Академический Документы
Профессиональный Документы
Культура Документы
The Respiratory System
Загружено:
annelle02190 оценок0% нашли этот документ полезным (0 голосов)
5 просмотров25 страницNotes for the respiratory system for anatomy
Авторское право
© © All Rights Reserved
Доступные форматы
PPTX, PDF или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документNotes for the respiratory system for anatomy
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF или читайте онлайн в Scribd
0 оценок0% нашли этот документ полезным (0 голосов)
5 просмотров25 страницThe Respiratory System
Загружено:
annelle0219Notes for the respiratory system for anatomy
Авторское право:
© All Rights Reserved
Доступные форматы
Скачайте в формате PPTX, PDF или читайте онлайн в Scribd
Вы находитесь на странице: 1из 25
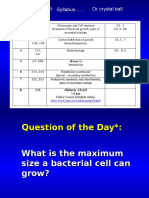
The Respiratory System II (Chapter 22)
Lecture # 9: Gas Exchange and
Transport
Objectives
1-Define partial pressure and discuss
its relationships to a gas mixture such
as air.
2- Discuss how partial pressure affects
gas transport by blood.
3- Describe the mechanism of
transporting O, and CO,
4- Describe the factors that govern
gas exchange in the lungs and
systemic capillaries.
Partial Pressure and Gas Exchange
Air is a mixture of gases. It contains :78.6 % nitrogen, 20.9% oxygen,
0.04% carbon dioxide, 0 - 4% water vapor depending on temperature
and humidity, and minor gases argon, neon, helium, methane and ozone.
These individual gases contribute to the atmospheric pressure, and the
sum of all contributions results in the atmospheric pressure = 760 mm
Hg (Dalton’s law).
Partial Pressureit is the separate contribution of each gas to the total
pressure in a mixture.
The partial pressure of a gas is directly proportional to the concentra-
tion of this gas in the mixture.
Example: The higher partial pressure in the air correspond to Nitrogen,
which is the most concentrated gas.
The partial pressure is symbolized with a P followed by the formula of
the gas:
Partial pressure of Nitrogen = Py, partial pressure of Oxygen= Poo
The partial pressure of a gas in the air is equal to the
concentration of this gas (%) X the atmospheric pressure:
PN,= 78.6% x 760 mm Hg = 597 mm Hg
PO, = 20.9% x 760 mm Hg = 159 mm Hg
PH,O= 0.5% x 760 mm Hg = 3.7 mm Hg
PCO, = 0.04% x 760 mm Hg = 0.3 mm Hg
PN, + PO, +PH,O + PCO, = 760 mmHg
The composition of inspired air and alveolar is different because of three
influences:
1- Air is humidifies by contact with mucous membranes. Alveolar PH,O is more
than 10 times higher than inhaled air.
2- Freshly inspired air mixes with residual air left from the previous respiratory
cycle. Oxygen is diluted and it is enriched with CO,
3- Alveolar air exchanges O, and CO, with the blood. PO, of alveolar air is
about 65% that of inspired air; PCO, is more than 130 times higher.
oT uno K}
Cuil) a Re Nol ae
aN] yee
Inspired Air* Alveolar Air
786% 597 mmHg 749% 569mm Hg
20.9% 159mm Hg 137% — 104mmHg
HO 05% = 3:7mmHg 62% 47 mmHg
co, 0.04% —03mmHg 53% 40 mmHg
Total 100% 760 mmHg 100% 760mm Hg
“Typical values for a cool cloar day; values vary with tomporature and
humidity, Other gases present in small amounts are disregarded.
Factors that Affect the Efficiency of
Alveolar Gas Exchange
1- Partial pressure of gases
(O, and CO,)
2- Solubility of gases in blood
(Oz and CO,) Henry's law
3- Thickness of the respiratory
membrane
4- Surface area of the respi-
ratory membrane
5- Ventilation-Perfusion
coupling
concentration
Asolution consists of particles of mater called solute mixed with
amore abundant substance (usually water) called the solvent.
Concentration Gradientit is the difference between the high
and low concentration areas.
The tendency of ions and molecules in a concentration
gradients is to move from the region of higher concentration
to the region of lower concentration.
Diffusion: It is the net movement of ions or molecules from
the region of higher concentration to the region of lower
concentration (down the concentration gradient).
Diffusion tends to eliminate the concentration gradient.
1- Partial pressure of gases (O, and CO,)
In the same way that molecules and ions in solution diffuse
from the region of higher concentration to the region of
lower concentration (down the concentration gradient),
each gas in a mixture diffuses down its own pressure
gradient.
Gases diffuse down their own concentration gradient until
the partial pressure of each gas in the air is equal to its
partial pressure in water.
Unopened Pressure Atnew equilibrium — Opened
soda can (b) soda can
Gases diffuse down their own concentration gradient until
the partial pressure of each gas in the air is equal to its
partial pressure in water.
The Po, of alveolar air is The Pcoz of the arriving blood is
initially higher than the Po, of initially higher than the Pco, of
the blood arriving at an alveolar air.
alveolus.
Equilibrium state Initial stato Equilibrium stato
(0) Oxygen
O, diffuses into the blood until
the two are in equilibrium.
(©) Carbon dioxide
CO, diffuses into the alveolus
until the two are in equilibrium.
It takes about 0.25 seconds
for both gases to reach the
equilibrium.
2- Solubility of gases in blood (O, and CO,)
In addition to the partial pressure, the solubility of gases
also affects the alveolar gas exchange.
Henry’s law: At the air-water interface, for a given
temperature, the amount of gas that dissolves in the water is
determined by its solubility in water and its partial
pressure in air.
CO, is much more
soluble than O,
therefore diffuses
more rapidly.
Pressure gradient
Alveolar air ' ; O,: 104 - 40 = 64 mm Hg
Pop 104mm Hg “C02: 46-40 = 6 mmHg
Pco2 40 mm Hg
Even though the pressure
gradient of O, (64 mm Hg)
is much higher than that of
CO, (6 mm Hg) , equal
amounts of O, and CO, are
exchanged across _ the
respiratory membrane
because CO, is much more
soluble and diffuses more
rapidly.
Equal amounts of O, and CO, are exchanged across the respiratory
membrane.
In addition to the partial pressure, the solubility of gases also affects the
alveolar gas exchange.
Henry’s law: At the air-water interface, for a given temperature, the amount of
gas that dissolves in the water is determined by its solubility in water and its
partial pressure in air.
CO, is 20 times as soluble in water as O,. Therefore, CO, diffuses more
rapidly.
Even though the pressure gradient of O, (64 mm Hg) is much higher than that of
CO, (6 mm Hg) , equal amounts of O, and CO, are exchanged across the
respiratory membrane because CO, is much more soluble and diffuses more
rapidly.
Deoxygenated Blood Alveolar air Pressure gradient
Po. 40 mm Hg Po: 104mmHg 104 - 40 = 64 mm Hg
Poon 46 mm Hg Peo 40mmHg = 46- 40= 6 mmHg
a so
Po, 104 mm Hg
= Po,40 mm Hg
cOvuntoa Peo. mn Hg Peo, 40 mm Hg
3- Thickness of the respiratory membrane
It is only 0.5 um thick, Thus, it presents little
obstacle to diffusion.
Pulmonary edema in left side ventricular failure
causes edema and thickening of the respiratory
membrane.
Pneumonia causes thickening of the respiratory
membrane.
Under these conditions, the gases have farther to
travel between blood and air and cannot equilibrate
fast enough to keep up with blood flow.
4- Surface area of the respiratory
membrane
In good health, each lung has about 70m? of
respiratory membrane available for gas exchange.
Emphysema, lung cancer, and tuberculosis decrease
surface area for gas exchange.
{el Emphysema
5- Ventilation-Perfusion Coupling
It is the ability to match ventilation and perfusion to each
other.
Gas exchange requires not only good ventilation to
alveolus, but also good perfusion of its capillaries.
Perfusion is the blood flow per given volume or mass of
tissue.
1- Ventilation Controls Perfusion through PO,
2- Perfusion Controls Ventilation through CO,
1- Ventilation Controls Perfusion
Reduced ventilation causes local constriction of the pulmonary arteries, reducing blood
flow to that area and redirecting this blood to better-ventilated alveoli
Good ventilation, by contrast, dilates the arteries and increases perfusion so that most
blood is directed to regions of the lungs where it can pick up the most oxygen.
aaa
Reduced Po: in Decreased Increased Elevated Po; in
blood vessels airflow airflow blood vessels.
Response
toincreased
ventilation
Vasoconstriction of \Vasodilation of
pulmonary vessels pulmonary vessels
Decreased Increased
blood flow blood flow
(a) Perfusion adjusted to changes
In ventilation
2- Perfusion Controls Ventilation
Ventilation is also adjustable. Poor ventilation causes local CO, accumulation, which
stimulates local bronchodilation and improves air flow. Low PCO, causes local
bronchoconstriction.
Decreased Increased
Reduced Pco, Elevated PCO,
inalveott De Boos Gos) inalveoli
Constrietion of Dilation of
bronchioles bronchioles
Decreased Increased
airflow airflow
(b) Ventilation adjusted to changes in perfusion
Gas Transport
Gas transport is the process of carrying gases from the
alveoli to the systemic tissues and vise versa.
1- Oxygen transport
About 98.5% of Oxygen is carried bound to hemoglobin, and 1.5%
dissolved in plasma.
Deoxyhemoglobin (HHb) + Oxygen >> Oxyhemogiobin (HbO,) + H*
2- Carbon dioxide transport ‘
Carbon dioxide is transported in three forms: 70% as bicarbonate ion,
23% bound to hemoglobin, 7% dissolved in plasma.
co, + #0 [o> H,cO, [=> Hco, +
(70%)
Hemoglobin (Hb) + Carbon dioxide "> Carbaminohemoglobin (HbCO,)
(23%)
The remaining 7% of the CO2 is carried in the blood as dissolved gas, like
CO2 in carbonated beverages.
Alveolar Gas Exchange
It is the unloading of CO, and
loading of O, at the pulmonary
capillaries.
a) O, loading
b) CO, unloading
Systemic Gas Exchange
It is the unloading of O, and
loading of CO, at the systemic
capillaries.
a) O, unloading
b) CO, loading
Alveolar Gas
Exchange
It is the unloading of
CO, and loading of O,
at the pulmonary
capillaries.
a) O, loading
1- O, from alveolar air diffuses to the plasma and travels as dissolved gas
(1.5% of O,)
2- O, from alveolar air diffuses to the plasma and binds to the Deoxy-
hemoglobin (98.5% of O,)
As Hb loads O, its affinity for H* decreases, H* dissociates from Hb. Those H*
will bind to HCO ; to help in CO, unloading
Deoxyhemoglobin + O, Oxyhemoglobin (HbO,) + H*
(HHb) (from alveolar air) (98.5% of O,)
b) CO, unloading
41- Unloading of CO, carried by HCO," (70% of CO.)
HCO, +H* » H,CO, co, + 4H,0
(70% of CO,) (to alveolar air)
Previous reactions take place within the RBC. As HCO,7is consumed and CO,
is released, more HCO, diffuses from the plasma to the interior of the RBC and
Ct diffuses outside the RBC.
Heo, This exchange of HCO, and Cl‘is called the
Plasma chloride shift.
2- Unloading of CO, carried by Carbaminohemoglobin and other
carbamino-compounds (23% of CO.)
Carbaminohemoglobin (HbCO,) > Hemoglobin (Hb) + CO,
(to alveolar air)
3- CO, as dissolved gas (7% of CO,) diffuses from plasma to the
alveolar air.
Alveolar Gas Exchange
Systemic Gas Exchange
Systemic gas exchange is the unloading of O, and loading
of CO, at the systemic capillaries.
Oxygenated Blood Tissue fluid Pressure gradient
Po. 95mm Hg Po, 40 mm Hg 95-40=55 mmHg
Peo, 40 mm Hg Poo, 46 mm Hg 46 -40= 6mmHg
‘Systemic circuit
a) O, unloading
1- O, dissolved in plasma as gas diffuses to the tissues (1.5% of O,)
2- Unloading of O, bind to Oxyhemoglobin (98.5%)
Oxyhemoglobin (HbO,) reduces its affinity for O, due the H* released
by H,CO,
H* + Oxyhemoglobin (HbO,)
(98.5% of O,)
H,cO, [> HCO, +Ht
> Deoxyhemoglobin (HHb) +O,
(to the
tissues)
b) CO, loading
1- Loading of CO, to HCO,(70%)
co, + H,0 » H,CO, » HCO; + H*
(from tissues) Carbonic (70% of CO.)
Anhydrase
cr Chloride shift keeps reaction proceeding,
Plasma —_ exchanges HCO,; for Cl-
2- Loading of CO, to Hemoglobin (23%)
Hemoglobin (Hb) + Carbon dioxide Carbaminohemoglobin
_, (HbCO,)
(23%of CO,)
3- CO, from tissues diffuses to the plasma and travels as dissolved
gas (7% of CO.)
Systemic Gas Exchange
Coupling of CO, - O, Exchange
1- In alveolar gas exchange
Loading of O, releases H* from Deoxyhemoglobin. Those H* bind to HCO,
and help in CO, unloading.
Deoxyhemoglobin (HHb) +O, =S> Oxyhemoglobin (HbO,) +Ht
Hoo, +H* => co, H==>co, + H,0
(70% of co.) {to alveolar air)
2- In systemic gas exchange
Loading of CO, releases H* from H,CO;. Those H* reduces the affinity of
Oxyhemoglobin (HbO,) for O2 and help in O, unloading.
CO, +H,0 [=> H,co, > HCOy +H
(from tissues) carbonic anhydrase coal
H* + Oxyhemoglobin (HbO,) = Deoxyhemoglobin (HHb) +0,
(98.5% of O;) {to tissues)
Вам также может понравиться
- Parasite Diseases: An Intro to Protozoans, Helminths & EctoparasitesДокумент33 страницыParasite Diseases: An Intro to Protozoans, Helminths & Ectoparasitesannelle0219Оценок пока нет
- Microbiology Microbial GrowthДокумент77 страницMicrobiology Microbial Growthannelle0219Оценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Session 4 Diagnostic Parasitology TechniquesДокумент46 страницSession 4 Diagnostic Parasitology Techniquesannelle0219Оценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Session 3 PathogenesisДокумент18 страницSession 3 Pathogenesisannelle0219Оценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- MicrobiologyДокумент132 страницыMicrobiologyannelle0219Оценок пока нет
- Thyroid CancerДокумент1 страницаThyroid Cancerannelle0219Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Esophageal Obstruction and Equine Gastric Ulcer SyndromeДокумент30 страницEsophageal Obstruction and Equine Gastric Ulcer Syndromeannelle0219Оценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Life Cycles Reveal Parasite DiagnosisДокумент26 страницLife Cycles Reveal Parasite Diagnosisannelle0219Оценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Equine dentistry guideДокумент38 страницEquine dentistry guideannelle0219Оценок пока нет
- DO NOT Incise The Tunica AlbugineaДокумент3 страницыDO NOT Incise The Tunica Albugineaannelle0219Оценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Lecture 3 Approach To Medical Diseases of The Equine Small IntestineДокумент37 страницLecture 3 Approach To Medical Diseases of The Equine Small Intestineannelle0219Оценок пока нет
- MicrobiologyДокумент83 страницыMicrobiologyannelle0219Оценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Lecture 4 Approach To Medical Diseases of The Equine Large ColonДокумент26 страницLecture 4 Approach To Medical Diseases of The Equine Large Colonannelle0219Оценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Lecture 2 Principles of Intestinal Injury & EndotoxemiaДокумент25 страницLecture 2 Principles of Intestinal Injury & Endotoxemiaannelle0219Оценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Midwestern University - Glendale, Az ACADEMIC CALENDAR 2017-2018Документ2 страницыMidwestern University - Glendale, Az ACADEMIC CALENDAR 2017-2018annelle0219Оценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- What Is This? Syllabus or Crystal BallДокумент96 страницWhat Is This? Syllabus or Crystal Ballannelle0219Оценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Syllabus 201720 20365Документ10 страницSyllabus 201720 20365annelle0219Оценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- Microbial Ecology: Gk. Oikos "House, Dwelling Place, Habitation"Документ53 страницыMicrobial Ecology: Gk. Oikos "House, Dwelling Place, Habitation"annelle0219Оценок пока нет
- SyllabusДокумент9 страницSyllabusannelle0219Оценок пока нет
- Vet SchoolsДокумент3 страницыVet Schoolsannelle0219Оценок пока нет
- Chapter 9 Organic Chemistry NotesДокумент20 страницChapter 9 Organic Chemistry Notesannelle0219Оценок пока нет
- Chapter 13 and 14 NotesДокумент15 страницChapter 13 and 14 Notesannelle0219Оценок пока нет
- Equation SheetДокумент5 страницEquation Sheetannelle0219Оценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- SyllabusДокумент6 страницSyllabusannelle0219Оценок пока нет
- SyllabusДокумент6 страницSyllabusannelle0219Оценок пока нет
- SyllabusДокумент6 страницSyllabusannelle0219Оценок пока нет
- SyllabusДокумент5 страницSyllabusannelle0219Оценок пока нет
- Confidential Academic Evaluation Form: Page 1 of 2Документ2 страницыConfidential Academic Evaluation Form: Page 1 of 2annelle0219100% (1)
- Veterinarian'S Confidential Evaluation Form: Page 1 of 3Документ3 страницыVeterinarian'S Confidential Evaluation Form: Page 1 of 3annelle0219Оценок пока нет
- College of Veterinary Medicine University of Florida: With A Grade Letter of C or AboveДокумент1 страницаCollege of Veterinary Medicine University of Florida: With A Grade Letter of C or Aboveannelle0219Оценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)