Академический Документы
Профессиональный Документы
Культура Документы
Nursing Care Plan Weebly
Загружено:
api-277498943Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Nursing Care Plan Weebly
Загружено:
api-277498943Авторское право:
Доступные форматы
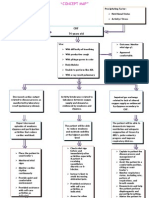
Nursing Diagnosis: Decreased cardiac output r/t impaired contractility of the heart, secondary to CHF, AEB weak peripheral
pulses, ARF, fatigue, and hx of AFIB
Long Term Goal: Pt will have adequate cardiac output
OUTCOME
CRITERIA
1.
2.
INTERVENTIONS
Pts BP will remain between
90/50-140/90mmHg; pulse
60-100bpm, regular rhythm;
respirations 12-20 per minute,
easy and unlabored; O2 sat
95-100%; and temp 96.8100.4F as assessed q4h
Independent/Assess:
Pt will remain alert and
oriented to person, place, and
time as assessed and at all
times
Independent/Assess:
Assess vital signs and O2
sat q4h and PRN
RATIONALE
EVALUATION
Most patients have compensatory
tachycardia and significantly decrease BP in
response to reduced cardiac output. Rapid
shallow respirations are characteristic of
reduced cardiac output. O2 sat would
decrease if blood was not adequately
perfusing the extremities. A decrease in
temp could also indicate inadequate
perfusion. Since this pt has CHF, Afib, and
fatigue, monitoring vitals would/could
indicate a change in health status (NCP
Gulanick/Myers p38).
Partially met. All
vitals were WNL
except respirations.
Respirations were
increased but pt
showed no other s/s
of distress.
A change in LOC is indicative of decreased
cerebral tissue perfusion and hypoxia.
Assess for any changes in Restlessness, irritability, and difficulty
concentrating may precede a change in
LOC q4h and PRN
LOC. If these s/s were to occur, they would
indicate reduced cerebral tissue perfusion
and require prompt intervention. A decrease
in cerebral tissue perfusion would be due to
decreased CO because the heart cant
contract well enough to get blood to the
brain (NCP Gulanick/Myers p38).
Outcome criteria
met.
3.
4.
Pt will maintain adequate
fluid balance and not gain
>2lbs per day when assessed
qday and PRN
Independent/Assess:
Pt will have S1 and S2 heart
sounds, and be free of S3 or
S4 heart sounds when
assessed q4h
Independent/Assess:
Assess fluid balance and
weight gain qday and
PRN
Assess heart sounds by
auscultating apical pulse
for 1 full min q4h
This pt has CHF, and acute renal failure.
One of the clinical manifestations of CHF is
excess fluid volume which increases
preload and afterload therefore decreasing
cardiac output. On admission the pt had s/s
oliguria, which is a sign of decreased renal
perfusion. Since the heart pumps blood to
the kidneys, which filter and excrete excess
fluid, ARF can compromise u/o and lead to
FVE (which decreases CO) (NCP
Gulanick/Myers p38).
Outcome criteria
met.
S1 and S2 heart sounds are normal/expected Outcome criteria
sounds (Lub/Dub). S3 or S4 sounds are
met.
abnormal. S3 sounds indicate excess fluid
volume and S4 sounds indicate stiff
ventricular wall. Since this pt has CHF, it is
essential to listen for abnormal heart sounds
to monitor for a change or worsening
condition. Impaired contractility of the heart
can lead to S3/S4 sounds which indicate
problems that can lead to decreased
peripheral pulses and renal perfusion (NCP
Gulanick/Myers p38).
5.
6.
Pt will be free of c/o fatigue
and will tolerate activities
when assessed q4h and PRN
Independent/Assess:
Pt will be free of c/o chest
pain when assessed q4h and
PRN
Independent/Assess:
Assess for reports of
fatigue and reduced
activity intolerance q4h
and PRN
Assess for chest pain q4h
and PRN
Low CO states can cause fatigue and
Unmet. When pt
exertional dyspnea d/t decreased
ambulated c/o
oxygenation of tissues. This pt has COPD as weakness.
well as CHF, so it is important to monitor
pts response to increase activity as
indicated. Activity promotes circulation and
therefore will increase tissue perfusion. The
increased tissue perfusion will strengthen
peripheral pulses and adequately perfuse the
tissues (NCP Gulanick/Myers p39).
The heart muscle can also have decreased
Outcome criteria
perfusion d/t decreased CO. If a lack of O2
met.
to the heart occurs, it presents as chest pain.
A myocardial infarction can be lifethreatening. Asking the pt if they have chest
pain can indicate if an MI is occurring.
Since this pt has CAD, ischemia may occur.
Pt also has DM, and may not feel pain d/t
neuropathy so other labs should be
monitored to also assess for an MI.
Decreased CO will lead to decreased
amounts of oxygen in the blood, which
decreases the O2 supply to the heart and this
presents as chest pain (NCP
Gulanick/Myers p39).
7.
8.
Pts peripheral pulses will
remain present at least 1+
strength/amplitude and cap
refill <3 seconds when
assessed q4h and PRN
Independent/Assess:
Pts HR will remain between
60-100bpm at a regular
rhythm at all times while
receiving Sotalol
Dependent:
Assess peripheral pulses
and capillary refill q4h
and PRN
Administer Sotalol PO
q24hrs (40mg)
(Betapace) per MD order
This pt is a 91 year old with a diagnosis of
CHF. This particular pt had peripheral
pulses at 1+amplitude. Stating an outcome
of 2+amplitude may not be possible for this
pt. The peripheral pulses may indicate
reduced circulatory efficacy, but they were
present and skin was warm. Cap refill also
monitors blood flow to extremities and
should be brisk (<3 seconds) to indicate
adequate circulation. Impaired contractility
means the heart doesnt have enough
strength to pump blood to all the
extremities, so peripheral pulses and cap
refill should be monitored (NCP
Gulanick/Myers p38)
Outcome criteria
met.
Sotalol is a class III antiarrhythmic. Since
Outcome criteria
the pt has a diagnosis of Afib, it is important met.
to maintain NSR. Atrial fibrillation
compromises CO because the atria only
quiver instead of adequately pumping and
giving the atrial kick. A lack of atrial kick
results in 30% decrease of CO. Maintaining
NSR results in increased effectiveness of
the heart and adequate CO (NCP
Gulanick/Myers p39/Davis Drug Guide
online)
9.
10.
Pts BP will remain between
90/50-140/90mmHg at all
times while receiving
Olmesartan
Dependent:
Pts BP will remain between
90/50-140/90mmHg within
approximately 3 days after
initiating Lasix therapy
Dependent:
Administer Olmesartan
tab PO qday (20mg)
(Benicar) per MD order
Administer Furosemide
tab PO qday (20mg)
(Lasix) per MD order
Pt has hx of HTN which increases afterload.
Afterload is the resistance the left ventricle
must overcome to circulate blood. Increased
afterload means increased cardiac workload
and increased stress on the left ventricle. If
the left ventricle is weak it can not pump
effectively which will decrease CO.
Keeping BP within an acceptable range
decreases afterload and improves CO.
Olmesartan is an angiotensin II receptor
antagonist which acts to decerease BP.
Impaired contractility means the heart
doesnt beat strong enough to circulate
blood (NCP Gulanick/Myers p39/Davis
Drug Guide online).
Outcome criteria
met.
Lasix is a loop diuretic. It initiates dieresis
Outcome criteria
(excretion of fluids) which decreases
met.
preload and therefore decreases BP. An
increased BP increases afterload and cardiac
workload especially for the left ventricle. If
the left ventricle does not pump effectively,
it will result in decreased CO. Keeping BP
and fluid status within an acceptable range
decreases afterload and improves CO.
Impaired contractility means the heart
doesnt beat strong enough to circulate
blood thoroughly. Increased afterload
(FVE) places even more pressure on the left
ventricle to pump blood (NCP
Gulanick/Myers p39/Davis Drug Guide
online).
11.
12.
Pts O2 sat will remain at or
above 92% when assessed
q4h
Dependent/Collaborate:
Pts heart will not show
significant changes on an
echocardiogram as ordered by
MD
Dependent/Collaborate:
Obtain MD order for O2
3LPM NC
Obtain MD order for an
echocardiogram to
monitor for changes in
heart structure
Since this pt has pneumonia and COPD,
they are at risk for respiratory distress and
decreased oxygen consumption. This pt also
has CHF which means the heart is not
working/pumping as effectively as it should
be. A failing heart may not be able to
respond to increased O2 demands, so
supplemental O2 will help keep O2
saturation at least 92% (NCP
Gulanick/Myers p39).
Outcome criteria
met.
An echocardiogram allows assessment of
size/shape of the heart, the hearts pumping
strength, valve regurgitation or stenosis, and
how the heart moves. This pt has a dx of
CHF and has had aortic valve replacement.
One echo was performed and results
showed left ventricular hypertrophy. This
thickening of the left ventricle can
eventually lead to weakness, and also
decreased CO from impaired contractility.
By monitoring for worsening changes,
further intervention can be performed
(heart.org/mayoclinic.com)
Unmet. Pt only had
one echo on file.
13.
14.
Pts BUN will remain
between 7-21mg/dL and
creatinine 0.6-1.3mg/dL when
resulted from labs ordered by
MD
Dependent/Monitor:
Pts BNP will be <100 when
resulted from labs as ordered
by MD
Dependent/Monitor:
Monitor kidney function
(BUN and creatinine)
labs as ordered by MD
Monitor BNP labs as
ordered by MD
An extensive amount of blood from the
heart gets pumped to the kidneys. If the
kidneys are not receiving adequate blood
flow to be perfused, they will not function
properly. If the kidneys are not functioning
properly, this may lead to excess fluid in the
body. Excess fluid then increases preload
and afterload which increases workload of
the heart. This can weaken the left ventricle
and compromise CO. Since this pt has ARF
and CHF, monitoring kidney function is
essential to assess for adequate renal
perfusion and also adequate fluid status
(NCP Gulanick/Myers p38/class notes).
Unmet. Pts BUN
and creatinine were
both elevated.
BNP is elevated with increasing filling
pressure (preload) and volume in the left
ventricle. An increased BNP indicates FVE
which is a clinical manifestation of CHF.
This pt was dx with CHF and had a BNP of
1840. After heart failure is diagnosed, BNP
is monitored to assess the effects of therapy.
Since this pt is receiving meds that increase
CO and decrease s/s of CHF, BNP should
be monitored to evaluate effectiveness of
treatment and fluid status. FVE increases
the workload of the heart d/t increased
afterload. Continuous stress on the left
ventricle will cause hypertrophy and
therefore impaired contractility (NCP
Gulanick/Myers p38/Lab tests and
Diagnostic Procedures).
Unmet. Pts most
recent BNP was
731 (but this was
significantly lower
than previous
draws).
15.
Pt and family will verbalize
understanding of meds and
their purpose by discharge
Teach:
Teach pt and family
about meds and their
purpose upon admission
By teaching the pt and family about the
medication regime, it provides them with
reasoning and understanding of meds. If the
pt and family understand why the meds are
prescribed, they will be more likely to
comply and perform the care needed for the
diagnosis. Since this pt has AFIB, CHF,
CAD, AAA, HTN, and
hypercholesterolemia, they have an
extensive cardiac hx and need to comply
with med to keep their health under control.
This will also improve CO by controlling
underlying problems (NCP Gulanick/Myers
p40).
Unmet. Pt was
discharged before
verbalizing
understanding. Pt
went to another
skilled nursing
facility where
teaching should
resume.
Вам также может понравиться
- Decreased Cardiac Output RM 7Документ9 страницDecreased Cardiac Output RM 7api-283470660Оценок пока нет
- Is The Most Common Extracranial Solid Tumor of InfancyДокумент7 страницIs The Most Common Extracranial Solid Tumor of InfancyEdamarie ChuaОценок пока нет
- NCPДокумент3 страницыNCPJanie StubbertОценок пока нет
- Welcome To The Case Study Presentation:-: Prostate CancerДокумент22 страницыWelcome To The Case Study Presentation:-: Prostate CancerDengo ChapatieeОценок пока нет
- NCP PTBДокумент9 страницNCP PTBecbarticanОценок пока нет
- 3M CVP Monitoring - Assisting in BMA ECG Interpretation - Final Draft - 3CДокумент65 страниц3M CVP Monitoring - Assisting in BMA ECG Interpretation - Final Draft - 3CAlexa GoteraОценок пока нет
- Nursing Care Plan For Heart Failure ChronicДокумент26 страницNursing Care Plan For Heart Failure ChronicbrantОценок пока нет
- ACTIVITY 1: Nursing Care PlanДокумент4 страницыACTIVITY 1: Nursing Care PlanChelsea JardelezaОценок пока нет
- Nursing Care PlanДокумент2 страницыNursing Care PlanAl RizkyОценок пока нет
- Assessment Diagnosis Planning Implementation Rationale EvaluationДокумент14 страницAssessment Diagnosis Planning Implementation Rationale EvaluationJennifer ArdeОценок пока нет
- Which It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToДокумент8 страницWhich It Is A Process Whereby Pancreatic Enzymes Destroy Its Own Tissue Leading ToAriane-Gay Cristobal DuranОценок пока нет
- NCP Acute Pain NCSДокумент3 страницыNCP Acute Pain NCSPaolo Vittorio Perdigueros GonzalesОценок пока нет
- Case 1 - Pneumonia (Final)Документ4 страницыCase 1 - Pneumonia (Final)Joegie ArioОценок пока нет
- Heart FailureДокумент4 страницыHeart FailureDane WrightОценок пока нет
- Cardiogenic ShockДокумент3 страницыCardiogenic Shockmerin sunilОценок пока нет
- Abdominal Aortic AneurysmДокумент2 страницыAbdominal Aortic AneurysmAria MontgomeryОценок пока нет
- Acetaminophen ToxicityДокумент14 страницAcetaminophen ToxicityJam MajОценок пока нет
- Assessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermДокумент4 страницыAssessment Diagnosis Scientific Explanation Objective Interventions Rationale Expected Outcome Short Term: Short TermGensen Cu RoxasОценок пока нет
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Документ9 страницNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel0% (1)
- Case No 45: of Intermittent Abdominal Pain Abdominal Bloating and Nausea and Vomiting (NVДокумент17 страницCase No 45: of Intermittent Abdominal Pain Abdominal Bloating and Nausea and Vomiting (NVPremiums of the RoseОценок пока нет
- Nursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveДокумент2 страницыNursing Care Plan Cues Nursing Diagnosis Objective Intervention Rationale Evaluation SubjectiveFreisanChenMandumotanОценок пока нет
- Case Study JatДокумент45 страницCase Study JatHSEINОценок пока нет
- Nursing Care PlanДокумент19 страницNursing Care PlanChic Dian UsmanОценок пока нет
- Case Stydy Angina PectorisДокумент46 страницCase Stydy Angina PectorissharenОценок пока нет
- Acute and Chronic Pancreatitis ShirleyДокумент6 страницAcute and Chronic Pancreatitis ShirleyVictor AladejanaОценок пока нет
- Diabetic Ketoacidosis Acute Management: A State of Absolute Insulin BankruptcyДокумент24 страницыDiabetic Ketoacidosis Acute Management: A State of Absolute Insulin BankruptcyGwEn LimОценок пока нет
- Discharge Plan EndoДокумент3 страницыDischarge Plan EndoCharlayne AnneОценок пока нет
- Impaired Tissue PerfusionДокумент2 страницыImpaired Tissue PerfusionLyka Mae Imbat - PacnisОценок пока нет
- CP-Rheumatic Heart Disease LandscapeДокумент13 страницCP-Rheumatic Heart Disease Landscapedecebelle alabaОценок пока нет
- Angina PectorisДокумент33 страницыAngina PectorisRosse Del MundoОценок пока нет
- Imbalanced NutritionДокумент3 страницыImbalanced NutritionIlisa ParilОценок пока нет
- Happ Lab 1Документ5 страницHapp Lab 1Jerwin TullaoОценок пока нет
- NCP CHF Er SettingДокумент9 страницNCP CHF Er SettingroseasОценок пока нет
- Ngo 2bsn1 Ncm109 Prelim NCPДокумент7 страницNgo 2bsn1 Ncm109 Prelim NCPAMIEL SIMON NGOОценок пока нет
- Assessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationДокумент6 страницAssessment Nsg. Diagnosis Sci. Explanation Planning Intervention Rationale EvaluationRoMarie AbainzaОценок пока нет
- Angina PectorisДокумент17 страницAngina PectorisRacel HernandezОценок пока нет
- Assessment: Nursing Diagnosis Planning Nursing Interventions Rationale Nursing Care Plan For HypertensionДокумент3 страницыAssessment: Nursing Diagnosis Planning Nursing Interventions Rationale Nursing Care Plan For HypertensionDelaine Mae MierОценок пока нет
- Nursing Management of Patient With Pericardial EffusionДокумент2 страницыNursing Management of Patient With Pericardial EffusionAgung Alber0% (3)
- Concept Map - Abby !Документ2 страницыConcept Map - Abby !Abegail Abaygar100% (3)
- Ineffective Airway Clearance CareplanДокумент6 страницIneffective Airway Clearance CareplanderreshaОценок пока нет
- Ineffective Cerebral Tissue Perfusion Related ToДокумент7 страницIneffective Cerebral Tissue Perfusion Related TohannahОценок пока нет
- Pneumonia and BronchiolitisДокумент48 страницPneumonia and Bronchiolitisshashank panwarОценок пока нет
- NCP of CavДокумент3 страницыNCP of CavHenry Roque TagalagОценок пока нет
- Levemir Product Insert PDFДокумент11 страницLevemir Product Insert PDFDegee O. GonzalesОценок пока нет
- Tetralogy of FallotДокумент5 страницTetralogy of FallotCharity OaniaОценок пока нет
- Propranolol, Prophylactic Warfarin, Low Molecular Weight Heparin (LMWH), Furosemide, AntibioticsДокумент8 страницPropranolol, Prophylactic Warfarin, Low Molecular Weight Heparin (LMWH), Furosemide, AntibioticsArlyn MarcelinoОценок пока нет
- NCP PainДокумент2 страницыNCP PainApril_Ivy_Raga_3835Оценок пока нет
- Nursing Care Plan Renal FailureДокумент18 страницNursing Care Plan Renal FailureKundan KumarОценок пока нет
- 403 Full PDFДокумент10 страниц403 Full PDFKuroto YoshikiОценок пока нет
- Gastrointestinal Bleeding: Prepared By: DR Gloria Lyimo Facilitated By: DR MbeleДокумент43 страницыGastrointestinal Bleeding: Prepared By: DR Gloria Lyimo Facilitated By: DR MbeleSamar AhmadОценок пока нет
- Nursing Care Plan FinalДокумент16 страницNursing Care Plan FinalErickson OcialОценок пока нет
- 2 Acute Myocardial InfarctionДокумент15 страниц2 Acute Myocardial InfarctionpauchanmnlОценок пока нет
- Management For Acute Lymphocytic LeukemiaДокумент3 страницыManagement For Acute Lymphocytic LeukemiamarivohОценок пока нет
- Nursing DiagnosisДокумент9 страницNursing Diagnosiskhikmatul mu'jizahОценок пока нет
- Code Green Introduction Reviewer - RedДокумент4 страницыCode Green Introduction Reviewer - RedJamieОценок пока нет
- GBS Nursing MangementДокумент21 страницаGBS Nursing MangementJoseph Namita SunnyОценок пока нет
- Jake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersДокумент8 страницJake Yvan Dizon Case Study, Chapter 49, Assessment and Management of Patients With Hepatic DisordersJake Yvan DizonОценок пока нет
- Course in The WardДокумент1 страницаCourse in The WardGeevee Naganag VentulaОценок пока нет
- Management of Tuberculosis: A guide for clinicians (eBook edition)От EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Оценок пока нет
- Risk For Decreased Cardiac OutputДокумент4 страницыRisk For Decreased Cardiac Outputapi-283482759Оценок пока нет
- Hearty Welcome To The Physician Assistant Session'Документ8 страницHearty Welcome To The Physician Assistant Session'Rushi PatelОценок пока нет
- Finite Element and Mechanobiological Modelling of Vascular DevicesДокумент166 страницFinite Element and Mechanobiological Modelling of Vascular DevicesASHISH AGARWALОценок пока нет
- Cardiovascular Disorders 1Документ44 страницыCardiovascular Disorders 1Nader Smadi100% (1)
- PDF Passive Leg Raise PLR Test Stroke Volume Index SviДокумент3 страницыPDF Passive Leg Raise PLR Test Stroke Volume Index SviNama ManaОценок пока нет
- Venous Intervention - GSV Ablation FINALДокумент43 страницыVenous Intervention - GSV Ablation FINALaaaaaaОценок пока нет
- Cardiac AssessmentДокумент48 страницCardiac AssessmentRatheesh NathОценок пока нет
- Congenital Heart Disease (CHD) : Kussia Ayano (MD)Документ54 страницыCongenital Heart Disease (CHD) : Kussia Ayano (MD)Yemata HailuОценок пока нет
- Komplikasi Pada Pasien Infark Miokard Akut ST-Elevasi (STEMI) Yang Mendapat Maupun Tidak Mendapat Terapi Reperfu..Документ13 страницKomplikasi Pada Pasien Infark Miokard Akut ST-Elevasi (STEMI) Yang Mendapat Maupun Tidak Mendapat Terapi Reperfu..aris hidayatul mОценок пока нет
- Should Norepinephrine, Rather Than PhenylephrineДокумент8 страницShould Norepinephrine, Rather Than PhenylephrineDiego Andres Rojas TejadaОценок пока нет
- Cvs PBLДокумент2 страницыCvs PBLYan RuОценок пока нет
- CRT Exam Test QuestionsДокумент4 страницыCRT Exam Test QuestionsDharlyn MungcalОценок пока нет
- Ghid ERHA Privitor NOAK 2018 PDFДокумент64 страницыGhid ERHA Privitor NOAK 2018 PDFSolaris CorbutОценок пока нет
- 13 BДокумент38 страниц13 BBruno100% (4)
- 1 s2.0 S2174204919302636 MainДокумент13 страниц1 s2.0 S2174204919302636 MainSara ArévaloCОценок пока нет
- Coronary CirculationДокумент47 страницCoronary CirculationSuresh KumarОценок пока нет
- Sotalol HydrochlorideДокумент2 страницыSotalol HydrochlorideLIEZEL GRACE VELAYOОценок пока нет
- Diagnostic Angiography SOPДокумент2 страницыDiagnostic Angiography SOPQuality Assurance DepartmentОценок пока нет
- Cardiorespiratory Adaptations To TrainingДокумент7 страницCardiorespiratory Adaptations To TrainingMozil Fadzil KamarudinОценок пока нет
- Week 2 Circulatory SystemДокумент7 страницWeek 2 Circulatory SystemCarl Brian L. MonteverdeОценок пока нет
- Vital SignsДокумент94 страницыVital Signsglennm68100% (5)
- A. Anti-Arrhythmic B.tech 5th SemДокумент49 страницA. Anti-Arrhythmic B.tech 5th SemNitesh SinghОценок пока нет
- Fetal CirculationДокумент2 страницыFetal CirculationEric Gato100% (3)
- ASSESSMENT OF THORAX, LUNGS, Heart Neck Vessels, Breast, Lymphatic, Peripheral Vascular SystemДокумент33 страницыASSESSMENT OF THORAX, LUNGS, Heart Neck Vessels, Breast, Lymphatic, Peripheral Vascular Systemandramercadejas730Оценок пока нет
- KARDIOLOGIДокумент120 страницKARDIOLOGIEsti IvanaОценок пока нет
- Spontaneous Coronary Artery Dissection With Clinical Presentation of Acute Myocardial InfarctionДокумент3 страницыSpontaneous Coronary Artery Dissection With Clinical Presentation of Acute Myocardial InfarctionSabrina JonesОценок пока нет
- Cardiopulmonary NPTE Questions FlashcardsДокумент61 страницаCardiopulmonary NPTE Questions Flashcardsdina sharaf100% (4)
- Cp201012 Learning Light-395Документ2 страницыCp201012 Learning Light-395jyothiОценок пока нет
- Congenital Heart Defect-VsdДокумент53 страницыCongenital Heart Defect-VsdAuni Akif AleesaОценок пока нет
- DefibrilationДокумент23 страницыDefibrilationShanmugam MurugesanОценок пока нет
- Endovascular Aortic Repair Current Techniques With Fenestrated, Branched and Parallel Stent-GraftsДокумент747 страницEndovascular Aortic Repair Current Techniques With Fenestrated, Branched and Parallel Stent-GraftsFrancisco Álvarez Marcos80% (5)