thermal
stimuli
b. Absence of spontaneous pain
2. Clinical examination
a. Large carious lesion
b. Absence of lymphadenopathy
c. Normal appearance of adjacent gingiva
d. Normal color of tooth
3. Radiographic examination
a. Large carious lesion in close proximity to the pulp
b. Normal lamina dura
c. Normal periodontal ligament space
d. No interradicular or periapical radiolucency
Contraindications. Findings that contraindicate
this procedure are listed below:
1. History
a. Sharp, penetrating pain that persists after
withdrawing stimulus
b. Prolonged spontaneous pain, particularly at night
866 Endodontics
2. Clinical examination
a. Excessive tooth mobility
b. Parulis in the gingiva approximating the roots of
the tooth
c. Tooth discoloration
d. Nonresponsiveness to pulp testing techniques
3. Radiographic examination
a. Large carious lesion with apparent pulp exposure
b. Interrupted or broken lamina dura
c. Widened periodontal ligament space
d. Radiolucency at the root apices or furcation areas
If the indications are appropriate for indirect pulp
capping, such treatment may be performed as a two-
appointment or a one-appointment procedure.
Two-Appointment Technique (First Sitting).
1. Administer local anesthesia and isolate with a
rubber dam.
2. Establish cavity outline with a high-speed hand-
piece.
3. Remove the majority of soft, necrotic, infected
dentin with a large round bur in a slow-speed hand-
piece without exposing the pulp.
4. Remove peripheral carious dentin with sharp spoon
excavators. Irrigate the cavity and dry with cotton
pellets.
5. Cover the remaining affected dentin with a hard-set-
ting calcium hydroxide dressing.
6. Fill or base the remainder of the cavity with a rein-
forced ZOE cement (IRM Dentsply-Caulk; Milford.)
or a glass-ionomer cement to achieve a good seal.
7. Do not disturb this sealed cavity for 6 to 8 weeks. It
may be necessary to use amalgam, composite resin,
or a stainless steel crown as a nal restoration to
maintain this seal.
Two-Appointment Technique (Second Sitting, 6 to
8 Weeks Later). If the tooth has been asymptomatic,
the surrounding soft tissues are free from swelling, and
the temporary lling is intact, the second step can be
performed:
1. Bitewing radiographs of the treated tooth should be
assessed for the presence of reparative dentin.
2. Again use local anesthesia and rubber dam isolation.
3. Carefully remove all temporary lling material,
especially the calcium hydroxide dressing over the
deep portions of the cavity oor.
4. The remaining affected carious dentin should
appear dehydrated and aky and should be easily
removed. The area around the potential exposure
Pediatric Endodontics 867
should appear whitish and may be soft; this is pre-
dentin. Do not disturb!
5. The cavity preparation should be irrigated and gen-
tly dried.
6. Cover the entire oor with a hard-setting calcium
hydroxide dressing.
7. A base should be placed with a reinforced ZOE or
glass ionomer cement, and the tooth should receive
a nal restoration.
One-Appointment Technique. The value of
re-entry and re-excavation has been questioned by
some clinicians when viewed in light of numerous
studies reporting success rates of indirect pulp capping
with calcium hydroxide ranging from 73 to 98% (Table
17-1). On this basis, the need to uncover the residual
dentin to remove dehydrated dentin and view the scle-
rotic changes has been questioned. The second entry
subjects the pulp to potential risk of exposure owing to
overzealous re-excavation.
7
Leung et al.
51
and Fairbourn and colleagues
52
have
been able to show a signicant decrease of bacteria in
deep carious lesions after being covered with calcium
hydroxide (Dycal, Dentsply-Caulk; Milford.) or a modi-
ed ZOE (IRM) for periods ranging from 1 to 15
months. These investigators suggested that re-entry to
remove the residual minimal carious dentin after cap-
ping with calcium hydroxide may not be necessary if the
nal restoration maintains a seal and the tooth is asymp-
tomatic.
After cavity preparation, if all carious dentin was
removed except the portion that would expose the pulp,
re-entry might be unnecessary.
7
Conversely, if the clini-
cian had to leave considerably more carious dentin
owing to patient symptoms, re-entry would be advised
to conrm reparative dentin and pulp exposure status. If
a pulp exposure occurs during re-entry, a more invasive
vital pulp therapy technique such as direct pulp capping
or pulpotomy would be indicated. Tooth selection for
one-appointment indirect pulp capping must be based
on clinical judgment and experience with many cases in
addition to the previously mentioned criteria.
Evaluation of Therapy. A histologic evaluation of
pulp reactions to indirect pulp capping has been report-
ed in a varying number of samples. Law and Lewis
reported irritational dentin formation, an active odonto-
blastic layer, an intact zone of Weil, and a slightly hyper-
active pulp with the presence of some inammatory
cells.
53
Held-Wydler demonstrated irritational dentin in
40 of 41 young molars in which the carious dentin was
covered with ZOE cement.
54
The pulp tissue was either
completely normal or mildly inamed over a period of
Table 17-1 Studies on Indirect Pulp Capping in Primary and Young Permanent Teeth
Study Agent Cases Observation Period % of Success
Sowden, 1956 Ca(OH)
2
4,000 Up to 7 y Very high
Law and Lewis, 1961 Ca(OH)
2
38 Up to 2 y 73.6
Hawes and DiMaggio, 1964 Ca(OH)
2
475 Up to 4 y 97
Kerkhove et al., 1964 Ca(OH)
2
41 12 mo 95
ZOE 35 12 mo 95
Held-Wydler, 1964 Ca(OH)
2
41 35630 d 88
King et al., 1965 Ca(OH)
2
21 25206 d 62
ZOE 22 88
Aponte, 1966 Ca(OH)
2
30 646 mo 93
Jordan and Suzuki, 1971 Ca(OH)
2
243 1012 wk 98
Nordstrom et al., 1974 Ca(OH)
2
64 94 d 84
SnFl 90
Magnusson, 1977 Ca(OH)
2
55 85
Sawusch, 1982 Ca(OH)
2
184 1315 mo 97
Nirschl and Avery, 1983 Ca(OH)
2
38 6 mo 94
Coll, 1988 Ca(OH)
2
26 2058 mo 92.3
Ca(OH)
2
= calcium hydroxide; ZOE = zinc oxideeugenol; SnFI = stannous uoride.
34 to 630 days. In the histologic sections, four layers
could be demonstrated (Figure 17-5): (1) carious decal-
cied dentin, (2) rhythmic layers of irregular reparative
dentin, (3) regular tubular dentin, and (4) normal pulp
with a slight increase in brous elements.
Clinical studies have shown no signicant differ-
ences in the ultimate success of this technique regard-
less of whether calcium hydroxide or ZOE cement is
used over residual carious dentin.
5557
However,
Torstenson et al. demonstrated slight to moderate
inammation when ZOE was used in deep unlined
cavities that were less than 0.5 mm to the pulp itself.
58
Nordstrom and colleagues reported that carious
dentin, wiped with a 10% solution of stannous uoride
for 5 minutes and covered with ZOE, can be remineral-
ized.
59
It was further stated that no particular differ-
ence was found in failure rates of teeth treated with cal-
cium hydroxide and those treated with stannous uo-
ride. As so many others have also concluded, the results
for primary and young permanent teeth do not differ
signicantly (see Table 17-1).
King and associates,
60
as well as Aponte et al.
61
and
Parikh et al.,
62
determined that the residual layer of
carious dentin, left in the indirect pulp-capping tech-
nique, can be sterilized with either ZOE cement or cal-
cium hydroxide. However, it cannot be presumed that
all of the remaining infected or affected dentin
868 Endodontics
becomes remineralized. In contrast to ZOE, residual
dentin will increase in mineral content when in contact
with calcium hydroxide.
63,64
Sawusch evaluated calcium hydroxide liners for
indirect pulp capping in primary and young perma-
nent teeth. After periods ranging from 13 to 21 months,
he concluded that Dycal was a highly effective agent.
65
Nirschl and Avery reported greater than 90% success
rates for both Dycal and LIFE (SybronEndo/Kerr
Corp.; Orange, Calif.) calcium hydroxide preparations
when used as bases in both primary and permanent
teeth for indirect pulp-capping therapy.
66
Coll et al., in an evaluation of several modes of pulp
therapy in primary incisors, stated that the success rates
of indirect pulp cappings in primary incisors did not
differ from comparable molar rates.
67
They showed a
92.3% success rate for treated incisors after a mean fol-
low-up time of 42 months.
The medicament choice for indirect pulp capping can
be based on the clinical history of the carious tooth in
question. Some investigators recommend ZOE because
of its sealing and obtundant properties, which reduce
pulp symptoms. Others recommend calcium hydroxide
because of its ability to stimulate a more rapid formation
of reparative dentin. Stanley believes that it makes no
difference which is used because neither is in direct con-
tact with pulp tissue, and increased dentin thickness was
observed to occur beneath deep lesions treated with both
agents.
57
However, in case of an undetected microscopic
pulp exposure during caries excavation, calcium hydrox-
ide will better stimulate a dentinal bridge.
57,68
Primosch
et al. noted that the majority of US pediatric dentistry
undergraduate programs used calcium hydroxide as the
principal indirect pulp capping medicament in their
teaching protocols.
69
Lado and Stanley demonstrated that light-cured cal-
cium hydroxide compounds were equally effective in
inhibiting growth of organisms commonly found at
the base of cavity preparations.
70
A minimum indirect pulp post-treatment time peri-
od of 6 to 8 weeks should be allowed to produce ade-
quate remineralization of the cavity oor.
7,17,71
This
desirable outcome is essentially dependent on the
maintenance of a patent seal against microleakage by
the temporary and nal restorations. In this regard, the
newer resin-reinforced glass ionomer cements and
dentin bonding agents should be considered.
DIRECT PULP CAPPING
Direct pulp capping involves the placement of a bio-
compatible agent on healthy pulp tissue that has been
inadvertently exposed from caries excavation or trau-
Figure 17-5 Photomicrograph of four layers of healing under
indirect pulp capping of a permanent molar of a 14
1
2-year-old
child. Zinc oxideeugenol cement capping after excavation of the
necrotic dentin layer only. No pain 480 days later when extracted. 1
= carious decalcied dentin; 2 = rhythmic layers of irregular irrita-
tional dentin; 3 = regular tubular dentin; 4 = normal pulp with
slight increase in brous elements. Reproduced with permission
from Held-Wydler E.
54
Pediatric Endodontics 869
matic injury
72
(Figure 17-6). The treatment objective is
to seal the pulp against bacterial leakage, encourage the
pulp to wall off the exposure site by initiating a dentin
bridge, and maintain the vitality of the underlying pulp
tissue regions (Figure 17-7).
Case Selection
Success with direct pulp capping is dependent on the
coronal and radicular pulp being healthy and free from
bacterial invasion.
73,74
The clinician must rely on the
physical appearance of the exposed pulp tissue, radi-
ographic assessment, and diagnostic tests to determine
pulpal status.
Indications. Tooth selection for direct pulp cap-
ping involves the same vital pulp therapy considerations
mentioned previously, to rule out signs of irreversible
pulp inammation and degeneration. The classic indi-
cation for direct pulp capping has been for pinpoint
mechanical exposures that are surrounded with sound
dentin.
3,7,2124
The exposed pulp tissue should be bright
red in color and have a slight hemorrhage that is easily
controlled with dry cotton pellets applied with minimal
pressure. Frigoletto noted that small exposures and a
good blood supply have the best healing potential.
75
Although imprecise, the term pinpoint conveys the
concept of smallness to the exposed tissue, which
should have the lowest possibility of bacterial access. An
empirical guideline has been to limit the technique to
exposure diameters of less than 1 mm. Stanley has
Figure 17-6 Direct pulp-capping technique. A, Capping material
covers pulp exposure and the oor of the cavity. B, Protective base
of zinc oxideeugenol cement. C, Amalgam restoration.
Figure 17-7 Effect of calcium hydroxide and time on the healing of the capped pulp. A, Twenty-four hours after application of calcium
hydroxide. B, After 2 or 3 weeks. C, After 4 or 5 weeks. D, After 8 weeks. Reproduced with permission from Vermeersch AG.
107
A B
C D
determined, however, that the size of the exposure is less
signicant than the quality of the capping technique in
avoiding contamination and mechanical trauma to the
exposure site and careful application of the medicament
to hemostatically controlled pulp tissue.
74
Equally
important is the quality of the temporary or permanent
restoration to exclude microleakage.
Contraindications. Contraindications to direct
pulp-capping therapy include a history of (1) sponta-
neous and nocturnal toothaches, (2) excessive tooth
mobility, (3) thickening of the periodontal ligament,
(4) radiographic evidence of furcal or periradicular
degeneration, (5) uncontrollable hemorrhage at the
time of exposure, and (6) purulent or serous exudate
from the exposure.
Clinical Success
The salient features of a clinically successful direct pulp-
capping treatment (with or without bridging) are (1)
maintenance of pulp vitality, (2) absence of sensitivity or
pain, (3) minimal pulp inammatory responses, and (4)
absence of radiographic signs of dystrophic changes.
Permanent Teeth. Several investigators have pro-
vided evidence that direct pulp capping cannot be suc-
cessful in the presence of pulpal inammation and
identify this condition as a contraindication to direct
pulp capping.
2
Tronstad and Mjr capped inamed
pulps in monkey teeth with calcium hydroxide or ZOE
and found no benecial healing of the exposed pulp
when calcium hydroxide was used.
76
More recently,
however, other investigators have shown in animal
870 Endodontics
studies that pulp healing can take place irrespective of
the presence of overt inammation.
77,78
Cotton
observed that when there is minimal pulp inamma-
tion, a bridge may form against the capping material,
but when inammation is more severe, the bridge is apt
to form at a distance from the exposure.
79
Dentin bridge formation has been considered to be
the sine qua non for success in response to direct pulp-
capping procedures.
73,8082
Weiss and Bjorvatn have
demonstrated, however, that a healthy pulp can exist
beneath a direct pulp cap even in the absence of a
dentinal bridge.
83
Kakehashi et al., in a germ-free ani-
mal study, found pulp exposure healing with bridging
even when left uncovered
84
(Figure 17-8). Seltzer and
Bender
42
and Langeland et al.
85
have shown that a
dentin bridge is not as complete as it appears, which
can ultimately lead to untoward pulp reactions. Cox
and Subay found that 89% of bridges formed in
response to calcium hydroxide direct pulp caps demon-
strated tunnel defects, which allowed access of
microleakage products beneath the restoration into the
pulp. They found recurrent pulp inammation
beneath 41% of all bridges formed in the sample.
86
It is generally considered that pulps inadvertently
exposed and asymptomatic in the preoperative period
are more apt to survive when capped. The prognosis is
far less favorable if an attempt is made to cap an
inamed pulp infected from caries or trauma.
87
Also,
the wide-open apices and high vascularity of young
permanent teeth enhance the successful outcome of
direct capping techniques.
Figure 17-8 Role of bacteria in dentin repair following pulp exposure. A, Germ-free specimen, obtained 14 days after surgery, with food
and debris in occlusal exposure. Nuclear detail of the surviving pulp tissue (arrow) can be observed beneath the bridge consisting of dentin
fragments united by a new matrix. B, Intentional exposure of a rst molar in a control rat (with bacteria) 28 days postoperatively. Complete
pulp necrosis with apical abscess. A reproduced with permission from Kakehashi S et al.
84
B reproduced with permission from Clark JW and
Stanley HR. Clinical dentistry. Hagerstown (MD): Harper & Row; 1976.
A B
Pediatric Endodontics 871
Primary Teeth. Kennedy and Kapala attributed
the high cellular content of pulp tissue to be responsi-
ble for direct pulp-capping failures in primary teeth.
88
Undifferentiated mesenchymal cells may give rise to
odontoclastic cells in response to either the caries
process or the pulp-capping material, resulting in
internal resorption.
Because of the pulp cellular content, increased
inammatory response, and increased incidence of
internal resorption, some pediatric dentists feel that the
direct capping procedure is contraindicated in primary
teeth.
27,89,90
Starkey and others feel that a high degree
of success with direct pulp capping in primary teeth
can be achieved in carefully selected cases using specif-
ic criteria and treatment methods.
9194
Treatment Considerations
Dbridement. Kalins and Frisbee have shown that
necrotic and infected dentin chips are invariably
pushed into the exposed pulp during the last stages of
caries removal.
95
This debris can impede healing in the
area by causing further pulpal inammation and
encapsulation of the dentin chips. Therefore, it is pru-
dent to remove peripheral masses of carious dentin
before beginning the excavation where an exposure
may occur. When an exposure occurs, the area should
be appropriately irrigated with nonirritating solutions
such as normal saline to keep the pulp moist.
81
Hemorrhage and Clotting. Hemorrhage at the
exposure site can be controlled with cotton pellet pres-
sure. A blood clot must not be allowed to form after the
cessation of hemorrhage from the exposure site as it
will impede pulpal healing.
96
The capping material
must directly contact pulp tissue to exert a reparative
dentin bridge response. Hemolysis of erythrocytes
results in an excess of hemosiderin and inammatory
cellular inltrate, which prolongs pulpal healing.
74
Exposure Enlargement. There have been recom-
mendations that the exposure site be enlarged by a
modication of the direct capping technique known as
pulp curettage or partial pulpotomy prior to the place-
ment of the capping material.
3,93,96,97
Enlarging this
opening into the pulp itself serves three purposes: (1) it
removes inamed and/or infected tissue in the exposed
area; (2) it facilitates removal of carious and noncari-
ous debris, particularly dentin chips; and (3) it ensures
intimate contact of the capping medicament with
healthy pulp tissue below the exposure site.
Cvek
98
and Zilberman et al.
99
have described highly
favorable results with this partial pulpotomy technique
for pulp-exposed, traumatized, anterior teeth and cari-
ous molars. After a 24-month waiting period, Mejare
and Cvek were able to show a 93.5% success rate of par-
tial pulpotomy in permanent posterior teeth with deep
carious lesions with exposed pulps.
100
Fuks et al. found
similar partial pulpotomy success rates above 90% in
permanent incisors with fracture-exposed pulps.
101
Bacterial Contamination. Watts and Paterson
102
and Cox
103
have both emphasized the fact that bacter-
ial microleakage under various restorations causes pul-
pal damage in deep lesions, not the toxic properties of
the cavity liners and/or restorative materials. The suc-
cess of pulp-capping procedures is dependent on pre-
vention of microleakage by an adequate seal. Cox et al.
have shown that pulp healing is more dependent on the
capacity of the capping material to prevent bacterial
microleakage rather than the specic properties of the
material itself.
104
Medications and Materials. Many medicaments
and materials have been suggested to cover pulp expo-
sures and initiate tissue healing and/or hard structure
repair. Calcium hydroxide, in one form or another, has
been singled out by a myriad of authors as the medica-
ment of choice for pulp exposures.
80,82,105,106
Antibiotics, calcitonin, collagen, corticosteroids, cyano-
acrylate, formocresol, and resorbable tricalcium phos-
phate ceramic have also been investigated, with varying
degrees of success. These latter compounds, with the
exception of formocresol, have not had sufficient clinical
impact to be adopted as the material of choice in direct
pulp capping, especially in the pediatric age groups.
Calcium Hydroxide. Calcium hydroxide produces
coagulation necrosis at the contact surface of the pulp.
The underlying tissue then differentiates into odonto-
blasts, which elaborate a matrix in about 4 weeks.
107
This results in the formation of a reparative dentin
bridge, caused by the irritating quality of the highly
alkaline calcium hydroxide, which has a pH of 11 to
12.
108
Stanley has identied that the dentin bridging
effects of calcium hydroxide occur only when the agent
is in direct contact with healthy pulp tissue.
74
Tamburic
et al. summarized the mineralizing effects of calcium
hydroxide, which include cellular adenosine triphos-
phate activation resulting from calcium and hydroxyl
ion enhancement of alkalinity in the mineralization
process.
109
Yoshiba et al. provided immunouorescence evi-
dence of the possible contribution of calcium hydrox-
ide to odontoblastic differentiation. They found
increased amounts of bronectin, an extracellular gly-
coprotein implicated in cell differentiation, among
migrating broblasts and newly formed odontoblasts
in areas of initial bridge calcication in response to cal-
cium hydroxide. They noted that although calcium
hydroxide was not unique in initiating reparative
dentinogenesis, it demonstrated the most rapid tubular
dentin formation in comparison to calcium phosphate
ceramics and tricalcium phosphate.
110
Calcium hydroxide has signicant antibacterial
action, which has been identied as an additional ben-
et in capping procedures.
111,112
Estrela et al. summa-
rized the antibacterial properties of calcium hydroxide,
which include hydrolyzing bacterial cell wall lipo-
polysaccharides, neutralizing bacterial endotoxins, and
reducing anaerobic organisms through carbon dioxide
absorption.
113
There is some controversy as to the source of calci-
um ions necessary for dentinal bridge repair at the
exposure site. Sciaky and Pisanti
114
and Attalla and
Noujaim
115
demonstrated that calcium ions from the
capping material were not involved in the bridge for-
mation. Stark and his colleagues, however, believe that
calcium ions from the capping medicament do enter
into bridge formation.
116
Holland et al. provided addi-
tional evidence to support this concept.
117
Seltzer and Bender identied the osteogenic potential
of calcium hydroxide.
42
It is capable of inducing calcif-
ic metamorphosis, resulting in obliteration of the pulp
chamber and root canals. This fact has raised concern
among clinicians.
42
Lim and Kirk, in an extensive review
of direct pulp capping literature, found little support for
pulp obliteration and internal resorption being a major
complication of pulp capping.
81
Although internal
resorption has been documented following calcium
hydroxide pulpotomies in primary teeth, it does not
appear to be a problem in permanent teeth.
Jeppersen, in a long-term study using a creamy mix
of calcium hydroxide placed on exposed pulps of pri-
mary teeth, reported a 97.6% clinical success and 88.4%
histologic success.
93
Although calcium hydroxide pastes
have been shown to be effective in promoting dentin
bridges, their higher pH, water solubility, and lack of
physical barrier strength led manufacturers to introduce
modied calcium hydroxide cements that set quickly
and hard for lining cavities and pulp capping.
Various studies have shown successful results of up
to 80% with calcium hydroxide pulp capping of
involved primary teeth with or without coronal
inammation.
65,94,96,118
These investigations support
the use of hard-set calcium hydroxide cements in place
of calcium hydroxide pastes without causing patholog-
ic sequelae, such as internal resorption, associated with
pulp-capping failure. For example, the so-called
necrobiotic and inammatory zones are minimal,
and dentin bridges seem to form directly under these
commercial compounds instead of at a distance from
872 Endodontics
the paste forms.
82,118,119
Antibacterial properties and
physical strength to support amalgam condensation
have been shown for the hard-set calcium hydroxide
cements.
51,103,120
After a clinical investigation of two formulas of a
hard, self-setting calcium hydroxide compound
(Dycal), Sawusch found calcium hydroxide liners to be
effective agents for direct and indirect pulp capping in
both primary and young permanent teeth.
65
He also
found that failures in this study tended to be associat-
ed with failed restorations and microleakage. Fuks et
al. observed an 81.5% success in young permanent
fractured teeth with pinpoint exposures when calcium
hydroxide was the capping material of choice.
121
With the advent of visible light-curing restorative
resins, it was inevitable that, in the interest of efficien-
cy and improving the hardness of a cavity lining mate-
rial, light-cured calcium hydroxide pulp-capping prod-
ucts were introduced. Stanley and Pameijer
122
and
Seale and Stanley,
123
in histologic studies, found that a
calcium hydroxide product (Prisma VLC Dycal, L. D.
Caulk Co.), cured by visible light, maintained all of the
characteristics of healing and bridge formation equiva-
lent to the original self-curing Dycal. Lado, in an in
vitro study comparing the bacterial inhibition of these
new light-cured products to the self-setting calcium
hydroxide cements, also found no differences.
112
Howerton and Cox reported the same results as Stanley
and Pameijer
122
and Seale and Stanley
123
using
light-cured calcium hydroxide in monkeys.
124
Alternative Agents to Calcium Hydroxide
Suggested for Direct Pulp Capping in Primary
and Permanent Teeth
Zinc OxideEugenol Cement. Glass and Zander
found that ZOE, in direct contact with the pulp tissue,
produced chronic inammation, a lack of calcic bar-
rier, and an end result of necrosis.
80
Hembree and Andrews, in a literature review of ZOE
used as a direct pulp-capping material, could nd no
positive recommendations.
125
Watts also found mild to
moderate inammation and no calcic bridges in the
specimens under his study,
126
and this was conrmed
by Holland et al.
127
Weiss and Bjorvatn, on the other
hand, noted negligible necrosis of the pulp in direct
contact with ZOE but stated that any calcic bridging
of an exposure site was probably a layer of dentinal
chips.
83
They also found no apparent difference in the
pulp reactions of primary and permanent teeth.
In spite of the reported lack of success with ZOE
cement, Sveen reported 87% success with the capping
of primary teeth with ZOE in ideal situations of pulp
Pediatric Endodontics 873
exposure.
128
He offered no histologic evidence, but
Tronstad and Mjr, comparing ZOE with calcium
hydroxide, found ZOE more benecial for inamed,
exposed pulps and felt that the production of a calcic
bridge is not necessary if the pulp is free of inamma-
tion following treatment.
76
Corticosteroids and Antibiotics. Corticosteroids
and/or antibiotics were suggested for direct pulp cap-
ping in the pretreatment phase and also to be mixed in
with calcium hydroxide with the thought of reducing
or preventing pulp inammation. These agents includ-
ed neomycin and hydrocortisone,
129
Cleocin,
130
corti-
sone,
131
Ledermix (calcium hydroxide plus pred-
nisolone),
132
penicillin,
133
and Kein (cephalothin
sodium).
134
Although many of these combinations
reduced pain for the most part, they were found only to
preserve chronic inammation and/or reduce repara-
tive dentin. Also, Watts and Paterson cautioned that
anti-inammatory compounds should not be used in
patients at risk from bacteremia.
135
Gardner et al.
found, however, that vancomycin, in combination with
calcium hydroxide, was somewhat more effective than
calcium hydroxide used alone and stimulated a more
regular reparative dentin bridge.
136
Polycarboxylate Cements. These cements have
also been suggested as a direct capping material. The
material was shown to lack an antibacterial effect and
did not stimulate calcic bridging in the pulps of mon-
key primary and permanent teeth.
134
Negm et al.
placed calcium hydroxide and zinc oxide into a 42%
aqueous polyacrylic acid and used this combination for
direct pulp exposure in patients from 10 to 45 years of
age. This mixture showed faster dentin bridging over
the exposures in 88 to 91% of the patients when com-
pared to Dycal as the control.
137
Inert Materials. Inert materials such as isobutyl
cyanoacrylate
138
and tricalcium phosphate ceramic
139
have also been investigated as direct pulp-capping
materials. Although pulpal responses in the form of
reduced inammation and unpredictable dentin bridg-
ing were found, to date, none of these materials have
been promoted to the dental profession as a viable
technique. At Istanbul University, dentists capped 44
pulps, half with tricalcium phosphate hydroxyapatite
and half with Dycal (calcium hydroxide). At 60 days,
none of the hydroxyapatite-capped pulps exhibited
hard tissue bridging but instead had mild inamma-
tion. Nearly all of the Dycal-capped pulps, however,
were dentin bridged, with little or no inammation.
140
Collagen Fibers. Because collagen bers are
known to inuence mineralization, Dick and
Carmichael placed modied wet collagen sponges with
reduced antigenicity in pulp-exposed teeth of young
dogs.
141
Although the material was found to be rela-
tively less irritating than calcium hydroxide, and with
minimal dentin bridging in 8 weeks, it was concluded
that collagen was not as effective in promoting a dentin
bridge as was calcium hydroxide. Fuks et al. did nd
dentin bridges after 2 months in 73% of pulpotomized
teeth that had been capped with an enriched collagen
solution.
142
They felt that a different mechanism exists
for the production of a truer dentin when a collagen
solution is used rather than with calcium hydroxide
because no coagulation necrosis was seen.
Formocresol. Because of the clinical success of
formocresol when used in primary pulp therapy such
as pulpotomies and pulpectomies, several investigators
have been intrigued by the possibility of its use as a
medicament in direct pulp-capping therapy. Arnold
applied full-strength formocresol for 2 minutes over
enlarged pulp exposures in primary teeth and found a
97% clinical success after 6 months.
97
Ibrahim et al.
reported the absence of inammation along with
dentin bridging in 15 experimental teeth when expo-
sures were medicated with formocresol for 5 minutes
and capped with a mixture of formocresol and ZOE
cement.
143
More recently, Garcia-Godoy obtained a
96% clinical and radiographic success rate in human
exposed primary molars when capped with a paste of
one-fth diluted formocresol mixed with a ZOE paste
and covered with a reinforced ZOE cement.
144
Hybridizing Bonding Agents. Recent evidence has
shown that elimination of bacterial microleakage is the
most signicant factor affecting restorative material bio-
compatibility.
145,146
A major shortcoming of calcium
hydroxide preparations is their lack of adhesion to hard
tissues and resultant inability to provide an adequate seal
against microleakage.
9,147
Furthermore, calcium hydrox-
ide materials have been found to dissolve under restora-
tions where microleakage has occurred, resulting in bacte-
rial access to the pulp.
148
Currently, hybridizing dentinal
bonding agents (such as AmalgamBond or C & B
MetaBond, Parkell Products, Farmingdale, N.Y.) represent
the state of the art in mechanical adhesion to dentin with
resultant microleakage control beneath restora-
tions.
9,149,150
Miyakoshi and et al. have shown the effec-
tiveness of 4-META-MMA-TBB adhesives in obtaining an
effective biologic seal.
151
Cox et al. demonstrated that
pulps sealed with 4-META showed reparative dentin
deposition without subjacent pulp pathosis.
152,153
A number of investigators have proposed that sealing
vital pulp exposures with hybridizing dentin bonding
agents may provide a superior outcome to calcium
hydroxide direct pulp-capping techniques.
9,154
Because
of their superior adhesion to peripheral hard tissues, an
effective seal against microleakage can be expected. These
proposals have been made in spite of concerns with the
effects of acid etchant and resin materials on pulp tissue.
Snuggs et al. demonstrated that pulpal healing
occurred, with bridge formation, in exposed primate
teeth capped with acidic materials such as silicate
cement and zinc phosphate cement. This was contin-
gent on the fact of the biologic surface seal of the over-
lying restoration remaining intact.
147
Kashiwada and
Takagi demonstrated 60 of 64 teeth to be vital and free
of any clinical and radiographic signs of pulp degener-
ation 12 months after pulp capping with a resin bond-
ing agent and composite resin. The pulp tissue was not
exposed to acid conditioner during the technique.
Selected third molars receiving this treatment were his-
tologically studied and demonstrated dentin bridge
formation below the area of exposure.
155
Heitman and Unterbrink studied a glutaraldehyde-
containing dentin bonding agent, in direct pulp-cap-
ping exposed pulps, in eight permanent teeth. All
exposed pulps were protected with calcium hydroxide
during application of the acid conditioner. After rins-
ing away the calcium hydroxide dressing and condi-
tioner, the bonding agent was applied directly to the
exposed pulp tissue and surrounding dentin. All teeth
were vital after a 6-month postoperative period.
156
These results have been further substantiated by Cox
and White and Bazzuchi et al.
153,157
Kanca reported a
4-year clinical and radiographic success with dentin
bonding agent application following etching material
applied directly to a fracture-induced exposed pulp
and dentin in rebonding a tooth fragment.
158
Conversely, other investigators provide conicting
evidence that does not support using dentin bonding
agents in pulp-capping techniques. Stanley has stated
that acid conditioning agents can harm the pulp when
placed in direct contact with exposed tissues.
159
In a
primate tooth sample with pulp exposures treated with
total-etch followed by application of a dentin bonding
agent, Pameijer and Stanley found that 45% became
nonvital and 25% exhibited bridge formation after 75
days. In the no etch calcium hydroxide pulp-capping
sample, 7% became nonvital and 82% exhibited bridge
formation after the same time period.
160
After 1 year,
Araujo et al. experienced a clinical and radiographic
success rate of 81% in primary tooth exposures etched
and capped with resin adhesives. Histologic assessment
of extracted sample teeth in advent of their exfoliation
demonstrated inammatory inltrate, microabscess
formation, and no dentin bridging. Furthermore, bac-
terial penetration occurred in 50% of the histologically
874 Endodontics
studied teeth. This occurred in spite of the nal com-
posite resin restorations being resealed at 6-month
intervals from the time of initial placement.
161
Gwinnett and Tay, using light microscopic and elec-
tron microscopic techniques, identied early and inter-
mediate pulp responses to total-etch followed by a resin
bonding agent and composite resin restoration in
human teeth. Some specimens demonstrated signs of
initial repair with dentin bridge formation along the
exposed site and reparative dentin adjacent to the
exposed site. Other specimens demonstrated persist-
ence of chronic inammation with a foreign body
response in the form of resin globules imbedded with-
in the exposed pulp tissue that were surrounded by
pulpal macrophages. This was also accompanied by a
mononuclear inammatory inltrate and an absence
of calcic bridge formation.
162
Although using dentin bonding agents as a replace-
ment for calcium hydroxide in the direct pulp-capping
technique has been advocated,
163
more long-term evi-
dence and histologic evaluation are needed. Until such
evidence is available, the clinician would be prudent to
employ a combination of calcium hydroxide as a
medicament for the exposed pulp followed by a
hybridizing resin bonding agent for a successful micro-
biologic seal.
164,165
This concept is further substantiated
by Katoh et al., who reported improved direct pulp-cap-
ping results with dentin bonding agents when they were
used in conjunction with calcium hydroxide.
166,167
Cell-Inductive Agents. A number of cell-inductive
agents have been proposed as potential direct pulp-cap-
ping alternatives to calcium hydroxide. These contempo-
rary substances mimic the reciprocal inductive activities
seen in embryologic development and tissue healing that
are receiving so much attention at this time.
Mineral trioxide aggregate (MTA) (Dentsply,
Tulsa; Tulsa, Okla.) cement was developed at Loma
Linda by Torabinejad for the purposes of root-end
lling and furcation perforation repair.
168
The mate-
rial consists of tricalcium silicate, tricalcium alumi-
nate, tricalcium oxide, and silicate oxide. It is a
hydrophilic material that has a 3-hour setting time in
the presence of moisture. Major MTA advantages
include excellent sealing ability, good compressive
strength (70 MPa) comparable to IRM, and good bio-
compatibility. Pitt Ford et al. documented superior
bridge formation and preservation of pulp vitality
with MTA when compared with calcium hydroxide in
a direct pulp-capping technique.
169
They also report-
ed normal cytokine activity in bone and cementum
regeneration in response to MTA, which is indicative
of its cell-inductive potential.
169
Pediatric Endodontics 875
Calcium phosphate cement has been developed for
repairing cranial defects following brain neurosurgery.
The components of this material include tetracalcium
phosphate and dicalcium phosphate, which react in an
aqueous environment to form hydroxyapatite, the min-
eral component of hard tissues. Chaung et al. histolog-
ically compared calcium phosphate cement with calci-
um hydroxide as a direct pulp-capping agent. Although
both materials produced similar results with respect to
pulp biocompatibility and hard tissue barrier forma-
tion, calcium phosphate cement was suggested as a
viable alternative because of (1) its more neutral pH
resulting in less localized tissue destruction, (2) its
superior compressive strength, and (3) its transforma-
tion into hydroxyapatite over time.
170
Yoshimine et al. demonstrated the potential benets of
direct pulp capping with tetracalcium phosphatebased
cement. As with calcium phosphate cement, this materi-
al has the ability to be gradually converted into hydroxy-
apatite over time. In contrast to calcium hydroxide, tetra-
calcium phosphate cement induced bridge formation
with no supercial tissue necrosis and signicant absence
of pulp inammation.
171
Summary: Direct Pulp Capping. Adherence to
established criteria for case selection is important to
achieve success. Although somewhat controversial
based on the previously reviewed studies, direct pulp
capping has been found to be less successful in pri-
mary teeth than indirect pulp therapy or coronal
pulpotomy. However, direct pulp capping tends to be
more successful in young permanent teeth.
PULPOTOMY
Pulpotomy is the most widely used technique in vital
pulp therapy for primary and young permanent teeth
with carious pulp exposures. A pulpotomy is dened as
the surgical removal of the entire coronal pulp pre-
sumed to be partially or totally inamed and quite pos-
sibly infected, leaving intact the vital radicular pulp
within the canals.
2
A germicidal medicament is then
placed over the remaining vital radicular pulp stumps
at their point of communication with the oor of the
coronal pulp chamber. This procedure is done to pro-
mote healing and retention of the vital radicular pulp.
Dentin bridging may occur as a treatment outcome of
this procedure depending on the type of medicament
used (Figure 17-9). Additional variables thought to
inuence treatment outcome include the medication
type, concentration, and time of tissue contact.
Indications. According to Dannenberg, pulpo-
tomies are indicated for cariously exposed primary
teeth when their retention is more advantageous than
extraction and replacement with a space maintainer.
172
Pulpotomy candidates should demonstrate clinical and
radiographic signs of radicular pulp vitality, absence of
pathologic change, restorability, and at least two-thirds
remaining root length. Pulpotomized teeth should
receive stainless steel crowns as nal restorations to
avoid potential coronal fracture at the cervical region.
Pulpotomy is also recommended for young permanent
teeth with incompletely formed apices and cariously
exposed pulps that give evidence of extensive coronal
tissue inammation.
Contraindications. According to Mejare, con-
traindications for pulpotomy in primary teeth exist
when (1) root resorption exceeds more than one-third
of the root length; (2) the tooth crown is nonrestorable;
(3) highly viscous, sluggish, or absent hemorrhage is
observed at the radicular canal orices; as well as (4)
marked tenderness to percussion; (5) mobility with
locally aggravated gingivitis associated with partial or
total radicular pulp necrosis exists; and (6) radiolucen-
cy exists in the furcal or periradicular areas.
173
Figure 17-9 Dentin bridge following calcium hydroxide pulpoto-
my with LIFE. (Courtesy of SybronEndo/Kerr Orange, Ca.)
Persistent toothaches and coronal pus should also be
considered contraindications.
Treatment Approaches for Primary Teeth. Ranly, in
reviewing the rationale and various medicaments that
have guided the historical development of the pulpoto-
my procedure, provided three categories of treatment
approaches. Devitalization was the rst approach to be
used with the intention of mummifying the radicular
pulp tissue.
174
The term mummied has been ascribed
to chemically treated pulp tissue that is inert, sterilized,
metabolically suppressed, and incapable of autolysis.
174
This approach involved the original two-sitting
formocresol pulpotomy, which resulted in complete
devitalization of the radicular pulp. Also included were
the 5-minute formocresol and 1:5 diluted formocresol
techniques, which both result in partial devitalization
with persistent chronic inammation.
174,175
The preservation approach involved medicaments
and techniques that provide minimal insult to the ori-
ce tissue and maintain the vitality and normal histo-
logic appearance of the entire radicular pulp.
Pharmacotherapeutic agents included in this category
are corticosteroids, glutaraldehyde, and ferric sulfate.
Nonpharmacotherapeutic techniques in this category
include electrosurgical and laser pulpotomies.
174
The regeneration approach includes pulpotomy
agents that have cell-inductive capacity to either
replace lost cells or induce existent cells to differentiate
into hard tissueforming elements. Historically, calci-
um hydroxide was the rst medicament to be used in a
regenerative capacity because of its ability to stimu-
late hard tissue barrier formation. The calcium hydrox-
ide pulpotomy is predicated on the healing of pulp tis-
sue beneath the overlying dentin bridge. Recently, its
regenerative capacity has been questioned owing to the
fact that calcium hydroxide tissue response is more
reactive than inductive. Examples of true cell-inductive
agents include transforming growth factor- (TGF-)
in the form of bone morphogenetic proteins,
176,177
freeze-dried bone,
178
and MTA.
168,169
These materials
are more representative of the regeneration category
and provide the direction for future research in vital
pulp therapy.
174
Formocresol Pulpotomy
Formocresol was introduced in 1904 by Buckley, who
contended that equal parts of formalin and tricresol
would react chemically with the intermediate and end
products of pulp inammation to form a new, colorless,
and non-infective compound of a harmless nature.
179
Buckleys formula, formocresol, consists of tricresol,
19% aqueous formaldehyde, glycerine, and water.
*
876 Endodontics
The formocresol pulpotomy technique currently
used is a modication of the original method reported
by Sweet in 1930.
180
By 1955, Sweet claimed 97% clini-
cal success in 16,651 cases.
181
It should be noted, how-
ever, that in this report, about one half of the primary
teeth exfoliated early.
Histology. In spite of regional popularity, the mul-
tiple-visit pulpotomy did not receive wide acceptance
because it was regarded as a nonvital or devitalization
method. In addition, histologic studies to support its
use were also lacking. It became overshadowed by the
so-called vital pulpotomy for primary teeth using
calcium hydroxide, which at that time was supported
by clinical and histologic evidence. Interest in
formocresol was renewed, however, with a reported
increase in clinical failures and radiographic evidence
of internal resorption with calcium hydroxide, even in
the presence of dentinal bridging.
188
At the same time,
improved clinical and histologic success rates were
reported with formocresol.
182
In spite of histologic studies that showed formalin,
creosol, and paraformaldehyde to be connective tissue
irritants, it was recognized early that formocresol is an
efficient bactericide. It was also found to have the
ability to prevent tissue autolysis by the complex
chemical binding of formaldehyde with protein.
However, this binding reaction may be reversible as
the protein molecule does not change in its basic
overall structure.
175
Massler and Mansukhani conducted a detailed his-
tologic investigation of the effect of formocresol on the
pulps of 43 human primary and permanent teeth in
multiple treatment intervals.
183
Fixation of the tissue
directly under the medicament was apparent. After a 7-
to 14-day application, the pulps developed three dis-
tinctive zones: (1) a broad eosinophilic zone of xa-
tion, (2) a broad pale-staining zone with poor cellular
denition, and (3) a zone of inammation diffusing
apically into normal pulp tissue. After 60 days, in a lim-
ited number of samples, the remaining tissue was
believed to be completely xed, appearing as a strand of
eosinophilic brous tissue.
183
Emmerson et al. also described the action of
formocresol on human pulp tissue.
184
They reported
*The formocresol used in this technique may be obtained under the
trade name Buckleys Formocresol (Roth, Chicago, IL). Composition:
35% cresol, 19% formalin in a vehicle of glycerine and water at a pH
of approximately 5.1. To dilute formocresol to one-fth strength,
thoroughly mix three parts of glycerine with one part of distilled
water. Add these four parts to one part of concentrated commercial
formocresol compound.
Pediatric Endodontics 877
that the effect on the pulp varied with the length of
time formocresol was in contact with the tissue. A
5-minute application resulted in surface xation of
normal tissue, whereas an application sealed in for 3
days produced calcic degeneration. They concluded
that formocresol pulpotomy in primary pulp therapy
may be classied as either vital or nonvital, depending
on the duration of the formocresol application.
Formocresol versus Calcium Hydroxide. Doyle et
al. compared the formocresol pulpotomy technique
with the calcium hydroxide technique in primary
canines and found the formocresol technique to be
95% clinically successful at the end of 1 year.
182
Although xation of pulp tissue and some loss of cellu-
lar denition were seen histologically, healthy, vital tis-
sue existed in the apical third. The calcium hydroxide
technique was considered to be 61% clinically success-
ful, and dentin bridge formation was seen in 50% of
the cases examined.
Spedding et al. also studied these two medicaments
in monkeys and produced essentially the same results
as Doyle and colleagues.
185
Law and Lewis evaluated
the clinical effectiveness of the formocresol technique
over a 4-year period and reported a 93 to 98% success
rate. Their failure rate was greatest between the rst
and second years.
186
Formocresol versus Zinc OxideEugenol. Berger
compared the pulpotomy effects of using a
one-appointment formocresol medication with those
of ZOE paste alone on the amputated pulps of carious-
ly exposed human primary molars.
187
Periods of eval-
uation ranged from 3 to 38 weeks postoperatively.
Clinically and radiographically, 97% of the formocre-
sol-treated teeth were judged successful, whereas only
58% of the teeth treated with ZOE were considered
successful. Histologically, 82% of the formocresol
group was judged successful, compared to total failure
with ZOE.
187
An intriguing part of this study was the nding of a
total absence of cellular detail in the apical third at 3
weeks, but by 7 weeks, connective tissue of a granular
type had ingrown through the apical foramen. In spec-
imens obtained after longer postoperative periods,
granulation tissue progressively replaced the necrotic
pulp tissue up to the coronal area. Small areas of
resorption of the dentinal walls were also being
replaced by osteodentin.
187
Spamer also conducted a histologic study of
caries-free human primary canines following a
one-appointment formocresol pulpotomy in which
the nal pulp covering was ZOE.
188
Again, the three
typical zones were distinguishable, including the api-
cal one-third tissue, which was normal and free of
inammatory reaction. Initially, Spamer observed an
acute inammatory reaction, succeeded by a chronic
inflammatory response, proliferation of odonto-
blasts, and an increase in collagen fibers. By 6
months, deposition of mature dentin and vital tissue
was seen throughout.
188
Formocresol Pulpotomy Outcomes: Primary Teeth.
Rolling and Thylstrup reported a clinical 3-year fol-
low-up study of pulpotomized primary molars using
formocresol.
189
Their results showed a progressively
decreasing survival rate of 91% at 3 months, 83% at 12
months, 78% at 24 months, and 70% at 36 months
after treatment. These investigators concluded that
although their rate of success was less than previous
studies had shown, the formocresol method must be
considered an acceptable clinical procedure compared
with other methods. Possibly, bacterial microleakage
over the longer time span accounted for their decreas-
ing success rate.
Rolling and coworkers, in later studies, investigated
the morphologic and enzyme histochemical reactions
of pulpotomies done with formocresol in human pri-
mary molars for periods ranging from 3 to 24 months
and 3 to 5 years.
190,191
In these studies, a wide range of
pulpal reactions occurred, from normal pulps to total
chronic inammation. In most instances, however, the
pulp tissue in the apical region was vital with minimal
inammation, which was in agreement with many
other studies. It was concluded from both studies that
the formocresol method should be regarded as only a
means to keep primary teeth with pulp exposures func-
tioning for a relatively short period of time.
Magnusson investigated therapeutic (ie, formocre-
sol) pulpotomies and stated that his histologic exami-
nations revealed early capricious diffusion of the
medicament through the pulp tissue, producing chron-
ic inammation and no healing in the apical areas along
with a small percentage of internal resorption.
192
From
a biologic standpoint, Magnusson felt that formocresol
was biologically inferior to calcium hydroxide in the
pulpotomy technique as the latter manifested true signs
of healing but in a low percentage in primary teeth.
192
Ranley and Lazzari concluded, however, that variations
in the interpretation of histologic studies with
formocresol, on either vital or nonvital tissue, are attrib-
utable to the length of exposure of the radicular tissue
to the drug, but there is no true healing.
193
In general, the results of many histologic studies on
the formocresol pulpotomy have shown that several
distinct zones are usually present in the pulp following
the application of the medicament:
1. Supercial debris along with dentinal chips at the
amputation site
2. Eosinophil-stained and compressed tissue
3. A palely stained zone with loss of cellular denition
4. An area of brotic and inammatory activity
5. An area of normal-appearing pulp tissue considered
to be vital
Formocresol Addition to Sub-base. Beaver et al.
investigated the differences in pulp reactions between a
5-minute application of formocresol using sub-bases of
either ZOE cement alone or with the addition of
formocresol.
194
There was no appreciable difference in
a histologic reaction of the remaining radicular pulp
tissue under either of these two types of sub-bases.
An alternative procedure reported clinically and his-
tologically successful is to incorporate diluted
formocresol into the ZOE dressing and then place it on
the pulpal stumps instead of a moistened formocresol
cotton pellet.
17,195,196
Ranly and Pope have shown in
vitro and in vivo that formocresol can leach out from a
ZOE sub-base when the two substances are com-
bined.
197
They have suggested that the initial applica-
tion of a formocresol-saturated cotton pellet on the
pulp might be an unnecessary step.
Formocresol Dilution. Venham suggested that
formocresol might be reduced to one-quarter strength
in the pulpotomy application.
198
The combined investi-
gations of Straffon and Han
199,200
and Loos et al.
201
on
the histologic and biochemical effects of formocresol
introduced new thinking in this type of pulp therapy.
Straffon and Han concluded from a study of connective
tissue in hamster pulps exposed to formocresol that the
medicament does not interfere with a prolonged recov-
ery of connective tissue and may even suppress the ini-
tial inammatory reaction. In a later report, they con-
cluded that formocresol at 1:5 strength might be equally
effective and possibly a less damaging pulpotomy agent.
Loos and colleagues concurred with the previous work
in a further study of diluted formocresol.
201
Morawa and
colleagues, in a 5-year clinical study of 70 cases, found
that the formocresol pulpotomy, using a 1:5 concentra-
tion, was as effective as a full concentration and also has
the advantage of reduced postoperative complications in
the periradicular region. In only ve teeth was there lim-
ited radicular internal resorption.
202
Fuks and Bimstein used this one-fth dilution of
formocresol in a clinical and radiographic study of pri-
mary teeth over a period of 4 to 36 months.
203
The clin-
ical success rate was reported at 94.3%, and 39% of 41
cases showed a slightly higher rate of premature root
resorption. Twenty-nine percent had radiographic evi-
878 Endodontics
dence of a root canal obliteration process. In a later
study with rhesus monkeys, using full-strength
formocresol compared with a 20% dilution, these
investigators found the same premature root resorp-
tion but a milder pulpal inammatory response with
the diluted concentration.
204
Garcia-Godoy, however,
did not nd any differences histologically between full-
strength and a one-fth dilution of formocresol when
applied in several ways over the amputated pulps.
195
Outcomes. Citing an 80% success rate of primary
molars pulpotomized with formocresol, Wright and
Widmer also found early root resorption of the pulpo-
tomized molars in comparison to the untreated
antimeres.
205
The permanent successors, however, were
not found to erupt signicantly earlier, as has been pre-
viously reported.
The hard tissue deposition or calcication of the
root canal walls following a formocresol pulpotomy
has also been observed radiographically in several
other studies.
203,206,207
These ndings imply that the
use of formocresol does not result in a complete loss of
pulp vitality.
More recently, the ndings of a retrospective radi-
ographic study of the formocresol pulpotomy tech-
nique with a post-treatment time ranging from 24 to
87 months were reported by Hicks et al.
196
In this
study, a ZOE paste into which full-strength formocre-
sol was incorporated was placed in the pulp chamber
after coronal amputation followed by restoration with
a stainless steel crown. Based on radiographic evalua-
tion criteria, which included abscess formation, radi-
olucencies, pathologic root resorption, calcic meta-
morphosis, and advanced or delayed exfoliation, the
procedure was considered to be successful in 93.8% of
the cases. Coll et al. compared the techniques of
formocresol pulpotomy versus pulpectomy in primary
incisors. They concluded that the pulpotomy was the
preferred technique for these teeth.
67
Formocresol Pulpotomy Technique in Primary Teeth
Correct diagnosis is essential to ensure the clinician
that inammation is limited to the coronal pulp.
208
Biopsy studies of pulp tissue removed from the open-
ing of root canals under pulpotomies have demonstrat-
ed the unreliability of clinical assessments in primary
teeth.
192
Radiographic examinations are therefore nec-
essary to conrm the need for pulpotomy therapy in
primary teeth. It is judicious to take bitewing and peri-
radicular radiographs so that the depth of caries may
be observed and the condition of the periradicular tis-
sues determined. Mejare found only a 55% success rate
in primary molars with either coronal or total chronic
Pediatric Endodontics 879
pulpitis that were treated by formocresol pulpotomy
after 2
1
2 years.
209
One-Appointment Pulpotomy. Indications. This
method of treatment should be carried out only on
those restorable teeth in which it has been determined
that inammation is conned to the coronal portion of
the pulp. When the coronal pulp is amputated, only
vital, healthy pulp tissue should remain in the root
canals (Figure 17-10).
Contraindications. Teeth with a history of spon-
taneous pain should not be considered. If profuse
hemorrhage occurs on entering the pulp chamber, the
one-step pulpotomy is also contraindicated. Other
contraindications are pathologic root resorption, roots
that are two-thirds resorbed or internal root resorp-
tion, interradicular bone loss, presence of a stula, or
presence of pus in the chamber (Figure 17-11).
Procedure.
1. Anesthetize the tooth and tissue.
2. Isolate the tooth to be treated with a rubber dam.
3. Excavate all caries.
4. Remove the dentin roof of the pulp chamber with a
high-speed ssure bur (Figure 17-12, A).
5. Remove all coronal pulp tissue with a slow-speed
No. 6 or 8 round bur (Figure 17-12, B). Sharp spoon
excavators can remove residual tissue remnants.
6. Achieve hemostasis with dry cotton pellets under
pressure.
7. Apply diluted formocresol to the pulp on a cotton
pellet for 3 to 5 minutes
210
(Figure 17-12, C).
8. Place a ZOE cement base without incorporation of
formocresol (Figure 17-12, D).
9. Restore the tooth with a stainless steel crown.
Two-Appointment Pulpotomy. Indications. The
two-appointment technique is indicated if there is (1)
evidence of sluggish or profuse bleeding at the ampu-
tation site, (2) difficult-to-control bleeding, (3) slight
purulence in the chamber but none at the amputation
site, (4) thickening of the periodontal ligament, or (5)
a history of spontaneous pain without other con-
traindications. The two-step pulpotomy can also be
used when shorter appointments are necessary to facil-
itate patient management problems. Miyamoto sug-
gested the two-appointment technique for uncoopera-
Figure 17-10 One-appointment formocresol pulpotomy. A, Root of the pulp chamber and coronal pulp removed. Cotton pellet with
formocresol in place for 5 minutes. B, Successful formocresol pulpotomy 1 year following treatment. (A courtesy of Dr. Constance B. Greeley;
B courtesy of Dr. Mark Wagner.)
Figure 17-11 Final failure of formocresol pulpotomy, mandibular
rst primary molar. Root resorption and interradicular bone loss
(arrows) prior to treatment forecast eventual failure. The tooth was
extracted. Reproduced with permission from Law DB, Lewis TM,
Davis JM. An atlas of pedodontics. Philadelphia: WB Saunders;
1969.
A
B
tive children to minimize chair time, especially for the
initial operative visit.
211
Contraindications. This technique should not be
done for teeth that are (1) nonrestorable, (2) soon to be
exfoliated, or (3) necrotic.
Procedure.
1. The steps are the same as for the one-appointment
procedure through step 6.
2. A cotton pellet moistened with diluted formocresol
is sealed into the chamber for 5 to 7 days with a
durable temporary cement.
880 Endodontics
3. At the second visit, the temporary lling and cotton
pellet are removed and the chamber is irrigated with
hydrogen peroxide.
4. A ZOE cement base is placed.
5. The tooth is restored with a stainless steel crown. As
previously stated, Verco and Allen found no differ-
ence in the success rate between one-stage and
two-stage procedures.
212
Avram and Pulver surveyed Canadian, American,
and selected dental schools throughout the world as
well as a limited number of pediatric dental specialists
Figure 17-12 Step-by-step technique in one-appointment formocresol pulpotomy. A, Exposure of pulp by roof removal. B, Coronal pulp
amputation with a round bur. Hemostasis with dry cotton or epinephrine. C, Application of formocresol for 1 minute. Excess medicament
is expressed from cotton before placement. D, Following formocresol removal, zinc oxideeugenol base and stainless steel crown are placed.
A B
C D
Pediatric Endodontics 881
to determine medicament choice and clinician attitude
toward pulpotomy therapy prevalent at the time of
investigation.
213
The most prevalent medicament used
in pediatric dental departments (40.8%) was
full-strength formocresol, followed by 36% for the 1:5
dilution. This 1:5 dilution was used by 50% of the pedi-
atric specialists, whereas 42% used-full strength
formocresol. Primosch et al. surveyed predoctoral
pediatric dentistry programs in 53 US dental schools to
determine the prevalence and types of primary tooth
pulp therapy techniques taught in those institutions.
Formocresol was the most widely taught pulpotomy
medicament, with 71.7% of the programs using dilut-
ed formocresol and 22.6% full-strength formocresol.
Zinc oxideeugenol was the base material of choice for
92.4% of all programs surveyed.
69
Clinical experience has shown that pulpotomized
primary molars are susceptible to cuspal and cervical
fracture. For this reason, the restoration of choice is a
well-tted stainless steel crown. Additional advan-
tages of this restoration include elimination of recur-
rent decay, elimination of intracoronal restoration
fracture, and reduction of microleakage. Although
composite resin restorations, incorporating the
dentin bonding agents, have been proposed for
pulpotomized primary molars, more studies are indi-
cated to determine their effectiveness relative to stain-
less steel crowns.
PULPOTOMY FOR YOUNG PERMANENT TEETH
Treatment of severely decayed and pulpally involved
young permanent teeth in the child or adolescent cre-
ates a dilemma. Complete endodontic therapy and a
cast full-crown restoration have been considered to be
the ideal treatment. However, this is time consuming
and, in many instances, beyond the family nancial
resources. Most importantly, canal obturation for
incompletely formed roots and open apices presents
unique problems with conventional endodontic tech-
niques. The relatively thin dentin walls of the large
obturated canals place the tooth at greater risk for root
fracture over time. In these instances, the treatment
objective is to maximize the opportunity for apical
development and closure, known as apexogenesis, and
enhance continual root dentin formation. These
objectives can occur only if the radicular pulp is main-
tained in a healthy statethe intent of the pulpotomy
technique. Although calcium hydroxide has been the
most recommended pulpotomy medicament for pul-
pally involved vital young permanent teeth with
incomplete apices, formocresol has also been proposed
as an alternative.
Formocresol
The well-documented success with formocresol pulpo-
tomies in primary teeth has led a number of clinicians
to extrapolate the use of this medication in young per-
manent teeth with a vital or, in some instances, nonvi-
tal pulp status at the start of operative treatment.
Canosa reported the widespread use of formocresol
pulpotomy in Cuba for all restorable molars with vital
pulps only. Restorable necrotic molars, as well as pre-
molars and anterior teeth, received full root canal ther-
apy. She reported an empirical success rate of 75% with
formocresol pulpotomies. Those cases that failed were
treated by endodontic cleaning, shaping, and lling
(I Canosa, personal communication, March 1994).
Ibrahim et al. studied the use of formocresol as a
pulpotomy medication in the permanent teeth of two
dogs and a monkey for up to 20 weeks.
214
Radio-
graphically, no evidence of apical pathosis was seen.
Histologically, calcication in the canal, continued api-
cal closure, and partial bridging were noted. Areas of
inammation were replaced with connective tissue.
Using formocresol, Trask reported clinical success
treating 43 permanent teeth with necrotic pulps in an
age range of 7 to 23 years.
215
Eight of these patients were
under 10 years of age, when root apices are presumed to
be still open. Trask sealed a small formocresol cotton
pellet in the pulp chamber by amalgam restoration or
stainless steel crown for an observed period of 14 to 33
months. The treated teeth were asymptomatic except in
one instance in which the tooth had to be retreated in
the same manner. He felt that the permanent tooth
formocresol pulpotomy was a better alternative than
extraction as conventional endodontics was economi-
cally unfeasible in this cohort of patients. He considered
it to be a temporizing treatment only and not a substi-
tute for complete root canal therapy, which was advo-
cated at a later date.
215
Myers also conducted a clinical study of formocresol
treatment in pulpless permanent molars. Sixty-six
cases were evaluated clinically for periods of time rang-
ing from 3 to 22 months. Fifty-six of the treated teeth
(85%) radiographically demonstrated elimination or
marked reduction of initial periradicular rarefaction.
Three of the teeth (4.5%) showed no change in appear-
ance, and seven teeth (10.6%) exhibited an increase in
periradicular rarefaction. An important nding was the
observation that all of the teeth treated with formocre-
sol exhibited continued apexication and increase in
root length.
216
Armstrong et al. found the same as well
as intracanal calcication.
217
Fiskio undertook a 5-year clinical study of 148 per-
manent teeth, using either a one-step or two-step
formocresol pulpotomy.
218
Ninety-one percent
required no further treatment. In the remaining 9%,
the initial use of formocresol did not prevent endodon-
tic therapy at a later date. The age of the patients at the
start of treatment had no signicant effect.
Spedding, in discussing the use of formocresol for
permanent molars, stated that a plug of xed tissues
forms in the root canals that can easily be removed
with endodontic instruments.
219
This is in contrast to
teeth treated with calcium hydroxide. He concluded,
however, that although few failures with formocresol
had been reported in permanent teeth, this treatment
rationale is empirical, and more denite information
about failures is needed.
Rothman observed 165 pulpotomized human perma-
nent teeth for 2 years with a two-treatment formocresol
medication.
220
He reported an average success rate of
71% as judged clinically and radiographically. Intracanal
calcication was seen in only three teeth.
Fuks et al., in studying radiographs of formocresol
pulpotomies in young permanent teeth of monkeys at
the end of 1 year, observed a favorable response with both
full-strength and diluted medication for continuing root
development and closed apices.
204
Histologically, mild
internal resorption was seen at a later date. The investiga-
tors stated that neither concentration produced ideal
results, but a milder degree of inammation was seen in
the diluted group.
Schwartz, surveying a group of Canadian practition-
ers and faculty on the use of formocresol for pulpo-
tomies in young permanent teeth, found that the
respondents felt that the procedure was a compromise
and that the teeth should be treated with conventional
endodontics at a later date.
221
Muniz et al. histologically studied 26 young perma-
nent teeth treated with the formocresol technique 5 to
20 months postoperatively.
222
This investigation was
based on an earlier study by Muniz in which he found
an overall success rate of 92% in both vital and nonvital
permanent teeth. He found inammation and necrosis
in the cervical third but brosis and osteodentin pre-
dominantly in the apical third, a response that seems to
indicate stages of biologic scar healing that probably
require around 10 to 20 months to be seen.
Akbar investigated the differences in formocresol
pulpotomy in permanent teeth with acute and chronic
pulpitis over a 5-year period.
223
On the basis of clinical
criteria only, he found the treatment to be more suc-
cessful in the acute pulpitis group (81%) than in the
chronic pulpitis group (70%).
In reviewing the literature on apical histologic
response to formocresol pulpotomies, Nishino identi-
882 Endodontics
ed a fallacy in extrapolating its success in primary
teeth to its use in permanent teeth.
224
A consistent
nding in pulpotomized primary teeth has been the
ingrowth of connective tissue through the apex in a
coronal direction through the pulpal areas of chroni-
cally inamed and brosed tissue. He identied that
favorable clinical responses could mask the reality of
histologic pulpal degeneration. Late symptoms from
pulp degeneration in pulpotomized primary teeth are
eliminated owing to their exfoliation. Young perma-
nent teeth, however, may have a greater potential for
developing periradicular infection with this technique
owing to the longer time exposure to the inammatory
degenerative process. Conversely, he hypothesized that
the formocresol treatment might be effective because
the open apical foramen of immature permanent teeth
would be conducive to an ingrowth of connective tissue
at the apex in the form of proliferating broblasts.
224
Because linear osteodentin calcication may develop
as a response to formocresol pulpotomies over time,
there has been considerable concern expressed by
endodontists of the difficulty in renegotiating treated
young permanent canals after the apices have closed.
Calcium Hydroxide
Calcium hydroxide was most favored as a pulpotomy
agent in the 1940s and mid-1950s because it was
thought to be more biologically acceptable owing to
the fact that it promoted reparative dentin bridge for-
mation and pulp vitality was maintained. This ration-
ale was introduced by Teuscher and Zander in 1938,
who described it as a vital technique.
225
Their histo-
logic studies showed that the pulp tissue adjacent to the
calcium hydroxide was rst necrotized by the high pH
(11 to 12) of the calcium hydroxide. This necrosis was
accompanied by acute inammatory changes in the
underlying tissue. After 4 weeks, a new odontoblastic
layer and, eventually, a bridge of dentin developed
(Figure 17-13). Later investigations showed three iden-
tiable histologic zones under the calcium hydroxide in
4 to 9 days: (1) coagulation necrosis, (2) deep-staining
basophilic areas with varied osteodentin, and (3) rela-
tively normal pulp tissue, slightly hyperemic, underly-
ing an odontoblastic layer.
As with direct pulp capping, the presence of a denti-
nal bridge is not the sole criterion of success. The
bridge may be incomplete and may appear histologi-
cally as doughnut, dome, or funnel shaped or lled
with tissue inclusions.
226,227
It is also possible for the
remaining pulp to be walled off by brous tissue with
no dentin bridge evident radiographically. Initial
reports by Berk and Brown indicated a success rate
Pediatric Endodontics 883
with calcium hydroxide for primary and young perma-
nent teeth in the range of 30 to 90%.
228,229
Calcium Hydroxide Pulpotomy Outcomes in
Primary Teeth
Via, in a 2-year study of calcium hydroxide pulpo-
tomies in primary teeth, had only a 31% success,
230
and
Law reported only a 49% success in a 1-year study.
231
In all investigations, failure was the result of chronic
pulpal inammation and internal resorption.
Magnusson
192
and Schrder and Granath
232
found
similar high failure rates with calcium hydroxide in
pulpotomized primary molars.
Internal resorption may result from overstimulation
of the primary pulp by the highly alkaline calcium
hydroxide. This alkaline-induced overstimulation
could cause metaplasia within the pulp tissue, leading
to the formation of odontoclasts (Figure 17-14). In
addition, undetected microleakage could allow large
numbers of bacteria to overwhelm the pulp and nullify
the benecial effects of calcium hydroxide.
Schrder also evaluated the progress of 33 pulpo-
tomized primary molars with calcium hydroxide as a
wound dressing.
233
After 2 years, the success rate was
59%, with failures manifested as internal resorption.
Histologic study revealed extra pulpal blood clots, over
the amputated sites, which Schrder felt interfered with
pulpal healing and dentin bridge formation.
In spite of these earlier discouraging reports, Phaneuf
et al. demonstrated signicant primary tooth pulpoto-
my success with calcium hydroxide in commercial
preparations such as Pulpdent (Pulpdent Corporation
Figure 17-13 Calcium hydroxide pulpotomy, young perma-
nent molar. A, Pulp of a rst permanent molar exposed by
caries (white arrow). B, Calcied dentin bridges (arrows) over
vital pulp in canals. Note open apices. C, Pulp recession
(arrows) and continued root development indicative of contin-
uing pulp vitality. Reproduced with permission from
McDonald RE. Dentistry for the child and adolescent. 2nd ed.
St. Louis: CV Mosby; 1974.
Figure 17-14 Massive internal resorption (arrows) of primary
mandibular molars after calcium hydroxide pulpotomy.
A
C
B
of America; Watertown, Mass.) and Dycal.
106
The dif-
ference in pulp response to these commercial prepara-
tions might be attributed to their lower pH values.
Calcium hydroxide incorporated in a methylcellulose
base, such as Pulpdent, showed earlier and more consis-
tent bridging than did other types of calcium hydroxide
preparations. Berk and Krakow
234
and Schrder
233
have
extensively studied calcium hydroxide pulpotomies and
believe that the state of the pulp, surgical trauma, or
amputation treatment may be more important than the
calcium hydroxide per se in inducing success. At pres-
ent, the calcium hydroxide pulpotomy technique can-
not be generally recommended for primary teeth
owing to its low success rate.
89,184,235
Permanent Tooth Pulpotomy: Indications
and Contraindications
Because of improved clinical outcomes, calcium
hydroxide is the recommended pulpotomy agent for
carious and traumatic exposures in young permanent
teeth, particularly with incomplete apical closure
(Figure 17-15). Following the closure of the apex, it is
generally recommended that conventional root canal
obturation be accomplished to avoid the potential
long-term outcome of root canal calcication.
236
Procedure.
1. Anesthetize the tooth to be treated and isolate under
a rubber dam.
884 Endodontics
2. Excavate all caries and establish a cavity outline.
3. Irrigate the cavity with water and lightly dry with
cotton pellets.
4. Remove the roof of the pulp chamber with a
high-speed ssure bur.
5. Amputate the coronal pulp with a large low-speed
round bur or a high-speed diamond stone with a
light touch.
237
6. Control hemorrhage with a cotton pellet applied with
pressure or a damp pellet of hydrogen peroxide.
7. Place a calcium hydroxide mixture over the radicu-
lar pulp stumps at the canal orices and dry with a
cotton pellet.
8. Place quick-setting ZOE cement or resin-reinforced
glass ionomer cement over the calcium hydroxide to
seal and ll the chamber.
9. If the crown is severely weakened by decay, a stain-
less steel crown rather than an amalgam restoration
should be used to prevent cusp fractures (Figure 17-
16).
ALTERNATIVES TO FORMOCRESOL IN
PRIMARY TEETH
Although diluted formocresol is currently the recom-
mended agent for pulpotomy treatment for carious
pulp exposures in vital primary teeth, some concern
has been expressed regarding its use as a pulp medica-
tion because of its biocompatibility deciencies. The
formaldehyde component of the medicament and its
Figure 17-15 Calcium hydroxide pulpotomies in young permanent teeth. A, Crown fracture exposure of a central incisor. The apex was
open at the time of pulpotomy. Note root growth, apical closure, and the dentin bridges (arrows). B, Partial root canal calcication (arrows)
following pulpotomy in a young rst permanent molar.
A
B
Pediatric Endodontics 885
close derivatives have been implicated for exerting
potentially harmful systemic and local effects.
Formocresol may not be conned solely to the radic-
ular tissue. Various investigations by Pashley et al.
238
and
Myers et al.
239
showed systemic uptake and tissue injury
of labeled formaldehyde that was later found in dentin,
periodontal tissue, bone, plasma, kidneys, and lungs.
Ranly and Horn, in studying the ingredients and actions
of formocresol, stated that although high levels of
formaldehyde or cresol can be mutagenic or carcino-
genic and produce histologic failures pulpally, it is not
realistic that enough multiple pulpotomies would be
performed to bring about a toxic systemic level.
240,241
Messer et al. reported a signicant number of enam-
el defects in the succedaneous teeth under formocresol
pulpotomies.
242
Rollings and Paulsen
243
and Mulder et
al.,
244
however, found no difference in the prevalence of
enamel defects in permanent teeth in relation to
formocresol pulpotomies.
Because of the potential concerns in the use of
formaldehyde in dentistry, it has been suggested that
research in alternative formulations be conducted for
use in pediatric pulpal therapy.
245
In spite of these con-
cerns, formocresol remains as the benchmark medica-
ment to which alternative agents are compared.
Sandler et al. sealed in Cresatin as the medicament
in pulpotomy and protected it with a covering of Cavit
(Premier Dental Products, Plymouth Meeting,
Mass.).
246
Clinically, only one failure occurred in their
test group. Histologically, tissue xation appeared at
the amputation site, and the apical-third pulp demon-
strated vital tissue in 84% of the 21 cases examined.
Nevins et al. were very successful in producing
dentin bridging and canal calcication using colla-
gen-calcium phosphate gel cross-linked with 0.6% glu-
taraldehyde to increase rmness and ber stability.
247
Fuks et al., using native collagen solutions enriched
with cell nutrients that promote cell proliferation and
healing of incision wounds, showed complete healing
of pulpotomized teeth in dogs and monkeys.
142
Glutaraldehyde
It was suggested by s-Gravenmade that formaldehyde
did not represent the ideal pulp xative in clinical
endodontic therapy. Inamed tissue that produces
toxic by-products should be xed rather than treated
with strong disinfectants.
248
He felt that satisfactory
xation with formocresol requires an excessive amount
of medication, as well as a longer period of interaction.
These requirements may lead to undesirable effects at
the periapex.
Also, the reactions of formaldehyde with proteins
should be considered less than stable and may be
reversible. He felt that a glutaraldehyde solution might
replace formocresol in endodontic therapy because of
its xative properties and bactericidal effectiveness and
result in less destruction of tissue.
Hill et al. compared glutaraldehyde to formocresol
in vitro with respect to its antimicrobial and cytotoxic
effects. Minimal antimicrobial concentrations were
3.125% for glutaraldehyde and 0.75% for formocresol.
More importantly, at these concentrations, glutaralde-
hyde was found to be less cytotoxic when used as a
pulpotomy agent. Formocresol at its lower concentra-
tion, however, was considerably more antimicrobial
than glutaraldehyde.
249
Wernes and s-Gravenmade, in an in vivo study of
permanent and primary dentitions, in which some
teeth were vital and others nonvital, found no evidence
of periradicular inammation after the application of
glutaraldehyde.
250
Dankert and colleagues found only
minimal diffusion through the apices.
251
The following attributes have been ascribed to glu-
taraldehyde as a more desirable medicament for pulpal
therapy when compared to formocresol: (1) it is a
bifunctional reagent, which allows it to form strong
intra- and intermolecular protein bonds, leading to
Figure 17-16 Calcium hydroxide pulpotomy in a young perma-
nent molar. The cavity is prepared, caries and the chamber roof are
removed, and the pulp is amputated to the canal orices. Following
hemostasis, commercial calcium hydroxide is placed and protected
with zinc oxideeugenol and amalgam lling or a stainless crown.
A, Vital pulp. B, Calcium hydroxide. C, Zinc oxideeugenol
quick-set cement. D, Amalgam.
superior xation by cross-linkage; (2) its diffusibility is
limited; (3) it is an excellent antimicrobial agent; (4) it
causes less necrosis of pulpal tissue; and (5) it causes
less dystrophic calcication in pulp canals.
In an initial clinical study, Kopel and colleagues used
a 2% glutaraldehyde solution as a medicament for
pulpotomies in vivo for cariously exposed primary
molars.
252
Histologic evaluations were made on
extracted teeth at 1 month, 3 months, 6 months, and 1
year. The most striking nding from this study was
that, histologically, the remaining root pulp tissue did
not resemble pulp tissue subjected to formocresol.
There was an initial zone of xation adjacent to the
dressing that did not proceed apically. The tissue
adjoining the xed zone and down to the apex had the
cellular detail of normal pulp and was presumably vital
(Figure 17-17). It was suggested that 2% glutaralde-
hyde, because of its biochemical effects on the pulp,
can be used for pulpotomies in primary teeth.
Following this initial clinical investigation with glu-
taraldehyde, many in vitro and in vivo studies began
with important implications and ndings for its use in
pediatric pulp therapy. Dilly and Courts found that
glutaraldehyde did not stimulate a signicant immune
response.
253
Lekka et al. later found that only a minimal
amount of glutaraldehyde diffused through the radicu-
lar pulp tissue when compared to formocresol.
254
Clinical studies in primary teeth have been conduct-
ed by Garcia-Godoy,
255
Fuks et al.,
256
and Alacam
257
for
periods ranging from 12, 19, and 42 months. Respective
success rates were found to be 98, 90.4, and 96%. Root
canal obliteration and internal resorption were seen in
the radiographs in a small percentage of the cases in
Fuks et al.s study. Other studies have investigated vari-
ous aspects in the use of glutaraldehyde as a pulpotomy
medicament such as concentration, pH, time, and
method of application as contrasted to the original val-
ues when it was rst used.
258260
After several investigations, Ranly et al. concluded
that buffering glutaraldehyde, increasing its concentra-
tion, and applying it for longer time periods all
enhanced the degree of xation.
261
They suggested that
clinical treatment might involve buffered glutaralde-
hyde at either 4% for 4 minutes or 8% for 2 minutes.
Lloyd et al. felt that the tissue becomes more stable with
longer application times of 2% glutaraldehyde.
260
Although Ranly and coworkers originally suggested
that glutaraldehyde might be incorporated in a ZOE
base over a pulpotomy,
261
a later clinical study found a
48.6% rate of failure with this procedure.
262
Hernandez et al. evaluated the clinical and radi-
ographic results of pulpotomies in permanent molars
886 Endodontics
medicated with either formocresol or 2% glutaralde-
hyde.
263
The observations showed a return to a more
normal trabecular bone pattern in perialveolar bone
after 2 years with the glutaraldehyde compared to the
formocresol treatment.
The same concerns that related to the systemic
absorption of formocresol have been expressed with
the use of glutaraldehyde in pulp therapy. Myers et al.
demonstrated some systemic absorption with ultimate
excretion of
14
C-glutaraldehyde following a 5-minute
application of 2% glutaraldehyde to multiple pulpoto-
my sites in dogs.
264
Figure 17-17 Glutaraldehyde pulpotomy. A, Section of the root of
a primary molar treated with glutaraldehyde 1 month earlier. Note
the Schiff-positive homogenous zone (S) in the coronal region. B,
Pulp tissue adjacent to the coronal region has dilated veins and
absence of inammatory cells. C, Tissue in the apical region is also
free of inammatory cells. A wide area of new irritational dentin is
evident. At 1 year, the collagen concentration increases with mild
inammation. Reproduced with permission from Kopel HM, et al.
The effect of gluteraldehyde on primary pulp tissue following coro-
nal amputation. J Dent Child 1980;47:425.
B
A C
Pediatric Endodontics 887
Ranly et al. also investigated the systemic distribu-
tion of 4% infused glutaraldehyde pulpotomies in rats
and found only an approximate 25% of the applied
dose. These investigators concluded that the use of glu-
taraldehyde as a pulpotomy agent in humans would be
free of any signicant toxicity.
265
Astringents
Schrder and Granath documented the fact that pulpal
hemorrhage control is critical for pulpotomy suc-
cess.
232
Kouri et al. compared formocresol pulpotomies
in primary teeth using epinephrine versus sterile water
and cotton pellets for hemorrhage control. After 6-
week to 3-month post-treatment periods, histologic
and electron microscopic evidence of healing was sim-
ilar for both groups. Bleeding times for the epineph-
rine-treated pulps were 50 seconds versus 251 seconds
for the sterile watertreated pulps. Less extravasated
blood occurred with the epinephrine-treated pulps and
was limited to the amputation site. No clinical or radi-
ographic failures occurred for either group.
266
Helig et al. compared aluminum chloride versus
sterile water in achieving hemostasis prior to medica-
ment placement in calcium hydroxide pulpotomies for
primary teeth in humans. They found a 25% radi-
ographic failure rate in the sterile water group versus
no radiographic failures with the aluminum chloride
group after 9 months.
267
Ferric sulfate has received the most recent attention
as a formocresol alternative in pulpotomy choices. This
material, when in contact with tissue, forms a ferric
ion-protein complex that mechanically occludes capil-
laries at the pulpal amputation site. The subjacent pulp
tissue is then allowed to heal. Landau and Johnson
found a more favorable pulpal response to a 15.5% fer-
ric sulfate solution than calcium hydroxide in primate
pulpotomies after 60 days.
268
Fei et al. found a com-
bined clinical and radiographic success rate of 96.3%
for ferric sulfate pulpotomies versus a 77.8% success
rate for diluted formocresol pulpotomies in humans
after 12 months.
269
Fuks et al. found a 92.7% success rate with ferric
sulfate versus 83.8% with diluted formocresol in pri-
mary tooth pulpotomies after a mean post-treatment
time of 20.5 months. They noted that these differences
were not statistically signicant and therefore conclud-
ed the success rates to be similar for both groups.
270
Fuks et al. conducted a histologic study of ferric sulfate
versus diluted formocresoltreated pulps in primate
teeth at 4- and 8-week observation periods. Mild
inammation was evident in 58% of the ferric sulfate
group versus 48% of the diluted formocresol group.
Severe inammation was noted in 35% of the ferric
sulfate group versus 29% of the diluted formocresol
group. Abscess and necrosis were noted in 3% of the
ferric sulfate group versus 13% of the diluted
formocresol group. They concluded that histologic
results were similar for both groups and did not com-
pare favorably with previously reported clinical nd-
ings of ferric sulfate potential superiority.
271
Cell-Inductive Agents
Mineral trioxide aggregate and calcium phosphate
cement have already been described with respect to
their potential cell-inductive properties in the context
of direct pulp-capping techniques. Their use in pulpo-
tomy techniques remains to be substantiated from con-
trol studies. Mineral trioxide aggregate was identied
as a potentially effective pulpotomy agent in a review of
this material with case examples by Abedi and Ingle.
272
Higashi and Okamoto reviewed the use of calcium
phosphate ceramics and hydroxyapatite as potential
pulpotomy agents. They studied the particle size effects
of hydroxyapatite and -tricalcium phosphate as vari-
ables in pulpotomy success as determined by hard tis-
sue formation. Osteodentin and tubular dentin forma-
tion occurred around large particles (300 mu) in con-
trast to small particles (40 mu), which demonstrated
pulp tissue inammation.
273
Yoshiba et al. provided
evidence of -tricalcium phosphate in combination
with calcium hydroxide being successful in bridge for-
mation with less local destruction of pulp tissue than
with calcium hydroxide alone.
274
Bone morphogenetic proteins have been proposed as
potential capping agents in direct pulp-capping and
pulpotomy techniques. Bone morphogenetic proteins 2
to 8 belong to TGF-, that are signaling proteins that reg-
ulate cell differentiation. Bone morphogenetic proteins 2
and 4 have been implicated in odontoblastic differentia-
tion. Nakashima demonstrated dentin bridging in dog
tooth coronal pulp amputation when the remaining tis-
sue was capped with BMP-2 and BMP-4, along with
recombinant human dentin matrix. After a 2-month
time interval, tubular dentin and osteodentin were found
histologically in response to both BMP types.
177
Fadhavi and Anderson compared freeze-dried bone,
calcium hydroxide, and ZOE in primate deciduous
tooth pulpotomies with respect to histologic inam-
mation and clinical/radiopathic pathology. After 6-
week and 6-month time periods, vital pulps with mod-
erate inammation were found in 83.3% of the freeze-
dried bone group. This was in contrast to the calcium
hydroxide group, which demonstrated moderate to
severe inammation in 50% of the cases and signs of
partial necrosis in 100%. Dentin bridge formation
occurred in 100% of the freeze-dried bone group ver-
sus 50% in the calcium hydroxide group. All of the
ZOE-treated teeth were necrotic at 6 months. They
concluded that freeze-dried bone was superior to calci-
um hydroxide within the parameters of their study and
might have potential as a pulpotomy agent if substan-
tiated by studies in humans.
178
Nonpharmacotherapeutic Pulpotomy Techniques:
Controlled Energy
Controlled energy in the form of electrosurgical and
laser heat application to the pulp stumps at the canal
orice site has been proposed as an alternative to the
more traditional pharmacotherapeutic techniques,
particularly those using formocresol. Ruemping et al.
identied electrosurgical pulpotomy advantages that
can be applied to the controlled energy category at
large and include (1) quick and efficient, (2) self-limit-
ing, (3) good hemostasis, (4) good visibility of the eld,
(5) no systemic effects, and (6) sterilization at the site
of application.
275
Electrosurgery. Ruemping et al. histologically
compared electrosurgery with formocresol in pulpoto-
my techniques for primate primary and young perma-
nent teeth. They mechanically amputated coronal
pulps and then either applied formocresol to the pulp
stump or performed momentary electrosurgery, fol-
lowed by ZOE cement placement.
275
After an 8-week
post-treatment period, the histologic appearance for
both groups was similar, with no evidence of pulp
necrosis or abscess formation. In the electrosurgery
group, secondary dentin was deposited along the later-
al canal walls, and the apical two-thirds of the pulp
revealed a slightly brotic to normal appearance.
275
Shaw et al. compared, after 6 months, the histologic
effects of electrosurgery with formocresol on the radic-
ular pulp. They found similar success rates of 80% for
the formocresol and 84% for the electrosurgical groups
according to their histologic criteria. They concluded
that neither technique was superior.
276
Conversely, Shulman et al. histologically compared
electrosurgery, formocresol, and electrosurgery plus
formocresol in primate pulpotomies.
277
They used
14
C-labeled formocresol and performed coronal ampu-
tation with electrosurgery subsequent to pulp chamber
roof removal. They found more periradicular and fur-
cal pathologic change after 65 days in the electro-
surgery group. They also noted that combining the two
techniques of electrosurgery and formocresol pro-
duced no better results. Both electrosurgical groups
were inferior to the formocresol group.
277
Sheller and
888 Endodontics
Morton histologically studied the effects of electrosur-
gical pulpotomies on the remaining radicular tissue in
11 primary canines at 6-day, 2-week, 8-week, and 13-
week post-treatment intervals. Varying degrees of
inammation, edema, and necrosis were seen at all
time periods, with the most favorable tissue appearance
occurring at the longer intervals. Those teeth judged to
be successful demonstrated reparative dentin forma-
tion along the lateral aspect of the radicular canal walls
but not across the amputation site. They concluded
that their results did not support the concept of elec-
trosurgery being less harmful to pulp tissue than con-
ventional pharmacotherapeutic techniques.
278
A form of electrosurgery, known as electrofulgura-
tion, has been suggested for pulpotomies in primary
teeth.
279
It involves establishing an electrical arc to the
targeted tissue without direct contact of the probe,
which ideally connes heat to the supercial tissue level.
Mack and Dean investigated the electrofulguration
pulpotomy technique in 164 primary molars.
279
After a
26-month post-treatment period, they found a 99.4%
clinical and radiographic success rate. They felt that this
compared favorably with a 93.9% formocresol pulpoto-
my success rate in a retrospective study by Hicks et al.
with a similar protocol.
196,279
Conversely, Fishman et al.
compared calcium hydroxide with ZOE when used as a
base over electrofulgurated pulp tissue. Although the
overall clinical success rate for the entire sample was 77
to 81%, the radiographic success was 57.3% for the elec-
trofulguration plus calcium hydroxide group and 54.6%
for the electrofulguration plus ZOE group.
280
Lasers. Application of laser irradiation in vital
pulp therapy has been proposed as another alternative
to pharmacotherapeutic techniques. Its advantages and
disadvantages are the same as for electrosurgery.
Adrian reported that irradiation of the buccal tooth
surface with the neodymium: yttrium-aluminum-gar-
net (Nd:YAG) laser produced less pulp damage than
the ruby laser with less histologic evidence of coagula-
tion and focal necrosis.
281
Shoji et al. histologically
studied the carbon-dioxide laser in the pulpotomy pro-
cedure. They noted that the least amount of pulp tissue
injury occurred with defocused irradiation with lower
power settings and shorter application. More tissue
destruction occurred in the defocused mode with high-
er irradiation power settings.
282
Kato et al. studied the
effects of the Nd:YAG laser on pulpotomized rat molars
at low (5 watts) and high (15 watts) power settings. At
2 weeks, histologic evidence showed osteodentin cover-
ing the amputated pulps with the low power setting
and brous dentin formation at the orice wall of the
root canal with the high power setting. Normal root
Pediatric Endodontics 889
development was observed in all specimens.
283
McGuire et al. compared the Nd:YAG laser with
formocresol in permanent tooth pulpotomies in dogs
at 6- and 12-week post-treatment periods. No signi-
cant differences in radiographic pathology were found
between the two groups. Histologically, the frequency
of pulpal inammation was higher for the laser group
(29%) at 12 weeks than for the formocresol group
(0%). No differences were found with respect to peri-
radicular inammation and root resorption.
284
Studies on controlled-energy pulpotomy techniques
are equivocal as to their effectiveness in reducing post-
treatment inammation when compared to conven-
tional pharmacotherapeutic techniques. Although clin-
ical reports of success exist, more controlled clinical
and histologic investigations are needed to address the
variables of power settings, application times, continu-
ous versus pulsed modes of application, and degree of
heat dissipation in the radicular pulp and surrounding
hard tissues.
NONVITAL PULP THERAPY IN PRIMARY
TEETH: PULPECTOMY
The treatment objectives in nonvital pulp therapy for
primary teeth are to (1) maintain the tooth free of
infection, (2) biomechanically cleanse and obturate the
root canals, (3) promote physiologic root resorption,
and (4) hold the space for the erupting permanent
tooth. The treatment of choice to achieve these objec-
tives is pulpectomy, which involves the removal of
necrotic pulp tissue followed by lling the root canals
with a resorbable cement. Indications for this proce-
dure include teeth with poor chance of vital pulp treat-
ment success, strategic importance with respect to
space maintenance, absence of severe root resorption,
absence of surrounding bone loss from infection, and
expectation of restorability.
Most negative attitudes toward primary teeth com-
plete pulpectomy have been based on the difficulty in
cleaning and shaping the bizarre and tortuous canal
anatomy of these teeth.
285,286
This was especially true
for primary molars with their resorbing and open
apices.
287,288
Removal of abscessed primary teeth has
been suggested because of their potential to create
developmental defects in the underlying permanent
successors.
289291
In spite of these objections, successful
root canal obturation of irreversibly inamed and non-
vital primary teeth can be successfully accomplished.
Modications of adult endodontic techniques, howev-
er, must be implemented because of the aforemen-
tioned anatomic differences between primary and per-
manent teeth.
Marsh and Largent indicated that the goal of the
pulpectomy procedure in primary teeth should be to
eliminate the bacteria and the contaminated pulp tis-
sue from the canal.
292
In primary teeth, more empha-
sis is placed on chemical means in conjunction with
limited mechanical dbridement to disinfect and
remove necrotic pulp remnants from the somewhat
inaccessible canals rather than conventional shaping
of the canals. Complete pulpectomy procedures have
been recommended for primary teeth even with evi-
dence of severe chronic inammation or necrosis in the
radicular pulp.
293295
Resorbable cements such as ZOE and iodoform-
containing pastes have been recommended as canal
obturants. Nonresorbable materials such as gutta-per-
cha and silver points are contraindicated as they will
not enhance the primary root physiologic resorptive
process (Figure 17-18). Rifkin identied criteria for an
ideal pulpectomy obturant that include it being (1)
resorbable, (2) antiseptic, (3) noninammatory and
nonirritating to the underlying permanent tooth germ,
(4) radiopaque, (5) easily inserted, and (6) easily
removed.
296
No currently available obturant meets all
of these criteria.
Owing to primary tooth exfoliation, the standard for
long-term pulpectomy success is shorter than for adult
endodontics. Primary tooth pulpectomies are success-
ful if the root is (1) rmly attached, (2) remains in
function without pain or infection until the permanent
successor is ready to erupt, (3) undergoes physiologic
resorption, and (4) is free from stulous tracts.
Radiographically, success is judged by the absence of
furcation or periradicular lesions and the re-establish-
ment of a normal periodontal ligament.
Historical Perspective
Sweet described a four- or ve-step technique using
formocresol for the treatment of pulpless teeth with
and without stulae.
180
A study of pediatric endodon-
tic procedures was reported by Rabinowitz in which
nonvital primary molars were treated with a 2- to 3-day
application of formocresol, followed by precipitation
of silver nitrate and a sealer of ZOE cement into the
canals.
297,298
Although he reported a high success rate,
his complicated procedure involved a range of 4 to 17
visits, with an average of 5.5 visits for teeth without
periradicular involvement and 7.7 visits for those with
periradicular involvement.
Hobson described pulpectomy techniques for
necrotic primary teeth in which the canals were not
dbrided. Beechwood creosote was used as a disinfec-
tant, usually for 2 weeks, followed by lling the pulp
chamber with a ZOE cement. Treatment proved equal-
ly successful for teeth with necrotic pulps or vital
infected pulps.
299
In treating primary molars, Lewis and Law used
conventional endodontics in canal preparation where
they instrumented, irrigated with sodium hypochlo-
rite, and dried the canals, which were then medicated
for 3 to 7 days with either eugenol, camphorated
parachlorophenol, or formocresol.
1
On the second
visit, the canals were mechanically prepared with les
and lled with one of various resorbable mixtures, such
as ZOE cement or ZOE mixed with iodoform crystals
(see Figure 17-18).
Judd and Kenny advocated a different complete
pulpectomy method for deciduous teeth.
300
For vital
pulp extirpation, two Hedstroem les, usually size 20,
were slid along opposite sides of the canal to entangle
pulp tissue. Ideal placement of the les just short of the
apex, with two or three rotations, will ensnare the pulp.
When withdrawn, the vital pulp will be removed in toto.
If the pulp has degenerated, then the canal should be
led with a single No. 20 to allow access for a red No. 1
890 Endodontics
Lentulo paste ller.
300
After water irrigation and air
drying, canals were obturated with a thin mix (viscosi-
ty similar to toothpaste) of a ne-grained, nonrein-
forced ZOE cement (ZOE 2200, Dentsply-Caulk;
Milford, Dela.) using a Lentulo spiral paste ller.
300
Gould reported a clinical study of primary teeth in
27 children, age 3
1
2 years to 8
1
2 years, using a
one-appointment technique.
301
In 35 frankly infect-
ed primary molars, a cotton pellet of camphorated
parachlorophenol was placed in the chamber for 5
minutes after the canals had been dbrided with les
over two-thirds of their length. Zinc oxideeugenol
cement was then pressed into the prepared canals. After
26 months of clinical and radiographic observation,
83% were judged to be therapeutically successful on the
basis of no lesions being detected.
In asymptomatic necrotic primary teeth, Frigoletto
suggested that canals be dbrided with a barbed
broach, irrigated with sodium hypochlorite, and dried.
Canals were then lled with root canal paste using a
specially designed pressure syringe.
75
In instances of
symptomatic teeth, Cresatin was mixed with the paste.
Figure 17-18 Root canal lling of a pulpless, maxillary primary lateral incisor. A, Carious exposure and pulp deatha candidate for
endodontic therapy. B, Six months following successful root canal lling with resorbable zinc oxideeugenol cement. Care must be taken not
to perforate the apex or overll and injure the developing permanent tooth bud. Reproduced with permission from Law DB, Lewis TM, Davis
JM. An atlas of pedodontics. Philadelphia: WB Saunders; 1969.
A B
Pediatric Endodontics 891
Starkey has described a one-appointment and
multiappointment method of treating cariously
involved primary pulp tissue.
91
The one-appointment
method is used in cases with vital pulp tissue, in which
inammation extends beyond the coronal pulp and no
radiographic evidence of periradicular involvement is
present. In these cases, Starkey recommended a partial
pulpectomy to remove the coronal aspects of the radic-
ular pulp, controlling hemorrhaging and lling the
canals and crown with a creamy mix of ZOE cement.
Starkeys multiappointment method was advocated
for cases with necrotic pulps and periradicular
involvement.
91
At the rst appointment, coronal pulp
debris is removed, but the canals are not instrumented.
A medicament such as formocresol or camphorated
monochlorophenol is placed in the pulp chamber and
sealed with IRM for 1 week. If the tooth and surround-
ing gingival tissues are asymptomatic and clinically
negative at the second visit, the canals are mechanical-
ly cleansed and dbrided and then lled with ZOE
cement (Figure 17-19). Modications of these proce-
dures have been described by Cullen,
302
Dugal and
Curgon,
303
Goerig and Camp,
304
Kopel,
305
Mathewson
and Primosch,
89
and Spedding.
306
It should be noted that some controversy exists with
respect to the relative effectiveness of the one-sitting and
two-sitting pulpectomy procedures. Coll et al. reported
an 80 to 86% success rate with the one-sitting tech-
nique.
307
Primosch et al. noted that 60% of US under-
graduate dental programs teach the one-sitting technique
versus 26% teaching the two-sitting technique.
69
Extension of formocresol use to the pulpectomy
technique was a logical sequence. Vander Wall et al. have
shown formocresol to be more effective than either
camphorated parachlorophenol or Cresatin as a root
canal medicament for inhibiting bacterial growth.
308
Several studies have evaluated the clinical and radi-
ographic ndings of the pulpectomy procedure for
nonvital primary molars and primary anteriors using
formocresol. Coll et al. evaluated a one-appointment
formocresol pulpectomy technique for nonvital pri-
mary molars. After a mean observation period of 70
months, 86.1% were judged successful.
307
They also
found that successful pulpectomized primary molars
were not over-retained and the successor premolars had
a very low incidence of hypoplastic defects.
307
Barr et al., in a radiographic retrospective evaluation
of primary molar pulpectomies performed in a private
practice with a mean observation period of 40.2
months, found an overall success rate of 85.5%.
309
Noteworthy ndings included 88% complete ZOE
paste resorption and a 25.8% reduction of preoperative
Figure 17-19 Three-year successful root canal lling of
mandibular second primary molar. (Courtesy of Dr. Paul E.
Starkey.) The canals have been thoroughly led and irrigat-
ed at the rst appointment and medicated with formocresol
or camphorated parachlorophenol. At the second appoint-
ment, the canals were lled with resorbable zinc
oxideeugenol cement. Reproduced with permission from
Law DB, Lewis TM, Davis JM. An atlas of pedodontics.
Philadelphia: WB Saunders; 1969.
radiolucencies. These clinicians suggested that posteri-
or primary molar pulpectomies have a relatively high
success rate in private practice.
Coll et al. and Flaitz et al. also evaluated the results of
pulpectomy treatment in primary anterior teeth.
310,311
Using clinical and radiographic evaluations, Coll and
colleagues completed 27 pulpectomies in primary inci-
sors and found that their 78% success rate did not differ
statistically from comparable primary molar rates after a
mean of 45 months.
310
Seventy-three percent were con-
sidered to have exfoliated normally. These investigators
concluded, however, that documented success rates for
indirect pulp capping and pulpotomies in primary ante-
rior teeth were higher than for pulpectomies.
Flaitz et al.s contrasting study compared 57 pulpo-
tomies versus 87 pulpectomies in primary anterior
teeth followed for a mean of 37 months.
311
Based on
the nal radiographs in the study, treatment was suc-
cessful in 68.5% of the pulpotomized group of anteri-
or teeth versus 84% of the pulpectomized group. They
concluded overall that pulpectomy was a better treat-
ment option for primary incisors even though they
may have shown more radiographic pathosis at the
time of the diagnosis.
Yacobi and Kenny have twice monitored their success
rates in vital pulpectomy and immediate ZOE (ZOE
2200, L. D. Caulk Co.; Milford, Dela.) lling. At 6 months,
their success rate was comparable to the formocresol
results of 89% for anterior teeth and 92% for posterior
teeth.
312
At 2 years, reporting on 81 patients and 253
teeth, Payne et al., using ZOE, reported a mean success
rate of 83% for anterior teeth and 90% for posterior
teeth. They conjectured that the discrepancy in rates
between anterior and posterior teeth was related to the
nal restorationsmicroleakage from composite resin
in the anterior regions and stainless crowns in the poste-
rior.
313
They believed this to be a most acceptable alter-
native method for saving primary teeth while avoiding
the compromising effects of the aldehydes.
Alternative Pulpectomy Canal Obturants
Zinc oxideeugenol cement has been the most fre-
quently used obturant in the pulpectomy technique.
Primosch et al. noted that 90% of US pediatric den-
tistry undergraduate programs teach ZOE as the
pulpectomy obturant of choice.
69
Although considered
to be resorbable, Coll et al., in a 6-year follow-up of 41
pulpectomized primary molars, found that ZOE parti-
cle retention in the gingival sulcus occurred in 8 of 17
patients followed to the time of premolar eruption.
307
Their technique included a 5-minute formocresol-
blotted paper point treatment of the canals prior to
892 Endodontics
obturation. As previously mentioned, there has been
concern about the use of formocresol in any form in
pediatric endodontic therapy. Alternative pulpectomy
agents have been proposed to improve on the biocom-
patibility limitations of ZOE and formocresol.
Hendry et al. compared calcium hydroxide with
ZOE as a pulpectomy obturant in primary teeth of
dogs. At 4 weeks post-treatment, canals treated with
calcium hydroxide exhibited less inammation, less
pathologic root resorption, and more hard tissue appo-
sition than ZOE and control-treated teeth.
314
Barker and Lockett identied the potential benets
of Kri paste, an iodoform compound, also containing
parachlorophenol, camphor, and menthol. The advan-
tages of this material include bactericidal properties
and excellent resorbability. Histologically, they found
that this material easily resorbed even when extruded
beyond the apex of the treated teeth. An ingress of con-
nective tissue was seen in the apical portions of the
treated canals.
315
Bactericidal iodoform pastes have
been reintroduced as a root canal lling.
245,316,317
Garcia-Godoy obtained a 95.6% success clinically and
radiographically with Kri paste during a 24-month
period for 43 teeth.
318
It was noted that this paste
would resorb within 2 weeks if found in the periradic-
ular or furcation areas.
319
Rifkin reported an 89% clin-
ical and radiographic success rate after 1 year with Kri
paste pulpectomies in primary teeth.
296
Holan and
Fuks clinically and radiographically compared Kri
paste with ZOE in human primary molars after 48
months postoperatively. They found overall success
rates of 84% with the Kri paste group versus 65% with
the ZOE group. Kri paste was almost twice as success-
ful in primary rst molars as ZOE. However, no signif-
icant differences between these two agents occurred in
primary second molars. Overlls with Kri paste result-
ed in 79% success versus 41% success with ZOE. They
concluded that iodoform-containing paste had a
potential advantage over ZOE in the pulpectomy pro-
cedure for primary teeth.
319
Treatment Considerations
The preceding review demonstrates the varied tech-
niques and successes for mastering pulp therapy for
nonvital and irreversibly inamed primary teeth.
Before outlining treatment methods, special considera-
tions, indications, and contraindications must be
addressed by the clinician.
General Considerations.
1. The patient should be healthy and cooperative. If
any systemic disorders are present that would com-
Pediatric Endodontics 893
promise a childs responses, the childs physician or
medical team should be consulted.
2. Informed consent, with a clear explanation of the
procedure to the parents, must be obtained.
Dental Considerations.
1. The tooth must be restorable after the root canal
treatment.
2. Chronologic and dental age must be evaluated to
rule out teeth with eminent exfoliation.
3. Psychological or cosmetic factors (anterior primary
teeth) must be considered, which are often more
important to the parent than to the child.
4. The number of teeth to be treated and strategic
importance to the developing occlusion must be
evaluated.
5. Primary molar root anatomy, along with the prox-
imity of the underlying succedaneous tooth, must be
evaluated.
Indications for a Pulpectomy Procedure.
1. Primary teeth with pulpal inammation extending
beyond the coronal pulp but with roots and alveo-
lar bone free of pathologic resorption
2. Primary teeth with necrotic pulps, minimum root
resorption, and minimum bony destruction in the
bifurcation area
3. Pulpless primary teeth with sinus tracts
4. Pulpless primary teeth without permanent successors
5. Pulpless primary second molars before the erup-
tion of the permanent rst molar
6. Pulpless primary teeth in hemophiliacs
7. Pulpless primary anterior teeth when speech,
crowded arches, or esthetics are a factor
8. Pulpless primary teeth next to the line of a palatal
cleft
9. Pulpless primary molars supporting orthodontic
appliances
10. Pulpless primary molars when arch length is de-
cient
11. Pulpless primary teeth when space maintainers or
continued supervision are not feasible (handi-
capped or isolated children
)
Contraindications.
1. Teeth with nonrestorable crowns
2. Periradicular involvement extending to the perma-
nent tooth bud
3. Pathologic resorption of at least one-third of the
root with a stulous sinus tract
4. Excessive internal resorption
5. Extensive pulp oor opening into the bifurcation
6. Young patients with systemic illness such as congen-
ital or rheumatic heart disease, hepatitis, or
leukemia and children on long-term corticosteroid
therapy or those who are immunocompromised
7. Primary teeth with underlying dentigerous or follic-
ular cysts
Clinical Procedures: Partial Pulpectomy
Partial pulpectomy can be considered an extension of
the pulpotomy procedure in that the coronal portion of
the radicular pulp is amputated, leaving vital tissue in
the canal that is assumed to be healthy. Although dis-
cussed in the context of nonvital pulp therapy, techni-
cally, it is a vital pulp therapy technique. The decision
to implement the partial pulpectomy is made after
removing the coronal pulp from the chamber and
encountering difficulty with hemorrhage control from
the radicular orice.
Hemorrhage control is achieved with endodontic
broaches used to remove one-third to one half of the
coronal portion of the radicular pulp tissue from the
canals. The canals and chamber are irrigated with
hydrogen peroxide followed by sodium hypochlorite
and then dried with cotton pellets. If hemorrhage is
still impossible to control, all remaining radicular pulp
tissue is to be removed, and the complete pulpectomy
procedure must be implemented.
After successful hemorrhage control from the
amputated radicular pulp, a formocresol-dampened
cotton pellet, squeezed dry, is placed in the pulp cham-
ber for 1 to 5 minutes. The pellet is removed, and a
nonreinforced fast-setting ZOE cement is packed with
pressure into the chamber and canals. A radiograph is
then taken, and if the canals appear to be adequately
lled, a stainless steel crown is placed as a permanent
restoration (Figure 17-20).
Clinic Procedures: Complete Pulpectomy
The child with a necrotic primary tooth presents a con-
siderable challenge for the clinician. In some instances,
the tooth may be totally asymptomatic from a clinical
standpoint. In other instances, the tooth may be acute-
ly or chronically abscessed, mobile and painful, with
Owing to the isolation of the children involved in its Bureau of
Indian Health Affairs, the US Public Health Service has recom-
mended root canal lling of primary teeth, whenever feasible,
rather than space maintainers that require lengthy supervision.
320
swollen periodontal tissues. In the latter case, the child
may be apprehensive and irritable, making relief of
pain and swelling the highest priority. In cases of
nondraining alveolar abscesses and cellulitis from
odontogenic origin, antibiotic therapy using rst- or
second-generation penicillins should be immediately
prescribed for a period of 4 to 7 days. Canal instru-
mentation can then be implemented.
The complete pulpectomy procedure involves the
following considerations. Under local anesthesia, the
pulp chamber is carefully opened with a high-speed
bur to relieve any pressure from the infected pulp. A
low-speed round bur or a spoon excavator may be used
to clean out the pulp chamber, which is then irrigated
with sodium hypochlorite. In cases of acute inamma-
tion, a camphorated monochlorophenol-dampened
cotton pellet is placed in the coronal chamber as an
interim medicament to chemically sterilize the pulp
canals. In cases of chronic abscess formation, a
formocresol-dampened cotton pellet is generally used
as the interim medicament. The chambers are then
sealed with a fast-setting ZOE cement, and the tooth
may need to be equilibrated to avoid hyperocclusion.
At the end of 1 week, if all acute symptoms includ-
ing pain and soft tissue swelling have resolved, nal
canal preparationcareful enlargement and dbride-
mentis completed with Hedstroem les. Canal irri-
gation is accomplished with hydrogen peroxide and
sodium hypochlorite. Tooth length should be carefully
894 Endodontics
determined, and instrumentation should not extend
beyond the apex. Fine les, in ultrasonic or sonic
endodontic handpieces, with copious irrigation can be
considered in this protocol.
The ribbon-shaped and tortuous root canals of pri-
mary teeth present a time-consuming problem in
obtaining adequate obturation. A pressure syringe was
developed by Greenberg for lling primary canals.
321
This technique has been described in detail by
Spedding
306
and by Krakow et al..
322
The material of
choice for lling the root canals of pulpectomized pri-
mary teeth is pure ZOE, rst mixed as a slurry and car-
ried into the canals using either paper points, a syringe,
a Jiffy tube, or a lentulo spiral root canal ller. Aylard
and Johnson showed that the lentulo was the best over-
all ZOE root canallling instrument for curved canals
and the pressure syringe technique was best for straight
canals.
323
The slurry may be further compressed into
the canals by packing the chamber with a stiffer mix of
ZOE. After the canals are estimated to be lled to the
chamber oor, the chamber itself is lled with a suit-
able cement such as a reinforced ZOE or a glass
ionomer. As previously mentioned, the tooth is pre-
pared for the placement of a stainless steel crown after
evaluation of the canal lling by a radiograph.
90
Mack and Halterman described the rationale and
technique for an innovative approach to pulpectomy for
primary anterior teeth by using a labial entry to the
canal instead of the traditional lingual opening. This
allows greater ease of instrumentation and provides
incorporation of the access chamber in the esthetic labi-
al veneer preparation. Bonded composite resin is used to
complete the nal esthetic restoration.
324
Clinical Variation: Pulpotomy for Nonvital
Primary Teeth
Less demanding techniques than the pulpectomy have
been reported for treating irreversibly inamed pri-
mary teeth, usually involving the formocresol pulpoto-
my technique. Ripa recommended that, owing to the
anatomy of primary tooth canals, it would be much
easier to perform complete dbridement in nonvital
primary molars using a pulpotomy technique, with
appropriate medicaments.
325
Although there is evi-
dence to support such a concept, the consensus is that
the pulpotomy technique should be conned to teeth
meeting the selection criteria for vital pulp therapy.
326
Velling
327
and Droter
328
reported high degrees of suc-
cess in nonvital primary molars with a coronal pulpoto-
my only, using formaldehyde-type medicaments in either
one- or two-appointment visits. The nal dressing in the
coronal pulp chamber was usually a modied ZOE
Figure 17-20 Root canal obturation and crown restoration for a
pulpless primary molar. At the rst appointment, following
mechanical and chemical canal dbridement, medicament is sealed
in place for 1 week. The canal is obturated at the second appoint-
ment with resorbable zinc oxideeugenol cement. A, Zinc
oxideeugenol cement root canal lling. B, Oxyphosphate of zinc
cement. C, Stainless steel crown.
Pediatric Endodontics 895
cement. Full described complete success in 20 children
with chronically abscessed primary molars and draining
stulae in a two-appointment formocresol technique.
329
All of the draining stulae were reported to be resolved.
As an extension of this technique, Meyer and Sayegh used
a combination treatment of formocresol in the pulp
chamber and curettage of the bifurcation to achieve an
87% clinical success at 5 years postoperatively.
330
In a survey of members of the American Academy of
Pediatric Dentistry, success rates of 72% were reported
in nonvital primary molars that had been treated by
cleaning only the coronal chamber and placing
formocresol versus instrumenting the canals. Both
treatments were concluded by lling the respectively
cleansed areas with a resorbable medicated cement and
placing a stainless steel crown.
331
Myers et al., in a recent histologic study of failed
pulpotomies in primary molars, stated that the devel-
opment of a furcation lesion has the potential for cys-
tic transformation and the tooth should be extract-
ed.
332
This conclusion also implies that pulpectomy
treatment for nonvital primary molars with furcation
lesions is contraindicated.
Pulpectomy Outcomes
Negative sequelae from endodontically treated primary
teeth in the form of accelerated resorption and exfolia-
tion have been a major concern of many clinicians.
Starkey felt that delayed eruption of the permanent suc-
cessors sometimes followed pulpotomy and pulpecto-
my treatment of primary molars, with some possible
deection in the eruption path.
333
This sequela was not
seen in the studies by Barr et al.
309
and Coll et al..
310
Ankylosis of the primary tooth with a root canal lling
has also been noted. Erausquin and Devoto have shown
that formaldehyde-containing cements frequently
caused partial ankylosis at different levels of the peri-
odontal ligament.
334
Coll and Sadrian, in a retrospective
study of pulpectomy outcomes, noted two parameters
that were the highest predictors of success.
Pretreatment pathologic root resorption, when evi-
dent, resulted in a 44.4% prevalence of enamel defects
in underlying permanent teeth after their eruption. In
the absence of pretreatment pathologic root resorption,
the pulpectomy success rate was 91.7%. The quality of
canal ll relative to the apex was another outcome
determinant, with 86.5% success rates occurring for
canals lled short of the apex, 88.9% success for canals
lled to the apex, and 57.7% success for canals lled
beyond the apex.
335
SUMMARY
The rationale for pediatric pulp therapy has developed
out of extensive clinical studies and improved histolog-
ic techniques. Ongoing research will result in modica-
tions that will enhance treatment outcomes.
A successful pediatric endodontic outcome should
be based on (1) re-establishment of healthy periodon-
tal tissues; (2) freedom from pathologic root resorp-
tion; (3) maintenance of the primary tooth in an infec-
tion-free state to hold space for the eruption of its per-
manent successor; (4) in the case of young permanent
teeth, maintenance of the maximum amount of nonin-
amed portions of pulp tissue to enhance apexogenesis
and root dentin formation. With adherence to sound
principles in case selection and techniques, pediatric
pulp therapy is a major health benet to the child. The
treatment modalities and medicaments that have been
Table 17-2 Pulp Treatment Summary: Current Recommendations
Indirect pulp cap Permanent teeth, primary teethcalcium hydroxide glass ionomer cement, resin
bonding agent
Direct pulp cap Permanent teethcalcium hydroxide, mineral trioxide aggregate, resin bonding agent (?)
Direct pulp cap Primary teeth (mechanical exposures only)calcium hydroxide
Pulpotomy Primary teethdiluted and full-strength formocresol, glutaraldehyde, ferric sulfate (?),
controlled energy techniques (?)
Pulpotomy Permanent teeth (apexogenesis)calcium hydroxide, formocresol (?), glutaraldehyde(?)
Partial pulpectomy Primary teethzinc oxideeugenol, zinc oxideeugenol + formocresol
Complete pulpectomy Permanent teeth (apexication)calcium hydroxide
Complete pulpectomy Primary teethzinc oxideeugenol, zinc oxideeugenol + formocresol, iodoform-
containing pastes (?), calcium hydroxide (?)
discussed are summarized in Table 17-2, highlighting
the most substantiated and qualifying those that need
further conrmation by additional research. The clini-
cian must realize that these recommendations are not
absolute and will continue to be modied.
REFERENCES
1. Lewis TM, Law DC. Pulpal treatment of primary teeth. In:
Finn SB, editor. Clinical pedodontics. 4th ed. Philadelphia:
WB Saunders; 1973.
2. Finn SB. Morphology of the primary teeth. In: Finn SB, editor.
Clinical pedodontics. 4th ed. Philadelphia: WB Saunders;
1973.
3. McDonald RE, Avery DR. Treatment of deep caries, vital pulp
exposure and pulpless teeth. In: McDonald RE, Avery DR,
editors. Dentistry for the child and adolescent. 6th ed. St.
Louis: CV Mosby; 1995. p. 42854.
4. Moss SJ, Addleston H. Histologic study of the pulpal oor of
deciduous molars. J Am Dent Assoc 1965;70:372.
5. Rengelstein D, Slow WK. The prevalence of furcation forami-
na in primary molars. Pediatr Dent 1989;11:198.
6. Wrbas KT, Kielbassa AM, Hellwig E. Microscopic studies of
accessory canals in primary molar furcations. J Dent Child
1997;64:118.
7. Greely CB. Pulp therapy for the primary and young perma-
nent dentition. In: Forrester DJ, Wagner ML, Fleming J,
editors. Pediatric dental medicine. Philadelphia: Lea &
Febiger; 1981. p. 45660.
8. Seltzer S, Bender IB. The dental pulpbiologic considerations
in dental procedures. 3rd ed. Philadelphia: JB Lippincott;
1984.
9. Cox CF, Suzuki S. Re-evaluating pulp protection: calcium
hydroxide liners vs. cohesive hybridization. J Am Dent
Assoc 1994;125:823.
10. Fox AG, Heeley JD. Histologic study of human primary teeth.
Arch Oral Biol 1980;25:103.
11. Massler M. Preventive endodontics: vital pulp therapy. Dent
Clin North Am 1967; p.670.
12. Bernick S. Innervation of the teeth and periodontium. Dent
Clin North Am 1959; p.503.
13. Rapp R, et al.. The distribution of nerves in human primary
teeth. Anat Rec 1967;159:89.
14. Benzer G, Bevelander S. Morphology and incidence of second-
ary dentin in human teeth. J Am Dent Assoc 1943;30:1075.
15. Ireland RI. Secondary dentin formation in deciduous teeth. J
Am Dent Assoc 1941;28:1626.
16. Corbett MD. The incidence of secondary dentin in carious
teeth. Br Dent J 1963;114:142.
17. Sayegh FS. Qualitative and quantitative evaluation of new
dentin in pulp capped teeth. J Dent Child 1968;35:7.
18. McDonald RE. Diagnostic aids and vital pulp therapy for
deciduous teeth. J Am Dent Assoc 1956;53:14.
19. Anderson AW, Sharav Y, Massler M. Reparative dentin forma-
tion and pulp morphology. Oral Surg Oral Patts Oral Med
1948;26:837.
20. Frankl SH. Pulp therapy in pedodontics. Oral Surg
1972;34:192.
21. Eidelman E, et al. Pulp pathology in deciduous teeth: clinical
and histological correlations. Isr J Med Sci 1968;4:1244.
22. Prophet AS, Miller J. The effect of caries on the deciduous
pulp. Br Dent J 1955;99:105.
896 Endodontics
23. Rayner JA, Southam II. Pulp changes in deciduous teeth asso-
ciated with deep carious dentin. J Dent 1970;7:39.
24. Taylor B, et al. Response of the pulp and dentine to dental
caries in primary molars. J Int Assoc Dent Child 1971;2:3.
25. Damele J. Clinical evaluation of indirect pulp capping: a
progress report. J Dent Res 1961;40:756.
26. Belanger G K. Pulp therapy for young permanent teeth. In:
Pinkham JR, Cassamassimo PS, Fields HW, et al., editors.
Pediatric dentistryinfancy through adolescence. 2nd ed.
Philadelphia: WB Saunders; 1988. p. 48391.
27. Troutman K, et al. Vital pulp therapy: part 1. In: Stewart RE, et
al., editors. Pediatric dentistry. St. Louis: CV Mosby; 1982.
p. 916.
28. DiMaggio JJ, et al. Histological evaluation of direct and indi-
rect pulp capping [abstract]. J Dent Res 1963.
29. Trowbridge H, Berger J. The clinical management of deep car-
ious lesions. Calif Dent J 1971;47:26.
30. Ishibaski M. A comparison between results of clinical and
histo-pathological diagnosis of disease of deciduous tooth
pulp. Dent Abstr 1958;3:547.
31. Reynolds RL. The determination of pulp vitality by means of
thermal and electrical stimuli. Oral Surg 1966;22:231.
32. Tomes J. A system of dental surgery. London: I. Churchill;
1859.
34. Miller WD. What antiseptics should be used for sterilizing cav-
ities before lling. Dent Cosmos 1891;33:337.
35. Black GV. A work on operative dentistry. Vol 2. Chicago:
Medico-Dental Publishing; 1908.
36. Dorfman A, Stephan RM, Muntz JA. In vitro studies of carious
dentin. II. Extent of infection in carious lesions. J Am Dent
Assoc 1943;30:1901.
37. MacGregor AB, et al. Experimental studies of dental caries. I.
The relationship of bacterial invasions to softening of the
dentine. Br Dent J 1956;101:203.
38. Fusayama T, et al. Relationship between hardness, discol-
oration and microbial invasion in carious dentin. J Dent
Res 1966;45:1033.
39. Fusayama T. Two layers of carious dentin: diagnosis and treat-
ment. Oper Dent 1979;4:63.
40. Whitehead FI, et al. The relationship of bacterial invasion of
softening of the dentin in permanent and deciduous teeth.
Br Dent J 1960;108:261.
41. Shovelton DS. A study of deep carious dentin. Int Dent J
1968;18:392.
42. Seltzer S, Bender IB. The dental pulp. Philadelphia: JB
Lippincott; 1965. p. 18498.
43. Reeves R, Stanley HR. The relationship of bacterial penetra-
tion and pulpal pathosis in carious teeth. Oral Surg
1966;22:59.
44. Shovelton DS. Studies of dentin and pulp in deep caries. Int
Dent J 1970;20:283.
45. Massler M. Op Cit. Ref no. 11.
46. Massler M, Pawlak J. The affected and infected pulp. Oral Surg
1977;43:929.
47. Canby CP, Bernier JL. Bacteriologic studies of carious dentin.
J Am Dent Assoc 1936;23:2083.
48. Kuwabara RK, Massler M. Pulpal reactions to active and
arrested carious lesions. J Dent Child 1966;33:190.
49. Bradford EW. The dentin, a barrier to caries. Br Dent J
1960;109:387.
Pediatric Endodontics 897
50. Young MA, Massler M. Some physical and chemical character-
istics of carious dentin. Br Dent J 1963;115:406.
51. Leung RL, et al. Effect of Dycal on bacteria in deep carious
lesions. J Am Dent Assoc 1980;10:193.
52. Fairbourn DR, et al. Effect of improved Dycal and IRM on bac-
teria in deep carious lesions. J Am Dent Assoc 1980;100:547.
53. Law DB, Lewis TM. The effects of calcium hydroxide on deep
carious lesions. Colorado Dent J 1964;42:27.
54. Held-Wydler E. Natural (indirect) pulp capping. J Dent Child
1964;31:107.
55. Kerkhove BC, et al. A clinical and television densitometric
evaluation of the indirect pulp capping technique. J Dent
Child 1967;34:192.
56. Ehrenreich DV. A comparison of the effects of zinc
oxide-eugenol and calcium hydroxide in carious dentin in
human primary molars. J Dent Child 1968;35:451.
57. Stanley HR. Pulpal response to dental techniques and materi-
als. Dent Clin North Am 1971;15:115.
58. Torstenson B, et al. Pulp reaction to IRM [abstract]. J Dent Res
1982;61:573.
59. Nordstrom DO, et al. Use of stannous uoride for indirect
pulp capping. J Am Dent Assoc 1974;88:997.
60. King J, et al. Indirect pulp capping: a bacteriologic study of
deep carious dentin in human teeth. Oral Surg 1965;20:663.
61. Aponte AJ, Hartsook JT, Crowley MC. Indirect pulp capping
veried. J Dent Child 1966;33:164.
62. Parikh SR, Massler M, Bahn A. Microorganisms in active and
arrested carious lesions of dentin. N Y State Dent J
1963;29:347.
63. Eidelman E, et al. Remineralization of carious dentin treated
with calcium hydroxide. J Dent Child 1965;32:218.
64. Mjr IA, et al. The effect of calcium hydroxide and amalgam
on noncarious vital dentin. Arch Oral Biol 1961;3:283.
65. Sawusch RH. Direct and indirect pulp capping with two new
products. J Am Dent Assoc 1982;104:459.
66. Nirschl R, Avery D. Evaluation of a new pulp capping agent in
indirect pulp therapy. J Dent Child 1983;50:25.
67. Coll JA, et al. An evaluation of pulp therapy in primary inci-
sors. Pediatr Dent 1988;10:178.
68. Schroder A. Indirect capping and the treatment of deep cari-
ous lesions. Int Dent J 1968;18:381.
69. Primosch RE, Glomb TA, Jerrell RG. Primary tooth pulp ther-
apy as taught in predoctoral pediatric dental programs in
the United States. Pediatr Dent 1997;19:11822.
70. Lado EA, Stanley HR. An in vitro study of bacterial inhibition
by VLC calcium hydroxide pulp cap compounds. Pediatr
Dent 1987;9:292.
71. Jordan RE, Suzuki M. Conservative treatment of deep carious
lesions. Can Dent Assoc J 1971;37:337.
72. Fuks AB. Pulp therapy for the primary dentition. In: Pinkham
JR, Cassamassimo PS, Fields HW, et al., editors. Pediatric
dentistryinfancy through adolescence. 2nd ed. WB
Saunders; 1988. p. 32638.
73. Langeland K. Capping exposed pulpal tissue. Dent Clin North
Am 1974;2:1.
74. Stanley HR. Criteria for standardizing and increasing credibil-
ity of direct pulp capping studies. Am. J Dent 1998;11:S17.
75. Frigoletto RT. Pulp therapy in pedodontics. J Am Dent Assoc
1973;86:1344.
76. Tronstad L, Mjr I.A. Capping of the inamed pulp. Oral Surg
1972;34:477.
77. Cox CF, Bergenholtz G. Healing sequence in capping inamed
dental pulps of rhesus monkeys. Int Endod J 1986;19:113.
78. Heide S, Kerekes K. Delayed direct pulp capping in permanent
incisors of monkeys. Int Endod J 1987;20:65.
79. Cotton WR. Bacterial contamination as a factor in healing of
pulp exposures. Oral Surg 1974;38:441.
80. Glass RL, Zander HA. Pulp healing. J Dent Res 1949;28:97.
81. Lim KC, Kirk EE. Direct pulp capping: a review. Endod Dent
Traumatol 1987;3:213.
82. Stanley HR, Lundy T. Dycal therapy for pulp exposures. Oral
Surg 1972;34:818.
83. Weiss MD, Bjorvatn K. Pulp capping in deciduous and newly
erupted permanent teeth of monkeys. Oral Surg 1970;29:769.
84. Kakehashi S, Stanley HR, Fitzgerald R J. The effects of surgical
exposures of the dental pulp in germ free and convention-
al laboratory rats. Oral Surg 1965;20:340.
85. Langeland K, et al. Human pulp changes of iatrogenic origin.
Oral Surg 1971;32:943.
86. Cox CF, Subay RK, Ostro E, et al. Tunnel defects in dentin
bridges: their formation following direct pulp capping.
Oper Dent 1996;21:4.
87. Baume L, Holz J. Long-term clinical assessment of direct pulp
capping. Int Dent J 1981;31:251.
88. Kennedy DB, Kapala JT. The dental pulp: biologic considera-
tions of protection and treatment. In: Braham RL, Morris
ME, editors. Textbook of pediatric dentistry. 2nd ed.
Baltimore: Williams and Wilkins; 1985. p. 492522.
89. Mathewson RJ, Primosch R. Pulp treatment. In: Fundamentals
of pediatric dentistry. 3rd ed. Chicago: Quintessence; 1995.
p. 25784.
90. Camp J. Pulp therapy for primary and young permanent teeth.
Dent Clin North Am 1984;28:651.
91. Starkey PE. Treatment of pulpally involved primary molars. In:
McDonald RE, et al., editors. Current therapy in dentistry.
Vol VII. St. Louis: CV Mosby; 1980.
92. Weine DM. The effect of calcium hydroxide in direct pulp cap-
ping in primary teeth [thesis]. Ann Arbor [MA]: Univ. of
Michigan School of Dentistry; 1963.
93. Jeppersen K. Direct pulp capping on primary teetha
long-term investigation. Int Assoc Dent Child 1971;12:10.
94. Jerrell RG, Courts FK, Stanley HR. A comparison of two calci-
um hydroxide agents in direct pulp capping of primary
teeth. J Dent Child 1984;51:34.
95. Kalins V, Frisbee HE. The effect of dentine fragments on the
healing of the exposed pulp. Arch Oral Biol 1960;2:96.
96. Schrder U, et al. A one-year follow-up of partial pulpotomy
and calcium hydroxide capping in primary molars. Endod
Dent Traumatol 1987;3:304.
97. Arnold DS. The use of formocresol as a pulp capping agent in
human primary teeth [thesis]. Lincoln, NE: Univ. of
Nebraska School of Dentistry; 1970.
98. Cvek M. A clinical report on partial pulpotomy and capping
with calcium hydroxide in permanent incisors with com-
plicated crown fracture. J Endod 1978;4:232.
99. Zilberman U, et al. Partial pulpotomy in carious permanent
molars. Am J Dent 1989;2:147.
100. Mejare I, Cvek M. Partial pulpotomy in young permanent
teeth with deep carious lesions. Endod Dent Traumatol
1993;9:238.
101. Fuks AB, Chosack A, Klein H, Eidelman E. Partial pulpotomy as
a treatment alternative for exposed pulps in crown-fractured
permanent incisors. Endod Dent Traumatol 1987;3:100.
898 Endodontics
125. Hembree JH, Andrews IT. Zinc oxide as a pulp capping agent.
Miss Dent J 1974;30:10.
126. Watts A. Zinc oxide as a pulp capping agent [abstract]. J Dent
Res 1977;56:D104.
127. Holland R, et al. The inuence of the sealing material in the heal-
ing process of inamed pulps capped with calcium hydroxide
or zinc oxide-eugenol cement. Acta Odontol Pediatr 1981;2:5.
128. Sveen OB. Pulp capping of primary teeth with zinc
oxide-eugenol. Odontol Tidskr 1969;77:427.
129. Brosch JW. Capping pulps with a compound of calcium phos-
phate, neomycin and hydrocortisone. J Dent Child
1966;33:42.
130. Soldali GD. Pulp capping with antibiotics. Fla Dent J
1975;46:18.
131. Bhaskar SH, et al. Tissue response to cortisone-containing and
cortisone-free calcium hydroxide. J Dent Child 1969;36:1.
132. Ulmansky M, Sela J. Response of pulpotomy wounds in nor-
mal human teeth to successively applied Ledermix and
Calxyl. Arch Oral Biol 1971;16:1393.
133. Haskell EW, et al. Direct pulp capping treatment: a long-term
follow-up. J Am Dent Assoc 1978;97:607.
134. McWalter G, et al. Long-term study of pulp capping in mon-
keys with three agents. J Am Dent Assoc 1976;933:105.
135. Watts A, Paterson RC. The response of the mechanically
exposed pulp to prednisolone and triamcinolone ace-
tonide. Int Endod J 1988;21:9.
136. Gardner DE, Mitchell DF, McDonald RE. Treatment of pulps
of monkeys with vancomycin and calcium hydroxide. JDR
1971;50:1273.
137. Negm M, et al. Clinical and histologic study of human pulpal
response to new cements containing calcium hydroxide.
Oral Surg 1980;50:462.
138. Bhaskar SH, et al. Human pulp capping with isobutylcyano-
acrylate. J Dent Res 1972;51:50.
139. Heys DR, Cox CF, Avery JK. Histological considerations of
direct pulp capping agents. J Dent Res 1981;68:1371.
140. Subay RK, Asci S. Human pulpal response to hydroxyapatite
and a calcium hydroxide material as direct capping agents.
Oral Surg 1993;76:485.
141. Dick HM, Carmichael DJ. Reconstituted antigen poor collagen
preparations as potential pulp capping agents. JOE
1980;6:641.
142. Fuks AB, et al. Enriched collagen solution as a pulp dressing in
pulpotomized teeth in monkeys. Pediatr Dent 1984;6:243.
143. Ibrahim SM, Mitchell DF, Healy HG. A histopathologic study
of the effects of formocresol in pulp capping of permanent
teeth. Egypt Dent J 1970;16:219.
144. Garcia-Godoy F. Direct pulp capping and partial pulpotomy
with diluted formocresol in primary molars. Acta Odontol
Pediatr 1984;5:57.
145. Bergenholtz G, et al. Bacterial leakage around dental restora-
tions: its effect on the dental pulp. J Oral Pathol 1982;11:439.
146. Cox CF. Evaluation and treatment of bacterial microleakage.
Am J Dent 1994;7:2935.
147. Snuggs HM, Cox CF, Powell CS, White KC. Pulpal healing and
dentinal bridge formation in an acidic environment.
Quintessence Int 1993;24:501.
148. Barnes IE, Kidd EAM. Disappearing Dycal. Br Dent J
1980;111:147.
149. Cox CF. Effects of adhesive resins and various dental cements
on the pulp. Oper Dent 1992;55:165.
102. Watts A, Paterson RC. Bacterial contamination as a factor
inuencing the toxicity of materials to the exposed pulp.
Oral Surg 1987;64:466.
103. Cox CF. Pulp capping of dental pulp mechanically exposed to
oral microora: a 1-2 year observation of wound healing in
the monkey. J Oral Pathol 1985;14:156.
104. Cox CF, et al. Biocompatibility of surface sealed dental materi-
als against exposed pulps. J Prosthet Dent 1987;57:1.
105. Nyborg H. Capping of the pulp. The processes involved and
their outcome. Odontol Tidskr 1958;66:296.
106. Phaneuf RA, Frankl S, Reuben M. A comparative histological
evaluation of three calcium hydroxide preparations on
human primary dental pulp. J Dent Child 1968;35:61.
107. Vermeersch AC. Pulp conservation. Oper Dent 1977;2:105.
108. Joos RW. Calcium hydroxide as a pulp capping agent.
Northwest Dent 1974;53:362.
109. Tamburic SD, Vuleta GM, Ognjanovic JM. In vitro release of
calcium and hydroxyl ions from two types of calcium
hydroxide preparations. Int Endod J 1993;26:125.
110. Yoshiba K, Yoshiba N, Nakamura H, et al., editors.
Immunolocalization of bronectin during reparative
dentinogenesis in human teeth after pulp capping with cal-
cium hydroxide. J Dent Res 1996;75:1590.
111. Fisher FJ. The effect of a calcium hydroxide/water paste on
micro-organisms in carious dentine. Br Dent J
1972;143:231.
112. Lado EA. In vitro antimicrobial activity of six pulp capping
agents. Oral Surg 1986;61:197.
113. Estrela C, Fabiana CP, Yoto I, Bammann LL. In vitro determi-
nation of direct antimicrobial effect of calcium hydroxide.
JOE 1998;24:15.
114. Sciaky I, Pisanti S. Localization of calcium placed over ampu-
tated pulps in dogs teeth. J Dent Res 1960;39:1128.
115. Attalla MN, Noujaim AA. Role of calcium hydroxide in the
formation of reparative dentin. Can Dent Assoc J
1969;35:267.
116. Stark MM, et al. The localization of radioactive Ca(OH)
2
(Ca45) over exposed pulps in rhesus monkey teeth: a pre-
liminary report. J Oral Ther Pharmacol 1964;3:290.
117. Holland R, et al. Histochemical analysis of the dogs dental
pulp after pulp capping with calcium, barium, and stron-
tium hydroxides. JOE 1982;8:444.
118. Turner C, Courts FJ, Stanley HR. A histological comparison of
direct pulp capping agents in primary canines. J Dent Child
1987;54:423.
119. Tronstad L. Reaction of the exposed pulp to Dycal treatment.
Oral Surg 1974;38:945.
120. Drahein R, Murrey A. Compressive strength of two calcium
hydroxide bases. J Prosthet Dent 1985;54:365.
121. Fuks AB, et al. Clinical and radiographic assessment of direct
pulp capping and pulpotomy in young permanent teeth.
Pediatr Dent 1982;4:240.
122. Stanley HR, Pameijer CH. Pulp capping with a new
visible-light-curing calcium hydroxide composition. Oper
Dent 1985;10:156.
123. Seale NS, Stanley HR. Pulpal response to a new visible light
cured composite calcium hydroxide pulp capping agent in
human premolars. Pediatr Dent 1988;10:239.
124. Howerton B, Cox CF. Pulpal biocompatibility of two
photo-cured Ca(OH)
2
containing materials [abstract].
JOE 1987;13:129.
Pediatric Endodontics 899
150. Kanca J III. Bonding to tooth structurea rationale for a clin-
ical protocol. J Esthet Dent 1989;1:1358.
151. Miyakoshi S, et al. Interfacial interaction of 4-META-MMA-TBB
resin and the pulp [abstract]. J Dent Res 1993;72:220.
152. Cox CF, et al. Pulp response following in vivo etching and
4-META bonding. J Dent Res 1993;72:213.
153. Cox CF, White KC. Biocompatibility of amalgam on exposed
pulps employing a biological seal [abstract]. J Dent Res
1992;71:187.
154. Tsuneda Y, Hayakawa T, Yamamoto H, et al. A histopathologi-
cal study of direct pulp capping with adhesive resins. Oper
Dent 1995;20:223.
155. Kashiwada T, Takagi M. New restoration and direct pulp cap-
ping systems using adhesive composite resin. Bull Tokyo
Med Dent Univ 1991;38:45.
156. Heitman T, Unterbrink G. Direct pulp capping with a dentinal
adhesive resin systema pilot study. Quintessence Int
1995;26:765.
157. Bazzuchi M, et al. Pulp response to direct capping of adhesive
resins and glass ionomer cements [abstract]. J Dent Res
1995;74:555.
158. Kanca J III. Replacement of a fractured incisor fragment over
pulpal exposure: a long-term case report. Quintessence Int
1996;27:829.
159. Stanley HR. Pulpal consideration of adhesive materials. Oper
Dent 1992;55:151.
160. Pameijer CH, Stanley HR. The disastrous effects of the total
etch technique in vital pulp capping in primates. Am J
Dent 1998;11:S45.
161. Araujo FB, Barata JS, Costa CAS, Garcia-Godoy F. Clinical,
radiographical and histological evaluation of direct cap-
ping with a resin adhesive in primary teeth [abstract]. J
Dent Res 1996;75:280.
162. Gwinnett AJ, Tay FR. Early and intermediate time response of
the dental pulp to an acid etch technique in vivo. Am J
Dent 1998;11:S35.
163. Kopel HM. The pulp capping procedure in primary teeth
revisited. J Dent Child 1997;64:327.
164. Cox CF, et al. Biocompatibility of various dental materials:
pulp healing with a surface seal. Int J Periodont Rest Dent
1996;16:241.
165. Stanley HR, Pameijer CH. Dentistrys friendcalcium
hydroxide. Oper Dent 1997; 22:1.
166. Katoh Y, et al. Direct capping effects on exposed pulp of maca-
ca fascicularis [abstract]. J Dent Res 1996;75:34.
167. Katoh Y, Kimura T, Inaba T. Clinical prognosis of pulp tissue
direct-capping with adhesive resins [abstract]. J Dent Res
1997;76:162.
168. Torabinejad M, et al. Physical and chemical properties of a new
root-end lling material. JOE 1995;21:349.
169. Pitt Ford TR, Torabinejad M, Abedi HR, et al. Using mineral
trioxide aggregate as a pulp capping material. J Am Dent
Assoc 1996;127:1491.
170. Chaung HM, et al. Comparison of calcium phosphate cement
mixture and pure calcium hydroxide as direct pulp-cap-
ping agents. J Formos Med Assoc 1996;95:545.
171. Yoshimine Y, Maeda K. Histologic evaluation of tetracalcium
phosphate-based cement as a direct pulp-capping agent.
Oral Surg Oral Med Oral Pathol Oral Radiol Endod
1995;79:351.
172. Dannenberg JL. Pedodontic endodontics. Dent Clin North Am
1974;18:367.
173. Mejare I. Pulpotomy of primary molars with coronal or total
pulpitis using formocresol technique. Scand J Dent Res
1979;87:208.
174. Ranly DM. Pulpotomy therapy in primary teeth: new modali-
ties for old rationales. Pediatr Dent 1994;16:403.
175. Berger JE. A review of the erroneously labeled mummica-
tion techniques of pulp therapy. Oral Surg 1972;34:131.
176. Urist M. Bone formation by autoinduction. Science
1965;150:893.
177. Nakashima M. Induction of dentin formation on canine
amputated pulp by recombinant human bone morpho-
genetic proteins (BMP)-2 and -4. J Dent Res 1994;73:1515.
178. Fadhavi S, Anderson AW. A comparison of the pulpal response
to freeze-dried bone, calcium hydroxide, and zinc oxide-
eugenol in primary teeth in two cynomolgus monkeys.
Pediatr Dent 1996;18:52.
179. Buckley JP. The chemistry of pulp decomposition with a
rational treatment for this condition and its sequelae. J Am
Dent Assoc 1904;3:764.
180. Sweet CA. Procedure for treatment of exposed and pulpless
deciduous teeth. J Am Dent Assoc 1930;17:1150.
181. Sweet CA. Treatment of vital primary teeth with pulpal
involvementtherapeutic pulpotomy. Colorado State
Dent Assoc J 1955;33:10.
182. Doyle WA, McDonald RE, Mitchell DF. Formocresol versus
calcium hydroxide in pulpotomy. J Dent Child 1962;29:86.
183. Massler M, Mansukhani H. Effects of formocresol on the den-
tal pulp. J Dent Child 1959;26:277.
184. Emmerson CC, Miyamoto O, Sweet CA Sr, Bhatia HD. Pulpal
changes following formocresol applications on rat molars
and human primary teeth. South Calif Dent Assoc J
1959;27:309.
185. Spedding RH, Mitchell DF, McDonald RE. Formocresol and
calcium hydroxide therapy. J Dent Res 1965;44:1023.
186. Law DB, Lewis TM. Formocresol pulpotomy in deciduous
teeth. J Am Dent Assoc 1964;69:601.
187. Berger J. Pulp tissue reaction from formocresol and zinc oxide
and eugenol. J Dent Child 1965;32:13.
188. Spamer RG. The formocresol pulpotomy: a histological study
of a single application of formocresol on the dental pulp of
human primary teeth [thesis]. Seattle (WA): Univ. of
Washington School of Dentistry; 1965.
189. Rolling I, Thylstrup A. A three-year clinical follow up study of
pulpotomized primary molars treated with the formocre-
sol technique. Scand J Dent Res 1975;83:47.
190. Rolling I, Hasselgren G, Tronstad L. Morphologic and enzyme
histochemical observations on the pulp of human primary
molars 3 to 5 years after formocresol condition. Oral Surg
1976;42:518.
191. Rolling I, Lambjerg-Hansen H. Pulp condition of successfully
formocresol-treated primary molars. Scand J Dent Res
1978;86:267.
192. Magnusson BO. Pulpotomy in primary molars: long-term
clinical and histological evaluation. Int Dent J 1980;13:143.
193. Ranly DM, Lazzari EP. The formocresol pulpotomy: the past,
the present and the future. J Pedod 1978;3:115.
194. Beaver HA, Kopel HM, Sabes WR. The effect of zinc
oxide-eugenol cement on a formocresolized pulp. J Dent
Child 1966;33:381.
195. Garcia-Godoy F. Penetration and pulpal response by two con-
centrations of formocresol using two methods of applica-
tion. J Pedod 1981;5:102.
196. Hicks JH, et al. Formocresol pulpotomies in primary molars: a
radiographic study in a pediatric dentistry practice. J.
Pedod 1986;10:331.
197. Ranly DM, Pope HO. An in vitro comparison of the release of
3
H-formaldehyde and
14
C-p-cresol from zinc oxide
eugenol cement. Pharm Ther Dent 1979;4:53.
198. Venham LJ. Pulpal responses to variations on the formocresol
pulpotomy technique [thesis]. Columbus, OH: Ohio State
Univ. College of Dentistry; 1967.
199. Straffon LH, Han SS. The effect of formocresol on hamster
connective tissue cells: a histologic and quantitative
radioautographic study with proline H3. Arch Oral Biol
1968;13:271.
200. Straffon LH, Han S S. Effects of varying concentrations of
formocresol on RNA synthesis of connective tissue in
sponge implants. Oral Surg 1970;29:915.
201. Loos PJ, Straffon LH, Han SS. Biological effects of formocre-
sol. J Dent Child 1973;40:193.
202. Morawa AP, et al. Clinical evaluation of pulpotomies using
dilute formocresol. J Dent Child 1975;45:28.
203. Fuks A, Bimstein E. Clinical evaluation of diluted formocresol
pulpotomies in the primary teeth of school children.
Pediatr Dent 1981;3:321.
204. Fuks A, et al. A radiographic and histologic evaluation of the
effect of two concentrations of formocresol on pulpo-
tomized primary and young permanent teeth in monkeys.
Pediatr Dent 1983;5:9.
205. Wright FA, Widmer RP. Pulpal therapy in primary molar teeth:
a retrospective study. J Pedod 1979;3:195.
206. Willard RM. Radiographic changes following formocresol
pulpotomies in primary molars. J Dent Child 1976;43:34.
207. Garcia-Godoy F. Radiographic evaluation of root canal calci-
cation following formocresol pulpotomy. J Dent Child
1983;50:430.
208. Koch G, Nyborg H. Correlation between clinical and histolog-
ic indications for pulpotomy of deciduous teeth. J Int Assoc
Dent Child 1970;1:3.
209. Mejare I. Pulpotomy of primary molars with coronal or total
pulpitis using formocresol technique. Scand J Dent Res
1979;87:208.
210. Garcia-Godoy F, et al. Pulpal response to different application
times of formocresol. J Pedod 1982;6:176.
211. Miyamoto O. Current status of pulpal therapy on primary and
young permanent teeth. J Acad Dent Handicapped
1974;1:27.
212. Verco PJ, Allen KR. Formocresol pulpotomies in primary
teeth. J Int A Dent Child 1984;15:51.
213. Avram DC, Pulver F. Pulpotomy medicaments for vital pri-
mary teeth. J Dent Child 1989;56:426.
214. Ibrahim SM, et al. A histopathological study of the effects of
formocresol in pulp capping of permanent teeth. Egypt
Dent J 1970;16:219.
215. Trask PA. Formocresol pulpotomy in young permanent teeth.
J Am Dent Assoc 1972;85:1316.
216. Myers DA. Effects of formocresol on pulps of cariously
exposed permanent molars [thesis]. Memphis, TN:
University of Tennessee School of Dentistry; 1972.
217. Armstrong RL, et al. Comparison of Dycal and formocresol
pulpotomies in young permanent teeth in monkeys. Oral
Surg 1979;48:160.
218. Fiskio HM. Pulpotomies in vital and non-vital permanent
teeth. Gen Dent 1974;22:27.
900 Endodontics
219. Spedding RH. Formocresol pulpotomies for permanent teeth.
In: Goldman HM, et al., editors. Current therapy in den-
tistry. Vol 5. St. Louis: CV Mosby; 1975.
220. Rothman MS. Formocresol pulpotomy: a practical procedure
for permanent teeth. Gen Dent 1977;25:29.
221. Schwartz EA. Formocresol vital pulpotomy on permanent
dentition. Can Dent Assoc J 1980;46:570.
222. Muniz MA, et al. The formocresol technique in young perma-
nent teeth. Oral Surg 1983;55:611.
223. Akbar A. A ve year clinical study of formocresol treatment in
120 cases of pulpotomy in permanent molars. J Pedod
1987;11:242.
224. Nishino PK. Apical histologic response to formocresol pulpo-
tomy. Chron Omaha Dent Soc 1974;37:242.
225. Teuscher GW, Zander HA. A preliminary report on pulpoto-
my. Northwest Univ Grad Bull 1938;39:4.
226. Ulmansky M, et al. Scanning electron microscopy of calcium
hydroxide induced bridges. J Oral Pathol 1972;1:244.
227. Goldberg F, et al. Evaluation of the dentinal bridge after pulpo-
tomy and calcium hydroxide dressing. JOE 1984;10:318.
228. Berk H. Effects of calcium hydroxide methyl-cellulose paste on
the dental pulp. J Dent Child 1950;17:65.
229. Brown WE Jr. The vital pulpotomy technique for the manage-
ment of vital exposed pulps in primary and young perma-
nent teeth. Univ Mich Alumni Bull 1947;48:14.
230. Via WR Jr. Evaluation of deciduous molars treated by pulpo-
tomy and calcium hydroxide. J Am Dent Assoc 1955;
50:34.
231. Law DB. An evaluation of the vital pulpotomy technique. J
Dent Child 1956;23:40.
232. Schrder U, Granath LE. On internal dentin resorption in
deciduous molars treated by pulpotomy and capped with
calcium hydroxide. Odontol Revy 1971;22:179.
233. Schrder U. A 2-year follow-up of primary molars, pulpo-
tomized with a gentle technique and capped with calcium
hydroxide. Scand J Dent Res 1978;86:273.
234. Berk H, Krakow A. A comparison of the management of pul-
pal pathosis in primary and permanent teeth. Oral Surg
1952;34:944.
235. Berson RB, Good D. Pulpotomy and pulpectomy for primary
teeth. In: Stewart RL, et al. editors. Pediatric dentistry: sci-
entic foundation and clinical practice. St. Louis: CV
Mosby; 1982. p. 91726.
236. Patterson SS. Pulp calcication due to operative procedures
pulpotomy. Int Dent J 1967;17:490.
237. Bimstein CD, et al. Histologic evaluation of the effect of dif-
ferent cutting techniques on pulpotomized teeth. Am J
Dent 1989;2:151.
238. Pashley EL, et al. Systemic distribution of
14
C-formaldehyde
from formocresol-treated pulpotomy sites. J Dent Res
1980;59:603.
239. Myers DR, et al. Tissue changes induced by the absorption of
formocresol from pulpotomy sites in dogs. Pediatr Dent
1983;5:6.
240. Ranly DM. Formocresol toxicity: current knowledge. Acta
Odontol Pediatr 1984;5:93.
241. Ranly DM, Horn D. Assessment of the systemic distribution
and toxicity of formaldehyde following pulpotomy treat-
ment. Part Two. J Dent Child 1987;54:404.
242. Messer LB, et al. Long-term effects of primary molar pulpo-
tomies on succedaneous bicuspids. J Dent Res 1980;59:116.
Pediatric Endodontics 901
243. Rollings I, Paulsen S. Formocresol pulpotomy of primary teeth
and occurrence of enamel defects of permanent successors.
Acta Odontol Scand 1978;36:243.
244. Mulder GR, et al. Consequences of endodontic treatment of
primary teeth. Part II. A clinical investigation into the
inuence of formocresol pulpotomy on the permanent
successor. J Dent Child 1987;54:35.
245. American Academy of Pediatric Dentistry. Use of formocresol
in pedodontics: a committee report. Chicago: 1984.
246. Sadler ES, Frankl S, Ruben MP. The histological response of
the dental pulp to Cresatin. J Dent Child 1971;38:49.
247. Nevins AJ, et al. Pulpotomy and partial pulpectomy proce-
dures in monkey teeth using cross-linked collagen-calcium
phosphate gel. Oral Surg 1980;49:360.
248. s-Gravenmade E J. Some biochemical considerations in
endodontics. JOE 1975;1:233.
249. Hill SD, et al. Comparison of antimicrobial and cytotoxic
effects of glutaraldehyde and formocresol. Oral Surg
1991;71:89.
250. Wernes JC, s-Gravenmade EJ. Glutaraldehyde: a new xative
in endodontics [abstract]. JDR 1973;52:601.
251. Dankert J, et al. Diffusion of formocresol and glutaraldehyde
through dentin and cementum. JOE 1976;2:42.
252. Kopel HM, Bernick S, Zachrisson E. The effects of glutaralde-
hyde on primary pulp tissue following coronal amputation:
an in vivo histologic study. J Dent Child 1980;47:425.
253. Dilly G, Courts FJ. Immunological response to four pulpal
medicaments. Pediatr Dent 1981;3:179.
254. Lekka M, et al. Comparison between formaldehyde and glu-
taraldehyde diffusion through root tissues of pulpotomy
treated teeth. J Pedod 1984;8:185.
255. Garcia-Godoy F. A 42 month clinical evaluation of glutaralde-
hyde pulpotomies in primary teeth. J Pedod 1986;10:148.
256. Fuks A, Bernstein E, Klein H. Assessment of a 2% buffered glu-
taraldehyde solution in pulpotomized primary teeth of
children: a preliminary report. J Pedod 1986;10:323.
257. Alacam A. Pulpal tissue changes following pulpotomies with
formocresol, glutaraldehyde-calcium hydroxide, glu-
taraldehyde-zinc oxide eugenol pastes in primary teeth. J
Pedod 1989;13:123.
258. Davis M, et al. An alternative to formocresol for vital pulpoto-
my. J Dent Child 1982;49:176.
259. Fuks AB, et al. Glutaraldehyde as a pulp dressing after pulpotomy
in primary teeth of baboon monkeys. Pediatr Dent 1986;8:32.
260. Lloyd JM, et al. The effects of various concentrations and
lengths of application of glutaraldehyde on monkey pulp
tissue. Pediatr Dent 1988;10:115.
261. Ranly DM, Garcia-Godoy F, et al. Time, concentration and pH
parameters for the use of glutaraldehyde as a pulpotomy
agent: an in vitro study. Pediatr Dent 1987;9:199.
262. Garcia-Godoy F, Ranly DM. Clinical evaluation of pulpo-
tomies with ZOE as the vehicle for glutaraldehyde. Pediatr
Dent 1987;9:144.
263. Hernandez JRP, et al. Evaluaion clinica y radiograca de
pulpotomies on formocresol o glutaraldehydo en dientes
phmonentes [abstract]. Acta Odontol Pediatr 1987;8:59.
264. Myers DR, et al. Systemic absorption of
14
C-glutaraldehyde
from glutaraldehyde-treated pulpotomy sites. Pediatr Dent
1986;8:134.
265. Ranly DB, et al. Assessment of the systemic distribution and
toxicity of glutaraldehyde as a pulpotomy agent. Pediatr
Dent 1989;11:8.
266. Kouri EM, Matthews JL, Taylor PP. Epinephrine in pulpotomy.
J Dent Child 1969;36:123
267. Helig J, Yates J, Siskin M, et al. Calcium hydroxide pulpotomy
for primary teeth: a clinical study. J Am Dent Assoc
1984;108:7758.
268. Landau M, Johnson D. Pulpal responses to ferric sulfate in
monkeys [abstract]. J Dent Res 1988;67:215.
269. Fei AL, Udin RD, Johnson R. A clinical study of ferric sulfate as
a pulpotomy agent in primary teeth. Pediatr Dent
1991;13:327.
270. Fuks AB, Holan G, Davis JM, Eidelman E. Ferric sulfate versus
dilute formocresol in pulpotomized primary molars: long-
term follow-up. Pediatr Dent 1997;19:327.
271. Fuks AB, Eidelman E, Cleaton-Jones P, Michaeli Y. Pulp
response to ferric sulfate, diluted formocresol, and IRM in
pulpotomized primary baboon teeth. J Dent Child
1997;64:2549.
272. Abedi HR, Ingle JI. Mineral trioxide aggregate: a review of a
new cement. Calif Dent Assoc J 1995;23:36.
273. Higashi T, Okamoto H. Inuence of particle size of calcium
phosphate ceramics as a capping agent on the formation of
a hard tissue barrier in amputated pulp. J Endod
1996;22:281.
274. Yoshiba K, Yoshiba N, Iwaku M. Histological observations of
hard tissue barrier formation in amputated dental pulp
capped with alpha-tricalcium phosphate containing calci-
um hydroxide. Endod Dent Traumatol 1994;10:113.
275. Ruemping DR, et al. Electrosurgical pulpotomy in primates
a comparison with formocresol. Pediatr Dent 1983;5:14.
276. Shaw DW, Sheller B, Barrus BD, Morton TH Jr. Electrosurgical
pulpotomya 6-month study in primates. JOE
1987;13:500.
277. Shulman ER, et al. Comparison of electrosurgery and
formocresol as pulpotomy techniques in monkey primary
teeth. Pediatr Dent 1987;9:189.
278. Sheller B, Morton TH. Electrosurgical pulpotomy: a pilot
study in humans. JOE 1987;13:69.
279. Mack RB, Dean JA. Electrosurgical pulpotomy: a retrospective
human study. J Dent Child 1993;60:107.
280. Fishman SA, Udin RD, Good DL, Rodef F. Success of electro-
fulguration pulpotomies covered by zinc oxide-eugenol or
calcium hydroxide: a clinical study. Pediatr Dent
1996;18:385.
281. Adrian JC. Pulp effect of neodymium laser. Oral Surg Oral
Med Oral Pathol Oral Radiol Endod 1977;44:301.
282. Shoji S, Nakamura M, Horiuchi H. Histopathological changes
in dental pulps irradiated by CO
2
laser: a preliminary
report on laser pulpotomy. JOE 1985;11:379.
283. Kato J, Hashimoto M, Ono H. Pulp reactions after pulpotomy
with Nd:YAG laser irradiation [abstract]. J Dent Res
1991;70:384.
284. McGuire S, et al. Comparison of Nd:YAG laser with formocre-
sol in permanent tooth pulpotomies in dogs [abstract]. J
Dent Res 1995;74:160.
285. Hibbard ED, Ireland RL. Morphology of the root canals of the
primary molar teeth. J Dent Child 1957;24:250.
286. Barker BC, et al. Anatomy of root canals. IV. Deciduous teeth.
Austr Dent J 1975;20:101.
287. Hartsook JT. Pulpal therapy in primary and young permanent
teeth. Dent Clin North Am 1966; p.385.
288. Hallett GE. Endodontic treatment and conservation of tempo-
rary teeth. Int Dent J 1968;18:520.
289. Matsumiya S. Experimental pathological study on the effect of
treatment of infected root canals in the deciduous tooth on
growth of the permanent tooth germ. Int Dent J
1968;18:546.
290. Valdenhaug J. Periradicular inammation in primary teeth
and its effect on the permanent successors. Int J Oral Surg
1974;3:171.
291. Brook AH, Winter GB. Developmental arrest of permanent
tooth germs following pulpal infection of deciduous teeth.
Br Dent J 1975;139:9.
292. Marsh SJ, Largent MD. A bacteriological study of the pulp
canals of infected primary molars. J Dent Child
1967;34:460.
293. ORiordan MW, Coll J. Pulpectomy procedure for deciduous
teeth with severe pulpal necrosis. J Am Dent Assoc
1979;99:480.
294. Tagger E, Sarnat H. Root canal therapy of infected primary
teeth. Acta Odontol Pediatr 1984;5:63.
295. Camp JH. Pedodontic-endodontic treatment. In: Cohen S,
Burns RC, editors. Pathways of the pulp. St. Louis: CV
Mosby; 1987. p. 685722.
296. Rifkin A. A simple, effective safe technique for the root canal
treatment of abscessed primary teeth. J Dent Child
1980;47:435.
297. Rabinowitz BZ. Pulp management of primary teeth. Oral Surg
1953; 6:542.
298. Rabinowitz BZ. Pulp management of primary teeth. Oral Surg
1953;6:671.
299. Hobson P. Pulp treatment of deciduous teeth. Br Dent J
1970;128:275.
300. Judd P, Kenny D. Non-aldehyde pulpectomy technique for pri-
mary teeth. Ontario Dentist 1991;68:25.
301. Gould JM. Root canal therapy for infected primary molar
teeth - preliminary report. J Dent Child 1970;34:23.
302. Cullen CL. Endodontic therapy of deciduous teeth. Compend
Contin Educ 1983;4:302.
303. Dugal MS, Curgon ME. Restoration of the broken down pri-
mary molar: 1. Pulpectomy technique. Dent Update
1989;16:26.
304. Goerig AC, Camp JH. Root canal treatment in primary teeth:
a review. Pediatr Dent 1983;5:33.
305. Kopel HM. Root canal therapy for primary teeth. Mich Dent
Assoc J 1970;52:28.
306. Spedding R. Endodontic treatment of primary molars. In:
Goldman HM, et al., editors. Current therapy in dentistry.
St. Louis: CV Mosby; 1977. p. 55869.
307. Coll JA, Josell S, Casper JS. Evaluation of a one appointment
formocresol pulpectomy technique for primary molars.
Pediatr Dent 1985;7:123.
308. Vander Wall GL, et al. Endodontic medicaments. Oral Surg
1972;25:238.
309. Barr ES, et al. Radiographic evaluation of primary molar
pulpectomies in a pediatric dental practice [abstract].
Pediatr Dent 1986;8:180.
310. Coll JA, et al. An evaluation of pulpal therapy in primary inci-
sors. Pediatr Dent 1988;10:178.
311. Flaitz CM, et al. Radiographic evaluation of pulpal therapy for
primary anterior teeth. J Dent Child 1989;56:182.
312. Yacobi R, et al. Evolving primary pulp therapy techniques. J
Am Dent Assoc 1991;122:83.
902 Endodontics
313. Payne RG, Kenny DJ, Johnston DH, Judd PL. Two year out-
come study of zinc oxide-eugenol root canal treatment for
vital primary teeth. J Can Dent Assoc 1993;59:1.
314. Hendry J, Jeansonne BG, Dummett CO Jr, Burrell W.
Comparison of calcium hydroxide and zinc oxide and
eugenol pulpectomies in primary teeth of dogs. Oral Surg
Oral Med Oral Pathol Oral Radiol Endod 1982;54:445.
315. Barker BC, Lockett BC. Endodontic experiments with
resorbable paste. Aust Dent J 1971;16:364.
316. Rifkin A. The root canal treatment of abscessed primary teeth:
a 3-4 year follow-up. J Dent Child 1982;49:428.
317. Zilberman UL, Mass E. Endodontic treatment of infected pri-
mary teeth using Maistos paste. J Dent Child 1989;56:117.
318. Garcia-Godoy F. Evaluation of an iodoform paste in root canal
therapy for infected primary teeth. J Dent Child
1987;54:30.
319. Holan G, Fuks AB. A comparison of pulpectomies using ZOE
and Kri Paste in primary molars: a retrospective study.
Pediatr Dent 1993;15:403.
320. Glauser RO. Preventive orthodontics and limited treatment
procedures. US Public Health Service, Division of Indian
Health; 1967.
321. Greenberg M. Filling root canals of deciduous teeth by an
injection technique. Dent Dig 1961;67:574.
322. Krakow A, et al. Advanced endodontics in pedodontics. In:
White G, editor. Clinical oral pediatrics. Chicago:
Quintessence; 1981. p. 24864.
323. Aylard S, Johnson R. Assessment of lling techniques for pri-
mary teeth. Pediatr Dent 1987;9:195.
324. Mack RB, Halterman CW. Labial pulpectomy access followed
by esthetic composite resin restoration for nonvital maxil-
lary deciduous incisors. J Am Dent Assoc 1980;100:374.
325. Ripa LW. Pulp therapy for the primary dentition. II. The treat-
ment of teeth with non-vital or degenerating pulps. Conn
State Dent Assoc J 1970;44:210.
326. American Academy of Pediatric Dentistry guidelines for pulp
therapy for primary and young permanent teeth. Pediatr
Dent 1998;20:43.
327. Velling RJ. A study of the treatment of infected and necrotic
primary teeth. J Dent Child 1961;28:213.
328. Droter JA. Pulp therapy in primary teeth. J Dent Child
1967;34:507.
329. Full CA. Pulpotomy treatment of stulated primary molars.
Quintessence Int 1979;10:73.
330. Meyer FW, Sayegh FS. Wound healing following curettement
of bifurcation abscesses of human primary molars. Oral
Surg 1979;47:267.
331. Parkins FM, et al. Coronal vs. canal therapy for non-vital pri-
mary molars: a clinical trial [abstract]. JDR 1977;56:143.
332. Myers DR, et al. Histopathology of radiolucent furcation
lesions associated with pulpotomy-treated primary molars.
Pediatr Dent 1988;10:291.
333. Starkey P. Treatment of pulpally involved primary molars. In:
McDonald RE, et al, editors. Current therapy in dentistry.
St. Louis: CV Mosby; 1980. p. 414.
334. Erausquin J, Devoto FC. Alveolodental ankylosis induced by
root canal treatment in rat molars. Oral Surg 1970;30:105.
335. Coll JA, Sadrian R. Predicting pulpectomy success and its rela-
tionship to exfoliation and succedaneous dentition. Pediatr
Dent 1996;18:57.
Вам также может понравиться
- Diagnostic Management of InterdenDtal SpacingДокумент3 страницыDiagnostic Management of InterdenDtal SpacingUngureanu DaniaОценок пока нет
- ProductsДокумент4 страницыProductsUngureanu DaniaОценок пока нет
- Start MeДокумент18 страницStart MeAlexandru Dumitru100% (1)
- Pharmacology of TicДокумент10 страницPharmacology of Ticab0maiОценок пока нет
- CH 19Документ38 страницCH 19Ungureanu DaniaОценок пока нет
- IndexДокумент24 страницыIndexUngureanu DaniaОценок пока нет
- CH 16Документ16 страницCH 16Ungureanu DaniaОценок пока нет
- CH 14Документ26 страницCH 14Ungureanu DaniaОценок пока нет
- Endodontic Cavity PreparationДокумент166 страницEndodontic Cavity Preparationagusaranp0% (1)
- CH 13Документ22 страницыCH 13Kamonrat LimОценок пока нет
- Dental TraumaДокумент50 страницDental TraumaElena PruniciОценок пока нет
- CH 08Документ70 страницCH 08Ungureanu DaniaОценок пока нет
- ch11Документ98 страницch11Alina TomaОценок пока нет
- CH 12Документ78 страницCH 12whussien7376100% (1)
- CH 09Документ48 страницCH 09Ungureanu DaniaОценок пока нет
- CH 04Документ80 страницCH 04flock_duxОценок пока нет
- Ch07 Dental PainДокумент28 страницCh07 Dental PainMaryam KatibehОценок пока нет
- CH06Документ56 страницCH06Prasun Sit SharmaОценок пока нет
- CH 03Документ32 страницыCH 03basharakmОценок пока нет
- Periradicular Lesions (Chapter 5)Документ28 страницPeriradicular Lesions (Chapter 5)revlieeОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Compliance Risks and Controls: Speaker: Dott. Fabio AccardiДокумент14 страницCompliance Risks and Controls: Speaker: Dott. Fabio AccardiJefferson WidodoОценок пока нет
- 2018 JC2 H2 Maths SA2 River Valley High SchoolДокумент50 страниц2018 JC2 H2 Maths SA2 River Valley High SchoolZtolenstarОценок пока нет
- PQ of Vial Washer Ensures Removal of ContaminantsДокумент25 страницPQ of Vial Washer Ensures Removal of ContaminantsJuan DanielОценок пока нет
- PhysicsLab PreReport201Документ9 страницPhysicsLab PreReport201Giuliana SchulzОценок пока нет
- Ut ProcedureДокумент2 страницыUt ProcedureJJ WeldingОценок пока нет
- MCS Adopts Milyli Software Redaction Tool BlackoutДокумент3 страницыMCS Adopts Milyli Software Redaction Tool BlackoutPR.comОценок пока нет
- Course Code: Hrm353 L1Документ26 страницCourse Code: Hrm353 L1Jaskiran KaurОценок пока нет
- NYU Stern Evaluation NewsletterДокумент25 страницNYU Stern Evaluation NewsletterCanadianValueОценок пока нет
- Candida by Shaw, George Bernard, 1856-1950Документ61 страницаCandida by Shaw, George Bernard, 1856-1950Gutenberg.orgОценок пока нет
- Nistha Tamrakar Chicago Newa VIIДокумент2 страницыNistha Tamrakar Chicago Newa VIIKeshar Man Tamrakar (केशरमान ताम्राकार )Оценок пока нет
- Explosive Loading of Engineering Structures PDFДокумент2 страницыExplosive Loading of Engineering Structures PDFBillОценок пока нет
- Making An Appointment PaperДокумент12 страницMaking An Appointment PaperNabila PramestiОценок пока нет
- CuegisДокумент2 страницыCuegisTrishaОценок пока нет
- Data Science From Scratch, 2nd EditionДокумент72 страницыData Science From Scratch, 2nd EditionAhmed HusseinОценок пока нет
- Viviana Rodriguez: Education The University of Texas at El Paso (UTEP)Документ1 страницаViviana Rodriguez: Education The University of Texas at El Paso (UTEP)api-340240168Оценок пока нет
- Certification of Psychology Specialists Application Form: Cover PageДокумент3 страницыCertification of Psychology Specialists Application Form: Cover PageJona Mae MetroОценок пока нет
- ARTICLE - Well Drilling & Completion Design and BarriersДокумент34 страницыARTICLE - Well Drilling & Completion Design and BarriersNathan RamalhoОценок пока нет
- Blocked threads jstack analysisДокумент69 страницBlocked threads jstack analysisMike TОценок пока нет
- Chapter 20: Sleep Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionДокумент4 страницыChapter 20: Sleep Garzon Maaks: Burns' Pediatric Primary Care, 7th EditionHelen UgochukwuОценок пока нет
- Berserker - Lifting Wood and Stone Like A Viking Strongman Bodybuilding Functional StrengthДокумент10 страницBerserker - Lifting Wood and Stone Like A Viking Strongman Bodybuilding Functional Strengthluciferr71Оценок пока нет
- Springhill Suites by Marriott / Houston Brookhollow Remit To:2750 N.Loop West, Houston TX 77092 713.290.9242Документ1 страницаSpringhill Suites by Marriott / Houston Brookhollow Remit To:2750 N.Loop West, Houston TX 77092 713.290.9242Josué SalazarОценок пока нет
- Generic Strategies: Lessons From Crown Cork & Seal and Matching DellДокумент16 страницGeneric Strategies: Lessons From Crown Cork & Seal and Matching DellavaОценок пока нет
- Doohap supplier and customer segmentationДокумент2 страницыDoohap supplier and customer segmentationPriyah RathakrishnahОценок пока нет
- Mechanical Function of The HeartДокумент28 страницMechanical Function of The HeartKarmilahNОценок пока нет
- PHCДокумент1 страницаPHCsinh24X7Оценок пока нет
- C ProgrammingДокумент205 страницC ProgrammingSrinivasan RamachandranОценок пока нет
- CVCITC Smoke-Free Workplace Policy & ProgramДокумент2 страницыCVCITC Smoke-Free Workplace Policy & ProgramKristine Joy CabujatОценок пока нет
- Environmental ScienceДокумент5 страницEnvironmental Sciencearijit_ghosh_18Оценок пока нет
- Name: Chakshu Purohit Course: BBA LLB Subject: Legal Research and Methodology Submitted To: Utkarsh MishraДокумент5 страницName: Chakshu Purohit Course: BBA LLB Subject: Legal Research and Methodology Submitted To: Utkarsh Mishrachakshu purohitОценок пока нет
- Alarm Management Second Ed - Hollifield Habibi - IntroductionДокумент6 страницAlarm Management Second Ed - Hollifield Habibi - IntroductionDavid DuranОценок пока нет