Академический Документы
Профессиональный Документы
Культура Документы
Así Se Extrajo Un Celular Que Se Tragó Un Hombre de 29 Años en Irlanda
Загружено:
Christian Tinoco SánchezОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Así Se Extrajo Un Celular Que Se Tragó Un Hombre de 29 Años en Irlanda
Загружено:
Christian Tinoco SánchezАвторское право:
Доступные форматы
CASE REPORT OPEN ACCESS
International Journal of Surgery Case Reports 22 (2016) 8689
Contents lists available at ScienceDirect
International Journal of Surgery Case Reports
journal homepage: www.casereports.com
An ingested mobile phone in the stomach may not be amenable to safe
endoscopic removal using current therapeutic devices: A case report
Obinna Obinwa , David Cooper, James M. ORiordan
Department of Surgery, The Adelaide and Meath Hospital, Dublin Incorporating the National Childrens Hospital, Tallaght, Dublin 24, Ireland
a r t i c l e
i n f o
Article history:
Received 30 January 2016
Received in revised form 28 March 2016
Accepted 28 March 2016
Available online 1 April 2016
Keywords:
Foreign body removal
Stomach
Endoscopic devices
Mobile phone
Surgery
Case report
a b s t r a c t
INTRODUCTION: This case report is intended to inform clinicians, endoscopists, policy makers and industry
of our experience in the management of a rare case of mobile phone ingestion.
PRESENTATION OF CASE: A 29-year-old prisoner presented to the Emergency Department with vomiting,
ten hours after he claimed to have swallowed a mobile phone. Clinical examination was unremarkable.
Both initial and repeat abdominal radiographs eight hours later conrmed that the foreign body remained
in situ in the stomach and had not progressed along the gastrointestinal tract. Based on these ndings,
upper endoscopy was performed under general anaesthesia. The object could not be aligned correctly
to accommodate endoscopic removal using current retrieval devices. Following unsuccessful endoscopy,
an upper midline laparotomy was performed and the phone was delivered through an anterior gastrotomy, away from the pylorus. The patient made an uneventful recovery and underwent psychological
counselling prior to discharge.
DISCUSSION: In this case report, the use of endoscopy in the management when a conservative approach
fails is questioned. Can the current endoscopic retrieval devices be improved to limit the need for surgical
interventions in future cases?
CONCLUSION: An ingested mobile phone in the stomach may not be amenable for removal using the
current endoscopic retrieval devices. Improvements in overtubes or additional modications of existing
retrieval devices to ensure adequate alignment for removal without injuring the oesophagus are needed.
2016 The Authors. Published by Elsevier Ltd. on behalf of IJS Publishing Group Ltd. This is an open
access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/).
1. Introduction
Foreign body ingestion is a relatively common emergency problem. The majority of cases occur in the paediatric population [1,2].
Those with psychiatric disorders, developmental delay, alcohol
intoxication and prisoners are also at increased risk [36]. General clinical guidelines on diagnosis and management of ingested
foreign bodies have been published by the American Society for
Gastrointestinal Endoscopy (ASGE) [6] and more recently, by the
European Society for Gastrointestinal Endoscopy (ESGE) [7]. Specic guidelines for the management of gastric foreign bodies also
exist but are conned to common objects such as coins, magnets,
narcotic packets and disc batteries [6].
The management of a rare case of a patient who swallowed a
mobile phone with particular focus on the lessons learned from the
failed endoscopic management of the object is therefore presented
here. This manuscript is written in accordance with the CAse REport
Corresponding author.
E-mail addresses: obinnaobinwa@rcsi.ie (O. Obinwa), cooperda@tcd.ie
(D. Cooper), James.ORiordan@amnch.ie (J.M. ORiordan).
(CARE) guidelines [8]. The report is intended to inform clinicians,
endoscopists and industry on our experience in the management
of this unusual case.
2. Presentation of case
A 29-year old male prisoner was brought in by ambulance to
the Emergency Department with a four-hour history of vomiting,
having claimed to have swallowed a foreign object six hours earlier
that day. He had no other associated symptoms. Of note, he had
complex psycho-social issues.
He was haemodynamically stable. Clinical examination was
unremarkable. All laboratory investigations were normal. An erect
chest X-ray partially showed the mobile phone in the epigastrium
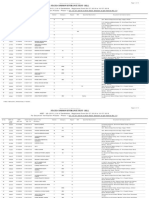
and there was no free air within the abdomen. An abdominal plain
lm revealed the complete device in the stomach (Fig. 1). The
patient was admitted and managed conservatively. He was kept nil
by mouth and commenced on intravenous uids and proton pump
inhibitors. A repeat abdominal radiograph, approximately eighteen
hours after the reported time of ingestion, showed that the mobile
phone remained in situ in the stomach and had not passed through
http://dx.doi.org/10.1016/j.ijscr.2016.03.043
2210-2612/ 2016 The Authors. Published by Elsevier Ltd. on behalf of IJS Publishing Group Ltd. This is an open access article under the CC BY-NC-ND license (http://
creativecommons.org/licenses/by-nc-nd/4.0/).
CASE REPORT OPEN ACCESS
O. Obinwa et al. / International Journal of Surgery Case Reports 22 (2016) 8689
Fig. 1. Plain lm abdomen showing the mobile phone.
the pylorus. At this time, the patient was consented for removal
under general anaesthesia (Fig. 2).
The patient was brought to the operating theatre, intubated and
the initial intervention was an upper gastrointestinal endoscopy.
The ndings are shown in Fig. 3. Following failed attempts at endoscopic removal, using endoscopic snares, graspers, tripod forceps
and baskets, the endoscopic approach was abandoned. The mobile
phone could not be aligned correctly to allow for a safe retrieval
while limiting the potential harm to the oesophagus. The use of
overtube was not an option in this case due to the size of the
phone. An upper midline laparotomy was then performed and an
Alexis O Wound Protector was used to protect the wound. A gastrotomy (34 cm) was made in the anterior stomach away from
the pylorus. The phone was delivered through the gastrotomy by
manual manipulation assisted by Babcock forceps. The dimensions
of the foreign body were 68 23 11 mm. This was followed by a
two-layer gastrotomy closure, fascial and skin closure. A nasogastric tube was placed during the surgery and secured with a bridle.
The mobile phone was sent as a specimen for forensic examination.
Postoperatively, the patient received analgesia, two further
doses of antibiotics, and was kept nil by mouth for three days. He
received intravenous uids and proton pump inhibitors during the
period of fasting. The nasogastric tube remained in situ for a further
three days. He also received chest physiotherapy and was seen by
the psychiatrist before discharge. He passed a bowel motion on the
6th postoperative day and was discharged well on the 7th postoperative day. He was reviewed in the out-patient clinic four months
later. He was well with no symptoms at this point.
3. Discussion
Surgery (laparotomy or laparoscopy) is required in less than
1% of cases of foreign body ingestion as most will resolve with
87
conservative management or require endoscopy in approximately
1020% of cases [7].
Consenting the patient for laparotomy before the patient was
anaesthetised was considered to be an important learning point,
given the limitation of endoscopy in this case. This approach helped
to limit the dilemma of waking up the patient again to discuss
surgery or the pressurized attempt at taking out a maligned object
endoscopically with potential risks of injury to the oesophagus.
Similarly, if the intervention were to be carried out by a gastroenterologist under anaesthesia, we would recommend that the on-call
surgeon should be consulted before the patient is anaesthetized and
the surgeon should be in-house in case a surgical intervention is
required. Further, the site of incision, wound protection technique,
and outlined postoperative care limited the morbidities in this case.
Additional modern perspectives in the management also include
the psychological evaluation before discharge. As the patient was a
prisoner, the mobile phone had to be sent as a specimen for forensic
examination.
The failure of endoscopy to remove the mobile phone, in this
case, highlights the limitations of this approach. The traditional
sequence of conservative approach, endoscopy and surgery when
endoscopy fails is challenged. This observation has raised a new
question: should clinicians proceed directly to surgery when clinical observation fails in these cases or should endoscopy still be
attempted? The potential benet of endoscopy is that it may be
used as a minimally invasive bridge to surgery in cases of failed
conservative management. There were no specic guidelines in
the management of this case [6,7]. The object size described here
was within the upper limit of what would have also been considered for conservative management in prisoners [9]. The presence
of continued symptoms and failure to progress within 18 h of
conservative management were indications for proceeding with
endoscopic removal under general anaesthesia. In this case report,
upper GI Endoscopy also helped to conrm the diagnosis as well as
the objects failure to progress along the gastrointestinal tract.
Besides these clinical management pearls, there are also other
aspects of the endoscopic management of this patient which affect
industry and policy makers. Our experience in this case was that an
overtube was not an option due to the size of the object and we also
could not nd any other suitable retrieval devices that ensured correct alignment for endoscopic removal of the mobile phone through
the oesophagogastric junction. Needed now is the development
of self-expandable overtubes that can accommodate such objects
without risk of damaging the oesophagus. The alternative is for
industry to create or improve on existing retrieval devices to ensure
adequate alignment for removal as shown in Fig. 4. Such improvement, ideally should be tested in-vitro before being considered in
human subjects. Successful endoscopic removal of a foreign object
obviates the need for surgery and associated morbidity. There are
also potential health savings in terms of reduced length of stay and
health costs if surgery could be avoided.
Finally, unlike most other cases of foreign body ingestion, the
specic case of ingestion of mobile phone is underreported in
the literature. The only case report of mobile phone ingestion
which we could nd in PUBMED database was that of a 35year old intoxicated male with pharyngeal impaction by a mobile
phone who had the phone endoscopically removed under a general anaesthesia [10]. A few other anecdotal reports of mobile
phones lodged in the stomach exist in non-scientic literature,
but the current management, or quality improvement issues are
not entirely described. Besides detailing the full management of
such an under-reported case, we have described how our ndings
might affect clinicians, industry and policy makers.
CASE REPORT OPEN ACCESS
88
O. Obinwa et al. / International Journal of Surgery Case Reports 22 (2016) 8689
Fig. 2. Timeline.
4. Conclusion
An ingested mobile phone in the stomach may not be amenable
for safe removal using the current endoscopic retrieval devices.
Therefore we recommend that all patients undergoing endoscopic
removal of a mobile phone should be consented for a laparotomy.
As well as this, there is need for the development of self-expandable
overtubes or additional improvement on existing retrieval devices
to ensure adequate alignment for removal without risks of damage
to the oesophagus.
Ethical approval
An ethical approval was not required.
Consent
Written informed consent was obtained from the patient for
publication of this case report and accompanying images. A copy
of the written consent is available for review by the Editor-in-Chief
of this journal on request.
Submission declaration
Conict of interest
The authors have no conicts of interest to disclose.
Funding
The authors have no extra or intra-institutional funding to
declare.
The authors declare: that the work described has not been published previously, that it is not under consideration for publication
elsewhere, that its publication is approved by all authors and tacitly or explicitly by the responsible authorities where the work was
carried out, and that, if accepted, it will not be published elsewhere
including electronically in the same form, in English or in any other
language, without the written consent of the copyright holder.
CASE REPORT OPEN ACCESS
O. Obinwa et al. / International Journal of Surgery Case Reports 22 (2016) 8689
89
Author contributors
O.O. and D.C. contributed equally in this case report. O.O. and
D.C. conceived the initial idea of the study. J.O.R., O.O., and D.C.
acquired the data for publication. O.O. and D.C. drafted the article,
and all authors revised it critically for important intellectual content. All authors approved the nal version of the manuscript to be
submitted.
Guarantor
Mr James ORiordan, Consultant General and Colorectal Surgeon,
Adelaide and Meath Hospital, Incorporating the National Childrens
Hospital, Tallaght, Dublin 24, Ireland.
References
Fig. 3. Gastroscopy showing the mobile phonein the stomach.
[1] W. Cheng, P.K. Tam, Foreign-body ingestion in children: experience with 1265
cases, J. Pediatr. Surg. 34 (1999) 14721476.
[2] E. Panieri, D.H. Bass, The management of ingested foreign bodies in
childrena review of 663 cases, Eur. J. Emerg. Med. 2 (1995) 8387.
[3] R. Palta, A. Sahota, A. Bemarki, P. Salama, N. Simpson, L. Laine, Foreign-body
ingestion: characteristics and outcomes in a lower socioeconomic population
with predominantly intentional ingestion, Gastrointest. Endosc. 69 (2009)
426433.
[4] S.T. Weiland, M.J. Schurr, Conservative management of ingested foreign
bodies, J. Gastrointest. Surg. 6 (2002) 496500.
[5] K.E. Blaho, K.S. Merigian, S.L. Winbery, L.J. Park, M. Cockrell, Foreign body
ingestions in the Emergency Department: case reports and review of
treatment, J. Emerg. Med. 16 (1998) 2126.
[6] S.O. Ikenberry, T.L. Jue, M.A. Anderson, V. Appalaneni, S. Banerjee, T.
Ben-Menachem, et al., Management of ingested foreign bodies and food
impactions, Gastrointest. Endosc. 73 (2011) 10851091.
[7] M. Birk, P. Bauerfeind, P.H. Deprez, M. Hafner, D. Hartmann, C. Hassan, et al.,
Removal of foreign bodies in the upper gastrointestinal tract in adults:
European Society of Gastrointestinal Endoscopy (ESGE) Clinical Guideline,
Endoscopy 48 (2016) 18.
[8] J.J. Gagnier, G. Kienle, D.G. Altman, D. Moher, H. Sox, D. Riley, The CARE
guidelines: consensus-based clinical case report guideline development, J.
Clin. Epidemiol. 67 (2014) 4651.
[9] Y. Ribas, D. Ruiz-Luna, M. Garrido, J. Bargallo, F. Campillo, Ingested foreign
bodies: do we need a specic approach when treating inmates, Am. Surg. 80
(2014) 131137.
[10] M.M. Ali, K. Bahl, M. Dross, S. Farooqui, P. Dross, Accidental cell phone
ingestion with pharyngeal impaction, Del. Med. J. 86 (2014) 277279.
Fig. 4. Ideal endoscopic alignment for safe removal.
Open Access
This article is published Open Access at sciencedirect.com. It is distributed under the IJSCR Supplemental terms and conditions, which
permits unrestricted non commercial use, distribution, and reproduction in any medium, provided the original authors and source are
credited.
Вам также может понравиться
- Los Empleadores Más Atractivos Del Mundo en 2017Документ26 страницLos Empleadores Más Atractivos Del Mundo en 2017Christian Tinoco SánchezОценок пока нет
- Ufo Highlights Guide 2013Документ12 страницUfo Highlights Guide 2013NRCОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Mocion Presentada en El Congreso Donde Se Solicita La Vacancia Del Presidente PPKДокумент4 страницыMocion Presentada en El Congreso Donde Se Solicita La Vacancia Del Presidente PPKChristian Tinoco SánchezОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- GPI 2017 Report 1Документ140 страницGPI 2017 Report 1Montevideo PortalОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Índice de Paz Mundial 2013Документ106 страницÍndice de Paz Mundial 2013Christian Tinoco SánchezОценок пока нет
- Worlds Healthiest CountriesДокумент5 страницWorlds Healthiest CountriesMD PraxОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Social Progress Index 2016Документ147 страницSocial Progress Index 2016Christian Tinoco Sánchez100% (1)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Full Report Energy Trilemma Index 2016Документ147 страницFull Report Energy Trilemma Index 2016Christian Tinoco SánchezОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Peligros de La Percepción 2016Документ30 страницPeligros de La Percepción 2016Christian Tinoco SánchezОценок пока нет
- Fallo de La Haya: Este Es El DocumentoДокумент71 страницаFallo de La Haya: Este Es El DocumentoLa RepúblicaОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Nation Brands Finance 2015Документ24 страницыNation Brands Finance 2015Christian Tinoco SánchezОценок пока нет
- FutureBrand's Country Brand IndexДокумент107 страницFutureBrand's Country Brand IndexskiftnewsОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Reply of The Government of PeruДокумент360 страницReply of The Government of PeruChristian Tinoco SánchezОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Rejoinder of The Government of ChileДокумент381 страницаRejoinder of The Government of ChileChristian Tinoco SánchezОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Counter-Memorial of The Government of ChileДокумент407 страницCounter-Memorial of The Government of ChileChristian Tinoco SánchezОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Memorial of The Government of PeruДокумент302 страницыMemorial of The Government of PeruChristian Tinoco SánchezОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Best Global Brands 2012Документ75 страницBest Global Brands 2012Christian Tinoco SánchezОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- Presentación de Peter Tomka, Presidente de La Corte de La HayaДокумент5 страницPresentación de Peter Tomka, Presidente de La Corte de La HayaChristian Tinoco SánchezОценок пока нет
- Eurobrand 2012 Global Top 100Документ10 страницEurobrand 2012 Global Top 100robinwautersОценок пока нет
- Yokohama Living GuideДокумент102 страницыYokohama Living GuideKriz EarnestОценок пока нет
- Seneca Rachel ResumeДокумент1 страницаSeneca Rachel Resumeapi-259257079Оценок пока нет
- FijiTimes - May 17 2013Документ48 страницFijiTimes - May 17 2013fijitimescanadaОценок пока нет
- Astron Hospital and Healthcare Consultants Pvt. Ltd.Документ22 страницыAstron Hospital and Healthcare Consultants Pvt. Ltd.Rekha ChakrabartiОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Boast 1 - Fragility Hip Fractures PDFДокумент1 страницаBoast 1 - Fragility Hip Fractures PDFSam BarnesОценок пока нет
- Accomplishment ReportДокумент8 страницAccomplishment ReportKevin Fernandez MendioroОценок пока нет
- List of Approved Hospital For Cashless Facility Under New Medical Insurance Scheme of IBAДокумент332 страницыList of Approved Hospital For Cashless Facility Under New Medical Insurance Scheme of IBAAnup PrakashОценок пока нет
- Status Epilepticus What's New For The IntensivistДокумент11 страницStatus Epilepticus What's New For The IntensivistBenjamínGalvanОценок пока нет
- Hospital Department Role Play Script in EnglishДокумент4 страницыHospital Department Role Play Script in EnglishAmita putriОценок пока нет
- Factors Affecting Location of Multi Specialty HospitalДокумент32 страницыFactors Affecting Location of Multi Specialty HospitalfrancisОценок пока нет
- PHD ProposalДокумент20 страницPHD ProposalMandusОценок пока нет
- ..... The Story: Stoica (Vuta) Ileana-Magdalena Engleza - Germana Anul IiiДокумент4 страницы..... The Story: Stoica (Vuta) Ileana-Magdalena Engleza - Germana Anul Iiiileana- magdalena stoicaОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Productivity ImprovementДокумент10 страницProductivity ImprovementBudi PermanaОценок пока нет
- Discharge SummaryДокумент9 страницDischarge SummaryAllwinОценок пока нет
- Proposed 100-Bed Hospital Architectural BriefДокумент2 страницыProposed 100-Bed Hospital Architectural Briefarshad khanОценок пока нет
- Ramachari Anaesthesiologist-Brief BiodataДокумент1 страницаRamachari Anaesthesiologist-Brief Biodatadr_saketram6146Оценок пока нет
- Bahan Pagets Disease of MaxillaДокумент3 страницыBahan Pagets Disease of MaxillayuniОценок пока нет
- Therapeutic CommunicationДокумент4 страницыTherapeutic CommunicationLloyd Rafael Estabillo100% (1)
- Completion of the Partogram in PregnancyДокумент9 страницCompletion of the Partogram in Pregnancyfei cuaОценок пока нет
- Community Quarantine RecommendationsДокумент5 страницCommunity Quarantine RecommendationsRapplerОценок пока нет
- Titles of CandidatesДокумент13 страницTitles of CandidatessanolОценок пока нет
- Sneha Nirav Marjadi V State of Maharashtra Ors and Connected PetitionsДокумент16 страницSneha Nirav Marjadi V State of Maharashtra Ors and Connected PetitionsNek PuriОценок пока нет
- Patan Academy of Health Sciences: Pcrlab@pahs - Edu.np Ewarsedcd@gmail - Co Pcrlab@pahs - Edu.npДокумент2 страницыPatan Academy of Health Sciences: Pcrlab@pahs - Edu.np Ewarsedcd@gmail - Co Pcrlab@pahs - Edu.npBhageshwar Chaudhary100% (1)
- SegHIS NormalДокумент51 страницаSegHIS Normalkaliyasa0% (1)
- Carriere® SLX Self-Ligating Bracket BrochureДокумент8 страницCarriere® SLX Self-Ligating Bracket BrochureOrtho Organizers100% (1)
- NP2 Nursing Board Exam June 2008 Answer KeyДокумент14 страницNP2 Nursing Board Exam June 2008 Answer KeyBettina SanchezОценок пока нет
- MGM 5Документ17 страницMGM 5Paul KwongОценок пока нет
- Respiratory Status of Adult Patients in The Postoperative Period of Thoracic or Upper Abdominal SurgeriesДокумент8 страницRespiratory Status of Adult Patients in The Postoperative Period of Thoracic or Upper Abdominal SurgeriesDimitreОценок пока нет
- Case StudyДокумент62 страницыCase StudyIyalisaiVijay0% (1)
- Sasha Chavezs ResumeДокумент2 страницыSasha Chavezs Resumeapi-478478393Оценок пока нет
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (402)
- Roxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingОт EverandRoxane Gay & Everand Originals: My Year of Psychedelics: Lessons on Better LivingРейтинг: 5 из 5 звезд5/5 (4)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (13)