Академический Документы
Профессиональный Документы
Культура Документы
03 Jadumani PDF
Загружено:
Nulul Ci LoolyИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
03 Jadumani PDF
Загружено:
Nulul Ci LoolyАвторское право:
Доступные форматы
Journal of Academia and Industrial Research (JAIR)
Volume 3, Issue 5 October 2014
215
ISSN: 2278-5213
RESEARCH ARTICLE
Etiology of Adult Patients of Portal Hypertension and Evaluation of
their Clinical Presentations
1,2
Jadumani Nayak1, Smaraka R. Panda2 and Sudeshna Behera3*
3
Dept. of Medicine, Dept. of Biochemistry, SCB Medical College, Cuttack, Odisha, India
drjadumani@gmail.com, drsmarak@gmail.com, 4sudeshna@gmail.com*; +91 9238826182
______________________________________________________________________________________________
Abstract
There are only few studies on etiology of Portal Hypertension (PH) among adults in India. Hence, this study
was conducted to assess the etiology of portal hypertension in adults and evaluate their clinical
presentations. The study enrolled 142 cases of portal hypertension patients admitted to the Dept. of General
Medicine and Hepatology unit, SCB Medical College, Cuttack, Odisha, India. All cases were thoroughly examined
along with complete history. Blood was collected for routine hemogram, Liver function test (LFT) and
Prothrombin time (PT), -fetoprotein level, estimation of hepatitis B surface antigen and hepatitis C virus
antibody. Totally 142 adult patients (>18 years) were enrolled in this study. Most common cause of portal
hypertension in our study was cirrhosis of liver (49%) followed by cirrhosis + Hepatocellular Ca (HCC) (15%),
Non-cirrhotic portal fibrosis (NCPF) (13%), Budd-Chiary syndrome (BCS) (7%) and Extra Hepatic Portal Vein
Obstruction (EHPVO) (7%). Similarly anemia (85%) was the most common presentation followed by
splenomegaly (62%), haematemesis (62%) and malena (56%). Hepatic encephalopathy was present in 31%
of cases. Cirrhosis of liver followed by alcohol, hepatitis B or HCV infection was the commonest cause of
portal hypertension in elderly patients. Anemia followed by splenomegaly, haematemesis and melena are the
common presenting features of portal hypertension.
Keywords: Portal hypertension, cirrhosis, Budd-Chiary syndrome, anemia, splenomegaly, haematemesis.
Introduction
Portal hypertension (PH) is a common clinical syndrome
defined as the elevation of hepatic venous pressure
gradient 5 mm Hg (Groszmann et al., 2005). It can be
present as esophageal variceal bleeding, ascitis or
hypersplenism. But it is important to understand the
cause of portal hypertension to put in place the strategies
to prevent/ameliorate the same. PH can be due to many
different causes at prehepatic, intrahepatic and
posthepatic sites. Proper diagnosis and management of
these are vital for improving quality of life and patients
survival (Merli et al., 2003). The cause of portal
hypertension in every country varies. With increasing
affluence, better standards of living as well as change to
more sedentary life style in India, metabolic syndrome
leading to non-alcohol related fatty liver disease (NAFLD)
as well as alcohol related cirrhosis are expected to
increase in the coming years while hepatitis B or C virus
related cirrhosis may be expected to decline (Goel et al.,
2013). Only few studies were done in India which
focused on the cause of portal hypertension (Ray et al.,
2000; Verghese et al., 2007). Ray et al. (2000) reported
Hepatitis B as the more important cause of portal
hypertension in adults in eastern India. Studies from
other part of world reported Hepatitis C and alcohol as
the predominant etiology of chronic liver disease
(Mendez-Sanchez et al., 2004; Michitaka et al., 2010).
Various clinical presentations are direct consequences of
portal hypertension.
Youth Education and Research Trust (YERT)
In other complications, portal hypertension plays a key
role, although it is not the only factor for its development
(Kaji et al., 2012). Considering all the above facts, this
study was conducted to document the etiology of adult
patients of portal hypertension and evaluate their clinical
presentations.
Materials and methods
Patients: The study enrolled 142 cases of portal
hypertension patients admitted to the Dept. of general
medicine and hepatology unit, SCB Medical College,
Cuttack, Odisha, India. Cases were selected on clinical
ground and based on different related biochemical and
radiological investigations along with upper GI
endoscopy and histological liver biopsy in selected
cases. Patients with septicemia, ischemic heart disease
and other comorbid conditions like uncontrolled diabetes
were excluded from the study.
Experimental investigation: All cases were thoroughly
examined along with complete history. Blood was
collected for routine hemogram, LFT and PT,
-fetoprotein level, estimation of hepatitis B surface
antigen and hepatitis C virus antibody. Along with these
biochemical and cytological investigations of ascetic
fluid, test for fecal occult blood, routine and microscopic
examinations of urine, ECG, chest X-ray, USG of
abdomen, Doppler USG, endoscopy and CT scan of
abdomen were done.
jairjp.com
Jadumani et al., 2014
Journal of Academia and Industrial Research (JAIR)
Volume 3, Issue 5 October 2014
216
Liver biopsy was done in selected cases, where space
occupying lesions were detected by USG.
Results
There was a male preponderance with M:F ratio of 3:1.
Majority of cases belonged to 35-45 years and oldest
was of 70 years. Most were from lower socio-economic
status which may be due to high prevalence of
alcoholism in this group. Past history of patients revealed
that majority of them were addicted to alcohol (31%),
22% had suffered from viral hepatitis and 20% had
hematemesis (Table 1). Although past history of viral
hepatitis was obtained in only 56 patients (31%), HBsAg
was positive in 66 patients (47%), out of which 50 were
cirrhosis and 16 having HCC (Table 2). Anti-HCV
antibody was positive in 26 patients (18%), out of which
20 were having cirrhosis and 6 were having HCC.
All cases of Non-cirrhotic portal fibrosis (NCPF),
Extrahepatic portal vein obstruction (EHPVO) and
Budd-Chiari syndrome (BCS) were HBV and HCV
negative. Out of 16 selected patients who underwent
liver biopsy, all were having cirrhosis and sinusoidal
fibrosis and 12 patients were having features of HCC
(75%) (Table 3). In this study, AFP level was found to be
elevated in 22 patients with HCC (Table 4). The cause of
portal hypertension in the study included mainly cirrhosis
of liver, HCC, Non-cirrotic portal fibrosis, extrahepatic
portal vein obstruction and Budd-Chiary syndrome
(Table 5). Anemia (85%), splenomegaly (62%), melena
(56%), hematemesis (45%), swelling of abdomen (38%),
jaundice (31%) were most common clinical features of
the study (Table 6).
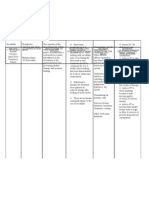
Table 1. Past history of patients.
Past history
History obtained
Alcoholism
56
Viral hepatitis
40
Haematemesis
36
Melena
24
Ascitis + Pedal oedema
26
Percentage
31%
22%
20%
13%
14%
Table 2. Prevalence of viral markers in patients.
No of
Status
cases
%
Disease
(n=71)
Cirrhosis
HBsAg +ve
66
47%
HCC
Anti-HCV
Cirrhosis
26
18%
antibody
HCC
NCPF
B -ve and
50
35%
EHPVO
C ve
BCS
Total
142
100%
No.
50
16
20
6
18
22
10
142
Table 3. Liver biopsy profile.
No of cases
Findings
Percentage
(n=16)
cirrhosis
16
100%
Sinusoidal fibrosis
16
100%
Features of HCC
12
75%
Youth Education and Research Trust (YERT)
Table 4. -fetoprotein (AFP) level in patients with HCC.
Level (mg/L)
No. of cases (n=22)
Percentage
< 500
0
0%
500-1000
2
9%
1000-1500
14
64%
>1500
6
27%
Total
22
100%
Table 5. Etiology of portal hypertension.
No. of
Cause
cases
Percentage
(n=142)
Cirrhosis of liver
70
49%
Cirrhosis +HCC
22
15%
Non-cirrhotic portal fibrosis
18
13%
Extrahepatic portal vein obstruction
22
15%
Budd-Chiari syndrome
10
7%
Total
142
100%
Table 6. Symptoms and signs of PH at presentation.
No. of
Symptoms and signs
cases
Percentage
(n=142)
Hematemesis
88
62%
Ascitis (swelling of abdomen)
56
38%
Melena
80
56%
Loss of appetite
40
28%
Swelling of feet
30
21%
Anemia
120
85%
Engorged abdominal vein
20
14
Hepatomegaly
30
21%
Splenomegaly
88
62%
Jaundice
44
31%
Fever
20
14%
Hepatic encephalopathy
44
31%
Discussion
Portal hypertension is the most challenging health
problem of people all over the world. It is a widely
prevalent condition affecting people in their most
precious years of live (5-45 years). A vast majority of
literatures on portal hypertension have been published
from western countries where etiology and outcome
differ significantly from that of tropics. Paucity of
data in tropics compounds the doctors difficulties in
management of portal hypertension. Many workers hold
the view that chronic alcohol intake is a potent
predisposing factor for development of cirrhosis
of liver (Bellentani et al., 1997; Corrao et al., 1998).
Other workers also have noted past history of infective
hepatitis as high as >20% of cases of cirrhosis patients
(Rodger et al., 2000; Joseph et al., 2006). Past history of
hematemesis was found in 20% of patients and melena
was found in 13% of cases. Lebrec et al. (1980) found
almost similar incidence of upper GI bleeding in case of
cirrhosis (Lebrec et al., 1980). Liver biopsy done in
16 patients showed cirrhosis and sinusoidal fibrosis in all
patients and features of HCC were found in 75%.
jairjp.com
Jadumani et al., 2014
Journal of Academia and Industrial Research (JAIR)
Volume 3, Issue 5 October 2014
217
On studying the AFP level, 22 patients were found to be
having high levels of AFP. In an adult, high level of AFP
without an obvious GI tumor strongly suggest HCC.
Rising level suggest progression of tumor or recurrence
after hepatic resection. After studying all the Tables,
commonest etiology of portal hypertension was found to
be cirrhosis of liver followed by alcohol (n=56) or
followed by hepatitis B (N=66) or HCV infection (n=16).
Other etiologies were found to be extra hepatic portal
vein obstruction (n=22), hepatocellular carcinoma (n=22),
non-cirrhotic portal fibrosis (n=18) and Budd-Chiary
syndrome (n=10). This report is in variance from the
study conducted in Southern India (Goel et al., 2013)
where cryptogenic chronic liver disease was found to be
the predominant cause of portal hypertension followed by
alcohol and hepatitis B related liver disease. But our
study report is similar to other studies (Michitaka et al.,
2010; Johnson et al., 2011), where alcohol and hepatitis
C were found to be the main cause of PH. Alcohol intake
in India is steadily increasing with decrease in the
initiation age. This alarming trend is noticed in many
areas of country (Das et al., 2006). In our study, alcohol
intake was a significant contributory factor and this may
be a reflection of referral bias, low socio-economic
situation or can be a reflection of changing trend. On
focusing the clinical presentation of portal hypertensive
patients of our study, we found anemia in almost 85% of
cases, splenomegaly in 62% of cases. According to
different studies, anemia of diverse etiology occurs in
about 75% of patients with chronic liver disease
(McHutchison et al., 2006). A major cause of it is
hemorrhage into GI tract and defect in blood coagulation
in severe hepatocellular disease (Gonzalez-Casas et al.,
2009). Similarly Sherlock (1997) stated that if there is
no splenomegaly in a case of PH, the diagnosis is
erroneous. There are many studies to justify the
coexistence of splenomegaly with PH (Bolognesi et al.,
2002; Voros et al., 2005). Clinically the spleen might
have been shrunken due to acute GI bleed. However, the
other general symptoms like hematemesis, melena,
swelling of abdomen, pedal edema were observed in our
study during the time of presentation.
Conclusion
Most common cause of portal hypertension in our study
was cirrhosis of liver (49%) followed by cirrhosis + HCC
(15%), Non-cirrhotic portal fibrosis (13%), Budd-Chiary
syndrome and EHPVO. Similarly, we conclude from our
study that anemia is the most common presentation
followed by splenomegaly, haematemesis and melena.
However, further studies are needed taking a larger
study population regarding etiology of portal
hypertension in adults and in elderly from different parts
of India, especially to analyze variations in different
socio-economic categories. Overall, portal hypertension
is largely a preventable condition because the
commonest etiology is alcoholism.
Youth Education and Research Trust (YERT)
References
1. Bellentani, S., Saccoccio, G., Costa, G., Tiribelli, C., Manenti, F.,
Sodde, M., Saveria Croce, L., Sasso, F., Pozzato, G. and
Cristianini, G. 1997. Brandi and the Dionysos study group. Drinking
habits as cofactors of risk for alcohol induced liver damage. Gut.
41: 845-850.
2. Bolognesi, M., Merkel, C., Sacerdoti, D., Nava, V. and Gatta, A.
2002. Role of spleen enlargement in cirrhosis with portal
hypertension. Digest. Liver Dis. 34(2): 144-150.
3. Corrao, G., Bagnardi, V., Zambon, A. and Torchio, P. 1998.
Meta-analysis of alcohol intake in relation to risk of liver cirrhosis.
Alcohol Alcoholism. 33(4): 381-392.
4. Das, S.K., Balakrishnan, V. and Vasudevan, D.M. 2006. Alcohol: Its
health and social impact in India. Natl. Med. J. Ind. 19: 94-99.
5. Goel, A., Madhu, K., Zachariah, U., Sajith, K.G., Ramachandran, J.,
Ramakrishna, B., Gibikote, S., Jude, J., Chandy, G.M. and Elias, E.
2013. A study of etiology of portal hypertension in adults (including
the elderly) at a tertiary centre in southern India. Ind.
J. Med. Res. 137: 922-927.
6. Gonzalez-Casas, E., Jones, A. and Moreno-Otero, R. 2009.
Spectrum of anemia associated with chronic liver disease. World J.
Gastroenterol. 15(37): 4653-4658.
7. Groszmann, R.J., Garcia-Tsao, G. and Bosch, J. 2005.
Beta-blockers to prevent gastroesophageal varices in patients with
cirrhosis. New Engl. J. Med. 353(21): 2254-2261.
8. Johnson, E.A., Spier, B.J., Leff, J.A., Lucey, M.R. and Said, A.
2011. Optimising the care of patients with cirrhosis and
gastrointestinal haemorrhage: A quality improvement study.
Aliment Pharmacol. Ther. 34: 76-82.
9. Kaji, B.C., Bhavsar, Y.R., Patel, N., Garg, A., Kevadiya, H. and
Mansuri, Z. A study of clinical profile of 50 patients with portal
hypertension and to evaluate role of non-invasive predictor of
esophageal varices. Ind. J. Clin. Pract. 22(9): 454-457.
10. Lebrec, D., Nouel, O., Corbic, M. and Benhamou, J.P. 1980.
Propranolol-A medical treatment for portal hypertension?
Lancet. 2(8187): 180-182.
11. McHutchison, J.G., Manns, M.P. and Longo, D.L. 2006. Definition
and management of anemia in patients infected with hepatitis C
virus. Liver Int. 26: 389-398.
12. Mendez-Sanchez, N., Aguilar-Ramirez, J.R., Reyes, A., Dehesa,
M., Juorez, A. and Castneda, B. 2004. Groupo de Estudio,
Asociaon Mexicana de Hepatologyia. Etiology of liver cirrhosis in
Mexico. Ann. Hepatol. 3: 30-33.
13. Merli, M., Nicolini, G. and Angeloni, S. 2003. Incidence and natural
history of small esophageal varices in cirrhotic patients. J. Hepatol.
38(3): 266-272.
14. Michitaka, K., Nishiguchi, S., Aoyagi, Y., Hiasa, Y., Tokumoto, Y.
and Onji, M. 2010. Japan etiology of liver cirrhosis study group.
Etiology of liver cirrhosis in Japan: A nationwide survey.
J. Gastroenterol. 45: 86-94.
15. Perz, J.F., Armstrong, G.L., Farrington, L.A., Hutin, Y.J.H. and Bell,
B.P. 2006. The contributions of hepatitis B virus and hepatitis C
virus infections to cirrhosis and primary liver cancer worldwide.
J. Hepatol. 45: 529-538.
16. Ray, G., Ghoshal, U.C., Banerjee, P.K., Pal, B.B., Dhar, K. and Pal,
A.K. 2000. Aetiological spectrum of chronic liver disease in eastern
India. Trop. Gastroenterol. 21: 60-62.
17. Rodger, A.J., Roberts, S., Lanigan, A., Bowden, S. And Crofts, N.
2000. Assessment of long-term outcomes of community-acquired
hepatitis C infection in a cohort with sera stored from 19711975.
Hepatol. 32: 582-587.
th
18. Sherlock, S. 1997. Disease of liver and billiary system, 9 edn.,
Blackwell Scientific Publications.
19. Verghese, J., Navaneethan, U. and Venkatraman, J. 2007. Clinical
pattern of elderly cirrhosis: An Indian experience. Eur. J.
Gastroenterol. Hepatol. 19: 1031-1033.
20. Voros, D., Mallas, E., Antoniou, A., Kafantari, E., Kokoris, S.E.,
Smyrniotis, B. and Pangalis, G.A. 2005. Splenomegaly and left
sided portal hypertension. Ann. Gastroenterol. 18(3): 341-345.
jairjp.com
Jadumani et al., 2014
Вам также может понравиться
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Algorithm GERD Primary Care Pathway Ahs SCN DH 2020 15262Документ7 страницAlgorithm GERD Primary Care Pathway Ahs SCN DH 2020 15262Mihaela ShimanОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Table e - Liver Anatomy Biliary SystemДокумент11 страницTable e - Liver Anatomy Biliary Systemapi-371971600Оценок пока нет
- PancreatitisДокумент6 страницPancreatitisMary AmaliaОценок пока нет
- Nursing Upper Gi BleedingДокумент23 страницыNursing Upper Gi BleedingLord Pozak Miller100% (3)
- Seminar: Pere Ginès, Aleksander Krag, Juan G Abraldes, Elsa Solà, Núria Fabrellas, Patrick S KamathДокумент18 страницSeminar: Pere Ginès, Aleksander Krag, Juan G Abraldes, Elsa Solà, Núria Fabrellas, Patrick S KamathcastillojessОценок пока нет
- Assessment and Management of Patients With Biliary DisordersДокумент16 страницAssessment and Management of Patients With Biliary DisordersJills JohnyОценок пока нет
- 461 706 1 PBДокумент6 страниц461 706 1 PBNulul Ci LoolyОценок пока нет
- Management of Portal Hypertension in Children: Ahmed Mahmoud El-Tawil, MSC, MRCS, PHDДокумент9 страницManagement of Portal Hypertension in Children: Ahmed Mahmoud El-Tawil, MSC, MRCS, PHDNulul Ci LoolyОценок пока нет
- Hypertension, Diuretic Use, and Risk of Hearing LossДокумент7 страницHypertension, Diuretic Use, and Risk of Hearing LossNulul Ci LoolyОценок пока нет
- Urinary Tract Infection in WomenДокумент11 страницUrinary Tract Infection in WomenDermovi Adika RangkutiОценок пока нет
- Leaflet SF68 Opportunity For New Territories 2009 Cerbios Probiotic CapsulesДокумент3 страницыLeaflet SF68 Opportunity For New Territories 2009 Cerbios Probiotic Capsulesamin138irОценок пока нет
- Abdominal Pain in ChildrenДокумент36 страницAbdominal Pain in ChildrenKiani LarasОценок пока нет
- პანკრეასიДокумент24 страницыპანკრეასიSASIDHARОценок пока нет
- Key Points SurgeryДокумент2 страницыKey Points SurgeryVyom ShrigodОценок пока нет
- 2-醫學四-住院病歷寫作範本 - 原則 增修版Документ6 страниц2-醫學四-住院病歷寫作範本 - 原則 增修版蘇西瓦Оценок пока нет
- Recent Advances in The Understanding of Bile Acid MalabsorptionДокумент15 страницRecent Advances in The Understanding of Bile Acid Malabsorptionbdalcin5512Оценок пока нет
- Perspectives in Clinical Gastroenterology and Hepatology: A Gastroenterologist's Guide To ProbioticsДокумент9 страницPerspectives in Clinical Gastroenterology and Hepatology: A Gastroenterologist's Guide To ProbioticsMihajilo TosicОценок пока нет
- Kokate List of Probiotics ApprovedДокумент3 страницыKokate List of Probiotics ApprovedHari ThekkethilОценок пока нет
- 2014 ProsidingSNIJAДокумент17 страниц2014 ProsidingSNIJASayu Putu Yuni ParyatiОценок пока нет
- Irritable Bowel SyndromeДокумент2 страницыIrritable Bowel SyndromeDeepthiОценок пока нет
- STUDIES ON ANTIULCER ACTIVITY OF Solanum Melongena (SOLANACEAE)Документ5 страницSTUDIES ON ANTIULCER ACTIVITY OF Solanum Melongena (SOLANACEAE)xiuhtlaltzinОценок пока нет
- 169166461003186341.1.2.virechan Patient ReferenceДокумент3 страницы169166461003186341.1.2.virechan Patient ReferenceBharathi PОценок пока нет
- Screenshot 2022-01-02 at 12.40.18 PMДокумент22 страницыScreenshot 2022-01-02 at 12.40.18 PMالقناة الرسمية للشيخ عادل ريانОценок пока нет
- Diarrhea - ChuДокумент19 страницDiarrhea - Chukint manlangitОценок пока нет
- EVH Cholangitis Cholangiohepatitis Syndrome 2019 220519 WebДокумент7 страницEVH Cholangitis Cholangiohepatitis Syndrome 2019 220519 WebLeo OoОценок пока нет
- Epigastric Pain and Indigestion CausesДокумент6 страницEpigastric Pain and Indigestion CausesNadia SalwaniОценок пока нет
- A Review of Crohn's Disease: Pathophysiology, Genetics, Immunology, Environmental Factors, Clinical Presentation, Diagnosis, ManagementДокумент18 страницA Review of Crohn's Disease: Pathophysiology, Genetics, Immunology, Environmental Factors, Clinical Presentation, Diagnosis, ManagementValentina RodriguezОценок пока нет
- Reviewer Digestive SystemДокумент12 страницReviewer Digestive SystemLorenzo Gabriel RSОценок пока нет
- Drug Study CHDCДокумент1 страницаDrug Study CHDCIannBlancoОценок пока нет
- Digestive-SystemДокумент93 страницыDigestive-SystemJulia Stefanel PerezОценок пока нет
- Organic DiseasesДокумент3 страницыOrganic DiseasesGlenn Cabance LelinaОценок пока нет
- CON 1B GI and Endocrine DisordersДокумент2 страницыCON 1B GI and Endocrine DisordersAllyza Trixia Joyce VillasotoОценок пока нет
- 1 PBДокумент7 страниц1 PBIka Wirya WirawantiОценок пока нет
- Hepatology Research - 2023 - Yoshiji - Management of Cirrhotic Ascites Seven Step Treatment Protocol Based On The JapaneseДокумент12 страницHepatology Research - 2023 - Yoshiji - Management of Cirrhotic Ascites Seven Step Treatment Protocol Based On The JapaneseSarah FaziraОценок пока нет