Академический Документы
Профессиональный Документы
Культура Документы
The Hidden Ectopic
Загружено:
Juniper PublishersАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
The Hidden Ectopic
Загружено:
Juniper PublishersАвторское право:
Доступные форматы
Journal of
Gynecology and Womens Health
Case Report
J Gynecol Womens Health
Copyright All rights are reserved by Niranjana Jayakrishnan
Volume 1 Issue 2 - May 2016
The Hidden Ectopic
Niranjana Jayakrishnan* and Jayakrishnan K
KJK Hospital, India
Submission: April 29, 2016; Published: May 24, 2016
*Corresponding author: Niranjana Jayakrishnan, KJK Hospital, Anjali, Golf Links Road, Kowdiar, Trivandrum, India, Tel: 9539193034; Email:
Abstract
46 year old nulliparous lady, with failed IVF cycles, underwent a repeat IVF. She conceived during that cycle. Beta hcg values were raised.
However there was no intrauterine or extrauterine sac on ultrasound. Diagnostic laparoscopy was done since the beta hcg values were high.
Dense bowel adhesions were seen on laparoscopy. Chorionic tissue was identified after dissecting the adhesions, though the tube could not be
clearly made out. Patient was followed up with beta hcg levels which became negligible in 5 weeks
Keywords: Ectopic pregnancy; Beta HCG; Laparoscopy
Case Report
46-year-old lady, nulliparous, was a known case of severe
endometriosis with adenomyosis. She had undergone 3
laparoscopic surgeries, first in 1993 for bilateral endometriotic
cysts, and the last one in 2013, which showed dense bowel
adhesions to the uterus with both adnexa completely covered
with bowel adhesions. She had a hydrosalpinx for which she
underwent right salpingectomy during the last laparoscopy.
Husband was diagnosed with non obstructive azoospermia with
elevated FSH levels. She underwent IVF in October 2015, during
which 2 embryos were transferred. Her beta hcg on day 14 was
1810. When repeated after 4 days, the value was 8025.
An ultrasound was done which revealed no intrauterine or
extrauterine sac. Patient was followed up with beta hcg levels,
after 2 days, which became 24813. Patient was asymptomatic,
and value repeated after 2 days was 28222. Ultrasound repeated
again, showed no intra uterine or extrauterine sac, and an
endometrium of 9mm in thickness. Since value was extremely
high, and as no intrauterine pregnancy was localized on
ultrasound, patient and bystanders were counseled and taken
up for operative laparoscopy. At laparoscopy, the bowel was seen
densely adherent to both adnexa, making it difficult to visualize
the adnexa. Bowel (rectosigmoid) was adherent to the posterior
surface as well as fundus of the uterus [1].
The bowel adhesions near the left adnexa were released
by sharp dissection. Bowel adhesiolysis could be only done
partially since there was a high risk of bowel injury. At one
J Gynecol Womens Health1(2): JGWH.MS.ID.555558 (2016)
point, tissue resembling chorionic tissue was seen projecting
out from a structure resembling the fallopian tube. Tube could
not be identified separately. Chorionic tissue was taken for
histopathological examination. Bleeding points were identified
from the suspected base of the tube, which was coagulated using
micro bipolar cautery. Since the vital structures like ureter and
iliac vessels were extremely close to the lateral wall, further
coagulation of the bleeding points could not be done. Drain was
inserted and patient was followed up with serial hcg. 4 days
after the surgery, decreased to 3110 mIU/ml. The following week
the value was 526mIU/ml. She was followed up with expectant
management with serial weekly monitoring of hcg. The value
reached negligible limits 5 weeks after surgery. (Figures 1-4).
Figure 1: Right adnexa adherent to bowel.
001
Journal of Gynecology and Womens Health
factors, a common factor for ectopic pregnancy is prior damage
to fallopian tube.
Useful ultrasonographic findings in the diagnosis of ectopic
pregnancy
Absence of intrauterine pregnancy (IUP)
Positive identification of an ectopic pregnancy mass:
inhomogeneous mass, empty adnexal gestation sac or
adnexal sac containing yolk sac or fetal pole
Figure 2: Left adnexa completely covered with dense bowel
adhesions.
Figure 3: Bowel adhesions partially released.
Figure 4: Products of conception retrieved through left lateral
port.
Discussion
An ectopic pregnancy is the implantation of the fertilized
ovum outside the uterine cavity. The incidence of ectopic is
around 1-3%. Though there are no major identifiable risk
002
Free fluid (i.e. blood): suggestive of ectopic pregnancy
in the absence of IUP, but not diagnostic (small amount may
be physiological [2].
In cases where an ectopic pregnancy is suspected and
ultrasound is inconclusive, a diagnostic laparoscopy may be
required. This is believed by many to be the gold standard
investigation in ectopic pregnancy. Indeed reluctance or delay in
performing a diagnostic laparoscopy has been highlighted as a
factor in fatal cases [1].
However, some small ectopic pregnancies may be missed
at the time of laparoscopy or laparotomy. An alternative
to diagnostic laparoscopy may involve a repeat ultrasound
examination, particularly when -hcg concentrations are close
to 1500 IU/l. Other strategies include alternative diagnostic
tests, such as serum progesterone or an endometrial biopsy,
or empirical medical treatment as the patient may well have
an ectopic pregnancy. If -hcg concentrations are falling but an
ectopic has not been excluded, consideration should be given
to performing serial -hcg measurements until levels become
undetectable, as rupture can still occur.
In selected cases of PUL, an endometrial biopsy may be
taken and analysed for the presence or absence of chorionic villi.
Their absence in the presence of a static -hcg is suggestive of
an ectopic pregnancy. A dilatation and curettage may be useful
when performed in association with a negative diagnostic
laparoscopy for a suspected ectopic pregnancy. The clinician
should be certain that the pregnancy, if intrauterine, is nonviable and appropriate consent obtained, as this procedure could
potentially interrupt a continuing pregnancy.
References
1. Robson SJ, OShea RT (1996) Undiagnosed ectopic pregnancy: a
retrospective analysis of 31 missed ectopic pregnancies at a teaching
hospital. Aust N Z J Obstet Gynaecol 36(2): 182-185.
2. Barnhart KT, Sammel MD, Rinaudo PF, Zhou L, Hummel AC, et al. (2004)
Symptomatic patients with an early viable intrauterine pregnancy:
HCG curves redefined. Obstet Gynecol 104(1): 50-55.
How to cite this article: Niranjana J, Jayakrishnan K. The Hidden Ectopic. J Gynecol Womens Health. 2016; 1(2): 555558.
Вам также может понравиться
- DiabesityДокумент1 страницаDiabesityJuniper PublishersОценок пока нет
- Experience and Knowledge of Female Genital Mutilation Amongst London Obstetrics and Gynaecology TraineesДокумент4 страницыExperience and Knowledge of Female Genital Mutilation Amongst London Obstetrics and Gynaecology TraineesJuniper PublishersОценок пока нет
- In The Era of Budgetary Constraints, Cost-Effective Management of Metabolic Syndrome, Type 2 Diabetes, and Obesity Is EssentialДокумент6 страницIn The Era of Budgetary Constraints, Cost-Effective Management of Metabolic Syndrome, Type 2 Diabetes, and Obesity Is EssentialJuniper PublishersОценок пока нет
- Critical Limb Ischemia Treatment Strategies in Diabetics: Present Deeds and Future ChallengesДокумент5 страницCritical Limb Ischemia Treatment Strategies in Diabetics: Present Deeds and Future ChallengesJuniper PublishersОценок пока нет
- Value of Urocortin As A Marker For Preterm LaborДокумент7 страницValue of Urocortin As A Marker For Preterm LaborJuniper Publishers100% (1)
- Type 2 Diabetic Patients On Insulin Can Reduce or Eliminate Insulin With Lifestyle Change and Carbohydrate RestrictionДокумент5 страницType 2 Diabetic Patients On Insulin Can Reduce or Eliminate Insulin With Lifestyle Change and Carbohydrate RestrictionJuniper PublishersОценок пока нет
- Lifestyle and DiabesityДокумент1 страницаLifestyle and DiabesityJuniper PublishersОценок пока нет
- Infertility Awareness Among UK University StudentsДокумент9 страницInfertility Awareness Among UK University StudentsJuniper PublishersОценок пока нет
- Endometrial Cancer Treatment: New Insights Into The Role of Erbb ReceptorsДокумент3 страницыEndometrial Cancer Treatment: New Insights Into The Role of Erbb ReceptorsJuniper PublishersОценок пока нет
- Safety and Efficacy of Yoga and Naturopathy Based Lifestyle in Patients Suffering From Rheumatoid ArthritisДокумент5 страницSafety and Efficacy of Yoga and Naturopathy Based Lifestyle in Patients Suffering From Rheumatoid ArthritisJuniper PublishersОценок пока нет
- Use of Semen Quality To Predict Pregnancy in Couples Undergoing ICSIДокумент4 страницыUse of Semen Quality To Predict Pregnancy in Couples Undergoing ICSIJuniper PublishersОценок пока нет
- Arsenic Pollution in Agriculture: Its Uptake and Metabolism in Plant SystemДокумент5 страницArsenic Pollution in Agriculture: Its Uptake and Metabolism in Plant SystemJuniper PublishersОценок пока нет
- Diagnostic Performance of Magnetic Resonance Imaging in The Pretreatment Evaluation of Invasive Cervical CarcinomaДокумент7 страницDiagnostic Performance of Magnetic Resonance Imaging in The Pretreatment Evaluation of Invasive Cervical CarcinomaJuniper PublishersОценок пока нет
- Six Million Ways of Science CommunicationДокумент2 страницыSix Million Ways of Science CommunicationJuniper PublishersОценок пока нет
- Unusual Clinical Presentation of Congenital Malaria: Cholestasis in NewbornДокумент3 страницыUnusual Clinical Presentation of Congenital Malaria: Cholestasis in NewbornJuniper PublishersОценок пока нет
- Quantifying The Trade Effects of Sanitary and Phytosanitary Regulations of The Eu On Sudan's Groundnuts ExportsДокумент9 страницQuantifying The Trade Effects of Sanitary and Phytosanitary Regulations of The Eu On Sudan's Groundnuts ExportsJuniper PublishersОценок пока нет
- Rural Composting For Improvement of Soil Health and Sustainable AgricultureДокумент8 страницRural Composting For Improvement of Soil Health and Sustainable AgricultureJuniper PublishersОценок пока нет
- Energy Balance in Modern Agroecosystems Why and How?Документ4 страницыEnergy Balance in Modern Agroecosystems Why and How?Juniper PublishersОценок пока нет
- Effect of Quercus Cortex Extract With Alum For Bacterial Metritis and Vaginitis Treatment in Different Ages in CowsДокумент5 страницEffect of Quercus Cortex Extract With Alum For Bacterial Metritis and Vaginitis Treatment in Different Ages in CowsJuniper PublishersОценок пока нет
- Transient Elastography is superior to the FIB 4 Index, Aspartate Platelet Ratio Index, Aspartate Alanine Aminotransferase Ratio, Age Platelet Index and Fibrosis Index in Diagnosing Fibrosis in Chronic Hepatitis B PatientsДокумент17 страницTransient Elastography is superior to the FIB 4 Index, Aspartate Platelet Ratio Index, Aspartate Alanine Aminotransferase Ratio, Age Platelet Index and Fibrosis Index in Diagnosing Fibrosis in Chronic Hepatitis B PatientsJuniper PublishersОценок пока нет
- Ogilvie's Syndrome Complicating A Hemorrhagic Stroke of BrainstemДокумент3 страницыOgilvie's Syndrome Complicating A Hemorrhagic Stroke of BrainstemJuniper PublishersОценок пока нет
- Serum Serotonin As A Novel Marker For Hepatocellular CarcinomaДокумент7 страницSerum Serotonin As A Novel Marker For Hepatocellular CarcinomaJuniper PublishersОценок пока нет
- Portal Venous Gas in A Patient With End-Stage Renal DiseaseДокумент4 страницыPortal Venous Gas in A Patient With End-Stage Renal DiseaseJuniper PublishersОценок пока нет
- Hepatic Artery Thrombosis After Orthotopic Liver TransplantationДокумент4 страницыHepatic Artery Thrombosis After Orthotopic Liver TransplantationJuniper PublishersОценок пока нет
- Evaluation of Human Epidermal Growth Factor As A Tumor Marker in Patients With Hepatocellular Carcinoma Related To Hepatitis C VirusДокумент5 страницEvaluation of Human Epidermal Growth Factor As A Tumor Marker in Patients With Hepatocellular Carcinoma Related To Hepatitis C VirusJuniper PublishersОценок пока нет
- Robotic by Pass Made SimpleДокумент1 страницаRobotic by Pass Made SimpleJuniper PublishersОценок пока нет
- Quality and Complications of Colonoscopy in Ahvaz Jundishapur UniversityДокумент4 страницыQuality and Complications of Colonoscopy in Ahvaz Jundishapur UniversityJuniper PublishersОценок пока нет
- A Randomized Comparative Study of Efficacy of Lamivudine and Adefovir Combination Versus Tenofovir Versus Entecavir in Decompensated Cirrhotic Patients of Hepatitis BДокумент5 страницA Randomized Comparative Study of Efficacy of Lamivudine and Adefovir Combination Versus Tenofovir Versus Entecavir in Decompensated Cirrhotic Patients of Hepatitis BJuniper PublishersОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Certificate: of EU Product NotificationДокумент2 страницыCertificate: of EU Product NotificationJsamCondoriОценок пока нет
- Acetaminophen (Paracetamol, Tylenol, Tempra, Panadol)Документ3 страницыAcetaminophen (Paracetamol, Tylenol, Tempra, Panadol)Jocelyn Rivera0% (1)
- Pelayanan PaliatifДокумент43 страницыPelayanan PaliatifBety RindaОценок пока нет
- Aga Khan University Postgraduate Medical Education (Pgme) Induction Frequently Asked QuestionsДокумент15 страницAga Khan University Postgraduate Medical Education (Pgme) Induction Frequently Asked QuestionsRamzan BibiОценок пока нет
- (Lecture 4) Vice, Drug Education and ControlДокумент25 страниц(Lecture 4) Vice, Drug Education and ControlJohnpatrick DejesusОценок пока нет
- The Effects of Exercise On The Nervous SystemДокумент2 страницыThe Effects of Exercise On The Nervous SystemramadanОценок пока нет
- Putrik 2014 - Access To RA BiologicsДокумент13 страницPutrik 2014 - Access To RA BiologicsNona Delia ChiriacОценок пока нет
- Activity Journal Mobile Blood Donation Advocacy 1Документ3 страницыActivity Journal Mobile Blood Donation Advocacy 1Cherrymae BenzonОценок пока нет
- Blood CirculationДокумент42 страницыBlood CirculationAshu kumar100% (1)
- United General Hospital ICU Expansion Case StudyДокумент7 страницUnited General Hospital ICU Expansion Case StudyTeddy Les Holladayz25% (4)
- PsoriasisДокумент0 страницPsoriasisaurax143Оценок пока нет
- Raised CA125 - What We Actually Know. - .: ReviewДокумент7 страницRaised CA125 - What We Actually Know. - .: Reviewaish25Оценок пока нет
- General Tonic Monograph and Pharmacology Shi Quan Da Bu WanДокумент8 страницGeneral Tonic Monograph and Pharmacology Shi Quan Da Bu WanrikiОценок пока нет
- Stylohyoid LigamentДокумент4 страницыStylohyoid LigamentArindom ChangmaiОценок пока нет
- Chapter 42 - Upper Urinary Tract: TraumaДокумент2 страницыChapter 42 - Upper Urinary Tract: TraumaSyahdat NurkholiqОценок пока нет
- Placenta PreviaДокумент12 страницPlacenta Previapatriciagchiu100% (3)
- Graphic Organizer ExampleДокумент1 страницаGraphic Organizer Exampleapi-398530613Оценок пока нет
- Gastritis CronicaДокумент12 страницGastritis CronicaKati RondonОценок пока нет
- Press Release On COVIDEXДокумент2 страницыPress Release On COVIDEXNasasira BensonОценок пока нет
- Twin Block Functional Therapy Applications in Dentofacial Orthopedics 3Документ565 страницTwin Block Functional Therapy Applications in Dentofacial Orthopedics 3Bianca Iovoaia100% (11)
- General Examination For CVSДокумент29 страницGeneral Examination For CVSstudymedic100% (1)
- IJMRBS 530b6369aa161Документ16 страницIJMRBS 530b6369aa161yogeshgharpureОценок пока нет
- Natures Hidden Health MiracleДокумент38 страницNatures Hidden Health MiracleGorneau100% (2)
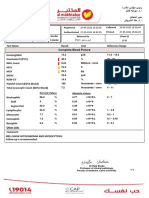
- Complete Blood Picture: 60 Year Female 23321506381Документ3 страницыComplete Blood Picture: 60 Year Female 23321506381SilavioОценок пока нет
- Daftar PustakaДокумент2 страницыDaftar PustakaErick PrasetyaОценок пока нет
- Aron FinalДокумент70 страницAron FinalJaime Pastrana Jr.Оценок пока нет
- Orbino, Frances Anne N. 4th Rot FdarДокумент2 страницыOrbino, Frances Anne N. 4th Rot FdarFrances OrbinoОценок пока нет
- 51-1606756076 TypДокумент6 страниц51-1606756076 TypbelaariyantiОценок пока нет
- Patient Education and NegotiationДокумент7 страницPatient Education and NegotiationSammy ChegeОценок пока нет
- Pain Fellowship ProgramДокумент14 страницPain Fellowship ProgramshahidkhattakОценок пока нет