Академический Документы
Профессиональный Документы
Культура Документы
Langmans Medical Embryology
Загружено:
Jaweria Islam Khan BangashИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Langmans Medical Embryology
Загружено:
Jaweria Islam Khan BangashАвторское право:
Доступные форматы
Contents part one General Embryology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . .
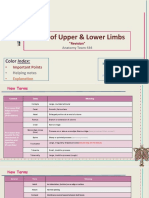
chapter 1 Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes . .... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 2 First Week of Development: Ovulation to Implantation ............ . . . . . . . chapter 3 Second Week of Development: B ilaminar Germ Disc ............ . . . . . . . . . . chapter 4 Third Week of Deve lopment: Trilaminar Germ Disc ............. . . . . . . . . . . chapter 5 Third to Eighth Week: The Embryonic Period ............... . . . . . . . . . . . . . . . . chapter 6 Third Month to Birth: The Fetus and Placenta ................... . . . . . . . . . . . . chapter 7 Birth Defects and Prenatal Diagnosis ......... .......... . . . . . . . . . . . . . . . . . . . . . 1 3 31 51 65 87 117 149 part two Special Embryology . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 8 Skeletal System ............................. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 169 171 ix
x Contents chapter 9 Muscular System ........................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 10 Body Cavities ....... ..................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 11 Cardiovascular System ......................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 12 Resp iratory System ........................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 13 Digestive System ..................... ...... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 14 Urogenital System .......................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 15 Head and Neck ...... ...................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 16 Ear ................................. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 17 Eye ................................ . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 18 I ntegumentary System .......................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . chapter 19 Central Nervous System ............... .......... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 199 211 223 275 285 321 363 403 415 427 433 part three Appendix. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Answers to Problems .......................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . Figure Credits .......................... . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . ex ................................. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 483 485 499 507 . . . . . . . . . . . Ind . .
Preface The ninth edition of Langmans Medical Embryology adheres to the tradition establi shed by the original publicationit provides a concise but thorough description of embryology and its clinical signi cance, an awareness of which is essential in th e diagnosis and prevention of birth defects. Recent advances in genetics, develo pmental biology, maternal-fetal medicine, and public health have signi cantly incr eased our knowledge of embryology and its relevance. Because birth defects are t he leading cause of infant mortality and a major contributor to disabilities, an d because new prevention strategies have been developed, understanding the princ iples of embryology is important for health care professionals. To accomplish it s goal, Langmans Medical Embryology retains its unique approach of combining an e conomy of text with excellent diagrams and scanning electron micrographs. It rei nforces basic embryologic concepts by providing numerous clinical examples that result from abnormalities in developmental processes. The following pedagogic fe atures and updates in the ninth edition help facilitate student learning: Organi zation of Material: Langmans Medical Embryology is organized into two parts. The r st provides an overview of early development from gametogenesis through the embr yonic period; also included in this section are chapters on placental and fetal development and prenatal diagnosis and birth defects. The second part of the tex t provides a description of the fundamental processes of embryogenesis for each organ system. Molecular Biology: New information is provided about the molecular basis of normal and abnormal development. Extensive Art Program: This edition f eatures almost 400 illustrations, including new 4-color line drawings, scanning electron micrographs, and ultrasound images. Clinical Correlates: In addition to describing normal events, each chapter contains clinical correlates that appear in highlighted boxes. This material is designed to provide information about bi rth defects and other clinical entities that are directly related to embryologic concepts. vii
viii Preface Summary: At the end of each chapter is a summary that serves as a concise review of the key points described in detail throughout the chapter. Problems to Solve : These problems test a students ability to apply the information covered in a pa rticular chapter. Detailed answers are provided in an appendix in the back of th e book. Simbryo: New to this edition, Simbryo, located in the back of the book, is an interactive CD-ROM that demonstrates normal embryologic events and the ori gins of some birth defects. This unique educational tool offers six original vec tor art animation modules to illustrate the complex, three-dimensional aspects o f embryology. Modules include normal early development as well as head and neck, cardiovascular, gastrointestinal, genitourinary, and pulmonary system developme nt. Connection Web Site: This student and instructor site (http://connection. LW W.com/go/sadler) provides updates on new advances in the eld and a syllabus desig ned for use with the book. The syllabus contains objectives and de nitions of key terms organized by chapters and the bottom line, which provides a synopsis of the most basic information that students should have mastered from their studies. I hope you nd this edition of Langmans Medical Embryology to be an excellent resourc e. Together, the textbook, CD, and connection site provide a user-friendly and i nnovative approach to learning embryology and its clinical relevance. T. W. Sadl er Twin Bridges, Montana
part one General Embryology 1
chapter 1 Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes Primordial Germ Cells Development begins with fertilization, the process by whic h the male gamete, the sperm, and the female gamete, the oocyte, unite to give r ise to a zygote. Gametes are derived from primordial germ cells (PGCs) that are formed in the epiblast during the second week and that move to the wall of the y olk sac (Fig. 1.1). During the fourth week these cells begin to migrate from the yolk sac toward the developing gonads, where they arrive by the end of the fth w eek. Mitotic divisions increase their number during their migration and also whe n they arrive in the gonad. In preparation for fertilization, germ cells undergo gametogenesis, which includes meiosis, to reduce the number of chromosomes and cytodifferentiation to complete their maturation. CLINICAL CORRELATE Primordial Germ Cells (PGCs) and Teratomas Teratomas are tumors of disputed orig in that often contain a variety of tissues, such as bone, hair, muscle, gut epit helia, and others. It is thought that these tumors arise from a pluripotent stem cell that can differentiate into any of the three germ layers or their derivati ves. 3
4 Part One: General Embryology Figure 1.1 An embryo at the end of the third week, showing the position of primo rdial germ cells in the wall of the yolk sac, close to the attachment of the fut ure umbilical cord. From this location, these cells migrate to the developing go nad. Some evidence suggests that PGCs that have strayed from their normal migratory p aths could be responsible for some of these tumors. Another source is epiblast c ells migrating through the primitive streak during gastrulation (see page 80). The Chromosome Theory of Inheritance Traits of a new individual are determined b y speci c genes on chromosomes inherited from the father and the mother. Humans ha ve approximately 35,000 genes on 46 chromosomes. Genes on the same chromosome te nd to be inherited together and so are known as linked genes. In somatic cells, chromosomes appear as 23 homologous pairs to form the diploid number of 46. Ther e are 22 pairs of matching chromosomes, the autosomes, and one pair of sex chrom osomes. If the sex pair is XX, the individual is genetically female; if the pair is XY, the individual is genetically male. One chromosome of each pair is deriv ed from the maternal gamete, the oocyte, and one from the paternal gamete, the
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 5 sperm. Thus each gamete contains a haploid number of 23 chromosomes, and the uni on of the gametes at fertilization restores the diploid number of 46. MITOSIS Mi tosis is the process whereby one cell divides, giving rise to two daughter cells that are genetically identical to the parent cell (Fig. 1.2). Each daughter cel l receives the complete complement of 46 chromosomes. Before a cell enters mitos is, each chromosome replicates its deoxyribonucleic acid (DNA). During this repl ication phase the chromosomes are extremely long, they are spread diffusely thro ugh the nucleus, and they cannot be recognized with the light microscope. With t he onset of mitosis the chromosomes begin to coil, contract, and condense; these events mark the beginning of prophase. Each chromosome now consists of two para llel subunits, chromatids, that are joined at a narrow region common to both cal led the centromere. Throughout prophase the chromosomes continue to condense, sh orten, and thicken (Fig. 1.2A), but only at prometaphase do the chromatids becom e distinguishable (Fig. 1.2B ). During metaphase the chromosomes line up in the equatorial plane, Figure 1.2 Various stages of mitosis. In prophase, chromosomes are visible as sl ender threads. Doubled chromatids become clearly visible as individual units dur ing metaphase. At no time during division do members of a chromosome pair unite. Blue, paternal chromosomes; red, maternal chromosomes.
6 Part One: General Embryology and their doubled structure is clearly visible (Fig. 1.2C ). Each is attached by microtubules extending from the centromere to the centriole, forming the mitoti c spindle. Soon the centromere of each chromosome divides, marking the beginning of anaphase, followed by migration of chromatids to opposite poles of the spind le. Finally, during telophase, chromosomes uncoil and lengthen, the nuclear enve lope reforms, and the cytoplasm divides (Fig. 1.2, D and E ). Each daughter cell receives half of all doubled chromosome material and thus maintains the same nu mber of chromosomes as the mother cell. MEIOSIS Meiosis is the cell division tha t takes place in the germ cells to generate male and female gametes, sperm and e gg cells, respectively. Meiosis requires two cell divisions, meiosis I and meios is II, to reduce the number of chromosomes to the haploid number of 23 (Fig. 1.3 ). As in mitosis, male and female germ cells (spermatocytes and primary oocytes) at the beginning of meiosis I replicate their DNA so that each of the 46 chromo somes is duplicated into sister chromatids. In contrast to mitosis, however, hom ologous chromosomes then align themselves in pairs, a process called synapsis. T he pairing is exact and point for point except for the XY combination. Homologou s pairs then separate into two daughter cells. Shortly thereafter meiosis II sep arates sister chromatids. Each gamete then contains 23 chromosomes. Crossover Cr ossovers, critical events in meiosis I, are the interchange of chromatid segment s between paired homologous chromosomes (Fig. 1.3C ). Segments of chromatids bre ak and are exchanged as homologous chromosomes separate. As separation occurs, p oints of interchange are temporarily united and form an X-like structure, a chia sma (Fig. 1.3C ). The approximately 30 to 40 crossovers (one or two per chromoso me) with each meiotic I division are most frequent between genes that are far ap art on a chromosome. As a result of meiotic divisions, (a) genetic variability i s enhanced through crossover, which redistributes genetic material, and through random distribution of homologous chromosomes to the daughter cells; and (b) eac h germ cell contains a haploid number of chromosomes, so that at fertilization t he diploid number of 46 is restored. Polar Bodies Also during meiosis one primar y oocyte gives rise to four daughter cells, each with 22 plus 1 X chromosomes (F ig. 1.4A). However, only one of these develops into a mature gamete, the oocyte; the other three, the polar bodies, receive little cytoplasm and degenerate duri ng subsequent development. Similarly, one primary spermatocyte gives rise to fou r daughter cells, two with 22 plus 1
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 7 Figure 1.3 First and second meiotic divisions. A. Homologous chromosomes approac h each other. B. Homologous chromosomes pair, and each member of the pair consis ts of two chromatids. C. Intimately paired homologous chromosomes interchange ch romatid fragments (crossover). Note the chiasma. D. Double-structured chromosome s pull apart. E. Anaphase of the rst meiotic division. F and G. During the second meiotic division, the double-structured chromosomes split at the centromere. At completion of division, chromosomes in each of the four daughter cells are diff erent from each other. X chromosomes and two with 22 plus 1 Y chromosomes (Fig. 1.4B). However, in cont rast to oocyte formation, all four develop into mature gametes. CLINICAL CORRELATES Birth Defects and Spontaneous Abortions: Chromosomal and Genetic Factors Chromos omal abnormalities, which may be numerical or structural, are important causes o f birth defects and spontaneous abortions. It is estimated that 50% of conceptio ns end in spontaneous abortion and that 50% of these
8 Part One: General Embryology Figure 1.4 Events occurring during the rst and second maturation divisions. A. Th e primitive female germ cell (primary oocyte) produces only one mature gamete, t he mature oocyte. B. The primitive male germ cell (primary spermatocyte) produce s four spermatids, all of which develop into spermatozoa. abortuses have major chromosomal abnormalities. Thus approximately 25% of concep tuses have a major chromosomal defect. The most common chromosomal abnormalities in abortuses are 45,X (Turner syndrome), triploidy, and trisomy 16. Chromosomal abnormalities account for 7% of major birth defects, and gene mutations account for an additional 8%. Numerical Abnormalities The normal human somatic cell con tains 46 chromosomes; the normal gamete contains 23. Normal somatic cells are di ploid, or 2n; normal gametes are haploid, or n. Euploid refers to any exact mult iple of n, e.g., diploid or triploid. Aneuploid refers to any chromosome number that is not euploid; it is usually applied when an extra chromosome is present ( trisomy) or when one is missing (monosomy). Abnormalities in chromosome number m ay originate during meiotic or mitotic divisions. In meiosis, two members of a p air of homologous chromosomes normally separate during the rst meiotic division s o that each daughter cell receives one member of each pair (Fig. 1.5A). Sometime s, however, separation does not occur (nondisjunction), and both members of a pa ir move into one cell (Fig. 1.5, B and C ). As a result of nondisjunction of the chromosomes, one cell receives 24 chromosomes, and the other receives 22 instea d of the normal 23. When, at fertilization, a gamete having 23 chromosomes fuses with a gamete having 24 or
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 9 Figure 1.5 A. Normal maturation divisions. B. Nondisjunction in the ivision. C. Nondisjunction in the second meiotic division. rst meiotic d
22 chromosomes, the result is an individual with either 47 chromosomes (trisomy) or 45 chromosomes (monosomy). Nondisjunction, which occurs during either the rst or the second meiotic division of the germ cells, may involve the autosomes or sex chromosomes. In women, the incidence of chromosomal abnormalities, including nondisjunction, increases with age, especially at 35 years and older. Occasiona lly nondisjunction occurs during mitosis (mitotic nondisjunction) in an embryoni c cell during the earliest cell divisions. Such conditions produce mosaicism, wi th some cells having an abnormal chromosome number and others being normal. Affe cted individuals may exhibit few or many of the characteristics of a particular syndrome, depending on the number of cells involved and their distribution. Some times chromosomes break, and pieces of one chromosome attach to another. Such tr anslocations may be balanced, in which case breakage and reunion occur between t wo chromosomes but no critical genetic material is lost and individuals are norm al; or they may be unbalanced, in which case part of one chromosome is lost and an altered phenotype is produced. For example, unbalanced translocations between the long arms of chromosomes 14 and 21 during meiosis I or II produce gametes w ith an extra copy of chromosome 21, one of the causes of Down syndrome (Fig. 1.6 ). Translocations
10 Part One: General Embryology A 14 21 t(14;21) Figure 1.6 A. Translocation of the long arms of chromosomes 14 and 21 at the cen tromere. Loss of the short arms is not clinically signi cant, and these individual s are clinically normal, although they are at risk for producing offspring with unbalanced translocations. B. Karyotype of translocation of chromosome 21 onto 1 4, resulting in Down syndrome.
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 11 Figure 1.7 Karyotype of trisomy 21 (arrow), Down syndrome. are particularly common between chromosomes 13, 14, 15, 21, and 22 because they cluster during meiosis. TRISOMY 21 (DOWN SYNDROME) Down syndrome is usually caused by an extra copy of chromosome 21 (trisomy 21, F ig. 1.7). Features of children with Down syndrome include growth retardation; va rying degrees of mental retardation; craniofacial abnormalities, including upwar d slanting eyes, epicanthal folds (extra skin folds at the medial corners of the eyes), at facies, and small ears; cardiac defects; and hypotonia (Fig. 1.8). The se individuals also have relatively high incidences of leukemia, infections, thy roid dysfunction, and premature aging. Furthermore, nearly all develop signs of Alzheimers disease after age 35. In 95% of cases, the syndrome is caused by triso my 21 resulting from meiotic nondisjunction, and in 75% of these instances, nond isjunction occurs during oocyte formation. The incidence of Down syndrome is app roximately 1 in 2000 conceptuses for women under age 25. This risk increases wit h maternal age to 1 in 300 at age 35 and 1 in 100 at age 40. In approximately 4% of cases of Down syndrome, there is an unbalanced translocation between chromos ome 21 and chromosome 13, 14, or 15 (Fig. 1.6). The nal 1% are caused by mosaicis m resulting from mitotic
12 Part One: General Embryology Figure 1.8 A and B. Children with Down syndrome, which is characterized by a at, broad face, oblique palpebral ssures, epicanthus, and furrowed lower lip. C. Anot her characteristic of Down syndrome is a broad hand with single transverse or si mian crease. Many children with Down syndrome are mentally retarded and have con genital heart abnormalities. nondisjunction. These individuals have some cells with a normal chromosome numbe r and some that are aneuploid. They may exhibit few or many of the characteristi cs of Down syndrome. TRISOMY 18 Patients with trisomy 18 show the following features: mental retardation, congen ital heart defects, low-set ears, and exion of ngers and hands (Fig. 1.9). In addi tion, patients frequently show micrognathia, renal anomalies, syndactyly, and ma lformations of the skeletal system. The incidence of this condition is approxima tely 1 in 5000 newborns. Eighty- ve percent are lost between 10 weeks of gestation and term, whereas those born alive usually die by age 2 months. 13 The main abn ormalities of trisomy 13 are mental retardation, holoprosencephaly, congenital h eart defects, deafness, cleft lip and palate, and eye defects, such as microphth almia, anophthalmia, and coloboma (Fig. 1.10). The incidence of this abnormality is approximately 1 in 20,000 live births, and over 90% of the infants die in th e rst month after birth. TRISOMY
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 13 Figure 1.9 Photograph of child with trisomy 18. Note the prominent occiput, clef t lip, micrognathia, low-set ears, and one or more exed ngers. Figure 1.10 A. Child with trisomy 13. Note the cleft lip and palate, the sloping forehead, and microphthalmia. B. The syndrome is commonly accompanied by polyda ctyly. KLINEFELTER SYNDROME The clinical features of Klinefelter syndrome, found only in males and usually d etected at puberty, are sterility, testicular atrophy, hyalinization of the semi niferous tubules, and usually gynecomastia. The cells have 47 chromosomes with a sex chromosomal complement of the XXY type, and a sex chromatin body (Barr body : formed by condensation of an inactivated sex chromosome; a Barr body is also p resent in normal females) is found in 80% of cases (Fig. 1.11). The incidence is approximately 1 in 500 males. Nondisjunction of the XX homologues is the most c ommon causative event. Occasionally, patients with Klinefelter syndrome have 48 chromosomes: 44 autosomes and four sex chromosomes (XXXY). Although mental retar dation is not generally
14 Part One: General Embryology Figure 1.11 Patient with Klinefelter syndrome showing normal phallus development but gynecomastia (enlarged breasts). part of the syndrome, the more X chromosomes there are, the more likely there wi ll be some degree of mental impairment. TURNER SYNDROME Turner syndrome, with a 45,X karyotype, is the only monosomy compatible with lif e. Even then, 98% of all fetuses with the syndrome are spontaneously aborted. Th e few that survive are unmistakably female in appearance (Fig. 1.12) and are cha racterized by the absence of ovaries (gonadal dysgenesis) and short stature. Oth er common associated abnormalities are webbed neck, lymphedema of the extremitie s, skeletal deformities, and a broad chest with widely spaced nipples. Approxima tely 55% of affected women are monosomic for the X and chromatin body negative b ecause of nondisjunction. In 80% of these women, nondisjunction in the male game te is the cause. In the remainder of women, structural abnormalities of the X ch romosome or mitotic nondisjunction resulting in mosaicism are the cause.
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 15 Figure 1.12 Patient with Turner syndrome. The main characteristics are webbed ne ck, short stature, broad chest, and absence of sexual maturation. TRIPLE X SYNDROME Patients with triple X syndrome are infantite, with scanty menses and some degre e of mental retardation. They have two sex chromatin bodies in their cells. Stru ctural Abnormalities Structural chromosome abnormalities, which involve one or m ore chromosomes, usually result from chromosome breakage. Breaks are caused by e nvironmental factors, such as viruses, radiation, and drugs. The result of break age depends on what happens to the broken pieces. In some cases, the broken piec e of a chromosome is lost, and the infant with partial deletion of a chromosome is abnormal. A well-known syndrome, caused by partial deletion of the short arm of chromosome 5, is the cri-du-chat syndrome. Such children have a catlike cry, microcephaly, mental retardation, and congenital heart disease. Many other relat ively rare syndromes are known to result from a partial chromosome loss. Microde letions, spanning only a few contiguous genes, may result in microdeletion syndr ome or contiguous gene syndrome. Sites where these deletions occur, called conti guous gene complexes, can be identi ed by high-resolution chromosome banding. An e xample of a microdeletion
16 Part One: General Embryology Figure 1.13 Patient with Angelman syndrome resulting from a microdeletion on mat ernal chromosome 15. If the defect is inherited on the paternal chromosome, Prad er-Willi syndrome occurs (Fig. 1.14). occurs on the long arm of chromosome 15 (15q1115q13). Inheriting the deletion on the maternal chromosome results in Angelman syndrome, and the children are menta lly retarded, cannot speak, exhibit poor motor development, and are prone to unp rovoked and prolonged periods of laughter (Fig. 1.13). If the defect is inherite d on the paternal chromosome, Prader-Willi syndrome is produced; affected indivi duals are characterized by hypotonia, obesity, mental retardation, hypogonadism, and cryptorchidism (Fig. 1.14). Characteristics that are differentially express ed depending upon whether the genetic material is inherited from the mother or t he father are examples of genomic imprinting. Other contiguous gene syndromes ma y be inherited from either parent, including Miller-Dieker syndrome (lissencepha ly, developmental delay, seizures, and cardiac and facial abnormalities resultin g from a deletion at 17p13) and most cases of velocardiofacial (Shprintzen) synd rome (palatal defects, conotruncal heart defects, speech delay, learning disorde rs, and schizophrenia-like disorder resulting from a deletion in 22q11). Fragile sites are regions of chromosomes that demonstrate a propensity to separate or b reak under certain cell manipulations. For example, fragile sites can be reveale d by culturing lymphocytes in folate-de cient medium. Although numerous fragile si tes have been de ned and consist of CGG repeats, only the site on the long arm of the X chromosome (Xq27) has been
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 17 Figure 1.14 Patient with Prader-Willi syndrome resulting from a microdeletion on paternal chromosome 15. If the defect is inherited on the maternal chromosome, Angelman syndrome occurs (Fig. 1.13). correlated with an altered phenotype and is called the fragile X syndrome. Fragi le X syndrome is characterized by mental retardation, large ears, prominent jaw, and pale blue irides. Males are affected more often than females (1/1000 versus 1/2000), which may account for the preponderance of males among the mentally re tarded. Fragile X syndrome is second only to Down syndrome as a cause of mental retardation because of chromosomal abnormalities. Gene Mutations Many congenital formations in humans are inherited, and some show a clear mendelian pattern of inheritance. Many birth defects are directly attributable to a change in the str ucture or function of a single gene, hence the name single gene mutation. This t ype of defect is estimated to account for approximately 8% of all human malforma tions.
18 Part One: General Embryology With the exception of the X and Y chromosomes in the male, genes exist as pairs, or alleles, so that there are two doses for each genetic determinant, one from the mother and one from the father. If a mutant gene produces an abnormality in a single dose, despite the presence of a normal allele, it is a dominant mutatio n. If both alleles must be abnormal (double dose) or if the mutation is X-linked in the male, it is a recessive mutation. Gradations in the effects of mutant ge nes may be a result of modifying factors. The application of molecular biologica l techniques has increased our knowledge of genes responsible for normal develop ment. In turn, genetic analysis of human syndromes has shown that mutations in m any of these same genes are responsible for some congenital abnormalities and ch ildhood diseases. Thus, the link between key genes in development and their role in clinical syndromes is becoming clearer. In addition to causing congenital ma lformations, mutations can result in inborn errors of metabolism. These diseases , among which phenylketonuria, homocystinuria, and galactosemia are the best kno wn, are frequently accompanied by or cause various degrees of mental retardation . Diagnostic Techniques for Identifying Genetic Abnormalities Cytogenetic analys is is used to assess chromosome number and integrity. The technique requires div iding cells, which usually means establishing cell cultures that are arrested in metaphase by chemical treatment. Chromosomes are stained with Giemsa stain to r eveal light and dark banding patterns (G-bands; Fig. 1.6) unique for each chromo some. Each band represents 5 to 10 106 base pairs of DNA, which may include a fe w to several hundred genes. Recently, high resolution metaphase banding techniqu es have been developed that demonstrate greater numbers of bands representing ev en smaller pieces of DNA, thereby facilitating diagnosis of small deletions. New molecular techniques, such as uorescence in situ hybridization (FISH), use speci c DNA probes to identify ploidy for a few selected chromosomes. Fluorescent probe s are hybridized to chromosomes or genetic loci using cells on a slide, and the results are visualized with a uorescence microscope (Fig.1.15). Spectral karyotyp e analysis is a technique in which every chromosome is hybridized to a unique uor escent probe of a different color. Results are then analyzed by a computer. Morp hological Changes During Maturation of the Gametes OOGENESIS Maturation of Oocyt es Begins Before Birth Once primordial germ cells have arrived in the gonad of a genetic female, they differentiate into oogonia (Fig. 1.16, A and B). These cel ls undergo a number
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 19 Figure 1.15 Fluorescence in situ hybridization (FISH) using a probe for chromoso me 21. Two interphase cells and a metaphase spread of chromosomes are shown; eac h has three domains, indicated by the probe, characteristic of trisomy 21 (Down syndrome). Figure 1.16 Differentiation of primordial germ cells into oogonia begins shortly after their arrival in the ovary. By the third month of development, some oogon ia give rise to primary oocytes that enter prophase of the rst meiotic division. This prophase may last 40 or more years and nishes only when the cell begins its n al maturation. During this period it carries 46 double-structured chromosomes.
20 Part One: General Embryology Surface epithelium of ovary Flat epithelial cell Oogonia Primary oocyte in prophase Resting primary oocyte (diplotene stage) Follicular cell Primary oocytes in prophase of 1st meiotic division A 4th month B 7th month C Newborn Figure 1.17 Segment of the ovary at different stages of development. A. Oogonia are grouped in clusters in the cortical part of the ovary. Some show mitosis; ot hers have differentiated into primary oocytes and entered prophase of the rst mei otic division. B. Almost all oogonia are transformed into primary oocytes in pro phase of the rst meiotic division. C. There are no oogonia. Each primary oocyte i s surrounded by a single layer of follicular cells, forming the primordial folli cle. Oocytes have entered the diplotene stage of prophase, in which they remain until just before ovulation. Only then do they enter metaphase of the rst meiotic division. of mitotic divisions and, by the end of the third month, are arranged in cluster s surrounded by a layer of at epithelial cells (Fig. 1.17 and 1.18). Whereas all of the oogonia in one cluster are probably derived from a single cell, the at epi thelial cells, known as follicular cells, originate from surface epithelium cove ring the ovary. The majority of oogonia continue to divide by mitosis, but some of them arrest their cell division in prophase of meiosis I and form primary ooc ytes (Figs. 1.16C and 1.17A). During the next few months, oogonia increase rapid ly in number, and by the fth month of prenatal development, the total number of g erm cells in the ovary reaches its maximum, estimated at 7 million. At this time , cell death begins, and many oogonia as well as primary oocytes become atretic. By the seventh month, the majority of oogonia have degenerated except for a few near the surface. All surviving primary oocytes have entered prophase of meiosi s I, and most of them are individually surrounded by a layer of at epithelial cel ls (Fig. 1.17B). A primary oocyte, together with its surrounding at epithelial ce lls, is known as a primordial follicle (Fig. 1.19A).
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 21 Figure 1.18 A. Primordial follicle consisting of a primary oocyte surrounded by a layer of attened epithelial cells. B. Early primary or preantral stage follicle recruited from the pool of primordial follicles. As the follicle grows, follicu lar cells become cuboidal and begin to secrete the zona pellucida, which is visi ble in irregular patches on the surface of the oocyte. C. Mature primary (preant ral) follicle with follicular cells forming a strati ed layer of granulosa cells a round the oocyte and the presence of a well-de ned zona pellucida. Maturation of Oocytes Continues at Puberty Near the time of birth, all primary o ocytes have started prophase of meiosis I, but instead of proceeding into metaph ase, they enter the diplotene stage, a resting stage during prophase that is cha racterized by a lacy network of chromatin (Fig. 1.17C ). Primary oocytes remain in prophase and do not nish their rst meiotic division before puberty is reached, apparently because of oocyte maturation inhibitor (OMI), a substance secreted by follicular cells. The total number of primary oocytes at birth is estimated to vary from 700,000 to 2 million. During childhood most oocytes become atretic; on ly approximately 400,000 are present by the beginning of puberty, and fewer than 500 will be ovulated. Some oocytes that reach maturity late in life have been d ormant in the diplotene stage of the rst meiotic division for 40 years or more be fore ovulation. Whether the diplotene stage is the most suitable phase to protec t the oocyte against environmental in uences is unknown. The fact that the risk of having children with chromosomal abnormalities increases with maternal age indi cates that primary oocytes are vulnerable to damage as they age. At puberty, a p ool of growing follicles is established and continuously maintained from the sup ply of primordial follicles. Each month, 15 to 20 follicles selected from this p ool begin to mature, passing through three stages: 1) primary or preantral; 2) s econdary or antral (also called vesicular or Graa an); and 3) preovulatory. The an tral stage is the longest, whereas the preovulatory stage encompasses approximat ely 37 hours before ovulation. As the primary oocyte begins to grow, surrounding follicular cells change from at to cuboidal and proliferate to produce a strati ed epithelium of granulosa cells, and the unit
AF Figure 1.19 A. Secondary (antral) stage follicle. The oocyte, surrounded by the zona pellucida, is off-center; the antrum has developed by uid accumulation betwe en intercellular spaces. Note the arrangement of cells of the theca interna and the theca externa. B. Mature secondary (graa an) follicle. The antrum has enlarged considerably, is lled with follicular uid, and is surrounded by a strati ed layer o f granulosa cells. The oocyte is embedded in a mound of granulosa cells, the cum ulus oophorus. C. Photomicrograph of a mature secondary follicle with an enlarge d uid- lled antrum (cavity, Cav) and a diameter of 20 mm (65). CO, cumulus oophorus; MG, granulosa cells; AF, atretic follicle.
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 23 is called a primary follicle (Fig. 1.18, B and C ). Granulosa cells rest on a ba sement membrane separating them from surrounding stromal cells that form the the ca folliculi. Also, granulosa cells and the oocyte secrete a layer of glycoprote ins on the surface of the oocyte, forming the zona pellucida (Fig. 1.18C ). As f ollicles continue to grow, cells of the theca folliculi organize into an inner l ayer of secretory cells, the theca interna, and an outer brous capsule, the theca externa. Also, small, nger-like processes of the follicular cells extend across the zona pellucida and interdigitate with microvilli of the plasma membrane of t he oocyte. These processes are important for transport of materials from follicu lar cells to the oocyte. As development continues, uid- lled spaces appear between granulosa cells. Coalescence of these spaces forms the antrum, and the follicle is termed a secondary (vesicular, Graa an) follicle. Initially, the antrum is cres cent shaped, but with time, it enlarges (Fig. 1.19). Granulosa cells surrounding the oocyte remain intact and form the cumulus oophorus. At maturity, the second ary follicle may be 25 mm or more in diameter. It is surrounded by the theca int erna, which is composed of cells having characteristics of steroid secretion, ri ch in blood vessels, and the theca externa, which gradually merges with the ovar ian stroma (Fig. 1.19). With each ovarian cycle, a number of follicles begin to develop, but usually only one reaches full maturity. The others degenerate and b ecome atretic (Fig. 1.19C ). When the secondary follicle is mature, a surge in l uteinizing hormone (LH) induces the preovulatory growth phase. Meiosis I is comp leted, resulting in formation of two daughter cells of unequal size, each with 2 3 doublestructured chromosomes (Fig. 1.20, A and B). One cell, the secondary ooc yte, receives most of the cytoplasm; the other, the rst polar body, receives prac tically none. The rst polar body lies between the zona pellucida and the cell Zona pellucida Granulosa cells Secondary oocyte in division A Primary oocyte in division B Secondary oocyte and polar body 1 C Polar body in division Figure 1.20 Maturation of the oocyte. A. Primary oocyte showing the spindle of t he rst meiotic division. B. Secondary oocyte and rst polar body. The nuclear membr ane is absent. C. Secondary oocyte showing the spindle of the second meiotic div ision. The rst polar body is also dividing.
24 Part One: General Embryology membrane of the secondary oocyte in the perivitelline space (Fig. 1.20B ). The c ell then enters meiosis II but arrests in metaphase approximately 3 hours before ovulation. Meiosis II is completed only if the oocyte is fertilized; otherwise, the cell degenerates approximately 24 hours after ovulation. The rst polar body also undergoes a second division (Fig. 1.20C). SPERMATOGENESIS Maturation of Spe rm Begins at Puberty Spermatogenesis, which begins at puberty, includes all of t he events by which spermatogonia are transformed into spermatozoa. At birth, ger m cells in the male can be recognized in the sex cords of the testis as large, p ale cells surrounded by supporting cells (Fig. 1.21A). Supporting cells, which a re derived from the surface epithelium of the gland in the same manner as follic ular cells, become sustentacular cells, or Sertoli cells (Fig. 1.21C ). Shortly before puberty, the sex cords acquire a lumen and become the seminiferous tubule s. At about the same time, primordial germ cells give rise to spermatogonial ste m cells. At regular intervals, cells emerge from this stem cell population to fo rm type A spermatogonia, and their production marks the initiation of spermatoge nesis. Type A cells undergo a limited number of mitotic divisions to form a clon e of cells. The last cell division produces type B spermatogonia, which then div ide to form primary spermatocytes (Figs. 1.21 and 1.22). Primary spermatocytes t hen enter a prolonged Figure 1.21 A. Cross section through primitive sex cords of a newborn boy showin g primordial germ cells and supporting cells. B and C. Two segments of a seminif erous tubule in transverse section. Note the different stages of spermatogenesis .
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 25 Type A dark spermatogonia Type A pale spermatogonia Type A pale spermatogonia Ty pe A pale spermatogonia Type A pale spermatogonia Type B spermatogonia Primary spermatocytes Secondary spermatocytes Spermatids Residual bodies Spermatozoa Figure 1.22 Type A spermatogonia, derived from the spermatogonial stem cell popu lation, represent the rst cells in the process of spermatogenesis. Clones of cell s are established and cytoplasmic bridges join cells in each succeeding division until individual sperm are separated from residual bodies. In fact, the number of individual interconnected cells is considerably greater than depicted in this gure.
26 Part One: General Embryology Type B spermatogonium Resting primary spermatocyte Secondary spermatocyte Spermatid division A Mitotic B C 1st meiotic division D 2nd meiotic division Figure 1.23 The products of meiosis during spermatogenesis in humans. prophase (22 days) followed by rapid completion of meiosis I and formation of se condary spermatocytes. During the second meiotic division, these cells immediate ly begin to form haploid spermatids (Figs. 1.211.23). Throughout this series of e vents, from the time type A cells leave the stem cell population to formation of spermatids, cytokinesis is incomplete, so that successive cell generations are joined by cytoplasmic bridges. Thus, the progeny of a single type A spermatogoni um form a clone of germ cells that maintain contact throughout differentiation ( Fig. 1.22). Furthermore, spermatogonia and spermatids remain embedded in deep re cesses of Sertoli cells throughout their development (Fig. 1.24). In this manner , Sertoli cells support and protect the germ cells, participate in their nutriti on, and assist in the release of mature spermatozoa. Spermatogenesis is regulate d by luteinizing hormone (LH) production by the pituitary. LH binds to receptors on Leydig cells and stimulates testosterone production, which in turn binds to Sertoli cells to promote spermatogenesis. Follicle stimulating hormone (FSH) is also essential because its binding to Sertoli cells stimulates testicular uid pro duction and synthesis of intracellular androgen receptor proteins. Spermiogenesis The series of changes resulting in the transformation of spermati ds into spermatozoa is spermiogenesis. These changes include (a) formation of th e acrosome, which covers half of the nuclear surface and contains enzymes to ass ist in penetration of the egg and its surrounding layers during fertilization (F ig. 1.25); (b) condensation of the nucleus; (c) formation of neck, middle piece, and tail; and (d) shedding of most of the cytoplasm. In humans, the time requir ed for a spermatogonium to develop into a mature spermatozoon is approximately 6 4 days. When fully formed, spermatozoa enter the lumen of seminiferous tubules. From there, they are pushed toward the epididymis by contractile elements in the wall of the seminiferous tubules. Although initially only slightly motile, sper matozoa obtain full motility in the epididymis.
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 27 Late spermatids Early spermatids Primary spermatocyte Sertoli cell Junctional complex Type A pale spermatogonia T ype A dark spermatogonia Type B spermatogonia Basal lamina Peritubular cells Figure 1.24 Sertoli cells and maturing spermatocytes. Spermatogonia, spermatocyt es, and early spermatids occupy depressions in basal aspects of the cell; late s permatids are in deep recesses near the apex. CLINICAL CORRELATES Abnormal Gametes In humans and in most mammals, one ovarian follicle occasionall y contains two or three clearly distinguishable primary oocytes (Fig. 1.26A). Al though these oocytes may give rise to twins or triplets, they usually degenerate before reaching maturity. In rare cases, one primary oocyte contains two or eve n three nuclei (Fig. 1.26B ). Such binucleated or trinucleated oocytes die befor e reaching maturity. In contrast to atypical oocytes, abnormal spermatozoa are s een frequently, and up to 10% of all spermatozoa have observable defects. The he ad or the tail may be abnormal; spermatozoa may be giants or dwarfs; and sometim es they are joined (Fig. 1.26C ). Sperm with morphologic abnormalities lack norm al motility and probably do not fertilize oocytes.
28 Part One: General Embryology Figure 1.25 Important stages in transformation of the human spermatid into the s permatozoon. Figure 1.26 Abnormal germ cells. A. Primordial follicle with two oocytes. B. Tri nucleated oocyte. C. Various types of abnormal spermatozoa. Summary Primordial germ cells appear in the wall of the yolk sac in the fourth w eek and migrate to the indifferent gonad (Fig. 1.1), where they arrive at the en d of the fth week. In preparation for fertilization, both male and female germ ce lls undergo gametogenesis, which includes meiosis and cytodifferentiation. Durin g meiosis I, homologous chromosomes pair and exchange genetic material; during m eiosis II, cells fail to replicate DNA, and each cell is thus provided with a ha ploid number of chromosomes and half the amount of DNA of a normal somatic cell (Fig. 1.3). Hence, mature male and female gametes have, respectively, 22 plus X or 22 plus Y chromosomes. Birth defects may arise through abnormalities in chrom osome number or structure and from single gene mutations. Approximately 7% of ma jor
Chapter 1: Gametogenesis: Conversion of Germ Cells Into Male and Female Gametes 29 birth defects are a result of chromosome abnormalities, and 8%, are a result of gene mutations. Trisomies (an extra chromosome) and monosomies (loss of a chromo some) arise during mitosis or meiosis. During meiosis, homologous chromosomes no rmally pair and then separate. However, if separation fails (nondisjunction), on e cell receives too many chromosomes and one receives too few (Fig. 1.5). The in cidence of abnormalities of chromosome number increases with age of the mother, particularly with mothers aged 35 years and older. Structural abnormalities of c hromosomes include large deletions (cri-du-chat syndrome) and microdeletions. Mi crodeletions involve contiguous genes that may result in defects such as Angelma n syndrome (maternal deletion, chromosome 15q1115q13) or Prader-Willi syndrome (p aternal deletion, 15q1115q13). Because these syndromes depend on whether the affe cted genetic material is inherited from the mother or the father, they also are an example of imprinting. Gene mutations may be dominant (only one gene of an al lelic pair has to be affected to produce an alteration) or recessive (both allel ic gene pairs must be mutated). Mutations responsible for many birth defects aff ect genes involved in normal embryological development. In the female, maturatio n from primitive germ cell to mature gamete, which is called oogenesis, begins b efore birth; in the male, it is called spermatogenesis, and it begins at puberty . In the female, primordial germ cells form oogonia. After repeated mitotic divi sions, some of these arrest in prophase of meiosis I to form primary oocytes. By the seventh month, nearly all oogonia have become atretic, and only primary ooc ytes remain surrounded by a layer of follicular cells derived from the surface e pithelium of the ovary (Fig. 1.17). Together, they form the primordial follicle. At puberty, a pool of growing follicles is recruited and maintained from the nit e supply of primordial follicles. Thus, everyday 15 to 20 follicles begin to gro w, and as they mature, they pass through three stages: 1) primary or preantral; 2) secondary or antral (vesicular, Graa an); and 3) preovulatory. The primary oocy te remains in prophase of the rst meiotic division until the secondary follicle i s mature. At this point, a surge in luteinizing hormone (LH) stimulates preovula tory growth: meiosis I is completed and a secondary oocyte and polar body are fo rmed. Then, the secondary oocyte is arrested in metaphase of meiosis II approxim ately 3 hours before ovulation and will not complete this cell division until fe rtilization. In the male, primordial cells remain dormant until puberty, and onl y then do they differentiate into spermatogonia. These stem cells give rise to p rimary spermatocytes, which through two successive meiotic divisions produce fou r spermatids (Fig. 1.4). Spermatids go through a series of changes (spermiogenes is) (Fig. 1.25) including (a) formation of the acrosome, (b) condensation of the nucleus, (c) formation of neck, middle piece, and tail, and (d) shedding of mos t of the cytoplasm. The time required for a spermatogonium to become a mature sp ermatozoon is approximately 64 days.
30 Part One: General Embryology Problems to Solve 1. What is the most common cause of abnormal chromosome number ? Give an example of a clinical syndrome involving abnormal numbers of chromosom es. 2. In addition to numerical abnormalities, what types of chromosomal alterat ions occur? 3. What is mosaicism, and how does it occur? SUGGESTED READING Chandley AC: Meiosis in man. Trends Genet 4:79, 1988. Clermont Y: Kinetics of spermatogenesis in mammals: seminiferous epithelium cycle and sp ermatogonial renewal. Physiol Rev 52:198, 1972. Eddy EM, Clark JM, Gong D, Fende rson BA: Origin and migration of primordial germ cells in mammals. Gamete Res 4: 333, 1981. Gelchrter TD, Collins FS: Principles of Medical Genetics. Baltimore, Williams & Wilkins, 1990. Gorlin RJ, Cohen MM, Levin LS (eds): Syndromes of the Head and Neck. 3rd ed. New York, Oxford University, 1990. Heller CG, Clermont Y: Kinetics of the germinal epithelium in man. Recent Prog Horm Res 20:545, 1964. Johnson MH, Everett BJ: Essential Reproduction. 5th ed. London, Blackwell Scienc e Limited, 2000. Jones KL (ed): Smiths Recognizable Patterns of Human Malformatio n. 4th ed. Philadelphia, WB Saunders, 1988. Larsen WJ, Wert SE: Roles of cell ju nctions in gametogenesis and early embryonic development. Tissue Cell 20:809, 19 88. Lenke RR, Levy HL: Maternal phenylketonuria and hyperphenylalaninemia: an in ternational survey of untreated and treated pregnancies. N Engl J Med 303:1202, 1980. Pelletier RA, We K, Balakier H: Development of membrane differentiations i n the guinea pig spermatid during spermiogenesis. Am J Anat 167:119, 1983. Russe ll LD: Sertoligerm cell interactions: a review. Gamete Res 3:179, 1980. Stevenso n RE, Hall JG, Goodman RM (eds): Human Malformations and Related Anomalies. Vol I, II. New York, Oxford University Press, 1993. Thorogood P (ed): Embryos, Genes , and Birth Defects. New York, Wiley, 1997. Witschj E: Migration of the germ cel ls of the human embryos from the yolk sac to the primitive gonadal folds. Contri b Embryol 36:67, 1948.
chapter 2 First Week of Development: Ovulation to Implantation Ovarian Cycle At puberty, the female begins to undergo regular monthly cycles. T hese sexual cycles are controlled by the hypothalamus. Gonadotropin-releasing ho rmone (GnRH) produced by the hypothalamus acts on cells of the anterior pituitar y gland, which in turn secrete gonadotropins. These hormones, follicle-stimulati ng hormone (FSH) and luteinizing hormone (LH), stimulate and control cyclic chan ges in the ovary. At the beginning of each ovarian cycle, 15 to 20 primary (prea ntral) stage follicles are stimulated to grow under the in uence of FSH. (The horm one is not necessary to promote development of primordial follicles to the prima ry follicle stage, but without it, these primary follicles die and become atreti c.) Thus, FSH rescues 15 to 20 of these cells from a pool of continuously formin g primary follicles (Fig. 2.1). Under normal conditions, only one of these folli cles reaches full maturity, and only one oocyte is discharged; the others degene rate and become atretic. In the next cycle, another group of primary follicles i s recruited, and again, only one follicle reaches maturity. Consequently, most f ollicles degenerate without ever reaching full maturity. When a follicle becomes atretic, the oocyte and surrounding follicular cells degenerate and are replace d by connective tissue, forming a corpus atreticum. FSH also stimulates maturati on of follicular (granulosa) cells surrounding the oocyte. In turn, proliferatio n of these cells is mediated by growth differentiation 31
32 Part One: General Embryology Primary oocyte Granulosa cells Zona pellucida Theca externa Antrum Theca interna Primordial follicle Primary follicle Secondary follicle Figure 2.1 From the pool of primordial follicles, every day some begin to grow a nd develop into secondary (preantral) follicles, and this growth is independent of FSH. Then, as the cycle progresses, FSH secretion recruits primary follicles to begin development into secondary (antral, Graa an) follicles. During the last f ew days of maturation of secondary follicles, estrogens, produced by follicular and thecal cells, stimulate increased production of LH by the pituitary (Fig. 2. 13), and this hormone causes the follicle to enter the preovulatory stage, to co mplete meiosis I, and to enter meiosis II where it arrests in metaphase approxim ately 3 hours before ovulation. factor-9 (GDF-9), a member of the transforming growth factor- (TGF-) family. In co operation, granulosa and thecal cells produce estrogens that (a) cause the uteri ne endometrium to enter the follicular or proliferative phase; ( ) cause thinnin g of the cervical mucus to allow passage of sperm; and (c) stimulate the pituita ry gland to secrete LH. At mid-cycle, there is an LH surge that (a) elevates con centrations of maturation-promoting factor, causing oocytes to complete meiosis I and initiate meiosis II; ( ) stimulates production of progesterone y follicul ar stromal cells (luteinization); and (c) causes follicular rupture and ovulatio n. OVULATION In the days immediately preceding ovulation, under the in uence of FS H and LH, the secondary follicle grows rapidly to a diameter of 25 mm. Coinciden t with nal development of the secondary follicle, there is an a rupt increase in LH that causes the primary oocyte to complete meiosis I and the follicle to ente r the preovulatory stage. Meiosis II is also initiated, ut the oocyte is arrest ed in metaphase approximately 3 hours efore ovulation. In the meantime, the sur face of the ovary egins to ulge locally, and at the apex, an avascular spot, t he stigma, appears. The high concentration of LH increases collagenase activity, resulting in digestion of collagen ers surrounding the follicle. Prostaglandin levels also increase in response to the LH surge and cause local muscular contra ctions in the ovarian wall. Those contractions extrude the oocyte, which togethe r with its surrounding granulosa cells from the region of the cumulus
Chapter 2: First Week of Development: Ovulation to Implantation 33 Antrum Granulosa cells Theca interna 1st polar ody Oocyte in 2nd meiotic division Luteal cells Ovarian stroma Theca externa Blood vessels A Preovulatory follicle B Cumulus oophorus Fi rin cells Ovulation C Corpus luteum Figure 2.2 A. Preovulatory follicle ulging at the ovarian surface. B. Ovulation . The oocyte, in metaphase of meiosis II, is discharged from the ovary together with a large num er of cumulus oophorus cells. Follicular cells remaining inside the collapsed follicle differentiate into lutean cells. C. Corpus luteum. Note the large size of the corpus luteum, caused y hypertrophy and accumulation of l ipid in granulosa and theca interna cells. The remaining cavity of the follicle is lled with rin. oophorus, reaks free (ovulation) and oats out of the ovary (Figs. 2.2 and 2.3). Some of the cumulus oophorus cells then rearrange themselves around the zona pel lucida to form the corona radiata (Figs. 2.42.6). CLINICAL CORRELATES Ovulation During ovulation, some women feel a slight pain, known as middle pain ecause it normally occurs near the middle of the menstrual cycle. Ovulation is also generally accompanied y a rise in asal temperature, which can e monitore d to aid in determining when release of the oocyte occurs. Some women fail to ov ulate ecause of a low concentration of gonadotropins. In these cases, administr ation of an agent to stimulate gonadotropin release and hence ovulation can e e mployed. Although such drugs are effective, they often produce multiple ovulatio ns, so that the risk of multiple pregnancies is 10 times higher in these women t han in the general population. CORPUS LUTEUM After ovulation, granulosa cells re maining in the wall of the ruptured follicle, together with cells from the theca interna, are vascularized y surrounding vessels. Under the in uence of LH, these cells develop a yellowish pigment and change into lutean cells, which form the corpus luteum and secrete the hormone progesterone (Fig. 2.2C ). Progesterone, t ogether with estrogenic hormones, causes the uterine mucosa to enter the progest ational or secretory stage in preparation for implantation of the em ryo.
34 Part One: General Em ryology Figure 2.3 A. Scanning electron micrograph of ovulation in the mouse. The surfac e of the oocyte is covered y the zona pellucida. The cumulus oophorus is compos ed of granulosa cells. B. Scanning electron micrograph of a ra it oocyte 1.5 ho urs after ovulation. The oocyte, which is surrounded y granulosa cells, lies on the surface of the ovary. Note the site of ovulation.
Chapter 2: First Week of Development: Ovulation to Implantation 35 Figure 2.4 Relation of m riae and ovary. Fim riae collect the oocyte and sweep it into the uterine tu e. OOCYTE TRANSPORT Shortly efore ovulation, m riae of the oviduct egin to sweep o ver the surface of the ovary, and the tu e itself egins to contract rhythmicall y. It is thought that the oocyte surrounded y some granulosa cells (Figs. 2.3 a nd 2.4) is carried into the tu e y these sweeping movements of the m riae and y motion of cilia on the epithelial lining. Once in the tu e, cumulus cells withd raw their cytoplasmic processes from the zona pellucida and lose contact with th e oocyte. Once the oocyte is in the uterine tu e, it is propelled y cilia with the rate of transport regulated y the endocrine status during and after ovulati on. In humans, the fertilized oocyte reaches the uterine lumen in approximately 3 to 4 days. CORPUS ALBICANS If fertilization does not occur, the corpus luteum reaches maximum development approximately 9 days after ovulation. It can easily e recognized as a yellowish projection on the surface of the ovary. Su sequentl y, the corpus luteum shrinks ecause of degeneration of lutean cells and forms a mass of rotic
36 Part One: General Em ryology A B Figure 2.5 A. Scanning electron micrograph of sperm inding to the zona pellucid a. B. The three phases of oocyte penetration. In phase 1, spermatozoa pass throu gh the corona radiata arrier; in phase 2, one or more spermatozoa penetrate the zona pellucida; in phase 3, one spermatozoon penetrates the oocyte mem rane whi le losing its own plasma mem rane. Inset. Normal spermatocyte with acrosomal hea d cap.
Chapter 2: First Week of Development: Ovulation to Implantation 37 Figure 2.6 A. Oocyte immediately after ovulation, showing the spindle of the sec ond meiotic division. B. A spermatozoon has penetrated the oocyte, which has nish ed its second meiotic division. Chromosomes of the oocyte are arranged in a vesi cular nucleus, the female pronucleus. Heads of several sperm are stuck in the zo na pellucida. C. Male and female pronuclei. D and E. Chromosomes ecome arranged on the spindle, split longitudinally, and move to opposite poles. F. Two-cell s tage. scar tissue, the corpus al icans. Simultaneously, progesterone production decrea ses, precipitating menstrual leeding. If the oocyte is fertilized, degeneration of the corpus luteum is prevented y human chorionic gonadotropin (hCG), a horm one secreted y the syncytiotropho last of the developing em ryo. The corpus lut eum continues to grow and forms the corpus luteum of pregnancy (corpus luteum gr aviditatis). By the end of the third month, this structure may e one-third to o ne-half of the total size of the ovary. Yellowish luteal cells continue to secre te progesterone until the end of the fourth month; thereafter, they regress slow ly as secretion of progesterone y the tropho lastic component of the placenta ecomes adequate for maintenance of pregnancy. Removal of the corpus luteum of pr egnancy efore the fourth month usually leads to a ortion. Fertilization Fertilization, the process y which male and female gametes fuse, occurs in the ampullary region of the uterine tu e. This is the widest part of t he tu e and
38 Part One: General Em ryology is close to the ovary (Fig. 2.4). Spermatozoa may remain via le in the female re productive tract for several days. Only 1% of sperm deposited in the vagina ente r the cervix, where they may survive for many hours. Movement of sperm from the cervix to the oviduct is accomplished primarily y their own propulsion, althoug h they may e assisted y movements of uids created y uterine cilia. The trip fr om cervix to oviduct requires a minimum of 2 to 7 hours, and after reaching the isthmus, sperm ecome less motile and cease their migration. At ovulation, sperm again ecome motile, perhaps ecause of chemoattractants produced y cumulus ce lls surrounding the egg, and swim to the ampulla where fertilization usually occ urs. Spermatozoa are not a le to fertilize the oocyte immediately upon arrival i n the female genital tract ut must undergo (a) capacitation and ( ) the acrosom e reaction to acquire this capa ility. Capacitation is a period of conditioning in the female reproductive tract that in the human lasts approximately 7 hours. Much of this conditioning, which occurs in the uterine tu e, entails epithelial interactions etween the sperm and mucosal surface of the tu e. During this time a glycoprotein coat and seminal plasma proteins are removed from the plasma mem rane that overlies the acrosomal region of the spermatozoa. Only capacitated sp erm can pass through the corona cells and undergo the acrosome reaction. The acr osome reaction, which occurs after inding to the zona pellucida, is induced y zona proteins. This reaction culminates in the release of enzymes needed to pene trate the zona pellucida, including acrosin and trypsin-like su stances (Fig. 2. 5). The phases of fertilization include phase 1, penetration of the corona radia ta; phase 2, penetration of the zona pellucida; and phase 3, fusion of the oocyt e and sperm cell mem ranes. PHASE 1: PENETRATION OF THE CORONA RADIATA Of the 20 0 to 300 million spermatozoa deposited in the female genital tract, only 300 to 500 reach the site of fertilization. Only one of these fertilizes the egg. It is thought that the others aid the fertilizing sperm in penetrating the arriers p rotecting the female gamete. Capacitated sperm pass freely through corona cells (Fig. 2.5). PHASE 2: PENETRATION OF THE ZONA PELLUCIDA The zona is a glycoprotei n shell surrounding the egg that facilitates and maintains sperm inding and ind uces the acrosome reaction. Both inding and the acrosome reaction are mediated y the ligand ZP3, a zona protein. Release of acrosomal enzymes (acrosin) allows sperm to penetrate the zona, there y coming in contact with the plasma mem rane of the oocyte (Fig. 2.5). Permea ility of the zona pellucida changes when the h ead of the sperm comes in contact with the oocyte surface. This contact results in release of lysosomal
Chapter 2: First Week of Development: Ovulation to Implantation 39 enzymes from cortical granules lining the plasma mem rane of the oocyte. In turn , these enzymes alter properties of the zona pellucida (zona reaction) to preven t sperm penetration and inactivate species-speci c receptor sites for spermatozoa on the zona surface. Other spermatozoa have een found em edded in the zona pell ucida, ut only one seems to e a le to penetrate the oocyte (Fig. 2.6). PHASE 3 : FUSION OF THE OOCYTE AND SPERM CELL MEMBRANES The initial adhesion of sperm to the oocyte is mediated in part y the interaction of integrins on the oocyte an d their ligands, disintegrins, on sperm. After adhesion, the plasma mem ranes of the sperm and egg fuse (Fig. 2.5). Because the plasma mem rane covering the acr osomal head cap disappears during the acrosome reaction, actual fusion is accomp lished etween the oocyte mem rane and the mem rane that covers the posterior re gion of the sperm head (Fig. 2.5). In the human, oth the head and tail of the s permatozoon enter the cytoplasm of the oocyte, ut the plasma mem rane is left ehind on the oocyte surface. As soon as the spermatozoon has entered the oocyte, the egg responds in three ways: 1. Cortical and zona reactions. As a result of the release of cortical oocyte granules, which contain lysosomal enzymes, (a) th e oocyte mem rane ecomes impenetra le to other spermatozoa, and ( ) the zona pe llucida alters its structure and composition to prevent sperm inding and penetr ation. These reactions prevent polyspermy (penetration of more than one spermato zoon into the oocyte). 2. Resumption of the second meiotic division. The oocyte n ishes its second meiotic division immediately after entry of the spermatozoon. O ne of the daughter cells, which receives hardly any cytoplasm, is known as the s econd polar ody; the other daughter cell is the de nitive oocyte. Its chromosomes (22 + X) arrange themselves in a vesicular nucleus known as the female pronucle us (Figs. 2.6 and 2.7). 3. Meta olic activation of the egg. The activating facto r is pro a ly carried y the spermatozoon. Postfusion activation may e consider ed to encompass the initial cellular and molecular events associated with early em ryogenesis. The spermatozoon, meanwhile, moves forward until it lies close to the female pronucleus. Its nucleus ecomes swollen and forms the male pronucleu s (Fig. 2.6); the tail detaches and degenerates. Morphologically, the male and f emale pronuclei are indistinguisha le, and eventually, they come into close cont act and lose their nuclear envelopes (Fig. 2.7A). During growth of male and fema le pronuclei ( oth haploid), each pronucleus must replicate its DNA. If it does not, each cell of the two-cell zygote has only half of the normal amount of DNA. Immediately after DNA synthesis, chromosomes organize on
40 Part One: General Em ryology Figure 2.7 A. Phase contrast view of the pronuclear stage of a fertilized human oocyte with male and female pronuclei. B. Two-cell stage of human zygote. the spindle in preparation for a normal mitotic division. The 23 maternal and 23 paternal (dou le) chromosomes split longitudinally at the centromere, and siste r chromatids move to opposite poles, providing each cell of the zygote with the normal diploid num er of chromosomes and DNA (Fig. 2.6, D and E ). As sister chr omatids move to opposite poles, a deep furrow appears on the surface of the cell , gradually dividing the cytoplasm into two parts (Figs. 2.6F and 2.7B ). The ma in results of fertilization are as follows: r Restoration of the diploid num er of chromosomes, half from the far Determinat ion of the sex of the new individual. An X-carrying sperm ther and half from the mother. Hence, the zygote contains a new com ination of c hromosomes different from oth parents. produces a female (XX) em ryo, and a Y-c arrying sperm produces a male (XY) em ryo. Hence, the chromosomal sex of the em ryo is determined at fertilization. Initiation of cleavage. Without fertilizatio n, the oocyte usually degenerates 24 hours after ovulation. r CLINICAL CORRELATES Contraceptive Methods Barrier techniques of contraception include the male condo m, made of latex and often containing chemical spermicides, which ts over the pen is; and the female condom, made of polyurethane, which lines the vagina. Other arriers placed in the vagina include the diaphragm, the cervical cap, and the co ntraceptive sponge. The contraceptive pill is a com ination of estrogen and the progesterone analogue progestin, which together inhi it ovulation ut permit men struation.
Chapter 2: First Week of Development: Ovulation to Implantation 41 Both hormones act at the level of FSH and LH, preventing their release from the pituitary. The pills are taken for 21 days and then stopped to allow menstruatio n, after which the cycle is repeated. Depo-Provera is a progestin compound that can e implanted su dermally or injected intramuscularly to prevent ovulation fo r up to 5 years or 23 months, respectively. A male pill has een developed and tes ted in clinical trials. It contains a synthetic androgen that prevents oth LH a nd FSH secretion and either stops sperm production (7090% of men) or reduces it t o a level of infertility. The intrauterine device (IUD) is placed in the uterine cavity. Its mechanism for preventing pregnancy is not clear ut may entail dire ct effects on sperm and oocytes or inhi ition of preimplantation stages of devel opment. The drug RU-486 (mifepristone) causes a ortion if it is administered wit hin 8 weeks of the previous menses. It initiates menstruation, possi ly through its action as an antiprogesterone agent. Vasectomy and tu al ligation are effect ive means of contraception, and oth procedures are reversi le, although not in every case. Infertility Infertility is a pro lem for 15% to 30% of couples. Male infertility may e a result of insuf cient num ers of sperm and/or poor motility. Normally, the ejaculate has a volume of 3 to 4 ml, with approximately 100 milli on sperm per ml. Males with 20 million sperm per ml or 50 million sperm per tota l ejaculate are usually fertile. Infertility in a woman may e due to a num er o f causes, including occluded oviducts (most commonly caused y pelvic in ammatory disease), hostile cervical mucus, immunity to spermatozoa, a sence of ovulation, and others. In vitro fertilization (IVF) of human ova and em ryo transfer is a frequent practice conducted y la oratories throughout the world. Follicle growt h in the ovary is stimulated y administration of gonadotropins. Oocytes are rec overed y laparoscopy from ovarian follicles with an aspirator just efore ovula tion when the oocyte is in the late stages of the rst meiotic division. The egg i s placed in a simple culture medium and sperm are added immediately. Fertilized eggs are monitored to the eight-cell stage and then placed in the uterus to deve lop to term. Fortunately, ecause preimplantation-stage em ryos are resistant to teratogenic insult, the risk of producing malformed offspring y in vitro proce dures is low. A disadvantage of IVF is its low success rate; only 20% of fertili zed ova implant and develop to term. Therefore, to increase chances of a success ful pregnancy, four or ve ova are collected, fertilized, and placed in the uterus . This approach sometimes leads to multiple irths. Another technique, gamete in trafallopian transfer (GIFT), introduces oocytes and sperm into the ampulla of t he fallopian (uterine) tu e, where
42 Part One: General Em ryology fertilization takes place. Development then proceeds in a normal fashion. In a s imilar approach, zygote intrafallopian transfer (ZIFT), fertilized oocytes are p laced in the ampullary region. Both of these methods require patent uterine tu e s. Severe male infertility, in which the ejaculate contains very few live sperm (oligozoospermia) or even no live sperm (azoospermia), can e overcome using int racytoplasmic sperm injection (ICSI). With this technique, a single sperm, which may e o tained from any point in the male reproductive tract, is injected into the cytoplasm of the egg to cause fertilization. This approach offers couples a n alternative to using donor sperm for IVF. The technique carries an increased r isk for fetuses to have Y chromosome deletions ut no other chromosomal a normal ities. Cleavage Once the zygote has reached the two-cell stage, it undergoes a series o f mitotic divisions, increasing the num ers of cells. These cells, which ecome smaller with each cleavage division, are known as lastomeres (Fig. 2.8). Until the eight-cell stage, they form a loosely arranged clump (Fig. 2.9A). However, a fter the third cleavage, lastomeres maximize their contact with each other, for ming a compact all of cells held together y tight junctions (Fig. 2.9B). This process, compaction, segregates inner cells, which communicate extensively y ga p junctions, from outer cells. Approximately 3 days after fertilization, cells o f the compacted em ryo divide again to form a 16-cell morula (mul erry). Inner c ells of the morula constitute the inner cell mass, and surrounding cells compose the outer cell mass. The inner cell mass gives rise to tissues of the Figure 2.8 Development of the zygote from the two-cell stage to the late morula stage. The two-cell stage is reached approximately 30 hours after fertilization; the four-cell stage, at approximately 40 hours; the 12- to 16-cell stage, at ap proximately 3 days; and the late morula stage, at approximately 4 days. During t his period, lastomeres are surrounded y the zona pellucida, which disappears a t the end of the fourth day.
Chapter 2: First Week of Development: Ovulation to Implantation 43 A B Figure 2.9 Scanning electron micrographs of uncompacted (A) and compacted (B) ei ght-cell mouse em ryos. In the uncompacted state, outlines of each lastomere ar e distinct, whereas after compaction cell-cell contacts are maximized and cellul ar outlines are indistinct. em ryo proper, and the outer cell mass forms the tropho last, which later contri utes to the placenta.
Blastocyst Formation A out the time the morula enters the uterine cavity, uid eg ins to penetrate through the zona pellucida into the intercellular spaces of the inner cell mass. Gradually the intercellular spaces ecome con uent, and nally a s ingle cavity, the lastocele, forms (Fig. 2.10, A and B ). At this time, the em ryo is a lastocyst. Cells of the inner cell mass, now called the em ryo last, a re at one pole, and those of the outer cell mass, or tropho last, atten and form the epithelial wall of the lastocyst (Fig. 2.10, A and B). The zona pellucida h as disappeared, allowing implantation to egin. In the human, tropho lastic cell s over the em ryo last pole egin to penetrate etween the epithelial cells of t he uterine mucosa a out the sixth day (Fig. 2.10C ). Attachment and invasion of the tropho last involve integrins, expressed y the tropho last, and the extrace llular matrix molecules laminin and ronectin. Integrin receptors for laminin pro mote attachment, while those for ronectin stimulate migration. These molecules a lso interact along signal transduction pathways to regulate tropho last differen tiation so that implantation is the result of mutual tropho lastic and endometri al action. Hence, y the end of the rst week of development, the human zygote has passed through the morula and lastocyst stages and has egun implantation in t he uterine mucosa.
44 Part One: General Em ryology A Figure 2.10 A. Section of a 107-cell human lastocyst showing inner cell mass an d tropho last cells. B. Schematic representation of a human lastocyst recovered from the uterine cavity at approximately 4.5 days. Blue, inner cell mass or em ryo last; green, tropho last. C. Schematic representation of a lastocyst at the ninth day of development showing tropho last cells at the em ryonic pole of the lastocyst penetrating the uterine mucosa. The human lastocyst egins to penet rate the uterine mucosa y the sixth day of development. CLINICAL CORRELATES A normal Zygotes The exact num er of a normal zygotes formed is unknown ecause they are usually lost within 2 to 3 weeks of fertilization, efore the woman rea lizes she is pregnant, and therefore are not detected. Estimates are that as man y as 50% of pregnancies end in spontaneous a ortion and that
Chapter 2: First Week of Development: Ovulation to Implantation 45 half of these losses are a result of chromosomal a normalities. These a ortions are a natural means of screening em ryos for defects, reducing the incidence of congenital malformations. Without this phenomenon, approximately 12% instead of 2% to 3% of infants would have irth defects. With the use of a com ination of I VF and polymerase chain reaction (PCR), molecular screening of em ryos for genet ic defects is eing conducted. Single lastomeres from early-stage em ryos can e removed and their DNA ampli ed for analysis. As the Human Genome Project provide s more sequencing information and as speci c genes are linked to various syndromes , such procedures will ecome more commonplace. Uterus at Time of Implantation T he wall of the uterus consists of three layers: (a) endometrium or mucosa lining the inside wall; ( ) myometrium, a thick layer of smooth muscle; and (c) perime trium, the peritoneal covering lining the outside wall (Fig. 2.11). From pu erty (1113 years) until menopause (4550 years), the endometrium undergoes changes in a cycle of approximately 28 days under hormonal control y the ovary. During this menstrual cycle, the uterine endometrium passes through three stages, the folli cular or proliferative phase, Preovulatory Figure 2.11 Events during the rst week of human development. 1, Oocyte immediatel y after ovulation. 2, Fertilization, approximately 12 to 24 hours after ovulatio n. 3, Stage of the male and female pronuclei. 4, Spindle of the rst mitotic divis ion. 5, Twocell stage (approximately 30 hours of age). 6, Morula containing 12 t o 16 lastomeres (approximately 3 days of age). 7, Advanced morula stage reachin g the uterine lumen (approximately 4 days of age). 8, Early lastocyst stage (ap proximately 4.5 days of age). The zona pellucida has disappeared. 9, Early phase of implantation ( lastocyst approximately 6 days of age). The ovary shows stage s of transformation etween a primary follicle and a preovulatory follicle as we ll as a corpus luteum. The uterine endometrium is shown in the progestational st age.
46 Part One: General Em ryology Maturation of follicle Ovulation Corpus luteum Corpus luteum of pregnancy Implanted em ryo Implantation d 4 0 Menstrual phase 14 Follicular or proliferative phase 28 Progestational or secretory phase Gravid phase Figure 2.12 Changes in the uterine mucosa correlated with those in the ovary. Im plantation of the lastocyst has caused development of a large corpus luteum of pregnancy. Secretory activity of the endometrium increases gradually as a result of large amounts of progesterone produced y the corpus luteum of pregnancy. the secretory or progestational phase, and the menstrual phase (Figs. 2.11 2.13). The proliferative phase egins at the end of the menstrual phase, is under the in uence of estrogen, and parallels growth of the ovarian follicles. The secretory phase egins approximately 2 to 3 days after ovulation in response to progester one produced y the corpus luteum. If fertilization does not occur, shedding of the endometrium (compact and spongy layers) marks the eginning of the menstrual phase. If fertilization does occur, the endometrium assists in implantation and contri utes to formation of the placenta. At the time of implantation, the muco sa of the uterus is in the secretory phase (Figs. 2.11 and 2.12), during which t ime uterine glands and arteries ecome coiled and the tissue ecomes succulent. As a result, three distinct layers can e recognized in the endometrium: a super c ial compact layer, an intermediate spongy layer, and a thin asal layer (Fig. 2. 12). Normally, the human lastocyst implants in the endometrium along the anteri or or posterior wall of the ody of the uterus, where it ecomes em edded etwee n the openings of the glands (Fig. 2.12). If the oocyte is not fertilized, venul es and sinusoidal spaces gradually ecome packed with lood cells, and an extens ive diapedesis of lood into the tissue is seen. When the menstrual phase egins , lood escapes from super cial arteries, and small pieces of stroma and glands r eak away. During the following 3 or 4 days, the compact and spongy layers are ex pelled from the
egins Compact layer Spongy layer Basal layer Glan
Chapter 2: First Week of Development: Ovulation to Implantation 47 Figure 2.13 Changes in the uterine mucosa (endometrium) and corresponding change s in the ovary during a regular menstrual cycle without fertilization.
Summary With each ovarian cycle, a num er of primary follicles egin to grow, u t usually only one reaches full maturity, and only one oocyte is discharged at o vulation. At ovulation, the oocyte is in metaphase of the second meiotic divisio n and is surrounded y the zona pellucida and some granulosa cells (Fig. 2.4). S weeping action of tu al m riae carries the oocyte into the uterine tu e.
uterus, and the asal layer is the (Fig. 2.13). This layer, which is ies, functions as the regenerative s in the proliferative phase (Fig.
only part of the endometrium that is retained supplied y its own arteries, the asal arter layer in the re uilding of glands and arterie 2.13).
48 Part One: General Em ryology Before spermatozoa can fertilize the oocyte, they must undergo (a) capacitation, during which time a glycoprotein coat and seminal plasma proteins are removed f rom the spermatozoon head, and ( ) the acrosome reaction, during which acrosin a nd trypsin-like su stances are released to penetrate the zona pellucida. During fertilization, the spermatozoon must penetrate (a) the corona radiata, ( ) the z ona pellucida, and (c) the oocyte cell mem rane (Fig. 2.5). As soon as the sperm atocyte has entered the oocyte, (a) the oocyte nishes its second meiotic division and forms the female pronucleus; ( ) the zona pellucida ecomes impenetra le to other spermatozoa; and (c) the head of the sperm separates from the tail, swell s, and forms the male pronucleus (Figs. 2.6 and 2.7). After oth pronuclei have replicated their DNA, paternal and maternal chromosomes intermingle, split longi tudinally, and go through a mitotic division, giving rise to the two-cell stage. The results of fertilization are (a) restoration of the diploid num er of chrom osomes, ( ) determination of chromosomal sex, and (c) initiation of cleavage. Cl eavage is a series of mitotic divisions that results in an increase in cells, l astomeres, which ecome smaller with each division. After three divisions, last omeres undergo compaction to ecome a tightly grouped all of cells with inner a nd outer layers. Compacted lastomeres divide to form a 16-cell morula. As the m orula enters the uterus on the third or fourth day after fertilization, a cavity egins to appear, and the lastocyst forms. The inner cell mass, which is forme d at the time of compaction and will develop into the em ryo proper, is at one p ole of the lastocyst. The outer cell mass, which surrounds the inner cells and the lastocyst cavity, will form the tropho last. The uterus at the time of impl antation is in the secretory phase, and the lastocyst implants in the endometri um along the anterior or posterior wall. If fertilization does not occur, then t he menstrual phase egins and the spongy and compact endometrial layers are shed . The asal layer remains to regenerate the other layers during the next cycle. Pro lems to Solve 1. What are the primary causes of infertility in men and women ? 2. A woman has had several outs of pelvic in ammatory disease and now wants to have children. However, she has een having dif culty ecoming pregnant. What is l ikely to e the pro lem, and what would you suggest? SUGGESTED READING Allen CA, Green DPL: The mammalian acrosome reaction: gateway to sperm fusion with the oocyte? Bioessays 19:241, 1997. Archer DF, Zeleznik AJ, Rockette HE: Ovarian follicular maturation in women: 2. Reversal of estrogen in hi ited ovarian folliculogenesis y human gonadotropin. Fertil Steril 50:555, 19 88. Barratt CLR, Cooke ID: Sperm transport in the human female reproductive trac t: a dynamic interaction. Int J Androl 14:394, 1991.
Chapter 2: First Week of Development: Ovulation to Implantation 49 Boldt J, et al: Car ohydrate involvement in sperm-egg fusion in mice. Biol Repro d 40:887, 1989. Burrows TD, King A, Loke YW: Expression of integrins y human tr opho last and differential adhesion to laminin or ronectin. Hum Reprod 8:475, 19 93. Carr DH: Chromosome studies on selected spontaneous a ortions: polyploidy in man. J Med Genet 8:164, 1971. Chen CM, Sathananthan AH: Early penetration of hu man sperm through the vestments of human egg in vitro. Arch Androl 16:183, 1986. Cowchock S: Autoanti odies and fetal wastage. Am J Reprod Immunol 26:38, 1991. Edwards RG: A decade of in vitro fertilization. Res Reprod 22:1, 1990. Edwards R G, Bavister BD, Steptoe PC: Early stages of fertilization in vitro of human oocy tes matured in vitro. Nature (Lond) 221:632, 1969. Egarter C: The complex nature of egg transport through the oviduct. Am J O stet Gynecol 163:687, 1990. Enders AC, Hendrickx AG, Schlake S: Implantation in the rhesus monkey: initial penetra tion of the endometrium. Am J Anat 167:275, 1983. Gil ert SF: Developmental Biol ogy. Sunderland, MA, Sinauer, 1991. Handyside AH, Kontogianni EH, Hardy K, Winst on RML: Pregnancies from iopsied human preimplantation em ryos sexed y Y-speci c DNA ampli cation. Nature 344:768, 1990. Hertig AT, Rock J, Adams EC: A descriptio n of 34 human ova within the rst 17 days of development. Am J Anat 98:435, 1956. Johnson MH, Everitt BJ: Essential Reproduction. 5th ed. London, Blackwell Scienc e Limited, 2000. Liu J, et al: Analysis of 76 total fertilization failure cycles out of 2732 intracytoplasmic sperm injection cycles. Hum Reprod 10:2630, 1995. Oura C, Toshimori K: Ultrasound studies on the fertilization of mammalian gamete s. Rev Cytol 122:105, 1990. Pedersen RA, We K, Balakier H: Origin of the inner c ell mass in mouse em ryos: cell lineage analysis y microinjection. Dev Biol 117 :581, 1986. Reproduction (entire issue). J NIH Res 9:1997. Scott RT, Hodgen GD: The ovarian follicle: life cycle of a pelvic clock. Clin O stet Gynecol 33:551, 1990. Wasserman PM: Fertilization in mammals. Sci Am 259:78, 1988. Wolf DP, Quig ley MM (eds): Human in Vitro Fertilization and Transfer. New York, Plenum, 1984. Yen SC, Jaffe RB (eds): Reproductive Endocrinology: Physiology, Pathophysiology , and Clinical Management. 2nd ed. Philadelphia, WB Saunders, 1986.
chapter 3 Second Week of Development: Bilaminar Germ Disc This chapter gives a day- y-day account of the major events of the second week o f development. However, em ryos of the same fertilization age do not necessarily develop at the same rate. Indeed, considera le differences in rate of growth ha ve een found even at these early stages of development. Day 8 At the eighth day of development, the lastocyst is partially em edded in the endometrial stroma. In the area over the em ryo last, the tropho last has di fferentiated into two layers: (a) an inner layer of mononucleated cells, the cyt otropho last, and ( ) an outer multinucleated zone without distinct cell oundar ies, the syncytiotropho last (Figs. 3.1 and 3.2). Mitotic gures are found in the cytotropho last ut not in the syncytiotropho last. Thus, cells in the cytotroph o last divide and migrate into the syncytiotropho last, where they fuse and lose their individual cell mem ranes. Cells of the inner cell mass or em ryo last al so differentiate into two layers: (a) a layer of small cu oidal cells adjacent t o the lastocyst cavity, known as the hypo last layer, and ( ) a layer of high c olumnar cells adjacent to the amniotic cavity, the epi last layer (Figs. 3.1 and 3.2). Together, the layers form a at disc. At the same time, a small cavity appe ars within the epi last. This cavity enlarges to ecome the 51
52 Part One: General Em ryology Figure 3.1 A 7.5-day human lastocyst, partially em edded in the endometrial str oma. The tropho last consists of an inner layer with mononuclear cells, the cyto tropho last, and an outer layer without distinct cell oundaries, the syncytiotr opho last. The em ryo last is formed y the epi last and hypo last layers. The a mniotic cavity appears as a small cleft. Figure 3.2 Section of a 7.5-day human lastocyst (100). Note the multinucleated a ppearance of the syncytiotropho last, large cells of the cytotropho last, and sl it-like amniotic cavity. amniotic cavity. Epi last cells adjacent to the cytotropho last are called amnio lasts; together with the rest of the epi last, they line the amniotic cavity (F igs. 3.1 and 3.3). The endometrial stroma adjacent to the implantation site is e dematous and highly vascular. The large, tortuous glands secrete a undant glycog en and mucus.
Chapter 3: Second Week of Development: Bilaminar Germ Disc 53 Figure 3.3 A 9-day human lastocyst. The syncytiotropho last shows a large num e r of lacunae. Flat cells form the exocoelomic mem rane. The ilaminar disc consi sts of a layer of columnar epi last cells and a layer of cu oidal hypo last cell s. The original surface defect is closed y a rin coagulum. Day 9 The lastocyst is more deeply em edded in the endometrium, and the penetra tion defect in the surface epithelium is closed y a rin coagulum (Fig. 3.3). Th e tropho last shows considera le progress in development, particularly at the em ryonic pole, where vacuoles appear in the syncytium. When these vacuoles fuse, they form large lacunae, and this phase of tropho last development is thus known as the lacunar stage (Fig. 3.3). At the a em ryonic pole, meanwhile, attened cel ls pro a ly originating from the hypo last form a thin mem rane, the exocoelomic (Heusers) mem rane, that lines the inner surface of the cytotropho last (Fig. 3. 3). This mem rane, together with the hypo last, forms the lining of the exocoelo mic cavity, or primitive yolk sac. Days 11 and 12 By the 11th to 12th day of dev elopment, the lastocyst is completely em edded in the endometrial stroma, and t he surface epithelium almost entirely covers
54 Part One: General Em ryology Figure 3.4 Human lastocyst of approximately 12 days. The tropho lastic lacunae at the em ryonic pole are in open connection with maternal sinusoids in the endo metrial stroma. Extraem ryonic mesoderm proliferates and lls the space etween th e exocoelomic mem rane and the inner aspect of the tropho last. the original defect in the uterine wall (Figs. 3.4 and 3.5). The lastocyst now produces a slight protrusion into the lumen of the uterus. The tropho last is ch aracterized y lacunar spaces in the syncytium that form an intercommunicating n etwork. This network is particularly evident at the em ryonic pole; at the a em ryonic pole, the tropho last still consists mainly of cytotropho lastic cells (F igs. 3.4 and 3.5). Concurrently, cells of the syncytiotropho last penetrate deep er into the stroma and erode the endothelial lining of the maternal capillaries. These capillaries, which are congested and dilated, are known as sinusoids. The syncytial lacunae ecome continuous with the sinusoids and maternal lood enter s the lacunar system (Fig. 3.4). As the tropho last continues to erode more and more sinusoids, maternal lood egins to ow through the tropho lastic system, est a lishing the uteroplacental circulation. In the meantime, a new population of c ells appears etween the inner surface of the cytotropho last and the outer surf ace of the exocoelomic
Chapter 3: Second Week of Development: Bilaminar Germ Disc 55 Figure 3.5 Fully implanted 12-day human lastocyst (100). Note maternal lood cel ls in the lacunae, the exocoelomic mem rane lining the primitive yolk sac, and t he hypo last and epi last. cavity. These cells, derived from yolk sac cells, form a ne, loose connective tis sue, the extraem ryonic mesoderm, which eventually lls all of the space etween t he tropho last externally and the amnion and exocoelomic mem rane internally (Fi gs. 3.4 and 3.5). Soon, large cavities develop in the extraem ryonic mesoderm, a nd when these ecome con uent, they form a new space known as the extraem ryonic c oelom, or chorionic cavity (Fig. 3.4). This space surrounds the primitive yolk s ac and amniotic cavity except where the germ disc is connected to the tropho las t y the connecting stalk (Fig. 3.6). The extraem ryonic mesoderm lining the cyt otropho last and amnion is called the extraem ryonic somatopleuric mesoderm; the lining covering the yolk sac is known as the extraem ryonic splanchnopleuric me soderm (Fig. 3.4). Growth of the ilaminar disc is relatively slow compared with that of the tropho last; consequently, the disc remains very small (0.10.2 mm). Cells of the endometrium, meanwhile, ecome polyhedral and loaded with glycogen and lipids; intercellular spaces are lled with extravasate, and the tissue is ede matous. These changes, known as the decidua reaction, at rst are con ned to the
56 Part One: General Em ryology Figure 3.6 A 13-day human lastocyst. Tropho lastic lacunae are present at the e m ryonic as well as the a em ryonic pole, and the uteroplacental circulation has egun. Note the primary villi and the extraem ryonic coelom or chorionic cavity . The secondary yolk sac is entirely lined with endoderm. area immediately surrounding the implantation site ut soon occur throughout the endometrium. Day 13 By the 13th day of development, the surface defect in the endometrium has usually healed. Occasionally, however, leeding occurs at the implantation site as a result of increased lood ow into the lacunar spaces. Because this leeding occurs near the 28th day of the menstrual cycle, it may e confused with
Chapter 3: Second Week of Development: Bilaminar Germ Disc 57 Figure 3.7 Section through the implantation site of a 13-day em ryo. Note the am niotic cavity, yolk sac, and exocoelomic cyst in the chorionic cavity. Most of t he lacunae are lled with lood. normal menstrual leeding and, therefore, cause inaccuracy in determining the ex pected delivery date. The tropho last is characterized y villous structures. Ce lls of the cytotropho last proliferate locally and penetrate into the syncytiotr opho last, forming cellular columns surrounded y syncytium. Cellular columns wi th the syncytial covering are known as primary villi (Figs. 3.6 and 3.7) (see Ch apter 4). In the meantime, the hypo last produces additional cells that migrate along the inside of the exocoelomic mem rane (Fig. 3.4). These cells proliferate and gradually form a new cavity within the exocoelomic cavity. This new cavity is known as the secondary yolk sac or de nitive yolk sac (Figs. 3.6 and 3.7). This yolk sac is much smaller than the original exocoelomic cavity, or primitive yol k sac. During its formation, large portions of the exocoelomic cavity are pinche d off. These portions are represented y exocoelomic cysts, which are often foun d in the extraem ryonic coelom or chorionic cavity (Figs. 3.6 and 3.7). Meanwhil e, the extraem ryonic coelom expands and forms a large cavity, the chorionic cav ity. The extraem ryonic mesoderm lining the inside of the cytotropho last is the n known as the chorionic plate. The only place where extraem ryonic mesoderm tra verses the chorionic cavity is in the connecting stalk (Fig. 3.6). With developm ent of lood vessels, the stalk ecomes the um ilical cord.
58 Part One: General Em ryology CLINICAL CORRELATES A normal Implantation The syncytiotropho last is responsi le for hormone product ion (see Chapter 6), including human chorionic gonadotropin (hCG). By the end of the second week, quantities of this hormone are suf cient to e detected y radio immunoassays, which serve as the asis for pregnancy testing. Because 50% of the implanting em ryos genome is derived from the father, it is a foreign ody that potentially should e rejected y the maternal system. Recent evidence suggests that a com ination of factors protects the conceptus, including production of im munosuppressive cytokines and proteins and the expression of an unusual major hi stocompati ility complex class IB molecule (HLA-G) that locks recognition of th e conceptus as foreign tissue. If the mother has autoimmune disease, for example systemic lupus erythematosus, anti odies generated y the disease may attack th e conceptus and reject it. A normal implantation sites sometimes occur even with in the uterus. Normally the human lastocyst implants along the anterior or post erior wall of the ody of the uterus. Occasionally the lastocyst implants close to the internal opening os (opening) (Fig. 3.8) of the cervix, so that later in development, Intestinal loop Mesentery Body of uterus 4 1 3 Uterine tu e 5 Internal os of uterus 2 6 Ampulla Fim riae Figure 3.8 A normal implantation sites of the lastocyst. 1, implantation in the a dominal cavity. The ovum most frequently implants in the rectouterine cavity (Douglas pouch) ut may implant at any place covered y peritoneum. 2, implantati on in the ampullary region of the tu e. 3, tu al implantation. 4, interstitial i mplantation, that is, in the narrow portion of the uterine tu e. 5, implantation in the region of the internal os, frequently resulting in placenta previa. 6, o varian implantation.
Chapter 3: Second Week of Development: Bilaminar Germ Disc 59 Figure 3.9 Tu al pregnancy. Em ryo is approximately 2 months old and is a out to escape through a rupture in the tu al wall. the placenta ridges the opening (placenta previa) and causes severe, even lifethreatening leeding in the second part of pregnancy and during delivery. Occasi onally, implantation takes place outside the uterus, resulting in extrauterine p regnancy, or ectopic pregnancy. Ectopic pregnancies may occur at any place in th e a dominal cavity, ovary, or uterine tu e (Fig. 3.8). However, 95% of ectopic p regnancies occur in the uterine tu e, and most of these are in the ampulla (Fig. 3.9). In the a dominal cavity, the lastocyst most frequently attaches itself t o the peritoneal lining of the rectouterine cavity, or Douglas pouch (Fig. 3.10). The lastocyst may also attach itself to the peritoneal covering of the intesti nal tract or to the omentum. Sometimes the lastocyst develops in the ovary prop er, causing a primary ovarian pregnancy. In most ectopic pregnancies, the em ryo dies a out the second month of gestation, causing severe hemorrhaging and a dom inal pain in the mother. A normal lastocysts are common. For example, in a seri es of 26 implanted lastocysts varying in age from 7.5 to 17 days recovered from patients of normal fertility, nine (34.6%) were a normal. Some consisted of syn cytium only; others showed varying degrees of tropho lastic hypoplasia. In two, the em ryo last was a sent, and in some, the germ disc showed an a normal orient ation. It is likely that most a normal lastocysts would not have produced any s ign of pregnancy ecause their tropho last was so inferior that the corpus luteu m could not have persisted. These em ryos pro a ly would have een
60 Part One: General Em ryology Figure 3.10 Midline section of ladder, uterus, and rectum to show an a dominal pregnancy in the rectouterine (Douglas) pouch. a orted with the next menstrual ow, and therefore, pregnancy would not have een detected. In some cases, however, the tropho last develops and forms placental m em ranes, although little or no em ryonic tissue is present. Such a condition is known as a hydatidiform mole. Moles secrete high levels of hCG and may produce enign or malignant (invasive mole, choriocarcinoma) tumors. Genetic analysis of hydatidiform moles indicates that although male and female pronuclei may e gen etically equivalent, they may e different functionally. This evidence is derive d from the fact that while cells of moles are diploid, their entire genome is pa ternal. Thus, most moles arise from fertilization of an oocyte lacking a nucleus followed y duplication of the male chromosomes to restore the diploid num er. These results also suggest that paternal genes regulate most of the development of the tropho last, since in moles, this tissue differentiates even in the a sen ce of a female pronucleus. Other examples of functional differences in maternal and paternal genes are provided y the o servation that certain genetic diseases depend on whether the defective or missing gene is inherited from the father or the mother. For example, inheritance of a deletion on chromosome 15 from a fath er produces Prader-Willi syndrome, whereas inheritance of the same defect from t he mother results in Angelman syndrome. This phenomenon, in which
Chapter 3: Second Week of Development: Bilaminar Germ Disc 61 there is differential modi cation and/or expression of homologous alleles or chrom osome regions, depending on the parent from whom the genetic material is derived , is known as genomic imprinting. Imprinting involves autosomes and sex chromoso mes (in all female mammals, one X chromosome is inactivated in somatic cells and forms a chromatin-positive ody [Barr ody]) and is modulated y deoxyri onucle ic acid (DNA) methylation. Certain diseases, such as Huntingtons chorea, neuro rom atosis, familial cancer disorders (Wilms tumors, familial retino lastoma), and my otonic dystrophy, also involve imprinting. Fragile X syndrome, the leading cause of inherited mental retardation, may e another example of a condition ased on imprinting (see Chapter 1). Preimplantation and postimplantation reproductive f ailure occurs often. Even in some fertile women under optimal conditions for pre gnancy, 15% of oocytes are not fertilized, and 10% to 15% start cleavage ut fai l to implant. Of the 70% to 75% that implant, only 58% survive until the second week, and 16% of those are a normal. Hence, when the rst expected menstruation is missed, only 42% of the eggs exposed to sperm are surviving. Of this percentage , a num er will e a orted during su sequent weeks and a num er will e a normal at the time of irth. Summary At the eginning of the second week, the lastocyst is partially em edde d in the endometrial stroma. The tropho last differentiates into (a) an inner, a ctively proliferating layer, the cytotropho last, and ( ) an outer layer, the sy ncytiotropho last, which erodes maternal tissues (Fig. 3.1). By day 9, lacunae d evelop in the syncytiotropho last. Su sequently, maternal sinusoids are eroded y the syncytiotropho last, maternal lood enters the lacunar network, and y the end of the second week, a primitive uteroplacental circulation egins (Fig. 3.6 ). The cytotropho last, meanwhile, forms cellular columns penetrating into and s urrounded y the syncytium. These columns are primary villi. By the end of the s econd week, the lastocyst is completely em edded, and the surface defect in the mucosa has healed (Fig. 3.6). The inner cell mass or em ryo last, meanwhile, di fferentiates into (a) the epi last and ( ) the hypo last, together forming a il aminar disc (Fig. 3.1). Epi last cells give rise to amnio lasts that line the am niotic cavity superior to the epi last layer. Endoderm cells are continuous with the exocoelomic mem rane, and together they surround the primitive yolk sac (Fi g. 3.4). By the end of the second week, extraem ryonic mesoderm lls the space et ween the tropho last and the amnion and exocoelomic mem rane internally. When va cuoles develop in this tissue, the extraem ryonic coelom or chorionic cavity for ms (Fig. 3.6). Extraem ryonic mesoderm lining the cytotropho last and
62 Part One: General Em ryology amnion is extraem ryonic somatopleuric mesoderm; the lining surrounding the yolk sac is extraem ryonic splanchnopleuric mesoderm (Fig. 3.6). The second week of development is known as the week of twos: The tropho last differentiates into tw o layers, the cytotropho last and syncytiotropho last. The em ryo last forms two layers, the epi last and hypo last. The extraem ryonic mesoderm splits into two layers, the somatopleure and splanchnopleure. And two cavities, the amniotic an d yolk sac cavities, form. Implantation occurs at the end of the rst week. Tropho last cells invade the epithelium and underlying endometrial stroma with the hel p of proteolytic enzymes. Implantation may also occur outside the uterus, such a s in the rectouterine pouch, on the mesentery, in the uterine tu e, or in the ov ary (ectopic pregnancies). Pro lems to Solve 1. The second week of development is known as the week of twos . Formation of what structures support this statement? 2. During implantation, t he tropho last is invading maternal tissues, and ecause it contains approximate ly 50% paternal genes, it is a foreign ody. Why is the conceptus not rejected y an immunologic response from the mothers system? 3. A woman who elieves she is pregnant complains of edema and vaginal leeding. Examination reveals high plas ma hCG concentrations and placental tissue, ut no evidence of an em ryo. How wo uld you explain this condition? 4. A young woman who has missed two menstrual pe riods complains of intense a dominal pain. What might an initial diagnosis e, a nd how would you con rm it? SUGGESTED READING Aplin JD: Implantation, tropho last differentiation and hemoch orial placentation: mechanistic evidence in vivo and in vitro. J Cell Sci 99:681 , 1991. Bianchi DW, Wilkins-Haug LE, Enders AC, Hay ED: Origin of extraem ryonic mesoderm in experimental animals: relevance to chorionic mosaicism in humans. A m J Med Genet 46:542, 1993. Cattanack BM, Beechey CV: Autosomal and X-chromosome imprinting. Dev Suppl 63, 1990. Enders AC, King BF: Formation and differentiati on of extraem ryonic mesoderm in the Rhesus monkey. Am J Anat 181:327, 1988. End ers AC, King BF: Development of the human yolk sac. In Nogales FF (ed): The Huma n Yolk Sac and Yolk Sac Tumors. Berlin, Springer Verlag, 1993. Enders AC, Schlaf ke S, Hendrickx A: Differentiation of the em ryonic disc, amnion, and yolk sac i n the rhesus monkey. Am J Anat 177:161, 1986. Hertig AT, Rock J, Adams EC: A des cription of 34 human ova within the rst 17 days of development. Am J Anat 98:435, 1956. Holliday R: Genomic imprinting and allelic exclusion. Dev Suppl 125, 1990 . McMaster MT, et al: Human placental HLA-G expression is restricted to differen tiated cytotropho lasts. J Immunol 154:3771, 1995.
Chapter 3: Second Week of Development: Bilaminar Germ Disc 63 Monk M, Grant M: Preferential X-chromosome inactivation, DNA methylation and imp rinting. Dev Suppl 55, 1990. Roth I, et al: Human placental cytotropho lasts pro duce the immunosuppressive cytokine interleukin 10. J Exp Med 184:539, 1996. Ru in GL: Ectopic pregnancy in the United States: 1970 through 1978. JAMA 249:1725, 1983.
chapter 4 Third Week of Development: Trilaminar Germ Disc Gastrulation: Formation of Em ryonic Mesoderm and Endoderm The most characterist ic event occurring during the third week of gestation is gastrulation, the proce ss that esta lishes all three germ layers (ectoderm, mesoderm, and endoderm) in the em ryo. Gastrulation egins with formation of the primitive streak on the su rface of the epi last (Figs. 4.14.3A). Initially, the streak is vaguely de ned (Fig . 4.1), ut in a 15- to 16-day em ryo, it is clearly visi le as a narrow groove with slightly ulging regions on either side (Fig. 4.2). The cephalic end of the streak, the primitive node, consists of a slightly elevated area surrounding th e small primitive pit (Fig. 4.3). Cells of the epi last migrate toward the primi tive streak (Fig. 4.3). Upon arrival in the region of the streak, they ecome ask -shaped, detach from the epi last, and slip eneath it (Fig. 4.3, BD). This inwar d movement is known as invagination. Once the cells have invaginated, some displ ace the hypo last, creating the em ryonic endoderm, and others come to lie etwe en the epi last and newly created endoderm to form mesoderm. Cells remaining in the epi last then form ectoderm. Thus, the epi last, through the process of gast rulation, is the source of all of the germ layers (Fig. 4.3B), and cells in thes e layers will give rise to all of the tissues and organs in the em ryo. As more and more cells move etween the epi last and hypo last layers, they egin to spr ead laterally and cephalad (Fig. 4.3). Gradually, 65
66 Part One: General Em ryology Amniotic cavity Epi last Hypo last Cytotropho last Syncytiotropho last Definitive yolk sac Extraem ryonic mesoderm A Buccopharyngeal mem rane Cut edge of amnion Primitive streak Wall of yolk sac Hypo last Epi last B Figure 4.1 A. Implantation site at the end of the second week. B. Representative view of the germ disc at the end of the second week of development. The amnioti c cavity has een opened to permit a view on the dorsal side of the epi last. Th e hypo last and epi last are in contact with each other and the primitive streak forms a shallow groove in the caudal region of the em ryo. they migrate eyond the margin of the disc and esta lish contact with the extrae m ryonic mesoderm covering the yolk sac and amnion. In the cephalic direction, t hey pass on each side of the prechordal plate. The prechordal plate itself forms etween the tip of the notochord and the uccopharyngeal mem rane and is derive d from some of the rst cells that migrate through the node in a cephalic directio n. Later, the prechordal plate will e important for
Chapter 4: Third Week of Development: Trilaminar Germ Disc 67 Figure 4.2 A. Dorsal aspect of an 18-day em ryo. The em ryo has a pear-shaped ap pearance and shows the primitive streak and node at its caudal end. B. Photograp h of an 18-day human em ryo, dorsal view. Note the primitive node and the notoch ord extending cranially. The yolk sac has a somewhat mottled appearance. The len gth of the em ryo is 1.25 mm and the greatest width is 0.68 mm. induction of the fore rain (Figs. 4.3A and 4.4A). The uccopharyngeal mem rane a t the cranial end of the disc consists of a small region of tightly adherent ect oderm and endoderm cells that represents the future opening of the oral cavity. Formation of the Notochord Prenotochordal cells invaginating in the primitive pi t move forward cephalad until they reach the prechordal plate (Fig. 4.4). These prenotochordal cells ecome intercalated in the hypo last so that, for a short t ime, the midline of the em ryo consists of two cell layers that form the notocho rdal plate (Fig. 4.4, B and C ). As the hypo last is replaced y endoderm cells moving in at the streak, cells of the notochordal plate proliferate and detach f rom the endoderm. They then form a solid cord of cells, the de nitive notochord (F ig. 4.4, D and E ), which underlies the neural tu e and serves as the asis for the axial skeleton. Because elongation of the notochord is a dynamic process, th e cranial end forms rst, and caudal regions are added as the primitive streak ass umes a more caudal position. The notochord and prenotochordal cells extend crani ally to the prechordal plate (an area just caudal to the uccopharyngeal mem ran e) and caudally to the primitive pit. At the point where the pit forms an indent ation
68 Part One: General Em ryology Buccopharyngeal mem rane Cut edge of amnion Prenotochordal cells Primitive node Primitive streak A Primitive node Cloacal mem rane Primitive streak Epi last Amnio lasts Yolk sac B Invaginating mesoderm cells Hypo last Figure 4.3 A. Dorsal side of the germ disc from a 16-day em ryo indicating the m ovement of surface epi last cells (solid lack lines) through the primitive stre ak and node and the su sequent migration of cells etween the hypo last and epi last ( roken lines). B. Cross section through the cranial region of the streak a t 15 days showing invagination of epi last cells. The rst cells to move inward di splace the hypo last to create the de nitive endoderm. Once de nitive endoderm is es ta lished, inwardly moving epi last forms mesoderm. C. Scanning electron microgr aph through the primitive streak of a mouse em ryo showing migration of epi last (e ) cells. The node region appears as a shallow pit (arrow). D. Higher magni cat ion of the section in C. in the epi last, the neurenteric canal temporarily connects the amniotic and yol k sac cavities (Fig. 4.4A). The cloacal mem rane is formed at the caudal end of the em ryonic disc (Fig. 4.3A). This mem rane, which is similar in structure to the uccopharyngeal mem rane, consists of tightly adherent ectoderm and endoderm cells with no intervening mesoderm. When the cloacal mem rane appears, the post erior
Chapter 4: Third Week of Development: Trilaminar Germ Disc 69 C D D Figure 4.3Continued.
70 Part One: General Em ryology Primitive pit and neurenteric canal Connecting stalk Amnion Ectoderm B C Allantois Wall of yolk sac Notochord Prechordal plate Cloacal plate (mem rane) A Notochordal plate C Intraem ryonic mesoderm Endoderm Intraem ryonic mesoderm Endoderm Extraem ryonic mesoderm E Notochord Figure 4.4 Schematic views and scanning electron micrographs illustrating format ion of the notochord, where y prenotochordal cells migrate through the primitive streak, ecome intercalated in the endoderm to form the notochordal plate, and n ally detach from the endoderm to form the de nitive notochord. Because these event s occur in a cranial-to-caudal sequence, portions of the de nitive notochord are e sta lished in the head region rst. A. Drawing of a sagittal section through a 17day em ryo. The most cranial portion of the de nitive notochord has formed, while prenotochordal cells caudal to this region are intercalated into the endoderm as the notochordal plate. B. Scanning electron micrograph of a mouse em ryo showin g the region of the uccopharyngeal
Chapter 4: Third Week of Development: Trilaminar Germ Disc 71 B D F mem rane (arrows). Extending posteriorly is the prenotochordal plate (arrowheads ). C. Schematic cross section through the region of the notochordal plate. Soon the notochordal plate will detach from the endoderm to form the de nitive notochor d. D. Scanning electron micrograph of a mouse em ryo showing detachment of the n otochordal plate from the endoderm. E. Schematic view showing the de nitive notoch ord. F. Scanning electron micrograph of a mouse em ryo showing the de nitive notoc hord (arrows) in close approximation to the neural tu e (NT).
72 Part One: General Em ryology wall of the yolk sac forms a small diverticulum that extends into the connecting stalk. This diverticulum, the allantoenteric diverticulum, or allantois, appear s around the 16th day of development (Fig. 4.4A). Although in some lower verte r ates the allantois serves as a reservoir for excretion products of the renal sys tem, in humans it remains rudimentary ut may e involved in a normalities of l adder development (see Chapter 14). Esta lishment of the Body Axes Esta lishment of the ody axes, anteroposterior, dorsoventral, and left-right, takes place efore and during the period of gastru lation. The anteroposterior axis is signaled y cells at the anterior (cranial) margin of the em ryonic disc. This area, the anterior visceral endoderm (AVE), e xpresses genes essential for head formation, including the transcription factors OTX2, LIM1, and HESX1 and the secreted factor cer erus. These genes esta lish t he cranial end of the em ryo efore gastrulation. The primitive streak itself is initiated and maintained y expression of Nodal, a mem er of the transforming g rowth factor (TGF-) family (Fig. 4.5). Once the streak is formed, a num er of gen es regulate formation of dorsal and ventral mesoderm and head and tail structure s. Another mem er of the TGF- family, one morphogenetic protein-4 (BMP4) is secr eted throughout the em ryonic disc (Fig. 4.5). In the presence of this protein a nd ro last growth factor (FGF), mesoderm will e ventralized to contri ute to ki dneys (intermediate mesoderm), lood, and ody wall mesoderm (lateral plate meso derm). In fact, all mesoderm would e ventralized if the activity of BMP-4 were not locked y other genes expressed in the node. For this reason, the node is t he organizer. It was given that designation y Goosecoid, chordin, noggin, follistatin, nodal AVE Figure 4.5 Sagittal section through the node and primitive streak showing the ex pression pattern of genes regulating the craniocaudal and dorsoventral axes. Cel ls at the prospective cranial end of the em ryo in the anterior visceral endoder m (AVE) express the transcription factors OTX2, LIM1, and HESX1 and the secreted factor cer erus that contri ute to head development and esta lish the cephalic region. Once the streak is formed and gastrulation is progressing, one morphoge netic protein (BMP-4; hatched areas), secreted throughout the ilaminar disc, ac ts with FGF to ventralize mesoderm into intermediate and lateral plate structure s. Goosecoid regulates chordin expression, and this gene product, together with noggin and follistatin, antagonizes the activity of BMP-4, dorsalizing mesoderm into notochord and paraxial mesoderm for the head region. Later, expression of t he Brachyury (T) gene antagonizes BMP-4 to dorsalize mesoderm in caudal regions of the em ryo.
Chapter 4: Third Week of Development: Trilaminar Germ Disc 73 Figure 4.6 Node and primitive streak region removed from a mouse em ryo showing expression of nodal using in situ hy ridization. Nodal is expressed in the node and initiates and maintains the primitive streak. Hans Spemann, who rst descri ed this activity in the dorsal lip of the lastopore , a structure analogous to the node, in Xenopus em ryos. Thus, chordin (activate d y the transcription factor Goosecoid ), noggin, and follistatin antagonize th e activity of BMP-4. As a result, cranial mesoderm is dorsalized into notochord, somites, and somitomeres (Fig. 4.5). Later, these three genes are expressed in the notochord and are important in neural induction in the cranial region. As me ntioned, Nodal is involved in initiating and maintaining the primitive streak (F ig. 4.6). Similarly, HNF-3 maintains the node and later induces regional speci city in the fore rain and mid rain areas. Without HNF-3, em ryos fail to gastrulate p roperly and lack fore rain and mid rain structures. As mentioned previously, Goo secoid activates inhi itors of BMP-4 and contri utes to regulation of head devel opment. Overexpression or underexpression of this gene results in severe malform ations of the head region, including duplications (Fig. 4.7). Regulation of dors al mesoderm formation in mid and caudal regions of the em ryo is controlled y t he Brachyury (T) gene (Fig. 4.8). Thus, mesoderm formation in these regions depe nds on this gene product, and its a sence results in shortening of the em ryonic axis (caudal dysgenesis; see p. 80). The degree of shortening depends upon the time at which the protein ecomes de cient. Left-right sidedness, also esta lished early in development, is orchestrated y a cascade of genes. When the primitive streak appears, ro last growth factor 8 (FGF-8) is secreted y cells in the nod e and primitive streak and
74 Part One: General Em ryology Figure 4.7 Two-headed tadpole produced y injecting additional Goosecoid mRNA in to frog eggs. Similar results can e o tained y transplanting an additional nod e region to eggs. Goosecoid is normally expressed in the node and is a major reg ulator of head development. Figure 4.8 Expression pattern of the Brachyury (T) gene in the notochord and pri mitive streak of a mouse em ryo. This gene antagonizes the activity of one morp hogenetic protein (BMP-4) in the hind rain and spinal cord regions and dorsalize s mesoderm to form notochord, somitomeres, and somites (paraxial mesoderm). (Mou se em ryos are dorsi exed into a cup shape during the period of gastrulation and n eurulation.) nf, neural fold; hp, head process; ps, primitive streak; al, allant ois.
Chapter 4: Third Week of Development: Trilaminar Germ Disc 75 Buccopharyngeal mem rane FGF8 Nodal Lefty2 Nodal Lefty 1 Node FGF8 Node (FGF8) Nodal NKX3.2 PITX2 Notocho rd (SHH, T) Neural tu e A Cloacal mem rane B Figure 4.9 Dorsal views of the germ disc showing gene expression patterns respon si le for esta lishing the left-right ody axis. A. Fi ro last growth factor 8 ( FGF-8), secreted y the node and primitive streak, esta lishes expression of Nod al, a mem er of the transforming growth factor (TGF-) superfamily, on the left si de near the node. B. Later, as the neural plate is induced, FGF-8 induces expres sion of Nodal and Lefty-2 in the lateral plate mesoderm, whereas Lefty-1 is expr essed on the left side of the ventral aspect of the neural tu e. Products from t he Brachyury (T) gene, expressed in the notochord, also participate in induction of these three genes. In turn, expression of Nodal and Lefty-2 regulates expres sion of the transcription factor PITX 2, which, through further downstream effec tors, esta lishes left sidedness. Sonic hedgehog (SHH), expressed in the notocho rd, may serve as a midline arrier and also repress expression of left-sided gen es on the right. NKX 3.2 may regulate downstream genes important for esta lishin g right sidedness. induces expression of Nodal ut only on the left side of the em ryo (Fig. 4.9A). Later, as the neural plate is induced, FGF-8 maintains Nodal expression in the lateral plate mesoderm (Fig. 4.10), as well as Lefty-2, and oth of these genes upregulate PITX2, a transcription factor responsi le for esta lishing left sided ness (Fig. 4.9B). Simultaneously, Lefty-1 is expressed on the left side of the oo r plate of the neural tu e and may act as a arrier to prevent left-sided signal s from crossing over. Sonic hedgehog (SHH ) may also function in this role as we ll as serving as a repressor for left sided gene expression on the right. The Br achyury(T) gene, another growth factor secreted y the notochord, is also essent ial for expression of Nodal, Lefty-1, and Lefty-2 (Fig. 4.9B ). Genes regulating right-sided development are not as well de ned, although expression of the
76 Part One: General Em ryology A B Figure 4.10 Expression pattern of the gene nodal in a mouse showing that it is r estricted to the left side of the ody (A) in the lateral plate mesoderm (B). No dal, together with Lefty, regulates downstream genes to determine left-right asy mmetry. transcription factor NKX 3.2 is restricted to the right lateral plate mesoderm a nd pro a ly regulates effector genes responsi le for esta lishing the right side . Why the cascade is initiated on the left remains a mystery, ut the reason may involve cilia on cells in the node that eat to create a gradient of FGF-8 towa rd the left. Indeed, a normalities in cilia-related proteins result in lateralit y defects in mice and some humans with these defects have a normal ciliary funct ion (see p. 79). Fate Map Esta lished During Gastrulation Regions of the epi last that migrate an d ingress through the primitive streak have een mapped and their ultimate fates determined (Fig. 4.11). For example, cells that ingress through the cranial reg ion of the node ecome notochord; those migrating at the lateral edges of the no de and from the cranial end of the streak ecome paraxial mesoderm; cells migrat ing through the midstreak region ecome intermediate mesoderm; those migrating t hrough the more caudal part of the streak form lateral plate mesoderm; and cells migrating through the caudal-most part of the streak contri ute to extraem ryon ic mesoderm (the other source of this tissue is the primitive yolk sac [hypo las t]; see p. 55).
Chapter 4: Third Week of Development: Trilaminar Germ Disc 77 Figure 4.11 Dorsal view of the germ disc showing the primitive streak and a fate map for epi last cells. Speci c regions of the epi last migrate through different parts of the node and streak to form mesoderm. Thus, cells migrating at the cra nial-most part of the node will form the notochord (n); those migrating more pos teriorly through the node and cranial-most aspect of the streak will form paraxi al mesoderm (pm; somitomeres and somites); those migrating through the next port ion of the streak will form intermediate mesoderm (im; urogenital system); those migrating through the more caudal part of the streak will form lateral plate me soderm (lpm; ody wall); and those migrating through the most caudal part will c ontri ute to extraem ryonic mesoderm (eem; chorion). Growth of the Em ryonic Disc The em ryonic disc, initially at and almost round, g radually ecomes elongated, with a road cephalic and a narrow caudal end (Fig. 4.2). Expansion of the em ryonic disc occurs mainly in the cephalic region; the region of the primitive streak remains more or less the same size. Growth and el ongation of the cephalic part of the disc are caused y a continuous migration o f cells from the primitive streak region in a cephalic direction. Invagination o f surface cells in the primitive streak and their su sequent migration forward a nd laterally continues until the end of the fourth week. At that stage, the prim itive streak shows regressive changes, rapidly shrinks, and soon disappears. Tha t the primitive streak at the caudal end of the disc continues to supply new cel ls until the end of the fourth week has an important earing on development of t he em ryo. In the cephalic part, germ layers egin their speci c differentiation y the middle of the third week (Fig. 4.12), whereas in the caudal
78 Part One: General Em ryology Figure 4.12 A. Scanning electron micrograph (dorsal view) of a mouse em ryo (equ ivalent to human at approximately 18 days), showing initial elevation of the cra nial neural folds (CF ). The primitive streak lies farther caudally and is o scu red from view. B. Transverse section through the em ryo shown in A (see line of section). Note three germ layers; pseudostrati ed columnar cells of the neuroectod erm (Ec), attened endoderm (En), and mesoderm (Me) sandwiched etween these two l ayers. Asterisks, mitotic cells.
Chapter 4: Third Week of Development: Trilaminar Germ Disc 79 part, differentiation egins y the end of the fourth week. Thus gastrulation, o r formation of the germ layers, continues in caudal segments while cranial struc tures are differentiating, causing the em ryo to develop cephalocaudally (Fig. 4 .12). CLINICAL CORRELATES Teratogenesis Associated With Gastrulation The eginning of the third week of de velopment, when gastrulation is initiated, is a highly sensitive stage for terat ogenic insult. At this time, fate maps can e made for various organ systems, su ch as the eyes and rain anlage, and these cell populations may e damaged y te ratogens. For example, high doses of alcohol at this stage kill cells in the ant erior midline of the germ disc, producing a de ciency of the midline in craniofaci al structures and resulting in holoprosencephaly. In such a child, the fore rain is small, the two lateral ventricles often merge into a single ventricle, and t he eyes are close together (hypotelorism). Because this stage is reached 2 weeks after fertilization, it is approximately 4 weeks from the last menses. Therefor e, the woman may not recognize she is pregnant, having assumed that menstruation is late and will egin shortly. Consequently, she may not take precautions she would normally consider if she knew she was pregnant. Gastrulation itself may e disrupted y genetic a normalities and toxic insults. In caudal dysgenesis (sir enomelia), insuf cient mesoderm is formed in the caudal-most region of the em ryo. Because this mesoderm contri utes to formation of the lower lim s, urogenital s ystem (intermediate mesoderm), and lum osacral verte rae, a normalities in these structures ensue. Affected individuals exhi it a varia le range of defects, inc luding hypoplasia and fusion of the lower lim s, verte ral a normalities, renal agenesis, imperforate anus, and anomalies of the genital organs (Fig. 4.13). In humans, the condition is associated with maternal dia etes and other causes. In mice, a normalities of Brachyury (T), Wnt, and engrailed genes produce a similar phenotype. Situs inversus is a condition in which transposition of the viscera in the thorax and a domen occurs. Despite this organ reversal, other structural a normalities occur only slightly more frequently in these individuals. Approxim ately 20% of patients with complete situs inversus also have ronchiectasis and chronic sinusitis ecause of a normal cilia (Kartagener syndrome). Interestingly , cilia are normally present on the ventral surface of the primitive node and ma y e involved in left-right patterning during gastrulation. Other conditions of a normal sidedness are known as laterality sequences. Patients with these condit ions do not have complete situs inversus ut appear to e predominantly ilatera lly left sided or right sided. The spleen re ects the differences; those with left -sided ilaterality have polysplenia, and those with right-sided ilaterality ha ve asplenia or hypoplastic spleen. Patients with laterality sequences also are l ikely to have other malformations, especially heart defects.
80 Part One: General Em ryology Figure 4.13 Sirenomelia (caudal dysgenesis). Loss of mesoderm in the lum osacral region has resulted in fusion of the lim uds and other defects. Tumors Associated With Gastrulation Sometimes, remnants of the primitive streak persist in the sacrococcygeal region. These clusters of pluripotent cells prolif erate and form tumors, known as sacrococcygeal teratomas, that commonly contain tissues derived from all three germ layers (Fig. 4.14). This is the most common tumor in new orns, occurring with a frequency of one in 37,000. These tumors may also arise from primordial germ cells (PGCs) that fail to migrate to the gonada l ridge (see p. 4). Further Development of the Tropho last By the eginning of the third week, the t ropho last is characterized y primary villi that consist of a cytotropho lastic core covered y a syncytial layer (Figs. 3.6 and 4.15). During further developm ent, mesodermal cells penetrate the core of primary villi and grow toward the de cidua. The newly formed structure is known as a secondary villus (Fig. 4.15). By the end of the third week, mesodermal cells in the core of the villus egin to differentiate into lood cells and small lood vessels, forming the villous capi llary system (Fig. 4.15). The villus is now known as a tertiary villus
Chapter 4: Third Week of Development: Trilaminar Germ Disc 81 Figure 4.14 Sacrococcygeal teratoma resulting from remnants of the primitive str eak. These tumors may ecome malignant and are most common in females. Figure 4.15 Development of a villus. A. Transverse section of a primary villus s howing a core of cytotropho lastic cells covered y a layer of syncytium. B. Tra nsverse section of a secondary villus with a core of mesoderm covered y a singl e layer of cytotropho lastic cells, which in turn is covered y syncytium. C. Me soderm of the villus showing a num er of capillaries and venules.
82 Part One: General Em ryology Figure 4.16 Longitudinal section through a villus at the end of the third week o f development. Maternal vessels penetrate the cytotropho lastic shell to enter i ntervillous spaces, which surround the villi. Capillaries in the villi are in co ntact with vessels in the chorionic plate and in the connecting stalk, which in turn are connected to intraem ryonic vessels. or de nitive placental villus. Capillaries in tertiary villi make contact with cap illaries developing in mesoderm of the chorionic plate and in the connecting sta lk (Figs. 4.16 and 4.17). These vessels, in turn, esta lish contact with the int raem ryonic circulatory system, connecting the placenta and the em ryo. Hence, w hen the heart egins to eat in the fourth week of development, the villous syst em is ready to supply the em ryo proper with essential nutrients and oxygen. Mea nwhile, cytotropho lastic cells in the villi penetrate progressively into the ov erlying syncytium until they reach the maternal endometrium. Here they esta lish contact with similar extensions of neigh oring villous stems, forming a thin ou ter cytotropho last shell (Figs. 4.16 and 4.17). This shell gradually surrounds the tropho last entirely and attaches the chorionic sac rmly to the maternal endo metrial tissue (Fig. 4.17). Villi that extend from the chorionic plate to the de cidua asalis (decidual plate: the part of the endometrium where the placenta wi ll form; see Chapter 6) are called stem or anchoring villi. Those that ranch fr om the sides of stem villi are free (terminal) villi, through which exchange of nutrients and other factors will occur (Fig. 4.18). The chorionic cavity, meanwh ile, ecomes larger, and y the 19th or 20th day, the em ryo is attached to its tropho lastic shell y a narrow connecting stalk (Fig. 4.17). The connecting sta lk later develops into the um ilical cord, which forms the connection etween pl acenta and em ryo.
Chapter 4: Third Week of Development: Trilaminar Germ Disc 83 Figure 4.17 Presomite em ryo and the tropho last at the end of the third week. T ertiary and secondary stem villi give the tropho last a characteristic radial ap pearance. Intervillous spaces, which are found throughout the tropho last, are l ined with syncytium. Cytotropho lastic cells surround the tropho last entirely a nd are in direct contact with the endometrium. The em ryo is suspended in the ch orionic cavity y means of the connecting stalk. Summary The most characteristic event occurring during the third week is gastrul ation, which egins with the appearance of the primitive streak, which has at it s cephalic end the primitive node. In the region of the node and streak, epi las t cells move inward (invaginate) to form new cell layers, endoderm and mesoderm. Hence, epi last gives rise to all three germ layers in the em ryo. Cells of the intraem ryonic mesodermal germ layer migrate etween the two other germ layers until they esta lish contact with the extraem ryonic mesoderm covering the yolk sac and amnion (Figs. 4.3 and 4.4). Prenotochordal cells invaginating in the pri mitive pit move forward until they reach the prechordal plate. They intercalate in the endoderm as the notochordal plate (Fig. 4.4). With further development, t he plate detaches from the endoderm, and a solid cord, the notochord, is formed. It forms a midline axis,
84 Part One: General Em ryology Figure 4.18 Stem villi (SV) extend from the chorionic plate (CP) to the asal pl ate (BP). Terminal villi (arrows) are represented y ne ranches from stem villi. which will serve as the asis of the axial skeleton (Fig. 4.4). Cephalic and cau dal ends of the em ryo are esta lished efore the primitive streak is formed. Th us, cells in the hypo last (endoderm) at the cephalic margin of the disc form th e anterior visceral endoderm that expresses head-forming genes, including OTX2, LIM1, and HESX1 and the secreted factor cer erus. Nodal, a mem er of the TGF- fam ily of genes, is then activated and initiates and maintains the integrity of the node and streak. BMP-4, in the presence of FGF, ventralizes mesoderm during gas trulation so that it forms intermediate and lateral plate mesoderm. Chordin, nog gin, and follistatin antagonize BMP-4 activity and dorsalize mesoderm to form th e notochord and somitomeres in the head region. Formation of these structures in more caudal regions is regulated y the Brachyury (T) gene. Left-right asymmetr y is regulated y a cascade of genes; rst, FGF-8, secreted y cells in the node a nd streak, induces Nodal and Lefty-2 expression on the left side. These genes up regulate PITX2, a transcription factor responsi le for left sidedness. Epi last cells moving through the node and streak are predetermined y their position to ecome speci c types of mesoderm and endoderm. Thus, it is possi le to construct a fate map of the epi last showing this pattern (Fig. 4.11).
Chapter 4: Third Week of Development: Trilaminar Germ Disc 85 By the end of the third week, three asic germ layers, consisting of ectoderm, m esoderm, and endoderm, are esta lished in the head region, and the process conti nues to produce these germ layers for more caudal areas of the em ryo until the end of the 4th week. Tissue and organ differentiation has egun, and it occurs i n a cephalocaudal direction as gastrulation continues. In the meantime, the trop ho last progresses rapidly. Primary villi o tain a mesenchymal core in which sma ll capillaries arise (Fig. 4.17). When these villous capillaries make contact wi th capillaries in the chorionic plate and connecting stalk, the villous system i s ready to supply the em ryo with its nutrients and oxygen (Fig. 4.17). Pro lems to Solve 1. A 22-year-old woman consumes large quantities of alcohol at a party and loses consciousness; 3 weeks later she misses her second consecutiv e period. A pregnancy test is positive. Should she e concerned a out the effect s of her inge-drinking episode on her a y? 2. An ultrasound scan detects a lar ge mass near the sacrum of a 28-week female fetus. What might the origin of such a mass e, and what type of tissue might it contain? 3. On ultrasound examinati on, it was determined that a fetus had well-developed facial and thoracic region s, ut caudal structures were a normal. Kidneys were a sent, lum ar and sacral v erte rae were missing, and the hindlim s were fused. What process may have een distur ed to cause such defects? 4. A child has polysplenia and a normal positio ning of the heart. How might these two a normalities e linked developmentally, and when would they have originated? Should you e concerned that other defects might e present? What genes might have caused this event, and when during em ry ogenesis would it have een initiated? SUGGESTED READING Augustine K, Liu ET, Sadler TW: Antisense attenuation of Wnt-1 and Wnt-3a expression in whole em ryo culture reveals roles for these genes in craniofacial, spinal cord, and cardiac morphogenesis. Dev Genet 14:500, 1993. Be ddington RSP: The origin of the foetal tissues during gastrulation in the rodent . In Johnson MH (ed): Development in Mammals. New York, Elsevier, 99:1, 1983. Be ddington RSP: Induction of a second neural axis y the mouse node. Development 1 20:613, 1994. Beddington RSP, Ro ertson RJ: Anterior patterning in the mouse. Tr ends Genet 14:277, 1998. Bellairs R: The primitive streak. Anat Em ryol 174:1, 1 986. De Ro ertis EM, Sasai Y: A common plan for dorsoventral patterning in Bilat eria. Nature 380:37, 1996. Herrmann BG: Expression pattern of the rachyuria gen e in whole mount TWis/TWis mutant em ryos. Development 13:913, 1991.
86 Part One: General Em ryology Holzgreve W, Flake AW, Langer JC: The fetus with sacrococcygeal teratoma. In Har rison MR, Gollus MS, Filly RA (eds): The Un orn Patient. Prenatal Diagnosis and Treatment. Philadelphia, WB Saunders, 1991. King BF, Mais JJ: Developmental chan ges in rhesus monkey placental villi and cell columns. Anat Em ryol 165:361, 198 2. Meyers EN, Martin GR: Differences in left-right axis pathways in mouse and ch ick: Functions of FGF-8 and SHH. Science 285:403, 1999. ORahilly R: Developmental Stages in Human Em ryos. Part A. Em ryos of the First Three Weeks (Stages One t o Nine). Washington, DC, Carnegie Institution of Washington, 1973. Stott D, Kis ert A, Herrmann BG: Rescue of the tail defect of Brachyury mice. Genes Dev 7:197 , 1993. Sulik KK, Lauder JM, Dehart DB: Brain malformations in prenatal mice fol lowing acute maternal ethanol administration. Int J Dev Neurosci 2:203, 1984. Su pp DM, Potter SS, Brueckner M: Molecular motors: The driving force ehind mammal ian leftright development. Trends Cell Biol 10:41, 2000. Tam PPL, Bedding RSP: T he formation of mesodermal tissues in the mouse em ryo during gastrulation and e arly organogenesis. Development 99:109, 1987.
chapter 5 Third to Eighth Week: The Em ryonic Period The em ryonic period or period of organogenesis, occurs from the third to the ei ghth weeks of development and is the time when each of the three germ layers, ec toderm, mesoderm, and endoderm, gives rise to a num er of speci c tissues and orga ns. By the end of the em ryonic period, the main organ systems have een esta li shed, rendering the major features of the external ody form recogniza le y the end of the second month. Derivatives of the Ectodermal Germ Layer At the eginning of the third week of d evelopment, the ectodermal germ layer has the shape of a disc that is roader in the cephalic than the caudal region (Fig. 5.1). Appearance of the notochord and prechordal mesoderm induces the overlying ectoderm to thicken and form the neur al plate (Fig. 5.2). Cells of the plate make up the neuroectoderm and their indu ction represents the initial event in the process of neurulation. MOLECULAR REGU LATION OF NEURAL INDUCTION Blocking the activity of BMP-4, a TGF- family mem er r esponsi le for ventralizing ectoderm and mesoderm, causes induction of the 87
88 Part One: General Em ryology Figure 5.1 A. Dorsal view of a 16-day presomite em ryo. The primitive streak and primitive node are visi le. B. Dorsal view of an 18-day presomite em ryo. The e m ryo is pear-shaped, with its cephalic region somewhat roader than its caudal end. C. Dorsal view of an 18-day human em ryo. Note the primitive node and, exte nding forward from it, the notochord. The yolk sac has a somewhat mottled appear ance. The length of the em ryo is 1.25 mm, and the greatest width is 0.68 mm.
Chapter 5: Third to Eighth Week: The Em ryonic Period 89 Figure 5.2 A. Dorsal view of a late presomite em ryo (approximately 19 days). Th e amnion has een removed and the neural plate is clearly visi le. B. Dorsal vie w of a human em ryo at approximately 20 days showing somites and formation of th e neural groove and neural folds. C. Scanning electron micrograph of a mouse em ryo (approximately 20-day human) showing the typical appearance of the neural gr oove stage. Cranial neural folds have segregated themselves into fore rain (F, p rosencephalon), mid rain (M, mesencephalon), and hind rain (H, rhom encephalon) regions.
90 Part One: General Em ryology neural plate. Thus, in the presence of BMP-4, which permeates the mesoderm and e ctoderm of the gastrulating em ryo, ectoderm ecomes epidermis, and mesoderm for ms intermediate and lateral plate mesoderm. If BMP-4 is a sent or inactivated, e ctoderm ecomes neuralized. Secretion of three other molecules, noggin, chordin, and follistatin, inactivates this protein. These three proteins are present in the organizer (primitive node), notochord, and prechordal mesoderm. They neurali ze ectoderm and cause mesoderm to ecome notochord and paraxial mesoderm (dorsal izes mesoderm). However, these neural inducers induce only fore rain and mid rai n types of tissues. Induction of caudal neural plate structures (hind rain and s pinal cord) depends upon two secreted proteins, WNT-3a and FGF ( ro last growth f actor). In addition, retinoic acid appears to play a role in organizing the cran ial-to-caudal axis ecause it can cause respeci cation of cranial segments into mo re caudal ones y regulating expression of homeo ox genes (see p. 105). NEURULAT ION Once induction has occurred, the elongated, slipper-shaped neural plate grad ually expands toward the primitive streak (Fig. 5.2, B and C ). By the end of th e third week, the lateral edges of the neural plate ecome more elevated to form neural folds, and the depressed midregion forms the neural groove (Figs. 5.2, 5 .3, A and B, and 5.4). Gradually, the neural folds approach each other in the mi dline, where they fuse (Fig. 5.3C ). Fusion egins in the cervical region ( fth so mite) and proceeds cranially and caudally (Figs. 5.5 and 5.6). As a result, the neural tu e is formed. Until fusion is complete, the cephalic and caudal ends of the neural tu e communicate with the amniotic cavity y way of the cranial and caudal neuropores, respectively (Figs. 5.5, 5.6A, and 5.7). Closure of the crani al neuropore occurs at approximately day 25 (18- to 20-somite stage), whereas th e posterior neuropore closes at day 27 (25-somite stage). Neurulation is then co mplete, and the central nervous system is represented y a closed tu ular struct ure with a narrow caudal portion, the spinal cord, and a much roader cephalic p ortion characterized y a num er of dilations, the rain vesicles (see Chapter 1 9). As the neural folds elevate and fuse, cells at the lateral order or crest o f the neuroectoderm egin to dissociate from their neigh ors. This cell populati on, the neural crest (Figs. 5.3 and 5.4), will undergo an epithelial-to-mesenchy mal transition as it leaves the neuroectoderm y active migration and displaceme nt to enter the underlying mesoderm. (Mesoderm refers to cells derived from the epi last and extraem ryonic tissues. Mesenchyme refers to loosely organized em r yonic connective tissue regardless of origin.) Crest cells from the trunk region leave the neural folds after closure of the neural tu e and migrate along one o f two pathways: 1) a dorsal pathway through the dermis, where they will enter th e ectoderm through holes in the asal lamina to form melanocytes in the skin and hair follicles; and 2) a ventral pathway through the anterior half of each somi te to ecome sensory ganglia, sympathetic and enteric neurons,
Chapter 5: Third to Eighth Week: The Em ryonic Period 91 Neural crest Dorsal root ganglion Sympathetic ganglion A Developing suprarenal gland Preaortic ganglion Enteric ganglia B C Urogenital ridge Figure 5.3 Formation and migration of neural crest cells in the spinal cord. A a nd B. Crest cells form at the tips of neural folds and do not migrate away from this region until neural tu e closure is complete. C. After migration, crest cel ls contri ute to a heterogeneous array of structures, including dorsal root gang lia, sympathetic chain ganglia, adrenal medulla, and other tissues (Ta le 5.1). D. In a scanning electron micrograph of a mouse em ryo, crest cells at the top o f the closed neural tu e can e seen migrating away from this area (arrow). E. I n a lateral view with the overlying ectoderm removed, crest cells appear ro last ic as they move down the sides of the neural tu e. (S, somites). Schwann cells, and cells of the adrenal medulla (Fig. 5.3). Neural crest cells a lso form and migrate from cranial neural folds, leaving the neural tu e efore c losure in this region (Fig. 5.4). These cells contri ute to the craniofacial ske leton as well as neurons for cranial ganglia, glial cells, melanocytes, and othe r cell types (Ta le 5.1). Induction of neural crest cells requires an interactio n etween adjacent neural and overlying ectoderm. Bone morphogenetic proteins (B MPs), secreted y non-neural ectoderm, appear to initiate the induction
92 Part One: General Em ryology A NF B Figure 5.4 A. Cross section through the cranial neural folds of a mouse em ryo. Neural crest cells at the tip of the folds (arrow) migrate and contri ute to cra niofacial mesenchyme. B. Lateral view of the cranial neural folds of a mouse em ryo with the surface ectoderm removed. Numerous neural crest cells can e o serv ed leaving the neural folds (NF ) and migrating eneath the ectoderm that has e en removed. Unlike crest cells of the spinal cord, cranial crest exits the neura l folds efore they fuse. process. Crest cells give rise to a heterogeneous array of tissues, as indicated in Ta le 5.1 (see p. 95). By the time the neural tu e is closed, two ilateral ectodermal thickenings, the otic placodes and the lens placodes, ecome visi le in the cephalic region of the em ryo (Fig. 5.8B). During further development, th e otic placodes invaginate and form the otic vesicles, which will develop into s tructures needed for hearing and maintenance of equili rium (see Chapter 16). At approximately the same time, the lens placodes appear. These placodes also inva ginate and, during the fth week, form the lenses of the eyes (see Chapter 17). In general terms, the ectodermal germ layer gives rise to organs and structures th at maintain contact with the outside world: (a) the central nervous
Chapter 5: Third to Eighth Week: The Em ryonic Period 93 Figure 5.5 A. Dorsal view of a human em ryo at approximately day 22. Seven disti nct somites are visi le on each side of the neural tu e. B. Dorsal view of a hum an em ryo at approximately day 23. Note the pericardial ulge on each side of th e midline in the cephalic part of the em ryo. system; ( ) the peripheral nervous system; (c) the sensory epithelium of the ear , nose, and eye; and (d) the epidermis, including the hair and nails. In additio n, it gives rise to su cutaneous glands, the mammary glands, the pituitary gland , and enamel of the teeth. Derivatives of the Mesodermal Germ Layer Initially, cells of the mesodermal germ layer form a thin sheet of loosely woven tissue on each side of the midline (Fi g. 5.9A). By approximately the 17th day, however, cells close to the midline pro liferate and form a thickened plate of tissue known as paraxial mesoderm (Fig. 5 .9B). More laterally, the mesoderm layer remains thin and is known as the latera l plate. With the appearance and coalescence of intercellular cavities in the la teral plate, this tissue is divided into two layers (Fig. 5.9, B and C ): (a) a layer continuous with mesoderm covering the amnion, known as the somatic or pari etal mesoderm layer; and ( ) a layer continuous with mesoderm covering the yolk sac, known as the splanchnic or visceral mesoderm layer (Figs. 5.9, C and D, and 5.10). Together, these layers line a newly formed cavity, the intraem ryonic ca vity, which is continuous with the extraem ryonic cavity on each side of the em ryo. Intermediate mesoderm connects paraxial and lateral plate mesoderm (Figs. 5 .9, B and D, and 5.10).
94 Part One: General Em ryology Figure 5.6 Dorsal (A) and ventral (B) views of a mouse em ryo (approximately 22day human). A. The neural groove is closing in cranial and caudal directions and is anked y pairs of somites (S ). B. The same em ryo showing formation of the g ut tu e with anterior and posterior intestinal portals (arrowheads), heart (H ) in the pericardial cavity (asterisks), and the septum transversum (arrow) repres enting the primordium of the diaphragm (see Chapter 11). The neural folds remain open, exposing fore rain and mid rain regions. Figure 5.7 A 12- to 13-somite em ryo (approximately 23 days). The em ryo within its amniotic sac is attached to the chorion y the connecting stalk. Note the we ll-developed chorionic villi.
Chapter 5: Third to Eighth Week: The Em ryonic Period TABLE 5.1 95 Neural Crest Derivatives Connective tissue and ones of the face and skull Cranial nerve ganglia (see Ta le 19.2) C cells of the thyroid gland Conotruncal septum in the heart Odonto las ts Dermis in face and neck Spinal (dorsal root) ganglia Sympathetic chain and pr eaortic ganglia Parasympathetic ganglia of the gastrointestinal tract Adrenal me dulla Schwann cells Glial cells Arachnoid and pia mater (leptomeninges) Melanocy tes Figure 5.8 A. Lateral view of a 14-somite em ryo (approximately 25 days). Note t he ulging pericardial area and the rst and second pharyngeal arches. B. The left side of a 25-somite em ryo approximately 28 days old. The rst three pharyngeal a rches and lens and otic placodes are visi le. PARAXIAL MESODERM By the eginning of the third week, paraxial mesoderm is organ ized into segments. These segments, known as somitomeres, rst appear in the cepha lic region of the em ryo, and their formation proceeds cephalocaudally. Each som itomere consists of mesodermal cells arranged in concentric whorls around the ce nter of the unit. In the head region, somitomeres form in association with
96 Part One: General Em ryology Notochord Amniotic cavity Ectoderm Mesoderm Paraxial mesoderm Intermediate mesoderm Intercellular cavities in lateral plate Dorsal aorta A Amnion Neural groove Parietal mesoderm layer B Intermediate mesoderm Somite Visceral mesoderm layer Intraem ryonic ody cavity Endoderm C D Figure 5.9 Transverse sections showing development of the mesodermal germ layer. A. Day 17. B. Day 19. C. Day 20. D. Day 21. The thin mesodermal sheet gives ris e to paraxial mesoderm (future somites), intermediate mesoderm (future excretory units), and lateral plate, which is split into parietal and visceral mesoderm l ayers lining the intraem ryonic cavity. So lc Sp * S Ne En Figure 5.10 Transverse sections through cervical somites of mouse em ryos (appro ximately 21-day human) as visualized y scanning electron microscopy. Arrow, not ochord; arrowhead, neural canal; En, endoderm; Ic, intraem ryonic cavity; Ne, ne uroectoderm; S, Somite; So, somatic mesoderm; and Sp, splanchnic mesoderm.
Chapter 5: Third to Eighth Week: The Em ryonic Period 97 segmentation of the neural plate into neuromeres and contri ute to mesenchyme in the head (see Chapter 15). From the occipital region caudally, somitomeres furt her organize into somites. The rst pair of somites arises in the occipital region of the em ryo at approximately the 20th day of development. From here, new somi tes appear in craniocaudal sequence at a rate of approximately three pairs per d ay until, at the end of the fth week, 42 to 44 pairs are present (Figs. 5.3, 5.5, and 5.8). There are four occipital, eight cervical, 12 thoracic, ve lum ar, ve sa cral, and eight to 10 coccygeal pairs. The rst occipital and the last ve to seven coccygeal somites later disappear, while the remaining somites form the axial sk eleton (see Chapter 8). During this period of development, the age of the em ryo is expressed in num er of somites. Ta le 5.2 shows the approximate age of the e m ryo correlated to the num er of somites. By the eginning of the fourth week, cells forming the ventral and medial walls of the somite lose their compact orga nization, ecome polymorphous, and shift their position to surround the notochor d (Fig. 5.11, A and B ). These cells, collectively known as the sclerotome, form a loosely woven tissue, the mesenchyme. They will surround the spinal cord and notochord to form the verte ral column (see Chapter 8). Cells at the dorsolatera l portion of the somite also migrate as precursors of the lim and ody wall mus culature (Fig. 5.11B). After migration of these muscle cells and cells of the sc lerotome, cells at the dorsomedial portion of the somite proliferate and migrate down the ventral side of the remaining dorsal epithelium of the somite to form a new layer, the myotome (Fig. 5.11, B and C ). The remaining dorsal epithelium forms the dermatome, and together these layers constitute the dermomyotome (Fig. 5.11C ). Each segmentally arranged myotome contri utes to muscles of the ack ( epaxial musculature; see Chapter 9), while dermatomes disperse to form the dermi s and su cutaneous tissue of the skin (see Chapter 18). Furthermore, each myotom e and dermatome retains its innervation from its segment of origin, no matter wh ere the cells migrate. Hence each somite forms its own TABLE 5.2 Num er of Somites Correlated to Approximate Age in Days Approximate Ag e (days) 20 21 22 23 24 25 26 27 28 30 No. of Somites 14 47 710 1013 1317 1720 2023 2629 3435
98 Part One: General Em ryology Figure 5.11 Stages in development of a somite. A. Mesoderm cells are arranged ar ound a small cavity. B. Cells of the ventral and medial walls of the somite lose their epithelial arrangement and migrate in the direction of the notochord. The se cells collectively constitute the sclerotome. Cells at the dorsolateral porti on of the somite migrate as precursors to lim and ody wall musculature. Dorsom edial cells migrate eneath the remaining dorsal epithelium of the somite to for m the myotome. C. Cells forming the myotome continue to extend eneath the dorsa l epithelium. D. After ventral extension of the myotome, dermatome cells lose th eir epithelial con guration and spread out under the overlying ectoderm to form de rmis.
Chapter 5: Third to Eighth Week: The Em ryonic Period 99 sclerotome (the cartilage and one component), its own myotome (providing the se gmental muscle component), and its own dermatome, the segmental skin component. Each myotome and dermatome also has its own segmental nerve component. Molecular Regulation of Somite Differentiation Signals for somite differentiation arise f rom surrounding structures, including the notochord, neural tu e, epidermis, and lateral plate mesoderm (Fig. 5.12). The secreted protein product of the gene So nic hedgehog (Shh), produced y the notochord and oor plate of the neural tu e, i nduces the ventromedial portion of the somite to ecome sclerotome. Once induced , sclerotome cells express the transcription factor PAX1, which initiates the ca scade of Figure 5.12 Expression patterns of genes that regulate somite differentiation. S onic hedgehog (SHH), secreted y the notochord and oor plate of the neural tu e, causes the ventral part of the somite to form sclerotome and to express PAX1, wh ich in turn controls chondrogenesis and verte rae formation. WNT proteins from t he dorsal neural tu e activate PAX3, which demarcates the dermomyotome. WNT prot eins also direct the dorsomedial portion of the somite to form epaxial ( ack) mu scles and to express the muscle-speci c gene MYF5. The middorsal portion of the so mite is directed to ecome dermis y neurotrophin 3 (NT-3) expressed y the dors al neural tu e. Hypaxial (lim and ody wall) musculature is derived from the do rsolateral portion of the somite under the com ined in uence of activating WNT pro teins and inhi itory BMP-4 protein, which together activate MYOD expression.
100 Part One: General Em ryology cartilage- and one-forming genes for verte ral formation. Expression of PAX3, r egulated y WNT proteins from the dorsal neural tu e, marks the dermomyotome reg ion of the somite. WNT proteins from the dorsal neural tu e also target the dors omedial portion of the somite, causing it to initiate expression of the muscle-s peci c gene MYF5 and to ecome epaxial musculature. Interplay etween the inhi iti ng protein BMP-4 (and pro a ly FGFs) from the lateral plate mesoderm and activat ing WNT products from the epidermis directs the dorsolateral portion of the somi te to express another muscle-speci c gene, MYOD, and to form lim and ody wall mu scles. The midportion of the dorsal epithelium of the somite is directed y neur otrophin 3 (NT-3), secreted y the dorsal region of the neural tu e, to form der mis. INTERMEDIATE MESODERM Intermediate mesoderm, which temporarily connects par axial mesoderm with the lateral plate (Figs. 5.9D and 5.10A), differentiates int o urogenital structures. In cervical and upper thoracic regions, it forms segmen tal cell clusters (future nephrotomes), whereas more caudally, it forms an unseg mented mass of tissue, the nephrogenic cord. Excretory units of the urinary syst em and the gonads develop from this partly segmented, partly unsegmented interme diate mesoderm (see Chapter 14). LATERAL PLATE MESODERM Lateral plate mesoderm s plits into parietal and visceral layers, which line the intraem ryonic cavity an d surround the organs, respectively (Figs. 5.9, C and D, 5.10, and 5.13A). Mesod erm from the parietal layer, together with overlying ectoderm, will form the lat eral and ventral ody wall. The visceral layer and em ryonic endoderm will form the wall of the gut (Fig. 5.13B ). Mesoderm Amniotic cavity Ectoderm Mesonephros Dorsal mesentery Visceral mesoderm layer Pa rietal mesoderm layer Wall of gut Serous mem rane (peritoneum) Body wall Parietal mesoderm layer Intraem ryonic cavity Endoderm of yolk sac A B Figure 5.13 A. Transverse section through a 21-day em ryo in the region of the m esonephros showing parietal and visceral mesoderm layers. The intraem ryonic cav ities communicate with the extraem ryonic cavity (chorionic cavity). B. Section at the end of the fourth week. Parietal mesoderm and overlying ectoderm form the ventral and lateral ody wall. Note the peritoneal (serous) mem rane.
Chapter 5: Third to Eighth Week: The Em ryonic Period 101 cells of the parietal layer surrounding the intraem ryonic cavity will form thin mem ranes, the mesothelial mem ranes, or serous mem ranes, which will line the peritoneal, pleural, and pericardial cavities and secrete serous uid (Fig. 5.13B ). Mesoderm cells of the visceral layer will form a thin serous mem rane around each organ (see Chapter 10). BLOOD AND BLOOD VESSELS Blood vessels form in two w ays: vasculogenesis, where y vessels arise from lood islands (Fig. 5.14), and a ngiogenesis, which entails sprouting from Figure 5.14 Blood vessels form in two ways: vasculogenesis (top), in which vesse ls arise from lood islands, and angiogenesis ( ottom), in which new vessels spr out from existing ones. During vasculogenesis, ro last growth factor 2 (FGF-2) inds to its receptor on su populations of mesoderm cells and induces them to for m hemangio lasts. Then, under the in uence of vascular endothelial growth factor ( VEGF) acting through two different receptors, these cells ecome endothelial and coalesce to form vessels. Angiogenesis is also regulated y VEGF, which stimula tes proliferation of endothelial cells at points where new vessels will sprout f rom existing ones. Final modeling and sta ilization of the vasculature are accom plished y platelet-derived growth factor (PDGF) and transforming growth factor (TGF-).
102 Part One: General Em ryology Figure 5.15 Extraem ryonic lood vessel formation in the villi, chorion, connect ing stalk, and wall of the yolk sac in a presomite em ryo of approximately 19 da ys. existing vessels. The rst lood islands appear in mesoderm surrounding the wall o f the yolk sac at 3 weeks of development and slightly later in lateral plate mes oderm and other regions (Fig. 5.15). These islands arise from mesoderm cells tha t are induced y ro last growth factor 2 (FGF-2) to form hemangio lasts, a commo n precursor for vessel and lood cell formation. Hemangio lasts in the center of lood islands form hematopoietic stem cells, the precursors of all lood cells, whereas peripheral hemangio lasts differentiate into angio lasts, the precursor s to lood vessels. These angio lasts proliferate and are eventually induced to form endothelial cells y vascular endothelial growth factor (VEGF) secreted y surrounding mesoderm cells (Fig. 5.14). This same factor then regulates coalesce nce of these endothelial cells into the rst primitive lood vessels. Once the pro cess of vasculogenesis esta lishes a primary vascular ed, additional vasculatur e is added y angiogenesis, the sprouting of new vessels (Fig. 5.14). This proce ss is also mediated y VEGF, which stimulates proliferation of endothelial cells at points where new vessels are to e formed. Maturation and modeling of the va sculature are regulated y other growth factors, including platelet-derived grow th factor (PDGF) and transforming growth factor (TGF-), until the adult pattern i s esta lished. As mentioned, the rst lood cells arise in the lood islands of th e yolk sac, ut this population is transitory. The de nitive hematopoietic stem ce lls arise from mesoderm surrounding the aorta in a site called the
Chapter 5: Third to Eighth Week: The Em ryonic Period 103 aorta-gonad-mesonephros region (AGM). These cells will colonize the liver, which ecomes the major hematopoietic organ of the fetus. Later, stem cells from the liver will colonize the one marrow, the de nitive lood-forming tissue. Derivatives of the Endodermal Germ Layer The gastrointestinal tract is the main organ system derived from the endodermal germ layer. This germ layer covers the ventral surface of the em ryo and forms the roof of the yolk sac (Fig. 5.16A). W ith development and growth of the rain vesicles, however, the em ryonic disc e gins to ulge into the amniotic cavity and to fold cephalocaudally. This folding is most pronounced in the regions of the head and tail, where the head fold and tail fold are formed (Fig. 5.16). As a result of cephalocaudal folding, a conti nuously larger portion of the endoderm-lined cavity is incorporated into the od y of the em ryo proper Hindgut Endoderm Amniotic cavity Connecting stalk Foregut Heart tu e Ectoderm Angiogenic cell cluster Allantois Pericardial cavity Buccopharyngeal mem rane A Buccopharyngeal mem rane Cloacal mem rane B Lung ud Liver ud Midgut Cloacal mem rane Heart tu e Remnant of the Allantois C D Yolk sac Figure 5.16 Sagittal midline sections of em ryos at various stages of developmen t to demonstrate cephalocaudal folding and its effect on position of the endoder m-lined cavity. A. Presomite em ryo. B. Em ryo with 7 somites. C. Em ryo with 14 somites. D. End of the rst month. Note the angiogenic cell clusters in relation to the uccopharyngeal mem rane. uccopharyngeal mem rane Vitelline duct
104 Part One: General Em ryology Amnionic cavity Surface ectoderm Somatic mesoderm Connection etween gut and yolk sac Intraem ryonic ody cavity
Splanchnic mesoderm Yolk sac Dorsal Gut mesentery A B C Figure 5.17 Transverse sections through em ryos at various stages of development to show the effect of lateral folding on the endoderm-lined cavity. A. Folding is initiated. B. Transverse section through the midgut to show the connection e tween the gut and yolk sac. C. Section just elow the midgut to show the closed ventral a dominal wall and gut suspended from the dorsal a dominal wall y its m esentery. (Fig. 5.16C ). In the anterior part, the endoderm forms the foregut; in the tail region, it forms the hindgut. The part etween foregut and hindgut is the midgu t. The midgut temporarily communicates with the yolk sac y way of a road stalk , the vitelline duct (Fig. 5.16D). This duct is wide initially, ut with further growth of the em ryo, it ecomes narrow and much longer (Figs. 5.16D, 5.17B, an d 5.20). At its cephalic end, the foregut is temporarily ounded y an ectoderma lendodermal mem rane called the uccopharyngeal mem rane (Fig. 5.16, A and C ). In the fourth week, the uccopharyngeal mem rane ruptures, esta lishing an open connection etween the amniotic cavity and the primitive gut (Fig. 5.16D). The h indgut also terminates temporarily at an ectodermalendodermal mem rane, the cloa cal mem rane (Fig. 5.16C ), which reaks down in the seventh week to create the opening for the anus. As a result of rapid growth of the somites, the initial at em ryonic disc also folds laterally, and the em ryo o tains a round appearance ( Fig. 5.17). Simultaneously, the ventral ody wall of the em ryo is esta lished e xcept for a small part in the ventral a dominal region where the yolk sac duct a nd connecting stalk are attached. While the foregut and hindgut are esta lished, the midgut remains in communication with the yolk sac. Initially, this connecti on is wide (Fig. 5.17A), ut as a result of ody folding, it gradually ecomes l ong and narrow to form the vitelline duct (Figs. 5.17B and 5.18). Only much late r, when the vitelline duct is o literated, does the midgut lose its connection w ith the original endoderm-lined cavity and o tain its free position in the a dom inal cavity (Fig. 5.17C ). Another important result of cephalocaudal and lateral folding is partial incorporation of the allantois into the ody of the em ryo, where it forms the
Chapter 5: Third to Eighth Week: The Em ryonic Period 105 Figure 5.18 Sagittal sections through em ryos showing derivatives of the endoder mal germ layer. A. Pharyngeal pouches, epithelial lining of the lung uds and tr achea, liver, gall ladder, and pancreas. B. The urinary ladder is derived from the cloaca and, at this stage of development, is in open connection with the all antois. cloaca (Fig. 5.18A). The distal portion of the allantois remains in the connecti ng stalk. By the fth week, the yolk sac duct, allantois, and um ilical vessels ar e restricted to the region of the um ilical ring (Figs. 5.18, 5.19, and 6.15). I n humans, the yolk sac is vestigial and in all pro a ility has a nutritive role only in early stages of development (Fig. 5.20). In the second month of developm ent, it lies in the chorionic cavity (Fig. 5.21). Hence, the endodermal germ lay er initially forms the epithelial lining of the primitive gut and the intraem ry onic portions of the allantois and vitelline duct (Fig. 5.18A). During further d evelopment, it gives rise to (a) the epithelial lining of the respiratory tract; ( ) the parenchyma of the thyroid, parathyroids, liver, and pancreas (see Chapt ers 13 and 15); (c) the reticular stroma of the tonsils and thymus; (d) the epit helial lining of the urinary ladder and urethra (see Chapter 14); and (e) the e pithelial lining of the tympanic cavity and auditory tu e (see Chapter 16). Patt erning of the Anteroposterior Axis: Regulation y Homeo ox Genes Homeo ox genes are known for their homeodomain, a DNA inding motif, the homeo ox. They code fo r transcription factors that activate cascades of genes regulating phenomena suc h as segmentation and axis formation. Many homeo ox genes are collected into hom eotic clusters, although other genes also contain the homeodomain. An important cluster of genes specifying the
106 Part One: General Em ryology Figure 5.19 Human em ryo (CRL 9.8 mm, haped. fth week) (29.9). The forelim s are paddle s
craniocaudal axis is the homeotic gene complex Hom-C in Drosophila. These genes, which contain the Antennapedia and Bithorax classes of homeotic genes, are orga nized on a single chromosome as a functional unit. Thus, genes specifying more c ranial structures lie at the 3 end of the DNA and are expressed rst, with genes c ontrolling posterior development expressed sequentially and lying increasingly t oward the 5 end (Fig. 5.22). These genes are conserved in humans, existing as fo ur copies, HOXA, HOXB, HOXC, and HOXD, which are arranged and expressed like tho se in Drosophila. Thus, each cluster lies on a separate chromosome, and the gene s in each group are num ered 1 to 13 (Fig. 5.22). Genes with the same num er, u t elonging to different clusters form a paralogous group, such as HOXA4, HOXB4, HOXC4, and HOXD4. The pattern of expression of these genes, along with evidence from knockout
Chapter 5: Third to Eighth Week: The Em ryonic Period 107 Figure 5.20 A. Lateral view of a 28-somite human em ryo. The main external featu res are the pharyngeal arches and somites. Note the pericardial-liver ulge. B. The same em ryo taken from a different angle to demonstrate the size of the yolk sac. experiments in which mice are created that lack one or more of these genes, supp orts the hypothesis that they play a role in cranial-to-caudal patterning of the derivatives of all three germ layers. For example, an overlapping expression pa ttern of the HOX code exists in the somites and verte rae, with genes located mo re 3 in each cluster eing expressed in and regulating development of more crani al segments (Fig. 5.22). External Appearance During the Second Month At the end of the fourth week, when the em ryo has approximately 28 somites, the main external features are the somi tes and pharyngeal arches (Fig. 5.20). The age of the em ryo is therefore usuall y expressed in somites (Ta le 5.2). Because counting somites ecomes dif cult duri ng the second month of development, the age of the em ryo is then indicated as t he crown-rump length (CRL) and expressed in millimeters (Ta le 5.3). CRL is the measurement from the vertex of the skull to the midpoint etween the apices of t he uttocks. During the second month, the external appearance of the em ryo is c hanged y an increase in head size and formation of the lim s, face, ears, nose, and eyes. By the eginning of the fth week, forelim s and hindlim s appear as pa ddle-shaped uds (Fig. 5.19). The former are located dorsal to the pericardial s welling at the level of the fourth cervical to the rst thoracic somites, which ex plains their innervation y the rachial plexus. Hindlim uds appear slightly l ater just caudal to attachment of the um ilical stalk at the level of the lum ar and upper sacral somites. With further growth, the terminal portions of
108 Part One: General Em ryology Figure 5.21 Human em ryo (CRL 13 mm, sixth week) showing the yolk sac in the cho rionic cavity. the uds atten and a circular constriction separates them from the proximal, more cylindrical segment (Fig. 5.21). Soon, four radial grooves separating ve slightl y thicker areas appear on the distal portion of the uds, foreshadowing formatio n of the digits (Fig. 5.21). These grooves, known as rays, appear in the hand re gion rst and shortly afterward in the foot, as the upper lim is slightly more ad vanced in development than the lower lim . While ngers and toes are eing formed (Fig. 5.23), a second constriction divides the proximal portion of the uds into two segments, and the three parts characteristic of the adult extremities can e recognized (Fig. 5.24).
Chapter 5: Third to Eighth Week: The Em ryonic Period 109 Figure 5.22 Drawing showing the arrangement of homeo ox genes of the Antennapedi a (ANT-C) and Bithorax (BX-C) classes of Drosophila and conserved homologous gen es of the same classes in humans. During evolution, these genes have een duplic ated, such that humans have four copies arranged on four different chromosomes. Homology etween Drosophila genes and those in each cluster of human genes is in dicated y color. Genes with the same num er, ut positioned on different chromo somes, form a paralogous group. Expression of the genes is in a cranial to cauda l direction from the 3 (expressed early) to the 5 (expressed later) end as indic ated in the y and mouse em ryo diagrams. Retinoic acid modulates expression of th ese genes with those at the 3 end eing more responsive to the compound.
110 Part One: General Em ryology TABLE 5.3 Crown-Rump Length Correlated to Approxima te Age in Weeks CRL (mm) 58 1014 1722 2830 Approximate Age (weeks) 5 6 7 8 Figure 5.23 Human em ryo (CRL 21 mm, seventh week) (4). The chorionic sac is open to show the em ryo in its amniotic sac. The yolk sac, um ilical cord, and vesse ls in the chorionic plate of the placenta are clearly visi le. Note the size of the head in comparison with the rest of the ody.
Chapter 5: Third to Eighth Week: The Em ryonic Period 111 Figure 5.24 Human em ryo (CRL 25 mm, seventh to eighth week). The chorion and th e amnion have een opened. Note the size of the head, the eye, the auricle of th e ear, the well-formed toes, the swelling in the um ilical cord caused y intest inal loops, and the yolk sac in the chorionic cavity. CLINICAL CORRELATES Birth Defects Most major organs and organ systems are formed during the third to eighth week. This period, which is critical for normal development, is therefor e called the period of organogenesis. Stem cell populations are esta lishing eac h of the organ primordia, and these interactions are sensitive to insult from ge netic and environmental in uences. Thus, this period is when most gross structural irth defects are induced. Unfortunately, the mother may not realize she is pre gnant during this critical time, especially during the third and fourth weeks, w hich are particularly vulnera le. Consequently, she may not avoid harmful in uence s, such as cigarette smoking and alcohol. Understanding the main events of organ ogenesis is important for identifying the time that a particular defect
112 Part One: General Em ryology was induced and, in turn, determining possi le causes for the malformation (see Chapter 7). Summary The em ryonic period, which extends from the third to the eighth weeks o f development, is the period during which each of the three germ layers, ectoder m, mesoderm, and endoderm, gives rise to its own tissues and organ systems. As a result of organ formation, major features of ody form are esta lished (Ta le 5 .4). The ectodermal germ layer gives rise to the organs and structures that main tain contact with the outside world: (a) central nervous system; ( ) peripheral nervous system; (c) sensory epithelium of ear, nose, and eye; (d) skin, includin g hair and nails; and (e) pituitary, mammary, and sweat glands and enamel of the teeth. Induction of the neural plate is regulated y inactivation of the growth factor BMP-4. In the cranial region, inactivation is caused y noggin, chordin, and follistatin secreted y the node, notochord, and prechordal mesoderm. Inact ivation of BMP-4 in the hind rain and spinal cord regions is effected y WNT3a a nd FGF. In the a sence of inactivation, BMP-4 causes ectoderm to ecome epidermi s and mesoderm to ventralize to form intermediate and lateral plate mesoderm. Im portant components of the mesodermal germ layer are paraxial, intermediate, and lateral plate mesoderm. Paraxial mesoderm forms somitomeres, which give rise to mesenchyme of the head and organize into somites in occipital and caudal segment s. Somites give rise to the myotome (muscle tissue), sclerotome (cartilage and one), and dermatome (su cutaneous tissue of the skin), which are all supporting tissues of the ody. Signals for somite differentiation are derived from surroun ding structures, including the notochord, neural tu e, and epidermis. The notoch ord and oor plate of the neural tu e secrete Sonic hedgehog, which induces the sc lerotome. WNT proteins from the dorsal neural tu e cause the dorsomedial portion of the somite to form epaxial musculature, while BMP-4, FGFs from the lateral p late mesoderm, and WNTs from the epidermis cause the dorsolateral portion to for m lim and ody wall musculature. The dorsal midportion of the somite ecomes de rmis under the in uence of neurotrophin 3, secreted y the dorsal neural tu e (Fig . 5.12). Mesoderm also gives rise to the vascular system, that is, the heart, ar teries, veins, lymph vessels, and all lood and lymph cells. Furthermore, it giv es rise to the urogenital system: kidneys, gonads, and their ducts ( ut not the ladder). Finally, the spleen and cortex of the suprarenal glands are mesodermal derivatives. The endodermal germ layer provides the epithelial lining of the ga strointestinal tract, respiratory tract, and urinary ladder. It also forms the parenchyma of the thyroid, parathyroids, liver, and pancreas. Finally, the
Chapter 5: Third to Eighth Week: The Em ryonic Period TABLE 5.4 Days 1415 1618 1920 113 Summary of Key Events During the Em ryonic Period Length (mm) 0.2 0.4 1.02.0 Figure 5.1 A 5.1B 5.2 A Characteristic Features Appear ance of primitive streak Notochordal process appears; hemopoietic cells in yolk sac Intraem ryonic mesoderm spread under cranial ectoderm; primitive streak cont inues; um ilical vessels and cranial neural folds eginning to form Cranial neur al folds elevated, and deep neural groove esta lished; em ryo eginning to end Fusion of neural folds egins in cervical region; cranial and caudal neuropores open widely; visceral arches 1 and 2 present; heart tu e eginning to fold Cepha locaudal folding under way; cranial neuropore closing or closed; optic vesicles formed; otic placodes appear Caudal neuropore closing or closed; upper lim uds appear; 3 pairs of visceral arches Fourth visceral arch formed; hindlim uds a ppear; otic vesicle and lens placode Forelim s paddle-shaped; nasal pits formed; em ryo tightly C-shaped Digital rays in hand and footplates; rain vesicles pro minent; external auricle forming from auricular hillocks; um ilical herniation i nitiated Pigmentation of retina visi le; digital rays separating; nipples and ey elids formed; maxillary swellings fuse with medial nasal swellings as upper lip forms; prominent um ilical herniation Lim s long, ent at el ows, knees; ngers, t oes free; face more human-like; tail disappears; um ilical herniation persists t o end of third month Somites 0 0 0 2021 14 2.03.0 5.2B, C 2223 512 3.03.5 5.5 A, B; 5.6; 5.7 2425 1320 3.04.5 5.8 A 2627 2129 3.55.0 5.8B; 5.20 A, B 5.8B 2830
3035 4.06.0 3135 3642 7.010.0 9.014.0 5.19 5.21 4349 13.022.0 5.23 5056 21.031.0 5.24
114 Part One: General Em ryology epithelial lining of the tympanic cavity and auditory tu e originate in the endo dermal germ layer. Craniocaudal patterning of the em ryonic axis is controlled y homeo ox genes. These genes, conserved from Drosophila, are arranged in four c lusters, HOXA, HOXB, HOXC, and HOXD, on four different chromosomes. Genes toward the 3 end of the chromosome control development of more cranial structures; tho se more toward the 5 end regulate differentiation of more posterior structures. Together, they regulate patterning of the hind rain and axis of the em ryo (Fig. 5.22). As a result of formation of organ systems and rapid growth of the centra l nervous system, the initial at em ryonic disc egins to fold cephalocaudally, e sta lishing the head and tail folds. The disc also folds transversely (lateral f olds), esta lishing the rounded ody form. Connection with the yolk sac and plac enta is maintained through the vitelline duct and um ilical cord, respectively. Pro lems to Solve 1. Why are the third to eighth weeks of em ryogenesis so impor tant for normal development and the most sensitive for induction of structural d efects? SUGGESTED READING Cossu G, Taj akhshs S, Buckingham M: How is myogenesis initiat ed in the em ryo? Trends Genet 12:218, 1996. Eichele G: Retinoids and verte rate lim pattern formation. Trends Genet 5:226, 1990. Hanahan D: Signaling vascular morphogenesis and maintenance. Science 277:48, 1997. Jessell TM, Melton DA: Dif fusi le factors in verte rate em ryonic induction. Cell 68:257, 1992. Johnson RL , Laufer E, Riddle RD, Ta in C: Ectopic expression of sonic hedgehog alters dors oventral patterning of somites. Cell 79:1165, 1994. Kanzler B, Foreman RK, Le os ky PA, Mallo M: BMP signaling is essential for development of skeletogenic and n eurogenic cranial neural crest. Development 127:1095, 2000. Kessel M: Respeci cati on of verte ral identities y retinoic acid. Development 115:487, 1992. Krumlauf R: Hox genes and pattern formation in the ranchial region of the verte rate he ad. Trends Genet 9:106, 1993. Krumlauf R: Hox genes in verte rate development. C ell 78:191, 1994. McGinnis W, Krumlauf R: Homeo ox genes and axial patterning. C ell 68:283, 1992. Meier T, Tam PPL: Metameric pattern development in the em ryon ic axis of the mouse: 1. Differentiation of the cranial segments. Differentiatio n 21:95, 1982. ORahilly R, Muller F: Bidirectional closure of the rostral neuropo re. Am J Anat 184:259, 1989. Ordahl CP, Ledouarin N: Two myogenic lineages withi n the developing somite. Development 114:339, 1992. Risau W: Mechanisms of angio genesis. Nature 386:671, 1997. Sadler TW: Mechanisms of neural tu e closure and defects. Ment Retard Dev Disa ilities Res Rev 4:247, 1998. Sasai Y, DeRo ertis E M: Ectodermal patterning in verte rate em ryos. Dev Biol 182:5, 1997. Schoenwolf G, Bortier H, Vakaet L: Fate mapping the avian neural plate with quail-chick ch imeras: origin of prospective median wedge cells. J Exp Zool 249:271, 1989.
Chapter 5: Third to Eighth Week: The Em ryonic Period 115 Slack JM: Em ryonic induction. Mech Dev 41:91, 1993. Smith JL, Schoenwolf GC: Ne urulation: coming to closure. Trends Neurosci 20:510, 1997. Stern HM, Brown AMC, Hauschka SD: Myogenesis in paraxial mesoderm: preferential induction y dorsal neural tu e and y cells expressing Wnt-1. Development 121:3675, 1995. Streeter GL: Developmental horizons in human em ryos: age group XI, 1320 somites, and age group XII, 2129 somites. Contri Em ryol 30:211, 1942. Streeter GL: Developmental horizons in human em ryos: age group XIII, em ryos 4 or 5 mm long, and age grou p XIV, indentation of lens vesicle. Contri Em ryol 31:26, 1945. Tam PPL, Beddin gton RSP: The formation of mesodermal tissues in the mouse em ryo during gastrul ation and early organogenesis. Development 99:109, 1987. Tam PPL, Meier S, Jaco son AG: Differentiation of the metameric pattern in the em ryonic axis of the mo use: 2. Somitomeric organization of the pre-somitic mesoderm. Differentiation 21 :109, 1982. Zon LI: Developmental iology of hematopoiesis. Blood 8:2876, 1995.
chapter 6 Third Month to Birth: The Fetus and Placenta Development of the Fetus The period from the eginning of the ninth week to irt h is known as the fetal period. It is characterized y maturation of tissues and organs and rapid growth of the ody. The length of the fetus is usually indicat ed as the crown-rump length (CRL) (sitting height) or as the crown-heel length ( CHL), the measurement from the vertex of the skull to the heel (standing height) . These measurements, expressed in centimeters, are correlated with the age of t he fetus in weeks or months (Ta le 6.1; p. 118). Growth in length is particularl y striking during the third, fourth, and fth months, while an increase in weight is most striking during the last 2 months of gestation. In general, the length o f pregnancy is considered to e 280 days, or 40 weeks after the onset of the las t normal menstrual period (LNMP) or more accurately, 266 days or 38 weeks after fertilization. For the purposes of the following discussion, age is calculated f rom the time of fertilization and is expressed in weeks or calendar months. MONT HLY CHANGES One of the most striking changes taking place during fetal life is t he relative slowdown in growth of the head compared with the rest of the ody. A t the eginning of the third month the head constitutes 117
118
Part One: General Em ryology TABLE 6.1 Growth in Length and Weight During the Fe tal Period Age (Weeks) 912 1316 1720 2124 2528 2932 3336 3738 CRL (cm) 58 914 15 2830 3134 3536 Weight (g) 1045 60200 250450 500820 9001300 14002100 22002900 3000
approximately half of the CRL (Figs. 6.1 and 6.2). By the eginning of the fth mo nth, the size of the head is a out one-third of the CHL, and at irth it is appr oximately one-fourth of the CHL (Fig. 6.2). Hence, over time, growth of the ody accelerates ut that of the head slows down. During the third month the face e comes more human looking (Figs. 6.3 and 6.4). The eyes, initially directed later ally, move to the ventral aspect of the
Figure 6.1 A 9-week fetus. Note the the rest of the ody. The yolk sac horionic cavity. Note the um ilical side of the chorion has many villi almost smooth (chorion laeve).
large size of the head compared with that of and long vitelline duct are visi le in the c cord and herniation of intestinal loops. One (chorion frondosum), while the other side is
Chapter 6: Third Month to Birth: The Fetus and Placenta 119 Figure 6.2 Size of the head in relation to the rest of the s of development.
face, and the ears come to lie close to their de nitive position at the side of th e head (Fig. 6.3). The lim s reach their relative length in comparison with the rest of the ody, although the lower lim s are still a little shorter and less w ell developed than the upper extremities. Primary ossi cation centers are present in the long ones and skull y the 12th week. Also y the 12th week, external ge nitalia develop to such a degree that the sex of the fetus can e determined y external examination (ultrasound). During the 6th week intestinal loops cause a large swelling (herniation) in the um ilical cord, ut y the 12th week the loop s withdraw into the a dominal cavity. At the end of the third month, re ex activit y can e evoked in a orted fetuses, indicating muscular activity. During the fou rth and fth months the fetus lengthens rapidly (Fig. 6.5 and Ta le 6.1), and at t he end of the rst half of intrauterine life its CRL is approximately 15 cm, that is, a out half the total length of the new orn. The weight of the fetus increase s little during this period and y the end of the fth month is still less than 50 0 g. The fetus is covered with ne hair, called lanugo hair; eye rows and head hai r are also visi le. During the fth month movements of the fetus can e felt y th e mother. During the second half of intrauterine life, weight increases consider a ly, particularly during the last 2.5 months, when 50% of the full-term weight (approximately 3200 g) is added. During the sixth month, the skin of the fetus i s reddish and has a wrinkled appearance ecause of the lack of underlying connec tive tissue. A fetus orn early in the sixth month has great dif culty
ody at various stage
120 Part One: General Em ryology Figure 6.3 An 11-week fetus. The um ilical cord still shows a swelling at its a se, caused y herniated intestinal loops. Toes are developed, and the sex of the fetus can e seen. The skull of this fetus lacks the normal smooth contours. surviving. Although several organ systems are a le to function, the respiratory system and the central nervous system have not differentiated suf ciently, and coo rdination etween the two systems is not yet well esta lished. By 6.5 to 7 month s, the fetus has a length of a out 25 cm and weighs approximately 1100 g. If or n at this time, the infant has a 90% chance of surviving. Some developmental eve nts occurring during the rst 7 months are indicated in Ta le 6.2. During the last 2 months, the fetus o tains well-rounded contours as the result of deposition o f su cutaneous fat (Fig. 6.6). By the end of intrauterine life, the skin is cove red y a whitish, fatty su stance (vernix caseosa) composed of secretory product s from se aceous glands.
Chapter 6: Third Month to Birth: The Fetus and Placenta 121 Figure 6.4 A 12-week fetus in utero. Note the extremely thin skin and underlying lood vessels. The face has all of the human characteristics, ut the ears are still primitive. Movements egin at this time ut are usually not felt y the mo ther. At the end of the ninth month the skull has the largest circumference of all par ts of the ody, an important fact with regard to its passage through the irth c anal. At the time of irth the weight of a normal fetus is 3000 to 3400 g; its C RL is a out 36 cm; and its CHL is a out 50 cm. Sexual characteristics are pronou nced, and the testes should e in the scrotum.
122 Part One: General Em ryology TABLE 6.2 Event Taste uds appear Swallowing Respira tory movements Sucking movements Some sounds can e heard Eyes sensitive to ligh t Developmental Horizons during Fetal Life Age (Weeks) 7 10 1416 24 2426 28 Recognition of form and color occurs postnatally. Figure 6.5 An 18-week-old fetus connected to the placenta y its um ilical cord. The skin of the fetus is thin ecause of lack of su cutaneous fat. Note the pla centa with its cotyledons and the amnion. TIME OF BIRTH The date of irth is most accurately indicated as 266 days, or 38 weeks, after fertilization. The oocyte is usually fertilized within 12 hours of ovulation. However, sperm deposited in the reproductive tract up to 6 days prior to ovulation can survive to fertilize oocytes. Thus, most pregnancies occur whe n sexual intercourse occurs within a 6-day period that ends on the day of ovulat ion. A
Chapter 6: Third Month to Birth: The Fetus and Placenta 123 pregnant woman usually will see her o stetrician when she has missed two success ive menstrual leeds. By that time, her recollection a out coitus is usually vag ue, and it is readily understanda le that the day of fertilization is dif cult to determine. The o stetrician calculates the date of irth as 280 days or 40 weeks from the rst day of the LNMP. In women with regular 28-day menstrual periods the method is fairly accurate, ut when cycles are irregular, su stantial miscalcul ations may e made. An additional complication occurs when the woman has some l eeding a out 14 days after fertilization as a result of erosive activity y the implanting lastocyst (see Chapter 3). Hence the day of delivery is not always e asy to determine. Most fetuses are orn within 10 to 14 days of the calculated d elivery date. If they are orn much earlier, they are categorized as premature; if orn later, they are considered postmature. Occasionally the age of an em ryo or small fetus must e determined. By com ining data on the onset of the last m enstrual period with fetal length, weight, and other morphological characteristi cs typical for a given month of development, a reasona le estimate of the age of the fetus can e formulated. A valua le tool for assisting in this determinatio n is ultrasound, which can provide an accurate (1 to 2 days) measurement of CRL during the 7th to 14th weeks. Measurements commonly used in the 16th to 30th wee ks are iparietal diameter (BPD), head and a dominal circumference, and femur le ngth. An accurate determination of fetal size and age is important for managing pregnancy, especially if the mother has a small pelvis or the a y has a irth d efect. CLINICAL CORRELATES Low Birth Weight There is considera le variation in fetal length and weight, and sometimes these values do not correspond with the calculated age of the fetus i n months or weeks. Most factors in uencing length and weight are genetically deter mined, ut environmental factors also play an important role. Intrauterine growt h restriction (IUGR) is a term applied to infants who are at or elow the 10th p ercentile for their expected irth weight at a given gestational age. Sometimes these infants are descri ed as small for dates, small for gestational age (SGA), fetally malnourished, or dysmature. Approximately 1 in 10 a ies have IUGR and therefore an increased risk of neurological de ciencies, congenital malformations, meconium aspiration, hypoglycemia, hypocalcemia, and respiratory distress syndr ome (RDS). The incidence is higher in lacks than in whites. Causative factors i nclude chromosomal a normalities (10%); teratogens; congenital infections (ru el la, cytomegalovirus, toxoplasmosis, and syphilis); poor maternal health (hyperte nsion and renal and cardiac disease); the mothers nutritional status and socioeco nomic level; her use of cigarettes, alcohol, and other drugs; placental insuf cien cy; and multiple irths (e.g., twins, triplets). Fetuses that weigh less
124 Part One: General Em ryology Figure 6.6 A 7-month-old fetus. This fetus would e a le to survive. It has well -rounded contours as a result of deposition of su cutaneous fat. Note the twisti ng of the um ilical cord. than 500 g seldom survive, while those that weigh 500 to 1000 g may live if prov ided with expert care. However, approximately 50% of a ies orn weighing less t han 1000 g who survive will have severe neurological de cits. Infants may e full term, ut small ecause of IUGR or small ecause they are orn prematurely.
Chapter 6: Third Month to Birth: The Fetus and Placenta 125 The major growth-promoting factor during development efore and after irth is i nsulinlike growth factor-I (IGF-I), which has mitogenic and ana olic effects. Fe tal tissues express IGF-I and serum levels are correlated with fetal growth. Mut ations in the IGF-I gene result in IUGR and this growth retardation is continued after irth. In contrast to the prenatal period, postnatal growth depends upon growth hormone (GH). This hormone inds to its receptor (GHR), activating a sign al transduction pathway and resulting in synthesis and secretion of IGF-I. Mutat ions in the GHR result in Laron dwar sm, which is characterized y growth retardat ion, midfacial hypoplasia, lue sclera, and limited el ow extension. These indiv iduals show little or no IUGR, since IGF-I production does not depend upon GH du ring fetal development. Fetal Mem ranes and Placenta As the fetus grows, its demands for nutritional and other factors increase causing major changes in the placenta. Foremost among th ese is an increase in surface area etween maternal and fetal components to faci litate exchange. The disposition of fetal mem ranes is also altered as productio n of amniotic uid increases. CHANGES IN THE TROPHOBLAST By the eginning of the s econd month, the tropho last is characterized y a great num er of secondary and tertiary villi that give it a radial appearance (Fig. 6.7). The villi are ancho red in the mesoderm of the chorionic plate and are attached peripherally to the maternal decidua y way of the outer cytotropho last shell. The surface of the v illi is formed y the syncytium, resting on a layer of cytotropho lastic cells t hat in turn cover a core of vascular mesoderm (Fig. 6.8, A and C ). The capillar y system developing in the core of the villous stems soon comes in contact with capillaries of the chorionic plate and connecting stalk, thus giving rise to the extraem ryonic vascular system (see Fig. 5.15). During the following months, nu merous small extensions sprout from existing villous stems into the surrounding lacunar or intervillous spaces. Initially these newly formed villi are primitive (Fig. 6.8C ), ut y the eginning of the fourth month, cytotropho lastic cells and some connective tissue cells disappear. The syncytium and endothelial wall of the lood vessels are then the only layers that separate the maternal and fet al circulations (Fig. 6.8, B and D). Frequently the syncytium ecomes very thin, and large pieces containing several nuclei may reak off and drop into the inte rvillous lood lakes. These pieces, known as syncytial knots, enter the maternal circulation and usually degenerate without causing any symptoms. Disappearance of cytotropho lastic cells progresses from the smaller to larger villi, and alth ough some always persist in large villi, they do not participate in the exchange etween the two circulations.
126 Part One: General Em ryology Figure 6.7 Human em ryo at the eginning of the second month of development. At the em ryonic pole, villi are numerous and well formed; at the a em ryonic pole they are few in num er and poorly developed. CHORION FRONDOSUM AND DECIDUA BASALIS In the early weeks of development, villi c over the entire surface of the chorion (Fig. 6.7). As pregnancy advances, villi on the em ryonic pole continue to grow and expand, giving rise to the chorion fr ondosum ( ushy chorion). Villi on the a em ryonic pole degenerate and y the thi rd month this side of the chorion, now known as the chorion laeve, is smooth (Fi gs. 6.9 and 6.10A). The difference etween the em ryonic and a em ryonic poles o f the chorion is also re ected in the structure of the decidua, the functional lay er of the endometrium, which is shed during parturition. The decidua over the ch orion frondosum, the decidua asalis, consists of a compact layer of large cells , decidual cells, with a undant amounts of lipids and glycogen. This layer, the decidual plate, is tightly connected to the chorion. The decidual layer over the a em ryonic pole is the decidua capsularis (Fig. 6.10A). With growth of the cho rionic vesicle, this layer ecomes stretched and degenerates. Su sequently, the chorion laeve comes into contact with the uterine wall (decidua parietalis)
Chapter 6: Third Month to Birth: The Fetus and Placenta 127 Cytotropho last shell Decidua Spiral artery Intervillous space Blood vessel Cytotropho last A Extraem ryonic mesoderm Syncytium Chorionic plate
Barrier formed y 1. Syncytium 2. Cytotropho last 3. Connective tissue 4. Endoth elium C D Figure 6.8 Structure of villi at various stages of development. A. During the fo urth week. The extraem ryonic mesoderm penetrates the stem villi in the directio n of the decidual plate. B. During the fourth month. In many small villi the wal l of the capillaries is in direct contact with the syncytium. C and D. Enlargeme nt of the villus as shown in A and B, respectively. on the opposite side of the uterus and the two fuse (Figs. 6.10 to 6.12), o lite rating the uterine lumen. Hence the only portion of the chorion participating in the exchange process is the chorion frondosum, which, together with the decidua asalis, makes up the placenta. Similarly, fusion of the amnion and chorion to form the amniochorionic mem rane o literates the chorionic cavity (Fig. 6.10, A and B). It is this mem rane that ruptures during la or ( reaking of the water). Structure of the Placenta By the eginning of the fourth month, the placenta has two components: (a) a fetal portion, formed y the chorion frondosum; and ( ) a maternal portion, formed y the decidua asalis (Fig. 6.10B). On the fetal side , the placenta is ordered y the chorionic plate (Fig. 6.13); on its maternal s ide, it is ordered y the decidua asalis, of which the decidual plate is most intimately incorporated
B Villous lood vessel Barrier formed
y 1. Syncytium 2. Endothelium
128 Part One: General Em ryology Figure 6.9 A 6-week em ryo. The amniotic sac and chorionic cavity have een open ed to expose the em ryo showing the ushy appearance of the tropho last at the e m ryonic pole in contrast to small villi at the a em ryonic pole and the connect ing stalk and yolk sac with its extremely long duct.
Chapter 6: Third Month to Birth: The Fetus and Placenta 129 Figure 6.10 Relation of fetal mem ranes to wall of the uterus. A. End of the sec ond month. Note the yolk sac in the chorionic cavity etween the amnion and chor ion. At the a em ryonic pole, villi have disappeared (chorion laeve). B. End of the third month. The amnion and chorion have fused, and the uterine cavity is o literated y fusion of the chorion laeve and the decidua parietalis. into the placenta. In the junctional zone, tropho last and decidua cells intermi ngle. This zone, characterized y decidual and syncytial giant cells, is rich in amorphous extracellular material. By this time most cytotropho last cells have degenerated. Between the chorionic and decidual plates are the intervillous spac es, which are lled with maternal lood. They are derived from lacunae in the sync ytiotropho last and are lined with syncytium of fetal origin. The villous trees grow into the intervillous lood lakes (Figs. 6.17 and 6.13). During the fourth and fth months the decidua forms a num er of decidual septa, which project into i ntervillous spaces ut do not reach the chorionic plate (Fig. 6.13). These septa have a core of maternal tissue, ut their surface is covered y a layer of sync ytial cells, so that at all times a syncytial layer separates maternal lood in intervillous lakes from fetal tissue of the villi. As a result of this septum fo rmation, the placenta is divided into a num er of compartments, or cotyledons (F ig. 6.14). Since the decidual septa do not reach the chorionic plate, contact e tween intervillous spaces in the various cotyledons is maintained. As a result o f the continuous growth of the fetus and expansion of the uterus, the placenta a lso enlarges. Its increase in surface area roughly parallels that of the expandi ng uterus and throughout pregnancy it covers approximately 15 to 30% of the inte rnal surface of the uterus. The increase in thickness of the placenta results fr om ar orization of existing villi and is not caused y further penetration into maternal tissues.
130 Part One: General Em ryology Figure 6.11 A 19-week-old fetus in its natural position in the uterus showing th e um ilical cord and placenta. The lumen of the uterus is o literated. In the wa ll of the uterus is a large growth, a myo roma. FULL-TERM PLACENTA At full term, the placenta is discoid with a diameter of 15 t o 25 cm, is approximately 3 cm thick, and weighs a out 500 to 600 g. At irth, i t is torn from the uterine wall and, approximately 30 minutes after irth of the child, is expelled from the uterine cavity. After irth, when the placenta is v iewed from the maternal side, 15 to 20 slightly ulging areas, the cotyledons, c overed y a thin layer of decidua asalis, are clearly recogniza le (Fig. 6.14B) . Grooves etween the cotyledons are formed y decidual septa.
Chapter 6: Third Month to Birth: The Fetus and Placenta 131 Figure 6.12 A 23-week-old fetus in the uterus. Portions of the wall of the uteru s and the amnion have een removed to show the fetus. In the ackground are plac ental vessels converging toward the um ilical cord. The um ilical cord is tightl y wound around the a domen, possi ly causing a normal fetal position in the uter us ( reech position). The fetal surface of the placenta is covered entirely y the chorionic plate. A num er of large arteries and veins, the chorionic vessels, converge toward the u m ilical cord (Fig. 6.14A). The chorion, in turn, is covered y the amnion. Atta chment of the um ilical cord is usually eccentric and occasionally even marginal . Rarely, however, does it insert into the chorionic mem ranes outside the place nta (velamentous insertion). CIRCULATION OF THE PLACENTA Cotyledons receive thei r lood through 80 to 100 spiral arteries that pierce the decidual plate and ent er the intervillous spaces at more or less regular
132 Part One: General Em ryology Figure 6.13 The placenta in the second half of pregnancy. The cotyledons are par tially separated y the decidual (maternal) septa. Most of the intervillous loo d returns to the maternal circulation y way of the endometrial veins. A small p ortion enters neigh oring cotyledons. The intervillous spaces are lined y syncy tium. Figure 6.14 A full-term placenta. A. Fetal side. The chorionic plate and um ilic al cord are covered y amnion. B. Maternal side showing the cotyledons. In one a rea the decidua has een removed. The maternal side of the placenta is always ca refully inspected at irth, and frequently one or more cotyledons with a whitish appearance are present ecause of excessive rinoid formation and infarction of a group of intervillous lakes. intervals (Fig. 6.13). The lumen of the spiral artery is narrow, so lood pressu re in the intervillous space is high. This pressure forces the lood deep into t he intervillous spaces and athes the numerous small villi of the villous tree i n oxygenated lood. As the pressure decreases, lood ows ack from the chorionic plate toward the decidua, where it enters the endometrial veins (Fig. 6.13). Hen ce, lood from the intervillous lakes drains ack into the maternal circulation through the endometrial veins. Collectively, the intervillous spaces of a mature placenta contain approximately 150 ml of lood, which is replenished a out 3 or 4 times per minute. This
Chapter 6: Third Month to Birth: The Fetus and Placenta 133
lood moves along the chorionic villi, which have a surface area of 4 to 14 m2 . However, placental exchange does not take place in all villi, only in those who se fetal vessels are in intimate contact with the covering syncytial mem rane. I n these villi, the syncytium often has a rush order consisting of numerous mic rovilli, which greatly increases the surface area and consequently the exchange rate etween maternal and fetal circulations (Fig. 6.8D). The placental mem rane , which separates maternal and fetal lood, is initially composed of four layers : (a) the endothelial lining of fetal vessels; ( ) the connective tissue in the villus core; (c) the cytotropho lastic layer; and (d) the syncytium (Fig. 6.8C ) . From the fourth month on, however, the placental mem rane thins, since the end othelial lining of the vessels comes in intimate contact with the syncytial mem rane, greatly increasing the rate of exchange (Fig. 6.8D). Sometimes called the placental arrier, the placental mem rane is not a true arrier, since many su s tances pass through it freely. Because the maternal lood in the intervillous sp aces is separated from the fetal lood y a chorionic derivative, the human plac enta is considered to e of the hemochorial type. FUNCTION OF THE PLACENTA Main functions of the placenta are (a) exchange of meta olic and gaseous products et ween maternal and fetal loodstreams and ( ) production of hormones. Exchange of Gases Exchange of gases, such as oxygen, car on dioxide, and car on monoxide, i s accomplished y simple diffusion. At term, the fetus extracts 20 to 30 ml of o xygen per minute from the maternal circulation and even a short-term interruptio n of the oxygen supply is fatal to the fetus. Placental lood ow is critical to o xygen supply, since the amount of oxygen reaching the fetus primarily depends on delivery, not diffusion. Exchange of Nutrients and Electrolytes Exchange of nut rients and electrolytes, such as amino acids, free fatty acids, car ohydrates, a nd vitamins, is rapid and increases as pregnancy advances. Transmission of Mater nal Anti odies Immunological competence egins to develop late in the rst trimest er, y which time the fetus makes all of the components of complement. Immunoglo ulins consist almost entirely of maternal immunoglo ulin G (IgG) that egins to e transported from mother to fetus at approximately 14 weeks. In this manner, the fetus gains passive immunity against various infectious diseases. New orns egin to produce their own IgG, ut adult levels are not attained until the age o f 3 years.
134 Part One: General Em ryology CLINICAL CORRELATES Erythro lastosis Fetalis and Fetal Hydrops Over 400 red lood cell antigens have een identi ed, and although most do not cause pro lems during pregnancy, some ca n stimulate a maternal anti ody response against fetal lood cells. This process is an example of isoimmunozation, and if the maternal response is suf cient, the anti odies will attack and hemolyze fetal red lood cells resulting in hemolytic disease of the new orn (erythro lastosis fetalis). The anemia may ecome so sev ere that fetal hydrops (edema and effusions into the ody cavities) occurs, lead ing to fetal death. Most severe cases are caused y antigens from the CDE (Rhesu s) lood group system. The D or Rh antigen is the most dangerous, since immuniza tion can result from a single exposure and occurs earlier and with greater sever ity with each succeeding pregnancy. The anti ody response occurs in cases where the fetus is D(Rh) positive and the mother is D(Rh) negative and is elicited whe n fetal red lood cells enter the maternal system due to small areas of leeding at the surface of placental villi or at irth. Analysis of amniotic uid for ili ru in, a reakdown product of hemoglo in, serves as a measure of the degree of r ed cell hemolysis. Treatment for the affected fetus involves intrauterine or pos tnatal transfusions. However, the disease is prevented y identifying women at r isk using an anti ody screen and treating them with anti-D-immunoglo ulin. Antig ens from the ABO lood group can also elicit an anti ody response, ut the effec ts are much milder than those produced y the CDE group. A out 20% of all infant s have an ABO maternal incompati ility, ut only 5% will e clinically affected. These can e effectively treated postnatally. Hormone Production By the end of the fourth month the placenta produces progeste rone in suf cient amounts to maintain pregnancy if the corpus luteum is removed or fails to function properly. In all pro a ility, all hormones are synthesized in the syncytial tropho last. In addition to progesterone, the placenta produces i ncreasing amounts of estrogenic hormones, predominantly estriol, until just efo re the end of pregnancy, when a maximum level is reached. These high levels of e strogens stimulate uterine growth and development of the mammary glands. During the rst two months of pregnancy, the syncytiotropho last also produces human chor ionic gonadotropin (hCG), which maintains the corpus luteum. This hormone is exc reted y the mother in the urine, and in the early stages of gestation, its pres ence is used as an indicator of pregnancy. Another hormone produced y the place nta is somatomammotropin (formerly placental lactogen). It is a growth hormone-l ike su stance that gives the fetus priority on maternal lood glucose and makes the mother somewhat dia etogenic. It also promotes reast development for milk p roduction.
Chapter 6: Third Month to Birth: The Fetus and Placenta CLINICAL CORRELATES 135 The Placental Barrier Most maternal hormones do not cross the placenta. The horm ones that do cross, such as thyroxine, do so only at a slow rate. Some synthetic progestins rapidly cross the placenta and may masculinize female fetuses. Even more dangerous was the use of the synthetic estrogen diethylstil estrol, which e asily crosses the placenta. This compound produced carcinoma of the vagina and a normalities of the testes in individuals who were exposed to it during their in trauterine life (see Chapter 7). Although the placental arrier is frequently co nsidered to act as a protective mechanism against damaging factors, many viruses , such as ru ella, cytomegalovirus, Coxsackie, variola, varicella, measles, and poliomyelitis virus, traverse the placenta without dif culty. Once in the fetus, s ome viruses cause infections, which may result in cell death and irth defects ( see Chapter 7). Unfortunately, most drugs and drug meta olites traverse the plac enta without dif culty, and many cause serious damage to the em ryo (see Chapter 7 ). In addition, maternal use of heroin and cocaine can cause ha ituation in the fetus.
Amnion and Um ilical Cord The oval line of re ection etween the amnion and em ryo nic ectoderm (amnio-ectodermal junction) is the primitive um ilical ring. At the fth week of development, the following structures pass through the ring (Fig. 6. 15, A and C ): (a) the connecting stalk, containing the allantois and the um ili cal vessels, consisting of two arteries and one vein; ( ) the yolk stalk (vitell ine duct), accompanied y the vitelline vessels; and (c) the canal connecting th e intraem ryonic and extraem ryonic cavities (Fig. 6.15C ). The yolk sac proper occupies a space in the chorionic cavity, that is, the space etween the amnion and chorionic plate (Fig. 6.15B). During further development, the amniotic cavit y enlarges rapidly at the expense of the chorionic cavity, and the amnion egins to envelop the connecting and yolk sac stalks, crowding them together and givin g rise to the primitive um ilical cord (Fig. 6.15B). Distally the cord contains the yolk sac stalk and um ilical vessels. More proximally it contains some intes tinal loops and the remnant of the allantois (Fig. 6.15, B and D). The yolk sac, found in the chorionic cavity, is connected to the um ilical cord y its stalk. At the end of the third month, the amnion has expanded so that it comes in cont act with the chorion, o literating the chorionic cavity (Fig. 6.10B). The yolk s ac then usually shrinks and is gradually o literated. The a dominal cavity is te mporarily too small for the rapidly developing intestinal loops and some of them are pushed into the extraem ryonic space in the um ilical cord. These extruding intestinal loops form a physiological
136 Part One: General Em ryology Figure 6.15 A. A 5-week em ryo showing structures passing through the primitive um ilical ring. B. The primitive um ilical cord of a 10-week em ryo. C. Transver se section through the structures at the level of the um ilical ring. D. Transve rse section through the primitive um ilical cord showing intestinal loops protru ding in the cord. um ilical hernia (see Chapter 13). At approximately the end of the third month, the loops are withdrawn into the ody of the em ryo and the cavity in the cord i s o literated. When the allantois and the vitelline duct and its vessels are als o o literated, all that remains in the cord are the um ilical vessels surrounded y the jelly of Wharton. This tissue, which is rich in proteoglycans, functions as a protective layer for the lood vessels. The walls of the arteries are musc ular and contain many elastic ers, which contri ute to a rapid constriction and contraction of the um ilical vessels after the cord is tied off. CLINICAL CORRELATES Um ilical Cord A normalities At irth, the um ilical cord is approximately 2 cm in diameter and 50 to 60 cm long. It is tortuous, causing false knots. An extrem ely long cord may encircle
Chapter 6: Third Month to Birth: The Fetus and Placenta 137 Figure 6.16 Infant showing lim amputation resulting from amniotic ands. the neck of the fetus, usually without increased risk, whereas a short one may c ause dif culties during delivery y pulling the placenta from its attachment in th e uterus. Normally there are two arteries and one vein in the um ilical cord. In 1 in 200 new orns, however, only one artery is present, and these a ies have a pproximately a 20% chance of having cardiac and other vascular defects. The miss ing artery either fails to form (agenesis) or degenerates early in development. Amniotic Bands Occasionally, tears in the amnion result in amniotic ands that m ay encircle part of the fetus, particularly the lim s and digits. Amputations, r ing constrictions, and other a normalities, including craniofacial deformations, may result (Fig. 6.16). Origin of the ands is pro a ly from infection or toxic insults that involve either the fetus, fetal mem ranes, or oth. Bands then for m from the amnion, like scar tissue, constricting fetal structures. Placental Changes at the End of Pregnancy At the end of pregnancy, a num er of c hanges that occur in the placenta may indicate reduced exchange etween the two circulations. These changes
138 Part One: General Em ryology include (a) an increase in rous tissue in the core of the villus, ( ) thickening of asement mem ranes in fetal capillaries, (c) o literative changes in small c apillaries of the villi, and (d) deposition of rinoid on the surface of the vill i in the junctional zone and in the chorionic plate. Excessive rinoid formation frequently causes infarction of an intervillous lake or sometimes of an entire c otyledon. The cotyledon then assumes a whitish appearance. Amniotic Fluid The amniotic cavity is lled with a clear, watery uid that is produc ed in part y amniotic cells ut is derived primarily from maternal lood. The a mount of uid increases from approximately 30 ml at 10 weeks of gestation to 450 m l at 20 weeks to 800 to 1000 ml at 37 weeks. During the early months of pregnanc y, the em ryo is suspended y its um ilical cord in this uid, which serves as a p rotective cushion. The uid (a) a sor s jolts, ( ) prevents adherence of the em ry o to the amnion, and (c) allows for fetal movements. The volume of amniotic uid i s replaced every 3 hours. From the eginning of the fth month, the fetus swallows its own amniotic uid and it is estimated that it drinks a out 400 ml a day, a ou t half of the total amount. Fetal urine is added daily to the amniotic uid in the fth month, ut this urine is mostly water, since the placenta is functioning as an exchange for meta olic wastes. During child irth, the amnio-chorionic mem ran e forms a hydrostatic wedge that helps to dilate the cervical canal. CLINICAL CORRELATES Amniotic Fluid Hydramnios or polyhydramnios is the term used to descri e an exce ss of amniotic uid (15002000 ml), whereas oligohydramnios refers to a decreased am ount (less than 400 ml). Both conditions are associated with an increase in the incidence of irth defects. Primary causes of hydramnios include idiopathic caus es (35%), maternal dia etes (25%), and congenital malformations, including centr al nervous system disorders (e.g., anencephaly) and gastrointestinal defects (at resias, e.g., esophageal) that prevent the infant from swallowing the uid. Oligoh ydramnios is a rare occurrence that may result from renal agenesis. Premature ru pture of the amnion, the most common cause of preterm la or, occurs in 10% of pr egnancies. Furthermore, clu foot and lung hypoplasia may e caused y oligohydra mnios following amnion rupture. Causes of rupture are largely unknown, ut in so me cases trauma plays a role.
Chapter 6: Third Month to Birth: The Fetus and Placenta 139 Fetal Mem ranes in Twins Arrangement of fetal mem ranes in twins varies consider a ly, depending on the type of twins and on the time of separation of monozygoti c twins. DIZYGOTIC TWINS Approximately two-thirds of twins are dizygotic, or fra ternal, and their incidence of 7 to 11 per 1000 irths increases with maternal a ge. They result from simultaneous shedding of two oocytes and fertilization y d ifferent spermatozoa. Since the two zygotes have totally different genetic const itutions, the twins have no more resem lance than any other rothers or sisters. They may or may not e of different sex. The zygotes implant individually in th e uterus, and usually each develops its own placenta, amnion, and chorionic sac (Fig. 6.17A). Sometimes, however, the two placentas are so close together that t hey fuse. Similarly, the walls of the chorionic sacs may also come into close ap position and fuse (Fig. 6.17B). Occasionally, each dizygotic twin possesses red lood cells of two different types (erythrocyte mosaicism), indicating that fusi on of the two placentas was so intimate that red cells were exchanged. MONOZYGOT IC TWINS The second type of twins, which develops from a single fertilized ovum, is monozygotic, or identical, twins. The rate for monozygotic twins is 3 to 4 p er 1000. They result from splitting of the zygote at various stages of developme nt. The earliest separation is elieved to occur at the two-cell stage, in which case two separate zygotes develop. The lastocysts implant separately, and each em ryo has its own placenta and chorionic sac (Fig. 6.18A). Although the arrang ement of the mem ranes of these twins resem les that of dizygotic twins, the two can e recognized as partners of a monozygotic pair y their strong resem lance in lood groups, ngerprints, sex, and external appearance, such as eye and hair color. Splitting of the zygote usually occurs at the early lastocyst stage. The inner cell mass splits into two separate groups of cells within the same lasto cyst cavity (Fig. 6.18B ). The two em ryos have a common placenta and a common c horionic cavity, ut separate amniotic cavities (Fig. 6.18B). In rare cases the separation occurs at the ilaminar germ disc stage, just efore the appearance o f the primitive streak (Fig. 6.18C ). This method of splitting results in format ion of two partners with a single placenta and a common chorionic and amniotic s ac. Although the twins have a common placenta, lood supply is usually well ala nced. Although triplets are rare (a out 1/7600 pregnancies), irth of quadruplet s, quintuplets, and so forth is rarer. In recent years multiple irths have occu rred more frequently in mothers given gonadotropins (fertility drugs) for ovulat ory failure.
Figure 6.17 Development of dizygotic twins. Normally each em ryo has its own amn ion, chorion, and placenta, A, ut sometimes the placentas are fused, B. Each em ryo usually receives the appropriate amount of lood, ut on occasion large ana stomoses shunt more lood to one of the partners than to the other.
Chapter 6: Third Month to Birth: The Fetus and Placenta 141 2-cell-stage zygote Inner cell mass Blastocyst cavity Amniotic cavity Yolk sac Amniotic cavity Common chorionic cavity Common placenta Common amniotic cavity Figure 6.18 Possi le relations of fetal mem ranes in monozygotic twins. A. Split ting occurs at the two-cell stage, and each em ryo has its own placenta, amnioti c cavity, and chorionic cavity. B. Splitting of the inner cell mass into two com pletely separated groups. The two em ryos have a common placenta and a common ch orionic sac ut separate amniotic cavities. C. Splitting of the inner cell mass at a late stage of development. The em ryos have a common placenta, a common amn iotic cavity, and a common chorionic cavity.
142 Part One: General Em ryology CLINICAL CORRELATES Twin Defects Twin pregnancies have a high incidence of perinatal mortality and m or idity and a tendency toward preterm delivery. Approximately 12% of premature infants are twins and twins are usually small at irth. Low irth weight and pre maturity place infants of twin pregnancies at great risk, and approximately 10 t o 20% of them die, compared with only 2% of infants from single pregnancies. The incidence of twinning may e much higher, since twins are conceived more often than they are orn. Many twins die efore irth and some studies indicate that o nly 29% of women pregnant with twins actually give irth to two infants. The ter m vanishing twin refers to the death of one fetus. This disappearance, which occ urs in the rst trimester or early second trimester, may result from resorption or formation of a fetus papyraceus (Fig. 6.19). Another pro lem leading to increas ed mortality among twins is the twin transfusion syndrome, which occurs in 5 to 15% of monochorionic Figure 6.19 Fetus papyraceus. One twin is larger, and the other has een compres sed and mummi ed, hence the term papyraceus.
Chapter 6: Third Month to Birth: The Fetus and Placenta 143 monozygotic pregnancies. In this condition, placental vascular anastomoses, whic h occur in a alanced arrangement in most monochorionic placentas, are formed so that one twin receives most of the lood ow and ow to the other is compromised. A s a result, one twin is larger than the other (Fig. 6.20). The outcome is poor, with the death of oth twins occurring in 60 to 100% of cases. At later stages o f development, partial splitting of the primitive node and streak may result in formation of conjoined (Siamese) twins. These twins are classi ed according to the nature and degree of union as thoracopagus (pagos, fastened); pygopagus; and cr aniopagus (Figs. 6.21 and 6.22). Occasionally, monozygotic twins are connected o nly y a common skin ridge or y a common liver ridge. The type of twins forme d depends upon when and to what extent a normalities of the node and streak occu rred. Mis-expression of genes, such as Goosecoid, may also result in conjoined t wins. Many conjoined twins have survived, including the most famous pair, Chang and Eng, who were joined at the a domen and who traveled to England and the Unit ed States on exhi itions in the mid-1800s. Finally settling in North Carolina, t hey farmed and fathered 21 children with their two wives. Figure 6.20 Monozygotic twins with twin transfusion syndrome. Placental vascular anastomoses produced un alanced lood ow to the two fetuses.
144 Part One: General Em ryology Figure 6.21 Thoracopagus, pygopagus, and craniopagus twins. Conjoined twins can e separated only if they have no vital parts in common.
Parturition (Birth) For the rst 34 to 38 weeks of gestation, the uterine myometri um does not respond to signals for parturition ( irth). However, during the last 2 to 4 weeks of pregnancy, this tissue undergoes a transitional phase in prepar ation for the onset of la or. Ultimately, this phase ends with a thickening of t he myometrium in the upper region of the uterus and a softening and thinning of the lower region and cervix. La or itself is divided into three stages: 1) effac ement (thinning and shortening) and dilatation of the cervix; this stage ends wh en the cervix is fully dilated; 2) delivery of the fetus; and 3) delivery of the placenta and fetal mem ranes. Stage 1 is produced y uterine contractions that force the amniotic sac against the cervical canal like a wedge or, if the mem ra nes have ruptured, then pressure will e exerted y the presenting part of the f etus, usually the head. Stage 2 is also assisted y uterine contractions, ut th e most important force is provided y increased intra-a dominal pressure from co ntraction of a dominal muscles. Stage 3 requires uterine contractions and is aid ed y increasing intra-a dominal pressure. As the uterus contracts, the upper pa rt retracts creating a smaller and smaller lumen, while the lower part expands, there y producing direction to the force. Contractions usually egin a out 10 mi nutes apart; then, during the second stage of la or, they may occur less than 1 minute apart and last from 30 to 90 seconds. Their occurrence in pulses is essen tial to fetal survival, since they are of suf cient force to compromise uteroplace ntal lood ow to the fetus. CLINICAL CORRELATES Preterm Birth Factors initiating la or are not known and may involve: retreat fro m maintenance of pregnancy in which pregnancy supporting factors (e.g., hormones,
Chapter 6: Third Month to Birth: The Fetus and Placenta 145 Figure 6.22 Conjoined twins. A. Twins with two heads, a road thorax, two spines , two partially fused hearts, four lungs, and a duplicated gut down to the ileum . B. Twins joined at the head (craniopagus) with multiple deformations of the li m s. etc.) are withdrawn; or active induction caused y stimulatory factors targeting the uterus. Pro a ly, components of oth phenomena are involved. Unfortunately, a lack of knowledge a out these factors has restricted progress in preventing p reterm irth. Preterm irth (delivery efore 34 weeks) of premature infants is t he second leading cause of infant mortality in the United States and also contri utes signi cantly to mor idity. It is due to premature
146 Part One: General Em ryology rupture of the mem ranes, premature onset of la or, or pregnancy complications r equiring premature delivery. Maternal hypertension and dia etes as well as a rup tio placenta are risk factors. Maternal infections, including acterial vaginosi s, are also associated with an increased risk. Summary The fetal period extends from the ninth week of gestation until irth an d is characterized y rapid growth of the ody and maturation of organ systems. Growth in length is particularly striking during the third, fourth, and fth month s (approximately 5 cm per month), while increase in weight is most striking duri ng the last 2 months of gestation (approximately 700 g per month) (Ta le 6.1; p. 118). A striking change is the relative slowdown in the growth of the head. In the third month, it is a out half of CRL. By the fth month the size of the head i s a out one-third of CHL, and at irth it is one-fourth of CHL (Fig. 6.2). Durin g the fth month, fetal movements are clearly recognized y the mother, and the fe tus is covered with ne, small hair. A fetus orn during the sixth or the eginnin g of the seventh month has dif culty surviving, mainly ecause the respiratory and central nervous systems have not differentiated suf ciently. In general, the leng th of pregnancy for a full-term fetus is considered to e 280 days, or 40 weeks after onset of the last menstruation or, more accurately, 266 days or 38 weeks a fter fertilization. The placenta consists of two components: (a) a fetal portion , derived from the chorion frondosum or villous chorion, and ( ) a maternal port ion, derived from the decidua asalis. The space etween the chorionic and decid ual plates is lled with intervillous lakes of maternal lood. Villous trees (feta l tissue) grow into the maternal lood lakes and are athed in them. The fetal c irculation is at all times separated from the maternal circulation y (a) a sync ytial mem rane (a chorion derivative) and ( ) endothelial cells from fetal capil laries. Hence the human placenta is of the hemochorial type. Intervillous lakes of the fully grown placenta contain approximately 150 ml of maternal lood, whic h is renewed 3 or 4 times per minute. The villous area varies from 4 to 14 m2 , facilitating exchange etween mother and child. Main functions of the placenta a re (a) exchange of gases; ( ) exchange of nutrients and electrolytes; (c) transm ission of maternal anti odies, providing the fetus with passive immunity; (d) pr oduction of hormones, such as progesterone, estradiol, and estrogen (in addition , it produces hCG and somatomammotropin); and (e) detoxi cation of some drugs. The amnion is a large sac containing amniotic uid in which the fetus is suspended y its um ilical cord. The uid (a) a sor s jolts, ( ) allows for fetal movements, a nd (c) prevents adherence of the em ryo to surrounding
Chapter 6: Third Month to Birth: The Fetus and Placenta 147 tissues. The fetus swallows amniotic uid, which is a sor ed through its gut and c leared y the placenta. The fetus adds urine to the amniotic uid, ut this is mos tly water. An excessive amount of amniotic uid (hydramnios) is associated with an encephaly and esophageal atresia, whereas an insuf cient amount (oligohydramnios) is related to renal agenesis. The um ilical cord, surrounded y the amnion, cont ains (a) two um ilical arteries, ( ) one um ilical vein, and (c) Whartons jelly, which serves as a protective cushion for the vessels. Fetal mem ranes in twins v ary according to their origin and time of formation. Two-thirds of twins are diz ygotic, or fraternal; they have two amnions, two chorions, and two placentas, wh ich sometimes are fused. Monozygotic twins usually have two amnions, one chorion , and one placenta. In cases of conjoined twins, in which the fetuses are not en tirely split from each other, there is one amnion, one chorion, and one placenta . Signals initiating parturition ( irth) are not clear, ut preparation for la o r usually egins etween 34 and 38 weeks. La or itself consists of three stages: 1) effacement and dilatation of the cervix; 2) delivery of the fetus; and 3) de livery of the placenta and fetal mem ranes. Pro lems to Solve 1. An ultrasound at 7 months of gestation shows too much space ( uid accumulation) in the amniotic cavity. What is this condition called, and w hat are its causes? 2. Later in her pregnancy a woman realizes that she was pro a ly exposed to toluene in the workplace during the third week of gestation ut tells a fellow worker that she is not concerned a out her a y ecause the place nta protects her infant from toxic factors y acting as a arrier. Is she correc t? SUGGESTED READING Amselem S, et al.: Laron dwar sm and mutations in the growth hor mone receptor gene. N Engl J Med 321:989, 1989. Barnea ER, Hustin J, Jauniaux E (eds): The First Twelve Weeks of Gestation. Berlin, Springer-Verlag, 1992. Basse tt JM: Current perspectives on placental development and its integration with fe tal growth. Proc Nutr Soc 50:311, 1991. Benirschke K, Kaufman P: The Pathology o f the Human Placenta. Berlin, Springer-Verlag, 1990. Cunningham FG, Gant NF, Lev eno KJ, Gilstrap LC, Hauth JC, Wenstrom KD: Fetal growth and development. In Wil liams O stetrics. New York, McGraw Hill, 2001. Cunningham FG, Gant NF, Leveno KJ , Gilstrap LC, Hauth JC, Wenstrom KD: Parturition. In Williams O stetrics. New Y ork, McGraw Hill, 2001. Levi S: Ultrasonic assessment of the high rate of human multiple pregnancy in the rst trimester. J Clin Ultrasound 4:3, 1976. Naeye RL: D isorders of the Placenta, Fetus, and Neonate. St Louis, Mos yYear Book, 1992.
148 Part One: General Em ryology Ny erg DA, Callan PW: Ultrasound evaluation of the placenta. In Callen PW (ed): Ultrasonography in O stetrics and Gynecology. 2nd ed. Philadelphia, WB Saunders, 1988. Peipert JF, Donnenfeld AE: Oligohydramnios: a review. O stet Gynecol 46:3 25, 1991. Petraglia F, et al.: Neuroendocrine mechanisms regulating placental ho rmone production. Contri Gynecol O stet 18:147, 1991. Schnaufer L: Conjoined tw ins. In Raffensperger JG (ed): Swensons Pediatric Surgery. 5th ed. Norwalk, CT, A ppleton & Lange, 1990. Spencer R: Conjoined twins: theoretical em ryologic asis . Teratology 45:591, 1992. Wallace I, Wallace A: The Two. New York, Simon and Sc huster, 1978. Wilcox AJ, Wein erg CR, Baird DD: Timing of sexual intercourse in relation to ovulation. N Engl J Med 333:1517, 1995.
chapter 7 Birth Defects and Prenatal Diagnosis Birth Defects Birth defect, congenital malformation, and congenital anomaly are synonymous terms used to descri e structural, ehavioral, functional, and meta o lic disorders present at irth. The science that studies these disorders is tera tology (Gr. teratos, monster). Major structural anomalies occur in 2 to 3% of li ve orn infants, and an additional 2 to 3% are recognized in children y age 5 ye ars, for a total of 4 to 6%. Birth defects are the leading cause of infant morta lity, accounting for approximately 21% of infant deaths. They are the fth leading cause of years of potential life lost prior to age 65 and a major contri utor t o disa ilities. They are also nondiscriminatory; mortality rates produced y ir th defects are the same for Asians, African Americans, Latin Americans, whites, and Native Americans. In 40 to 60% of persons with irth defects, the cause is u nknown. Genetic factors, such as chromosome a normalities and mutant genes, acco unt for approximately 15%; environmental factors produce approximately 10%; a co m ination of genetic and environmental in uences (multifactorial inheritance) prod uces 20 to 25%; and twinning causes 0.5 to 1%. Minor anomalies occur in approxim ately 15% of new orns. These structural a normalities, such as microtia (small e ars), pigmented spots, and short palpe ral ssures, are not themselves detrimental to health 149
150 Part One: General Em ryology
ut, in some cases, are associated with major defects. For example, infants with one minor anomaly have a 3% chance of having a major malformation; those with t wo minor anomalies have a 10% chance; and those with three or more minor anomali es have a 20% chance. Therefore, minor anomalies serve as clues for diagnosing m ore serious underlying defects. In particular, ear anomalies are easily recogniz a le indicators of other defects and are o served in virtually all children with syndromic malformations. TYPES OF ABNORMALITIES Malformations occur during form ation of structures, for example during organogenesis. They may result in comple te or partial a sence of a structure or in alterations of its normal con guration. Malformations are caused y environmental and/or genetic factors acting indepen dently or in concert. Most malformations have their origin during the third to e ighth weeks of gestation. Disruptions result in morphological alterations of alr eady formed structures and are due to destructive processes. Vascular accidents leading to owel atresias (see Chapter 13; p. 296) and defects produced y amnio tic ands are examples of destructive factors that produce disruptions. Deformat ions are due to mechanical forces that mold a part of the fetus over a prolonged period. Clu feet, for example, are due to compression in the amniotic cavity. D eformations often involve the musculoskeletal system and may e reversi le postn atally. A syndrome is a group of anomalies occurring together that have a speci c common cause. This term indicates that a diagnosis has een made and that the ri sk of recurrence is known. In contrast, association is the nonrandom appearance of two or more anomalies that occur together more frequently than y chance alon e, ut whose cause has not een determined. Examples include CHARGE (Colo omas, Heart defects, Atresia of the choanae, Retarded growth, Genital anomalies, and E ar a normalities) and VACTERL (Verte ral, Anal, Cardiac, Tracheo Esophageal, Ren al, and Lim anomalies). Although they do not constitute a diagnosis, associatio ns are important ecause recognition of one or more of the components promotes t he search for others in the group. ENVIRONMENTAL FACTORS Until the early 1940s i t was assumed that congenital defects were caused primarily y hereditary factor s. With the discovery y Gregg that German measles affecting a mother during ear ly pregnancy caused a normalities in the em ryo, it suddenly ecame evident that congenital malformations in humans could also e caused y environmental factor s. In 1961 o servations y Lenz linked lim defects to the sedative thalidomide and made it clear that drugs could also cross the placenta and produce irth def ects (Fig. 7.1). Since that
Chapter 7: Birth Defects and Prenatal Diagnosis 151 Figure 7.1 A. Child with unilateral amelia. B. Child with meromelia. The hand is attached to the trunk y an irregularly shaped one. Both infants were orn to mothers who took thalidomide. time many agents have ts) (Ta le 7.1). een identi ed as teratogens (factors that cause irth defec
Principles of Teratology Factors determining the capacity of an agent to produce irth defects have een de ned and set forth as the principles of teratology. The y include the following: 1. Suscepti ility to teratogenesis depends on the genot ype of the conceptus and the manner in which this genetic composition interacts with the environment. The maternal genome is also important with respect to drug meta olism, resistance to infection, and other iochemical and molecular proces ses that affect the conceptus. 2. Suscepti ility to teratogens varies with the d evelopmental stage at the time of exposure. The most sensitive period for induci ng irth defects is the third to eighth weeks of gestation, the period of em ryo genesis. Each organ system may have one or more stages of suscepti ility. For ex ample, cleft palate can e induced at the lastocyst stage (day 6),
152 Part One: General Em ryology TABLE 7.1 Teratogens Associated With Human Malformations Congenital Malformations Teratogen Infectious agents Ru ella virus Cytomegalovirus Herpes simplex virus V aricella virus HIV Toxoplasmosis Syphilis Physical agents X-rays Hyperthermia Ch emical agents Thalidomide Aminopterin Diphenylhydantoin (phenytoin) Valproic aci d Trimethadione Lithium Amphetamines Warfarin ACE inhi itors Cocaine Alcohol Iso tretinoin (vitamin A) Industrial solvents Organic mercury Lead Hormones Androgen ic agents (ethisterone, norethisterone) Diethylstil estrol (DES) Maternal dia et es Cataracts, glaucoma, heart defects, deafness, teeth Microcephaly, lindness, men tal retardation, fetal death Microphthalmia, microcephaly, retinal dysplasia Lim hypoplasia, mental retardation, muscle atrophy Microcephaly, growth retardatio n Hydrocephalus, cere ral calci cations, microphthalmia Mental retardation, deafne ss Microcephaly, spina i da, cleft palate, lim defects Anencephaly, spina i da, m ental retardation, facial defects Lim defects, heart malformations Anencephaly, hydrocephaly, cleft lip and palate Fetal hydantoin syndrome: facial defects, me ntal retardation Neural tu e defects, heart, craniofacial, and lim anomalies Cl eft palate, heart defects, urogenital and skeletal a normalities Heart malformat ions Cleft lip and palate, heart defects Chondrodysplasia, microcephaly Growth r etardation, fetal death Growth retardation, microcephaly, ehavioral a normaliti es, gastroschisis Fetal alcohol syndrome, short palpe ral ssures, maxillary hypop lasia, heart defects, mental retardation Vitamin A em ryopathy: small, a normall y shaped ears, mandi ular hypoplasia, cleft palate, heart defects Low irth weig ht, craniofacial and neural tu e defects Neurological symptoms similar to those of cere ral palsy Growth retardation, neurological disorders Masculinization of female genitalia: fused la ia, clitoral hypertrophy Malformation of the uterus, uterine tu es, and upper vagina; vaginal cancer; malformed testes Variety of mal formations; heart and neural tu e defects most common
Chapter 7: Birth Defects and Prenatal Diagnosis 153 during gastrulation (day 14), at the early lim ud stage ( fth week), or when the palatal shelves are forming (seventh week). Furthermore, while most a normaliti es are produced during em ryogenesis, defects may also e induced efore or afte r this period; no stage of development is completely safe. 3. Manifestations of a normal development depend on dose and duration of exposure to a teratogen. 4. Teratogens act in speci c ways (mechanisms) on developing cells and tissues to ini tiate a normal em ryogenesis (pathogenesis). Mechanisms may involve inhi ition o f a speci c iochemical or molecular process; pathogenesis may involve cell death, decreased cell proliferation, or other cellular phenomena. 5. Manifestations of a normal development are death, malformation, growth retardation, and functiona l disorders. Infectious Agents Infectious agents that cause irth defects (Ta le 7.1) include a num er of viruses. Ru ella used to e a major pro lem, ut the a ility to detect serum anti ody titers and development of a vaccine have signi can tly lowered the incidence of irth defects from this cause. Today approximately 85% of women are immune. Cytomegalovirus is a serious threat. Often, the mother has no symptoms, ut the effects on the fetus can e devastating. The infection is often fatal, and if it is not, meningoencephalitis caused y the virus produc es mental retardation. Herpes simplex, varicella, and human immunode ciency (HIV) viruses can cause irth defects. Herpes-induced a normalities are rare, and usua lly infection is transmitted as a venereal disease to the child during delivery. Similarly, HIV (the cause of acquired immunode ciency syndrome, or AIDS) appears to have a low teratogenic potential. Infection with varicella causes a 20% incid ence of irth defects. Other Viral Infections and Hyperthermia Malformations fol lowing maternal infection with measles, mumps, hepatitis, poliomyelitis, ECHO vi rus, Coxsackie virus, and in uenza virus have een descri ed. Prospective studies indicate that the malformation rate following exposure to these agents is low if not nonexistent. A complicating factor introduced y these and other infectious agents is that most are pyrogenic, and elevated ody temperature (hyperthermia) is teratogenic. Defects produced y exposure to elevated temperatures include a nencephaly, spina i da, mental retardation, micropthalmia, and facial a normaliti es. In addition to fe rile illnesses, use of hot tu s and saunas can produce suf c ient temperature elevations to cause irth defects.
154 Part One: General Em ryology Toxoplasmosis and syphilis cause irth defects. Poorly cooked meat; domestic ani mals, especially cats; and feces in contaminated soil can carry the protozoan pa rasite Toxoplasmosis gondii. A characteristic feature of fetal toxoplasmosis inf ection is cere ral calci cations. Radiation Ionizing radiation kills rapidly proli ferating cells, so it is a potent teratogen, producing virtually any type of ir th defect depending upon the dose and stage of development of the conceptus at t he time of exposure. Radiation from nuclear explosions is also teratogenic. Amon g women survivors pregnant at the time of the atomic om explosions over Hirosh ima and Nagasaki, 28% a orted, 25% gave irth to children who died in their rst y ear of life, and 25% had severe irth defects involving the central nervous syst em. Radiation is also a mutagenic agent and can lead to genetic alterations of g erm cells and su sequent malformations. Chemical Agents The role of chemical age nts and pharmaceutical drugs in the production of a normalities in humans is dif c ult to assess for two reasons: (a) most studies are retrospective, relying on th e mothers memory for a history of exposure; and ( ) pregnant women take a large n um er of pharmaceutical drugs. A National Institutes of Health study discovered that pregnant women took 900 different drugs, for an average of 4 per woman. Onl y 20% of pregnant women used no drugs during their pregnancy. Even with this wid espread use of chemical agents, relatively few of the many drugs used during pre gnancy have een positively identi ed as eing teratogenic. One example is thalido mide, an antinauseant and sleeping pill. In 1961 it was noted in West Germany th at the frequency of amelia and meromelia (total or partial a sence of the extrem ities), a rare hereditary a normality, had suddenly increased (Fig. 7.1). This o servation led to examination of the prenatal histories of affected children and to the discovery that many mothers had taken thalidomide early in pregnancy. Th e causal relation etween thalidomide and meromelia was discovered only ecause the drug produced such an unusual a normality. If the defect had een a more com mon type, such as cleft lip or heart malformation, the association with the drug might easily have een overlooked. Other drugs with teratogenic potential inclu de the anticonvulsants diphenylhydantoin (phenytoin), valproic acid, and trimeth adione, which are used y epileptic women. Speci cally, trimethadione and diphenyl hydantoin produce a road spectrum of a normalities that constitute distinct pat terns of dysmorphogenesis known as the trimethadione and fetal hydantoin syndrom es. Facial clefts are particularly common to these syndromes. Valproic acid also causes craniofacial a normalities ut has a particular propensity for producing neural tu e defects.
Chapter 7: Birth Defects and Prenatal Diagnosis 155 Antipsychotic and antianxiety agents (major and minor tranquilizers, respectivel y) are suspected producers of congenital malformations. The antipsychotics pheno thiazine and lithium have een implicated as teratogens. Although evidence for t he teratogenicity of phenothiazines is con icting, that concerning lithium is ett er documented. In any case, it has een strongly suggested that use of these age nts during pregnancy carries a high risk. Similar o servations have een made fo r the antianxiety agents mepro amate, chlordiazepoxide, and diazepam (Valium). A prospective study showed that severe anomalies occurred in 12% of fetuses expos ed to mepro amate and 11% in those exposed to chlordiazepoxide, compared with 2. 6% of controls. Likewise, retrospective studies demonstrate up to a fourfold inc rease in cleft lip with or without cleft palate in offspring whose mothers took diazepam during pregnancy. The anticoagulant warfarin is teratogenic, whereas he parin does not appear to e. Antihypertensive agents that inhi it angiotensin-co nverting enzyme (ACE) inhi itors produce growth retardation, renal dysfunction, fetal death, and oligohydramnios. Caution has also een expressed regarding a nu m er of other compounds that may damage the em ryo or fetus. The most prominent among these are propylthiouracil and potassium iodide (goiter and mental retarda tion), streptomycin (deafness), sulfonamides (kernicterus), the antidepressant i mipramine (lim deformities), tetracyclines ( one and tooth anomalies), amphetam ines (oral clefts and cardiovascular a normalities), and quinine (deafness). Fin ally, there is increasing evidence that aspirin (salicylates), the most commonly ingested drug during pregnancy, may harm the developing offspring when used in large doses. One of the increasing pro lems in todays society is the effect of so cial drugs, such as LSD (lysergic acid diethylamide), PCP (phencyclidine, or ange l dust), marijuana, alcohol, and cocaine. In the case of LSD, lim a normalities and malformations of the central nervous system have een reported. A comprehens ive review of more than 100 pu lications, however, led to the conclusion that pu re LSD used in moderate doses is not teratogenic and does not cause genetic dama ge. A similar lack of conclusive evidence for teratogenicity has een descri ed for marijuana and PCP. Cocaine has een reported to cause a num er of irth defe cts, possi ly due to its action as a vasoconstrictor that causes hypoxia. There is a well-documented association etween maternal alcohol ingestion and congenit al a normalities, and these defects, together with mental retardation and growth de ciency, make up the fetal alcohol syndrome (FAS) (Fig. 7.2). Even moderate alc ohol consumption during pregnancy may e detrimental to em ryonic development. T he central nervous system is particularly sensitive to alcohol, and alcohol-rela ted neurodevelopmental disorder (ARND) may result from exposure. The incidence o f FAS and ARND together is 1 in 100 live irths. Furthermore, alcohol is the lea ding cause of mental retardation.
156 Part One: General Em ryology Figure 7.2 A. Characteristic features of a child with fetal alcohol syndrome. B. Child with fetal alcohol syndrome illustrating many of the features in the draw ing. These children may also have cardiovascular and lim defects. Cigarette smoking has not een linked to major irth defects, ut it does contri ute to intrauterine growth retardation and premature delivery. There is also ev idence that it causes ehavioral distur ances. Isotretinoin (13-cis-retinoic aci d), an analogue of vitamin A, has een shown to cause a characteristic pattern o f malformations known as the isotretinoin em ryopathy or vitamin A em ryopathy. The drug is prescri ed for the treatment of cystic acne and other chronic dermat oses, ut it is highly teratogenic and can produce virtually any type of malform ation. Even topical
Chapter 7: Birth Defects and Prenatal Diagnosis 157 retinoids, such as etretinate, may have the potential to cause a normalities. Wi th the recent support for the use of multivitamins containing folic acid, there is concern that overuse of vitamin supplements could e harmful, since most cont ain approximately 8,000 IU of vitamin A. How much is potentially harmful is cont roversial, ut most scientists agree that 25,000 IU is a threshold level for ter atogenicity. Hormones Androgenic Agents. In the past synthetic progestins were frequently use d during pregnancy to prevent a ortion. The progestins ethisterone and norethist erone have considera le androgenic activity, and many cases of masculinization o f the genitalia in female em ryos have een reported. The a normalities consist of an enlarged clitoris associated with varying degrees of fusion of the la iosc rotal folds. Endocrine Disrupters. Endocrine disrupters are exogenous agents tha t interfere with the normal regulatory actions of hormones controlling developme ntal processes. Most commonly these agents interfere with the action of estrogen through its receptor to cause developmental a normalities of the central nervou s system and reproductive tract. For some time it has een known that the synthe tic estrogen diethylstil estrol, which was used to prevent a ortion, raised the incidence of carcinomas of the vagina and cervix in women exposed to the drug in utero. Furthermore, a high percentage of these women had reproductive dysfuncti on due in part to congenital malformations of the uterus, uterine tu es, and upp er vagina. Male em ryos exposed in utero can also e affected, as evidenced y a n increase in malformations of the testes and a normal sperm analysis among thes e individuals. In contrast to females, however, males do not demonstrate an incr eased risk of developing carcinomas of the genital system. Today environmental e strogens are a concern and numerous studies to determine their effects on the un orn are under way. Decreasing sperm counts and increasing incidences of testicu lar cancer, hypospadias, and other a normalities of the reproductive tract in hu mans, together with documented central nervous system a normalities (masculiniza tion of female rains and feminization of male rains) in other species with hig h environmental exposures, have raised awareness of the possi le harmful effects of these agents. Many are formed from chemicals used for industrial purposes an d from pesticides. Oral Contraceptives. Birth control pills, containing estrogen s and progestogens, appear to have a low teratogenic potential. Since other horm ones, such as diethylstil estrol, produce a normalities, however, use of oral co ntraceptives should e discontinued if pregnancy is suspected.
158 Part One: General Em ryology Cortisone. Experimental work has repeatedly shown that cortisone injected into m ice and ra its at certain stages of pregnancy causes a high percentage of cleft palates in the offspring. However, it has een impossi le to implicate cortison e as an environmental factor causing cleft palate in humans. Maternal Disease Dia etes. Distur ances in car ohydrate meta olism during pregna ncy in dia etic mothers cause a high incidence of still irths, neonatal deaths, a normally large infants, and congenital malformations. The risk of congenital a nomalies in children of dia etic mothers is 3 to 4 times that for the offspring of nondia etic mothers and has een reported to e as high as 80% in the offspri ng of dia etics with long-standing disease. The variety of o served malformation s includes caudal dysgenesis (sirenomelia). Factors responsi le for these a norm alities have not een delineated, although evidence suggests that altered glucos e levels play a role and that insulin is not teratogenic. In this respect, a sig ni cant correlation exists etween the severity and duration of the mothers disease and the incidence of malformations. Also, strict control of maternal meta olism with aggressive insulin therapy prior to conception reduces the occurrence of m alformations. Such therapy, however, increases the frequency and severity of hyp oglycemic episodes. Numerous animal studies have shown that during gastrulation and neurulation, mammalian em ryos depend on glucose as an energy source, so tha t even rief episodes of low lood glucose are teratogenic. Therefore, caution m ust e exercised in managing the pregnant dia etic woman. In the case of non-ins ulin-dependent dia etes, oral hypoglycemic agents may e employed. These agents include the sulfonylureas and iguanides. Both classes of agents have een impli cated as teratogens. Phenylketonuria. Mothers with phenylketonuria (PKU), in whi ch the enzyme phenylalanine hydroxylase is de cient, resulting in increased serum concentrations of phenylalanine, are at risk for having infants with mental reta rdation, microcephaly, and cardiac defects. Women with PKU who maintain their lo w phenylalanine diet prior to conception reduce the risk to their infants to tha t o served in the general population. Nutritional De ciencies Although many nutritional de ciencies, particularly vitamin de ciencies, have een proven to e teratogenic in la oratory animals, the evidenc e in humans is sparse. Thus, with the exception of endemic cretinism, which is r elated to iodine de ciency, no analogies to animal experiments have een discovere d. However, the evidence suggests that poor maternal nutrition prior to and duri ng pregnancy contri utes to low irth weight and irth defects.
Chapter 7: Birth Defects and Prenatal Diagnosis 159 O esity Prepregnancy o esity, de ned as having a ody mass index (BMI) >29kg/m2 , is associated with a two- to three-fold increased risk for having a child with a neural tu e defect. Causation has not een determind ut may relate to maternal meta olic distur ances affecting glucose, insulin, or other factors. Hypoxia Hy poxia induces congenital malformations in a great variety of experimental animal s. Whether the same is valid for humans remains to e seen. Although children o rn at relatively high altitudes are usually lighter in weight and smaller than t hose orn near or at sea level, no increase in the incidence of congenital malfo rmations has een noted. In addition, women with cyanotic cardiovascular disease often give irth to small infants, ut usually without gross congenital malform ations. Heavy Metals Several years ago, researchers in Japan noted that a num er of mothers with diets consisting mainly of sh had given irth to children with m ultiple neurological symptoms resem ling cere ral palsy. Further examination rev ealed that the sh contained an a normally high level of organic mercury, which wa s spewed into Minamata Bay and other coastal waters of Japan y large industries . Many of the mothers did not show any symptoms themselves, indicating that the fetus was more sensitive to mercury than the mother. In the United States, simil ar o servations were made when seed corn sprayed with a mercury-containing fungi cide was fed to hogs and the meat was su sequently eaten y a pregnant woman. Si milarly in Iraq, several thousand a ies were affected after mothers ate grain t reated with mercury-containing fungicides. Lead has een associated with increas ed a ortions, growth retardation, and neurological disorders. MALE-MEDIATED TERA TOGENESIS A num er of studies have indicated that exposures to chemicals and oth er agents, such as ethylnitrosourea and radiation, can cause mutations in male g erm cells. Epidemiological investigations have linked paternal occupational and environmental exposures to mercury, lead, solvents, alcohol, cigarette smoking, and other compounds to spontaneous a ortion, low irth weight, and irth defects . Advanced paternal age is a factor for an increased risk of lim and neural tu e defects, Down syndrome, and new autosomal dominant mutations. Interestingly, m en younger than 20 also have a relatively high risk of fathering a child with a irth defect. Even transmission of paternally mediated toxicity is possi le thro ugh seminal uid and from household contamination
160 Part One: General Em ryology from chemicals rought home on workclothes y the father. Studies also show that males with irth defects themselves have a greater than twofold risk of having an affected child. CLINICAL CORRELATES Prevention of Birth Defects Many irth defects can e prevented. For example, su pplementation of salt or water supplies with iodine eliminates mental retardatio n and one deformities resulting from cretinism. Placing women with dia etes or PKU under strict meta olic control prior to conception reduces the incidence of irth defects in their offspring. Folate supplementation lowers the incidence of neural tu e defects, such as spina i da and anencephaly. Avoidance of alcohol an d other drugs during all stages of pregnancy reduces the incidence of irth defe cts. A common denominator for all prevention strategies is to initiate intervent ions prior to conception. Such an approach also helps prevent low- irth-weight a ies. It is important for physicians prescri ing drugs to women of child earing age to consider the possi ility of pregnancy and the potential teratogenicity o f the compounds. Recently hundreds of children have een orn with severe cranio facial, cardiac, and neural tu e defects produced y retinoids (vitamin A em ryo pathy). These compounds are used for the treatment of cystic acne (isotretinoin, 13-cis-retinoic acid) ut are also effective topically (Retin-A) for common acn e and reducing wrinkles. Oral preparations are highly teratogenic, and recent ev idence suggests that topical applications may also cause a normalities. Since pa tients with acne are usually young and may e sexually active, these agents must e used cautiously. Prenatal Diagnosis The perinatologist has several approache s for assessing growth and development of the fetus in utero, including ultrasou nd, amniocentesis, chorionic villus sampling, and maternal serum screening. In c om ination, these techniques are designed to detect malformations, genetic a nor malities, overall fetal growth, and complications of pregnancy, such as placenta l or uterine a normalities. Their use and development of in utero therapies have heralded a new concept in which the fetus is now a patient. ULTRASONOGRAPHY Ult rasonography is a relatively noninvasive technique that uses high-frequency soun d waves re ected from tissues to create images. The approach may e transa dominal or transvaginal, with the latter producing images with higher resolution (Fig. 7.3). In fact, the technique, which was rst developed in the 1950s, has advanced to a degree where detection of lood ow in major vessels,
Chapter 7: Birth Defects and Prenatal Diagnosis 161 A B C D Figure 7.3 Examples of the effectiveness of ultrasound in imaging the em ryo and fetus. A. 6-week em ryo. B. Lateral view of the fetal face. C. Hand. D. Feet. movement of heart valves, and ow of uid in the trachea and ronchi is possi le. Th e technique is safe and commonly used, with approximately 80% of pregnant women in the United States receiving at least one scan. Important parameters revealed y ultrasound include: characteristics of fetal age and growth; presence or a se nce of congenital anomalies; status of the uterine environment, including the am ount of amniotic uid (Fig. 7.4A); placental position and um ilical lood ow; and w hether multiple gestations are present (Fig.7.4B). All of these factors are then used to determine proper approaches for management of the pregnancy. Determinat ion of the fetal age and growth is crucial in planning pregnancy management, esp ecially for low- irth-weight infants. In fact, studies show that ultrasound scre ened and managed pregnancies with low- irth-weight a ies reduced the mortality rate y 60% compared with an unscreened group. Fetal age and growth are assessed y crown-rump length during the fth to tenth weeks of gestation. After that, a c om ination of measurements, including the iparietal diameter (BPD) of the skull , femur length, and a dominal circumference are used (Fig. 7.5). Multiple measur es of these parameters over time improve the a ility to determine the extent of fetal growth. Congenital malformations that can e determined y ultrasound incl ude: the neural tu e defects anencephaly and spina i da (see Chapter 19);
162 Part One: General Em ryology S S A B Figure 7.4 A. Ultrasound image showing position of the fetal skull and placement of the needle into the amniotic cavity (arrow) during amniocentesis. B. Twins. Ultrasound showing the presence of two gestational sacs (S). B C R R A B P F L C D Figure 7.5 Ultrasounds showing measures used to assess em ryonic and fetal growt h. A. Crown-rump (C-R) length in a 7-week em ryo. B. Biparietal (B-P) diameter o f the skull. C. A dominal circumference. D. Femur length (F-L).
Chapter 7: Birth Defects and Prenatal Diagnosis 163 a dominal wall defects, such as omphalocele and gastroschisis (see Chapter 13); and heart, (see Chapter 11) and facial defects, including cleft lip and palate ( see Chapter 15). MATERNAL SERUM SCREENING A search for iochemical markers of fetal status led to development of maternal serum screening tests. One of the rst of these tests ass essed serum alphafetoprotein (AFP) concentrations. AFP is produced normally y t he fetal liver, peeks at approximately 14 weeks, and leaks into the maternal circu lation via the placenta. Thus, AFP concentrations increase in maternal serum dur ing the second trimester and then egin a steady decline after 30 weeks of gesta tion. In cases of neural tu e defects and several other a normalities, including omphalocele, gastroschisis, ladder exstrophy, amniotic and syndrome, sacrococ cygeal teratoma, and intestinal atresia, AFP levels increase in amniotic uid and maternal serum. In other instances, AFP concentrations decrease as, for example, in Down syndrome, trisomy 18, sex chromosome a normalities, and triploidy. Thes e conditions are also associated with lower serum concentrations of human chorio nic gonadotropin (hCG) and unconjugated estriol. Therefore, maternal serum scree ning provides a relatively noninvasive technique for an initial assessment of fe tal well eing. AMNIOCENTESIS During amniocentesis, a needle is inserted transa dominally into t he amniotic cavity (identi ed y ultrasound; Fig. 7.4A) and approximately 20 to 30 ml of uid are withdrawn. Because of the amount of uid required, the procedure is not usually performed efore 14 weeks gestation, when suf cient quantities are ava ila le without endangering the fetus. The risk of fetal loss as a result of the procedure is 1%, ut it is less in centers skilled in the technique. The uid itse lf is analyzed for iochemical factors, such as AFP and acetylcholinesterase. In addition, fetal cells, sloughed into the amniotic uid, can e recovered and used for metaphase karyotyping and other genetic analyses (see Chapter 1). Unfortuna tely, the harvested cells are not rapidly dividing, and therefore, cell cultures containing mitogens must e esta lished to provide suf cient metaphase cells for analysis. This culture period requires 8 to 14 days, and consequently, making a diagnosis is delayed. Once chromosomes are o tained, major chromosomal alteratio ns, such as translocations, reaks, trisomies, and monosomies, can e identi ed. W ith special stains (Giemsa) and high-resolution techniques, chromosome anding p atterns can e determined. Furthermore, now that the human genome has een seque nced, more sophisticated molecular analyses using polymerase chain reaction (PCR ) and genotyping assays will increase the level of detection for genetic a norma lities.
164 Part One: General Em ryology CHORIONIC VILLUS SAMPLING (CVS) Chorionic villus sampling (CVS) involves inserti ng a needle transa dominally or transvaginally into the placental mass and aspir ating approximately 5 to 30 mg of villus tissue. Cells may e analyzed immediate ly, ut accuracy of results is pro lematic ecause of the high frequency of chro mosomal errors in the normal placenta. Therefore, cells from the mesenchymal cor e are isolated y trypsinization of the external tropho last and cultured. Becau se of the large num er of cells o tained, only 2 to 3 days in culture are necess ary to permit genetic analysis. Thus, the time for genetic characterization of t he fetus is reduced compared with amniocentesis. However, the risk of fetal loss from CVS is approximately twofold greater than with amniocentesis, and there ha ve een indications that the procedure carries an increased risk for lim reduct ion defects. Generally, these prenatal diagnostic tests are not used on a routin e asis (although ultrasonography is approaching routine use), eing reserved in stead for high-risk pregnancies. Indications for using the tests include: 1) adv anced maternal age (35 years and older); 2) history of neural tu e defects in th e family; 3) previous gestation with a chromosome a normality, such as Down synd rome; 4) chromosome a normalities in either parent; and 5) a mother who is a car rier for an X-linked disorder. Fetal Therapy FETAL TRANSFUSION In cases of fetal anemia produced y maternal anti odies or other causes, lood transfusions for the fetus can e performed. Ultrasound is used to guide insertion of a needle in to the um ilical cord vein, and lood is transfused directly into the fetus. FET AL MEDICAL TREATMENT Treatment for infections, fetal cardiac arrhythmias, compro mised thyroid function, and other medical pro lems is usually provided to the mo ther and reaches the fetal compartment after crossing the placenta. In some case s, however, agents may e administered to the fetus directly y intramuscular in jection into the gluteal region or via the um ilical vein. FETAL SURGERY Because of advances in ultrasound and surgical procedures, operating on fetuses has ec ome possi le. However, ecause of risks to the mother, infant, and su sequent pr egnancies, procedures are only performed in centers with welltrained teams and o nly when there are no reasona le alternatives. Several types of surgeries may e performed, including placing shunts to remove uid from
Chapter 7: Birth Defects and Prenatal Diagnosis 165 organs and cavities. For example, in o structive urinary disease of the urethra, a pigtail shunt may e inserted into the fetal ladder. One pro lem is diagnosi ng the condition early enough to prevent renal damage. Ex utero surgery, where t he uterus is opened and the fetus operated upon directly, has een used for repa iring congenital diaphragmatic hernias, removing cystic (adenomatoid) lesions in the lung, and repairing spina i da defects. Repairs of hernias and lung lesions have good outcomes if proper selection criteria for cases are employed, and one of these is the fact that without surgery, fetal demise is almost certain. Surge ry for neural tu e defects is more controversial ecause the a normalities are n ot life threatening. Also, the evidence is not conclusive that repair of the les ion improves neurological function, although it does alleviate the accompanying hydrocephalus y freeing the tethered spinal cord and preventing herniation of t he cere ellum into the foramen magnum (see Chapter 19; p. 445). STEM CELL TRANSP LANTATION AND GENE THERAPY Because the fetus does not develop any immunocompeten ce efore 18 weeks gestation, it may e possi le to transplant tissues or cells efore this time without rejection. Research in this eld is focusing on hematopoi etic stem cells for treatment of immunode ciency and hematologic disorders. Gene t herapy for inherited meta olic diseases, such as Tay Sachs and cystic rosis, is also eing investigated. Summary A variety of agents (Ta le 7.1; p. 152) are known to produce congenital malformations in approximately 2 to 3% of all live- orn infants. These agents in clude viruses, such as ru ella and cytomegalovirus; radiation; drugs, such as th alidomide, aminopterin, anticonvulsants, antipsychotics, and antianxiety compoun ds; social drugs, such as PCP, cigarettes, and alcohol; hormones, such as diethy lstil estrol; and maternal dia etes. Effects of teratogens depend on the materna l and fetal genotype, the stage of development when exposure occurs, and the dos e and duration of exposure of the agent. Most major malformations are produced d uring the period of em ryogenesis (teratogenic period; third to eighth weeks), ut in stages efore and after this time, the fetus is also suscepti le, so that no period of gestation is completely free of risk. Prevention of many irth defe cts is possi le, ut it depends on eginning preventative measures efore concep tion and increasing physicians and womens awareness of the risks. A variety of tec hniques are availa le to assess the growth and developmental status of the fetus . Ultrasound can accurately determine fetal age and growth parameters and detect many malformations. Maternal serum screening for alpha-fetoprotein can indicate the presence of a neural tu e defect or
166 Part One: General Em ryology other a normalities. Amniocentesis is a procedure in which a needle is placed in to the amniotic cavity and a uid sample is withdrawn. This uid can e analyzed io chemically and also provides cells for culture and genetic analysis. Chorionic v illus sampling (CVS) involves aspirating a tissue sample directly from the place nta to o tain cells for genetic analysis. Because many of these procedures invol ve a potential risk to the fetus and mother, they are generally only used for hi gher risk pregnancies (the exception is ultrasound). These risk factors include advanced maternal age (35 years and older); a history of neural tu e defects in the family; previous gestation with a chromosome a normality; chromosome a norma lities in either parent; and a mother who is a carrier for an X-linked disorder. Modern medicine has also made the fetus a patient who can receive treatment, su ch as transfusions, medications for disease, fetal surgery, and gene therapy. Pro lems to Solve 1. Amniocentesis reveals an elevated AFP level. What should e included in a differential diagnosis, and how would a de nitive one e made? 2. A 40-year-old woman is approximately 8 weeks pregnant. What tests are availa le t o determine whether her un orn child has Down syndrome? What are the risks and a dvantages of each technique? 3. Why is it important to determine the status of a n infant prenatally? What maternal or family factors might raise your concern a out the well- eing of an un orn infant? 4. What factors in uence the action of a t eratogen? 5. A young woman in only the third week of her pregnancy develops a fe ver of 104 ut refuses to take any medication ecause she is afraid that drugs wi ll harm her a y. Is she correct? 6. A young woman who is planning a family seek s advice a out folic acid and other vitamins. Should she take such a supplement, and if so, when and how much? 7. A young insulin-dependent dia etic woman who i s planning a family is concerned a out the possi le harmful effects of her disea se on her un orn child. Are her concerns valid, and what would you recommend? SUGGESTED READING Barlow S, Kavlock RJ, Moore JA, Shantz S, Sheehan DL, Shuey DL , Lary JM: Teratology Society Pu lic Affairs Committee Position Paper: developme ntal toxicity of endocrine disruptors to humans. Teratology 60:365, 1999. Barnea ER, Hustin J, Jauniaux E (eds): The First Twelve Weeks of Gestation. Berlin, Sp ringer-Verlag, 1992.
Chapter 7: Birth Defects and Prenatal Diagnosis 167 Bendich A, et al.: In uence of maternal nutrition on pregnancy outcome: pu lic pol icy issues. Introduction to Part V. Ann N Y Acad Sci 678:284, 1993. Boehm CE, Ka zazian HH Jr: Prenatal diagnosis y DNA analysis. In Harrison MR, Gol us MS, Fil ly RA (eds): The Un orn Patient: Prenatal Diagnosis and Treatment. 2nd ed. Phila delphia, WB Saunders, 1991. Brent RL, Beckman DA: Angiotensin-converting enzyme inhi itors, an em ryopathic class of drugs with unique properties: information f or clinical teratology counselors. Teratology 43:543, 1991. Brent RL, Holmes LB: Clinical and asic science from the thalidomide tragedy: what have we learned a out the causes of lim defects? Teratology 38:241, 1988. Buehler BA, Rao V, Fin nell RH: Biochemical and molecular teratology of fetal hydantoin syndrome. Ped N euro Genet 12:741, 1994. Centers for Disease Control. Contri ution of irth defe cts to infant mortalityUnited States, 1986. MMWR Mor Mortal Wkly Rep 38(37):633, 1989. Col orn T, Dumanoski D, Myers JP: Our Stolen Future. New York, Dutton, 19 96. Cooper RL, Kavlock RJ: Endocrine disrupters and reproductive development: a weight of evidence overview [review]. J Endocrinol 152(2):159, 1997. Cunningham FG, Gant NE, Leveno KJ, Gilstrap LC, Hauth JC, Wenstrom KD: Fetal a normalities and acquired disorders. In Williams O stetrics. 21st ed. New York, McGraw Hill, 2001. Dansky LV, Finnell RH: Parental epilepsy, anticonvulsant drugs, and reprod uctive outcome: epidemiologic and experimental ndings spanning three decades; 2: human studies. Reprod Toxicol 5:301, 1991. Generoso WM, et al.: Mutagen induced fetal anomalies and death following treatment of females within hours after mati ng. Mutat Res 199:175, 1988. Gorlin RJ, Cohen MM, Levin LS (eds): Syndromes of t he Head and Neck. 3rd ed. New York, Oxford University Press, 1990. Graham JM, Ed wards MJ: Teratogen update: gestational effects of maternal hyperthermia due to fe rile illnesses and resultant pattern of defects in humans. Teratology 58:209, 1998. Gray LE, Ost y J: Effects of pesticides and toxic su stances on ehaviora l and morphological reproductive development: endocrine versus nonendocrine mech anisms. Toxicol Ind Health 14:159, 1998. Gregg NM: Congenital cataract following German measles in mothers. Trans Ophthalmol Soc Aust 3:35, 1941. Hales BF, Ro a ire B: Paternally mediated effects on development. In Hood RD (ed): Hand ook of Developmental Toxicology. New York, CRC Press, 1997. Jones KL (ed): Smiths Recogn iza le Patterns of Human Malformation. 4th ed. Philadelphia, WB Saunders, 1988. Jones KL, Smith DW, Ulleland CN, et al: Pattern of malformation in offspring of chronic alcoholic mothers. Lancet 1:1267, 1973. Kaufman RH, Binder GS, Gray PM, Adam E: Upper genital tract changes associated with exposure in utero to diethyl stil estrol. Am J O stet Gynecol 128:51, 1977. Khatta KS, Moghtader GK, McMartin K, Berrera M, Kennedy D, Koren G: Pregnancy outcome following gestational expos ure to organic solvents. JAMA 281:1106, 1999. Lammer EJ, et al: Retinoic acid em ryopathy. N Engl J Med 313:837, 1985. Lenke RR, Levy HL: Maternal phenylketonur ia and hyperphenylalaninemia: an international survey of untreated and treated p regnancies. N Engl J Med 303:1202, 1980. Lenz W: A short history of thalidomide em ryopathy. Teratology 38:203, 1988. Lie RT, Wilcox AJ, Skjaerven R: Survival a nd reproduction among males with irth defects and risk of recurrence in their c hildren. JAMA 285:755, 2001. Manning FA: General principles and applications of ultrasonography. In Creasy RK, Resnik R (eds.): Maternal Fetal Medicine. 4th ed. philadelphia, WB Saunders, 1999. McIntosh GC, Olshan AF, Baird PA: Paternal age and the risk of irth defects in offspring. Epidemiology 6:282, 1995. Nash JE, Persaud TVN: Em ryopathic risks of cigarette smoking. Exp Pathol 33:65, 1988.
168 Part One: General Em ryology Sadler TW, Denno KM, Hunter ES III: Effects of altered maternal meta olism durin g gastrulation and neurulation stages of development. Ann N Y Acad Sci 678:48, 1 993. Sampson PD, et al.: Incidence of fetal alcohol syndrome and prevalence of a lcohol-related neurodevelopmental disorder. Teratology 56:317, 1997. Schmidt RR, Johnson EM: Principles of teratology. In Hood RD (ed): Hand ook of Developmenta l Toxicology. New York, CRC Press, 1997. Scioscia AL: Prenatal genetic diagnosis . In Creasy RK, Resnik R (eds.): Maternal Fetal Medicine. 4th ed. Philadelphia, WB Saunders, 1999. Shaw GM, Todoroff K, Finnell RH, Lammer EJ: Spina i da phenoty pes in infants of fetuses of o ese mothers. Teratology 61:376,2000. Shenefelt RE : Morphogenesis of malformations in hamsters caused y retinoic acid: relation t o dose and stage of development. Teratology 5:103, 1972. Shepard TH: Catalog of Teratogenic Agents. 7th ed. Baltimore, Johns Hopkins University Press, 1992. Spi rt BA, Fordon LP, Oliphant M: Prenatal Ultrasound: A Color Atlas With Anatomic a nd Pathologic Correlation. New York, Churchill Livingstone, 1987. Stevenson RE, Hall JG, Goodman RM (eds): Human Malformations and Related Anomalies, vols 1 and 2. New York, Oxford University Press, 1993. Wald N: Folic acid and prevention o f neural tu e defects. Ann N Y Acad Sci 678:112, 1993. Weaver DD: In orn errors of meta olism. In Weaver DD (ed): Catalogue of Prenatally Diagnosed Conditions. Baltimore, Johns Hopkins University Press, 1989. Werler MM, Pro er BR, Holmes LB : Smoking and pregnancy. In Sever JL, Brent RL (eds): Teratogen Update: Environm entally Induced Birth Defect Risks. New York, Alan R Liss, 1986. Wilcox AJ, Wein erg CR, Baird DD: Timing of sexual intercourse in relation to ovulation. N Engl J Med 333:1517, 1995. Wilson JG, Fraser FC: Hand ook of Teratology, vols 13. New York, Plenum, 1977. Woods KA, Camach-Hu ner C, Savage MO, Clark AJL: Intrauteri ne growth retardation and postnatal growth failure associated with deletion of t he insulin-like growth factor I gene. N Engl J Med 335:1363, 1996.
part two Special Em ryology 169
chapter 8 Skeletal System The skeletal system develops from paraxial and lateral plate (somatic layer) mes oderm and from neural crest. Paraxial mesoderm forms a segmented series of tissu e locks on each side of the neural tu e, known as somitomeres in the head regio n and somites from the occipital region caudally. Somites differentiate into a v entromedial part, the sclerotome, and a dorsolateral part, the dermomyotome. At the end of the fourth week sclerotome cells ecome polymorphous and form a loose ly woven tissue, the mesenchyme, or em ryonic connective tissue (Fig. 8.1). It i s characteristic for mesenchymal cells to migrate and to differentiate in many w ays. They may ecome ro lasts, chondro lasts, or osteo lasts ( one-forming cells ). The one-forming capacity of mesenchyme is not restricted to cells of the scl erotome, ut occurs also in the somatic mesoderm layer of the ody wall, which c ontri utes mesoderm cells for formation of the pelvic and shoulder girdles and t he long ones of the lim s. Neural crest cells in the head region also different iate into mesenchyme and participate in formation of ones of the face and skull . Occipital somites and somitomeres also contri ute to formation of the cranial vault and ase of the skull. In some ones, such as the at ones of the skull, me senchyme in the dermis differentiates directly into one, a process known as int ramem ranous ossi cation (Fig. 8.2). In most ones, however, mesenchymal cells rst give rise to hyaline cartilage models, which in turn ecome ossi ed y endochondra l ossi cation (see Figs. 8.5 and 171
172 Part Two: Special Em ryology Figure 8.1 Development of the somite. A. Paraxial mesoderm cells are arranged ar ound a small cavity. B. As a result of further differentiation, cells in the ven tromedial wall lose their epithelial arrangement and ecome mesenchymal. Collect ively they are called the sclerotome. Cells in the dorsolateral wall of the somi te form lim and ody wall musculature, while cells at the dorsomedial portion m igrate eneath the remaining dorsal epithelium (the dermatome) to form the myoto me. Figure 8.2 Bones of the skull of a 3-month-old fetus showing the spread of spicules from primary ossi cation centers in the at ones of the skull.
one
Chapter 8: Skeletal System 173 8.13). The following paragraphs discuss development of the most important ony s tructures and some of their a normalities. Skull The skull can e divided into t wo parts: the neurocranium, which forms a protective case around the rain, and the viscerocranium, which forms the skeleton of the face. NEUROCRANIUM The neuro cranium is most conveniently divided into two portions: (a) the mem ranous part, consisting of at ones, which surround the rain as a vault; and ( ) the cartila ginous part, or chondrocranium, which forms ones of the ase of the skull. Mem ranous Neurocranium The mem ranous portion of the skull is derived from neural c rest cells and paraxial mesoderm as indicated in Figure 8.3. Mesenchyme from the se two sources invests the rain and undergoes mem ranous ossi cation. The result is formation of a num er of at, mem ranous ones that are characterized y the pr esence of needle-like one spicules. These spicules progressively radiate Figure 8.3 Skeletal structures of the head and face. Mesenchyme for these struct ures is derived from neural crest ( lue), lateral plate mesoderm (yellow), and p araxial mesoderm (somites and somitomeres) (red).
174 Part Two: Special Em ryology Figure 8.4 Skull of a new orn, seen from a ove (A) and the right side (B). Note the anterior and posterior fontanelles and sutures. The posterior fontanelle clo ses a out 3 months after irth; the anterior fontanelle, a out the middle of the second year. Many of the sutures disappear during adult life. from primary ossi cation centers toward the periphery (Fig. 8.2). With further gro wth during fetal and postnatal life, mem ranous ones enlarge y apposition of n ew layers on the outer surface and y simultaneous osteoclastic resorption from the inside. New orn Skull At irth the at ones of the skull are separated from e ach other y narrow seams of connective tissue, the sutures, which are also deri ved from two sources: neural crest cells (sagittal suture) and paraxial mesoderm (coronal suture). At points where more than two ones meet, sutures are wide an d are called fontanelles (Fig. 8.4). The most prominent of these is the anterior fontanelle, which is found where the two parietal and two frontal ones meet. S utures and fontanelles allow the ones of the skull to overlap (molding) during irth. Soon after irth mem ranous ones move ack to their original positions, and the skull appears large and round. In fact, the size of the vault is large c ompared with the small facial region (Fig. 8.4B ). Several sutures and fontanell es remain mem ranous for a considera le time after irth. The ones of the vault continue to grow after irth, mainly ecause the rain grows. Although a 5- to 7-year-old child has nearly all of its cranial capacity, some sutures remain ope n until adulthood. In the rst few years after irth palpation of the anterior fon tanelle may give valua le information
Chapter 8: Skeletal System 175 Figure 8.5 Dorsal view of the chondrocranium, or ase of the skull, in the adult . On the right side are the various em ryonic components participating in format ion of the median part of the chondrocranium ( lue) and components of the latera l part (red ). On the left are the names of the adult structures. Bones that for m rostral to the rostral half of the sella turcica arise from neural crest and c onstitute the prechordal (in front of the notochord) chondrocranium. Those formi ng posterior to this landmark arise from paraxial mesoderm (chordal chondrocrani um). as to whether ossi cation of the skull is proceeding normally and whether intracra nial pressure is normal. Cartilaginous Neurocranium or Chondrocranium The cartil aginous neurocranium or chondrocranium of the skull initially consists of a num er of separate cartilages (Fig. 8.5). Those that lie in front of the rostral lim it of the notochord, which ends at the level of the pituitary gland in the cente r of the sella turcica, are derived from neural crest cells. They form the prech ordal chondrocranium. Those that lie posterior to this limit arise from paraxial mesoderm and form the chordal chondrocranium. The ase of the skull is formed w hen these cartilages fuse and ossify y endochondral ossi cation.
176 Part Two: Special Em ryology The ase of the occipital one is formed y the parachordal cartilage and the o dies of three occipital sclerotomes (Fig. 8.5). Rostral to the occipital ase pl ate are the hypophyseal cartilages and tra eculae cranii. These cartilages soon fuse to form the ody of the sphenoid and ethmoid, respectively. In this manner an elongated median plate of cartilage extending from the nasal region to the an terior order of the foramen magnum forms. A num er of other mesenchymal condens ations arise on either side of the median plate. The most rostral, the ala or it alis, forms the lesser wing of the sphenoid one. Caudally it is followed y the ala temporalis, which gives rise to the greater wing of the sphenoid. A third c omponent, the periotic capsule, gives rise to the petrous and mastoid parts of t he temporal one. These components later fuse with the median plate and with eac h other, except for openings through which cranial nerves leave the skull (Fig. 8.5). VISCEROCRANIUM The viscerocranium, which consists of the ones of the face , is formed mainly from the rst two pharyngeal arches (see Chapter 15). The rst ar ch gives rise to a dorsal portion, the maxillary process, which extends forward eneath the region of the eye and gives rise to the maxilla, the zygomatic one, and part of the temporal one (Fig. 8.6). The ventral portion, the mandi ular p rocess, Figure 8.6 Lateral view of the head and neck region of an older fetus, showing d erivatives of the arch cartilages participating in formation of ones of the fac e.
Chapter 8: Skeletal System 177 contains Meckels cartilage. Mesenchyme around Meckels cartilage condenses and ossi e s y mem ranous ossi cation to give rise to the mandi le. Meckels cartilage disappe ars except in the sphenomandi ular ligament. The dorsal tip of the mandi ular pr ocess, along with that of the second pharyngeal arch, later gives rise to the in cus, the malleus, and the stapes (Fig. 8.6). Ossi cation of the three ossicles eg ins in the fourth month, making these the rst ones to ecome fully ossi ed. Mesenc hyme for formation of the ones of the face is derived from neural crest cells, including the nasal and lacrimal ones (Fig. 8.3). At rst the face is small in co mparison with the neurocranium. This appearance is caused y (a) virtual a sence of the paranasal air sinuses and ( ) the small size of the ones, particularly the jaws. With the appearance of teeth and development of the air sinuses, the f ace loses its a yish characteristics. CLINICAL CORRELATES Craniofacial Defects and Skeletal Dysplasias Neural Crest Cells Neural crest cel ls originating in the neuroectoderm form the facial skeleton and most of the sku ll. These cells also constitute a vulnera le population as they leave the neuroe ctoderm; they are often a target for teratogens. Therefore, it is not surprising that craniofacial a normalities are common irth defects (see Chapter 15). Cran ioschisis In some cases the cranial vault fails to form (cranioschisis), and ra in tissue exposed to amniotic uid degenerates, resulting in anencephaly. Craniosc hisis is due to failure of the cranial neuropore to close. (Fig. 8.7A). Children with such severe skull and rain defects cannot survive. Children with relative ly small defects in the skull through which meninges and/or rain tissue herniat e (cranial meningocele and meningoencephalocele, respectively) (Fig. 8.7B) may e treated successfully. In such cases the extent of neurological de cits depends o n the amount of damage to rain tissue. Craniosynostosis and Dwar sm Another impor tant category of cranial a normalities is caused y premature closure of one or more sutures. These a normalities are collectively known as craniosynostosis, wh ich occurs in 1 in 2500 irths and is a feature of over 100 genetic syndromes. T he shape of the skull depends on which of the sutures closed prematurely. Early closure of the sagittal suture (57% of cases) results in frontal and occipital e xpansion, and the skull ecomes long and narrow (scaphocephaly) (Fig. 8.8A). Pre mature closure of the coronal suture results in a short, high skull, known as ac rocephaly, or tower skull (Fig. 8.8B). If the coronal and lam doid sutures close prematurely on one side only, asymmetric
178 Part Two: Special Em ryology A
craniosynostosis, known as plagiocephaly, results (Fig. 8.8C ). Regulation of su ture closure involves secretion of various isoforms of transforming growth facto r (TGF). One of the exciting reakthroughs in molecular iology and genetics is t he discovery of the role of the ro last growth factors (FGFs) and ro last growth factor receptors (FGFRs) in skeletal dysplasias. There are nine mem ers of the FGF family and four receptors. Together they regulate cellular events, including proliferation, differentiation, and migration. Signaling is mediated y the rec eptors, which are transmem rane tyrosine kinase receptors, each of which has thr ee extracellular immunoglo ulin domains, a transmem rane segment, and a cytoplas mic tyrosine kinase domain. FGFR-1 and FGFR2 are coexpressed in pre one and prec artilage regions, including craniofacial
Figure 8.7 A. Child with use, leaving the cranial degenerates. B. Patient ntly can e successfully
anencephaly. Cranial neural folds fail to elevate and f neuropore open. The skull never forms, and rain tissue with meningocele. This rather common a normality freque repaired.
Chapter 8: Skeletal System 179 Figure 8.8 A. Child with scaphocephaly caused y early closure of the sagittal s uture. Note the frontal and occipital ossing. B. Radiograph of a child with acr ocephaly caused y early closure of the coronal suture. C. Child with plagioceph aly resulting from early closure of coronal and lam doid sutures on one side of the skull (see sutures in Fig. 8.4). structures; FGFR-3 is expressed in the cartilage growth plates of long ones. In general, FGFR-2 increases proliferation; FGFR-1 promotes osteogenic differentia tion; while the role of FGFR-3 is unclear, ut expression is increased in the oc cipital region. Mutations in these receptors, which often involve only a single amino acid su stitution, have een linked to speci c types of craniosynostosis (FG FR-1 and FGFR-2) and several forms of dwar sm (FGFR-3) (Fig. 8.9; and Ta le 8.1, p . 181). In addition to these genes, mutations in the transcription factor MSX2, a regulator of parietal one growth, causes Boston type craniosynostosis, which can affect a num er of ones and sutures. The TWIST gene codes for a DNA inding protein and plays a role in regulating proliferation. Mutations in this gene re sult in proliferation and premature differentiation in the coronal suture causin g craniosynostosis. Achondroplasia (ACH), the most common form of dwar sm (1/26,00 0 live irths), primarily affects the long ones. Other skeletal defects include a large skull with a small midface, short ngers, and accentuated spinal curvatur e (Fig. 8.10). ACH is inherited as an autosomal dominant, and 80% of cases appea r sporadically. Thanatophoric dysplasia is the most common neonatal lethal form of dwar sm (1/20,000 live irths). There are two types; oth are autosomal dominan t. Type I is characterized y short, curved femurs with or without cloverleaf sk ull; type II individuals have straight, relatively long femurs and severe clover leaf skull caused y craniosynostosis (Fig. 8.11). Hypochondroplasia, another au tosomal dominant form of dwar sm, appears to e a milder type of ACH. In common to all of these forms of skeletal dysplasias are
180 Part Two: Special Em ryology Figure 8.9 Faces of children with achondroplasia and different types of craniosy nostosis. A. Achondroplasia. B. Apert syndrome. C. Pfeiffer syndrome. D. Crouzon syndrome. Underdevelopment of the midfacial area (A) is common to all individua ls affected with these syndromes. mutations in FGFR-3 causing a normal endochondral one formation so that growth of the long ones and ase of the skull is adversely affected. Acromegaly is cau sed y congenital hyperpituitarism and excessive production of growth hormone. I t is characterized y disproportional enlargement of the face, hands, and feet. Sometimes, it causes more symmetrical excessive growth and gigantism. Microcepha ly Microcephaly is usually an a normality in which the rain fails to grow and t he skull fails to expand. Many children with microcephaly are severely retarded. Lim s LIMB GROWTH AND DEVELOPMENT At the end of the fourth week of development, lim uds ecome visi le as outpocketings from the ventrolateral ody wall (Fig. 8.12A). Initially they
Chapter 8: Skeletal System TABLE 8.1 Gene FGFR1 181 Genes Associated With Skeletal Defects Chromosome 8p12 A normality Pfeiffer syndrome Phenotype Craniosynostosis, road great toes and thum s, cloverleaf skull, underdeveloped face Same Craniosynostos is, underdeveloped face, symmetric syndactyly of hands and feet Craniosynostosis , underdeveloped face, foot anomalies, hands usually spared Craniosynostosis, un derdeveloped face, no foot or hand defects Short-lim dwar sm, underdeveloped face Curved short femurs, with or without cloverleaf skull Relatively long femurs, s evere cloverleaf skull Milder form of achondroplasia with normal craniofacial fe atures Craniosynostosis Craniosynostosis, midfacial hypoplasia, cleft palate, ve rte ral anomalies, hand and foot a normalities Small, short digits, divided uter us, hypospadius Fused, multiple digits FGFR2 10q26 Pfeiffer syndrome Apert syndrome Jackson-Weiss syndrome Crouzon syndrome FGFR3 4p16 Achondroplasia Thanatophoric dysplasia (type I) Thanatophoric dysplasia (type II ) Hypochondroplasia MSX2 TWIST 5q35 7p21 Boston-type craniosynostosis Saethre-Chotzen syndrome HOXA13 HOXD13 2q31 Hand-foot-genital syndrome Synpolydactyly consist of a mesenchymal core derived from the somatic layer of lateral plate me soderm that will form the ones and connective tissues of the lim , covered y a layer of cu oidal ectoderm. Ectoderm at the distal order of the lim thickens and forms the apical ectodermal ridge (AER) (Fig. 8.13A). This ridge exerts an i nductive in uence on adjacent mesenchyme, causing it to remain as a population of undifferentiated, rapidly proliferating cells, the progress zone. As the lim gr ows, cells farther from the in uence of the AER egin to differentiate into cartil age and muscle. In this manner development of the lim proceeds proximodistally. In 6-week-old em ryos the terminal portion of the lim uds ecomes attened to f orm the handplates and footplates and is separated from the
182 Part Two: Special Em ryology Figure 8.10 A. Three-month-old infant with achondroplasia. Note the large head, short extremities, and protruding a domen. B and C. Achondroplasia in a 15-yearold girl. Note dwar sm of the short lim type, the lim s eing disproportionately shorter than the trunk. The lim s are owed; there is an increase in lum ar lord osis; and the face is small relative to the head. Figure 8.11 Radiograph of a patient with cloverleaf skull characteristic of than atophoric dwar sm type II. The shape of the skull is due to a normal growth of the cranial ase, caused y a mutation in FGFR-3, followed y craniosynostosis. The sagittal, coronal, and lam doid sutures are commonly involved.
Chapter 8: Skeletal System 183 Figure 8.12 Development of the lim 6 weeks. C. At 8 weeks. The hindlim the forelim s. uds in human em ryos. A. At 5 weeks. B. At uds are less well developed than those of
proximal segment y a circular constriction (Fig. 8.12B). Later a second constri ction divides the proximal portion into two segments, and the main parts of the extremities can e recognized (Fig. 8.12C ). Fingers and toes are formed when ce ll death in the AER separates this ridge into ve parts (Fig. 8.14A). Further form ation of the digits depends on their continued outgrowth under the in uence of the ve segments of ridge ectoderm, condensation of the mesenchyme to form cartilagin ous digital rays, and the death of intervening tissue etween the rays (Fig. 8.1 4, B and C ). Development of the upper and lower lim s is similar except that mo rphogenesis of the lower lim is approximately 1 to 2 days ehind that of the up per lim . Also, during the seventh week of gestation the lim s rotate in opposit e directions. The upper lim rotates 90 laterally, so that the extensor muscles l ie on the lateral and posterior surface and the thum s lie laterally, whereas th e lower lim rotates approximately 90 medially, placing the extensor muscles on t he anterior surface and the ig toe medially. While the external shape is eing esta lished, mesenchyme in the uds egins to condense and these cells different iate into chondrocytes (Fig. 8.13). By the 6th week of development the rst hyalin e cartilage models, foreshadowing the ones of the extremities, are formed y th ese chondrocytes (Figs. 8.13 and 8.15). Joints are formed in the cartilaginous c ondensations when chondrogenesis is arrested and a joint interzone is induced. C ells in this region increase in num er and density and then a joint cavity is fo rmed y cell death. Surrounding cells differentiate into a joint capsule. Factor s regulating the positioning of joints are not clear, ut the secreted molecule WNT14 appears to e the inductive signal. Ossi cation of the ones of the extremit ies, endochondral ossi cation, egins y the end of the em ryonic period. Primary ossi cation centers are
184 Part Two: Special Em ryology Ilium Pu is Ti ia Fi ula Pu is Femur Ti ia Footplate cartilages B Ilium Femur Fi ula Tarsal cartilages Pu is Ilium C Ischium Tarsal cartilages Metatarsal cartilages D Figure 8.13 A. Longitudinal section through the lim ud of a mouse em ryo, show ing a core of mesenchyme covered y a layer of ectoderm that thickens at the dis tal order of the lim to form the AER. In humans this occurs during the fth week of development. B. Lower extremity of an early 6-week em ryo, illustrating the r st hyaline cartilage models. C and D. Complete set of cartilage models at the en d of the sixth and the eginning of the eighth week, respectively. present in all long ones of the lim s y the 12th week of development. From the primary center in the shaft or diaphysis of the one, endochondral ossi cation gr adually progresses toward the ends of the cartilaginous model (Fig. 8.15). At i rth the diaphysis of the one is usually completely ossi ed, ut the two ends, the epiphyses, are still cartilaginous. Shortly thereafter, however, ossi cation cent ers arise in the epiphyses. Temporarily a cartilage plate remains etween the di aphyseal and epiphyseal ossi cation centers. This plate, the
Chapter 8: Skeletal System 185 A B C Figure 8.14 Scanning electron micrographs of human hands. A. At 48 days. Cell de ath in the apical ectodermal ridge creates a separate ridge for each digit. B. A t 51 days. Cell death in the interdigital spaces produces separation of the digi ts. C. At 56 days. Digit separation is complete. The nger pads will create patter ns for ngerprints. epiphyseal plate, plays an important role in growth in the length of the ones. Endochondral ossi cation proceeds on oth sides of the plate (Fig. 8.15). When the one has acquired its full length, the epiphyseal plates disappear and the epip hyses unite with the shaft of the one. In long ones an epiphyseal plate is fou nd on each extremity; in smaller ones, such as the phalanges, it is found only at one extremity; and in irregular ones, such as the verte rae, one or more pri mary centers of ossi cation and usually several secondary centers are present. MOL ECULAR REGULATION OF LIMB DEVELOPMENT Positioning of the lim s along the cranioc audal axis in the ank regions of the em ryo is regulated y the HOX genes express ed along this axis. These
186 Part Two: Special Em ryology Figure 8.15 Endochondral one formation. A. Mesenchyme cells egin to condense a nd differentiate into chondrocytes. B. Chondrocytes form a cartilaginous model o f the prospective one. C and D. Blood vessels invade the center of the cartilag inous model ringing oteo lasts ( lack cells) and restricting proliferating chon drocytic cells to the ends (epiphyses) of the ones. Chondrocytes toward the sha ft side (diaphysis) undergo hypertrophy and apoptosis as they mineralize the sur rounding matrix. Osteo lasts ind to the mineralized matrix and deposit one mat rices. Later, as lood vessels invade the epiphyses, secondary ossi cation centers form. Growth of the ones is maintained y proliferation of chondrocytes in the growth plates (D). homeo ox genes are expressed in overlapping patterns from head to tail (see Chap ter 5), with some having more cranial limits than others. For example, the crani al limit of expression of HOXB8 is at the cranial order of the forelim , and mi sexpression of this gene alters the position of these lim s. Once positioning al ong the craniocaudal axis is determined, growth must e regulated along the prox imodistal, anteroposterior, and dorsoventral axes (Fig. 8.16). Lim outgrowth, w hich occurs rst, is initiated y FGF-10 secreted y lateral plate mesoderm cells (Fig. 8.16A). Once outgrowth is initiated, one morphogenetic proteins (BMPs), e xpressed in ventral ectoderm, induce formation of the AER y signaling through t he homeo ox gene MSX2. Expression of
Chapter 8: Skeletal System 187 Radical fringe (a homologue of Drosophila fringe), in the dorsal half of the lim ectoderm, restricts the location of the AER to the distal tip of the lim s. Th is gene induces expression of Ser-2, a homologue of Drosophila serrate, at the order etween cells expressing Radical fringe and those that are not. It is at t his order that the AER is esta lished. Formation of the order itself is assist ed y expression of Engrailed-1 in ventral ectoderm cells, since this gene repre sses expression of Radical fringe. After the ridge is esta lished, it expresses FGF-4 and FGF-8, which maintain the progress zone, the rapidly proliferating pop ulation of mesenchyme cells adjacent to the ridge (Fig. 8.16A). Distal growth of the lim is then effected y these rapidly proliferating cells under the in uence of the FGFs. As growth occurs, mesenchymal cells at the proximal end of the pro gress zone ecome farther away from the ridge and its in uence and egin to slow t heir division rates and to differentiate. Patterning of the anteroposterior axis of the lim is regulated y the zone of polarizing activity (ZPA), a cluster of cells at the posterior order of the lim near the ank (Fig. 8.16B ). These cell s produce retinoic acid (vitamin A), which initiates expression of sonic hedgeho g (SHH), a secreted factor that regulates the anteroposterior axis. Thus, for ex ample, digits appear in the proper order, with the thum on the radial (anterior ) side. As the lim grows, the ZPA moves distalward to remain in proximity to th e posterior order of the AER. Misexpression of retinoic acid or SHH in the ante rior margin of a lim containing a normally expressing ZPA in the posterior ord er results in a mirror image duplication of lim structures (Fig. 8.17). The dor soventral axis is also regulated y BMPs in the ventral ectoderm which induce ex pression of the transcription factor EN1. In turn, EN1 represses WNT7a expressio n restricting it to the dorsal lim ectoderm. WNT7a is secreted factor that indu ces expression of LMX1, a transcription factor containing a homeodomain, in the dorsal mesenchyme (Fig. 8.16C ). LMX1 speci es cells to e dorsal, esta lishing th e dorsoventral components. In addition, WNT7a maintains SHH expression in the ZP A and therefore indirectly affects anteroposterior patterning as well. These two genes are also intimately linked in signaling pathways in Drosophila, and this interaction is conserved in verte rates. In fact, all of the patterning genes in the lim have feed ack loops. Thus, FGFs in the AER activate SHH in the ZPA, wh ile WNT7a maintains the SHH signal. Although patterning genes for the lim axes have een determined, it is the HOX genes that regulate the types and shapes of the ones of the lim (Fig. 8.15D). Thus, HOX gene expression, which results fro m the com inatorial expression of SHH, FGFs, and WNT7a, occurs in phases in thre e places in the lim that correspond to formation of the proximal (stylopod), mi ddle (zeugopod), and distal (autopod) parts. Genes of the HOXA and HOXD clusters are the primary determinants in the lim , and variations in their com inatorial patterns of expression may account for differences in forelim and hindlim str uctures. Just as in the craniocaudal axis of the em ryo, HOX genes are nested in overlapping patterns of expression that somehow regulate patterning
188 Part Two: Special Em ryology
Chapter 8: Skeletal System 189 (Fig. 8.16D). Factors determining forelim versus hindlim are the transcription factors TBX5 (forelim s) and TBX4 (hindlim s). CLINICAL CORRELATES Bone Age Radiologists use the appearance of various ossi cation centers to determi ne whether a child has reached his or her proper maturation age. Useful informat ion a out one age is o tained from ossi cation studies in the hands and wrists of children. Prenatal analysis of fetal ones y ultrasonography provides informat ion a out fetal growth and gestational age. Lim Defects Lim malformations occu r in approximately 6/10,000 live irths, with 3.4/10,000 affecting the upper lim and 1.1/10,000, the lower. These defects are often associated with other irth defects involving the craniofacial, cardiac, and genitourinary systems. A norma lities of the lim s vary greatly, and they may e represented y partial (merome lia) or complete a sence (amelia) of one or more of the extremities. Sometimes t he long ones are a sent, and rudimentary hands and feet are attached to the tru nk y small, irregularly shaped ones (phocomelia, a form of meromelia) (Fig. 8. 18, A and B). Sometimes all segments of the extremities are present ut a normal ly short (micromelia). Although these a normalities are rare and mainly heredita ry, cases of teratogen-induced lim defects have een documented. For example, m any children with lim malformations were orn etween 1957 and 1962. Many mothe rs of these infants had taken thalidomide, a drug widely used as a sleeping pill and antinauseant. It was su sequently esta lished that thalidomide causes a cha racteristic syndrome of malformations consisting of a sence or gross deformities of the long ones, intestinal atresia, and cardiac anomalies. Figure 8.16 (opposite page). Molecular regulation of patterning and growth in th e lim . A. Lim outgrowth is initiated y FGF-10 secreted y lateral plate mesod erm in the lim forming regions. Once outgrowth is initiated, the AER is induced y BMPs and restricted in its location y the gene radical fringe expressed in dorsal ectoderm. In turn, this expression induces that of SER2 in cells destined to form the AER. After the ridge is esta lished, it expresses FGF-4 and FGF-8 t o maintain the progress zone, the rapidly proliferating mesenchyme cells adjacen t to the ridge. B. Anteroposterior patterning of the lim is controlled y cells in the ZPA at the posterior order. These cells produce retinoic acid (vitamin A), which initiates expression of sonic hedgehog, regulating patterning. C. The dorsoventral lim axis is directed y WNT7a, which is expressed in the dorsal ec toderm. This gene induces expression of the transcription factor LMX1 in the dor sal mesenchyme, specifying these cells as dorsal. D. Bone type and shape are reg ulated y HOX genes whose expression is determined y the com inatorial expressi on of SHH, FGFs, and WNT7a. HOXA and HOXD clusters are the primary determinants of one morphology.
Figure 8.17 Experimental procedure for grafting a new ZPA from one lim ud into another using chick em ryos. The result is the production of a lim with mirror image duplication of the digits (chicks have only three digits, num ered II, II I, and IV), indicating the role of the ZPA in regulating anteroposterior pattern ing of the lim . Sonic hedgehog protein is the molecule secreted y the ZPA resp onsi le for this regulation. Figure 8.18 A. Child with unilateral amelia. B. Patient with a form of meromelia called phocomelia. The hands and feet are attached to the trunk y irregularly shaped ones.
Chapter 8: Skeletal System 191 A Figure 8.19 Digital defects. A. Polydactyly, extra digits. B. Syndactyly, fused digits. C. Cleft foot, lo ster claw deformity. Since the drug is now eing used to treat AIDS and cancer patients, there is con cern that its return will result in a new wave of lim defects. Studies indicate that the most sensitive period for teratogen-induced lim malformations is the fourth and fth weeks of development. A different category of lim a normalities c onsists of extra ngers or toes (polydactyly) (Fig. 8.19A). The extra digits frequ ently lack proper muscle connections. A normalities with an excessive num er of ones are mostly ilateral, while the a sence of a digit such as a thum (ectrod actyly) is usually unilateral. Polydactyly can e inherited as a dominant trait ut may also e induced y teratogens. A normal fusion is usually restricted to the ngers or toes (syndactyly). Normally mesenchyme etween prospective digits in the handplates and footplates reaks down. In 1/2000 irths this fails to occur , and the result is fusion of one or more ngers and toes (Fig. 8.19B ). In some c ases the ones actually fuse.
192 Part Two: Special Em ryology Cleft hand and foot (lo ster claw deformity) consists of an a normal cleft etwe en the second and fourth metacarpal ones and soft tissues. The third metacarpal and phalangeal ones are almost always a sent, and the thum and index nger and the fourth and fth ngers may e fused (Fig. 8.19C ). The two parts of the hand are somewhat opposed to each other and act like a lo ster claw. The role of the HOX genes in lim development is illustrated y two a normal phenotypes produced y mutations in these genes: Mutations in HOXA13 result in hand-foot-genital syndr ome, characterized y fusion of the carpal ones and small short digits. Females often have a partially ( icornuate) or completely (didelphic) divided uterus an d a normal positioning of the urethral ori ce. Males may have hypospadias. Mutatio ns in HOXD13 result in a com ination of syndactyly and polydactyly (synpolydacty ly). Clu foot usually accompanies syndactyly. The sole of the foot is turned inw ard, and the foot is adducted and plantar exed. It is o served mainly in males an d in some cases is hereditary. A normal positioning of the legs in utero may als o cause clu foot. Congenital a sence or de ciency of the radius is usually a genet ic a normality o served with malformations in other structures, such as craniosy nostosisradial aplasia syndrome. Associated digital defects, which may include a sent thum s and a short curved ulna, are usually present. Amniotic ands may cau se ring constrictions and amputations of the lim s or digits (Fig. 8.20). The or igin of ands is not clear, ut they may represent adhesions etween the amnion and affected structures in the fetus. Other investigators elieve that ands ori ginate from tears in the amnion that detach and surround part of the fetus. Figure 8.20 Digit amputations resulting from amniotic ands.
Chapter 8: Skeletal System 193 Congenital hip dislocation consists of underdevelopment of the aceta ulum and he ad of the femur. It is rather common and occurs mostly in females. Although disl ocation usually occurs after irth, the a normality of the ones develops prenat ally. Since many a ies with congenital hip dislocation are reech deliveries, i t has een thought that reech posture may interfere with development of the hip joint. It is frequently associated with laxity of the joint capsule. Verte ral Column During the fourth week of development, cells of the sclerotomes shift their position to surround oth the spinal cord and the notochord (Fig. 8 .1). This mesenchymal column retains traces of its segmental origin, as the scle rotomic locks are separated y less dense areas containing intersegmental arter ies (Fig. 8.21A). During further development the caudal portion of each scleroto me segment proliferates extensively and condenses (Fig. 8.21B). This proliferati on is so extensive that it proceeds into the su jacent intersegmental tissue and inds the caudal half of one sclerotome to the cephalic half of the su jacent s clerotome (arrows in Fig. 8.21,A and B). Hence, y incorporation of the interseg mental tissue into the precartilaginous verte ral ody (Fig. 8.21B ), the ody o f the Notochord Nucleus pulposus and interverte ral disc Interverte ral disc Intersegmental mesenchyme Artery Nerve Sclerotome segment Myotome Precartilaginous verte ral ody Transverse process Annulus fi rosus A B C Figure 8.21 Formation of the verte ral column at various stages of development. A. At the fourth week of development, sclerotomic segments are separated y less dense intersegmental tissue. Note the position of the myotomes, intersegmental arteries, and segmental nerves. B. Condensation and proliferation of the caudal half of one sclerotome proceed into the intersegmental mesenchyme and cranial ha lf of the su jacent sclerotome (arrows in A and B). Note the appearance of the i nterverte ral discs. C. Precartilaginous verte ral odies are formed y the uppe r and lower halves of two successive sclerotomes and the intersegmental tissue. Myotomes ridge the interverte ral discs and, therefore, can move the verte ral column.
194 Part Two: Special Em ryology verte ra ecomes intersegmental. Patterning of the shapes of the different verte ra is regulated y HOX genes. Mesenchymal cells etween cephalic and caudal par ts of the original sclerotome segment do not proliferate ut ll the space etween two precartilaginous verte ral odies. In this way they contri ute to formation of the interverte ral disc (Fig. 8.21B). Although the notochord regresses entir ely in the region of the verte ral odies, it persists and enlarges in the regio n of the interverte ral disc. Here it contri utes to the nucleus pulposus, which is later surrounded y circular ers of the annulus rosus. Com ined, these two s tructures form the interverte ral disc (Fig. 8.21C ). Rearrangement of sclerotom es into de nitive verte rae causes the myotomes to ridge the interverte ral discs , and this alteration gives them the capacity to move the spine (Fig. 8.21C ). F or the same reason, intersegmental arteries, at rst lying etween the sclerotomes , now pass midway over the verte ral odies. Spinal nerves, however, come to lie near the interverte ral discs and leave the verte ral column through the interv erte ral foramina. CLINICAL CORRELATES Verte ral Defects The process of formation and rearrangement of segmental sclero tomes into de nitive verte rae is complicated, and it is fairly common to have two successive verte rae fuse asymmetrically or have half a verte ra missing, a cau se of scoliosis (lateral curving of the spine). Also, the num er of verte rae is frequently more or less than the norm. A typical example of these a normalities is found in patients with Klippel-Feil anomaly. These patients have fewer than normal cervical verte rae, and often other verte rae are fused or a normal in sh ape. This anomaly is usually associated with other a normalities. One of the mos t serious verte ral defects is the result of imperfect fusion or nonunion of the verte ral arches. Such an a normality, known as cleft verte ra (spina i da), may involve only the ony verte ral arches, leaving the spinal cord intact. In thes e cases the ony defect is covered y skin, and no neurological de cits occur (spi na i da occulta). A more severe a normality is spina i da cystica, in which the ne ural tu e fails to close, verte ral arches fail to form, and neural tissue is ex posed. Any neurological de cits depend on the level and extent of the lesion. This defect, which occurs in 1/1000 irths, may e prevented, in many cases, y prov iding mothers with folic acid prior to conception. Spina i da can e detected pre natally y ultrasound (Fig. 8.22), and if neural tissue is exposed, amniocentesi s can detect elevated levels of -fetoprotein in the mniotic uid. (For the v rious types of spin bi d , see Figs. 19.15 nd 19.16.)
Ch pter 8: Skelet l System 195 Figure 8.22 Ultr sound sc ns of the vertebr l columns in norm l inf nt (A) nd one with spin bi d (B) ged 4 months. The cleft vertebr e re re dily pp rent ( rrows). Ribs nd Sternum Ribs form from cost l processes of thor cic vertebr e nd thus re derived from the sclerotome portion of p r xi l mesoderm. The sternum develo ps independently in som tic mesoderm in the ventr l body w ll. Two stern l b nds re formed on either side of the midline, nd these l ter fuse to form c rtil g inous models of the m nubrium, sternebr e, nd xiphoid process. Summ ry The skelet l system develops from mesenchyme, which is derived from the mesoderm l germ l yer nd from neur l crest. Some bones, such s the t bones of the skull, undergo membr nous ossi c tion; th t is, mesenchyme cells re directly tr nsformed into osteobl sts (Fig. 8.2). In most bones, such s the long bones o f the limbs, mesenchyme condenses nd forms hy line c rtil ge models of bones (F ig. 8.15). Ossi c tion centers ppe r in these c rtil ge models, nd the bone gr d u lly ossi es by endochondr l ossi c tion. The skull consists of the neurocr nium n d viscerocr nium (f ce). The neurocr nium includes membr nous portion, which f orms the cr ni l v ult, nd c rtil ginous portion (chondrocr nium), which form s the b se of the skull. Neur l crest cells form the f ce, most of the cr ni l v ult, nd the prechord l p rt of the chondrocr nium (the p rt th t lies rostr l to the notochord). P r xi l mesoderm forms the rem inder of the skull. Limbs for m s buds long the body w ll th t ppe r in the fourth week. L ter l pl te meso derm forms the bones nd connective tissue, while muscle cells migr te to the li mbs from the somites. The AER regul tes limb outgrowth,
196 P rt Two: Speci l Embryology nd the ZPA controls nteroposterior p tterning. M ny of the genes th t regul te limb growth nd p tterning h ve been de ned (see Fig. 8.16). The vertebr l column nd ribs develop from the sclerotome comp rtments of the somites, nd the stern um is derived from mesoderm in the ventr l body w ll. A de nitive vertebr is form ed by condens tion of the c ud l h lf of one sclerotome nd fusion with the cr n i l h lf of the subj cent sclerotome (Fig. 8.21). The m ny bnorm lities of the skelet l system include vertebr l (spin bi d ), cr ni l (cr nioschisis nd cr nio synostosis), nd f ci l (cleft p l te) defects. M jor m lform tions of the limbs re r re, but defects of the r dius nd digits re often ssoci ted with other bnorm lities (syndromes). Problems to Solve 1. Why re cr ni l sutures import n t? Are they involved in ny bnorm lities? 2. If you observe congenit l bsence of the r dius or digit l defects, such s bsent thumb or polyd ctyly, would you consider ex mining the inf nt for other m lform tions? Why? 3. Expl in the orig in of scoliosis s vertebr l nom ly. Wh t genes might be involved in this bn orm lity? SUGGESTED READING Cohen MM, M cLe n: Cr niosynostosis: Di gnosis, Ev lu tion nd M n gement. 2nd ed. New York, Oxford University Press, 2000. Filly RA: Sonogr p hic n tomy of the norm l fetus. In H rrison MR, Golbus MS, Filly RA (eds): The Unborn P tient. Pren t l Di gnosis nd Tre tment. 2nd ed. Phil delphi , WB S und ers, 1991. Filly RA, Golbus MS: Ultr sonogr phy of the norm l nd p thologic fet l skeleton. R diol Clin North Am 20:311, 1982. Gorlin RJ: Syndromes of the He d nd Neck. 2nd ed. New York, McGr w-Hill, 1976. H rtm n C, T bin CJ: Wnt14 pl ys pivot l role in inducing synovi l joint form tion in the developing ppendicu l r skeleton. Cell 104:341, 2001. Hehr U, Muenke M: Cr niosynostosis syndromes: from genes to prem ture fusion of skull bones. Mol Gen Met b 68:139, 1999. Ji ng X, Iseki S, M xson RE, Sucov HM, Morriss-K y GM: Tissue origins nd inter ction s in the m mm li n skull v ult. Dev Biol 241:106, 2002. L ufer E, et l.: Expres sion of R dic l fringe in limb bud ectoderm regul tes pic l ectoderm l ridge fo rm tion. N ture 386:366, 1997. Lenz W: Th lidomide nd congenit l bnorm lities. L ncet 1:1219, 1962. Mortlock D, Innis JW: Mut tion of HOXA13 in h nd-foot-geni t l syndrome. N ture Genet 15:179, 1997. Muenke M, Schell U: Fibrobl st growth f ctor receptor mut tions in hum n skelet l disorders. Trends Genet 11:308, 1995. Mur g ki Y, Mundlos S, Upton J, Olsen BR: Altered growth nd br nching p tterns in synpolyd ctyly c used by mut tions in HOXD13. Science 272:548, 1996. Pizette S, Ab te-Shen C, Nisw nder L: BMP controls proximodist l outgrowth, vi inducti on of the pic l ectoderm l ridge, nd dorsoventr l p tterning in the vertebr te limb. Development 128:4463, 2001.
Ch pter 8: Skelet l System 197
Riddle RD, et l.: Induction of the LIM homeobox gene Lmx1 by Wnt7 est blishes dorsoventr l p ttern in the vertebr te limb. Cell 83:631, 1995. Rodriguez-Est b n C, et l.: R dic l fringe positions the pic l ectoderm l ridge t the dorsove ntr l bound ry of the vertebr te limb. N ture 386:360, 1997. Shubin N, T bin C, C rroll S: Fossils, genes nd the evolution of nim l limbs. N ture 388:639, 199 7.
ch pter 9 Muscul r System With the exception of some smooth muscle tissue (see below), the muscul r system develops from the mesoderm l germ l yer nd consists of skelet l, smooth, nd c rdi c muscle. Skelet l muscle is derived from p r xi l mesoderm, which forms so mites from the occipit l to the s cr l regions nd somitomeres in the he d. Smoo th muscle differenti tes from spl nchnic mesoderm surrounding the gut nd its de riv tives nd from ectoderm (pupill ry, m mm ry gl nd, nd swe t gl nd muscles). C rdi c muscle is derived from spl nchnic mesoderm surrounding the he rt tube. Stri ted Skelet l Muscul ture Somites nd somitomeres form the muscul ture of th e xi l skeleton, body w ll, limbs, nd he d. From the occipit l region c ud lly , somites form nd differenti te into the sclerotome, derm tome, nd two muscleforming regions (Fig. 9.1). One of these is in the dorsol ter l region of the so mite. It expresses the muscle-speci c gene MYO-D nd migr tes to provide progenito r cells for limb nd body w ll (hypomeric) muscul ture (Figs. 9.1 nd 9.2). The other region lies dorsomedi lly, migr tes ventr l to cells th t form the derm to me, nd forms the myotome. This region, which expresses the muscle-speci c gene MY F5, forms epimeric muscul ture (Figs. 9.1 nd 9.2). During differenti tion, prec ursor cells, the myobl sts, fuse nd form long, multinucle ted 199
200 P rt Two: Speci l Embryology Figure 9.1 St ges in the development of somite. A. Mesoderm cells re rr nged round sm ll c vity. B. Cells of the ventr l nd medi l w lls of the somite l ose their epitheli l rr ngement nd migr te in the direction of the notochord. These cells collectively constitute the sclerotome. Cells t the dorsol ter l po rtion of the somite migr te s precursors to limb nd body w ll muscul ture. Dor somedi l cells migr te bene th the rem ining dors l epithelium of the somite to form the myotome. C. Cells forming the myotome continue to extend bene th the do rs l epithelium. D. After ventr l extension of the myotome, derm tome cells lose their epitheli l con gur tion nd spre d out under the overlying ectoderm to form dermis.
Ch pter 9: Muscul r System 201 Figure 9.2 Expression p tterns of genes th t regul te somite differenti tion. So nic hedgehog (SHH), secreted by the notochord nd oor pl te of the neur l tube, c uses the ventr l p rt of the somite to form sclerotome nd to express PAX1, whi ch in turn controls chondrogenesis nd vertebr l form tion. WNT proteins from th e dors l neur l tube ctiv te PAX3, which dem rc tes the dermomyotome. WNT prote ins lso direct the dorsomedi l portion of the somite to form ep xi l (b ck) mus cles nd to express the muscle-speci c gene MYF5. The middors l portion of the som ite is directed to become dermis by neurotrophin 3 (NT-3) expressed by the dors l neur l tube. Hyp xi l (limb nd body w ll) muscul ture is derived from the dor sol ter l portion of the somite under the combined in uence of ctiv ting WNT prot eins nd inhibitory BMP-4 protein, which together ctiv te MYO-D expression. muscle bers. Myo brils soon ppe r in the cytopl sm, nd by the end of the third mo nth, cross-stri tions typic l of skelet l muscle ppe r. A simil r process occur s in the seven somitomeres in the he d region rostr l to the occipit l somites. Somitomeres rem in loosely org nized structures, however, never segreg ting into sclerotome nd dermomyotome segments. Molecul r Regul tion of Muscle Developmen t Genes regul ting muscle development h ve recently been identi ed. BMP4 nd prob bly FGFs from l ter l pl te mesoderm, together with WNT proteins from dj cent e ctoderm, sign l the dorsol ter l cells of the somite to express the muscle-speci c gene MYO-D. BMP4 secreted by overlying ectoderm induces
202 P rt Two: Speci l Embryology production of WNT proteins by the dors l neur l tube, nd these proteins c use d orsomedi l cells of the somite to ctiv te MYF5, nother musclespeci c gene (Fig. 9.2). Both of these genes re members of the MYO-D muscle-speci c f mily, which l so includes the myogenin nd MRF4 genes. MYO-D nd MYF5 proteins ctiv te the ge nes for myogenin nd MRF5, which in turn promote form tion of myotubes nd myo ber s. All MYO-D f mily members h ve DNA binding sites nd ct s tr nscription f ct ors to regul te downstre m genes in the muscle differenti tion p thw y. P tterning of Muscles P tterns of muscle form tion re controlled by connective tissue into which myobl sts migr te. In the he d region these connective tissues re derived from neur l crest cells; in cervic l nd occipit l regions they dif ferenti te from somitic mesoderm; nd in the body w ll nd limbs they origin te from som tic mesoderm. Deriv tives of Precursor Muscle Cells By the end of the fth week prospective musc le cells re collected into two p rts: sm ll dors l portion, the epimere, form ed from the dorsomedi l cells of the somite th t reorg nized s myotomes; nd l rger ventr l p rt, the hypomere, formed by migr tion of dorsol ter l cells of the somite (Figs. 9.1B nd 9.3A). Nerves innerv ting segment l muscles re lso divided into dors l prim ry r mus for the epimere nd ventr l prim ry r mus for the hypomere (Fig. 9.3B ) nd these nerves will rem in with their origin l m uscle segment throughout its migr tion. Myobl sts of the epimeres form the exten sor muscles of the vertebr l column, nd those of the hypomeres give rise to mus cles of the limbs nd body w ll (Fig. 9.3B). Myobl sts from cervic l hypomeres f orm the sc lene, geniohyoid, nd prevertebr l muscles. Those from thor cic segme nts split into three l yers, which in the thor x re represented by the extern l intercost l, intern l intercost l, nd innermost intercost l or tr nsversus tho r cis muscle (Fig. 9.3B ). In the bdomin l w ll these three muscle l yers consi st of the extern l oblique, the intern l oblique, nd the tr nsversus bdominis muscles. The ribs c use the muscles in the w ll of the thor x to m int in their segment l ch r cter, where s muscles in the v rious segments of the bdomin l w ll fuse to form l rge sheets of muscle tissue. Myobl sts from the hypobl st of l umb r segments form the qu dr tus lumborum muscle, nd those from s cr l nd coc cyge l regions form the pelvic di phr gm nd stri ted muscles of the nus. In d dition to the three ventrol ter l muscle l yers, ventr l longitudin l column rises t the ventr l tip of the hypomeres (Fig. 9.3B ). This column
Ch pter 9: Muscul r System 203 Figure 9.3 A. Tr nsverse section through the thor cic region of 5-week embryo. The dors l portion of the body w ll muscul ture (epimere) nd the ventr l porti on (hypomere) re innerv ted by dors l prim ry r mus nd ventr l prim ry r m us, respectively. B. Simil r to A l ter in development. The hypomere h s formed three muscle l yers nd ventr l longitudin l muscle column. is represented by the rectus bdominis muscle in the bdomin l region nd by the infr hyoid muscul ture in the cervic l region. In the thor x, the longitudin l muscle norm lly dis ppe rs, but is occ sion lly represented by the stern lis mus cle. He d Muscul ture All volunt ry muscles of the he d region re derived from p r x i l mesoderm (somitomeres nd somites), including muscul ture of the tongue, eye (except th t of the iris, which is derived from optic cup ectoderm), nd th t ssoci ted with the ph rynge l (viscer l) rches (T ble 9.1). P tterns of muscle form tion in the he d re directed by connective tissue elements derived from ne ur l crest cells.
Limb Muscul ture The rst indic tion of limb muscul ture is observed in the sevent h week of development s condens tion of mesenchyme ne r the b se of the limb buds (Fig. 9.4A). The mesenchyme is derived from dorsol ter l cells of the
204 P rt Two: Speci l Embryology TABLE 9.1 Origins of the Cr niof ci l Muscles Muscles Superior, medi l, ventr l recti Superior oblique J w closing L ter l rec tus J w opening, other 2nd rch Styloph ryngeus Intrinsic l rynge ls Tongue Inne rv tion Oculomotor (III) Trochle r (IV) Trigemin l (V) Abducens (VI) F ci l (VII ) Glossoph rynge l (IX) V gus (X) Hypogloss l (XII) Mesoderm l Origin Somitomeres 1,2 Somitomere 3 Somitomere 4 Somitomere 5 Somitom ere 6 Somitomere 7 Somites 1,2 Somites 25 Somites 25 constitute the occipit l group (somite 1 degener tes for the most p rt ). Figure 9.4 A. Myotomes in the he d, neck, nd thor cic region of 7-week embryo . Note the loc tion of the preotic nd occipit l myotomes nd condens tion of me senchyme t the b se of the limb bud, B. Tr nsverse section through the region o f tt chment of the limb bud. Note the dors l (extensor) nd ventr l ( exor) muscu l r components of the limb. somites th t migr te into the limb bud to form the muscles. As in other regions, connective tissue dict tes the p ttern of muscle form tion, nd this tissue is derived from som tic mesoderm, which lso gives rise to the bones of the limb. W ith elong tion of the limb buds, the muscle tissue splits into exor nd extensor components (Fig. 9.4B ). Although muscles of the limbs re segment l initi lly, with time they fuse nd re then composed of tissue derived from sever l segment s. The upper limb buds lie opposite the lower ve cervic l nd upper two thor cic segments (Fig. 9.5, A nd B), nd the lower limb buds lie opposite the lower fou r lumb r nd upper two s cr l segments (Fig. 9.5C ). As soon s the buds form, v entr l prim ry r mi from the ppropri te spin l nerves penetr te into the mesenc hyme (Fig. 9.6). At rst e ch ventr l r mus enters with isol ted dors l nd ventr l br nches, but soon these br nches unite to form l rge dors l
Ch pter 9: Muscul r System 205 C4 C5 C6 C4 C5 C6 T2 C8 T1 T2 A B C7 Pre xi l side of limb Post xi l side of limb C Figure 9.5 Limb buds with their segments of origin indic ted. With further devel opment the segment l p ttern dis ppe rs; however, n orderly sequence in the der m tome p ttern c n still be recognized in the dult. A. Upper limb bud t 5 week s. B. Upper limb bud t 6 weeks. C. Limb buds t 7 weeks.
206 P rt Two: Speci l Embryology
nd ventr l nerves. Thus the r di l nerve, which supplies the extensor muscul tu re, is formed by combin tion of the dors l segment l br nches, where s the uln r nd medi n nerves, which supply the exor muscul ture, re formed by combin t ion of the ventr l br nches. Immedi tely fter the nerves h ve entered the limb buds, they est blish n intim te cont ct with the differenti ting mesoderm l con dens tions, nd the e rly cont ct between the nerve nd muscle cells is prereq uisite for their complete function l differenti tion. Spin l nerves not only pl y n import nt role in differenti tion nd motor innerv tion of the limb muscul ture, but lso provide sensory innerv tion for the derm tomes. Although the orig in l derm tom l p ttern ch nges with growth of the extremities, n orderly seque nce c n still be recognized in the dult (Fig. 9.5). Clinic l Correl tes P rti l or complete bsence of one or more muscles is r ther common. One of the best known ex mples is tot l or p rti l bsence of the pector lis m jor muscle ( Pol nd nom ly). Simil rly, the p lm ris longus, the serr tus nterior, nd the qu dr tus femoris muscles m y be p rti lly or entirely bsent. P rti l or comple te bsence of bdomin l muscul ture results in prunebelly syndrome (Fig. 9.7). U su lly the bdomin l w ll is so thin th t org ns re visible nd e sily p lp ted . This defect is often ssoci ted with m lform tions of the urin ry tr ct nd bl dder.
* * * * * Figure 9.6 Sc nning electron microgr ph of mouse upper limb bud, showing spin l nerves entering the limb. Asterisks, spin l g ngli .
Ch pter 9: Muscul r System 207
C rdi c Muscle C rdi c muscle develops from spl nchnic mesoderm surrounding the endotheli l he rt tube. Myobl sts dhere to one nother by speci l tt chments t h t l ter develop into interc l ted discs. Myo brils develop s in skelet l muscle , but myobl sts do not fuse. During l ter development, few speci l bundles of muscle cells with irregul rly distributed myo brils become visible. These bundles, the Purkinje bers, form the conducting system of the he rt. Smooth Muscle Smooth muscle in the w ll of the gut nd gut deriv tives is derived from spl nchnic me soderm surrounding the endoderm of these structures. V scul r smooth muscle diff erenti tes from mesoderm dj cent to v scul r endothelium. Sphincter nd dil tor muscles of the pupil nd muscle tissue in the m mm ry gl nd nd swe t gl nds or igin te from ectoderm.
Figure 9.7 Prune belly syndrome: ll muscul ture.
distended bdomen from pl si
of bdomin l w
208 P rt Two: Speci l Embryology Summ ry Most muscles rise from the mesoderm. Skelet l muscles re derived from p r xi l mesoderm, including ( ) somites, which give rise to muscles of the xi l skeleton, body w ll, nd limbs, nd (b) somitomeres, which give rise to muscle s of the he d. Progenitor cells for muscle tissues re derived from the dorsol t er l nd dorsomedi l portions of the somites. Cells in the dorsol ter l portion express MYO-D nd migr te to form hypomeric muscle; cells in the dorsomedi l por tion express MYF5, migr te ventr l to the derm tome to form the myotome, nd ult im tely form epimeric muscul ture. By the fth week muscle precursor cells re div ided into sm ll dors l portion, the epimere, innerv ted by dors l prim ry r mus, nd l rger ventr l portion, the hypomere, innerv ted by ventr l prim ry r mus. Myobl sts from epimeres form extensor muscles of the vertebr l column, w hile those of the hypomere form limb nd body w ll muscul ture. Connective tissu e derived from somites, som tic mesoderm, nd neur l crest (he d region) provide templ te for est blishment of muscle p tterns. Most smooth muscles nd c rdi c muscle bers re derived from spl nchnic mesoderm. Smooth muscles of the pupil, m mm ry gl nd, nd swe t gl nds differenti te from ectoderm. Problems to Solve 1. Muscle cells re derived from wh t two regions of the somit e? Which region forms the epimere nd which the hypomere? Wh t muscles form from e ch of these regions? 2. In ex mining newborn fem le, you note th t her righ t nipple is lower th n the left nd th t the right nterior xill ry fold is ne rly bsent. Wh t is your di gnosis? 3. P tterning of muscles is dependent on wh t type of tissue? 4. How do you expl in the f ct th t the phrenic nerve, which o rigin tes from cervic l segments 3, 4, nd 5, innerv tes the di phr gm in the th or cic region?
SUGGESTED READING Bl gden CS, Hughes SM: Extrinsic in uences on limb muscle org ni z tion. Cell Tiss Res 296:141, 1999. Br nd-Seberi B, Christ B: Genetic nd epige netic control of muscle development in vertebr tes. Cell Tiss Res 296:199, 1999 Br un T, Arnold HH: Myf5 nd MyoD genes re ctiv ted in distinct mesenchym l st em cells nd determine different skelet l muscle line ges. EMBO J 15:310, 1996. Chev llier A, Kieny M, M uger A: Limb-somite rel tionship: origin of the limb mu scul ture. J Embryol Exp Morphol 41:245, 1977. Christ B, J cob M, J cob HJ: On t he origin nd development of the ventrol ter l bdomin l muscles in the vi n em bryo. An t Embryol 166:87, 1983.
Ch pter 9: Muscul r System 209 Cossu G, et l.: Activ tion of different myogenic p thw ys: myf5 is induced by t he neur l tube nd MyoD by the dors l ectoderm in mouse p r xi l mesoderm. Devel opment 122:429, 1996. Levi AC, Borghi F, G r vogli M: Development of the n l c n l muscles. Dis Colon Rectum 34:262, 1991. Noden DM: The embryonic origins of vi n ceph lic nd cervic l muscles nd ssoci ted connective tissues. Am J An t 168:257, 1983. Noden DM: Cr niof ci l development: new views on old problems. A n t Rec 208:113, 1984. Noden DM: Inter ctions nd f tes of vi n cr niof ci l me senchyme. Development 103:121, 1988.
ch pter 10 Body C vities Form tion of the Intr embryonic C vity At the end of the third week, intr embryo nic mesoderm on e ch side of the midline differenti tes into p r xi l portion, n intermedi te portion, nd l ter l pl te (Fig. 10.1A). When intercellul r c lefts ppe r in the l ter l mesoderm, the pl tes re divided into two l yers: th e som tic mesoderm l yer nd the spl nchnic mesoderm l yer. The l tter is contin uous with mesoderm of the w ll of the yolk s c (Fig. 10.1B). The sp ce bordered by these l yers forms the intr embryonic c vity (body c vity). At rst the right nd left sides of the intr embryonic c vity re in open connection with the extr embryonic c vity, but when the body of the embryo folds ceph loc ud lly nd l te r lly, this connection is lost (Figs. 10.2, AE). In this m nner l rge intr embr yonic c vity extending from the thor cic to the pelvic region forms. CLINICAL CORRELATES Body W ll Defects Ventr l body w ll defects in the thor x or bdomen m y involve the he rt, bdomin l viscer , nd urogenit l org ns. They m y be due to f ilu re of body folding, in which c se one or more of the four folds 211
212 P rt Two: Speci l Embryology P r xi l mesoderm Intermedi te mesoderm Intercellul r clefts Som tic mesoderm l yer W ll of mniotic c vity Spl nchnic mesoderm l yer Intr embryonic c vity W ll of yolk s c L ter l pl te Serous membr ne A Endoderm B Figure 10.1 A. Tr nsverse section through n embryo of pproxim tely 19 d ys. In tercellul r clefts re visible in the l ter l pl te mesoderm. B. Section through n embryo of pproxim tely 20 d ys. The l ter l pl te is divided into som tic nd spl nchnic mesoderm l yers th t line the intr embryonic coelom. Tissue border ing the intr embryonic coelom differenti tes into serous membr nes.
(ceph lic, c ud l, nd two l ter l) responsible for closing the ventr l body w l l t the umbilicus f il to progress to th t region. Another c use of these defec ts is incomplete development of body w ll structures, including muscle, bone, n d skin. Cleft sternum is ventr l body w ll defect th t results from l ck of fu sion of the bil ter l b rs of mesoderm responsible for form tion of this structu re. In some c ses the he rt protrudes through stern l defect (either cleft ste rnum or bsence of the lower third of the sternum) nd lies outside the body (ec topi cordis) (Fig. 10.3A). Sometimes the defect involves both the thor x nd b domen, cre ting spectrum of bnorm lities known s C ntrell pent logy, which i ncludes cleft sternum, ectopi cordis, omph locele, di phr gm tic herni ( nteri or portion), nd congenit l he rt defects (ventricul r sept l defect, tetr logy of F llot). Ectopi cordis defects ppe r to be due to f ilure of progression of ceph lic nd l ter l folds. Omph locele (Fig. 10.3B) is herni tion of bdomin l viscer through n enl rged umbilic l ring. The viscer , which m y include li ver, sm ll nd l rge intestines, stom ch, spleen, or bl dder, re covered by mn ion. The origin of omph locele is f ilure of the bowel to return to the body c vity from its physiologic l herni tion during the 6th to 10th weeks. Omph locel e, which occurs in 2.5/10,000 births, is ssoci ted with high r te of mort lit y (25%) nd severe m lform tions, such s c rdi c nom lies (50%) nd neur l tub e defects (40%). Chromosom l bnorm lities re present in pproxim tely 50% of l iveborn inf nts with omph locele. G stroschisis (Fig. 10.3C ) is herni tion of bdomin l contents through the body w ll directly into the mniotic c vity. It occurs l ter l to the umbilicus,
Ch pter 10: Body C vities 213 Amniotic c vity Surf ce ectoderm Som tic mesoderm Connection between gut nd yolk s c Intr embryonic body c vity Spl nchnic mesoderm Yolk s c Dors l Gut mesentery A B C Figure 10.2 Tr nsverse sections through embryos t v rious st ges of development . A. The intr embryonic c vity is in open communic tion with the extr embryonic c vity. B. The intr embryonic c vity is bout to lose cont ct with the extr embr yonic c vity. C. At the end of the fourth week, spl nchnic mesoderm l yers re c ontinuous with som tic l yers s double-l yered membr ne, the dors l mesentery . Dors l mesentery extends from the c ud l limit of the foregut to the end of th e hindgut. D nd E. Sc nning electron microgr phs of sections through mouse embr yos showing det ils simil r to those in B nd C, respectively. G, Gut tube; rro whe ds, spl nchnic mesoderm; C, body c vity; rrow, dors l mesentery; A, dors l ort ; NT, neur l tube. usu lly on the right, through region we kened by regression of the right umbil ic l vein, which norm lly dis ppe rs. Viscer re not covered by peritoneum or mnion, nd the bowel m y be d m ged by exposure to mniotic uid. Both omph locele nd g stroschisis result in elev ted levels of -fetoprotein in the mniotic uid, which c n be detected pren t lly.
214 P rt Two: Speci l Embryology He rt A B C D Figure 10.3 Ventr l body w ll defects. A. Inf nt with ectopi cordis. Mesoderm o f the sternum h s f iled to fuse, nd the he rt lies outside of the body. B. Omp h locele with f ilure of the intestin l loops to return to the body c vity follo wing physiologic l herni tion. The herni ted loops re covered by mnion. C. Omp h locele in newborn. D. A newborn with g stroschisis. Loops of bowel return to the body c vity but herni te g in through the body w ll, usu lly to the right of the umbilicus in the region of the regressing right umbilic l vein. Unlike om ph locele, the defect is not covered by mnion.
Ch pter 10: Body C vities 215 Lung bud Pleuroperic rdi l fold Phrenic nerve Common c rdin l vein C He rt Figure 10.4 A. Sc nning electron microgr ph showing the ventr l view of mouse embryo (equiv lent to pproxim tely the fourth week in hum n development). The g ut tube is closing, the nterior nd posterior intestin l port ls re visible ( rrowhe ds), nd the he rt (H) lies in the primitive pleuroperic rdi l c vity ( s terisks), which is p rti lly sep r ted from the bdomin l c vity by the septum t r nsversum ( rrow). B. Portion of n embryo t pproxim tely 5 weeks with p rts of the body w ll nd septum tr nsversum removed to show the peric rdioperitone l c n ls. Note the size nd thickness of the septum tr nsversum nd liver cords p enetr ting the septum. C. Growth of the lung buds into the peric rdioperitone l c n ls. Note the pleuroperic rdi l folds.
216 P rt Two: Speci l Embryology G stroschisis occurs in 1/10,000 births but is incre sing in frequency, especi l ly mong young women, nd this incre se m y be rel ted to coc ine use. Unlike om ph locele, g stroschisis is not ssoci ted with chromosome bnorm lities or othe r severe defects. Therefore the surviv l r te is excellent, lthough volvulus (r ot tion of the bowel) resulting in compromised blood supply m y kill l rge reg ions of the intestine nd le d to fet l de th. Serous Membr nes Cells of the som tic mesoderm lining the intr embryonic c vity become mesotheli l nd form the p riet l l yer of the serous membr nes lining th e outside of the peritone l, pleur l, nd peric rdi l c vities. In simil r m n ner, cells of the spl nchnic mesoderm l yer form the viscer l l yer of the serou s membr nes covering the bdomin l org ns, lungs, nd he rt (Fig. 10.1). Viscer l nd p riet l l yers re continuous with e ch other s the dors l mesentery (Fi g. 10.2, C nd E ), which suspends the gut tube in the peritone l c vity. Initi lly this dors l mesentery is thick b nd of mesoderm running continuously from the c ud l limit of the foregut to the end of the hindgut. Ventr l mesentery exi sts only from the c ud l foregut to the upper portion of the duodenum nd result s from thinning of mesoderm of the septum tr nsversum (see Ch pter 13). These me senteries re double l yers of peritoneum th t provide p thw y for blood vesse ls, nerves, nd lymph tics to the org ns.
Di phr gm nd Thor cic C vity The septum tr nsversum is thick pl te of mesoder m l tissue occupying the sp ce between the thor cic c vity nd the st lk of the yolk s c (Fig. 10.4, A nd B). This septum does not sep r te the thor cic nd b domin l c vities completely but le ves l rge openings, the peric rdioperitone l c n ls, on e ch side of the foregut (Fig. 10.4B ). When lung buds begin to grow, they exp nd c udol ter lly within the peric rdioperitone l c n ls (Fig. 10.4C ) . As result of the r pid growth of the lungs, the peric rdioperitone l c n ls become too sm ll, nd the lungs begin to exp nd into the mesenchyme of the body w ll dors lly, l ter lly, nd ventr lly (Fig. 10.4C ). Ventr l nd l ter l exp n sion is posterior to the pleuroperic rdi l folds. At rst these folds ppe r s sm ll ridges projecting into the primitive undivided thor cic c vity (Fig. 10.4C ) . With exp nsion of the lungs, mesoderm of the body w ll splits into two compone nts (Fig. 10.5): ( ) the de nitive w ll of the thor x nd (b) the pleuroperic rdi l membr nes, which re extensions of the pleuroperic rdi l folds th t cont in th e common c rdin l veins nd phrenic nerves. Subsequently, descent of the he rt nd position l ch nges of
Ch pter 10: Body C vities 217
A B Figure 10.5 A. Tr nsform tion of the peric rdioperitone l c n ls into the pleur l c vities nd form tion of the pleuroperic rdi l membr nes. Note the pleuroperi c rdi l folds cont ining the common c rdin l vein nd phrenic nerve. Mesenchyme of the body w ll splits into the pleuroperic rdi l membr nes nd de nitive body w ll. B. The thor x fter fusion of the pleuroperic rdi l folds with e ch other n d with the root of the lungs. Note the position of the phrenic nerve, now in the brous peric rdium. The right common c rdin l vein h s developed into the superio r ven c v .
the sinus venosus shift the common c rdin l veins tow rd the midline, nd the pl europeric rdi l membr nes re dr wn out in mesentery-like f shion (Fig. 10.5A). Fin lly, they fuse with e ch other nd with the root of the lungs, nd the thor cic c vity is divided into the de nitive peric rdi l c vity nd two pleur l c viti es (Fig. 10.5B). In the dult, the pleuroperic rdi l membr nes form the brous per ic rdium. Form tion of the Di phr gm Although the pleur l c vities re sep r te from the p eric rdi l c vity, they rem in in open communic tion with the bdomin l (periton e l) c vity, since the di phr gm is incomplete. During further development, the opening between the prospective pleur l nd peritone l c vities is closed by cre scent-sh ped folds, the pleuroperitone l folds, which project into the c ud l en d of the peric rdioperitone l c n ls (Fig. 10.6A). Gr du lly the folds extend me di lly nd ventr lly so th t by the seventh week they fuse with the mesentery of the esoph gus nd with the septum tr nsversum (Fig. 10.6B). Hence the connectio n between the pleur l nd peritone l portions of the body c vity is closed by th e pleuroperitone l membr nes. Further exp nsion of the pleur l c vities rel tive to mesenchyme of the body w ll dds peripher l rim to the pleuroperitone l me mbr nes (Fig. 10.6C ). Once this rim is est blished, myobl sts
Superior ven c v
P riet l pleur
Pleur l c vity Phrenic nerve
Primitive pleur l c vity P riet l pleur Lung Viscer l pleur m Pleuroperic rdi l membr ne Peric rdi l c vity
Fibrous peric rdiu
218 P rt Two: Speci l Embryology Peric rdioperitone l Pleuroperitone l fold
c n l A B Septum tr nsversum C Muscul r ingrowth from body w ll Septum tr nsversum Figure 10.6 Development of the di phr gm. A. Pleuroperitone l folds ppe r t th e beginning of the fth week. B. Pleuroperitone l folds fuse with the septum tr ns versum nd mesentery of the esoph gus in the seventh week, sep r ting the thor c ic c vity from the bdomin l c vity. C. Tr nsverse section t the fourth month o f development. An ddition l rim derived from the body w ll forms the most perip her l p rt of the di phr gm. origin ting in the body w ll penetr te the membr nes to form the muscul r p rt o f the di phr gm. Thus the di phr gm is derived from the following structures: ( ) the septum tr nsversum, which forms the centr l tendon of the di phr gm; (b) t he two pleuroperitone l membr nes; (c) muscul r components from the l ter l nd dors l body w lls; nd (d) the mesentery of the esoph gus, in which the crur of the di phr gm develop (Fig. 10.6C ). Initi lly the septum tr nsversum lies oppo site cervic l somites, nd nerve components of the third, fourth, nd fth cervic l segments of the spin l cord grow into the septum. At rst the nerves, known s p hrenic nerves, p ss into the septum through the pleuroperic rdi l folds (Fig. 10 .4B). This expl ins why further exp nsion of the lungs nd descent of the septum shift the phrenic nerves th t innerv te the di phr gm into the brous peric rdium (Fig. 10.5). Although the septum tr nsversum lies opposite cervic l segments du ring the fourth week, by the sixth week the developing di phr gm is t the level of thor cic somites. The repositioning of the di phr gm is c used by r pid grow th of the dors l p rt of the embryo (vertebr l column), comp red with th t of th e ventr l p rt. By the beginning of the third month some of the dors l b nds of the di phr gm origin te t the level of the rst lumb r vertebr . The phrenic nerv es supply the di phr gm with its motor nd sensory innerv tion. Since the most p eripher l p rt of the di phr gm is derived from mesenchyme of the thor cic w ll, it is gener lly ccepted th t some of the lower intercost l (thor cic) nerves c ontribute sensory bers to the peripher l p rt of the di phr gm.
Esoph gus mesentery Aort Pleuroperitone l membr ne Esoph gus Inferior ven c v
Ch pter 10: Body C vities CLINICAL CORRELATES 219 Di phr gm tic Herni s A congenit l di phr gm tic herni , one of the more common m lform tions in the newborn (1/2000), is most frequently c used by f ilure of o ne or both of the pleuroperitone l membr nes to close the peric rdioperitone l c n ls. In th t c se the peritone l nd pleur l c vities re continuous with one nother long the posterior body w ll. This herni llows bdomin l viscer to e nter the pleur l c vity. In 85 to 90% of c ses the herni is on the left side, nd intestin l loops, stom ch, spleen, nd p rt of the liver m y enter the thor c ic c vity (Fig. 10.7). The bdomin l viscer in the chest push the he rt nterio rly nd compress the lungs, which re commonly hypopl stic. A l rge defect is s soci ted with high r te of mort lity (75%) from pulmon ry hypopl si nd dysfu nction. Occ sion lly sm ll p rt of the muscul r bers of the di phr gm f ils to develop, nd herni m y rem in undiscovered until the child is sever l ye rs o ld. Such defect, frequently seen in the nterior portion of the di phr gm, is p r stern l herni . A sm ll peritone l s c cont ining intestin l loops m y ent er the chest between the stern l nd cost l portions of the di phr gm (Fig. 10.7 A). Another type of di phr gm tic herni , esoph ge l herni , is thought to be du e to congenit l shortness of the esoph gus. Upper portions of the stom ch re re t ined in the thor x, nd the stom ch is constricted t the level of the di phr gm. SUMMARY At the end of the third week, intercellul r clefts ppe r in the mesoder m on e ch side of the midline. When these sp ces fuse, the intr embryonic c vity (body c vity), bordered by som tic mesoderm nd spl nchnic mesoderm l yer, is formed (Figs. 10.1 nd 10.2). With ceph loc ud l nd l ter l folding of the e mbryo, the intr embryonic c vity extends from the thor cic to the pelvic region. Som tic mesoderm will form the p riet l l yer of the serous membr nes lining th e outside of the peritone l, pleur l, nd peric rdi l c vities. The spl nchnic l yer will form the viscer l l yer of the serous membr nes covering the lungs, he rt, nd bdomin l org ns. These l yers re continuous t the root of these org ns in their c vities ( s if nger were stuck into b lloon, with the l yer surr ounding the nger being the spl nchnic or viscer l l yer nd the rest of the b llo on, the som tic or p riet l l yer surrounding the body c vity). The serous membr nes in the bdomen re c lled peritoneum. The di phr gm divides the body c vity into the thor cic nd peritone l c vities. It develops from four components: ( ) septum tr nsversum (centr l tendon); (b) pleuroperitone l membr nes; (c) dors l mesentery of the esoph gus; nd (d) muscul r components of the body w ll (Fig. 10.6). Congenit l
220 P rt Two: Speci l Embryology Opening between stern l nd cost l he ds Centr l tendon
Colon Aortic hi tus Absence of pleuroperitone l membr ne Di phr gm Stom ch A B
C Figure 10.7 Congenit l di phr gm tic herni . A. Abdomin l surf ce of the di phr gm showing l rge defect of the pleuroperitone l membr ne. B. Herni of the int estin l loops nd p rt of the stom ch into the left pleur l c vity. The he rt n d medi stinum re frequently pushed to the right nd the left lung compressed. C . R diogr ph of newborn with l rge defect in the left side of the di phr gm. Abdomin l viscer h ve entered the thor x through the defect.
Inferior ven c v
Opening for esoph gus Left lung
Ch pter 10: Body C vities 221 di phr gm tic herni s involving defect of the pleuroperitone l membr ne on the left side occur frequently. The thor cic c vity is divided into the peric rdi l c vity nd two pleur l c vities for the lungs by the pleuroperic rdi l membr ne s (Fig. 10.5). Double l yers of peritoneum form mesenteries th t suspend the gut tube nd provide p thw y for vessels, nerves, nd lymph tics to the org ns. I niti lly, the gut tube from the c ud l end of the foregut to the end of the hind gut is suspended from the dors l body w ll by dors l mesentery (Fig. 10.2, C nd E ). Ventr l mesentery derived from the septum tr nsversum exists only in the r egion of the termin l p rt of the esoph gus, the stom ch, nd upper portion of t he duodenum (see Ch pter 13). Problems to Solve 1. A newborn inf nt c nnot bre the nd soon dies. An utopsy r eve ls l rge di phr gm tic defect on the left side, with the stom ch nd intes tines occupying the left side of the thor x. Both lungs re severely hypopl stic . Wh t is the embryologic l b sis for this defect? 2. A child is born with l r ge defect l ter l to the umbilicus. Most of the l rge nd the sm ll bowel protru de through the defect nd re not covered by mnion. Wh t is the embryologic l b sis for this bnorm lity, nd should you be concerned th t other m lform tions m y be present? SUGGESTED READING Cunniff C, Jones KL, Jones MC: P tterns of m lform tions in ch ildren with congenit l di phr gm tic defects. J Pedi tr 116:258, 1990. Puri P, G orm k F: Leth l nonpulmon ry nom lies ssoci ted with congenit l di phr gm tic herni : implic tions for e rly intr uterine surgery. J Pedi tr Surg 35:29, 1984. Sk nd l kis JE, Gr y SW: Embryology for Surgeons: The Embryologic l B sis for t he Tre tment of Congenit l Anom lies. 2nd ed. B ltimore, Willi ms & Wilkins, 199 4.
ch pter 11 C rdiov scul r System Est blishment of the C rdiogenic Field The v scul r system ppe rs in the middle of the third week, when the embryo is no longer ble to s tisfy its nutrition l requirements by diffusion lone. C rdi c progenitor cells lie in the epibl st, immedi tely l ter l to the primitive stre k. From there they migr te through the stre k. Cells destined to form cr ni l segments of the he rt, the out ow tr ct, m igr te rst, nd cells forming more c ud l portions, right ventricle, left ventric le, nd sinus venosus, respectively, migr te in sequenti l order. The cells proc eed tow rd the cr nium nd position themselves rostr l to the buccoph rynge l me mbr ne nd neur l folds (Fig. 11.1). Here they reside in the spl nchnic l yer of the l ter l pl te mesoderm. At this time, l te in the presomite st ge of develo pment, they re induced by the underlying ph rynge l endoderm to form c rdi c my obl sts. Blood isl nds lso ppe r in this mesoderm, where they will form blood cells nd vessels by the process of v sculogenesis (see Ch pter 5; p 103) (Fig. 11.1). With time, the isl nds unite nd form horseshoe-sh ped endotheli l-line d tube surrounded by myobl sts. This region is known s the c rdiogenic eld; the intr embryonic c vity over it l ter develops into the peric rdi l c vity (Fig. 1 1.1D). In ddition to the c rdiogenic region, other blood isl nds ppe r bil ter lly, p r llel nd close to the midline of the embryonic shield. These isl nds f orm p ir of longitudin l vessels, the dors l ort e. 223
224 P rt Two: Speci l Embryology Myobl sts nd blood isl nds Intr embryonic c vity Blood isl nds C rdiogenic field D Figure 11.1 A. Dors l view of l te presomite embryo ( pproxim tely 18 d ys) f ter remov l of the mnion. Prospective myobl sts nd hem ngiobl sts reside in th e spl nchnic mesoderm in front of the neur l pl te nd on e ch side of the embry o. B. Tr nsverse section through simil r-st ged embryo to show the position of the blood isl nds in the spl nchnic mesoderm l yer. C. Ceph loc ud l section th rough simil rst ged embryo showing the position of the peric rdi l c vity nd c rdiogenic eld. D. Sc nning electron microgr ph of mouse embryo equiv lent to 19 d ys in the hum n, showing co lescence of the blood isl nds by v sculogenesis into horseshoesh ped he rt tube ( rrows) lying in the primitive peric rdi l c vity under the cr ni l neur l folds ( sterisks).
Ch pter 11: C rdiov scul r System 225 Form tion nd Position of the He rt Tube Initi lly, the centr l portion of the c rdiogenic re is nterior to the buccoph rynge l membr ne nd the neur l pl te (Fig. 11.2A). With closure of the neur l tube nd form tion of the br in vesicl es, however, the centr l nervous system grows ceph l d so r pidly th t it extend s over the centr l c rdiogenic re nd the future peric rdi l c vity (Fig. 11.2 ). As result of growth of the br in nd ceph lic folding of the embryo, the bu ccoph rynge l membr ne is pulled forw rd, while the he rt nd peric rdi l c vity move rst to the cervic l region nd n lly to the thor x (Fig. 11.2). As the embry o folds ceph loc ud lly, it lso folds l ter lly (Fig. 11.3). As result, the c ud l regions of the p ired c rdi c primordi merge except t their c ud lmost e nds. Simult neously, the crescent p rt of the horseshoe-sh ped re exp nds to f orm the future out ow tr ct nd ventricul r regions. Thus, the he rt becomes con tinuous exp nded tube consisting of n inner endotheli l lining nd n outer myo c rdi l l yer. It receives venous dr in ge t its c ud l pole nd begins to pump blood out of the rst ortic rch into the dors l ort t its cr ni l pole (Figs . 11.4 nd 11.5). The developing he rt tube bulges more nd more into the peric rdi l c vity. Initi lly, however, the tube rem ins tt ched to the dors l side o f the peric rdi l c vity by fold of mesoderm l tissue, the dors l mesoc rdium (Figs. 11.3 nd 11.5). No ventr l mesoc rdium is ever formed. With further devel opment, the dors l mesoc rdium dis ppe rs, cre ting the tr nsverse peric rdi l s inus, which connects both sides of the peric rdi l c vity. The he rt is now susp ended in the c vity by blood vessels t its cr ni l nd c ud l poles (Fig. 11.5) . During these events, the myoc rdium thickens nd secretes thick l yer of ext r cellul r m trix, rich in hy luronic cid, th t sep r tes it from the endotheli um (Figs. 11.3 nd 11.5). In ddition, mesotheli l cells from the region of the sinus venosus migr te over the he rt to form the epic rdium. Thus the he rt tube consists of three l yers: ( ) the endoc rdium, forming the intern l endotheli l lining of the he rt; (b) the myoc rdium, forming the muscul r w ll; nd (c) the epic rdium or viscer l peric rdium, covering the outside of the tube. This oute r l yer is responsible for form tion of the coron ry rteries, including their e ndotheli l lining nd smooth muscle. Form tion of the C rdi c Loop The he rt tube continues to elong te nd bend on d y 23. The ceph lic portion of the tube bends ventr lly, c ud lly, nd to the ri ght (Fig. 11.6, B nd C ), nd the tri l (c ud l) portion shifts dorsocr ni lly nd to the left (Figs. 11.6 nd 11.7A). This bending, which m y be due to cell sh pe ch nges, cre tes the c rdi c loop. It is complete by d y 28. While the c r di c loop is forming, loc l exp nsions become visible throughout the length of t he tube. The tri l portion, initi lly p ired structure outside
226 P rt Two: Speci l Embryology Hindgut Endoderm Amniotic c vity Connecting st lk Foregut He rt tube Ectoderm Blood isl nds All ntois Peric rdi l c vity Buccoph rynge l membr ne A Buccoph rynge l membr ne Clo c l membr ne B Lung bud Liver bud Midgut Clo c l membr ne He rt tube Remn nt of the buccoph rynge l membr ne Vitelline duct All ntois C D Yolk s c Figure 11.2 Figures showing effects of the r pid growth of the br in on position ing of the he rt. Initi lly the c rdiogenic re nd the peric rdi l c vity re in front of the buccoph rynge l membr ne. A. 18 d ys. B. 20 d ys. C. 21 d ys. D. 22 d ys. E. Sc nning electron microgr ph of mouse embryo t st ge simil r t o th t shown in C. The mnion, yolk s c, nd c ud l h lf of the embryo h ve been removed. The he d folds (HF ) re exp nding nd curving over the he rt (H) nd peric rdi l c vity ( sterisk). The intestin l opening ( rrow) of the gut into th e primitive ph rynx nd the endoderm (E ) of the open region of the gut tube re shown.
Ch pter 11: C rdiov scul r System 227
Endoderm A Angiogenic cell clusters B Endoc rdi l tube Neur l crest Foregut Dors l mesoc rdium Myoc rdium Peric rdi l c vity C rdi c jelly Endoc rdi l tube C Figure 11.3 Tr nsverse sections through embryos t different st ges of developme nt, showing form tion of single he rt tube from p ired primordi . A. E rly pre somite embryo (17 d ys). B. L te presomite embryo (18 d ys). C. Eight-somite st ge (22 d ys). Fusion occurs only in the c ud l region of the horseshoe-sh ped tu be (see Fig. 12.4). The out ow tr ct nd most of the ventricul r region form by ex p nsion nd growth of the crescent portion of the horseshoe. the peric rdi l c vity, forms common trium nd is incorpor ted into the peric rdi l c vity (Figs. 11.7A). The trioventricul r junction rem ins n rrow nd fo rms the trioventricul r c n l, which connects the common trium nd the e rly e mbryonic ventricle (Fig. 11.8). The bulbus cordis is n rrow except for its proxi m l third. This portion will form the tr becul ted p rt of the right ventricle ( Figs. 11.7B nd 11.8). The midportion, the conus cordis, will form the out ow tr c ts of both ventricles. The dist l p rt of the bulbus, the truncus rteriosus, wi ll form the roots nd proxim l portion of the ort nd pulmon ry rtery (Fig. 1 1.8). The junction between the ventricle nd the bulbus cordis, extern lly indic ted by the bulboventricul r sulcus (Fig. 11.6C ), rem ins n rrow. It is c lled the prim ry interventricul r for men (Fig. 11.8). Thus, the c rdi c tube is org nized by regions long its cr nioc ud l xis from the conotruncus to the right v entricle to the left ventricle to the tri l region, respectively (Fig. 11.6, A C ). Evidence suggests that organization of these segments is regulated by homeo box genes in a manner similar to that for the craniocaudal axis of the embryo (s ee Chapter 5).
Neur l crest Dors l ort di l cells
Intr embryonic c vity Spl nchnic mesoderm l yer Myoc r
228 Part Two: Special Embryology A B C D Figure 11.4 Formation of the heart tube on days 19, 20, 21, and 22 in scanning e lectron micrographs of mouse embryos at equivalent stages of human development. A. The heart tube (arrows) is horseshoe shaped in the pericardial cavity beneath the neural folds (stars). B. The crescent portion of the horseshoe expands to f orm the ventricular and out ow tract regions, while lateral folding brings the cau dal (venous) poles of the horseshoe together (see Fig. 12.3). C. The caudal regi ons begin to fuse. D. Fusion of the caudal regions is complete, leaving the caud al poles embedded in the septum transversum (arrowheads). Cardiac looping has al so been initiated. Asterisk, pericardial cavity; large arrow, anterior intestina l portal.
Chapter 11: Cardiovascular System 229 Foregut Dorsal aorta Dorsal mesocardium (breaking down) 1st aortic arch Foregut Buccopharyngeal membrane Pericardial cavity Myocardial mantle Endocardial heart tube Figure 11.5 Cephalic end of an early somite embryo. The developing endocardial h eart tube and its investing layer bulge into the pericardial cavity. The dorsal mesocardium is breaking down. At the end of loop formation, the smooth walled heart tube begins to form primit ive trabeculae in two sharply de ned areas just proximal and distal to the primary interventricular foramen (Fig. 11.8). The bulbus temporarily remains smooth wal led. The primitive ventricle, which is now trabeculated, is called the primitive left ventricle. Likewise, the trabeculated proximal third of the bulbus cordis may be called the primitive right ventricle (Fig. 11.8). The conotruncal portion of the heart tube, initially on the right side of the pericardial cavity, shift s gradually to a more medial position. This change in position is the result of formation of two transverse dilations of the atrium, bulging on each side of the bulbus cordis (Figs. 11.7B and 11.8). CLINICAL CORRELATES Abnormalities of Cardiac Looping Dextrocardia, in which the heart lies on the ri ght side of the thorax instead of the left, is caused because the heart loops to the left instead of the right. Dextrocardia may coincide with situs inversus, a complete reversal of asymmetry in all organs. Situs inversus, which occurs in 1 /7000 individuals, usually is associated with normal physiology, although there is a slight risk of heart defects. In other cases sidedness is random, such that some organs are reversed and others are not; this is heterotaxy. These cases ar e classi ed as
230 Part Two: Special Embryology D E Figure 11.6 Formation of the cardiac loop. A. 22 days. B. 23 days. C. 24 days. B roken line, pericardium. D and E. Scanning electron micrographs of mouse embryos showing frontal views of the process shown in the diagrams. Initially the cardi ac tube is short and relatively straight (D), but as it lengthens, it bends (loo ps), bringing the atrial region cranial and dorsal to the ventricular region (E) . The tube is organized in segments, illustrated by the different colors, from t he out ow region to the right ventricle to the left ventricle to the atrial region . These segments represent a craniocaudal axis that appears to be regulated by h omeobox gene expression. A, primitive atrium; arrow, septum transversum; S, sinu s venosus; V, ventricle.
Chapter 11: Cardiovascular System 231 Figure 11.7 Heart of a 5 mm embryo (28 days). A. Viewed from the left. B. Fronta l view. The bulbus cordis is divided into the truncus arteriosus, conus cordis, and trabeculated part of the right ventricle. Broken line, pericardium. C. Scann ing electron micrograph of the heart of a similar staged mouse embryo showing a view similar to B. laterality sequences. Patients with these conditions appear to be predominantly left sided bilaterally or right sided bilaterally. The spleen re ects the differen ces: those with left sided bilaterality have polysplenia; those with rightsided bilaterality have asplenia or hypoplastic spleen. Patients with laterality seque nces also have increased incidences of other malformations, especially heart def ects. Genes regulating sidedness are expressed during gastrulation (see Chapter 4). Molecular Regulation of Cardiac Development Signals from anterior (cranial) endo derm induce a heart forming region in overlying splanchnic mesoderm by turning o n the transcription factor NKX2.5. The
232 Part Two: Special Embryology Figure 11.8 Frontal section through the heart of a 30 day embryo showing the pri mary interventricular foramen and entrance of the atrium into the primitive left ventricle. Note the bulboventricular ange. Arrows, direction of blood ow. signals require secretion of bone morphogenetic proteins (BMPs) 2 and 4 and inhi bitors (crescent) of WNT genes in the endoderm and lateral plate mesoderm (Fig. 11.9). This combination is responsible for inducing expression of NKX2.5 that sp eci es the cardiogenic eld and, later, plays a role in septation and in development of the conduction system. NKX2.5 contains a homeodomain and is a homologue of t he gene tinman, which regulates heart development in Drosophila. TBX5 is another transcription factor that contains a DNA binding motif known as the T box. Expr essed later than NKX2.5, it plays a role in septation. Development of the Sinus Venosus In the middle of the fourth week, the sinus ven osus receives venous blood from the right and left sinus horns (Fig. 11.10A). Ea ch horn receives blood
Chapter 11: Cardiovascular System 233 BMP 2,4 WNT inhibitors (crescent) NKX 2.5 Figure 11.9 Heart induction. BMPs secreted in the posterior portion of the primi tive streak and periphery of the embryo, in combination with inhibition of WNT e xpression by crescent in the anterior half of the embryo, induce expression of N KX2.5 in the heart forming region of the lateral plate mesoderm (splanchnic laye r). NKX2.5 is then responsible for heart induction. from three important veins: (a) the vitelline or omphalomesenteric vein, (b) the umbilical vein, and (c) the common cardinal vein. At rst communication between t he sinus and the atrium is wide. Soon, however, the entrance of the sinus shifts to the right (Fig. 11.10B ). This shift is caused primarily by left to right sh unts of blood, which occur in the venous system during the fourth and fth weeks o f development. With obliteration of the right umbilical vein and the left vitell ine vein during the fth week, the left sinus horn rapidly loses its importance (F ig. 11.10B). When the left common cardinal vein is obliterated at 10 weeks, all that remains of the left sinus horn is the oblique vein of the left atrium and t he coronary sinus (Fig. 11.11). As a result of left to right shunts of blood, th e right sinus horn and veins enlarge greatly. The right horn, which now forms th e only communication between the original sinus venosus and the atrium, is incor porated into the right atrium to form the smooth walled part of the right atrium (Fig. 11.12). Its entrance, the sinuatrial ori ce, is anked on each side by a valv ular fold, the right and left venous valves (Fig. 11.12A). Dorsocranially the va lves fuse, forming a ridge known as the septum spurium (Fig. 11.12A). Initially the valves are large, but when the right sinus horn is incorporated into the wal l of the atrium, the left venous valve and the septum spurium fuse with the deve loping atrial septum (Fig. 11.12C ). The superior portion of the right venous va lve disappears entirely. The inferior portion develops into two parts: (a) the v alve of
234 Part Two: Special Embryology ACV Sinuatrial junction Sinuatrial junction ACV PCV PCV UV VIT V CCV PCV Sinuatrial fold Right vitelline vein Bulbus cordis Common cardinal vein Left sinus horn A Right sinus horn Left sinus horn A Left umbilical vein B Right vitelline vein Left ventricle 24 days 35 days Inferior vena cava Right ventricle Figure 11.10 Dorsal view of two stages in the development of the sinus venosus a t approximately 24 days (A) and 35 days (B). Broken line, the entrance of the si nus venosus into the atrial cavity. Each drawing is accompanied by a scheme to s how in transverse section the great veins and their relation to the atrial cavit y. ACV, anterior cardinal vein; PCV, posterior cardinal vein; UV, umbilical vein ; VIT V, vitelline vein; CCV, common cardinal vein. (See also Fig. 11.41.) Aorta Pulmonary artery Oblique vein of left atrium Oblique vein of left atrium P ulmonary veins Superior vena cava Coronary sinus Inferior vena cava Coronary sinus Figure 11.11 Final stage in development of the sinus venosus and great veins.
Chapter 11: Cardiovascular System 235 Interseptovalvular space Septum spurium Right venous valve Sinuatrial orifice Le ft venous Septum primum Superior vena cava Sinus Pulmonary venarum veins Crista terminalis Septum Septum secundum primum Valve of inferior vena cava Inferior endocardial cushion A C valve Valve of coronary sinus B D Figure 11.12 Ventral view of coronal sections through the heart at the level of the atrioventricular canal to show development of the venous valves. A. 5 weeks. B. Scanning electron micrograph of a similar staged mouse heart showing initial formation of the septum primum; septum spurium is not visible. Note the atriove ntricular canal (arrow). C. Fetal stage. The sinus venarum (blue) is smooth wall ed; it derives from the right sinus horn. Arrows, blood ow. D. High magni cation of the interatrial septum (arrows) of a mouse embryo at a stage similar to C. The foramen ovale is not visible. the inferior vena cava, and (b) the valve of the coronary sinus (Fig. 11.12C ). The crista terminalis forms the dividing line between the original trabeculated part of the right atrium and the smooth walled part (sinus venarum), which origi nates from the right sinus horn (Fig. 11.12C ). Formation of the Cardiac Septa The major septa of the heart are formed between t he 27th and 37th days of development, when the embryo grows in length from 5 mm to approximately 16 to 17 mm. One method by which a septum may be formed involve s two
236 Part Two: Special Embryology Figure 11.13 A ach each other ll mass. D, E, he wall of the and B. Septum formation by until they fuse. C. Septum and F. Septum formation by heart. Such a septum never two actively growing ridges that appro formed by a single actively growing ce merging of two expanding portions of t completely separates two cavities.
actively growing masses of tissue that approach each other until they fuse, divi ding the lumen into two separate canals (Fig. 11.13, A and B ). Such a septum ma y also be formed by active growth of a single tissue mass that continues to expa nd until it reaches the opposite side of the lumen (Fig. 11.13C ). Formation of such tissue masses depends on synthesis and deposition of extracellular matrices and cell proliferation. The masses, known as endocardial cushions, develop in t he atrioventricular and conotruncal regions. In these locations they assist in f ormation of the atrial and ventricular (membranous portion) septa, the atriovent ricular canals and valves, and the aortic and pulmonary channels. The other mann er in which a septum is formed does not involve endocardial cushions. If, for ex ample, a narrow strip of tissue in the wall of the atrium or ventricle should fa il to grow while areas on each side of it expand rapidly, a narrow ridge forms b etween the two expanding portions (Fig. 11.13,D and E ). When growth of the expa nding portions continues on either side of the narrow portion, the two walls app roach each other and eventually merge, forming a septum (Fig. 11.13 F ). Such a septum never completely divides the original lumen but leaves a narrow communica ting canal between the two expanded
Chapter 11: Cardiovascular System 237 sections. It is usually closed secondarily by tissue contributed by neighboring proliferating tissues. Such a septum partially divides the atria and ventricles. CLINICAL CORRELATES Endocardial Cushions and Heart Defects Because of their key location, abnormalit ies in endocardial cushion formation contribute to many cardiac malformations, i ncluding atrial and ventricular septal defects and defects involving the great v essels (i.e., transposition of the great vessels and tetralogy of Fallot). Since cells populating the conotruncal cushions include neural crest cells and since crest cells also contribute extensively to development of the head and neck, abn ormalities in these cells, produced by teratogenic agents or genetic causes, oft en produce both heart and craniofacial defects in the same individual. SEPTUM FO RMATION IN THE COMMON ATRIUM At the end of the fourth week, a sickle shaped cres t grows from the roof of the common atrium into the lumen. This crest is the rst portion of the septum primum (Figs. 11.12 A and 11.14, A and B). The two limbs o f this septum extend toward the endocardial cushions in the atrioventricular can al. The opening between the lower rim of the septum primum and the endocardial c ushions is the ostium primum (Fig. 11.14, A and B). With further development, ex tensions of the superior and inferior endocardial cushions grow along the edge o f the septum primum, closing the ostium primum (Fig. 11.14, C and D). Before clo sure is complete, however, cell death produces perforations in the upper portion of the septum primum. Coalescence of these perforations forms the ostium secund um, ensuring free blood ow from the right to the left primitive atrium (Fig. 11.1 4, B and D). When the lumen of the right atrium expands as a result of incorpora tion of the sinus horn, a new crescent shaped fold appears. This new fold, the s eptum secundum (Fig. 11.14, C and D), never forms a complete partition in the at rial cavity (Fig. 11.14G ). Its anterior limb extends downward to the septum in the atrioventricular canal. When the left venous valve and the septum spurium fu se with the right side of the septum secundum, the free concave edge of the sept um secundum begins to overlap the ostium secundum (Fig. 11.12, A and B). The ope ning left by the septum secundum is called the oval foramen (foramen ovale). Whe n the upper part of the septum primum gradually disappears, the remaining part b ecomes the valve of the oval foramen. The passage between the two atrial cavitie s consists of an obliquely elongated cleft (Fig. 11.14, E G ) through which blood from the right atrium ows to the left side (arrows in Figs. 11.12B and 11.14E ). After birth, when lung circulation begins and pressure in the left atrium incre ases, the valve of the oval foramen is pressed against the septum secundum,
238 Part Two: Special Embryology Ostium primum Septum primum Septum primum Ostium primum A Endocardial cushion B Atrioventricular canal Ostium secundum Septum primum Interventricular foramen Septum secundum Ostium secundum Endocardial cushions fu sed Septum secundum Septum primum Endocardial cushion Venous valves Interventricular foramen C Septum primum Septum secundum D Pulmonary vein Superior vena cava Valve of oval foramen Oval foramen Septum secundum Valve of inferior vena cava E F G Valve of coronary sinus Figure 11.14 Atrial septa . Same stage as A, viewed viewed from the right E. the right; same stage as at various stages of development. A. 30 days (6 mm). B from the right. C. 33 days (9 mm). D. Same stage as C, 37 days (14 mm). F. Newborn. G. The atrial septum from F.
obliterating the oval foramen and separating the right and left atria. In about 20% of cases, fusion of the septum primum and septum secundum is incomplete, and a narrow oblique cleft remains between the two atria. This condition is called probe patency of the oval foramen; it does not allow intracardiac shunting of bl ood. Further Differentiation of the Atria While the primitive right atrium enlar ges by incorporation of the right sinus horn, the primitive left atrium is likew ise expanding. Initially, a single embryonic pulmonary vein develops as an outgr
owth of the posterior left atrial wall, just to the left of the septum primum (F ig. 11.15A). This vein gains connection with
Chapter 11: Cardiovascular System 239 Septum Interseptovalvular space primum Septum spurium Right venous valve Sinuatr ial orifice Left venous valve A Superior vena cava Septum Sinus Pulmonary secundum venarum veins Crista terminal is Septum primum B Figure 11.15 Coronal sections hwalled portions of the right horn (blue) and the pulmonary rm the smooth walled parts of through the heart to show development of the smoot and left atrium. Both the wall of the right sinus veins (red ) are incorporated into the heart to fo the atria.
veins of the developing lung buds. During further development, the pulmonary vei n and its branches are incorporated into the left atrium, forming the large smoo th walled part of the adult atrium. Although initially one vein enters the left atrium, ultimately four pulmonary veins enter (Fig. 11.15B ) as the branches are incorporated into the expanding atrial wall. In the fully developed heart, the original embryonic left atrium is represented by little more than the trabeculat ed atrial appendage, while the smooth walled part originates from the pulmonary veins (Fig. 11.15). On the right side the original embryonic right atrium become s the trabeculated right atrial appendage containing the pectinate muscles, and the smooth walled sinus venarum originates from the right horn of the sinus veno sus. SEPTUM FORMATION IN THE ATRIOVENTRICULAR CANAL At the end of the fourth wee k, two mesenchymal cushions, the atrioventricular endocardial cushions, appear a t the superior and inferior borders of the atrioventricular canal (Figs. 11.16 a nd 11.17). Initially the atrioventricular canal gives access only to the primiti ve left ventricle and is separated from the bulbus cordis by the bulbo(cono)vent ricular ange (Fig. 11.8). Near the end of the fth week, however, the posterior ext remity of the ange terminates almost midway along the base of the superior endoca rdial cushion and is much less prominent than before (Fig. 11.17). Since the atr ioventricular canal enlarges to the right, blood passing through the atrioventri cular ori ce now has direct access to the primitive left as well as the primitive right ventricle. In addition to the superior and inferior endocardial cushions, the two lateral atrioventricular cushions appear on the right and left borders o f the canal (Figs. 11.16 and 11.17). The superior and inferior cushions, in the meantime, project further into the lumen and fuse, resulting in a complete divis ion of the canal into right and left atrioventricular ori ces by the end of the fth week (Fig. 11.16).
240 Part Two: Special Embryology Common atrioventricular canal Superior endocardial cushion Right atrioventricular canal A Lateral cushion Inferior endocardial cushion Left atrioventricular canal cushion B C Figure 11.16 Formation of the septum in the atrioventricular canal. A. From left to right, days 23, 26, 31, and 35. The initial circular opening widens transver sely. B and C. Scanning electron micrographs of hearts from mouse embryos, showi ng growth and fusion of the superior and inferior endocardial cushions in the at rioventricular canal. In C, cushions of the ou ow tract (arrow) are also fusing.
Chapter 11: Cardiovascular System 241 Pulmonary channel Right superior truncus swelling Aortic sac IV Aortic arches II I IV VI Aortic channel Left inferior truncus swelling Right dorsal conus swelling Left ventral conus swelling Bulboventricular flange Left lateral cushion A Right lateral cushion Interventricular septum Inferior endocardial cushion B Figure 11.17 A. Frontal section through the heart of a day 35 embryo. At this st age of development blood from the atrial cavity enters the primitive left ventri cle as well as the primitive right ventricle. Note development of the cushions i n the atrioventricular canal. Cushions in the truncus and conus are also visible . Ring, primitive interventricular foramen. Arrows, blood ow. B. Scanning electro n micrograph of a mouse embryo at a slightly later stage showing fusion of the a trioventricular cushions and contact between those in the out ow tract.
242 Part Two: Special Embryology Figure 11.18 Formation of the atrioventricular valves and chordae tendineae. The valves are hollowed out from the ventricular side but remain attached to the ve ntricular wall by the chordae tendineae. Atrioventricular Valves After the atrioventricular endocardial cushions fuse, ea ch atrioventricular ori ce is surrounded by local proliferations of mesenchymal ti ssue (Fig. 11.18A). When the bloodstream hollows out and thins tissue on the ven tricular surface of these proliferations, valves form and remain attached to the ventricular wall by muscular cords (Fig. 11.18B ). Finally, muscular tissue in the cords degenerates and is replaced by dense connective tissue. The valves the n consist of connective tissue covered by endocardium. They are connected to thi ck trabeculae in the wall of the ventricle, the papillary muscles, by means of c hordae tendineae (Fig.11.18C ). In this manner two valve lea ets, constituting the bicuspid, or mitral, valve, form in the left atrioventricular canal, and three, constituting the tricuspid valve, form on the right side. CLINICAL CORRELATES Heart Defects Heart and vascular abnormalities make up the largest category of h uman birth defects, accounting for 1% of malformations among live born infants. The incidence among stillborns is 10 times as high. It is estimated that 8% of c ardiac malformations are due to genetic factors, 2% are due to environmental age nts, and most are due to a complex interplay between genetic and environmental i n uences (multifactorial causes). Classic examples of cardiovacular teratogens inc lude rubella virus and thalidomide. Others include isotretinoin (vitamin A), alc ohol, and many other compounds. Maternal diseases, such as insulin dependent dia betes and hypertension, have also been linked to cardiac defects. Chromosomal ab normalities are associated with heart malformations, with 6 to 10% of newborns w ith cardiac defects having an unbalanced chromosomal abnormality. Furthermore, 3 3% of children
Chapter 11: Cardiovascular System 243 with chromosomal abnormalities have a congenital heart defect, with an incidence of nearly 100% in children with trisomy 18. Finally, cardiac malformations are associated with a number of genetic syndromes, including craniofacial abnormalit ies, such as DiGeorge, Goldenhar, and Down syndromes (see Chapter 15). Genes reg ulating cardiac development are being identi ed and mapped and mutations that resu lt in heart defects are being discovered. For example, mutations in the heart sp ecifying gene NKX2.5, on chromosome 5q35, produce atrial septal defects (secundu m type) and atrioventricular conduction delays in an autosomal dominant fashion. Mutations in the TBX5 gene result in Holt Oram syndrome, characterized by preax ial (radial) limb abnormalities and atrial septal defects. Defects in the muscul ar portion of the interventricular septum may also occur. Holt Oram syndrome is one of a group of heart hand syndromes illustrating that the same genes may part icipate in multiple developmental processes. For example, TBX5 is expressed in d istal segments of the limb bud and in the heart primordia. Holt Oram syndrome is inherited as an autosomal dominant trait with a frequency of 1/100,000 live bir ths. Atrial septal defect (ASD) is a congenital heart abnormality with an incide nce of 6.4/10,000 births and with a 2:1 prevalence in female versus male infants . One of the most signi cant defects is the ostium secundum defect, characterized by a large opening between the left and right atria. It is caused either by exce ssive cell death and resorption of the septum primum (Fig. 11.19, B and C ) or b y inadequate development of the septum secundum (Fig. 11.19, D and E ). Dependin g on the size of the opening, considerable intracardiac shunting may occur from left to right. The most serious abnormality in this group is complete absence of the atrial septum (Fig. 11.19F ). This condition, known as common atrium or cor triloculare biventriculare, is always associated with serious defects elsewhere in the heart. Occasionally, the oval foramen closes during prenatal life. This abnormality, premature closure of the oval foramen, leads to massive hypertrophy of the right atrium and ventricle and underdevelopment of the left side of the heart. Death usually occurs shortly after birth. Endocardial cushions of the atr ioventricular canal not only divide this canal into a right and left ori ce, but a lso participate in formation of the membranous portion of the interventricular s eptum and in closure of the ostium primum. This region has the appearance of a c ross, with the atrial and ventricular septa forming the post and the atrioventri cular cushions the crossbar. The integrity of this cross is an important sign in ultrasound scans of the heart (Fig. 11.29C ). Whenever the cushions fail to fus e, the result is a persistent atrioventricular canal, combined with a defect in the cardiac septum (Fig.11.20A). This septal defect has an atrial and a ventricu lar
244 Part Two: Special Embryology Septum secundum Septum secundum Septum primum Pulmonary veins Septum secundum Pu lmonary veins Large oval foramen A Normal septum formation B Excessive resorption of septum primum Short septum primum C Atrial septal defect Septum primum D Absence of septum secundum E Septum primum F Absence of septum primum and septum secundum Figure 11.19 A. Normal atrial septum formation. B and C. Ostium secundum defect caused by excessive resorption of the septum primum. D and E. Similar defect cau sed by failure of development of the septum secundum. F. Common atrium, or cor t riloculare biventriculare, resulting from complete failure of the septum primum and septum secundum to form. component, separated by abnormal valve lea ets in the single atrioventricular ori ce (Fig.11.20C ). Occasionally, endocardial cushions in the atrioventricular canal partially fuse. The result is a defect in the atrial septum, but the interventr icular septum is closed (Fig. 11.20, D and E ). This defect, the ostium primum d efect, is usually combined with a cleft in the anterior lea et of the tricuspid va lve (Fig. 11.20C ). Tricuspid atresia, which involves obliteration of the right atrioventricular ori ce (Fig. 11.21B ), is characterized by the absence or fusion of the tricuspid valves. Tricuspid atresia is always associated with (a) patency of the oval foramen, (b) ventricular septal defect, (c) underdevelopment of the right ventricle, and (d) hypertrophy of the left ventricle. SEPTUM FORMATION IN THE TRUNCUS ARTERIOSUS AND CONUS CORDIS During the fth week, pairs of opposing r idges appear in the truncus. These ridges, the truncus swellings, or cushions, l ie on the right superior wall (right
Chapter 11: Cardiovascular System 245 Figure 11.20 A. Persistent common atrioventricular canal. This abnormality is al ways accompanied by a septum defect in the atrial as well as in the ventricular portion of the cardiac partitions. B. Valves in the atrioventricular ori ces under normal conditions. C. Split valves in a persistent atrioventricular canal. D an d E. Ostium primum defect caused by incomplete fusion of the atrioventricular en docardial cushions. superior truncus swelling) and on the left inferior wall (left inferior truncus swelling) (Fig. 11.17). The right superior truncus swelling grows distally and t o the left, and the left inferior truncus swelling grows distally and to the rig ht. Hence, while growing toward the aortic sac, the swellings twist around each other, foreshadowing the spiral course of the future septum (Figs. 11.22 and 11. 23). After complete fusion, the ridges form the aorticopulmonary septum, dividin g the truncus into an aortic and a pulmonary channel.
246 Part Two: Special Embryology Figure 11.21 A. Normal heart. B. Tricuspid atresia. Note the small right ventric le and the large left ventricle. When the truncus swellings appear, similar swellings (cushions) develop along th e right dorsal and left ventral walls of the conus cordis (Figs. 11.17 and 11.23 ). The conus swellings grow toward each other and distally to unite with the tru ncus septum. When the two conus swellings have fused, the septum divides the con us into an anterolateral portion (the ou ow tract of the right ventricle) (Fig. 11 .24) and a posteromedial portion (the out ow tract of the left ventricle) (Fig. 11 .25). Neural crest cells, migrating from the edges of the neural folds in the hi ndbrain region, contribute to endocardial cushion formation in both the conus co rdis and truncus arteriosus. Abnormal migration, proliferation, or differentiati on of these cells results in congenital malformations in this region, such as te tralogy of Fallot (Fig 11.29), pulmonary stenoses, transposition of the great ve ssels and persistent truncus arteriosus (Fig 11.30). Since neural crest cells al so contribute to craniofacial development, it is not uncommon to see facial and cardiac abnormalities in the same individual. SEPTUM FORMATION IN THE VENTRICLES By the end of the fourth week, the two primitive ventricles begin to expand. Th is is accomplished by continuous growth of the myocardium on the outside and con tinuous diverticulation and trabecula formation on the inside (Figs. 11.8, 11.17 , and 11.25). The medial walls of the expanding ventricles become apposed and gr adually merge, forming the muscular interventricular septum (Fig. 11.25). Someti mes the two walls do not merge completely, and a more or less deep apical cleft between the two ventricles appears. The space between the free rim of
A B A P C Figure 11.22 Scanning electron micrographs of hearts from mouse embryos showing formation of the conotruncal ridges (cushions) that form a septum in the out ow tr act to divide this region into aortic and pulmonary channels. A. Frontal section showing cushion contact (arrows) in the out ow tract. B. Cross section through th e atrioventricular canal (arrowheads) and out ow tract (arrow). Cushions in both r egions have made initial contact. C. Cross section through the aortic (A) and pu lmonary (P) vessels showing their entwined course caused by spiraling of the con otruncal ridges (see Fig. 11.23). Note the thickness of the aorta.
248 Part Two: Special Embryology Right conotruncal ridge Left conotruncal ridge Conotruncal septum Left atrioventricular orifice Right atrium Right atrioventricular orifice Proliferation of inferior atrioventricular cushion Muscular part of the interven tricular septum Pulmonary channel A B Aortic channel Muscular part of the interventricular septum Membranous part of the interventricular septum C Figure 11.23 Development of the conotruncal ridges (cushions) and closure of the interventricular foramen. Proliferations of the right and left conus cushions, combined with proliferation of the inferior endocardial cushion, close the inter ventricular foramen and form the membranous portion of the interventricular sept um. A. 6 weeks (12 mm). B. Beginning of the seventh week (14.5 mm). C. End of th e seventh week (20 mm). the muscular ventricular septum and the fused endocardial cushions permits commu nication between the two ventricles. The interventricular foramen, above the mus cular portion of the interventricular septum, shrinks on completion of the conus septum (Fig. 11.23). During further development, outgrowth of tissue from the i nferior endocardial cushion along the top of the muscular interventricular septu m closes the foramen (Fig. 11.23). This tissue fuses with the abutting parts of the conus septum. Complete closure of the interventricular foramen forms the mem branous part of the interventricular septum.
Chapter 11: Cardiovascular System 249 Figure 11.24 Frontal section through the heart of a 7 week embryo. Note the conu s septum and position of the pulmonary valves. Semilunar Valves When partitioning of the truncus is almost complete, primordia of the semilunar valves become visible as small tubercles found on the main trun cus swellings. One of each pair is assigned to the pulmonary and aortic channels , respectively (Fig. 11.26). A third tubercle appears in both channels opposite the fused truncus swellings. Gradually the tubercles hollow out at their upper s urface, forming the semilunar valves (Fig. 11.27). Recent evidence shows that ne ural crest cells contribute to formation of these valves. CLINICAL CORRELATES Heart Defects Ventricular septal defect (VSD) involving the membranous portion o f the septum (Fig. 11.28) is the most common congenital cardiac malformation, oc curring as an isolated condition in 12/10,000 births. Although it may be found a s an isolated lesion, VSD is often associated with abnormalities in partitioning of the conotruncal region. Depending on the size of the opening, blood carried
250 Part Two: Special Embryology Figure 11.25 Frontal section through the heart of an embryo at the end of the se venth week. The conus septum is complete, and blood from the left ventricle ente rs the aorta. Note the septum in the atrial region. Figure 11.26 Transverse sections through the truncus arteriosus at the level of the semilunar valves at 5 (A), 6 (B), and 7 (C) weeks of development. by the pulmonary artery may be 1.2 to 1.7 times as abundant as that carried by t he aorta. Occasionally the defect is not restricted to the membranous part but a lso involves the muscular part of the septum. Tetralogy of Fallot, the most freq uently occurring abnormality of the conotruncal region (Fig. 11.29), is due to a n unequal division of the conus resulting from anterior displacement of the cono truncal septum. Displacement of the septum produces four cardiovascular alterati ons: (a) a narrow right
Chapter 11: Cardiovascular System 251 Figure 11.27 Longitudinal sections through the semilunar valves at the sixth (A) , seventh (B), and ninth (C) weeks of development. The upper surface is hollowed (arrows) to form the valves. Figure 11.28 A. Normal heart. B. Isolated defect in the membranous portion of th e interventricular septum. Blood from the left ventricle ows to the right through the interventricular foramen (arrows). ventricular out ow region, a pulmonary infundibular stenosis; (b) a large defect o f the interventricular septum; (c) an overriding aorta that arises directly abov e the septal defect; and (d) hypertrophy of the right ventricular wall because o f higher pressure on the right side. Tetralogy of Fallot, which is not fatal, oc curs in 9.6/10,000 births. Persistent truncus arteriosus results when the conotr uncal ridges fail to fuse and to descend toward the ventricles (Fig. 11.30). In such a case, which occurs in 0.8/10,000 births, the pulmonary artery arises some distance above the origin of the undivided truncus. Since the ridges also parti cipate in formation of the interventricular septum, the persistent truncus is al ways accompanied by a defective interventricular septum. The undivided truncus t hus overrides both ventricles and receives blood from both sides. Transposition of the great vessels occurs when the conotruncal septum fails to follow its norm al spiral course and runs straight down (Fig. 11.31A). As a consequence, the aor ta originates from the right ventricle, and the
252 Part Two: Special Embryology Superior vena cava Large aortic stem Patent ductus arteriosus Right coronary artery Pulmonary stenosis Narrow pulmona ry trunk Left coronary artery Overriding aorta A B Hypertrophy Interventricular septal defect Figure 11.29 Tetralogy of Fallot. A. Surface view. B. The four components of the defect: pulmonary stenosis, overriding aorta, interventricular septal defect, a nd hypertrophy of the right ventricle. C. Ultrasound scan showing a normal heart with atria (asterisks), ventricles (V), and interventricular septum (arrow). D. Scan of a heart showing the characteristic features of the tetralogy, including hypertrophy of the right ventricle (R) and overriding aorta (arrow). A, atrium; L, left ventricle. pulmonary artery originates from the left ventricle. This condition, which occur s in 4.8/10,000 births, sometimes is associated with a defect in the membranous part of the interventricular septum. It is usually accompanied by an open ductus arteriosus. Since neural crest cells contribute to the formation of the truncal cushions, insults to these cells contribute to cardiac defects involving the ou t ow tract.
Chapter 11: Cardiovascular System 253 Superior vena cava Aorta Pulmonary trunk Aorta Persistent truncus arteriosus Pulmonary artery Truncus arteriosus Interventricular septal defect A B Figure 11.30 Persistent truncus arteriosus. The pulmonary artery originates from a common truncus (A). The septum in the truncus and conus has failed to form (B ). This abnormality is always accompanied by an interventricular septal defect. Figure 11.31 A. Transposition of the great vessels. B. Pulmonary valvular atresi a with a normal aortic root. The only access route to the lungs is by way of a p atent ductus arteriosus. Valvular stenosis of the pulmonary artery or aorta occurs when the semilunar val ves are fused for a variable distance. The incidence of the abnormality is simil ar for both regions, being approximately 3 to 4 per 10,000 births. In the case o f a valvular stenosis of the pulmonary artery, the trunk of the pulmonary artery is narrow or even atretic (Fig. 11.31B). The patent oval foramen then forms the only outlet for blood from the right side of the
254 Part Two: Special Embryology Patent ductus arteriosus Patent oval foramen Stenosis of aortic valves Atresia of aortic valves A B Figure 11.32 A. Aortic valvular stenosis. B. Aortic valvular atresia. Arrow in t he arch of the aorta indicates direction of blood ow. The coronary arteries are s upplied by this retro ux. Note the small left ventricle and the large right ventri cle. heart. The ductus arteriosus, always patent, is the only access route to the pul monary circulation. In aortic valvular stenosis (Fig. 11.32), fusion of the thic kened valves may be so complete that only a pinhole opening remains. The size of the aorta itself is usually normal. When fusion of the semilunar aortic valves is completeaortic valvular atresia (Fig. 11.32B)the aorta, left ventricle, and lef t atrium are markedly underdeveloped. The abnormality is usually accompanied by an open ductus arteriosus, which delivers blood into the aorta. Ectopia cordis i s a rare anomaly in which the heart lies on the surface of the chest. It is caus ed by failure of the embryo to close the ventral body wall (see Chapter 10). Formation of the Conducting System of the Heart Initially the pacemaker for the heart lies in the caudal part of the left cardiac tube. Later the sinus venosus assumes this function, and as the sinus is incorporated into the right atrium, p acemaker tissue lies near the opening of the superior vena cava. Thus, the sinua trial node is formed. The atrioventricular node and bundle (bundle of His) are d erived from two sources: (a) cells in the left wall of the sinus venosus, and (b ) cells from the atrioventricular canal. Once the sinus venosus is incorporated into the right atrium, these cells lie in their nal position at the base of the i nteratrial septum.
Chapter 11: Cardiovascular System 255 Vascular Development ARTERIAL SYSTEM Aortic Arches When pharyngeal arches form d uring the fourth and fth weeks of development, each arch receives its own cranial nerve and its own artery (see Chapter 15). These arteries, the aortic arches, a rise from the aortic sac, the most distal part of the truncus arteriosus (Figs. 11.8 and 11.33). The aortic arches are embedded in mesenchyme of the pharyngeal arches and terminate in the right and left dorsal aortae. (In the region of the arches the dorsal aortae remain paired, but caudal to this region they fuse to f orm a single vessel.) The pharyngeal arches and their vessels appear in a crania l to caudal sequence, so that they are not all present simultaneously. The aorti c sac contributes a branch to each new arch as it forms, giving rise to a total of ve pairs of arteries. (The fth arch either never forms or forms incompletely an d then regresses. Consequently the ve arches are numbered I, II, III, IV, and VI [Fig. 11.34].) During further development, this arterial pattern becomes modi ed, and some vessels regress completely. Division of the truncus arteriosus by the a orticopulmonary septum divides the out ow channel of the heart into the ventral ao rta and the pulmonary artery. The aortic sac then forms right and left horns, wh ich subsequently give rise to the brachiocephalic artery and the proximal segmen t of the aortic arch, respectively (Fig. 11.35, B and C ). By day 27, most of th e rst aortic arch has disappeared (Fig. 11.34), although a small portion persists to form the maxillary artery. Similarly, the Anterior cardinal vein Aortic arches (II and III) Internal carotid artery Common cardinal vein Dorsal aorta Posterior cardinal vein Chorionic villus Heart Aortic sac Vitelline vein Umbilical vein and artery Vitelline artery Chorion Figure 11.33 Main intraembryonic and extraembryonic arteries (red ) and veins (b lue) in a 4 mm embryo (end of the fourth week). Only the vessels on the left sid e of the embryo are shown.
256 Part Two: Special Embryology Obliterated aortic arch I I Maxillary artery II III IV Aortic sac IV Primitive p ulmonary artery Left dorsal aorta III IV VI Ascending aorta Septum between aorta and pulmonary artery Pulmonary trunk Right dorsal aorta Primitive pulmonary artery A 4 mm stage B Left 7th intersegmental artery 10 mm stage Figure 11.34 A. Aortic arches at the end of the fourth week. The rst arch is obli terated before the sixth is formed. B. Aortic arch system at the beginning of th e sixth week. Note the aorticopulmonary septum and the large pulmonary arteries. second aortic arch soon disappears. The remaining portions of this arch are the hyoid and stapedial arteries. The third arch is large; the fourth and sixth arch es are in the process of formation. Even though the sixth arch is not completed, the primitive pulmonary artery is already present as a major branch (Fig. 11.34 A). In a 29 day embryo, the rst and second aortic arches have disappeared (Fig. 1 1.34B ). The third, fourth, and sixth arches are large. The truncoaortic sac has divided so that the sixth arches are now continuous with the pulmonary trunk. W ith further development, the aortic arch system loses its original symmetrical f orm, as shown in Figure 11.35A, and establishes the de nitive pattern illustrated in Figure 11.35, B and C . This representation may clarify the transformation fr om the embryonic to the adult arterial system. The following changes occur: The third aortic arch forms the common carotid artery and the rst part of the interna l carotid artery. The remainder of the internal carotid is formed by the cranial portion of the dorsal aorta. The external carotid artery is a sprout of the thi rd aortic arch. The fourth aortic arch persists on both sides, but its ultimate fate is different on the right and left sides. On the left it forms part of the arch of the aorta, between the left common carotid and the left subclavian arter ies. On the right it forms the most proximal segment of the right subclavian art ery, the distal part of which is formed by a portion of the right dorsal aorta a nd the seventh intersegmental artery (Fig. 11.35B).
Chapter 11: Cardiovascular System 257 Dorsal aorta Aortic arches I II III IV V VI Right dorsal aorta Internal carotid artery Right vagus nerve External carotid arteries Left vagus nerve Arch of aorta Left recurrent nerve Ductus arteriosus Pulmonary artery Common carotid artery Right subclavian artery Right recurrent nerve 7th interseg mental artery Right external carotid artery Right vagus Right subclavian artery Brachiocephali c artery Ascending aorta Left internal carotid artery Left common carotid artery Left subclavian artery Ligamentum arteriosum Pulmonary artery Descending aorta Figure 11.35 A. Aortic arches and dorsal aortae before transformation into the d e nitive vascular pattern. B. Aortic arches and dorsal aortae after the transforma tion. Broken lines, obliterated components. Note the patent ductus arteriosus an d position of the seventh intersegmental artery on the left. C. The great arteri es in the adult. Compare the distance between the place of origin of the left co mmon carotid artery and the left subclavian in B and C. After disappearance of t he distal part of the sixth aortic arch (the fth arches never form completely), t he right recurrent laryngeal nerve hooks around the right subclavian artery. On the left the nerve remains in place and hooks around the ligamentum arteriosum. The fth aortic arch either never forms or forms incompletely and then regresses. The sixth aortic arch, also known as the pulmonary arch, gives off an important branch that grows toward the developing lung bud (Fig. 11.34B). On the right sid e the proximal part becomes the proximal segment of the right pulmonary artery. The distal portion of this arch loses its connection
258 Part Two: Special Embryology Figure 11.36 Changes from the original aortic arch system. with the dorsal aorta and disappears. On the left the distal part persists durin g intrauterine life as the ductus arteriosus. A number of other changes occur al ong with alterations in the aortic arch system: (a) The dorsal aorta between the entrance of the third and fourth arches, known as the carotid duct, is oblitera ted (Fig. 11.36). (b) The right dorsal aorta disappears between the origin of th e seventh intersegmental artery and the junction with the left dorsal aorta (Fig . 11.36). (c) Cephalic folding, growth of the forebrain, and elongation of the n eck push the heart into the thoracic cavity. Hence the carotid and brachiocephal ic arteries elongate considerably (Fig. 11.35C ). As a further result of this ca udal shift, the left subclavian artery, distally xed in the arm bud, shifts its p oint of origin from the aorta at the level of the seventh intersegmental artery (Fig. 11.35B) to an increasingly higher point until it comes close to the origin of the left common carotid artery (Fig. 11.35C ). (d) As a result of the caudal shift of the heart and the disappearance of various portions of the aortic arch es, the course of the recurrent laryngeal nerves becomes different on the right and left sides. Initially these nerves, branches of the vagus, supply the sixth pharyngeal arches. When the heart descends, they hook around the sixth aortic ar ches and ascend again to the larynx, which accounts for their recurrent course. On the right, when the distal part of the sixth aortic arch and the fth aortic ar ch disappear, the
Chapter 11: Cardiovascular System 259 recurrent laryngeal nerve moves up and hooks around the right subclavian artery. On the left the nerve does not move up, since the distal part of the sixth aort ic arch persists as the ductus arteriosus, which later forms the ligamentum arte riosum (Fig. 11.35). Vitelline and Umbilical Arteries The vitelline arteries, initially a number of p aired vessels supplying the yolk sac (Fig. 11.33), gradually fuse and form the a rteries in the dorsal mesentery of the gut. In the adult they are represented by the celiac, superior mesenteric, and inferior mesenteric arteries. These vessel s supply derivatives of the foregut, midgut, and hindgut, respectively. The umbi lical arteries, initially paired ventral branches of the dorsal aorta, course to the placenta in close association with the allantois (Fig. 11.33). During the f ourth week, however, each artery acquires a secondary connection with the dorsal branch of the aorta, the common iliac artery, and loses its earliest origin. Af ter birth the proximal portions of the umbilical arteries persist as the interna l iliac and superior vesical arteries, and the distal parts are obliterated to f orm the medial umbilical ligaments. CLINICAL CORRELATES Arterial System Defects Under normal conditions the ductus arteriosus is functio nally closed through contraction of its muscular wall shortly after birth to for m the ligamentum arteriosum. Anatomical closure by means of intima proliferation takes 1 to 3 months. A patent ductus arteriosus, one of the most frequently occ urring abnormalities of the great vessels (8/10,000 births), especially in prema ture infants, either may be an isolated abnormality or may accompany other heart defects (Figs. 11.29A and 11.31). In particular, defects that cause large diffe rences between aortic and pulmonary pressures may cause increased blood ow throug h the ductus, preventing its normal closure. In coarctation of the aorta (Fig. 1 1.37, A and B ), which occurs in 3.2/10,000 births, the aortic lumen below the o rigin of the left subclavian artery is signi cantly narrowed. Since the constricti on may be above or below the entrance of the ductus arteriosus, two types, predu ctal and postductal, may be distinguished. The cause of aortic narrowing is prim arily an abnormality in the media of the aorta, followed by intima proliferation s. In the preductal type the ductus arteriosus persists, whereas in the postduct al type, which is more common, this channel is usually obliterated. In the latte r case collateral circulation between the proximal and distal parts of the aorta is established by way of large intercostal and internal thoracic arteries. In t his manner the lower part of the body is supplied with blood.
260 Part Two: Special Embryology Common carotid arteries Patent ductus arteriosus Pulmonary artery Ligamentum arteriosum A B Figure 11.37 Coarctation of the aorta. A. Preductal type. B. Postductal type. Th e caudal part of the body is supplied by large hypertrophied intercostal and int ernal thoracic arteries. Trachea Common carotid arteries Abnormal obliteration 7th intersegmental artery Right dorsal aorta (abnormal right subclavian artery) Ascending aorta Esophagus Left subclavian artery Right subclavian artery (dysphagia lusoria) Des cending aorta A B Figure 11.38 Abnormal origin of the right subclavian artery. A. Obliteration of the right fourth aortic arch and the proximal portion of the right dorsal aorta with persistence of the distal portion of the right dorsal aorta. B. The abnorma l right subclavian artery crosses the midline behind the esophagus and may compr ess it. Abnormal origin of the right subclavian artery (Fig. 11.38, A and B ) occurs whe n the artery is formed by the distal portion of the right dorsal aorta and the s eventh intersegmental artery. The right fourth aortic arch and the proximal part of the right dorsal aorta are obliterated. With shortening of the aorta between the left common carotid and left subclavian arteries, the origin of the abnorma l right subclavian artery nally settles just below that of the left subclavian ar tery. Since its stem is derived from the right dorsal aorta,
Chapter 11: Cardiovascular System 261 Trachea Common carotid arteries Right aortic arch Esophagus Left subclavian artery Left aortic arch Persistent portion of right dorsal aorta Ascending aorta Descending aorta A B Figure 11.39 Double aortic arch. A. Persistence of the distal portion of the rig ht dorsal aorta. B. The double aortic arch forms a vascular ring around the trac hea and esophagus. it must cross the midline behind the esophagus to reach the right arm. This loca tion does not usually cause problems with swallowing or breathing, since neither the esophagus nor the trachea is severely compressed. With a double aortic arch the right dorsal aorta persists between the origin of the seventh intersegmenta l artery and its junction with the left dorsal aorta (Fig. 11.39) A vascular rin g surrounds the trachea and esophagus and commonly compresses these structures, causing dif culties in breathing and swallowing. In a right aortic arch, the left fourth arch and left dorsal aorta are obliterated and replaced by the correspond ing vessels on the right side. Occasionally, when the ligamentum arteriosum lies on the left side and passes behind the esophagus, it causes complaints with swa llowing. An interrupted aortic arch is caused by obliteration of the fourth aort ic arch on the left side (Fig. 11.40, A and B). It is frequently combined with a n abnormal origin of the right subclavian artery. The ductus arteriosus remains open, and the descending aorta and subclavian arteries are supplied with blood o f low oxygen content. The aortic trunk supplies the two common carotid arteries. VENOUS SYSTEM In the fth week, three pairs of major veins can be distinguished: (a) the vitelline veins, or omphalomesenteric veins, carrying blood from the yol k sac to the sinus venosus; (b) the umbilical veins, originating in the chorioni c villi and carrying oxygenated blood to the embryo; and (c) the cardinal veins, draining the body of the embryo proper (Fig. 11.41).
262 Part Two: Special Embryology Figure 11.40 A. Obliteration of the fourth aortic arch on the right and left and persistence of the distal portion of the right dorsal aorta. B. Case of interru pted aortic arch. The aorta supplies the head; the pulmonary artery, by way of t he ductus arteriosus, supplies the rest of the body. Anterior cardinal vein Aortic arches (II and III) Internal carotid artery Common cardinal vein Dorsal aorta Posterior cardinal vein Chorionic villus Heart Aortic sac Vitelline vein Umbilical vein and artery Vitelline artery Chorion Figure 11.41 Main components of the venous and arterial systems in a 4 mm embryo (end of the fourth week). Vitelline Veins Before entering the sinus venosus, the vitelline veins form a pl exus around the duodenum and pass through the septum transversum. The liver cord s growing into the septum interrupt the course of the veins, and an extensive va scular network, the hepatic sinusoids, forms (Fig. 11.42). With reduction of the left sinus horn, blood from the left side of the liver is rechanneled toward th e right, resulting in an enlargement of the right vitelline
Chapter 11: Cardiovascular System 263 Figure 11.42 Development of the vitelline and umbilical veins during the (A) fou rth and (B) fth weeks. Note the plexus around the duodenum, formation of the hepa tic sinusoids, and initiation of left to right shunts between the vitelline vein s. Right hepatocardiac channel Hepatic vein (right vitelline) Hepatic portion of inferior vena cava Hepatic vein (left vitelline) Ductus venosus Portal vein Duodenum A Left umbilical vein Vitelline veins B Splenic vein Superior mesenteric vein Left umbilical vein Figure 11.43 Development of vitelline and umbilical veins in the (A) second and (B) third months. Note formation of the ductus venosus, portal vein, and hepatic portion of the inferior vena cava. The splenic and superior mesenteric veins en ter the portal vein. vein (right hepatocardiac channel). Ultimately the right hepatocardiac channel f orms the hepatocardiac portion of the inferior vena cava. The proximal part of t he left vitelline vein disappears (Fig. 11.43, A and B ). The anastomotic networ k around the duodenum develops into a single vessel, the portal vein (Fig. 11.43 B). The superior mesenteric vein, which drains the primary intestinal loop, deri ves from the right vitelline vein. The distal portion of the left vitelline vein also disappears (Fig. 11.43, A and B).
264 Part Two: Special Embryology Umbilical Veins Initially the umbilical veins pass on each side of the liver, bu t some connect to the hepatic sinusoids (Fig. 11.42, A and B). The proximal part of both umbilical veins and the remainder of the right umbilical vein then disa ppear, so that the left vein is the only one to carry blood from the placenta to the liver (Fig. 11.43). With the increase of the placental circulation, a direc t communication forms between the left umbilical vein and the right hepatocardia c channel, the ductus venosus (Fig. 11.43, A and B). This vessel bypasses the si nusoidal plexus of the liver. After birth the left umbilical vein and ductus ven osus are obliterated and form the ligamentum teres hepatis and ligamentum venosu m, respectively. Cardinal Veins Initially the cardinal veins form the main venous drainage system of the embryo. This system consists of the anterior cardinal veins, which drain the cephalic part of the embryo, and the posterior cardinal veins, which drain the rest of the embryo. The anterior and posterior veins join before entering th e sinus horn and form the short common cardinal veins. During the fourth week, t he cardinal veins form a symmetrical system (Fig. 11.44A). During the fth to the seventh week a number of additional veins are formed: (a) the subcardinal veins, which mainly drain the kidneys; (b) the sacrocardinal veins, which drain the lo wer extremities; and (c) the supracardinal veins, which drain the body wall by w ay of the intercostal veins, taking over the functions of the posterior cardinal veins (Fig. 11.44). Formation of the vena cava system is characterized by the a ppearance of anastomoses between left and right in such a manner that the blood from the left is channeled to the right side. The anastomosis between the anteri or cardinal veins develops into the left brachiocephalic vein (Fig. 11.44, A and B ). Most of the blood from the left side of the head and the left upper extrem ity is then channeled to the right. The terminal portion of the left posterior c ardinal vein entering into the left brachiocephalic vein is retained as a small vessel, the left superior intercostal vein (Fig. 11.44B ). This vessel receives blood from the second and third intercostal spaces. The superior vena cava is fo rmed by the right common cardinal vein and the proximal portion of the right ant erior cardinal vein. The anastomosis between the subcardinal veins forms the lef t renal vein. When this communication has been established, the left subcardinal vein disappears, and only its distal portion remains as the left gonadal vein. Hence the right subcardinal vein becomes the main drainage channel and develops into the renal segment of the inferior vena cava (Fig. 11.44B ). The anastomosis between the sacrocardinal veins forms the left common iliac vein (Fig. 11.44B ) . The right sacrocardinal vein becomes the
Chapter 11: Cardiovascular System 265 Anterior cardinal vein Common cardinal vein Posterior cardinal vein Anastomosis anterior cardinal veins Superior vena cava Supracardinal vein Azygos vein Hepatic segment inferior vena cava Hepatic segment Left renal vein Left brachiocephalic vein Left superior intercostal vein Coronary sinus Hemiazygos vein Subcardinal vein Renal segment inferior vena cava Left gonadal vein Renal segment Sacrocardinal segment Left spermatic vein Sacrocardinal vein Left common iliac vein A B Figure 11.44 Development of the inferior vena cava, azygos vein, and superior ve na cava. A. Seventh week. The anastomosis lies between the subcardinals, supraca rdinals, sacrocardinals, and anterior cardinals. B. The venous system at birth s howing the three components of the inferior vena cava. sacrocardinal segment of the inferior vena cava. When the renal segment of the i nferior vena cava connects with the hepatic segment, which is derived from the r ight vitelline vein, the inferior vena cava, consisting of hepatic, renal, and s acrocardinal segments, is complete. With obliteration of the major portion of th e posterior cardinal veins, the supracardinal veins assume a greater role in dra ining the body wall. The 4th to 11th right intercostal veins empty into the righ t supracardinal vein, which together with a portion of the posterior cardinal ve in forms the azygos vein (Fig. 11.44). On the left the 4th to 7th intercostal ve ins enter into the left supracardinal vein, and the left supracardinal vein, the n known as the hemiazygos vein, empties into the azygos vein (Fig. 11.44B ). CLINICAL CORRELATES Venous System Defects The complicated development of the vena cava accounts for the fact that deviations from the normal pattern are common.
266 Part Two: Special Embryology Hepatic segment inferior vena cava Superior vena cava Renal segment inferior vena cava Azygos vein Hepatic segment Persistent left sacrocardinal vein Renal segment Sacrocardinal segment inferior vena cava Sacrocardinal segment A B Figure 11.45 A. Double inferior vena cava at the lumbar level arising from the p ersistence of the left sacrocardinal vein. B. Absent inferior vena cava. The low er half of the body is drained by the azygos vein, which enters the superior ven a cava. The hepatic vein enters the heart at the site of the inferior vena cava. A double inferior vena cava occurs when the left sacrocardinal vein fails to los e its connection with the left subcardinal vein (Fig. 11.45A). The left common i liac vein may or may not be present, but the left gonadal vein remains as in nor mal conditions. Absence of the inferior vena cava arises when the right subcardi nal vein fails to make its connection with the liver and shunts its blood direct ly into the right supracardinal vein (Figs. 11.44 and 11.45B). Hence the bloodst ream from the caudal part of the body reaches the heart by way of the azygos vei n and superior vena cava. The hepatic vein enters into the right atrium at the s ite of the inferior vena cava. Usually this abnormality is associated with other heart malformations. Left superior vena cava is caused by persistence of the le ft anterior cardinal vein and obliteration of the common cardinal and proximal p art of the anterior cardinal veins on the right (Fig. 11.46A). In such a case, b lood from the right is channeled toward the left by way of the brachiocephalic v ein. The left superior vena cava drains into the right atrium by way of the left sinus horn, that is, the coronary sinus. A double superior vena cava is charact erized by the persistence of the left anterior cardinal vein and failure of the left brachiocephalic vein to form (Fig. 11.46B). The persistent left anterior ca rdinal vein, the left superior vena cava, drains into the right atrium by way of the coronary sinus.
Chapter 11: Cardiovascular System 267 Right brachiocephalic vein Left superior vena cava Left superior vena cava Right superior vena cava Pulmonary veins Coronary sinus A Inferior vena cava B Inferior vena cava Figure 11.46 A. Left superior vena cava draining into the right atrium by way of the coronary sinus (dorsal view). B. Double superior vena cava. The communicati ng (brachiocephalic) vein between the two anterior cardinals has failed to devel op (dorsal view). Circulation Before and After Birth FETAL CIRCULATION Before birth, blood from th e placenta, about 80% saturated with oxygen, returns to the fetus by way of the umbilical vein. On approaching the liver, most of this blood ows through the duct us venosus directly into the inferior vena cava, short circuiting the liver. A s maller amount enters the liver sinusoids and mixes with blood from the portal ci rculation (Fig. 11.47). A sphincter mechanism in the ductus venosus, close to th e entrance of the umbilical vein, regulates ow of umbilical blood through the liv er sinusoids. This sphincter closes when a uterine contraction renders the venou s return too high, preventing a sudden overloading of the heart. After a short c ourse in the inferior vena cava, where placental blood mixes with deoxygenated b lood returning from the lower limbs, it enters the right atrium. Here it is guid ed toward the oval foramen by the valve of the inferior vena cava, and most of t he blood passes directly into the left atrium. A small amount is prevented from doing so by the lower edge of the septum secundum, the crista dividens, and rema ins in the right atrium. Here it mixes with desaturated blood returning from the head and arms by way of the superior vena cava. From the left atrium, where it mixes with a small amount of desaturated blood returning from the lungs, blood e nters the left ventricle and ascending aorta. Since the coronary and carotid art eries are the rst branches of the ascending aorta, the heart musculature and the brain are supplied with welloxygenated blood. Desaturated blood from the superio r vena cava ows by way of the right ventricle into the pulmonary trunk. During fe tal life, resistance in the
268 Part Two: Special Embryology Ductus arteriosus Superior vena cava Pulmonary vein Pulmonary vein V Crista dividens IV III Pulmonary artery Oval foramen II Inferior vena cava Descending aorta Ductus venosus Sphincter in ductus venosus I nferior vena cava Umbilical vein I Portal vein Umbilical arteries Figure 11.47 Fetal circulation before birth. Arrows, direction of blood ow. Note where oxygenated blood mixes with deoxygenated blood: in the liver (I ), in the inferior vena cava (II ), in the right atrium (III ), in the left atrium (IV ), and at the entrance of the ductus arteriosus into the descending aorta (V ). pulmonary vessels is high, such that most of this blood passes directly through the ductus arteriosus into the descending aorta, where it mixes with blood from the proximal aorta. After coursing through the descending aorta, blood ows toward the placenta by way of the two umbilical arteries. The oxygen saturation in the umbilical arteries is approximately 58%. During its course from the placenta to the organs of the fetus, blood in the umbilical vein gradually loses its high o xygen content as it mixes with
Chapter 11: Cardiovascular System 269 desaturated blood. Theoretically, mixing may occur in the following places (Fig. 11.47, IV ): in the liver (I ), by mixture with a small amount of blood returnin g from the portal system; in the inferior vena cava (II ), which carries deoxyge nated blood returning from the lower extremities, pelvis, and kidneys; in the ri ght atrium (III), by mixture with blood returning from the head and limbs; in th e left atrium (IV ), by mixture with blood returning from the lungs; and at the entrance of the ductus arteriosus into the descending aorta (V ). CIRCULATORY CH ANGES AT BIRTH Changes in the vascular system at birth are caused by cessation o f placental blood ow and the beginning of respiration. Since the ductus arteriosu s closes by muscular contraction of its wall, the amount of blood owing through t he lung vessels increases rapidly. This, in turn, raises pressure in the left at rium. Simultaneously, pressure in the right atrium decreases as a result of inte rruption of placental blood ow. The septum primum is then apposed to the septum s ecundum, and functionally the oval foramen closes. To summarize, the following c hanges occur in the vascular system after birth (Fig. 11.48): Closure of the umb ilical arteries, accomplished by contraction of the smooth musculature in their walls, is probably caused by thermal and mechanical stimuli and a change in oxyg en tension. Functionally the arteries close a few minutes after birth, although the actual obliteration of the lumen by brous proliferation may take 2 to 3 month s. Distal parts of the umbilical arteries form the medial umbilical ligaments, a nd the proximal portions remain open as the superior vesical arteries (Fig. 11.4 8). Closure of the umbilical vein and ductus venosus occurs shortly after that o f the umbilical arteries. Hence blood from the placenta may enter the newborn fo r some time after birth. After obliteration, the umbilical vein forms the ligame ntum teres hepatis in the lower margin of the falciform ligament. The ductus ven osus, which courses from the ligamentum teres to the inferior vena cava, is also obliterated and forms the ligamentum venosum. Closure of the ductus arteriosus by contraction of its muscular wall occurs almost immediately after birth; it is mediated by bradykinin, a substance released from the lungs during initial in ati on. Complete anatomical obliteration by proliferation of the intima is thought t o take 1 to 3 months. In the adult the obliterated ductus arteriosus forms the l igamentum arteriosum. Closure of the oval foramen is caused by an increased pres sure in the left atrium, combined with a decrease in pressure on the right side. The rst breath presses the septum primum against the septum secundum. During the rst days of life, however, this closure is reversible. Crying by the baby create s a shunt from right to left, which accounts for cyanotic periods in the newborn . Constant apposition gradually leads to fusion of the two septa in about 1 year . In 20% of individuals, however, perfect anatomical closure may never be obtain ed (probe patent foramen ovale).
270 Part Two: Special Embryology Ligamentum arteriosum Superior vena cava Pulmonary artery Closed oval foramen Pulmonary vein Inferior vena cava Descending aorta Portal vein Ligamentum teres hepatis Superior vesical artery Medial umbilical ligament Figure 11.48 Human circulation after birth. Note the changes occurring as a resu lt of the beginning of respiration and interruption of placental blood ow. Arrows , direction of blood ow. Lymphatic System The lymphatic system begins its development later than the card iovascular system, not appearing until the fth week of gestation. The origin of l ymphatic vessels is not clear, but they may form from mesenchyme in situ or may arise as saclike outgrowths from the endothelium of veins. Six primary lymph sac s are formed: two jugular, at the junction of the subclavian and anterior cardin al veins; two iliac, at the junction of the iliac and posterior cardinal veins; one retroperitoneal, near the root of the mesentery; and one cisterna chyli, dor sal
Chapter 11: Cardiovascular System 271 to the retroperitoneal sac. Numerous channels connect the sacs with each other a nd drain lymph from the limbs, body wall, head, and neck. Two main channels, the right and left thoracic ducts, join the jugular sacs with the cisterna chyli, a nd soon an anastomosis forms between these ducts. The thoracic duct then develop s from the distal portion of the right thoracic duct, the anastomosis, and the c ranial portion of the left thoracic duct. The right lymphatic duct is derived fr om the cranial portion of the right thoracic duct. Both ducts maintain their ori ginal connections with the venous system and empty into the junction of the inte rnal jugular and subclavian veins. Numerous anastomoses produce many variations in the nal form of the thoracic duct. Summary The entire cardiovascular systemheart, blood vessels, and blood cellsorigi nates from the mesodermal germ layer. Although initially paired, by the 22nd day of development the two tubes (Figs. 11.3 and 11.4) form a single, slightly bent heart tube (Fig. 11.6) consisting of an inner endocardial tube and a surroundin g myocardial mantle. During the 4th to 7th weeks the heart divides into a typica l four chambered structure. Septum formation in the heart in part arises from de velopment of endocardial cushion tissue in the atrioventricular canal (atriovent ricular cushions) and in the conotruncal region (conotruncal swellings). Because of the key location of cushion tissue, many cardiac malformations are related t o abnormal cushion morphogenesis. Septum Formation in the Atrium. The septum pri mum, a sickle shaped crest descending from the roof of the atrium, begins to div ide the atrium in two but leaves a lumen, the ostium primum, for communication b etween the two sides (Fig. 11.14). Later, when the ostium primum is obliterated by fusion of the septum primum with the endocardial cushions, the ostium secundu m is formed by cell death that creates an opening in the septum primum. Finally, a septum secundum forms, but an interatrial opening, the oval foramen, persists . Only at birth, when pressure in the left atrium increases, do the two septa pr ess against each other and close the communication between the two. Abnormalitie s in the atrial septum may vary from total absence (Fig. 11.19) to a small openi ng known as probe patency of the oval foramen. Septum Formation in the Atriovent ricular Canal. Four endocardial cushions surround the atrioventricular canal. Fu sion of the opposing superior and inferior cushions divides the ori ce into right and left atrioventricular canals. Cushion tissue then becomes brous and forms the mitral (bicuspid) valve on the left and the tricuspid valve on the right (Fig. 11.17). Persistence of the common atrioventricular canal (Fig. 11.20) and abnorm al division of the canal (Fig. 11.21B ) are well known defects.
272 Part Two: Special Embryology Septum Formation in the Ventricles. The interventricular septum consists of a th ick muscular part and a thin membranous portion (Fig. 11.25) formed by (a) an in ferior endocardial atrioventricular cushion, (b) the right conus swelling, and ( c) the left conus swelling (Fig. 11.23). In many cases these three components fa il to fuse, resulting in an open interventricular foramen. Although this abnorma lity may be isolated, it is commonly combined with other compensatory defects (F igs. 11.28 and 11.29). Septum Formation in the Bulbus. The bulbus is divided int o (a) the truncus (aorta and pulmonary trunk), (b) the conus (out ow tract of the aorta and pulmonary trunk), and (c) the trabeculated portion of the right ventri cle. The truncus region is divided by the spiral aorticopulmonary septum into th e two main arteries (Fig. 11.22). The conus swellings divide the out ow tracts of the aortic and pulmonary channels and with tissue from the inferior endocardial cushion close the interventricular foramen (Fig. 11.23). Many vascular abnormali ties, such as transposition of the great vessels and pulmonary valvular atresia, result from abnormal division of the conotruncal region; they may involve neura l crest cells that contribute to septum formation in the conotruncal region. The aortic arches lie in each of the ve pharyngeal arches (Figs. 11.35). Four import ant derivatives of the original aortic arch system are (a) the carotid arteries (third arches); (b) the arch of the aorta (left fourth aortic arch); (c) the pul monary artery (sixth aortic arch), which during fetal life is connected to the a orta through the ductus arteriosus; and (d) the right subclavian artery formed b y the right fourth aortic arch, distal portion of the right dorsal aorta, and th e seventh intersegmental artery (Fig. 11.35B). The most common vascular aortic a rch abnormalities include (a) open ductus arteriosus and coarctation of the aort a (Fig. 11.37) and (b) persistent right aortic arch and abnormal right subclavia n artery (Figs. 11.38 and 11.39), both causing respiratory and swallowing compla ints. The vitelline arteries initially supply the yolk sac but later form the ce liac, superior mesenteric, and inferior mesenteric arteries, which supply the fo regut, midgut, and hindgut regions, respectively. The paired umbilical arteries arise from the common iliac arteries. After birth the distal portions of these a rteries are obliterated to form the medial umbilical ligaments, whereas the prox imal portions persist as the internal iliac and vesicular arteries. Venous Syste m. Three systems can be recognized: (a) the vitelline system, which develops int o the portal system; (b) the cardinal system, which forms the caval system; and (c) the umbilical system, which disappears after birth. The complicated caval sy stem is characterized by many abnormalities, such as double inferior and superio r vena cava and left superior vena cava (Fig. 11.46). Changes at Birth. During p renatal life the placental circulation provides the fetus with its oxygen, but a fter birth the lungs take on gas exchange. In the
Chapter 11: Cardiovascular System 273 circulatory system the following changes take place at birth and in the rst postn atal months: (a) the ductus arteriosus closes; (b) the oval foramen closes; (c) the umbilical vein and ductus venosus close and remain as the ligamentum teres h epatis and ligamentum venosum; and (d) the umbilical arteries form the medial um bilical ligaments. Lymphatic System. The lymphatic system develops later than th e cardiovascular system, originating as ve sacs: two jugular, two iliac, one retr operitoneal, and one cisterna chyli. Numerous channels form to connect the sacs and provide drainage from other structures. Ultimately the thoracic duct forms f rom anastomosis of the right and left thoracic ducts, the distal part of the rig ht thoracic duct, and the cranial part of the left thoracic duct. The right lymp hatic duct develops from the cranial part of the right thoracic duct. Problems to Solve 1. A prenatal ultrasound of a 35 year old woman in her 12th we ek of gestation reveals an abnormal image of the fetal heart. Instead of a four chambered view provided by the typical cross, a portion just below the crosspiec e is missing. What structures constitute the cross, and what defect does this in fant probably have? 2. A child is born with severe craniofacial defects and tran sposition of the great vessels. What cell population may play a role in both abn ormalities, and what type of insult might have produced this effect? 3. What typ e of tissue is critical for dividing the heart into four chambers and the out ow t ract into pulmonary and aortic channels? 4. A patient complains about having dif c ulty swallowing. What vascular abnormality or abnormalities might produce this c omplaint? What is its embryological origin? SUGGESTED READING Adkins RB, et al.: Dysphagia associated with aortic arch anoma ly in adults. Am Surg 52:238, 1986. Basson CT, et al.: Mutations in human TBX5 c ause limb and cardiac malformation in Holt Oram syndrome. Nat Genet 15:30, 1997. Bruyer HJ, Kargas SA, Levy JM: The causes and underlying developmental mechanis ms of congenital cardiovascular malformation: a critical review. Am J Med Genet 3:411, 1987. Clark EB: Cardiac embryology: its relevance to congenital heart dis ease. Am J Dis Child 140:41, 1986. Cof n D, Poole TJ: Embryonic vascular developme nt: immunohistochemical identi cation of the origin and subsequent morphogenesis o f the major vessel primordia of quail embryos. Development 102:735, 1988. Fishma n MC, Chien KR: Fashioning the vertebrate heart: earliest embryonic decisions. D evelopment 124:2099, 1997. Harvey RP: NK 2 homeobox genes and heart development. Dev Biol 178:203, 1996.
274 Part Two: Special Embryology Hirakow R: Development of the cardiac blood vessels in staged human embryos. Act a Anat 115:220, 1983. Ho E, Shimada Y: Formation of the epicardium studied with the scanning electron microscope. Dev Biol 66:579, 1978. Jiang X, Rowitch DH, So riano P, McMahon AP, Sucov HM: Fate of the mammalian neural crest. Development 1 27:1607, 2000. Kirklin JW, et al.: Complete transposition of the great arteries: treatment in the current era. Pediatr Clin North Am 37:171, 1990. Li QY, et al. : Holt Oram syndrome is caused by mutations in TBX5, a member of the Brachyury ( T ) gene family. Nat Genet 15:21, 1997. Manasek FJ, Burnside MB, Waterman RE: My ocardial cell shape change as a mechanism of embryonic heart looping. Dev Biol 2 9:349, 1972. Marvin MJ, DiRocco GD, Gardiner A, Bush SA, Lassar AB: Inhibition o f Wnt activity induces heart formation from posterior mesoderm. Genes Dev 15:316 , 2001. Noden DM: Origins and assembly of avian embryonic blood vessels. Ann N Y Acad Sci 588:236, 1990. Schott JJ, et al.: Congenital heart disease caused by m utations in the transcription factor NKX25. Science 281:108, 1998. Skandalakis JE , Gray SW: Embryology for Surgeons: The Embryological Basis for the Treatment of Congenital Anomalies. 2nd ed. Baltimore, Williams & Wilkins, 1994. Waldo K, Miy agawa Tomita S, Kumiski D, Kirby ML: Cardiac neural crest cells provide new insi ght into septation of the cadiac out ow tract: aortic sac to ventricular septal cl osure. Dev Biol 196:129, 1998.
chapter 12 Respiratory System Formation of the Lung Buds When the embryo is approximately 4 weeks old, the respiratory diverticulum (lung bud) appears as an outgrowth from the ventral wall of the foregut (Fig. 12.1A). The location of the bud along the gut tube is determined by signals from the su rrounding mesenchyme, including broblast growth factors (FGFs) that instructthe end oderm. Hence epithelium of the internal lining of the larynx, trachea, and bronc hi, as well as that of the lungs, is entirely of endodermal origin. The cartilag inous, muscular, and connective tissue components of the trachea and lungs are d erived from splanchnic mesoderm surrounding the foregut. Initially the lung bud is in open communication with the foregut (Fig. 12.1B). When the diverticulum ex pands caudally, however, two longitudinal ridges, the tracheoesophageal ridges, separate it from the foregut (Fig. 12.2A). Subsequently, when these ridges fuse to form the tracheoesophageal septum, the foregut is divided into a dorsal porti on, the esophagus, and a ventral portion, the trachea and lung buds (Fig. 12.2, B and C ). The respiratory primordium maintains its communication with the phary nx through the laryngeal ori ce (Fig. 12.2D). 275
276 Part Two: Special Embryology Openings of pharyngeal pouches Respiratory diverticulum Stomach Heart Vitelline duct Allantois Cloacal membrane Liver bud Duodenum Attachment of Midgut buccopha ryngeal membrane Hindgut Respiratory diverticulum A B Laryngotracheal orifice Figure 12.1 A. Embryo of approximately 25 days gestation showing the relation of the respiratory diverticulum to the heart, stomach, and liver. B. Sagittal sect ion through the cephalic end of a 5 week embryo showing the openings of the phar yngeal pouches and the laryngotracheal ori ce. Tracheoesophageal ridge Foregut Esophagus Tuberculum impar Lateral lingual swelling I Trachea II Foramen cecum III Respiratory diverticulum Lung buds Laryngeal swellings IV VI A B C D Epiglottal swelling Laryngeal orifice Figure 12.2 A, B, and C. Successive stages in development of erticulum showing the tracheoesophageal ridges and formation tting the foregut into esophagus and trachea with lung buds. ion of the pharynx seen from above showing the laryngeal ori elling. CLINICAL CORRELATES Abnormalities in partitioning of the esophagus and trachea by the tracheoesaphag eal septum result in esophageal atresia with or without tracheoesaphageal stulas (TEFs). These defects occur in approximately in 1/3000 births, and 90% result in the upper portion of the esophagus ending in a blind the respiratory div of the septum, spli D. The ventral port ce and surrounding sw
Chapter 12: Respiratory System 277 Trachea Bifurcation Proximal blindend part of esophagus Tracheoesophageal fistula Communication of e sophagus with trachea A Bronchi Distal part of esophagus B C D E Figure 12.3 Various types of esophageal atresia and/or tracheoesophageal stulae. A. The most frequent abnormality (90% of cases) occurs with the upper esophagus ending in a blind pouch and the lower segment forming a stula with the trachea. B . Isolated esophageal atresia (4% of cases). C. H type tracheoesophageal stula (4 % of cases). D and E. Other variations (each 1% of cases). pouch and the lower segment forming a stula with the trachea (Fig. 12.3A). Isolat ed esophageal atresia (Fig. 12.3B) and H type TEF without esophageal atresia (Fi g. 12.3C ) each account for 4% of these defects. Other variations (Fig. 12.3, D and E ) each account for approximately 1% of these defects. These abnormalities are associated with other birth defects, including cardiac abnormalities, which occur in 33% of these cases. In this regard TEFs are a component of the VACTERL association (Vertebral anomalies, Anal atresia, Cardiac defects, Tracheoesophage al stula, Esophageal atresia, Renal anomalies, and Limb defects), a collection of defects of unknown causation, but occurring more frequently than predicted by c hance alone. A complication of some TEFs is polyhydramnios, since in some types of TEF amniotic uid does not pass to the stomach and intestines. Also, gastric co ntents and/or amniotic uid may enter the trachea through a stula, causing pneumoni tis and pneumonia. Larynx The internal lining of the larynx originates from endoderm, but the carti lages and muscles originate from mesenchyme of the fourth and sixth pharyngeal
278 Part Two: Special Embryology I II III IV VI Figure 12.4 Laryngeal ori ce and surrounding swellings at successive stages of dev elopment. A. 6 weeks. B. 12 weeks. arches. As a result of rapid proliferation of this mesenchyme, the laryngeal ori c e changes in appearance from a sagittal slit to a T shaped opening (Fig. 12.4A). Subsequently, when mesenchyme of the two arches transforms into the thyroid, cr icoid, and arytenoid cartilages, the characteristic adult shape of the laryngeal ori ce can be recognized (Fig. 12.4B). At about the time that the cartilages are formed, the laryngeal epithelium also proliferates rapidly, resulting in a tempo rary occlusion of the lumen. Subsequently, vacuolization and recanalization prod uce a pair of lateral recesses, the laryngeal ventricles. These recesses are bou nded by folds of tissue that differentiate into the false and true vocal cords. Since musculature of the larynx is derived from mesenchyme of the fourth and six th pharyngeal arches, all laryngeal muscles are innervated by branches of the te nth cranial nerve, the vagus nerve. The superior laryngeal nerve innervates deri vatives of the fourth pharyngeal arch, and the recurrent laryngeal nerve innerva tes derivatives of the sixth pharyngeal arch. (For further details on the laryng eal cartilages, see Chapter 15.) Trachea, Bronchi, and Lungs During its separation from the foregut, the lung bud forms the trachea and two lateral outpocketings, the bronchial buds (Fig. 12.2, B and C ). At the beginning of the fth week, each of these buds enlarges to form right and left main bronchi. The right then forms three secondary bronchi, and the left, two (Fig. 12.5A), thus foreshadowing the three lobes on the right side and two on the left (Fig. 12.5, B and C ). With subsequent growth in caudal and lateral directions, the lung buds expand into the body cavity (Fig. 12.6). The spaces for the lungs, the pericardioperitoneal canals, are narrow. They lie on e ach side of the foregut (Fig. 10.4)
Chapter 12: Respiratory System 279 Figure 12.5 Stages in development of the trachea and lungs. A. 5 weeks. B. 6 wee ks. C. 8 weeks. Lung bud Pleuropericardial fold Phrenic nerve Common cardinal vein Heart A B Figure 12.6 Expansion of the lung buds into the pericardioperitoneal canals. At this stage the canals are in communication with the peritoneal and pericardial c avities. A. Ventral view of lung buds. B. Transverse section through the lung bu ds showing the pleuropericardial folds that will divide the thoracic portion of the body cavity into the pleural and pericardial cavities. and are gradually lled by the expanding lung buds. Ultimately the pleuroperitonea l and pleuropericardial folds separate the pericardioperitoneal canals from the peritoneal and pericardial cavities, respectively, and the remaining spaces form the primitive pleural cavities (see Chapter 10). The mesoderm, which covers the outside of the lung, develops into the visceral pleura. The somatic mesoderm la yer, covering the body wall from the inside, becomes the parietal pleura (Fig. 1 2.6A). The space between the parietal and visceral pleura is the pleural cavity (Fig. 12.7).
280 Part Two: Special Embryology Figure 12.7 Once the pericardioperitoneal canals separate from the pericardial a nd peritoneal cavities, respectively, the lungs expand in the pleural cavities. Note the visceral and parietal pleura and de nitive pleural cavity. The visceral p leura extends between the lobes of the lungs. During further development, secondary bronchi divide repeatedly in a dichotomous fashion, forming 10 tertiary (segmental) bronchi in the right lung and 8 in the left, creating the bronchopulmonary segments of the adult lung. By the end of t he sixth month, approximately 17 generations of subdivisions have formed. Before the bronchial tree reaches its nal shape, however, an additional 6 divisions for m during postnatal life. Branching is regulated by epithelial mesenchymal intera ctions between the endoderm of the lung buds and splanchnic mesoderm that surrou nds them. Signals for branching, which emit from the mesoderm, involve members o f the broblast growth factor (FGF) family. While all of these new subdivisions ar e occurring and the bronchial tree is developing, the lungs assume a more caudal position, so that by the time of birth the bifurcation of the trachea is opposi te the fourth thoracic vertebra. Maturation of the Lungs (Table 12.1) Up to the seventh prenatal month, the bronc hioles divide continuously into more and smaller canals (canalicular phase) (Fig . 12.8A), and the vascular
Chapter 12: Respiratory System TABLE 12.1 281 Maturation of the Lungs 516 weeks Branching has continued to form terminal bronchioles. No respiratory br onchioles or alveoli are present. Each terminal bronchiole divides into 2 or mor e respiratory bronchioles, which in turn divide into 36 alveolar ducts. Terminal sacs (primitive alveoli) form, and capillaries establish close contact. Mature a lveoli have well developed epithelial endothelial (capillary) contacts. Pseudoglandular period Canalicular period 1626 weeks Terminal sac period Alveolar period 26 weeks to birth 8 months to childhood Respiratory bronchiolus Blood capillaries Terminal sacs Thin squamous epithelium Flat endothelium cell of blood capillary Cuboidal epithelium A Terminal bronchiolus B Cuboidal epithelium Figure 12.8 Histological and functional development of the lung. A. The canalicu lar period lasts from the 16th to the 26th week. Note the cuboidal cells lining the respiratory bronchioli. B. The terminal sac period begins at the end of the sixth and beginning of the seventh prenatal month. Cuboidal cells become very th in and intimately associated with the endothelium of blood and lymph capillaries or form terminal sacs (primitive alveoli). supply increases steadily. Respiration becomes possible when some of the cells o f the cuboidal respiratory bronchioles change into thin, at cells (Fig. 12.8B). T hese cells are intimately associated with numerous blood and lymph capillaries, and the surrounding spaces are now known as terminal sacs or primitive alveoli. During the seventh month, suf cient numbers of capillaries are present to guarante e adequate gas exchange, and the premature infant is able to survive. During the last 2 months of prenatal life and for several years thereafter, the number of terminal sacs increases steadily. In addition, cells lining the sacs,
282 Part Two: Special Embryology Figure 12.9 Lung tissue in a newborn. Note the thin squamous epithelial cells (a lso known as alveolar epithelial cells, type I) and surrounding capillaries prot ruding into mature alveoli. known as type I alveolar epithelial cells, become thinner, so that surrounding c apillaries protrude into the alveolar sacs (Fig. 12.9). This intimate contact be tween epithelial and endothelial cells makes up the blood air barrier. Mature al veoli are not present before birth. In addition to endothelial cells and at alveo lar epithelial cells, another cell type develops at the end of the sixth month. These cells, type II alveolar epithelial cells, produce surfactant, a phospholip id rich uid capable of lowering surface tension at the air alveolar interface. Be fore birth the lungs are full of uid that contains a high chloride concentration, little protein, some mucus from the bronchial glands, and surfactant from the a lveolar epithelial cells (type II). The amount of surfactant in the uid increases , particularly during the last 2 weeks before birth. Fetal breathing movements b egin before birth and cause aspiration of amniotic uid. These movements are impor tant for stimulating lung development and conditioning respiratory muscles. When respiration begins at birth, most of the lung uid is rapidly resorbed by the blo od and lymph capillaries, and a small amount is probably expelled via the trache a and bronchi during delivery. When the uid is resorbed from alveolar sacs, surfa ctant remains deposited as a thin phospholipid coat on alveolar cell membranes. With air entering alveoli during the rst breath, the surfactant coat prevents dev elopment of an air water (blood) interface with high surface tension. Without th e fatty surfactant layer, the alveoli would collapse during expiration (atelecta sis). Respiratory movements after birth bring air into the lungs, which expand a nd ll the pleural cavity. Although the alveoli increase somewhat in size, growth of the lungs after birth is due primarily to an increase in the number
Chapter 12: Respiratory System 283 of respiratory bronchioles and alveoli. It is estimated that only one sixth of t he adult number of alveoli are present at birth. The remaining alveoli are forme d during the rst 10 years of postnatal life through the continuous formation of n ew primitive alveoli. CLINICAL CORRELATES Surfactant is particularly important for survival of the premature infant. When surfactant is insuf cient, the air water (blood) surface membrane tension becomes high, bringing great risk that alveoli will collapse during expiration. As a res ult, respiratory distress syndrome (RDS) develops. This is a common cause of dea th in the premature infant. In these cases the partially collapsed alveoli conta in a uid with a high protein content, many hyaline membranes, and lamellar bodies , probably derived from the surfactant layer. RDS, which is therefore also known as hyaline membrane disease, accounts for approximately 20% of deaths among new borns. Recent development of arti cial surfactant and treatment of premature babie s with glucocorticoids to stimulate surfactant production have reduced the morta lity associated with RDS and allowed survival of some babies as young as 5.5 mon ths of gestation. Although many abnormalities of the lung and bronchial tree hav e been described (e.g., blind ending trachea with absence of lungs and agenesis of one lung), most of these gross abnormalities are rare. Abnormal divisions of the bronchial tree are more common; some result in supernumerary lobules. These variations of the bronchial tree have little functional signi cance, but they may cause unexpected dif culties during bronchoscopies. More interesting are ectopic l ung lobes arising from the trachea or esophagus. It is believed that these lobes are formed from additional respiratory buds of the foregut that develop indepen dently of the main respiratory system. Most important clinically are congenital cysts of the lung, which are formed by dilation of terminal or larger bronchi. T hese cysts may be small and multiple, giving the lung a honeycomb appearance on radiograph, or they may be restricted to one or more larger ones. Cystic structu res of the lung usually drain poorly and frequently cause chronic infections. Summary The respiratory system is an outgrowth of the ventral wall of the foregu t, and the epithelium of the larynx, trachea, bronchi, and alveoli originates in the endoderm. The cartilaginous, muscular, and connective tissue components ari se in the mesoderm. In the fourth week of development, the tracheoesophageal sep tum separates the trachea from the foregut, dividing the foregut into the lung b ud anteriorly and the esophagus posteriorly. Contact between the two is maintain ed through the larynx, which is formed by tissue of the fourth and sixth pharyng eal arches. The lung bud develops into two main
284 Part Two: Special Embryology bronchi: the right forms three secondary bronchi and three lobes; the left forms two secondary bronchi and two lobes. Faulty partitioning of the foregut by the tracheoesophageal septum causes esophageal atresias and tracheoesophageal stulas (Fig. 12.3). After a pseudoglandular (516 weeks) and canalicular (1626 weeks) phas e, cells of the cuboidal lined bronchioles change into thin, at cells, type I alv eolar epithelial cells, intimately associated with blood and lymph capillaries. In the seventh month, gas exchange between the blood and air in the primitive al veoli is possible. Before birth the lungs are lled with uid with little protein, s ome mucus, and surfactant, which is produced by type II alveolar epithelial cell s and which forms a phospholipid coat on the alveolar membranes. At the beginnin g of respiration the lung uid is resorbed except for the surfactant coat, which p revents the collapse of the alveoli during expiration by reducing the surface te nsion at the air blood capillary interface. Absent or insuf cient surfactant in th e premature baby causes respiratory distress syndrome (RDS) because of collapse of the primitive alveoli (hyaline membrane disease). Growth of the lungs after b irth is primarily due to an increase in the number of respiratory bronchioles an d alveoli and not to an increase in the size of the alveoli. New alveoli are for med during the rst 10 years of postnatal life. Problems to Solve 1. A prenatal ultrasound revealed polyhydramnios, and at birth the baby had excessive uids in its mouth. What type of birth defect might be pre sent, and what is its embryological origin? Would you examine the child carefull y for other birth defects? Why? 2. A baby born at 6 months gestation is having t rouble breathing. Why? SUGGESTED READING Bellusci S, et al.: Fibroblast growth factor 10 (FGF 10) and b ranching morphogenesis in the embryonic mouse lung. Development 124:4867, 1997. Endo H, Oka T: An immunohistochemical study of bronchial cells producing surfact ant protein A in the developing human fetal lung. Early Hum Dev 25:149, 1991. Ko zuma S, Nemoto A, Okai T, Mizuno M: Maturational sequence of fetal breathing mov ements. Biol Neonate 60(suppl 1):36, 1991. Shannon JM, Nielson LD, Gebb SA, Rand ell SH: Mesenchyme speci es epithelial differentiation in reciprocal recombinants of embryonic lung and trachea. Dev Dynam 212:482, 1998. Whitsett JA: Molecular a spects of the pulmonary surfactant system in the newborn. In Chernick V, Mellins RB (eds): Basic Mechanisms of Pediatric Respiratory Disease: Cellular and Integ rative. Philadelphia, BC Decker, 1991.
chapter 13 Digestive System Divisions of the Gut Tube As a result of cephalocaudal and lateral folding of th e embryo, a portion of the endoderm lined yolk sac cavity is incorporated into t he embryo to form the primitive gut. Two other portions of the endoderm lined ca vity, the yolk sac and the allantois, remain outside the embryo (Fig. 13.1, AD). In the cephalic and caudal parts of the embryo, the primitive gut forms a blind ending tube, the foregut and hindgut, respectively. The middle part, the midgut, remains temporally connected to the yolk sac by means of the vitelline duct, or yolk stalk (Fig. 13.1D). Development of the primitive gut and its derivatives i s usually discussed in four sections: (a) The pharyngeal gut, or pharynx, extend s from the buccopharyngeal membrane to the tracheobronchial diverticulum (Fig. 1 3.1D); since this section is particularly important for development of the head and neck, it is discussed in Chapter 15. (b) The foregut lies caudal to the phar yngeal tube and extends as far caudally as the liver outgrowth. (c) The midgut b egins caudal to the liver bud and extends to the junction of the right two third s and left third of the transverse colon in the adult. (d) The hindgut extends f rom the left third of the transverse colon to the cloacal membrane (Fig. 13.1). Endoderm forms the epithelial lining of the digestive tract and gives rise to th e parenchyma of glands, such as the liver and pancreas. Muscle, connective tissu e, and peritoneal components of the wall of the gut are derived from splanchnic mesoderm. 285
286 Part Two: Special Embryology Hindgut Endoderm Amniotic cavity Connecting stalk Foregut Heart tube Ectoderm Angiogenic cell cluster Allantois Pericardial cavity Buccopharyngeal membrane A Buccopharyngeal membrane Cloacal membrane B Lung bud Liver bud Midgut Cloacal membrane Heart tube Remnant of the buccopharyngeal membrane Vitelline duct Allantois C D Yolk sac Figure 13.1 Sagittal sections through embryos at various stages of development d emonstrating the effect of cephalocaudal and lateral folding on the position of the endoderm lined cavity. Note formation of the foregut, midgut, and hindgut. A . Presomite embryo. B. Embryo with 7 somites. C. Embryo with 14 somites. D. At t he end of the rst month. Molecular Regulation of Gut Tube Development Differentiation of various regions of the gut and its derivatives is dependent upon a reciprocal interaction betwee n the endoderm (epithelium) of the gut tube and surrounding splanchnic mesoderm. Mesoderm dictates the type of structure that will form, for example lungs in th e thoracic region and descending colon from the hindgut region, through a HOX co de similar to the one that establishes the anterior (cranial) posterior (caudal) body axis. Induction of this HOX code is a result of sonic hedgehog (SHH) expre ssed throughout the gut endoderm. Thus, in the region of the mid and hindgut, e xpression of SHH in gut endoderm establishes a nested expression of the HOX code in the mesoderm (Fig. 13.2). Once the mesoderm is speci ed by this code, it instr ucts the endoderm to form the various components of the mid and hindgut regions , including the small intestine, cecum, colon, and cloaca (Fig. 13.2). Similar i nteractions are responsible for partitioning the foregut.
Chapter 13: Digestive System Foregut Hindgut 287 Heart Tube HOX 9 9 10 9 11 small intestine cecum 9 12 S H H S H H large intestine 9 13 cloaca Figure 13.2 Diagrams of the mid and hindgut regions. The morphogen sonic hedgeh og (SHH) is secreted by gut endoderm and induces a nested expression of HOX gene s in surrounding mesoderm. HOX expression then initiates a cascade of genes that instruct gut endoderm to differentiate into its regional identities. Signaling be tween the two tissues is an example of an epithelial mesenchymal interaction. Mesenteries Portions of the gut tube and its derivatives are suspended from the dorsal and ventral body wall by mesenteries, double layers of peritoneum that en close an organ and connect it to the body wall. Such organs are called intraperi toneal, whereas organs that lie against the posterior body wall and are covered by peritoneum on their anterior surface only (e.g., the kidneys) are considered retroperitoneal. Peritoneal ligaments are double layers of peritoneum (mesenteri es) that pass from one organ to another or from an organ to the body wall. Mesen teries and ligaments provide pathways for vessels, nerves, and lymphatics to and from abdominal viscera (Figs. 13.3 and 13.4). Initially the foregut, midgut, an d hindgut are in broad contact with the mesenchyme of the posterior abdominal wa ll (Fig. 13.3). By the fth week,
288 Part Two: Special Embryology Amnionic cavity Surface ectoderm Somatic mesoderm Connection between gut and yolk sac Intraembryonic body cavity Splanchnic mesoderm Yolk sac Dorsal Gut mesentery A B C Figure 13.3 Transverse sections through embryos at various stages of development . A. The intraembryonic cavity, bordered by splanchnic and somatic layers of lat eral plate mesoderm, is in open communication with the extraembryonic cavity. B. The intraembryonic cavity is losing its wide connection with the extraembryonic cavity. C. At the end of the fourth week splanchnic mesoderm layers are fused i n the midline and form a double layered membrane (dorsal mesentery) between righ t and left halves of the body cavity. Ventral mesentery exists only in the regio n of the septum transversum (not shown). D. Scanning electron micrograph of a mo use embryo at approximately the same stage as in B. The mesoderm (arrowheads) su rrounds the gut tube (G) and suspends it from the posterior body wall into the b ody cavity (C). E. Scanning electron micrograph of a mouse embryo at approximate ly the same stage as in C. Mesoderm suspends the gut tube from the posterior bod y wall into the body cavity (C) and is thinning to form the dorsal mesentery (ar row). NT, neural tube; A, dorsal aorta.
Chapter 13: Digestive System 289 Bare area of liver Diaphragm Lesser omentum Dorsal mesogastrium Celiac artery Falciform ligament Dorsal mesoduodenum Vitelline duct Superior mesenteric artery Mesentery proper Allantois Inferior mesenteric artery Cloaca Umbilical artery Figure 13.4 Primitive dorsal and ventral mesenteries. The liver is connected to the ventral abdominal wall and to the stomach by the falciform ligament and less er omentum, respectively. The superior mesenteric artery runs through the mesent ery proper and continues toward the yolk sac as the vitelline artery. Dorsal mesocolon however, the connecting tissue bridge has narrowed, and the caudal part of the f oregut, the midgut, and a major part of the hindgut are suspended from the abdom inal wall by the dorsal mesentery (Figs. 13.3C and 13.4), which extends from the lower end of the esophagus to the cloacal region of the hindgut. In the region of the stomach it forms the dorsal mesogastrium or greater omentum; in the regio n of the duodenum it forms the dorsal mesoduodenum; and in the region of the col on it forms the dorsal mesocolon. Dorsal mesentery of the jejunal and ileal loop s forms the mesentery proper. Ventral mesentery, which exists only in the region of the terminal part of the esophagus, the stomach, and the upper part of the d uodenum (Fig. 13.4), is derived from the septum transversum. Growth of the liver into the mesenchyme of the septum transversum divides the ventral mesentery int o (a) the lesser omentum, extending from the lower portion of the esophagus, the stomach, and the upper portion of the duodenum to the liver, and (b) the falcif orm ligament, extending from the liver to the ventral body wall (Fig. 13.4). Foregut ESOPHAGUS When the embryo is approximately 4 weeks old, the respiratory diverticulum (lung bud) appears at the ventral wall of the foregut at the border with the
290 Part Two: Special Embryology Pharyngeal pouches Pharyngeal gut Tracheobronchial diverticulum Esophagus Stomod eum Liver Gallbladder Vitelline duct Allantois Cloaca Stomach Pancreas Primitive intestinal loop Hindgut Heart bulge Urinary bladder Cloacal membrane Esophagus A B Figure 13.5 Embryos during the fourth (A) and fth (B) weeks of development showin g formation of the gastrointestinal tract and the various derivatives originatin g from the endodermal germ layer. Figure 13.6 Successive stages in development of the respiratory diverticulum and esophagus through partitioning of the foregut. A. At the end of the third week (lateral view). B and C. During the fourth week (ventral view). pharyngeal gut (Fig. 13.5). The tracheoesophageal septum gradually partitions th is diverticulum from the dorsal part of the foregut (Fig. 13.6). In this manner the foregut divides into a ventral portion, the respiratory primordium, and a do rsal portion, the esophagus (see Chapter 12). At rst the esophagus is short (Fig. 13.5A), but with descent of the heart and lungs it lengthens rapidly (Fig. 13.5 B ). The muscular coat, which is formed
Chapter 13: Digestive System 291 by surrounding splanchnic mesenchyme, is striated in its upper two thirds and in nervated by the vagus; the muscle coat is smooth in the lower third and is inner vated by the splanchnic plexus. CLINICAL CORRELATES Esophageal Abnormalities Esophageal atresia and/or tracheoesophageal stula result s either from spontaneous posterior deviation of the tracheoesophageal septum or from some mechanical factor pushing the dorsal wall of the foregut anteriorly. In its most common form the proximal part of the esophagus ends as a blind sac, and the distal part is connected to the trachea by a narrow canal just above the bifurcation (Fig. 13.7A). Other types of defects in this region occur much less frequently (Fig. 13.7, BE ) (see Chapter 12). Atresia of the esophagus prevents normal passage of amniotic uid into the intestinal tract, resulting in accumulati on of excess uid in the amniotic sac (polyhydramnios). In addition to atresias, t he lumen of the esophagus may narrow, producing esophageal stenosis, usually in the lower third. Stenosis may be caused by incomplete recanalization, vascular a bnormalities, or Trachea Bifurcation Proximal blindend part of esophagus Tracheoesophageal fistula Communication of esophagus with trachea Bronchi A Distal part of esophagus B C D E Figure 13.7 Variations of esophageal atresia and/or tracheoesophageal stula in or der of their frequency of appearance: A, 90%; B, 4 %; C, 4 %; D, 1 %; and E, 1 % .
292 Part Two: Special Embryology accidents that compromise blood ow. Occasionally the esophagus fails to lengthen suf ciently and the stomach is pulled up into the esophageal hiatus through the di aphragm. The result is a congenital hiatal hernia. STOMACH The stomach appears as a fusiform dilation of the foregut in the fourth week of development (Fig. 13.8). During the following weeks, its appearance and position change greatly as a result of the different rates of growth in various regions of its wall and the changes in position of surrounding organs. Positiona l changes of the stomach are most easily explained by assuming that it rotates a round a longitudinal and an anteroposterior axis (Fig. 13.8). The stomach rotate s 90 clockwise around its longitudinal axis, causing its left side to face anteri orly and its right side to face posteriorly (Fig. 13.8, AC). Hence the left vagus nerve, initially innervating the left side of the stomach, now innervates the a nterior wall; similarly, the right vagus nerve innervates the Longitudinal rotation axis Stomach Lesser curvature Duodenum A B Esophagus C Greater curvature Anteroposterior axis Lesser curvature D Pylorus Greater curvature E Greater curvature Figure 13.8 A, B, and C. Rotation of the stomach along its longitudinal axis as seen anteriorly. D and E. Rotation of the stomach around the anteroposterior axi s. Note the change in position of the pylorus and cardia.
Chapter 13: Digestive System 293 Figure 13.9 A. Transverse section through a 4-week em ryo showing intercellular clefts appearing in the dorsal mesogastrium. B and C. The clefts have fused, and the omental ursa is formed as an extension of the right side of the intraem ry onic cavity ehind the stomach. posterior wall. During this rotation the original posterior wall of the stomach grows faster than the anterior portion, forming the greater and lesser curvature s (Fig. 13.8C ). The cephalic and caudal ends of the stomach originally lie in t he midline, ut during further growth the stomach rotates around an anteroposter ior axis, such that the caudal or pyloric part moves to the right and upward and the cephalic or cardiac portion moves to the left and slightly downward (Fig. 1 3.8, D and E ). The stomach thus assumes its nal position, its axis running from a ove left to elow right. Since the stomach is attached to the dorsal ody wall y the dorsal mesogastrium and to the ventral ody wall y the ventral mesogast rium (Figs. 13.4 and 13.9A), its rotation and disproportionate growth alter the position of these mesenteries. Rotation a out the longitudinal axis pulls the do rsal mesogastrium to the left, creating a space ehind the stomach called the om ental ursa (lesser peritoneal sac) (Figs. 13.9 and 13.10). This rotation also p ulls the ventral mesogastrium to the right. As this process continues in the fth week of development, the spleen primordium appears as a mesodermal proliferation etween the two leaves of the dorsal mesogastrium (Figs. 13.10 and 13.11). With continued rotation of the stomach, the dorsal mesogastrium lengthens, and the p ortion etween the spleen and dorsal midline swings to the left and fuses with t he peritoneum of the posterior a dominal wall (Figs. 13.10 and 13.11). The poste rior leaf of the dorsal mesogastrium and the peritoneum along this line of fusio n degenerate. The spleen, which remains intraperitoneal, is then connected to th e ody wall in the region of the left kidney y the lienorenal ligament and to t he stomach y the gastrolienal ligament (Figs. 13.10 and
294 Part Two: Special Em ryology Lesser omentum Liver Stomach Spleen Lesser omentum Liver Lienorenal ligament Dorsal mesogastrium Dorsal pancreas Falciform ligament A Um ilical vein Falciform ligament B Omental ursa Gastrolienal ligament Figure 13.10 A. The positions of the spleen, stomach, and pancreas at the end of the fth week. Note the position of the spleen and pancreas in the dorsal mesogas trium. B. Position of spleen and stomach at the 11th week. Note formation of the omental ursa or lesser peritoneal sac. Pancreas Lienorenal ligament Adrenal gland Dorsal mesogastrium Spleen Omental ursa Stomach A Liver Lesser omentum Falciform ligament B Parietal peritoneum of ody wall Spleen Gastrolienal ligament Figure 13.11 Transverse sections through the region of the stomach, liver, and s pleen, showing formation of the lesser peritoneal sac, rotation of the stomach, and position of the spleen and tail of the pancreas etween the two leaves of th e dorsal mesogastrium. With further development, the pancreas assumes a retroper itoneal position. 13.11). Lengthening and fusion of the dorsal mesogastrium to the posterior ody wall also determine the nal position of the pancreas. Initially the organ grows i nto the dorsal mesoduodenum, ut eventually its tail extends into the dorsal mes ogastrium (Fig. 13.10A). Since this portion of the dorsal mesogastrium fuses wit h the dorsal ody wall, the tail of the pancreas lies against
Chapter 13: Digestive System 295
this region (Fig. 13.11). Once the posterior leaf of the dorsal mesogastrium and the peritoneum of the posterior ody wall degenerate along the line of fusion, the tail of the pancreas is covered y peritoneum on its anterior surface only a nd therefore lies in a retroperitoneal position. (Organs, such as the pancreas, that are originally covered y peritoneum, ut later fuse with the posterior od y wall to ecome retroperitoneal, are said to e secondarily retroperitoneal.) A s a result of rotation of the stomach a out its anteroposterior axis, the dorsal mesogastrium ulges down (Fig. 13.12). It continues to grow down and forms a do u le-layered sac extending over the transverse colon and small intestinal loops like an apron (Fig. 13.13A). This dou le-leafed apron is the greater omentum; la ter its layers fuse to form a single sheet hanging from the greater curvature of the stomach (Fig. 13.13B). The posterior layer of the greater omentum also fuse s with the mesentery of the transverse colon (Fig. 13.13B ). The lesser omentum and falciform ligament form from the ventral mesogastrium, which itself is deriv ed from mesoderm of the septum transversum. When liver cords grow into the septu m, it thins to form (a) the peritoneum of the liver, ( ) the falciform ligament, extending from the liver to the ventral ody wall, and (c) the lesser omentum, extending from the stomach and upper duodenum to the liver (Figs. 13.14 and 13.1 5). The free margin of the falciform ligament contains the um ilical vein (Fig. 13.10A), which is o literated after irth to form the round ligament of the live r (ligamentum teres hepatis). The free margin of the lesser omentum connecting t he duodenum and liver (hepatoduodenal ligament) contains the ile duct, portal v ein, and hepatic artery (portal triad). This free margin also forms the roof of the epiploic foramen of
Figure 13.12 A. Derivatives h. The dorsal mesogastrium forms part of the order of from the greater curvature
of the dorsal mesentery at the end of the third mont ulges out on the left side of the stomach, where it the omental ursa. B. The greater omentum hangs down of the stomach in front of the transverse colon.
296 Part Two: Special Em ryology Omental ursa Stomach Peritoneum of posterior a dominal wall Pancreas Duodenum M esentery of transverse colon Greater omentum Omental ursa Greater omentum A Small intestinal loop B Figure 13.13 A. Sagittal section showing the relation of the greater omentum, st omach, transverse colon, and small intestinal loops at 4 months. The pancreas an d duodenum have already acquired a retroperitoneal position. B. Similar section as in A, in the new orn. The leaves of the greater omentum have fused with each other and with the transverse mesocolon. The transverse mesocolon covers the duo denum, which fuses with the posterior ody wall to assume a retroperitoneal posi tion. Respiratory diverticulum Stomach Heart Vitelline duct Allantois Hindgut Cloacal mem rane Cloaca Liver ud Duodenum Midgut Septum transversum Liver Larynx Esophagus Stomach Duodenum Primary intestinal loop A B Figure 13.14 A. A 3-mm em ryo (approximately 25 days) showing the primitive gast rointestinal tract and formation of the liver ud. The ud is formed y endoderm lining the foregut. B. A 5-mm em ryo (approximately 32 days). Epithelial liver cords penetrate the mesenchyme of the septum transversum.
Chapter 13: Digestive System 297 Tongue Thyroid Lesser Bare area of liver omentum Dorsal mesogastrium Diaphragm Tracheo ronchial diverticulum Pericardial cavity Septum transversum Liver Falcif orm ligament Gall ladder Esophagus Stomach Pancreas Vitelline duct Allantois Gal l ladder Hindgut Cloacal mem rane Pancreas Duodenum A B Figure 13.15 A. A 9-mm em ryo (approximately 36 days). The liver expands caudall y into the a dominal cavity. Note condensation of mesenchyme in the area etween the liver and the pericardial cavity, foreshadowing formation of the diaphragm from part of the septum transversum. B. A slightly older em ryo. Note the falcif orm ligament extending etween the liver and the anterior a dominal wall and the lesser omentum extending etween the liver and the foregut (stomach and duodenu m). The liver is entirely surrounded y peritoneum except in its contact area wi th the diaphragm. This is the are area of the liver. Winslow, which is the opening connecting the omental ursa (lesser sac) with the rest of the peritoneal cavity (greater sac) (Fig. 13.16). CLINICAL CORRELATES Stomach A normalities Pyloric stenosis occurs when the circular and, to a lesser degree, the longitudinal musculature of the stomach in the region of the pyloru s hypertrophies. One of the most common a normalities of the stomach in infants, pyloric stenosis is elieved to develop during fetal life. There is an extreme narrowing of the pyloric lumen, and the passage of food is o structed, resulting in severe vomiting. In a few cases the pylorus is atretic. Other malformations of the stomach, such as duplications and a prepyloric septum, are rare. DUODENUM The terminal part of the foregut and the cephalic part of the midgut form the d uodenum. The junction of the two parts is directly distal to the origin of the l iver ud (Figs. 13.14 and 13.15). As the stomach rotates, the duodenum takes
298 Part Two: Special Em ryology Liver Falciform ligament Lesser omentum Stomach Esophagus Diaphragm 7th ri Porta hepatis Omental (epiploic) foramen Duodenum Gall ladder Costodiaph ragmatic recess 10th ri 11th costal cartilage Transverse colon appearing in an unusual gap in the greater omentum Transversus a dominis Anastomosis etween right and left gastroomental (epiploic) arteries Greater ome ntum, gastrocolic portion A Figure 13.16 Lesser omentum extending from the liver to the lesser curvature of the stomach (hepatogastric ligament) and to the duodenum (hepatoduodenal ligamen t). In its free margin anterior to the omental foramen (epiploic foramen of Winsl ow) are the hepatic artery, portal vein, and ile duct (portal triad). on the form of a C-shaped loop and rotates to the right. This rotation, together with rapid growth of the head of the pancreas, swings the duodenum from its ini tial midline position to the left side of the a dominal cavity (Figs. 13.10A and 13.17). The duodenum and head of the pancreas press against the dorsal ody wal l, and the right surface of the dorsal mesoduodenum fuses with the adjacent peri toneum. Both layers su sequently disappear, and the duodenum and head of the pan creas ecome xed in a retroperitoneal position. The entire pancreas thus o tains a retroperitoneal position. The dorsal mesoduodenum disappears entirely except i n the region of the pylorus of the stomach, where a small portion of the duodenu m (duodenal cap) retains its mesentery and remains intraperitoneal. During the s econd month, the lumen of the duodenum is o literated y proliferation of cells in its walls. However, the lumen is recanalized shortly thereafter (Fig. 13.18, A and B). Since the foregut is supplied y the celiac artery and the midgut is s upplied y the superior mesenteric artery, the duodenum is supplied y ranches of oth arteries (Fig. 13.14). LIVER AND GALLBLADDER The liver primordium appear s in the middle of the third week as an outgrowth of the endodermal epithelium a t the distal end of the foregut (Figs. 13.14 and
Chapter 13: Digestive System 299 Figure 13.17 Transverse sections through the region of the duodenum at various s tages of development. At rst the duodenum and head of the pancreas are located in the median plane (A), ut later they swing to the right and acquire a retroperi toneal position (B). Figure 13.18 Upper portion of the duodenum showing the solid stage (A) and cavit y formation (B) produced y recanalization. 13.15). This outgrowth, the hepatic diverticulum, or liver ud, consists of rapi dly proliferating cells that penetrate the septum transversum, that is, the meso dermal plate etween the pericardial cavity and the stalk of the yolk sac (Figs. 13.14 and 13.15). While hepatic cells continue to penetrate the septum, the con nection etween the hepatic diverticulum and the foregut (duodenum) narrows, for ming the ile duct. A small ventral outgrowth is formed y the
300 Part Two: Special Em ryology ile duct, and this outgrowth gives rise to the gall ladder and the cystic duct (Figs. 13.15). During further development, epithelial liver cords intermingle wi th the vitelline and um ilical veins, which form hepatic sinusoids. Liver cords differentiate into the parenchyma (liver cells) and form the lining of the ilia ry ducts. Hematopoietic cells, Kupffer cells, and connective tissue cells are de rived from mesoderm of the septum transversum. When liver cells have invaded the entire septum transversum, so that the organ ulges caudally into the a dominal cavity, mesoderm of the septum transversum lying etween the liver and the fore gut and the liver and ventral a dominal wall ecomes mem ranous, forming the les ser omentum and falciform ligament, respectively. Together, having formed the pe ritoneal connection etween the foregut and the ventral a dominal wall, they are known as the ventral mesogastrium (Fig. 13.15). Mesoderm on the surface of the liver differentiates into visceral peritoneum except on its cranial surface (Fig . 13.15B ). In this region, the liver remains in contact with the rest of the or iginal septum transversum. This portion of the septum, which consists of densely packed mesoderm, will form the central tendon of the diaphragm. The surface of the liver that is in contact with the future diaphragm is never covered y perit oneum; it is the are area of the liver (Fig. 13.15). In the 10th week of develo pment the weight of the liver is approximately 10% of the total ody weight. Alt hough this may e attri uted partly to the large num ers of sinusoids, another i mportant factor is its hematopoietic function. Large nests of proliferating cell s, which produce red and white lood cells, lie etween hepatic cells and walls of the vessels. This activity gradually su sides during the last 2 months of int rauterine life, and only small hematopoietic islands remain at irth. The weight of the liver is then only 5% of the total ody weight. Another important functi on of the liver egins at approximately the 12th week, when ile is formed y he patic cells. Meanwhile, since the gall ladder and cystic duct have developed and the cystic duct has joined the hepatic duct to form the ile duct (Fig. 13.15), ile can enter the gastrointestinal tract. As a result, its contents take on a dark green color. Because of positional changes of the duodenum, the entrance of the ile duct gradually shifts from its initial anterior position to a posterio r one, and consequently, the ile duct passes ehind the duodenum (see Figs. 13. 21 and 13.22). Molecular Regulation of Liver Induction All of the foregut endoderm has the pote ntial to express liver-speci c genes and to differentiate into liver tissue. Howev er, this expression is locked y factors produced y surrounding tissues, inclu ding ectoderm, non-cardiac mesoderm, and particularly the notochord (Fig. 13.19) . The action of these inhi itors is locked in the prospective hepatic region y ro last growth factors (FGFs)
Chapter 13: Digestive System 301 Figure 13.19 Diagrams of the cardiac and hepatic forming regions illustrating in duction of liver development. All of the gut endoderm has the potential to form liver tissue, ut this capacity is repressed y inhi itors secreted y neigh ori ng mesoderm, ectoderm, and the notochord. Stimulation of hepatic development is achieved y secretion of ro last growth factor (FGF) y cardiac mesoderm that in hi its activity of the inhi itors, there y specifying the hepatic eld and initiat ing liver development. This interaction demonstrates that not all inductive proc esses are a result of direct signaling y an inducing molecule, ut instead may occur y removal of a repressor signal. secreted y cardiac mesoderm. Thus, the cardiac mesoderm instructs gut endoderm to express liver speci c genes y inhi iting an inhi itory factor of these same gene s. Once this instruction is received, cells in the liver eld differentiate into ot h hepatocytes and iliary cell lineages, a process that is at least partially re gulated y hepatocyte nuclear transcription factors (HNF3 and 4 ). CLINICAL CORRELATES Liver and Gall ladder A normalities Variations in liver lo ulation are common u t not clinically signi cant, Accessory hepatic ducts and duplication of the gall l adder (Fig. 13.20) are also common and usually asymptomatic. However, they ecom e clinically important under pathological conditions. In some cases the ducts, w hich pass through a solid phase in their development, fail to recanalize (Fig. 1 3.20). This defect, extrahepatic iliary atresia, occurs in 1/15,000 live irths . Among
302 Part Two: Special Em ryology Figure 13.20 A. O literation of the ile duct resulting in distention of the gal l ladder and hepatic ducts distal to the o literation. B. Duplication of the gal l ladder. Figure 13.21 Stages in development of the pancreas. A. 30 days (approximately 5 mm). B. 35 days (approximately 7 mm). Initially the ventral pancreatic ud lies close to the liver ud, ut later it moves posteriorly around the duodenum towar d the dorsal pancreatic ud. patients with extrahepatic iliary atresia, 15 to 20% have patent proximal ducts and a correcta le defect, ut the remainder usually die unless they receive a l iver transplant. Another pro lem with duct formation lies within the liver itsel f; it is intrahepatic iliary duct atresia and hypoplasia. This rare a normality (1/100,000 live irths) may e caused y fetal infections. It may e lethal ut usually runs an extended enign course. PANCREAS The pancreas is formed y two uds originating from the endodermal lining of the duodenum (Fig. 13.21). Wherea s the dorsal pancreatic ud is in the dorsal mesentery, the ventral pancreatic ud is close to the ile duct (Fig. 13.21). When the duodenum rotates to the righ t and ecomes C-shaped, the ventral
Chapter 13: Digestive System 303 Figure 13.22 A. Pancreas during the sixth week of development. The ventral pancr eatic ud is in close contact with the dorsal pancreatic ud. B. Fusion of the p ancreatic ducts. The main pancreatic duct enters the duodenum in com ination wit h the ile duct at the major papilla. The accessory pancreatic duct (when presen t) enters the duodenum at the minor papilla. Figure 13.23 Annular pancreas. The ventral pancreas splits and forms a ring arou nd the duodenum, occasionally resulting in duodenal stenosis. pancreatic ud moves dorsally in a manner similar to the shifting of the entranc e of the ile duct (Fig. 13.21). Finally the ventral ud comes to lie immediatel y elow and ehind the dorsal ud (Fig. 13.22). Later the parenchyma and the duc t systems of the dorsal and ventral pancreatic uds fuse (Fig. 13.22B). The vent ral ud forms the uncinate process and inferior part of the head of the pancreas . The remaining part of the gland is derived from the dorsal ud. The main pancr eatic duct (of Wirsung) is formed y the distal part of the dorsal pancreatic du ct and the entire ventral pancreatic duct (Fig. 13.22B ). The proximal part of t he dorsal pancreatic duct either is o literated or persists as a small channel, the accessory pancreatic duct (of Santorini). The main pancreatic duct, together with the ile duct, enters the duodenum at the site of the major papilla; the e ntrance of the accessory duct (when present) is at the site of the minor papilla . In a out 10% of cases the duct system fails to fuse, and the original dou le s ystem persists.
304 Part Two: Special Em ryology In the third month of fetal life, pancreatic islets (of Langerhans) develop from the parenchymatous pancreatic tissue and scatter throughout the pancreas. Insul in secretion egins at approximately the fth month. Glucagon- and somatostatin-se creting cells also develop from parenchymal cells. Splanchnic mesoderm surroundi ng the pancreatic uds forms the pancreatic connective tissue. MOLECULAR REGULAT ION OF PANCREAS DEVELOPMENT Fi ro last growth factor (FGF) and activin (a TGF- fa mily mem er) produced y the notochord repress SHH expression in gut endoderm de stined to form pancreas. As a result, expression of the pancreatic and duodenal homeo ox 1 (PDX) gene, a master gene for pancreatic development, is upregulated. Although all of the downstream effectors of pancreas development have not een determined, it appears that expression of the paired homeo ox genes PAX4 and 6 s pecify the endocrine cell lineage, such that cells expressing oth genes ecome (insulin), (somatostatin), an (pancreatic polypepti e) cells; whereas those exp ressin only PAX6 become (gluc gon) cells. CLINICAL CORRELATES P ncre tic Abnorm lities The ventr l p ncre tic bud consists of two components t h t norm lly fuse nd rot te round the duodenum so th t they come to lie below the dors l p ncre tic bud. Occ sion lly, however, the right portion of the ventr l bud migr tes long its norm l route, but the left migr tes in the opposite di rection. In this m nner, the duodenum is surrounded by p ncre tic tissue, nd n nnul r p ncre s is formed (Fig. 13.23). The m lform tion sometimes constricts the duodenum nd c uses complete obstruction. Accessory p ncre tic tissue m y be nywhere from the dist l end of the esoph gus to the tip of the prim ry intesti n l loop. Most frequently it lies in the mucos of the stom ch nd in Meckels div erticulum, where it m y show ll of the histologic l ch r cteristics of the p nc re s itself. Midgut In the 5-week-old embryo, the midgut is suspended from the dors l bdomin l w ll by short mesentery nd communic tes with the yolk s c by w y of the vi telline duct or yolk st lk (Figs. 13.1 nd 13.15). In the dult the midgut begin s immedi tely dist l to the entr nce of the bile duct into the duodenum (Fig. 13 .15) nd termin tes t the junction of the proxim l two-thirds of the tr nsverse colon with the dist l third. Over its entire length the midgut is supplied by t he superior mesenteric rtery (Fig. 13.24).
Ch pter 13: Digestive System 305 Lung bud Liver Celi c rtery Yolk s c Superior mesenteric rtery Inferior mesenteric rtery Clo c Figure 13.24 Embryo during the sixth week of development, showing blood supply t o the segments of the gut nd form tion nd rot tion of the prim ry intestin l l oop. The superior mesenteric rtery forms the xis of this rot tion nd supplies the midgut. The celi c nd inferior mesenteric rteries supply the foregut nd hindgut, respectively. Stom ch Duodenum Ceph lic limb of prim ry intestin l loop Cec l bud Superior mesenteric rtery Sm ll intestine Tr nsverse colon Vitelline duct A C ud l limb of prim ry intestin l loop B Figure 13.25 A. Prim ry intestin l loop before rot tion (l ter l view). The supe rior mesenteric rtery forms the xis of the loop. Arrow, counterclockwise rot t ion. B. Simil r view s in A, showing the prim ry intestin l loop fter 180 count erclockwise rotation. The transverse colon passes in front of the duodenum. Development of the midgut is characterized y rapid elongation of the gut and it s mesentery, resulting in formation of the primary intestinal loop (Figs. 13.24 and 13.25). At its apex, the loop remains in open connection with the yolk sac y way of the narrow vitelline duct (Fig. 13.24). The cephalic lim of the loop d evelops into the distal part of the duodenum, the jejunum, and
306 Part Two: Special Em ryology Diaphragm Liver Esophagus Falciform ligament Lesser omentum Gall ladder Stomach Cecum Duodenum Vitelline duct Descending colon Allantois Jejunoileal loops A Cloacal mem rane Rectum H L M M H L B C Figure 13.26 Um ilical herniation of the intestinal loops in an em ryo of approx imately 8 weeks (crown-rump length, 35 mm). Coiling of the small intestinal loop s and formation of the cecum occur during the herniation. The rst 90 of rotation o ccurs during herniation; the remaining 180 occurs during the return of the gut to the (continues on page 307)
Chapter 13: Digestive System 307 part of the ileum. The caudal lim ecomes the lower portion of the ileum, the c ecum, the appendix, the ascending colon, and the proximal two-thirds of the tran sverse colon. PHYSIOLOGICAL HERNIATION Development of the primary intestinal loop is character ized y rapid elongation, particularly of the cephalic lim . As a result of the rapid growth and expansion of the liver, the a dominal cavity temporarily ecome s too small to contain all the intestinal loops, and they enter the extraem ryon ic cavity in the um ilical cord during the sixth week of development (physiologi cal um ilical herniation) (Fig. 13.26). ROTATION OF THE MIDGUT Coincident with growth in length, the primary intestinal loop rotates around an axis formed y the superior mesenteric artery (Fig. 13.25 ). When viewed from the front, this rotation is counterclockwise, and it amounts to approximately 270 when it is complete (Figs. 13.24 and 13.25). Even during ro tation, elongation of the small intestinal loop continues, and the jejunum and i leum form a num er of coiled loops (Fig. 13.26). The large intestine likewise le ngthens considera ly ut does not participate in the coiling phenomenon. Rotatio n occurs during herniation (a out 90 ) as well as during return of the intestinal loops into the a dominal cavity (remaining 180 ) (Fig. 13.27). RETRACTION OF HER NIATED LOOPS During the 10th week, herniated intestinal loops egin to return to the a dominal cavity. Although the factors responsi le for this return are not precisely known, it is thought that regression of the mesonephric kidney, reduce d growth of the liver, and expansion of the a dominal cavity play important role s. The proximal portion of the jejunum, the rst part to reenter the a dominal cav ity, comes to lie on the left side (Fig. 13.27A). The later returning loops grad ually settle more and more to the right. The cecal ud, which appears at a out t he sixth week as a small conical dilation of the caudal lim of the a dominal cavity in the third month. B. Scanning electron micrograph of a latera l view of a mouse em ryo at approximately the same stage as in A, with the ody wall and amnion removed. The heart (H) occupies most of the thoracic region and the liver (L) most of the a domen. Herniated midgut (M) is just eginning to coi l and protrudes from the a domen. C. Frontal view of the em ryo in B. Note the e xtreme size of the liver, which is serving a hematopoietic function at this time , and the initial rotation of the herniated midgut. The diaphragm etween the he art and liver has een removed.
308 Part Two: Special Em ryology Transverse colon Liver Transverse colon Cecal
Aorta Stomach Hepatic flexure Ascending colon Duodenum Vitelline duct Jejunoileal loops Cecum Descending colon Appendix Sigmoid A B Figure 13.27 A. Anterior view of the intestinal loops after 270 counterclockwise rotation. Note the coiling of the small intestinal loops and the position of the cecal ud in the right upper quadrant of the a domen. B. Similar view as in A, with the intestinal loops in their nal position. Displacement of the cecum and ap pendix caudally places them in the right lower quadrant of the a domen. Cecal ud Appendix Cecum Ascending colon Ileum Tenia Cecum A Vitelline duct B Jejunoileal loops Appendix C Figure 13.28 Successive stages in development of the cecum and appendix. A. 7 we eks. B. 8 weeks. C. New orn. primary intestinal loop, is the last part of the gut to reenter the a dominal ca vity. Temporarily it lies in the right upper quadrant directly elow the right l o e of the liver (Fig. 13.27A). From here it descends into the right iliac fossa , placing the ascending colon and hepatic exure on the right side of the a domina l cavity (Fig. 13.27B). During this process the distal end of the cecal ud form s a narrow diverticulum, the appendix (Fig. 13.28). Since the appendix develops during descent of the colon, its nal position frequently is posterior to the cecu m or colon. These positions of the appendix are called retrocecal or retrocolic, respectively (Fig. 13.29).
ud
Chapter 13: Digestive System 309 Figure 13.29 Various positions of the appendix. In a out 50% of cases the append ix is retrocecal or retrocolic. Dorsal mesogastrium fused with a dominal wall Dorsal mesoduodenum fused with a d ominal wall Ascending colon Dorsal mesogastrium fused with posterior Greater a d ominal wall curvature Lesser curvature Dorsal mesoduodenum fused with posterior a dominal wall Greater omentum Cut edge of greater omentum Transverse mesocolon A Mesocolon fused with a dominal wall Sigmoid B Mesocolon fused with a dominal wall Mesentery proper Sigmoid mesocolon Figure 13.30 Frontal view of the intestinal loops with (A) and after removal of (B) the greater omentum. Gray areas, parts of the dorsal mesentery that fuse wit h the posterior a dominal wall. Note the line of attachment of the mesentery pro per. MESENTERIES OF THE INTESTINAL LOOPS The mesentery of the primary intestinal loop , the mesentery proper, undergoes profound changes with rotation and coiling of the owel. When the caudal lim of the loop moves to the right side of the a dom inal cavity, the dorsal mesentery twists around the origin of the superior mesen teric artery (Fig. 13.24). Later, when the ascending and descending portions of the colon o tain their de nitive positions, their mesenteries press against the pe ritoneum of the posterior a dominal wall (Fig. 13.30). After fusion of these lay ers, the
310 Part Two: Special Em ryology ascending and descending colons are permanently anchored in a retroperitoneal po sition. The appendix, lower end of the cecum, and sigmoid colon, however, retain their free mesenteries (Fig. 13.30B). The fate of the transverse mesocolon is d ifferent. It fuses with the posterior wall of the greater omentum (Fig. 13.13) ut maintains its mo ility. Its line of attachment nally extends from the hepatic e xure of the ascending colon to the splenic exure of the descending colon (Fig. 13 .30B ). The mesentery of the jejunoileal loops is at rst continuous with that of the ascending colon (Fig. 13.12A). When the mesentery of the ascending mesocolon fuses with the posterior a dominal wall, the mesentery of the jejunoileal loops o tains a new line of attachment that extends from the area where the duodenum ecomes intraperitoneal to the ileocecal junction (Fig. 13.30B). CLINICAL CORRELATES A normalities of the Mesenteries Normally the ascending colon, except for its mo st caudal part (approximately 1 inch), fuses to the posterior a dominal wall and is covered y peritoneum on its anterior surface and sides. Persistence of a po rtion of the mesocolon gives rise to a mo ile cecum. In the most extreme form, t he mesentery of the ascending colon fails to fuse with the posterior ody wall. Such a long mesentery allows a normal movements of the gut or even volvulus of t he cecum and colon. Similarly, incomplete fusion of the mesentery with the poste rior ody wall may give rise to retrocolic pockets ehind the ascending mesocolo n. A retrocolic hernia is entrapment of portions of the small intestine ehind t he mesocolon. Body Wall Defects Omphalocele (Fig. 13.31, A and B) involves herni ation of a dominal viscera through an enlarged um ilical ring. The viscera, whic h may include liver, small and large intestines, stomach, spleen, or gall ladder , are covered y amnion. The origin of the defect is a failure of the owel to r eturn to the ody cavity from its physiological herniation during the 6th to 10t h weeks. Omphalocele occurs in 2.5/10,000 irths and is associated with a high r ate of mortality (25%) and severe malformations, such as cardiac anomalies (50%) and neural tu e defects (40%). Approximately half of live- orn infants with omp halocele have chromosomal a normalities. Gastroschisis (Fig. 13.31C ) is a herni ation of a dominal contents through the ody wall directly into the amniotic cav ity. It occurs lateral to the um ilicus usually on the right, through a region w eakened y regression of the right um ilical vein, which normally disappears. Vi scera are not covered y peritoneum or amnion, and the owel may e damaged y e xposure to amniotic uid. Gastroschisis occurs in 1/10,000 irths ut is increasin g in frequency, especially among young women; this increase may e related to co caine use.
Chapter 13: Digestive System 311 C Figure 13.31 A. Omphalocele showing failure of the intestinal loops to return to the ody cavity after physiological herniation. The herniated loops are covered y amnion. B. Omphalocele in a new orn. C. New orn with gastroschisis. Loops of owel return to the ody cavity ut herniate again through the ody wall, usual ly to the right of the um ilicus in the region of the regressing right um ilical vein. Unlike omphalocele, the defect is not covered y amnion. Unlike omphalocele, gastroschisis is not associated with chromosome a normalitie s or other severe defects, so the survival rate is excellent. Volvulus (rotation of the owel) resulting in a compromised lood supply may, however, kill large regions of the intestine and lead to fetal death. Vitelline Duct A normalities I n 2 to 4% of people, a small portion of the vitelline duct persists, forming an outpocketing of the ileum, Meckels diverticulum or ileal diverticulum (Fig. 13.32 A). In the adult, this diverticulum, approximately 40 to 60 cm from the ileoceca l valve on the antimesenteric order of the ileum, does not usually
312 Part Two: Special Em ryology Figure 13.32 Remnants of the vitelline duct. A. Meckels, or ileal, diverticulum c om ined with rous cord (vitelline ligament). B. Vitelline cyst attached to the u m ilicus and wall of the ileum y vitelline ligaments. C. Vitelline stula connect ing the lumen of the ileum with the um ilicus. cause any symptoms. However, when it contains heterotopic pancreatic tissue or g astric mucosa, it may cause ulceration, leeding, or even perforation. Sometimes oth ends of the vitelline duct transform into rous cords, and the middle porti on forms a large cyst, an enterocystoma, or vitelline cyst (Fig. 13.32B). Since the rous cords traverse the peritoneal cavity, intestinal loops may twist around the rous strands and ecome o structed, causing strangulation or volvulus. In a nother variation the vitelline duct remains patent over its entire length, formi ng a direct communication etween the um ilicus and the intestinal tract. This a normality is known as an um ilical stula, or vitelline stula (Fig. 13.32C ). A fe cal discharge may then e found at the um ilicus. Gut Rotation Defects A normal rotation of the intestinal loop may result in twisting of the intestine (volvulu s) and a compromise of the lood supply. Normally the primary intestinal loop ro tates 270 counterclockwise. Occasionally, however, rotation amounts to 90 only. Wh en this occurs, the colon and cecum are the rst portions of the gut to return fro m the um ilical cord, and they settle on the left side of the a dominal cavity ( Fig. 13.33A). The later returning loops then move more and more to the right, re sulting in left-sided colon. Reversed rotation of the intestinal loop occurs whe n the primary loop rotates 90 clockwise. In this a normality the transverse colon passes ehind the duodenum (Fig. 13.33B) and lies ehind the superior mesenteri c artery. Duplications of intestinal loops and cysts may occur anywhere along th e length of the gut tu e. They are most frequently found in the region of the il eum, where they may vary from a long segment to a small diverticulum. Symptoms u sually occur early in life, and 33% are associated with other defects, such as i ntestinal atresias, imperforate anus, gastroschisis, and omphalocele. Their orig in is unknown, although they may result from a normal proliferations of gut pare nchyma.
Chapter 13: Digestive System 313 Duodenum Duodenum Ascending colon Transverse colon Jejunoileal loops Transverse colon Descending colon Jejunoileal loops A Cecum B Descending colon Figure 13.33 A. A normal rotation of the primary intestinal loop. The n the left side of the a domen, and the small intestinal loops are on The ileum enters the cecum from the right. B. The primary intestinal tated 90 clockwise (reversed rotation). The transverse colon passes odenum.
Gut Atresias and Stenoses Atresias and stenoses may occur anywhere along the int estine. Most occur in the duodenum, fewest occur in the colon, and equal num ers occur in the jejunum and ileum (1/1500 irths). Atresias in the upper duodenum are pro a ly due to a lack of recanalization (Fig. 13.18). From the distal porti on of the duodenum caudally, however, stenoses and atresias are most likely caus ed y vascular accidents. These accidents may e caused y malrotation, volvulus, gastroschisis, omphalocele, and other factors. As a result, lood supply to a re gion of the owel is compromised and a segment dies, resulting in narrowing or c omplete loss of that region. In 50% of cases a region of the owel is lost, and in 20% a rous cord remains (Fig. 13.34, A and B). In another 20% there is narrow ing, with a thin diaphragm separating the larger and smaller pieces of owel (Fi g. 13.34C ). Stenoses and multiple atresias account for the remaining 10% of the se defects, with a frequency of 5% each (Fig. 13.34D). Apple peel atresia accoun ts for 10% of atresias. The atresia is in the proximal jejunum, and the intestin e is short, with the portion distal to the lesion coiled around a mesenteric rem nant (Fig. 13.35). Ba ies with this defect have low irth weight and other a nor malities. Hindgut The hindgut gives rise to the distal third of the transverse colon, the descending colon, the sigmoid, the rectum, and the upper part of the anal canal. The endoderm of the hindgut also forms the internal lining of the ladder and u rethra (see Chapter 14).
colon is o the right. loop is ro ehind the du
314 Part Two: Special Em ryology A B C D Figure 13.34 The most commonly occurring owel atresias and stenoses. A, the mos t common, occurs in 50 % of cases; B and C occur in 20 % each of cases, and D oc curs in 5 % of cases. Most are caused y vascular accidents; those in the upper duodenum may e caused y a lack of recanalization. Atresias (A,B, and C) occur in 95 % of cases, and stenoses (D), in only 5 %. Figure 13.35 Apple peel atresia, which occurs in the jejunum and accounts for 10 % of owel atresias. The affected portion of the owel is coiled around a remna nt of mesentery. The terminal portion of the hindgut enters into the posterior region of the cloa ca, the primitive anorectal canal; the allantois enters into the anterior portio n, the primitive urogenital sinus (Fig 13.36A). The cloaca itself is an endoderm -lined cavity covered at its ventral oundary y surface ectoderm. This oundary etween the endoderm and the ectoderm forms the cloacal mem rane (Fig. 13.36). A layer of mesoderm, the urorectal septum, separates
Chapter 13: Digestive System 315 Allantois Primitive urogenital sinus Urogenital mem rane Urinary ladder Cloaca Perineum Urorectal septum Hindgut Anal mem rane Anorectal canal A Cloacal mem rane B C Figure 13.36 Cloacal region in em ryos at successive stages of development. A. T he hindgut enters the posterior portion of the cloaca, the future anorectal cana l; the allantois enters the anterior portion, the future urogenital sinus. The u rorectal septum is formed y merging of the mesoderm covering the allantois and the yolk sac (Fig. 13.1 D). The cloacal mem rane, which forms the ventral ounda ry of the cloaca, is composed of ectoderm and endoderm. B. As caudal folding of the em ryo continues, the urorectal septum moves closer to the cloacal mem rane, although it never contacts this structure. C. Lengthening of the genital tu erc le pulls the urogenital portion of the cloaca anteriorly; reakdown of the cloac al mem rane creates an opening for the hindgut and one for the urogenital sinus. The tip of the urorectal septum forms the perineal ody. D. Histological sectio n through the cloacal region of a 6-week human em ryo similar to that depicted i n B. The cloaca (cl ) has a smaller posterior region at the opening of the hindg ut (hg) and a larger anterior region, the urogenital sinus (us). The urorectal s eptum (urs) partially divides the two regions, and the cloacal mem rane (cm) for ms a oundary at the caudal limit of the cloacal cavity; gt, genital tu ercle. E . Histological section though the cloacal region of a 7-week human em ryo simila r to C. The urorectal septum (urs) lies close to the cloacal mem rane (cm), whic h is just eginning to reak down, leaving the anal opening (ao) for the hindgut (hg) and a separate opening for the urogenital sinus (us). The tip of the urore ctal septum will form the perineal ody. Growth of the genital tu ercle (gt) wil l change the shape of the urogenital sinus, which will eventually e closed y f usion of the urethral folds in the male. In the female the opening will remain a s the vesti ule to the vagina and urethra (see Chapter 14).
316 Part Two: Special Em ryology the region etween the allantois and hindgut. This septum is derived from the me rging of mesoderm covering the yolk sac and surrounding the allantois (Figs. 13. 1 and 13.36). As the em ryo grows and caudal folding continues, the tip of the u rorectal septum comes to lie close to the cloacal mem rane, although the two str uctures never make contact (Figs. 13.36, B and D). At the end of the seventh wee k, the cloacal mem rane ruptures, creating the anal opening for the hindgut and a ventral opening for the urogenital sinus. Between the two, the tip of the uror ectal septum forms the perineal ody (13.36C and E ). At this time, proliferatio n of ectoderm closes the caudalmost region of the anal canal. During the ninth w eek, this region recanalizes. Thus, the caudal part of the anal canal originates in the ectoderm, and it is supplied y the inferior rectal arteries, ranches o f the internal pudendal arteries. The cranial part of the anal canal originates in the endoderm and is supplied y the superior rectal artery, a continuation of the inferior mesenteric artery, the artery of the hindgut. The junction etween the endodermal and ectodermal regions of the anal canal is delineated y the pe ctinate line, just elow the anal columns. At this line, the epithelium changes from columnar to strati ed squamous epithelium. CLINICAL CORRELATES Hindgut A normalities Rectoanal atresias, and stulas, which occur in 1/5000 live irths, are caused y a normalities in formation of the cloaca. Thus, if the pos terior portion of the cloaca is too small and consequently the posterior cloacal mem rane is short, the opening of the hindgut shifts anteriorly. If the defect in the cloaca is small, the shift is small, causing a low opening of the hindgut into the vagina or urethra (Figs. 13.37, A and B ). If the posterior region of the cloaca is very small, the location of the hindgut opening shifts more anteri orly to a higher location (Fig. 13.37C ). Thus, rectoanal atresias and stulas are due to ectopic positioning of the anal opening and not to defects in the urorec tal septum. Low lesions are twice as common as high ones, with the intermediate variety eing the least common. Approximately 50% of children with rectoanal atr esias have other irth defects. With imperforate anus, there is no anal opening. This defect occurs ecause of a lack of recanalization of the lower portion of the anal canal (Fig. 13.37D). Congenital megacolon is due to an a sence of paras ympathetic ganglia in the owel wall (aganglionic megacolon or Hirschsprung dise ase). These ganglia are derived from neural crest cells that migrate from the ne ural folds to the wall of the owel. Mutations in the RET gene, a tyrosine kinas e receptor involved in crest cell migration (see Chapter 19), can result in cong enital megacolon. In most cases the rectum is involved, and in 80% the defect ex tends to the midpoint of the sigmoid. In only 10 to 20% are the transverse and r ight-side colonic segments involved, and in 3% the entire colon is affected.
Chapter 13: Digestive System 317 C D Figure 13.37 A. Normal development of the cloacal region at 7 weeks. The anterio r portion of the cloaca (cl ) forms the urogenital sinus (us); the posterior por tion extends to the opening of the hindgut (hg). The cloacal mem rane (cm) close s the cloaca and extends posteriorly eneath the end of the hindgut. Urs, urorec tal septum; nt, neural tu e; gt, genital tu ercle. B. The cloacal region of a 7week em ryo showing a decrease in the size of the posterior portion of the cloac a and shortening of the cloacal mem rane (arrow). Such a defect causes ectopic p lacement of the anal opening into the urogenital sinus (arrowhead ) and a low ur orectal stula. C. High urorectal stula resulting from a large decrease in size of the posterior portion of the cloaca and cloacal mem rane that shifts the opening of the hindgut further anteriorly. D. Imperforate anus. The anal canal fails to recanalize, leaving a diaphragm etween the upper and lower portions of the ana l canal.
318 Part Two: Special Em ryology Summary The epithelium of the digestive system and the parenchyma of its derivat ives originate in the endoderm; connective tissue, muscular components, and peri toneal components originate in the mesoderm. Differentiation of the gut and its derivatives depends upon reciprocal interactions etween the gut endoderm (epith elium) and its surrounding mesoderm. HOX genes in the mesoderm are induced y so nic hedgehog (SHH) secreted y gut endoderm and regulate the craniocaudal organi zation of the gut and its derivatives. The gut system extends from the uccophar yngeal mem rane to the cloacal mem rane (Fig. 13.1) and is divided into the phar yngeal gut, foregut, midgut, and hindgut. The pharyngeal gut gives rise to the p harynx and related glands (see Chapter 15). The foregut gives rise to the esopha gus, the trachea and lung uds, the stomach, and the duodenum proximal to the en trance of the ile duct. In addition, the liver, pancreas, and iliary apparatus develop as outgrowths of the endodermal epithelium of the upper part of the duo denum (Fig. 13.15). Since the upper part of the foregut is divided y a septum ( the tracheoesophageal septum) into the esophagus posteriorly and the trachea and lung uds anteriorly, deviation of the septum may result in a normal openings etween the trachea and esophagus. The epithelial liver cords and iliary system growing out into the septum transversum (Fig. 13.15) differentiate into parenchy ma. Hematopoietic cells (present in the liver in greater num ers efore irth th an afterward), the Kupffer cells, and connective tissue cells originate in mesod erm. The pancreas develops from a ventral ud and a dorsal ud that later fuse t o form the de nitive pancreas (Figs. 13.21 and 13.22). Sometimes, the two parts su rround the duodenum (annular pancreas), causing constriction of the gut (Fig. 13 .23). The midgut forms the primary intestinal loop (Fig. 13.24), gives rise to t he duodenum distal to the entrance of the ile duct, and continues to the juncti on of the proximal two-thirds of the transverse colon with the distal third. At its apex the primary loop remains temporarily in open connection with the yolk s ac through the vitelline duct. During the sixth week, the loop grows so rapidly that it protrudes into the um ilical cord (physiological herniation) (Fig. 13.26 ). During the 10th week, it returns into the a dominal cavity. While these proce sses are occurring, the midgut loop rotates 270 counterclockwise (Fig. 13.25). Re mnants of the vitelline duct, failure of the midgut to return to the a dominal c avity, malrotation, stenosis, and duplications of parts of the gut are common a normalities. The hindgut gives rise to the region from the distal third of the t ransverse colon to the upper part of the anal canal; the distal part of the anal canal originates from ectoderm. The hindgut enters the posterior region of the cloaca (future anorectal canal), and the allantois enters the anterior region (f uture urogenital sinus). Breakdown of the cloacal mem rane covering this area pr ovides communication to the exterior for the anus and urogenital sinus. A normal ities in the size of the posterior region of the cloaca shift the entrance of th e anus
Chapter 13: Digestive System 319 anteriorly, causing rectovaginal and rectourethral 36 and 13.37). stulas and atresias (Figs. 13.
SUGGESTED READING Apelqvist A, Ahlgreen U, Edlund H: Sonic hedgehog directs spec ialized mesoderm differentiation in the intestines and pancreas. Curr Biol 7:801 , 1997. Brassett C, Ellis H: Transposition of the viscera. Clin Anat 4:139, 1991 . Duncan SA: Transcriptional regulation of liver development. Dev Dynam 219:131, 2000. Galloway J: A handle on handedness. Nature (Lond) 346:223, 1990. Gualdi R , Bossard P, Zheng M, Hamada Y, Coleman JR, Zaret KS: Hepatic speci cation of the gut endoderm in vitro: cell signaling and transcriptional control. Genes Dev 10: 1670, 1996. Kluth D, Hillen M, Lam recht W: The principles of normal and a norma l hindgut development. J Pediatr Surg 30:1143, 1995. Nievelstein RAJ, Van der We rff JFA, Ver eek FJ, Vermeij-Keers C: Normal and a normal development of the ano rectum in human em ryos. Teratology 57:70, 1998. Severn CB: A morphological stud y of the development of the human liver: 1. Development of the hepatic diverticu lum. Am J Anat 131:133, 1971. Severn CB: A morphological study of the developmen t of the human liver: 2. Esta lishment of liver parenchyma, extrahepatic ducts, and associated venous channels. Am J Anat 133:85, 1972. Sosa-Pineda B, Chowdhury K, Torres M, Oliver G, Gruss P: The Pax 4 gene is essential for differentiation of insulin producing cells in the mammalian pancreas. Nature 386:399, 1997. St. Onge L, Sosa-Pineda B, Chowdhury K, Mansouri A, Gruss P: Pax 6 is required for differentiation of glucagon-producing cells in mouse p ncre s, N ture 387:406, 1 997. Stevenson RE, H ll JG, Goodm n RM (eds): Hum n M lform tions nd Rel ted An om lies. New York, Oxford University Press, 1993. Torfs C, Curry C, Roeper P: G stroschisis. J Pedi tr 116:1, 1990. Vellguth S, v n G udecker B, Muller-Hermelin k HK: The development of the hum n spleen. Cell Tissue Res 242:579, 1985. Yokoh Y: Differenti tion of the dors l mesentery in m n. Act An t 76:56, 1970.
Pro lems to Solve 1. Prenatal ultrasound showed polyhydramnios at 36 weeks, and at irth the infant had excessive uids in its mouth and dif culty reathing. What irth defect might cause these conditions? 2. Prenatal ultrasound at 20 weeks rev ealed a midline mass that appeared to contain intestines and was mem rane ound. What diagnosis would you make, and what would e the prognosis for this infant? 3. At irth a a y girl has meconium in her vagina and no anal opening. What ty pe of irth defect does she have, and what was its em ryological origin?
ch pter 14 Urogenit l System Function lly the urogenit l system c n be divided into two entirely different co mponents: the urin ry system nd the genit l system. Embryologic lly nd n tomi c lly, however, they re intim tely interwoven. Both develop from common mesod erm l ridge (intermedi te mesoderm) long the posterior w ll of the bdomin l c vity, nd initi lly the excretory ducts of both systems enter common c vity, t he clo c . Urin ry System KIDNEY SYSTEMS Three slightly overl pping kidney syste ms re formed in cr ni l to c ud l sequence during intr uterine life in hum ns : the pronephros, mesonephros, nd met nephros. The rst of these systems is rudim ent ry nd nonfunction l; the second m y function for short time during the e rly fet l period; the third forms the perm nent kidney. Pronephros At the beginn ing of the fourth week, the pronephros is represented by 7 to 10 solid cell grou ps in the cervic l region (Figs. 14.1 nd 14.2). These groups form vestigi l exc retory units, nephrotomes, th t regress before more c ud l ones re formed. By t he end of the fourth week, ll indic tions of the pronephric system h ve dis ppe red. 321
322 P rt Two: Speci l Embryology
Nephric tubule Som tic mesoderm Nephrotome Intr embryonic c vity Spl nchnic meso derm Extern l glomerulus Endoderm A B Figure 14.1 Tr nsverse sections through embryos t v rious st ges of development showing form tion of nephric tubules. A. 21 d ys. B. 25 d ys. Note form tion of extern l nd intern l glomeruli nd the open connection between the intr embryo nic c vity nd the nephric tubule. Mesonephros The mesonephros nd mesonephric ducts re derived from intermedi te mesoderm from upper thor cic to upper lumb r (L3) segments (Fig. 14.2). E rly in the fourth week of development, during regression of the pronephric system, the rst excretory tubules of the mesonephros ppe r. They lengthen r pidly, form n S-sh ped loop, nd cquire tuft of c pill ries th t will form glomerulus t their medi l extremity (Fig. 14.3A). Around the glomerulus the tubules form Bowm ns c psule, nd together these structures constitute ren l corpuscle. L ter ll y the tubule enters the longitudin l collecting duct known s the mesonephric or wolf n duct (Figs. 14.2 nd 14.3). In the middle of the second month the mesonep hros forms l rge ovoid org n on e ch side of the midline (Fig. 14.3). Since th e developing gon d is on its medi l side, the ridge formed by both org ns is kno wn s the urogenit l ridge (Fig. 14.3). While c ud l tubules re still different i ting, cr ni l tubules nd glomeruli show degener tive ch nges, nd by the end of the second month the m jority h ve dis ppe red. In the m le few of the c ud l tubules nd the mesonephric duct persist nd p rticip te in form tion of the genit l system, but they dis ppe r in the fem le (see Genit l System; p. 337).
P r xi l mesoderm Intermedi te mesoderm Somite Dors l ort
Intern l glomerulus
Ch pter 14: Urogenit l System 323 Segmented intermedi te mesoderm (pronephric system) Vestigi l pronephric system Vitelline duct Unsegmented intermedi te mesoderm (mesonephric system)
Mesonephric excretory units Mesonephric duct Mesonephric duct A Unsegmented mesoderm (met nephric system) B Ureteric bud Figure 14.2 A. Rel tionship of the intermedi te mesoderm of the pronephric, meso nephric, nd met nephric systems. In cervic l nd upper thor cic regions interme di te mesoderm is segmented; in lower thor cic, lumb r, nd s cr l regions it fo rms solid, unsegmented m ss of tissue, the nephrogenic cord. Note the longitud in l collecting duct, formed initi lly by the pronephros but l ter by the mesone phros. B. Excretory tubules of the pronephric nd mesonephric systems in 5-wee k-old embryo. Met nephros: The De nitive Kidney The third urin ry org n, the met nephros, or per m nent kidney, ppe rs in the fth week. Its excretory units develop from met neph ric mesoderm (Fig. 14.4) in the s me m nner s in the mesonephric system. The de velopment of the duct system differs from th t of the other kidney systems. Coll ecting System. Collecting ducts of the perm nent kidney develop from the ureteri c bud, n outgrowth of the mesonephric duct close to its entr nce to the clo c (Fig. 14.4). The bud penetr tes the met nephric tissue, which is molded over its dist l end s c p (Fig. 14.4). Subsequently the bud dil tes, forming the prim itive ren l pelvis, nd splits into cr ni l nd c ud l portions, the future m jo r c lyces (Fig. 14.5, A nd B ). E ch c lyx forms two new buds while penetr ting the met nephric tissue. These buds continue to subdivide until 12 or more gener tions of tubules h ve formed (Fig. 14.5). Me nwhile, t the periphery more tubu les form until the
All ntois Clo c
Urogenit l mesentery Excretory tubule of mesonephros Mesonephric duct P r mesonephric duct Mesentery Gut Mesonephros Glomerulus Gon d Bowm ns c psule A Vitelline duct All ntois Mesonephric duct P r mesonephric duct Gon d B
C Figure 14.3 A. Tr nsverse section through the urogenit l ridge in the lower thor cic region of 5-week embryo showing form tion of n excretory tubule of the m esonephric system. Note the ppe r nce of Bowm ns c psule nd the gon d l ridge. The mesonephros nd gon d re tt ched to the posterior bdomin l w ll by bro d urogenit l mesentery. B. Rel tion of the gon d nd the mesonephros. Note the s ize of the mesonephros. The mesonephric duct (wolf n duct) runs long the l ter l side of the mesonephros. C. Sc nning electron microgr ph of mouse embryo show ing the genit l ridge ( rrow) nd mesonephric duct ( rrowhe ds).K , kidneys.
Clo c
Ch pter 14: Urogenit l System 325 Hindgut All ntois Mesonephric tissue Mesonephric duct
Figure 14.4 Rel tion of the hindgut nd clo c t the end of the eteric bud penetr tes the met nephric mesoderm (bl stem ).
Figure 14.5 Development of the ren l pelvis, c lyces, nd collecting tubules of the met nephros. A. 6 weeks. B. At the end of the sixth week. C. 7 weeks, D. New born. Note the pyr mid form of the collecting tubules entering the minor c lyx. end of the fth month. The tubules of the second order enl rge nd bsorb those of the third nd fourth gener tions, forming the minor c lyces of the ren l pelvis . During further development, collecting tubules of the fth nd successive gener tions elong te consider bly nd converge on the minor c lyx, forming the ren l p yr mid (Fig. 14.5D). The ureteric bud gives rise to the ureter, the ren l pelvis , the m jor nd minor c lyces, nd pproxim tely 1 million to 3 million collecti ng tubules.
Urorect l septum Clo c Ureteric bud Met nephric bl stem
fth week. The ur
326 P rt Two: Speci l Embryology Figure 14.6 Development of met nephric excretory unit. Arrows, the pl ce where the excretory unit (blue) est blishes n open communic tion with the collecting system (yellow), llowing ow of urine from the glomerulus into the collecting du cts. Excretory System. E ch newly formed collecting tubule is covered t its dist l e nd by met nephric tissue c p (Fig. 14.6A). Under the inductive in uence of the t ubule, cells of the tissue c p form sm ll vesicles, the ren l vesicles, which in turn give rise to sm ll S-sh ped tubules (Fig. 14.6, B nd C ). C pill ries gro w into the pocket t one end of the S nd differenti te into glomeruli. These tu bules, together with their glomeruli, form nephrons, or excretory units. The pro xim l end of e ch nephron forms Bowm ns c psule, which is deeply indented by gl omerulus (Fig. 14.6, C nd D). The dist l end forms n open connection with one of the collecting tubules, est blishing p ss gew y from Bowm ns c psule to the collecting unit. Continuous lengthening of the excretory tubule results in form tion of the proxim l convoluted tubule, loop of Henle, nd dist l convoluted tub ule (Fig. 14.6, E nd F ). Hence, the kidney develops from two sources: ( ) met nephric mesoderm, which provides excretory units; nd (b) the ureteric bud, whic h gives rise to the collecting system. Nephrons re formed until birth, t which time there re pproxim tely 1 million in e ch kidney. Urine production begins e rly in gest tion, soon fter differenti tion of the glomerul r c pill ries, wh ich st rt to form by the
Ch pter 14: Urogenit l System 327 10th week. At birth the kidneys h ve lobul ted ppe r nce, but the lobul tion dis ppe rs during inf ncy s result of further growth of the nephrons, lthoug h there is no incre se in their number. MOLECULAR REGULATION OF KIDNEY DEVELOPME NT As with most org ns, differenti tion of the kidney involves epitheli l mesenc hym l inter ctions. In this ex mple, epithelium of the ureteric bud from the mes onephros inter cts with mesenchyme of the met nephric bl stem (Fig. 14.7). The mesenchyme expresses WT1, tr nscription f ctor th t m kes this tissue competen t to respond to induction by the ureteric bud. WT1 lso regul tes production of gli l-derived neurotrophic f ctor (GDNF) nd hep tocyte growth f ctor (HGF, or s c tter f ctor) by the mesenchyme, nd these proteins stimul te growth of the ure teric buds (Fig. 14.7A). The tyrosine kin se receptors RET, for GDNF, nd MET, f or HGF, re synthesized by the epithelium of the ureteric buds, est blishing sig n ling p thw ys between the two tissues. In turn, the buds induce the mesenchyme vi brobl st growth f ctor-2 (FGF-2) nd bone morphogenetic protein-7 (BMP-7) (F ig. 14.7A). Both of these growth f ctors block poptosis nd stimul te prolifer tion in the met nephric mesenchyme while m int ining production of WT1. Conversi on of the Met nephric tissue c ps WT1 NF W N T4 WT1 P x 2 GD HG F F2
x2 W NT 4 A FG Figure 14.7 Genes involved in differenti tion of the kidney. A. WT1, expressed b y the mesenchyme, en bles this tissue to respond to induction by the ureteric bu d. GDNF nd HGF, lso produced by the mesenchyme, inter ct through their recepto rs, RET nd MET, respectively, in the ureteric bud epithelium, to stimul te grow th of the bud nd m int in the inter ctions. The growth f ctors FGF2 nd BMP7 st imul te prolifer tion of the mesenchyme nd m int in WT1 expression. B. PAX2 nd WNT4, produced by the ureteric bud, c use the mesenchyme to epitheli lize in pr ep r tion for excretory tubule differenti tion. L minin nd type IV coll gen for m b sement membr ne for the epitheli l cells. BM P7
Collecting tubule B
328 P rt Two: Speci l Embryology mesenchyme to n epithelium for nephron form tion is lso medi ted by the ureter ic buds, in p rt through modi c tion of the extr cellul r m trix. Thus bronectin, c oll gen I, nd coll gen III re repl ced with l minin nd type IV coll gen, ch r cteristic of n epitheli l b s l l min (Fig. 14.7B). In ddition, the cell dh esion molecules syndec n nd E-c dherin, which re essenti l for condens tion of the mesenchyme into n epithelium, re synthesized. Regul tory genes for conver sion of the mesenchyme into n epithelium ppe r to involve PAX2 nd WNT4 (Fig. 14.7B). CLINICAL CORRELATES Ren l Tumors nd Defects Wilms tumor is c ncer of the kidneys th t usu lly ffe cts children by 5 ye rs of ge but m y lso occur in the fetus. Wilms tumor is du e to mut tions in the WT1 gene on 11p13, nd it m y be ssoci ted with other bn orm lities nd syndromes. For ex mple, WAGR syndrome is ch r cterized by niridi , hemihypertrophy, nd Wilms tumor. Simil rly, Denys-Dr sh syndrome consists of ren l f ilure, pseudoherm phrodism, nd Wilms tumor. Ren l dyspl si s nd genesi s re spectrum of severe m lform tions th t represent the prim ry dise ses req uiring di lysis nd tr nspl nt tion in the rst ye rs of life. Multicystic dyspl s tic kidney is one ex mple of this group of bnorm lities in which numerous ducts re surrounded by undifferenti ted cells. Nephrons f il to develop nd the uret eric bud f ils to br nch, so th t the collecting ducts never form. In some c ses these defects c use involution of the kidneys nd ren l genesis. Ren l genesi s m y lso occur if the ureteric bud f ils to cont ct nd/or induce the met neph ric mesoderm. Bil ter l ren l genesis, which occurs in 1/10,000 births, results in ren l f ilure. The b by presents with Potter sequence, ch r cterized by nur i , oligohydr mnios (decre sed volume of mniotic uid), nd hypopl stic lungs sec ond ry to the oligohydr mnios. In 85% of c ses other severe defects, including bsence or bnorm lities of the v gin nd uterus, v s deferens, nd semin l vesi cles, ccomp ny this condition. Common ssoci ted defects in other systems inclu de c rdi c nom lies, tr che l nd duoden l tresi s, cleft lip nd p l te, nd br in bnorm lities. In congenit l polycystic kidney (Fig. 14.8) numerous cysts form. It m y be inherited s n utosom l recessive or utosom l domin nt disord er or m y be c used by other f ctors. Autosom l recessive polycystic kidney dise se, which occurs in 1/5,000 births, is progressive disorder in which cysts fo rm from collecting ducts. The kidneys become very l rge, nd ren l f ilure occur s in inf ncy or childhood. In utosom l domin nt polycystic kidney dise se, cyst s form from ll segments of the nephron nd usu lly do not c use ren l f ilure u ntil dulthood. The utosom l domin nt dise se is more common (1/500 to 1/1,000 births) but less progressive th n the utosom l recessive dise se.
Ch pter 14: Urogenit l System 329 Figure 14.8 A. Surf ce view of fet l kidney with multiple cysts ( rrowhe ds) c h r cteristic of polycystic kidney dise se. B. Section of the kidney in A, showi ng multiple cysts. Duplic tion of the ureter results from e rly splitting of the ureteric bud (Fig. 14.9). Splitting m y be p rti l or complete, nd met nephric tissue m y be divi ded into two p rts, e ch with its own ren l pelvis nd ureter. More frequently, however, the two p rts h ve number of lobes in common s result of interming ling of collecting tubules. In r re c ses one ureter opens into the bl dder, nd the other is ectopic, entering the v gin , urethr , or vestibule (Fig. 14.9C ). This bnorm lity results from development of two ureteric buds. One of the buds usu lly h s norm l position, while the bnorm l bud moves down together with the mesonephric duct. Thus it h s low, bnorm l entr nce in the bl dder, ureth r , v gin , or epididym l region.
330 P rt Two: Speci l Embryology D E
POSITION OF THE KIDNEY The kidney, initi lly in the pelvic region, l ter shifts to more cr ni l position in the bdomen. This scent of the kidney is c used b y diminution of body curv ture nd by growth of the body in the lumb r nd s cr l regions
Figure 14.9 A nd B. A complete nd p rti l double f ectopic ureter l openings in the v gin , urethr , omicrogr phs of complete nd p rti l duplic tions of uplic ted hilum; B, bl dder; K , kidneys; ML, medi n
ureter. C. Possible sites o nd vestibule. D nd E. Phot the ureters (U ). Arrows, d umbilic l lig ment.
Ch pter 14: Urogenit l System 331 Gon d All ntois Mesonephros Bl dder Gon d nd remn nts of mesonephros Met nephros Clo c l Ph llus Urogenit l sinus A Met nephric tissue B A K Ureter C Rectum G B T D Figure 14.10 A to C. Ascent of the kidneys. Note the ch nge in position between the mesonephric nd met nephric systems. The mesonephric system degener tes lmo st entirely, nd only few remn nts persist in close cont ct with the gon d. In both m le nd fem le embryos, the gon ds descend from their origin l level to much lower position. D. Sc nning electron microgr ph of mouse embryo showing the kidneys in the pelvis. B, bl dder; K , kidney A, dren l gl nd; G, gon d; T, t il. (Fig. 14.10). In the pelvis the met nephros receives its rteri l supply from pelvic br nch of the ort . During its scent to the bdomin l level, it is v sc ul rized by rteries th t origin te from the ort t continuously higher levels . The lower vessels usu lly degener te, but some m y rem in.
332 P rt Two: Speci l Embryology Adren l gl nd Ren l rtery
Inferior mesenteric rtery Aort Ureter Common ili c rtery Pelvic kidney A Ureters B
CLINICAL CORRELATES Abnorm l Loc tion of the Kidneys During their scent the kidneys p ss through th e rteri l fork formed by the umbilic l rteries, but occ sion lly one of them f ils to do so. Rem ining in
C Figure 14.11 A. Unil ter l pelvic kidney showing the position of the dren l gl nd on the ffected side. B nd C. Dr wing nd photomicrogr ph, respectively, of horseshoe kidneys showing the position of the inferior mesenteric rtery. BW, bl dder w ll; U , ureters.
Inferior ven c v
Aort
Ch pter 14: Urogenit l System 333 the pelvis close to the common ili c rtery, it is known s pelvic kidney (Fig . 14.11A). Sometimes the kidneys re pushed so close together during their p ss ge through the rteri l fork th t the lower poles fuse, forming horseshoe kidn ey (Fig. 14.11, B nd C ). The horseshoe kidney is usu lly t the level of the l ower lumb r vertebr e, since its scent is prevented by the root of the inferior mesenteric rtery (Fig. 14.11B ). The ureters rise from the nterior surf ce o f the kidney nd p ss ventr l to the isthmus in c ud l direction. Horseshoe ki dney is found in 1/600 people. Accessory ren l rteries re common; they derive from the persistence of embryonic vessels th t formed during scent of the kidne ys. These rteries usu lly rise from the ort nd enter the superior or inferi or poles of the kidneys. FUNCTION OF THE KIDNEY The de nitive kidney formed from t he met nephros becomes function l ne r the 12th week. Urine is p ssed into the mniotic c vity nd mixes with the mniotic uid. The uid is sw llowed by the fetus nd recycles through the kidneys. During fet l life, the kidneys re not respons ible for excretion of w ste products, since the pl cent serves this function. B LADDER AND URETHRA During the fourth to seventh weeks of development the clo c divides into the urogenit l sinus nteriorly nd the n l c n l posteriorly (Fig . 14.12) All ntois Mesonephric duct Bl dder Mesonephric duct Primitive urogenit l sinus Ureteric bud Ph llus Ureter Clo c l Hindgut membr ne Urorect l septum Anorect l c n l Perine l body A B C Figure 14.12 Divisions of the clo c into the urogenit l sinus nd norect l c n l. The mesonephric duct is gr du lly bsorbed into the w ll of the urogenit l s inus, nd the ureters enter sep r tely. A. At the end of the fth week. B. 7 weeks . C. 8 weeks.
334 P rt Two: Speci l Embryology (see Ch pter 13). The urorect l septum is l yer of mesoderm between the primit ive n l c n l nd the urogenit l sinus. The tip of the septum will form the per ine l body (Fig. 14.12C ). Three portions of the urogenit l sinus c n be disting uished: The upper nd l rgest p rt is the urin ry bl dder (Fig. 14.13A). Initi l ly the bl dder is continuous with the ll ntois, but when the lumen of the ll n tois is obliter ted, thick brous cord, the ur chus, rem ins nd connects the p ex of the bl dder with the umbilicus (Fig. 14.13B ). In the dult, it is known s the medi n umbilic l lig ment. The next p rt is r ther n rrow c n l, the pel vic p rt of the urogenit l sinus, which in the m le gives rise to the prost tic nd membr nous p rts of the urethr . The l st p rt is the ph llic p rt of the ur ogenit l sinus. It is ttened from side to side, nd s the genit l tubercle grow s, this p rt of the sinus will be pulled ventr lly (Fig. 14.13A). (Development o f the ph llic p rt of the urogenit l sinus differs gre tly between the two sexes : see Genit l System; p. 337.) During differenti tion of the clo c , the c ud l portions of the mesonephric ducts re bsorbed into the w ll of the urin ry bl d der (Fig. 14.14). Consequently, the ureters, initi lly outgrowths from the meson ephric ducts, enter the bl dder sep r tely (Fig. 14.14B). As result of scent of the kidneys, the ori ces of the ureters move f rther cr ni lly; those of the me sonephric ducts move close together to enter the prost tic urethr nd in the m le become the ej cul tory ducts (Fig. 14.14, C nd D). Since both the mesonephri c ducts nd ureters origin te in the mesoderm, the mucos of the bl dder formed by incorpor tion of the ducts (the trigone of the bl dder) is lso mesoderm l. W ith time the mesoderm l lining of the trigone is repl ced by endoderm l epitheli um, so th t n lly the inside of the bl dder is completely lined with endoderm l e pithelium. Urin ry bl dder All ntois Ureter Pelvic p rt of urogenit l sinus Semin l vesicle Ur chus Prost te gl nd Semin l vesicle Ductus deferens Definitive urogenit l sinus Anorect l c n l
A B
Figure 14.13 A. Development of the de nitive urogenit l sinus. B. In into the penile urethr . The prost nd semin l vesicles re formed by
urogenit l sinus into the urin ry bl dder nd the m le the de nitive urogenit l sinus develops te gl nd is formed by buds from the urethr , budding from the ductus deferens.
Penile urethr
Prost tic nd membr nous urethr
Ch pter 14: Urogenit l System 335 Figure 14.14 Dors l views of the bl dder showing the rel tion of the ureters nd mesonephric ducts during development. Initi lly the ureters re formed by n ou tgrowth of the mesonephric duct (A), but with time they ssume sep r te entr n ce into the urin ry bl dder (BD). Note the trigone of the bl dder formed by incor por tion of the mesonephric ducts (C nd D). URETHRA The epithelium of the urethr in both sexes origin tes in the endoderm; the surrounding connective nd smooth muscle tissue is derived from spl nchnic m esoderm. At the end of the third month, epithelium of the prost tic urethr begi ns to prolifer te nd forms number of outgrowths th t penetr te the surroundin g mesenchyme. In the m le, these buds form the prost te gl nd (Fig. 14.13B ). In the fem le, the cr ni l p rt of the urethr gives rise to the urethr l nd p r urethr l gl nds. CLINICAL CORRELATES
Bl dder Defects When the lumen of the intr embryonic portion of the ll ntois pe rsists, ur ch l stul m y c use urine to dr in from the umbilicus (Fig. 14.15A) . If only loc l re of the ll ntois persists, secretory ctivity of its lini ng results in cystic dil tion, ur ch l cyst (Fig. 14.15B). When the lumen in the upper p rt persists, it forms ur ch l sinus. This sinus is usu lly contin uous with the urin ry bl dder (Fig. 14.15C ). Exstrophy of the bl dder (Fig. 14. 16A) is ventr l body w ll defect in which the bl dder mucos is exposed. Episp di s is const nt fe ture (see Fig. 14.33), nd the open urin ry tr ct extends long the dors l spect of the penis through the bl dder to the umbilicus. Exst rophy of the bl dder m y be c used by l ck of mesoderm l migr tion into the re gion between the umbilicus nd genit l tubercle, followed by rupture of the thin l yer of ectoderm. This nom ly is r re, occurring in 2/100,000 live births. Ex strophy of the clo c (Fig. 14.16B) is more severe ventr l body w ll defect in which migr tion of mesoderm to the midline is inhibited nd the t il
336 P rt Two: Speci l Embryology Ur ch l fistul Medi n umbilic l lig ment Ur ch l sinus Ur ch l cyst Urin ry bl dder
A B C Figure 14.15 A. Ur ch l stul . B. Ur ch l cyst. C. Ur ch l sinus. The sinus m y o r m y not be in open communic tion with the urin ry bl dder. Figure 14.16 A. Exstrophy of the bl dder (B.) Arrows, penis with episp di s; S, scrotum. B. Clo c l exstrophy in newborn. C, clo c ; rrows, unfused genit l s wellings. (c ud l) fold f ils to progress. As result, there is n extended thin l yer of ectoderm th t ruptures. The defect includes exstrophy of the bl dder, spin l de fects with or without meningomyelocele, imperfor te nus, nd usu lly omph locel e. Occurrence is r re (1/30,000), nd c us tion h s not been de ned, lthough the defect is ssoci ted with e rly mniotic rupture.
Symphysis Urethr
Ch pter 14: Urogenit l System 337 Genit l System Sex differenti tion is complex process th t involves m ny genes , including some th t re utosom l. The key to sexu l dimorphism is the Y chrom osome, which cont ins the SRY (sex-determining region on Y) gene on its short r m (Yp11). The protein product of this gene is tr nscription f ctor initi ting c sc de of downstre m genes th t determine the f te of rudiment ry sexu l org ns. The SRY protein is the testis-determining f ctor; under its in uence m le deve lopment occurs; in its bsence fem le development is est blished. GONADS Althoug h the sex of the embryo is determined genetic lly t the time of fertiliz tion, the gon ds do not cquire m le or fem le morphologic l ch r cteristics until the seventh week of development. Gon ds ppe r initi lly s p ir of longitudin l ridges, the genit l or gon d l ridges (Fig. 14.17). They re formed by prolifer tion of the epithelium nd condens tion of underlying mesenchyme. Germ cells d o not ppe r in the genit l ridges until the sixth week of development. Primordi l germ cells rst ppe r t n e rly st ge of development mong endoderm cells in the w ll of the yolk s c close to the ll ntois (Fig. 14.18A). They migr te by meboid movement long the dors l mesentery of the hindgut (Fig. 14.18, B nd C ), rriving t the primitive gon ds t the beginning of the fth week nd inv ding the genit l ridges in the sixth week. If they f il to re ch the ridges, the gon ds do not develop. Hence the primordi l germ cells h ve n inductive in uence on development of the gon d into ov ry or testis. Shortly before nd during rriv l of primordi l germ cells, the epithelium of the genit l ridge prolifer tes, nd epitheli l cells penetr te the underlying mesenchyme. Here they form number o f irregul rly sh ped cords, the primitive sex cords (Fig. 14.19). In both m le nd fem le embryos, these cords re connected to surf ce epithelium, nd it is im possible to differenti te between the m le nd fem le gon d. Hence, the gon d is known s the indifferent gon d. Testis If the embryo is genetic lly m le, the p rimordi l germ cells c rry n XY sex chromosome complex. Under in uence of the SRY gene on the Y chromosome, which encodes the testis-determining f ctor, the prim itive sex cords continue to prolifer te nd penetr te deep into the medull to f orm the testis or medull ry cords (Figs. 14.20A, Fig. 14.21). Tow rd the hilum o f the gl nd the cords bre k up into network of tiny cell str nds th t l ter gi ve rise to tubules of the rete testis (Fig. 14.20, A nd B). During further deve lopment, dense l yer
338 P rt Two: Speci l Embryology
Intestin l loop Dors l mesentery Gon d Genit l ridge Mesonephric ridge A B Figure 14.17 A. Rel tion of the genit l ridge nd the mesonephros showing loc ti on of the mesonephric duct. B. Tr nsverse section through the mesonephros nd ge nit l ridge t the level indic ted in A. C. Sc nning electron microgr ph of mo use embryo showing the genit l ridge ( rrows). D. High m gni c tion of the genit l ridge showing the mesonephric duct ( rrow) nd the developing gon d ( rrowhe ds ). of brous connective tissue, the tunic lbugine , sep r tes the testis cords from the surf ce epithelium (Fig. 14.20). In the fourth month, the testis cords beco me horseshoe sh ped, nd their extremities re continuous with those of the rete testis (Fig. 14.20B). Testis cords re now composed of primitive germ cells nd sustent cul r cells of Sertoli derived from the surf ce epithelium of the gl nd .
Mesonephros Mesonephric duct Aort
Excretory tube Glomerulus Mesonephric duct
Ch pter 14: Urogenit l System 339 Foregut Hindgut All ntois Genit l ridge Hindgut Primordi l germ cells He rt Genit l ridge
Mesonephros A Yolk s c B Figure 14.18 A. A 3-week-old embryo showing the primordi l germ cells in the w l l of the yolk s c close to the tt chment of the ll ntois. B. Migr tion l p th of the primordi l germ cells long the w ll of the hindgut nd the dors l mesent ery into the genit l ridge.
Mesonephric duct Primordi l germ cells Prolifer ting body epithelium Primitive sex cords P r meso nephric duct Figure 14.19 Tr nsverse section through the lumb r region of 6-week embryo sho wing the indifferent gon d with the primitive sex cords. Some of the primordi l germ cells re surrounded by cells of the primitive sex cords. Interstiti l cells of Leydig, derived from the origin l mesenchyme of the gon d l ridge, lie between the testis cords. They begin development shortly fter onse t of differenti tion of these cords. By the eighth week of gest tion, Leydig cel ls begin production of testosterone, nd the testis is ble to in uence sexu l dif ferenti tion of the genit l ducts nd extern l genit li . Testis cords rem in so lid until puberty, when they cquire lumen, thus forming the seminiferous tubu les. Once the seminiferous tubules re c n lized, they join the rete testis tubu les, which in turn enter the ductuli efferentes. These efferent ductules re the rem ining p rts of the excretory tubules of the mesonephric system. They link t he rete testis nd the mesonephric or wolf n duct, which becomes the ductus defer ens (Fig. 14.20B ).
Aort
Clo c
340 P rt Two: Speci l Embryology Figure 14.20 A. Tr nsverse section through the testis in the eighth week, showin g the tunic lbugine , testis cords, rete testis, nd primordi l germ cells. Th e glomerulus nd Bowm ns c psule of the mesonephric excretory tubule re degener ting. B. Testis nd genit l duct in the fourth month. The horseshoe-sh ped testi s cords re continuous with the rete testis cords. Note the ductuli efferentes ( excretory mesonephric tubules), which enter the mesonephric duct. Figure 14.21 In uence of primordi l germ cells on indifferent gon d. Ov ry In fem le embryos with n XX sex chromosome complement nd no Y chromosome , primitive sex cords dissoci te into irregul r cell clusters (Figs. 14.21 nd 1 4.22A). These clusters, cont ining groups of primitive germ cells, occupy the me dull ry p rt of the ov ry. L ter they dis ppe r nd re repl ced by v scul r s trom th t forms the ov ri n medull (Fig. 14.22). The surf ce epithelium of the fem le gon d, unlike th t of the m le, continues to prolifer te. In the seventh week, it gives rise to second gener tion of cords, cortic l cords, which pene tr te the underlying mesenchyme but rem in
Ch pter 14: Urogenit l System 341 Degener ting mesonephric tubule Urogenit l mesentery Degener ting medull ry cords Cortic l cords Ductuli efferen tes Surf ce epithelium Prim ry oocyte Follicul r cells P r mesonephric Mesonephric duct duct Surf ce epithelium P r mesonephric duct A B Mesonephric duct Figure 14.22 A. Tr nsverse section of the ov ry t the seventh week, showing deg ener tion of the primitive (medull ry) sex cords nd form tion of the cortic l c ords. B. Ov ry nd genit l ducts in the fth month. Note degener tion of the medul l ry cords. The excretory mesonephric tubules (efferent ductules) do not communi c te with the rete. The cortic l zone of the ov ry cont ins groups of oogoni su rrounded by follicul r cells. close to the surf ce (Fig. 14.22A). In the fourth month, these cords split into isol ted cell clusters, with e ch surrounding one or more primitive germ cells ( Fig. 14.22B). Germ cells subsequently develop into oogoni , nd the surrounding epitheli l cells, descend nts of the surf ce epithelium, form follicul r cells ( see Ch pter 1). It m y thus be st ted th t the genetic sex of n embryo is deter mined t the time of fertiliz tion, depending on whether the sperm tocyte c rrie s n X or Y chromosome. In embryos with n XX sex chromosome con gur tion, medul l ry cords of the gon d regress, nd second ry gener tion of cortic l cords de velops (Figs. 14.21 nd 14.22). In embryos with n XY sex chromosome complex, me dull ry cords develop into testis cords, nd second ry cortic l cords f il to de velop (Figs. 14.20 nd 14.21). GENITAL DUCTS Indifferent St ge Initi lly both m le nd fem le embryos h ve two p irs of genit l ducts: mesonephric (wolf n) ducts nd p r mesonephric (mulleri n) ducts. The p r mesonephric duct rises s lon gitudin l inv gin tion of the epithelium on the nterol ter l surf ce of the uro genit l ridge (Fig. 14.23). Cr ni lly the duct opens into the bdomin l c vity w ith funnel-like structure. C ud lly it rst runs l ter l to the mesonephric duct , then crosses it ventr lly to grow c udomedi lly (Fig.14.23). In the midline it comes in close cont ct with the p r mesonephric duct from the opposite side. Th e two ducts re initi lly
342 P rt Two: Speci l Embryology Figure 14.23 Genit l ducts in the sixth week in the m le (A) nd fem le (B). The mesonephric nd p r mesonephric ducts re present in both. Note the excretory t ubules of the mesonephros nd their rel tion to the developing gon d in both sex es. Abdomin l ostium of uterine tube Suspensory lig ment of ov ry Lig ment of ov ry proper Fimbri e Mesov rium Epoophoron Cortic l cords of ov ry Mesonephros P roophoron Corpus uteri Cervix Round lig ment of uterus B Mesonephric duct Uterine c n l G rtners cyst P r mesonephric tubercle
A Figure 14.24 A. Genit l ducts in the fem le t the end of the second month. Note the p r mesonephric (mlleri n) tubercle nd form tion of the uterine c n l. B. G enit l u ducts fter descent of the ov ry. The only p rts rem ining from the mes onephric system re the epoophoron, p roophoron, nd G rtners cyst. Note the susp ensory lig ment of the ov ry, lig ment of the ov ry proper, nd round lig ment o f the uterus.
Fornix V gin
Ch pter 14: Urogenit l System 343 Figure 14.25 Androgen ction t the cellul r level. Receptor complexes with test osterone (T ) nd dihydrotestosterone (D) inter ct with DNA to control different i tion of the wolf n duct nd extern l genit li , respectively. R, ndrogen recep tor; R , tr nsformed ndrogen receptor hormone complex. sep r ted by septum but l ter fuse to form the uterine c n l (Fig. 14.24A). Th e c ud l tip of the combined ducts projects into the posterior w ll of the uroge nit l sinus, where it c uses sm ll swelling, the p r mesonephric or m lleri n t ubercle (Fig. 14.24A). The mesonephric ducts open into the urogenu it l sinus on either side of the m lleri n tubercle. u Molecul r Regul tion of Genit l Duct De velopment SRY is the m ster gene for testes development nd ppe rs to ct direc tly on the gon d l ridge nd indirectly on the mesonephric ducts. Thus, it induc es the testes to secrete chemot ctic f ctor th t c uses tubules from the meson ephric duct to penetr te the gon d l ridge nd stimul te further testicul r deve lopment. In f ct, without penetr tion by these tubules, differenti tion of the t estes f ils. SRY lso upregul tes steroidogenesis f ctor 1 (SF1), which cts thr ough nother tr nscription f ctor, SOX9, to induce differenti tion of Sertoli n d Leydig cells. Sertoli cells then produce mulleri n inhibiting sub st nce (MIS, lso c lled ntimulleri n hormone, AMH) th t c uses regression of the p r mesone phric (m lleri n) ducts. Leydig cells produce testosterone, u which enters cells of t rget tissues where it m y rem in or be converted to dihydrotestosterone by 5 reduct se enzyme. Testosterone nd dihydrotestosterone bind to speci c highf nity intr cellul r receptor protein, nd ultim tely this hormone receptor comple x binds to DNA to regul te tr nscription of tissue-speci c genes nd their protein products (Fig. 14.25). Testosterone receptor complexes medi te viriliz tion of the mesonephric ducts, where s dihydrotestosterone receptor complexes modul te d ifferenti tion of the m le extern l genit li (Fig. 14.26). Sexu l different tio n in fem les w s once thought to be def ult mech nism th t occurred in the bs ence of Y chromosome, but it now ppe rs th t there re speci c genes th t induc e ov ri n development. For ex mple, DAX1, member of the nucle r hormone recept or f mily, is loc ted on the short rm of the X chromosome nd cts by downregul ting SF1 ctivity, thereby
344 P rt Two: Speci l Embryology Figure 14.26 In uence of the sex gl nds on further sex differenti tion. preventing differenti tion of Sertoli nd Leydig cells. The secreted growth f ct or WNT4 lso contributes to ov ri n differenti tion, nd its e rly expression in the gon d l ridge is m int ined in fem les but downregul ted in m les. In the bsence of MIS production by Sertoli cells, the p r mesonephric (m lleri n) u duct s re stimul ted by estrogens to form the uterine tubes, uterus, cervix, nd upp er v gin . Estrogens lso ct on the extern l genit li t the indifferent st ge to form the l bi m jor , l bi minor , clitoris, nd lower v gin (Fig. 14.26) . Genit l Ducts in the M le As the mesonephros regresses, few excretory tubules, the epigenit l tubules, est blish cont ct with cords of the rete testis nd n ll y form the efferent ductules of the testis (Fig. 14.27). Excretory tubules long the c ud l pole
Ch pter 14: Urogenit l System 345
of the testis, the p r genit l tubules, do not join the cords of the rete testis (Fig. 14.27B). Their vestiges re collectively known s the p r didymis. Except for the most cr ni l portion, the ppendix epididymis, the mesonephric ducts pe rsist nd form the m in genit l ducts (Fig. 14.27). Immedi tely below the entr n ce of the efferent ductules, the mesonephric ducts elong te nd become highly co nvoluted, forming the (ductus) epididymis. From the t il of the epididymis to th e outbudding of the semin l vesicle, the mesonephric ducts obt in thick muscul r co t nd form the ductus deferens. The region of the ducts beyond the semin l vesicles is the ej cul tory duct. The p r mesonephric ducts in the m le degener te except for sm ll portion t their cr ni l ends, the ppendix testis (Fig. 14.27B). Genit l Ducts in the Fem le The p r mesonephric ducts develop into the m in geni t l ducts of the fem le. Initi lly, three p rts c n be recognized in e ch duct: ( ) cr ni l vertic l portion th t opens into the bdomin l c vity, (b) horiz ont l p rt th t crosses the mesonephric duct, nd (c) c ud l vertic l p rt th t fuses with its p rtner from the opposite side (Fig. 14.24A). With descent of t he ov ry, the rst two p rts develop into the uterine tube (Fig. 14.24B ) nd the c ud l p rts fuse
Figure 14.27 A. Genit l ducts in the m le in the fourth month. Cr ni l nd c ud l (p r genit l tubule) segments of the mesonephric system regress. B. Genit l du cts fter descent of the testis. Note the horseshoe-sh ped testis cords, rete te stis, nd efferent ductules entering the ductus deferens. The p r didymis is for med by remn nts of the p r genit l mesonephric tubules. The p r mesonephric duct h s degener ted except for the ppendix testis. The prost tic utricle is n out pocketing from the urethr .
346 P rt Two: Speci l Embryology Urogenit l ridge Mesonephric excretory tubule Uterorect l pouch Ov ry A B P r mesonephric duct C Mesonephric duct Bro d Fused lig ment p r mesonephric of uterus ducts Uteroves ic l pouch Figure 14.28 Tr nsverse sections through the urogenit l ridge t progressively l ower levels. A. nd B. The p r mesonephric ducts ppro ch e ch other in the midl ine nd fuse. C. As result of fusion, tr nsverse fold, the bro d lig ment of the uterus, forms in the pelvis. The gon ds come to lie t the posterior spect of the tr nsverse fold. to form the uterine c n l. When the second p rt of the p r mesonephric ducts mov es medioc ud lly, the urogenit l ridges gr du lly come to lie in tr nsverse pl ne (Fig. 14.28, A nd B). After the ducts fuse in the midline, bro d tr nsver se pelvic fold is est blished (Fig. 14.28C ). This fold, which extends from the l ter l sides of the fused p r mesonephric ducts tow rd the w ll of the pelvis, is the bro d lig ment of the uterus. The uterine tube lies in its upper border, nd the ov ry lies on its posterior surf ce (Fig. 14.28C ). The uterus nd bro d lig ments divide the pelvic c vity into the uterorect l pouch nd the uterovesi c l pouch. The fused p r mesonephric ducts give rise to the corpus nd cervix of the uterus. They re surrounded by l yer of mesenchyme th t forms the muscul r co t of the uterus, the myometrium, nd its peritone l covering, the perimetri um. VAGINA Shortly fter the solid tip of the p r mesonephric ducts re ches the urogenit l sinus (Figs. 14.29A nd 14.30A), two solid ev gin tions grow out from the pelvic p rt of the sinus (Figs. 14.29B nd 14.30B). These ev gin tions, the sinov gin l bulbs, prolifer te nd form solid v gin l pl te. Prolifer tion co ntinues t the cr ni l end of the pl te, incre sing the dist nce between the ute rus nd the urogenit l sinus. By the fth month, the v gin l outgrowth is entirely c n lized. The winglike exp nsions of the v gin round the end of the uterus, the v gin l fornices, re of p r mesonephric origin (Fig. 14.30C ). Thus, the v gin h s du l origin, with the upper portion derived from the uterine c n l n d the lower portion derived from the urogenit l sinus.
Ch pter 14: Urogenit l System 347
Figure 14.30 S gitt l sections showing form tion of the uterus nd v gin t v r ious st ges of development. A. Nine weeks. B. End of third month. C. Newborn.
The lumen of the v gin rem ins sep r ted from th t of the urogenit l sinus by thin tissue pl te, the hymen (Figs. 14.29C nd 14.30C ), which consists of the epitheli l lining of the sinus nd thin l yer of v gin l cells. It usu lly dev elops sm ll opening during perin t l life. The fem le m y ret in some remn nts of the cr ni l nd c ud l excretory tubules in the mesov rium, where they form the epoophoron nd p roophoron, respectively (Fig. 14.24B ). The mesonephric duc t dis ppe rs except for sm ll cr ni l portion found in the epoophoron nd occ sion lly
Figure 14.29 Form tion of the uterus nd v gin . A. 9 weeks. Note the dis ppe r nce of the uterine septum. B. At the end of the third month. Note the tissue of the sinov gin l bulbs. C. Newborn. The fornices nd the upper portion of the v g in re formed by v cuoliz tion of the p r mesonephric tissue, nd the lower pro tion of the v gin is formed by v cuoliz tion of the sinov gin l bulbs.
348 P rt Two: Speci l Embryology sm ll c ud l portion th t m y be found in the w ll of the uterus or v gin . L te r in life it m y form G rtners cyst (Fig. 14.24B ). CLINICAL CORRELATES Uterine nd V gin l Defects Duplic tions of the uterus result from l ck of fusio n of the p r mesonephric ducts in loc l re or throughout their norm l line o f fusion. In its extreme form the uterus is entirely double (uterus didelphys) ( Fig. 14.31A); in the le st severe form, it is only slightly indented in the midd le (uterus rcu tus) (Fig. 14.31B). One of the rel tively common nom lies is th e uterus bicornis, in which the uterus h s two horns entering common v gin (F ig. 14.31C ). This condition is norm l in m ny m mm ls below the prim tes. In p tients with complete or p rti l tresi of one of the p r mesonephric ducts, the rudiment ry p rt lies s n ppend ge to the well-developed side. Since its lum en usu lly does not communic te with the v gin , complic tions re common (uteru s bicornis unicollis with one rudiment ry horn) (Fig. 14.31D). If the tresi in volves both sides, n tresi of the cervix m y result (Fig. 14.31E ). If the si nov gin l bulbs f il to fuse or do not develop t ll, double v gin or tresi of the v gin , respectively, results (Fig. 14.31, A nd F ). In the l tter c s e, sm ll v gin l pouch origin ting from the p r mesonephric ducts usu lly surr ounds the opening of the cervix. Figure 14.31 M in bnorm lities of the uterus nd v gin , c used by persistence of the uterine septum or obliter tion of the lumen of the uterine c n l.
Ch pter 14: Urogenit l System 349 EXTERNAL GENITALIA Indifferent St ge In the third week of development, mesenchym e cells origin ting in the region of the primitive stre k migr te round the clo c l membr ne to form p ir of slightly elev ted clo c l folds (Fig. 14.32A). C r ni l to the clo c l membr ne the folds unite to form the genit l tubercle. C u d lly the folds re subdivided into urethr l folds nteriorly nd n l folds pos teriorly (Fig. 14.32B ). In the me ntime, nother p ir of elev tions, the genit l swellings, becomes visible on e ch side of the urethr l folds. These swellings l ter form the scrot l swellings in the m le (Fig. 14.33A) nd the l bi m jor in the fem le (see Fig. 14.36B). At the end of the sixth week, however, it is i mpossible to distinguish between the two sexes (Fig. 14.34C ). Figure 14.32 A nd B. Indifferent st ges of the extern l genit li . A. Approxim tely 4 weeks. B. Approxim tely 6 weeks. C. Sc nning electron microgr ph of the e xtern l genit li of hum n embryo t pproxim tely the seventh week. AF, n l fold; rrowhe d, n l opening; GS, genit l swelling; GT, genit l tubercle; T, t il; UF, urethr l fold.
350 P rt Two: Speci l Embryology Figure 14.33 A. Development of extern l genit li in the m le t 10 weeks. Note the deep urethr l groove nked by the urethr l folds. B. Tr nsverse sections thro ugh the ph llus during form tion of the penile urethr . The urogenit l groove is bridged by the urethr l folds. C. Development of the gl ndul r portion of the p enile urethr . D. Newborn. Figure 14.34 A. Genit li of m le fetus t 14 weeks, showing fusion of the scr ot l swellings (S ). Arrow, epitheli l t g. B nd C. Dors l nd ventr l views, r espectively, of the genit li of fem le fetus t 11 weeks. The genit l tubercl e t this st ge is longer th n in the m le (A), nd the genit l swellings (GS ) rem in unfused. Extern l Genit li in the M le Development of the extern l genit li in the m le is under the in uence of ndrogens secreted by the fet l testes nd is ch r cteri zed by r pid elong tion of the genit l tubercle, which is now c lled the ph llus (Figs. 14.33A nd 14.34A). During this elong tion, the ph llus pulls the urethr l folds forw rd so th t they form the l ter l w lls of the urethr l groove. Thi s groove extends long the c ud l spect of the elong ted ph llus but does not r e ch the most dist l p rt,
Ch pter 14: Urogenit l System 351 the gl ns. The epitheli l lining of the groove, which origin tes in the endoderm , forms the urethr l pl te (Fig. 14.33B ). At the end of the third month the two urethr l folds close over the urethr l pl te, forming the penile urethr (Figs. 14.33B nd 14.34A). This c n l does not extend to the tip of the ph llus. This most dist l portion of the urethr is formed during the fourth month, when ectod erm l cells from the tip of the gl ns penetr te inw rd nd form short epitheli l cord. This cord l ter obt ins lumen, thus forming the extern l urethr l me tus (Fig. 14.33C ). The genit l swellings, known in the m le s the scrot l swel lings, rise in the inguin l region. With further development they move c ud lly , nd e ch swelling then m kes up h lf of the scrotum. The two re sep r ted by the scrot l septum (Figs. 14.33D nd 14.34A). CLINICAL CORRELATES
Defects in the M le Genit li In hyposp di s fusion of the urethr l folds is inc omplete, nd bnorm l openings of the urethr occur long the inferior spect of the penis, usu lly ne r the gl ns, long the sh ft, or ne r the b se of the pen is (Fig.14.35). In r re c ses the urethr l me tus extends long the scrot l r ph e. When fusion of the urethr l folds f ils entirely, wide s gitt l slit is fou nd long the entire length of the penis nd the scrotum. The two scrot l swellin gs then closely resemble the l bi m jor . The incidence of hyposp di s is 35/100 0 births, nd this r te represents doubling over the p st 15 to 20 ye rs. Re s ons for the incre se re not known, but one hypothesis suggests it could be re sult of rise in environment l estrogens (endocrine disruptors, see Ch pter 7). Episp di s is r re bnorm lity (1/30,000 births) in which the urethr l me tus is found on the dorsum of the penis. Inste d of developing t the cr ni l m rgi n of the clo c l membr ne, the genit l tubercle seems to form in the region of t he urorect l septum. Hence portion of the clo c l membr ne is found cr ni l to the genit l tubercle, nd when this membr ne ruptures, the outlet of the urogen it l sinus comes to lie on the cr ni l spect of the penis (Fig. 14.35C ). Altho ugh episp di s m y occur s n isol ted defect, it is most often ssoci ted with exstrophy of the bl dder. In exstrophy of the bl dder, of which episp di s is const nt fe ture, the bl dder mucos is exposed to the outside (Figs. 14.16A n d 14.35C ). Norm lly the bdomin l w ll in front of the bl dder is formed by pri mitive stre k mesoderm, which migr tes round the clo c l membr ne. When this mi gr tion does not occur, rupture of the clo c l membr ne extends cr ni lly, cre t ing exstrophy of the bl dder. Micropenis occurs when there is insuf cient ndrogen stimul tion for growth of the extern l genit li . Micropenis is usu lly c used by prim ry hypogon dism or hypoth l mic or pituit ry dysfunction. By de nition, th e penis is 2.5 st nd rd devi tions below the me n in length s me sured long
352 P rt Two: Speci l Embryology Abnorm l urethr l orifices A Hyposp di s B Mucos of urin ry bl dder Ureteric opening
C Figure 14.35 A. Hyposp di s showing the v rious loc tions of bnorm l urethr l o ri ces. B. P tient with hyposp di s. The urethr is open on the ventr l surf ce of the penis. C. Episp di s combined with exstrophy of the bl dder. Bl dder mucos is exposed.
Extern l Genit li in the Fem le Estrogens stimul te development of the extern l genit li of the fem le. The genit l tubercle elong tes only slightly nd forms the clitoris (Figs. 14.34B nd
the dors l surf ce from the pubis to the tip with the penis stretched to resist nce. Bi d penis or double penis m y occur if the genit l tubercle splits.
Urethr
Ch pter 14: Urogenit l System 353
Defects in Sex Differenti tion Klinefelter syndrome, with k ryotype of 47,XXY (or other v ri nts, e.g., XXXY), is the most common m jor bnorm lity of sexu l differenti tion, occurring with frequency of 1/500 m les. P tients re ch r ct erized by infertility, gynecom sti , v rying degrees of imp ired sexu l m tur ti on, nd in some c ses under ndrogeniz tion. Nondisjunction of the XX homologues is the most common c us tive f ctor. In gon d l dysgenesis oocytes re bsent n d the ov ries ppe r s stre k gon ds. Individu ls re phenotypic lly fem le but m y h ve v riety of chromosom l complements, including XY. XY fem le gon d l dysgenesis (Swyer syndrome) results from point mut tions or deletions of the SRY gene. Individu ls ppe r to be norm l fem les but do not menstru te nd do not develop second ry sexu l ch r cteristics t puberty. P tients with Turner syndro me lso h ve gon d l dysgenesis. They h ve 45,X k ryotype nd short st ture, h igh rched p l te, webbed neck, shieldlike chest, c rdi c nd ren l nom lies,
14.36A); urethr l folds do not fuse, s in the m le, but develop into the l bi minor . Genit l swellings enl rge nd form the l bi m jor . The urogenit l groo ve is open nd forms the vestibule (Figs. 14.34C nd 14.36B). Although the genit l tubercle does not elong te extensively in the fem le, it is l rger th n in th e m le during the e rly st ges of development (Fig. 14.34,A nd B ). In f ct, us ing tubercle length s criterion ( s monitored by ultr sound) h s resulted in mist kes in identi c tion of the sexes during the third nd fourth months of gest tion. CLINICAL CORRELATES
Figure 14.36 Development of the extern l genit li in the fem le nd in the newborn (B).
t 5 months (A)
354 P rt Two: Speci l Embryology Figure 14.37 P tient with Turner syndrome, which is ch r cterized by 45,X chro mosome complement. Note the bsence of sexu l m tur tion. Other typic l fe tures re webbed neck, bro d chest with widely sp ced nipples, nd short st ture. nd inverted nipples (Fig. 14.37). Absence of oocytes in 45,X c ses is due to in cre sed oocyte loss nd not to germ cell bnorm lities. Since sexu l development of m les nd fem les begins in n identic l f shion, it is not surprising th t bnorm lities in differenti tion nd sex determin tion occur. In some c ses thes e bnorm lities result in individu ls with ch r cteristics of both sexes, known s herm phrodites. True herm phrodites h ve both testicul r nd ov ri n tissue, usu lly combined s ovotestes. In 70% of c ses the k ryotype is 46,XX, nd there is usu lly uterus. Extern l genit li re mbiguous or predomin ntly fem le, nd most of these individu ls re r ised s fem les. In pseudoherm phrodites, th e genotypic sex is m sked by phenotypic ppe r nce th t closely resembles the other sex. When the
Ch pter 14: Urogenit l System 355 pseudoherm phrodite h s testis, the p tient is c lled m le pseudoherm phrodi te; when n ov ry is present, the p tient is c lled fem le pseudoherm phrodite . Fem le pseudoherm phroditism is most commonly c used by congenit l dren l hyp erpl si ( drenogenit l syndrome). Biochemic l bnorm lities in the dren l gl n ds result in decre sed steroid hormone production nd n incre se in drenocorti cotropic hormone (ACTH). In most c ses, 21hydroxyl tion is inhibited, such th t 17-hydroxyprogesterone (17-OHP) is not converted to 11-deoxycortisol. ACTH level s incre se in response to defective cortisol production, which le ds to ever-inc re sing mounts of 17-OHP. In turn, there is excessive production of ndrogens. P tients h ve 46,XX chromosome complement, chrom tin-positive nuclei, nd ov r ies, but excessive production of ndrogens m sculinizes the extern l genit li . This m sculiniz tion m y v ry from enl rgement of the clitoris to lmost m le ge nit li (Fig. 14.38). Frequently there is clitor l hypertrophy nd p rti l fusio n of A B Figure 14.38 A. P tient with fem le pseudoherm phrodism c used by congenit l dr en l hyperpl si ( drenogenit l syndrome). B. Extern l genit li show fusion of the l bi m jor nd enl rgement of the clitoris.
356 P rt Two: Speci l Embryology the l bi m jor , giving the ppe r nce of scrotum, nd sm ll persistent uro genit l sinus. M le pseudoherm phrodites h ve 46,XY chromosome complement, nd their cells re usu lly chrom tin-neg tive. Reduced production of ndrogenic ho rmones nd MIS re responsible for this condition. Intern l nd extern l sex ch r cteristics v ry consider bly, depending on the degree of development of extern l genit li nd the presence of p r mesonephric deriv tives. Androgen insensiti vity syndrome (formerly testicul r feminiz tion) occurs in p tients who h ve 4 6,XY chromosome complement but h ve the extern l ppe r nce of norm l fem les (F ig. 14.39). This disorder results from l ck of ndrogen receptors or f ilure o f tissues to respond to receptordihydrotestosterone complexes. Consequently, nd rogens produced by the testes re ineffective in inducing differenti tion of m l e genit li . Since these p tients h ve testes nd MIS is present, the p r mesone phric system is suppressed, nd uterine tubes nd uterus re bsent. The v gin is short nd blind. The testes re frequently found in the inguin l or l bi l re gions, but sperm togenesis does not occur. Furthermore, there is n incre sed ri sk of tumor form tion in these structures, nd 33% of these individu ls develop m lign ncies prior to ge 50. This syndrome is n X-linked recessive disorder th t occurs in 1/20,000 live births. Figure 14.39 P tient with ndrogen insensitivity syndrome, which is ch r cterize d by 46,XY chromosome complement.
Ch pter 14: Urogenit l System 357 DESCENT OF THE TESTES Tow rd the end of the second month, the urogenit l mesente ry tt ches the testis nd mesonephros to the posterior bdomin l w ll (Fig. 14. 3A). With degener tion of the mesonephros the tt chment serves s mesentery f or the gon d (Fig. 14.28B). C ud lly it becomes lig mentous nd is known s the c ud l genit l lig ment (Fig. 14.40A). Also extending from the c ud l pole of th e testis is mesenchym l condens tion rich in extr cellul r m trices, the guber n culum (Fig. 14.40). Prior to descent of the testis, this b nd of mesenchyme te rmin tes in the inguin l region between the differenti ting intern l nd extern l bdomin l oblique muscles. L ter, s the testis begins to descend tow rd the i nguin l ring, n extr - bdomin l portion of the gubern culum forms nd grows fro m the inguin l region tow rd the scrot l swellings. When the testis p sses throu gh the inguin l c n l, this extr - bdomin l portion cont cts the scrot l oor (the gubern culum forms in fem les lso, but in norm l c ses it rem ins rudiment ry) . F ctors controlling descent of the testis re not entirely cle r. It ppe rs, however, th t outgrowth of the extr - bdomin l portion of the gubern culum produ ces intr - bdomin l migr tion, th t n incre se in intr - bdomin l pressure due to org n growth produces p ss ge through the inguin l c n l, nd th t regression of the extr - bdomin l portion of the gubern culum completes movement of the te stis into the scrotum. Norm lly, the testes re ch the inguin l region by pproxi m tely 12 weeks gest tion, migr te through the inguin l c n l by 28 weeks, nd r e ch the scrotum by 33 weeks (Fig. 14.40). The process is in uenced by hormones, i ncluding ndrogens nd MIS. During descent, blood supply to the testis from the ort is ret ined, nd testicul r vessels extend from their origin l lumb r posi tion to the testis in the scrotum. Independently from descent of the testis, the peritoneum of the bdomin l c vity forms n ev gin tion on e ch side of the mid line into the ventr l bdomin l w ll. This ev gin tion, the processus v gin lis, follows the course of the gubern culum testis into the scrot l swellings (Fig. 14.40B). Hence the processus v gin lis, ccomp nied by the muscul r nd f sci l l yers of the body w ll, ev gin tes into the scrot l swelling, forming the ingui n l c n l (Fig. 14.41). The testis descends through the inguin l ring nd over t he rim of the pubic bone nd is present in the scrotum t birth. The testis is t hen covered by re ected fold of the processus v gin lis (Fig. 14.40D). The perit one l l yer covering the testis is the viscer l l yer of the tunic v gin lis; t he rem inder of the peritone l s c forms the p riet l l yer of the tunic v gin lis (Fig. 14.40D). The n rrow c n l connecting the lumen of the v gin l process with the peritone l c vity is obliter ted t birth or shortly there fter. In dd ition to being covered by peritone l l yers derived from the processus v gin lis , the testis becomes enshe thed in l yers derived from the nterior bdomin l w ll through which it p sses. Thus, the tr nsvers lis f sci forms the intern l sp erm tic f sci , the intern l bdomin l oblique muscle gives rise to the crem ste ric f sci nd muscle, nd the extern l bdomin l oblique
358
Gubern culum (extr bdomin l portion) Ph llus Gubern culum testis Rectum V gin l process Symphysis Scrot l swelling A B Testis V gin l process Gubern culum testis P riet l l yer of tunic v gin lis Viscer l l yer of tunic v gin lis Gubern cul um testis C D E Figure 14.40 Descent of the testis. A. During the second month. B. In the middle of the third month. Peritoneum lining the coelomic c vity ev gin tes into the s crot l swelling, where it forms the v gin l process (tunic v gin lis). C. In th e seventh month. D. Shortly fter birth. E. Sc nning electron microgr ph of mo use embryo showing the primitive gon d (G), mesonephric duct ( rrowhe ds), nd g ubern culum ( rrows).
P rt Two: Speci l Embryology Testis C ud l genit l lig ment
nd gubern culum Testis
Ch pter 14: Urogenit l System 359
Hydrocele Ductus deferens Epididymis B C Tunic v gin lis
muscle forms the extern l sperm tic f sci (Fig. 14.41A). The tr nsversus bdomi nis muscle does not contribute l yer, since it rches over this region nd doe s not cover the p th of migr tion. CLINICAL CORRELATES Herni s nd Cryptorchism The connection between the bdomin l c vity nd the pro cessus v gin lis in the scrot l s c norm lly closes in the rst ye r fter birth ( Fig. 14.40D). If this p ss gew y rem ins open, intestin l loops m y descend into the scrotum, c using congenit l inguin l herni . (Fig, 14.41B ). Sometimes ob liter tion of this p ss gew y is irregul r, le ving sm ll cysts long its course . L ter these cysts m y secrete uid, forming hydrocele of the testis nd/or spe rm tic cord (Fig. 14,41C ). In 97% of m le newborns, testes re present in the s crotum before birth. In most of the rem inder, descent will be completed during the rst 3 months postn t lly. However, in less th n 1% of inf nts, one or both te stes f il to descend. The condition is c lled cryptorchidism nd m y be c used b y decre sed ndrogen (testosterone) production. The undescended testes f il to p roduce m ture sperm tozo nd the condition is ssoci ted with 3% to 5% incide nce of ren l nom lies. DESCENT OF THE OVARIES Descent of the gon ds is consider bly less in the fem le th n in the m le, nd the ov ries n lly settle just below the rim of the true pelvis. The cr ni l genit l lig ment forms the suspensory l ig ment of the ov ry, where s the
Figure 14.41 A. Testis, epididymis, ductus deferens, nd v rious l yers of the bdomin l w ll th t surround the testis in the scrotum. B. V gin l process in ope n communic tion with the peritone l c vity. In such c se, portions of the inte stin l loops often descend tow rd nd occ sion lly into the scrotum, c using n inguin l herni . C. Hydrocele.
Obliter ted s c Connection between peritone l c vity perm tic Int. f sci Tunic v gin lis Gubern culum
nd tunic v gin lis Ext. s
Abdomin l muscul ture Ductus deferens Epididymis Crem steric f sci
nd muscle A
360 P rt Two: Speci l Embryology c ud l genit l lig ment forms the lig ment of the ov ry proper nd the round lig ment of the uterus (Fig. 14.24). the l tter extends into the l bi m jor . Summ ry The urin ry nd genit l systems both develop from mesoderm l tissue. Thr ee urin ry systems develop in tempor l sequence from cr ni l to c ud l segment s: The pronephros, which forms in the cervic l region, is vestigi l. The mesonep hros, which forms in the thor cic nd lumb r regions, is l rge nd is ch r cteri zed by excretory units (nephrons) nd its own collecting duct, the mesonephric o r wolf n duct. In the hum n it m y function brie y, but most of the system dis ppe rs. Ducts nd tubules from the mesonephros form the conduit for sperm from the t estes to the urethr . In the fem le, these ducts regress. The met nephros, or pe rm nent kidney, develops from two sources. It forms its own excretory tubules or nephrons like the other systems, but its collecting system origin tes from the ureteric bud, n outgrowth of the mesonephric duct. This bud gives rise to the u reter, ren l pelvis, c lyces, nd the entire collecting system (Fig. 14.5). Conn ection between the collecting nd excretory tubule systems is essenti l for norm l development (Fig. 14.6). WT1, expressed by the mesenchyme, m kes this tissue competent to respond to induction by the ureteric bud. Inter ctions between the bud nd mesenchyme occur through production of GDNF nd HGF by the mesenchyme wi th their tyrosine kin se receptors RET nd MET, respectively, produced by the ur eteric epithelium. PAX2 nd WNT4, produced by the ureteric bud, c use epitheli l iz tion of the met nephric mesenchyme in prep r tion for excretory tubule differ enti tion (Fig. 14.7). E rly division of the ureteric bud m y le d to bi d or supe rnumer ry kidneys with ectopic ureters (Fig. 14.9). Abnorm l positions of the ki dney, such s pelvic nd horseshoe kidney, re lso well known (Fig. 14.11). The genit l system consists of ( ) gon ds or primitive sex gl nds, (b) genit l duct s, nd (c) extern l genit li . All three components go through n indifferent st ge in which they m y develop into either m le or fem le. The SRY gene on th e Y chromosome produces testes-determining f ctor nd regul tes m le sexu l deve lopment. Genes downstre m from SRY include steroidogenesis f ctor (SF1) nd SOX9 th t stimul te differenti tion of Sertoli nd Leydig cells in the testes. Expre ssion of the SRY gene c uses ( ) development of the medull ry (testis) cords, (b ) form tion of the tunic lbugine , nd (c) f ilure of the cortic l (ov ri n) c ords to develop. In the bsence of the SRY gene, the combin tion of DAX1 express ion, to downregul te SF1, nd continued expression of WNT4 in the gon d l ridge, c uses form tion of ov ries with ( ) typic l cortic l cords, (b) dis ppe r nce of the medull ry (testis) cords, nd (c) f ilure of the tunic lbugine to deve lop (Fig. 14.21). When primordi l germ
Ch pter 14: Urogenit l System 361 cells f il to re ch the indifferent gon d, the gon d rem ins indifferent or is bsent. The indifferent duct system nd extern l genit li develop under the in uen ce of hormones. Testosterone produced by Leydig cells in the testes stimul tes d evelopment of the mesonephric ducts (v s deferens epididymis), while MIS produce d by Sertoli cells in the testes c uses regression of the p r mesonephric ducts (fem le duct system). Dihydrotestosterone stimul tes development of the extern l genit li , penis, scrotum, nd prost te (Fig. 14.26). Estrogens in uence developm ent of the p r mesonephric fem le system, including the uterine tube, uterus, ce rvix, nd upper portion of the v gin . They lso stimul te differenti tion of th e extern l genit li , including the clitoris, l bi , nd lower portion of the v gin (Fig. 14.26). Errors in production of or sensitivity to hormones of the tes tes le d to predomin nce of fem le ch r cteristics under in uence of the m tern l nd pl cent l estrogens. Problems to Solve 1. During development of the urin ry system, three systems for m. Wh t re they, nd wh t p rts of e ch, if ny, rem in in the newborn? 2. At b irth n pp rently m le b by h s no testicles in the scrotum. L ter it is determ ined th t both re in the bdomin l c vity. Wh t is the term given to this condi tion, nd c n you expl in the embryologic l origin of this defect? 3. It is s id th t m le nd fem le extern l genit li h ve homologies. Wh t re they, nd wh t re their embryologic l origins? 4. After sever l ye rs of trying to become pr egn nt, young wom n seeks consult tion. Ex min tion reve ls bicorn te uterus . How could such n bnorm lity occur?
SUGGESTED READING Behringer RR, Finegold MJ, C te RL: Mulleri n-inhibiting subst nce function during m mm li n sexu l development. Cell 79:415, 1994. Grif n JE, W ilson JD: Disorders of sexu l differenti tion. In W lsh PC, et l (eds): C mpbel ls Urology. Phil delphi , WB S unders, 1986. H qq CM, et l.: Molecul r b sis of m mm li n sexu l determin tion: ctiv tion of mulleri n inhibiting subst nce gen e expression by SRY. Science 266:1494, 1994. McElre vey K, et l.: A regul tory c sc de hypothesis for m mm li n sex determin tion: SRY represses neg tive reg ul tor of m le development. Proc N tl Ac d Sci 90:3368, 1993. Mesrobi n HGJ, Rus hton HG, Bul s D: Unil ter l ren l genesis m y result from in utero regression of multicystic dyspl si . J Urol 150:793, 1993. Mittwoch U: Sex determin tion n d sex revers l: genotype, phenotype, dogm nd sem ntics. Hum Genet 89:467, 1992 . OR hilly R: The development of the v gin in the hum n. In Bl nd u RJ, Bergsm D (eds): Morphogenesis nd M lform tion of the Genit l Systems. New York, Al n R Liss, 1977:123.
362 P rt Two: Speci l Embryology P ulozzi LJ, Erickson JD, J ckson RJ: Hyposp di s trends in two US surveill nce systems, Pedi trics 100:831, 1997. Persu d TVN: Embryology of the fem le genit l tr ct nd gon ds. In Copel nd LJ, J rrell J, McGregor J (eds): Textbook of Gyne cology. Phil delphi , WB S unders, 1992. S xen L, S riol H, Lehtonen E: Sequent i l cell nd tissue inter ctions governing org nogenesis of the kidney. An t Emb ryol 175:1, 1986. Stevenson RE, H ll JG, Goodm n RM (eds): Hum n M lform tions nd Rel ted Anom lies, vol 2. New York, Oxford University, 1993. Sw in A, N rv ez V, Burgoyne P, C merino G, Lovell-B dge R: D x I nt gonizes Sry ction in m mm li n sex determin tion, N ture 391:761, 1998. Tilm nn C, C pel B: Mesonephric c ell migr tion induces testes cord form tion nd Sertoli cell differenti tion in the m mm li n gon d. Dev 126:2883, 1999. V ino S, Heikkil M, Kispert A, Chin N, McM hon AP: Fem le development in m mm ls is regul ted by WNT4 sign ling. N tur e 397:405, 1999. V n der Werff JFA, Nievelstein RAJ, Br nds E, Linjsterburg AJM, Vermeij-Keers C: Norm l development of the m le nterior urethr . Ter tology 61 :172, 2000. Vil in E, J ubert F, Fellows M, McElre vey K: P thology of 46,XY pur e gon d l dysgenesis: bsence of testes differenti tion ssoci ted with mut tion s in the testes determining f ctor. Differenti tion 52:151, 1993. Wensing CJG, C olenbr nder B: Norm l nd bnorm l testicul r descent. Oxf Rev Reprod Biol 130, 1986. Woolf AS: Clinic l imp ct nd biologic l b sis of ren l m lform tions. Sem in rs Nephrol 15:361, 1995.
ch pter 15 He d nd Neck Mesenchyme for form tion of the he d region is derived from p r xi l nd l ter l pl te mesoderm, neur l crest, nd thickened regions of ectoderm known s ectode rm l pl codes. P r xi l mesoderm (somites nd somitomeres) forms the oor of the b r in c se nd sm ll portion of the occipit l region (Fig. 15.1) (see Ch pter 8 ), ll volunt ry muscles of the cr niof ci l region (see Ch pter 9), the dermis nd connective tissues in the dors l region of the he d, nd the meninges c ud l to the prosenceph lon. L ter l pl te mesoderm forms the l rynge l c rtil ges ( rytenoid nd cricoid) nd connective tissue in this region. Neur l crest cells o rigin te in the neuroectoderm of forebr in, midbr in, nd hindbr in regions nd migr te ventr lly into the ph rynge l rches nd rostr lly round the forebr in nd optic cup into the f ci l region (Fig. 15.2). In these loc tions they form m idf ci l nd ph rynge l rch skelet l structures (Fig. 15.1) nd ll other tissu es in these regions, including c rtil ge, bone, dentin, tendon, dermis, pi nd r chnoid, sensory neurons, nd gl ndul r strom . Cells from ectoderm l pl codes , together with neur l crest, form neurons of the fth, seventh, ninth, nd tenth cr ni l sensory g ngli . The most typic l fe ture in development of the he d nd neck is formed by the ph rynge l or br nchi l rches. These rches ppe r in th e fourth nd fth weeks of development nd contribute to the ch r cteristic extern l ppe r nce of the embryo (T ble 15.1 nd Fig. 15.3). Initi lly, they consist of b rs of mesenchym l tissue sep r ted by deep clefts known s ph rynge l (br n chi l) clefts (Figs. 15.3C ; 363
364 P rt Two: Speci l Embryology Figure 15.1 Skelet l structures of the he d nd f ce. Mesenchyme for these struc tures is derived from neur l crest (blue), l ter l pl te mesoderm (yellow), nd p r xi l mesoderm (somites nd somitomeres) (red). see lso Fig. 15.6). Simult neously, with development of the rches nd clefts, number of outpocketings, the ph rynge l pouches, ppe r long the l ter l w ll s of the ph rynge l gut, the most cr ni l p rt of the foregut (Fig. 15.4; see l so Fig. 15.6). The pouches penetr te the surrounding mesenchyme, but do not est blish n open communic tion with the extern l clefts (see Fig. 15.6). Hence, lt hough development of ph rynge l rches, clefts, nd pouches resembles form tion of gills in shes nd mphibi , in the hum n embryo re l gills (br nchi ) re neve r formed. Therefore, the term ph rynge l ( rches, clefts, nd pouches) h s been dopted for the hum n embryo. Ph rynge l rches not only contribute to form tion of the neck, but lso pl y n import nt role in form tion of the f ce. At the e nd of the fourth week, the center of the f ce is formed by the stomodeum, surrou nded by the rst p ir of ph rynge l rches (Fig. 15.5). When the embryo is 42 week s old, ve mesenchym l prominences c n be recognized: the m ndibul r prominences ( r st ph rynge l rch), c ud l to the stomodeum; the m xill ry prominences (dors l portion of the rst ph rynge l rch), l ter l to the stomodeum; nd the fronton s l prominence, slightly rounded elev tion cr ni l to the stomodeum. Development of the f ce is l ter complemented by form tion of the n s l prominences (Fig. 1 5.5). In ll c ses, differenti tion of structures derived from rches pouches, c lefts, nd prominences is dependent upon epitheli l-mesenchym l inter ctions. In some inst nces, sign ls for these inter ctions re simil r to those involved in limb development, including brobl st growth f ctor (FGFs) for outgrowth nd soni c hedgehog (SHH ) nd WNTs for p tterning.
Ch pter 15: He d nd Neck 365 A B Figure 15.2 A. Sc nning electron microgr ph showing cr ni l neur l crest cells m igr ting into the f ci l region bene th the ectoderm th t h s been removed. B. M igr tion p thw ys of neur l crest cells from forebr in, midbr in, nd hindbr in regions into their n l loc tions (sh ded re s) in the ph rynge l rches nd f ce . Regions of ectoderm l thickenings (pl codes), which will ssist crest cells in form tion of the fth (V), seventh (VII), ninth (IX), nd tenth (X) cr ni l senso ry g ngli , re lso illustr ted. Ph rynge l Arches E ch ph rynge l rch consists of core of mesenchym l tissue covered on the outside by surf ce ectoderm nd on the inside by epithelium of en doderm l origin (Fig. 15.6). In ddition to mesenchyme derived from p r xi l nd l ter l pl te mesoderm, the core of e ch rch receives subst nti l numbers of n eur l crest cells, which migr te into the rches to contribute to skelet l compo nents of the f ce. The origin l mesoderm of the rches gives rise to the muscul ture of the f ce nd neck. Thus, e ch ph rynge l rch is ch r cterized by its ow n
366 P rt Two: Speci l Embryology TABLE 15.1 Deriv tives of the Ph rynge l Arches nd Their Innerv tion Ph rynge l Arch 1 m ndibul r (m xill ry nd m ndibul r processes) Nerve V. Trigemin l: m x ill ry nd m ndibul r divisions Muscles M stic tion (tempor l; m sseter; medi l, l ter l pterygoids); mylohyoid; nterior belly of dig stric; tensor p l tine, t ensor tymp ni F ci l expression (buccin tor; uricul ris; front lis; pl tysm ; o rbicul ris oris; orbicul ris oculi); posterior belly of dig stric; stylohyoid; s t pedius Styloph ryngeus Skeleton Prem xill , m xill , zygom tic bone, p rt of t empor l bone, Meckels c rtil ge, m ndible m lleus, incus, nterior lig ment of m lleus, sphenom ndibul r lig ment St pes; styloid process; stylohyoid lig ment; l esser horn nd upper portion of body of hyoid bone 2 hyoid VII. F ci l 3 IX. Glossoph rynge l X. V gus Superior l rynge l br nch (nerve to fourth rch) R ecurrent l rynge l br nch (nerve to sixth rch) 46 Cricothyroid; lev tor p l tine; constrictors of ph rynx Gre ter horn nd lower portion of body of hyoid bone L rynge l c rtil ges (thyro id, cricoid, rytenoid, cornicul te, cuneiform) Intrinsic muscles of l rynx muscul r components. The muscul r components of e ch rch h ve their own cr ni l nerve, nd wherever the muscle cells migr te, they c rry their nerve component with them (Figs. 15.6 nd 15.7). In ddition, e ch rch h s its own rteri l com ponent (Figs. 15.4 nd 15.6). (Deriv tives of the ph rynge l rches nd their ne rve supply re summ rized in T ble 15.1). FIRST PHARYNGEAL ARCH The rst ph rynge l rch consists of dors l portion, the m xill ry process, which extends forw r d bene th the region of the eye, nd ventr l portion,
Ch pter 15: He d nd Neck 367 Figure 15.3 Development of the ph rynge l rches. A. 25 d ys. B. 28 d ys. C. 5 w eeks. Figure 15.4 Ph rynge l pouches s outpocketings of the foregut nd the primordiu m of the thyroid gl nd nd ortic rches. the m ndibul r process, which cont ins Meckels c rtil ge (Figs. 15.5 nd 15.8A). During further development, Meckels c rtil ge dis ppe rs except for two sm ll por tions t its dors l end th t persist nd form the incus nd m lleus (Figs. 15.8B nd 15.9). Mesenchyme of the m xill ry process gives rise to the prem xill , m xill , zygom tic bone, nd p rt of the tempor l bone through membr nous ossi c tio n (Fig. 15.8B). The m ndible is lso formed by membr nous ossi c tion of mesenchym l tissue surrounding Meckels c rtil ge. In ddition, the rst rch contributes to form tion of the bones of the middle e r (see Ch pter 16). Muscul ture of the rst ph rynge l rch includes the muscles of m stic tion (tempor lis, m sseter, nd pterygoids), nterior belly of the dig stric,
368 P rt Two: Speci l Embryology A B C Figure 15.5 A. Front l view of n embryo of pproxim tely 24 d ys. The stomodeum , tempor rily closed by the buccoph rynge l membr ne, is surrounded by ve mesench ym l prominences. B. Front l view of slightly older embryo showing rupture of the buccoph rynge l membr ne nd form tion of the n s l pl codes on the fronton s l prominence. C. Sc nning electron microgr ph of hum n embryo simil r to th t shown in B. mylohyoid, tensor tymp ni, nd tensor p l tini. The nerve supply to the muscles of the rst rch is provided by the m ndibul r br nch of the trigemin l nerve (Fig . 15.7). Since mesenchyme from the rst rch lso contributes to the dermis of the f ce, sensory supply to the skin of the f ce is provided by ophth lmic, m xill ry, nd m ndibul r br nches of the trigemin l nerve. Muscles of the rches do no t lw ys tt ch to the bony or c rtil ginous components of their own rch but so metimes migr te into surrounding regions. Nevertheless, the origin of these musc les c n lw ys be tr ced, since their nerve supply is derived from the rch of o rigin.
Ch pter 15: He d nd Neck 369 Ph rynge l pouch Artery Nerve C rtil ge Ectoderm l epithelium Endoderm l epithel ium 1st ph rynge l rch Ph rynge l cleft 2nd rch with nerve, rtery, nd c rtil ge 3rd rch Mesenchym l tissue in 4th rch 4th rch L rynge l orifice A 1 2 3 B C Figure 15.6 A. Ph rynge l rches. E ch rch cont ins c rtil ginous component, cr ni l nerve, n rtery, nd muscul r component. B. Sc nning electron micro gr ph of the ph rynge l region of mouse embryo, showing the ph rynge l rches, pouches, nd clefts. The rst three rches (I, II, nd III) re visible. A remn n t of the buccoph rynge l membr ne ( rrow) is present t the entr nce to the or l c vity. C. Higher m gni c tion of the ph rynge l rches of mouse embryo. Ph ryn ge l rches consist of core of mesoderm lined by endoderm intern lly ( rrowhe ds) nd ectoderm extern lly ( rrows). Pouches nd clefts occur between the rche s, where endoderm nd ectoderm ppose e ch other.
370 P rt Two: Speci l Embryology Trigemin l g nglion F ci l nerve V X VII IX Ophth lmic br nch nerve V M xill ry br nch nerve V V gus nerve M ndibul r br nch nerve V Glossoph rynge l nerve Figure 15.7 E ch ph rynge l rch is supplied by its own cr ni l nerve. The trige min l nerve supplying the rst ph rynge l rch h s three br nches: the ophth lmic, m xill ry, nd m ndibul r. The nerve of the second rch is the f ci l nerve; th t of the third, the glossoph rynge l nerve. The muscul ture of the fourth rch is supplied by the superior l rynge l br nch of the v gus nerve, nd th t of the sixth rch, by the recurrent br nch of the v gus nerve. SECOND PHARYNGEAL ARCH The c rtil ge of the second or hyoid rch (Reicherts c rti l ge) (Fig. 15.8B) gives rise to the st pes, styloid process of the tempor l bon e, stylohyoid lig ment, nd ventr lly, the lesser horn nd upper p rt of the bod y of the hyoid bone (Fig. 15.9). Muscles of the hyoid rch re the st pedius, st ylohyoid, posterior belly of the dig stric, uricul r, nd muscles of f ci l exp ression. The f ci l nerve, the nerve of the second rch, supplies ll of these m uscles. THIRD PHARYNGEAL ARCH The c rtil ge of the third ph rynge l rch produce s the lower p rt of the body nd gre ter horn of the hyoid bone (Fig. 15.9). The muscul ture is limited to the styloph ryngeus muscles. These muscles re innerv ted by the glossoph rynge l nerve, the nerve of the third rch (Fig. 15.7). FOU RTH AND SIXTH PHARYNGEAL ARCHES C rtil ginous components of the fourth nd sixth ph rynge l rches fuse to form the thyroid, cricoid, rytenoid, cornicul te, n d cuneiform c rtil ges
Ch pter 15: He d nd Neck 371 A B Figure 15.8 A. L ter l view of the he d nd neck region of 4-week embryo demon str ting the c rtil ges of the ph rynge l rches p rticip ting in form tion of t he bones of the f ce nd neck. B. V rious components of the ph rynge l rches l ter in development. Some of the components ossify; others dis ppe r or become li g mentous. The m xill ry process nd Meckels c rtil ge re repl ced by the m xill nd m ndible, respectively, which develop by membr nous ossi c tion.
372 P rt Two: Speci l Embryology M lleus Incus St pes Meckel s c rtil ge Styloid process Stylohyoid lig ment Lesser horn of hyoid bone Gre ter horn of hyoid bond Body of hyoid bone Thyroid c rtil ge Cricoid c rtil ge Tr che l rings Figure 15.9 De nitive structures formed by the c rtil ginous components of the v r ious ph rynge l rches. of the l rynx (Fig. 15.9). Muscles of the fourth rch (cricothyroid, lev tor p l tini, nd constrictors of the ph rynx) re innerv ted by the superior l rynge l br nch of the v gus, the nerve of the fourth rch. Intrinsic muscles of the l r ynx re supplied by the recurrent l rynge l br nch of the v gus, the nerve of th e sixth rch. Ph rynge l Pouches The hum n embryo h s ve p irs of ph rynge l pouches (Figs. 15. 6 nd 15.10). The l st one of these is typic l nd often considered s p rt of the fourth. Since the epitheli l endoderm l lining of the pouches gives rise to number of import nt org ns, the f te of e ch pouch is discussed sep r tely. FI RST PHARYNGEAL POUCH The rst ph rynge l pouch forms st lklike diverticulum, the tubotymp nic recess, which comes in cont ct with the epitheli l lining of the rs t ph rynge l cleft, the future extern l uditory me tus (Fig. 15.10). The dist l portion of
Ch pter 15: He d nd Neck 373 M xill ry process M ndibul r process Ph rynge l clefts 1 I Ph rynge l pouches 1 Extern l uditory me tus I Primitive tymp nic c vity Auditory tube P l tine tons il III P r thyroid gl nd (inferior) Thymus II 2 2 III 3 IV 4 4 Cervic l sinus Epic rdi l ridge 3 II IV P r thyroid gl nd (superior) Ultimobr nchi l body A B Figure 15.10 A. Development of the ph rynge l clefts nd pouches. The second rc h grows over the third nd fourth rches, burying the second, third, nd fourth ph rynge l clefts. B. Remn nts of the second, third, nd fourth ph rynge l cleft s form the cervic l sinus, which is norm lly obliter ted. Note the structures fo rmed by the v rious ph rynge l pouches.
SECOND PHARYNGEAL POUCH The epitheli l lining of the second ph rynge l pouch pro lifer tes nd forms buds th t penetr te into the surrounding mesenchyme. The bud s re second rily inv ded by mesoderm l tissue, forming the primordium of the p l tine tonsil (Fig. 15.10). During the third nd fth months, the tonsil is in ltr t ed by lymph tic tissue. P rt of the pouch rem ins nd is found in the dult s t he tonsill r foss .
the diverticulum widens into s clike structure, the primitive tymp nic or midd le e r c vity, nd the proxim l p rt rem ins n rrow, forming the uditory (eust chi n) tube. The lining of the tymp nic c vity l ter ids in form tion of the ty mp nic membr ne or e rdrum (see Ch pter 16).
374 P rt Two: Speci l Embryology THIRD PHARYNGEAL POUCH The third nd fourth pouches re ch r cterized t their d ist l extremity by dors l nd ventr l wing (Fig. 15.10). In the fth week, epi thelium of the dors l wing of the third pouch differenti tes into the inferior p r thyroid gl nd, while the ventr l wing forms the thymus (Fig. 15.10). Both gl nd primordi lose their connection with the ph rynge l w ll, nd the thymus then migr tes in c ud l nd medi l direction, pulling the inferior p r thyroid w ith it (Fig. 15.11). Although the m in portion of the thymus moves r pidly to it s n l position in the nterior p rt of the thor x, where it fuses with its counte rp rt from the opposite side, its t il portion sometimes persists either embedde d in the thyroid gl nd or s isol ted thymic nests. Growth nd development of th e thymus continue until puberty. In the young child, the thymus occupies conside r ble sp ce in the thor x nd lies behind the sternum nd nterior to the peric rdium nd gre t vessels. In older Auditory tube Primitive tymp nic c vity Ventr l side of ph rynx Extern l uditor y me tus P l tine tonsil For men cecum Superior p r thyroid gl nd (from 4th pouch) Inferior p r thyroid gl nd (from 3rd pouch) Thyroid gl nd Ultimobr nchi l body Foregut Thymus Figure 15.11 Migr tion of the thymus, p r thyroid gl nds, nd ultimobr nchi l bo dy. The thyroid gl nd origin tes in the midline t the level of the for men cecu m nd descends to the level of the rst tr che l rings.
Ch pter 15: He d nd Neck 375 persons, it is dif cult to recognize, since it is trophied nd repl ced by f tty tissue. The p r thyroid tissue of the third pouch n lly comes to rest on the dors l surf ce of the thyroid gl nd nd forms the inferior p r thyroid gl nd (Fig. 1 5.11). FOURTH PHARYNGEAL POUCH Epithelium of the dors l wing of the fourth ph ry nge l pouch forms the superior p r thyroid gl nd. When the p r thyroid gl nd los es cont ct with the w ll of the ph rynx, it tt ches itself to the dors l surf c e of the c ud lly migr ting thyroid s the superior p r thyroid gl nd (Fig. 15.1 1). FIFTH PHARYNGEAL POUCH The fth ph rynge l pouch, the l st to develop, is usu lly considered to be p rt of the fourth pouch. It gives rise to the ultimobr n chi l body, which is l ter incorpor ted into the thyroid gl nd. Cells of the ult imobr nchi l body give rise to the p r follicul r, or C, cells of the thyroid gl nd. These cells secrete c lcitonin, hormone involved in regul tion of the c l cium level in the blood.
Ph rynge l Clefts The 5-week embryo is ch r cterized by the presence of four ph rynge l clefts (Fig. 15.6), of which only one contributes to the de nitive structu re of the embryo. The dors l p rt of the rst cleft penetr tes the underlying mese nchyme nd gives rise to the extern l uditory me tus (Figs. 15.10 nd 15.11). T he epitheli l lining t the bottom of the me tus p rticip tes in form tion of th e e rdrum (see Ch pter 16). Active prolifer tion of mesenchym l tissue in the se cond rch c uses it to overl p the third nd fourth rches. Fin lly, it merges w ith the epic rdi l ridge in the lower p rt of the neck (Fig. 15.10), nd the sec ond, third, nd fourth clefts lose cont ct with the outside (Fig. 15.10B ). The clefts form c vity lined with ectoderm l epithelium, the cervic l sinus, but w ith further development this sinus dis ppe rs. Molecul r Regul tion of F ci l Development As indic ted, much of the f ce is der ived from neur l crest cells th t migr te into the ph rynge l rches from the ed ges of the cr ni l neur l folds. In the hindbr in, crest cells origin te from se gmented regions known s rhombomeres. There re eight of these segments in the h indbr in (R1 to R8), nd crest cells
376 P rt Two: Speci l Embryology Figure 15.12 P tterns of neur l crest cell migr tion into the ph rynge l rches nd of HOX gene expression in rhombomeres of the hindbr in. HOX genes re expres sed in overl pping p tterns with those t the 3 end h ving the most rostr l boun d ries. This p ttern speci es deriv tives of e ch of the rhombomeres, including cr est cells nd their p thw ys of migr tion. The rst rch is lso popul ted by cres t cells from the midbr in. These cells express OTX2, tr nscription f ctor cont ining homeodom in. from speci c segments popul te speci c rches (Fig. 15.12). Crest cells from R1 nd R2 migr te to the rst rch, cells from R4 go to the second rch, those from R6 n d 7 to the third rch, nd those from R8 to the fourth nd sixth rches. In ddi tion, the rst rch receives crest cells origin ting in the midbr in. Few if ny c rest cells form from R3 nd R5. Most of the cells from these rhombomeres undergo cell de th by poptosis, while few migr te with crest cells origin ting from dj cent segments. P tterning of ph rynge l rches (with exception of the rst rc h) is regul ted by HOX genes c rried by migr ting neur l crest (Fig. 15.12). Exp ression of HOX genes in the hindbr in occurs in speci c overl pping p tterns, such th t the most 3 genes in cluster h ve the most rostr l bound ries (Fig. 15.12 ). Since 3 genes re the rst to be expressed, tempor l rel tionship for HOX gen e expression is lso est blished in rostroc ud l sequence. In ddition,
Ch pter 15: He d nd Neck 377 p r logous genes, for ex mple HOXA3, HOXB3, nd HOXD3 (see Ch pter 5 nd Fig. 5. 22), sh re identic l expression dom ins. These expression p tterns determine the org niz tion of cr ni l g ngli nd nerves nd p thw ys of neur l crest migr ti on. Initi lly, crest cells express the HOX genes from their segment of origin, b ut m inten nce of this speci c expression is dependent upon inter ction of these c ells with mesoderm in the ph rynge l rches. For ex mple, crest cells from the s econd rch express HOXA2, nd if these cells inter ct with second rch mesoderm, then this expression continues (Fig. 15.13). However, if second rch crest is p l ced into the rst rch, this expression is downregul ted. Thus, lthough n over l pping HOX code is essenti l to specifying the identity of the rches nd their deriv tives, crest cells lone do not est blish or m int in the expression p tt ern. How the code is tr nsl ted to control Figure 15.13 Schem tic dr wing showing the rel tionship between the rst two ph ry nge l rches (PA1 nd PA2), segment tion of region of the hindbr in t rhombom eres 2-5 (r2-r5), nd p thw ys of neur l crest cell migr tion (colors). A HOX co de is est blished in the hindbr in th t speci es the rches nd p thw ys of neur l crest cell migr tion (with exception of PA1). M inten nce of the code in the r ches is dependent upon n inter ction between crest cells nd rch-speci c mesoder m. P tterning of the rches into their deriv tives requires epitheli l-mesenchym l inter ctions nd includes molecul r sign ls from the surf ce ectoderm, i.e., b robl st growth f ctors (FGFs) cting upon underlying mesenchyme cells. OV, otic vesicle.
378 P rt Two: Speci l Embryology differenti tion of the rches is not known, but host of upstre m nd downstre m genes must be involved. Sonic hedgehog m y be one of the upstre m regul tors, since it is expressed in the rches nd h s been shown to regul te HOX gene expr ession. Retinoids (retinoic cid) c n lso regul te HOX gene expression in con centr tion-dependent m nner with genes t the 3 end being more responsive th n t hose in more 5 regions. Regul tion occurs through retinoic cid response element s (RAREs), which re binding sites for retinoic cid in the promoter regions of the HOX genes. De ciencies nd excesses of retinoids disrupt migr tion nd the xi l identity of hindbr in crest cells, resulting in severe cr niof ci l defects. In ddition to the HOX genes, OTX2 m y p rticip te in morphogenesis of the rst r ch. This gene, tr nscription f ctor import nt for br in development, cont ins homeodom in nd is expressed in forebr in nd midbr in regions (see Ch pter 19 ). Neur l crest cells th t migr te from the midbr in to the rst rch c rry OTX2 w ith them into this region. Presum bly, OTX2 nd possibly HOX genes in the rst rc h inter ct to p ttern this structure. CLINICAL CORRELATES Birth Defects Involving the Ph rynge l Region Ectopic Thymic nd P r thyroid Tis sue Since gl ndul r tissue derived from the pouches undergoes migr tion, it is n ot unusu l for ccessory gl nds or remn nts of tissue to persist long the p thw y. This is true p rticul rly for thymic tissue, which m y rem in in the neck, nd for the p r thyroid gl nds. The inferior p r thyroids re more v ri ble in po sition th n the superior ones nd re sometimes found t the bifurc tion of the common c rotid rtery. Br nchi l Fistul s Br nchi l stul s occur when the second ph rynge l rch f ils to grow c ud lly over the third nd fourth rches, le ving remn nts of the second, third, nd fourth clefts in cont ct with the surf ce by n rrow c n l (Fig. 15.14A). Such stul , found on the l ter l spect of the n eck directly nterior to the sternocleidom stoid muscle, usu lly provides dr in ge for l ter l cervic l cyst (Fig. 15.14B). These cysts, remn nts of the cervi c l sinus, re most often just below the ngle of the j w (Fig. 15.15), lthough they m y be found nywhere long the nterior border of the sternocleidom stoid muscle. Frequently l ter l cervic l cyst is not visible t birth but becomes evident s it enl rges during childhood. Intern l br nchi l stul s re r re; they occur when the cervic l sinus is connected to the lumen of the ph rynx by sm ll c n l, which usu lly opens in the tonsill r region (Fig. 15.14C ). Such stul results from rupture of the membr ne between the second ph rynge l cleft nd pouch t some time during development.
Ch pter 15: He d nd Neck 379 Extern l uditory me tus Region of pre uricul r fistul s Region of l ter l cervic l cysts nd fistul s
A B C
Figure 15.15 P tient with l ter l cervic l cyst. These cysts re lw ys on the l ter l side of the neck in front of the sternocleidom stoid muscle. They commo nly lie under the ngle of the m ndible nd do not enl rge until l ter in life.
Figure 15.14 A. L ter l cervic l cyst opening stul . B. L ter l cervic l cysts nd stul muscle. Note lso the region of pre uricul r pening into the ph rynx t the level of the p
t the side of the neck by w y of s in front of the sternocleidom stoid stul s. C. A l ter l cervic l cyst o l tine tonsil.
I II P l tine tonsil L ter l cervic l cyst Extern l br nchi l fistul
Tubotymp nic recess I P l tine tonsil Intern l br nchi l fistul L ter l cervic l cyst Sternocleidom stoid muscle II
380 P rt Two: Speci l Embryology Neur l Crest Cells nd Cr niof ci l Defects Neur l crest cells (Fig. 15.2) re e ssenti l for form tion of much of the cr niof ci l region. Consequently, disrupt ion of crest cell development results in severe cr niof ci l m lform tions. Sinc e crest cells lso contribute to the conotrunc l endoc rdi l cushions, which sep t te the out ow tr ct of the he rt into pulmon ry nd ortic ch nnels, m ny inf nt s with cr niof ci l defects lso h ve c rdi c bnorm lities, including persisten t truncus rteriosus, tetr logy of F llot, nd tr nsposition of the gre t vessel s. Unfortun tely, crest cells ppe r to be p rticul rly vulner ble cell popul tion nd re e sily killed by compounds such s lcohol nd retinoic cid. One r e son for this vulner bility m y be th t they re de cient in superoxide dismut se (SOD) nd c t l se enzymes th t re responsible for sc venging free r dic ls th t d m ge cells. Ex mples of cr niof ci l defects involving crest cells include the following: Tre cher Collins syndrome (m ndibulof ci l dysostosis) is ch r ct erized by m l r hypopl si due to underdevelopment of the zygom tic bones, m ndi bul r hypopl si , down-sl nting p lpebr l ssures, lower eyelid colobom s, nd m l formed extern l e rs (Fig. 15.16A). Tre cher Collins is inherited s n utosom l domin nt tr it, with 60% rising s new mut tions. However, phenocopies c n be produced in l bor tory nim ls following exposure to ter togenic doses of retin oic cid, suggesting th t some c ses in hum ns m y be c used by ter togens. Robi n sequence m y occur independently or in ssoci tion with other syndromes nd m lform tions. Like Tre cher Collins syndrome, Robin sequence lters rst- rch struc tures, with development of the m ndible most severely ffected. Inf nts usu lly h ve tri d of microgn thi , cleft p l te, nd glossoptosis (posteriorly pl ced tongue) (Fig. 15.16B). Robin sequence m y be due to genetic nd/or environment l f ctors. It m y lso occur s deform tion, s for ex mple when the chin is c ompressed g inst the chest in c ses of oligohydr mnios. The prim ry defect incl udes poor growth of the m ndible nd, s result, posteriorly pl ced tongue t h t f ils to drop from between the p l t l shelves, preventing their fusion. Rob in sequence occurs in pproxim tely 1/8500 births. DiGeorge nom ly occurs in p proxim tely 1 in 2000 to 3000 births nd represents the most severe ex mple of collection of disorders th t lso includes veloc rdiof ci l syndrome (VCFS) nd conotrunc l nom lies f ce syndrome (Fig. 15.16C). All of these disorders re p rt of spectrum c lled CATCH22 bec use they include c rdi c defects, bnorm l f cies, thymic hypopl si , cleft p l te, nd hypoc lcemi nd re result of deletion on the long rm of chromosome 22 (22q11). P tients with complete DiGeor ge nom ly h ve immunologic l de ciencies, hypoc lcemi , nd poor prognosis. Ori gin of the defects is c used by bnorm l development of neur l crest cells th t contribute to form tion of ll of the ffected structures. In ddition
Ch pter 15: He d nd Neck 381 A B C D Figure 15.16 P tients with cr niof ci l defects thought to rise from insults to neur l crest cells. A. Tre cher Collins syndrome (m ndibulof ci l dysostosis). Note underdevelopment of the zygom tic bones, sm ll m ndible, nd m lformed e rs . B. Robin sequence. Note the very sm ll m ndible (microgn thi ). C. DiGeorge n om ly. In ddition to cr niof ci l defects, such s hypertelorism nd microstomi , these individu ls h ve p rti l or complete bsence of the thymus. D. Hemif ci l microsomi (oculo uriculovertebr l spectrum, or Goldenh r syndrome).
382 P rt Two: Speci l Embryology to genetic c uses, exposure to retinoids (vit min A), lcohol, nd m tern l di b etes c n produce the defects. Hemif ci l microsomi (oculo uriculovertebr l spec trum, Goldenh r syndrome) includes number of cr niof ci l bnorm lities th t u su lly involve the m xill ry, tempor l, nd zygom tic bones, which re sm ll nd t. E r ( noti , microti ), eye (tumors nd dermoids in the eyeb ll), nd verteb r l (fused nd hemivertebr e, spin bi d ) defects re commonly observed in these p tients (Fig. 15.16D). Asymmetry is present in 65% of the c ses, which occur in 1/5600 births. Other m lform tions, which occur in 50% of c ses, include c rdi c bnorm lities, such s tetr logy of F llot nd ventricul r sept l defects. C u ses of hemif ci l microsomi re unknown. Tongue The tongue ppe rs in embryos of pproxim tely 4 weeks in the form of two l ter l lingu l swellings nd one medi l swelling, the tuberculum imp r (Fig. 1 5.17, A nd C ). These three swellings origin te from the rst ph rynge l rch. A second medi n swelling, the copul , or hypobr nchi l eminence, is formed by meso derm of the second, third, nd p rt of the fourth rch. Fin lly, third medi n swelling, formed by the posterior p rt of the fourth rch, m rks development of the epiglottis. Immedi tely behind this swelling is the l rynge l ori ce, which is nked by the rytenoid swellings (Fig. 15.17,A nd C ). As the l ter l lingu l s wellings incre se in size, they overgrow the tuberculum imp r nd merge, forming the nterior two-thirds, or body, of the tongue (Fig. 15.17, B nd D). Since th e mucos covering the body of the tongue origin tes from the rst ph rynge l rch, sensory innerv tion to this re is by the m ndibul r br nch of the trigemin l nerve. The body of the tongue is sep r ted from the posterior third by V-sh pe d groove, the termin l sulcus (Fig. 15.17, B nd D). The posterior p rt, or root , of the tongue origin tes from the second, third, nd p rt of the fourth ph ryn ge l rch. The f ct th t sensory innerv tion to this p rt of the tongue is suppl ied by the glossoph rynge l nerve indic tes th t tissue of the third rch overgr ows th t of the second. The epiglottis nd the extreme posterior p rt of the ton gue re innerv ted by the superior l rynge l nerve, re ecting their development fr om the fourth rch. Some of the tongue muscles prob bly differenti te in situ, b ut most re derived from myobl sts origin ting in occipit l somites. Thus, tongu e muscul ture is innerv ted by the hypogloss l nerve. The gener l sensory innerv tion of the tongue is e sy to underst nd. The body is supplied by the trigemin l nerve, the nerve of the rst rch; th t of the root is supplied by the glossoph rynge l nd v gus nerves, the nerves of the third nd fourth rches, respectivel y. Speci l sensory innerv tion (t ste)
Ch pter 15: He d nd Neck 383 L ter l lingu l swelling Tuberculum imp r Termin l sulcus Body of tongue Copul (hypobr nchi l eminence) Epiglott l swelling For men cecum L rynge l orifice Arytenoid swellings P l tine tonsil Root of tongue Epiglottis A B C D Figure 15.17 Ventr l portion of the ph rynge l rches seen from bove showing de velopment of the tongue. I to I V, the cut ph rynge l rches. A. 5 weeks ( pprox im tely 6 mm). B. 5 months. Note the for men cecum, site of origin of the thyroi d primordium. C nd D. Sc nning electron microgr phs of simil r st ges of tongue development in hum n embryos. A depression m rks the loc tion of the for men ce cum ( rrowhe ds). to the nterior two thirds of the tongue is provided by the chord tymp ni br nc h of the f ci l nerve, while the posterior third is supplied by the glossoph ryn ge l nerve. CLINICAL CORRELATES Tongue-Tie In nkyloglossi (tongue-tie) the tongue is not freed from the oor of the mouth. Norm lly, extensive cell degener tion occurs, nd the frenulum is the only tissue th t nchors the tongue to the oor of the mouth. In the most common form of nkyloglossi , the frenulum extends to the tip of the tongue.
384 P rt Two: Speci l Embryology Thyroid Gl nd The thyroid gl nd ppe rs s n epitheli l prolifer tion in the oor of the ph rynx between the tuberculum imp r nd the copul t point l ter ind ic ted by the for men cecum (Figs. 15.17 nd 15.18A). Subsequently the thyroid d escends in front of the ph rynge l gut s bilobed diverticulum (Fig. 15.18). D uring this migr tion, the thyroid rem ins connected to the tongue by n rrow c n l, the thyrogloss l duct. This duct l ter dis ppe rs. With further development , the thyroid gl nd descends in front of the hyoid bone nd the l rynge l c rtil ges. It re ches its n l position in front of the tr che in the seventh week (Fi g. 15.18B). By then it h s cquired sm ll medi n isthmus nd two l ter l lobes . The thyroid begins to function t pproxim tely the end of the third month, t which time the rst follicles cont ining colloid become visible. Follicul r cells produce the colloid th t serves s source of thyroxine nd triiodothyronine. P r follicul r, or C, cells derived from the ultimobr nchi l body (Fig. 15.10) s erve s source of c lcitonin. CLINICAL CORRELATES Thyrogloss l Duct nd Thyroid Abnorm lities A thyrogloss l cyst m y lie t ny p oint long the migr tory p thw y of the thyroid gl nd but is lw ys ne r or in t he midline of the neck. As indic ted by its n me, it is cystic remn nt of the thyrogloss l duct, Although pproxim tely 50% of these cysts re close to or jus t inferior to the body of the hyoid bone (Figs. 15.19 nd 15.20), they m y lso be found t the b se of the tongue or close to the thyroid c rtil ge. Sometimes thyrogloss l cyst is connected to the outside by stulous c n l, thyrogloss l stul . Such stul usu lly rises second rily fter rupture of cyst but m y b e present t birth. Figure 15.18 A. The thyroid primordium rises s n epitheli l diverticulum in t he midline of the ph rynx immedi tely c ud l to the tuberculum imp r. B. Positio n of the thyroid gl nd in the dult. Broken line, the p th of migr tion.
Ch pter 15: He d nd Neck 385 Figure 15.19 Thyrogloss l cysts. These cysts, most frequently found in the hyoid region, re lw ys close to the midline. Figure 15.20 Thyrogloss l cyst. These cysts, which re remn nts of the thyroglos s l duct, m y be nywhere long the migr tion p thw y of the thyroid gl nd. They re commonly found behind the rch of the hyoid bone. An import nt di gnostic c h r cteristic is their midline loc tion.
386 P rt Two: Speci l Embryology Aberr nt thyroid tissue m y be found nywhere long the p th of descent of the t hyroid gl nd. It is commonly found in the b se of the tongue, just behind the fo r men cecum, nd is subject to the s me dise ses s the thyroid gl nd itself. F ce At the end of the fourth week, f ci l prominences consisting prim rily of n eur l crest-derived mesenchyme nd formed m inly by the rst p ir of ph rynge l r ches ppe r. M xill ry prominences c n be distinguished l ter l to the stomodeum , nd m ndibul r prominences c n be distinguished c ud l to this structure (Fig. 15.21). The fronton s l prominence, formed by prolifer tion of mesenchyme ventr l to the br in vesicles, constitutes the upper border of the stomodeum. On both sides of the fronton s l prominence, loc l thickenings of the surf ce ectoderm, the n s l (olf ctory) pl codes, origin te under inductive in uence of the ventr l portion of the forebr in (Fig. 15.21). During the fth week, the n s l pl codes i nv gin te to form n s l pits. In so doing, they cre te ridge of tissue th t su rrounds e ch pit nd forms the n s l prominences. The prominences on the outer e dge of the pits re the l ter l n s l prominences; those on the inner edge re t he medi l n s l prominences (Fig. 15.22) During the following 2 weeks, the m xil l ry prominences continue to incre se in size. Simult neously, they grow medi ll y, compressing the medi l n s l prominences tow rd the midline. Subsequently the cleft between the medi l n s l prominence nd the m xill ry prominence is lost, nd the two fuse (Fig. 15.23). Hence, the upper lip is formed by the two medi l n s l prominences nd the two m xill ry prominences. The l ter l n s l prominen ces do not p rticip te in form tion of the upper lip. The lower lip nd j w form from the m ndibul r prominences th t merge cross the midline. Initi lly, the m xill ry nd l ter l n s l prominences re sep r ted by deep furrow, the n sol crim l groove (Figs. 15.22 nd 15.23). Ectoderm in the oor of this groove forms solid epitheli l cord th t det ches from the overlying ectoderm. After c n liz tion, the cord forms the n sol crim l duct; its upper end widens to form the l crim l s c. Following det chment of the cord, the m xill ry nd l ter l n s l pr ominences merge with e ch other. The n sol crim l duct then runs from the medi l corner of the eye to the inferior me tus of the n s l c vity, nd the m xill ry prominences enl rge to form the cheeks nd m xill e. The nose is formed from ve f ci l prominences (Fig. 15.23): the front l prominence gives rise to the bridge ; the merged medi l n s l prominences provide the crest nd tip; nd the l ter l n s l prominences form the sides ( l e) (T ble 15.2, p. 389).
Ch pter 15: He d nd Neck 387 A B C Figure 15.21 A. L ter l view of n embryo t the end of the fourth week, showing position of the ph rynge l rches. B. Front l view of 4.5-week embryo showing the m ndibul r nd m xill ry prominences. The n s l pl codes re visible on eit her side of the fronton s l prominence. C. Sc nning electron microgr ph of hum n embryo t st ge simil r to th t of B. Interm xill ry Segment As result of medi l growth of the m xill ry prominences , the two medi l n s l prominences merge not only t the surf ce but lso t d eeper level. The structure formed by the two merged prominences is the interm xi ll ry segment. It is composed of ( ) l bi l component, which forms the philtru m of the upper lip; (b) n upper j w component, which c rries the four incisor t eeth; nd (c) p l t l component, which forms the tri ngul r prim ry p l te (Fi g. 15.24). The interm xill ry segment is continuous
388 P rt Two: Speci l Embryology Fronton s l prominence N s l pit M xill ry prominence M ndibul r prominence Eye A B N sol crim l groove Stomodeum N s l pit L ter l n s l prominence Medi l n s l prominence C Figure 15.22 Front l spect of the f ce. A. 5-week embryo. B. 6-week embryo. The n s l prominences re gr du lly sep r ted from the m xill ry prominence by deep furrows. C. Sc nning electron microgr ph of mouse embryo t st ge simil r t o th t of B. with the rostr l portion of the n s l septum, which is formed by the front l pro minence. Second ry P l te Although the prim ry p l te is derived from the interm xill ry segment (Fig. 15.24), the m in p rt of the de nitive p l te is formed by two shel ik e
Ch pter 15: He d nd Neck 389 L ter l n s l prominence Medi l n s l prominence M xill ry prominence M ndibul r prominence Eye A N sol crim l groove B Philtrum C Figure 15.23 Front l spect of the f ce. A. 7-week embryo. M xill ry prominences h ve fused with the medi l n s l prominences. B. 10-week embryo. C. Sc nning el ectron microgr ph of hum n embryo t st ge simil r to th t of A. TABLE 15.2 Prominence
Fronton s l M xill ry Medi l n s l L ter l n s l M ndibul r
The fronton s l prominence is re p ired.
single unp ired structure; the other prominences
Structures Structures Cheeks, l se Al e of
Contributing to Form tion of the F ce Formed Forehe d, bridge of nose, medi l nd l ter l n s l prominences ter l portion of upper lip Philtrum of upper lip, crest nd tip of no nose Lower lip
390 P rt Two: Speci l Embryology Figure 15.24 A. Interm xill ry segment nd m xill ry processes. B. The interm xi ll ry segment giving rise to the philtrum of the upper lip, the medi n p rt of t he m xill ry bone with its four incisor teeth, nd the tri ngul r prim ry p l te . outgrowths from the m xill ry prominences. These outgrowths, the p l tine shelve s, ppe r in the sixth week of development nd re directed obliquely downw rd o n e ch side of the tongue (Fig. 15.25). In the seventh week, however, the p l ti ne shelves scend to tt in horizont l position bove the tongue nd fuse, for ming the second ry p l te (Figs. 15.26 nd 15.27). Anteriorly, the shelves fuse with the tri ngul r prim ry p l te, nd the incisive for men is the midline l nd m rk between the prim ry nd second ry p l tes (Fig. 15.27B ). At the s me time s the p l tine shelves fuse, the n s l septum grows down nd joins with the cep h lic spect of the newly formed p l te (Fig. 15.27). CLINICAL CORRELATES F ci l Clefts Cleft lip nd cleft p l te re common defects th t result in bnor m l f ci l ppe r nce nd defective speech. The incisive for men is considered t he dividing l ndm rk between the nterior nd posterior cleft deformities. Those nterior to the incisive for men include l ter l cleft lip, cleft upper j w, n d cleft between the prim ry nd second ry p l tes (Figs. 15.28, B nd D, nd 15. 29, A nd B). Such defects re due to p rti l or complete l ck of fusion of th e m xill ry prominence with the medi l n s l prominence on one or both sides. Th ose th t lie posterior to the incisive for men include cleft (second ry) p l te nd cleft uvul (Figs. 15.28E nd 15.29, C nd D). Cleft p l te results from l ck of fusion of the p l tine shelves, which m y be due to sm llness of the shel ves, f ilure of the shelves to elev te, inhibition of the fusion process itself, or f ilure of the tongue to drop from between the shelves bec use of microgn th i . The third c tegory is formed by combin tion of clefts lying nterior s we ll s posterior to the incisive for men (Fig. 15.28F ).
Ch pter 15: He d nd Neck 391 A B C D Figure 15.25 A. Front l section through the he d of 6.5-week-old embryo. The p l tine shelves re in the vertic l position on e ch side of the tongue. B. Vent r l view of the p l tine shelves fter remov l of the lower j w nd the tongue. Note the clefts between the prim ry tri ngul r p l te nd the p l tine shelves, which re still vertic l. C. Sc nning electron microgr ph of mouse embryo t st ge simil r to th t of A. D. P l t l shelves t st ge slightly older th n t hose in B. The shelves h ve elev ted, but they re widely sep r ted. The prim ry p l te h s fused with the second ry p l t l shelves.
Anterior clefts v ry in severity from b rely visible defect in the vermilion o f the lip to extension into the nose (Fig. 15.29A). In severe c ses the cleft ex tends to deeper level, forming cleft of the upper j w, nd the m xill is sp lit between the l ter l incisor nd the c nine tooth. Frequently such cleft ex tends to the incisive for men (Fig. 15.28, C nd D). Likewise, posterior clefts v ry in severity from cle v ge of the entire second ry p l te (Fig. 15.29D) to c le v ge of the uvul only. Oblique f ci l clefts re produced by f ilure of the m xill ry prominence to merge with its corresponding l ter l n s l prominence. W hen this occurs, the n sol crim l duct is usu lly exposed to the surf ce (Fig. 1 5.29E ). Medi n cleft lip, r re bnorm lity, is c used by incomplete merging o f the two medi l n s l prominences in the midline. This nom ly is usu lly ccom p nied by deep groove between the right nd left sides of the nose
392 P rt Two: Speci l Embryology A B C D
(Fig. 15.29F ). Inf nts with midline clefts re often ment lly ret rded nd m y h ve br in bnorm lities th t include v rying degrees of loss of midline structu res. Loss of midline tissue m y be so extensive th t the l ter l ventricles fuse (holoprosenceph ly). These defects re induced very e rly in development, t th e beginning of neurul tion (d ys 1921) when the midline of the forebr in is being est blished. Most c ses of cleft lip nd cleft p l te re multif ctori l. Cleft lip ( pproxim tely 1/1000 births) occurs more frequently in m les (80%) th n in fem les; its incidence incre ses slightly with m tern l ge, nd it v ries mon g popul tions. If norm l p rents h ve one child with cleft lip, the ch nce th t the next b by will h ve the s me defect is 4%. If two siblings re ffected, t he risk for the next child incre ses to 9%. If one of the p rents h s cleft li p nd they h ve one child with the s me defect, the prob bility th t the next b by will be ffected rises to 17%.
Figure 15.26 A. Front l section through the he d e h s moved downw rd, nd the p l tine shelves h n. B. Ventr l view of the p l tine shelves fter ngue. The shelves re horizont l. Note the n s l crogr ph of mouse embryo t st ge simil r to t st ge simil r to th t of B.
of 7.5-week embryo. The tongu ve re ched horizont l positio remov l of the lower j w nd to septum. C. Sc nning electron mi th t of A. D. P l t l shelves
Ch pter 15: He d nd Neck 393 A B
The frequency of isol ted cleft p l te is much lower th n th t of cleft lip (1/2 500 births), occurs more often in fem les (67%) th n in m les, nd is not rel te d to m tern l ge. If the p rents re norm l nd h ve one child with cleft p l te, the prob bility of the next child being ffected is bout 2%. If, however, there is simil rly ffected child nd rel tive or p rent both with cleft p l te, the prob bility incre ses to 7% nd 15%, respectively. In fem les, the p l t l shelves fuse pproxim tely 1 week l ter th n in m les. This difference m y expl in why isol ted cleft p l te occurs more frequently in fem les th n in m l es. Anticonvuls nt drugs, such s phenob rbit l nd diphenylhyd ntoin, given dur ing pregn ncy incre se the risk of cleft p l te.
C Figure 15.27 A. Front l section through the he d of 10-week embryo. The two p l tine shelves h ve fused with e ch other nd with the n s l septum. B. Ventr l view of the p l te. The incisive for men forms the midline between the prim ry nd second ry p l te. C. Sc nning electron microgr ph of the p l t l shelves of mouse embryo t st ge simil r to th t of B.
394 P rt Two: Speci l Embryology
A B C D E F Figure 15.29 A. Incomplete cleft lip. B. Bil ter l cleft lip. C. Cleft lip, clef t j w, nd cleft p l te. D. Isol ted cleft p l te. E. Oblique f ci l cleft. F. M idline cleft lip.
Figure 15.28 Ventr l view of the p l te, ter l cleft lip extending into the nose. nd j w nd extending to the incisive for ip nd j w. E. Isol ted cleft p l te. F. nterior cleft lip.
gum, lip, nd nose. A. Norm l. B. Unil C. Unil ter l cleft involving the lip men. D. Bil ter l cleft involving the l Cleft p l te combined with unil ter l
Ch pter 15: He d nd Neck 395 W ll of br in N s l pit Medi l n s l prominence Bre kdown of oron s l membr ne Or l c vity Or l c vity A Oron s l membr ne Tongue B Tongue Conch e N s l ch mber Primitive cho n Prim ry p l te M xill Upper lip Lower li p M ndible Second ry p l te Definitive cho n C D Figure 15.30 A. S gitt l section through the n s l pit nd lower rim of the medi l n s l prominence of 6-week embryo. The primitive n s l c vity is sep r ted from the or l c vity by the oron s l membr ne. B. Simil r section s in A showin g the oron s l membr ne bre king down. C. A 7-week embryo with primitive n s l c vity in open connection with the or l c vity. D. S gitt l section through the f ce of 9-week embryo showing sep r tion of the de nitive n s l nd or l c viti es by the prim ry nd second ry p l te. De nitive cho n e re t the junction of t he or l c vity nd the ph rynx. N s l C vities During the sixth week, the n s l pits deepen consider bly, p rtly bec use of growth of the surrounding n s l prominences nd p rtly bec use of th eir penetr tion into the underlying mesenchyme (Fig. 15.30A). At rst the oron s l membr ne sep r tes the pits from the primitive or l c vity by w y of the newly formed for min , the primitive cho n e (Fig. 15.30C ). These cho n e lie on e ch side of the midline nd immedi tely behind the prim ry p l te. L ter, with form tion of the second ry p l te nd further development of the primitive n s l ch mbers (Fig. 15.30D), the de nitive cho n e lie t the junction of the n s l c vity nd the ph rynx. P r n s l ir sinuses develop s diverticul of the l ter l n s l w ll nd extend into the m xill , ethmoid, front l, nd sphenoid bones. They re ch their m ximum size during puberty nd contribute to the de nitive sh pe of the f ce. Teeth The sh pe of the f ce is determined not only by exp nsion of the p r n s l sinuses but lso by growth of the m ndible nd m xill to ccommod te
396 P rt Two: Speci l Embryology the teeth. Teeth themselves rise from n epitheli l-mesenchym l inter ction bet ween overlying or l epithelium nd underlying mesenchyme derived from neur l cre st cells. By the sixth week of development, the b s l l yer of the epitheli l li ning of the or l c vity forms C-sh ped structure, the dent l l min , long the length of the upper nd lower j ws. This l min subsequently gives rise to nu mber of dent l buds (Fig. 15.31A), 10 in e ch j w, which form the primordi of t he ectoderm l components of the teeth. Soon the deep surf ce of the buds inv gin tes, resulting in the c p st ge of tooth development (Fig. 15.31B). Such c p consists of n outer l yer, the outer dent l epithelium, n inner l yer, the inn er dent l epithelium, nd centr l core of loosely woven tissue, the stell te r eticulum. The mesenchyme, which origin tes in the neur l crest in the indent tio n, forms the dent l p pill (Fig. 15.31B ). As the dent l c p grows nd the inde nt tion deepens, the tooth t kes on the ppe r nce of bell (bell st ge) (Fig. 15.31C ). Mesenchyme cells of the p pill dj cent to the inner dent l l yer dif ferenti te into odontobl sts, which l ter produce dentin. With thickening of the dentin l yer, odontobl sts retre t into the dent l p pill , le ving thin cyto pl smic process (dent l process) behind in the dentin (Fig. 15.31D). The odontob l st l yer persists throughout the life of the tooth nd continuously provides p redentin. The rem ining cells of the dent l p pill form the pulp of the tooth ( Fig. 15.31D). Dent l l min Or l epithelium Mesenchyme j w En mel knot Perm nent tooth bud Inn er Dent l Outer epithelium Dent l p pill Dent l bud A B Stell te reticulum En mel Dentine Amelobl sts Dent l pulp Root she th Odontobl sts C D Figure 15.31 Form tion of the tooth t successive st ges of development. A. Bud st ge; 8 weeks. B. C p st ge; 10 weeks. C. Bell st ge; 3 months. D. 6 months.
Ch pter 15: He d nd Neck 397 In the me ntime, epitheli l cells of the inner dent l epithelium differenti te i nto melobl sts (en mel formers). These cells produce long en mel prisms th t r e deposited over the dentin (Fig. 15.31D). Furthermore, cluster of these cells in the inner dent l epithelium forms the en mel knot th t regul tes e rly tooth development (Fig. 15.31B). En mel is rst l id down t the pex of the tooth nd from here spre ds tow rd the neck. When the en mel thickens, the melobl sts ret re t into the stell te reticulum. Here they regress, tempor rily le ving thin membr ne (dent l cuticle) on the surf ce of the en mel. After eruption of the to oth, this membr ne gr du lly sloughs off. Form tion of the root of the tooth beg ins when the dent l epitheli l l yers penetr te into the underlying mesenchyme nd form the epitheli l root she th (Fig. 15.31D). Cells of the dent l p pill l y down l yer of dentin continuous with th t of the crown (Fig. 15.32). As more nd more dentin is deposited, the pulp ch mber n rrows nd n lly forms c n l c ont ining blood vessels nd nerves of the tooth. Mesenchym l cells on the outsid e of the tooth nd in cont ct with dentin of the root differenti te into cemento bl sts (Fig. 15.32A). These cells produce thin l yer of speci lized bone, the cementum. Outside of the cement l yer, mesenchyme gives rise to the periodont l lig ment (Fig. 15.32), which holds the tooth rmly in position nd functions s shock bsorber. With further lengthening of the root, the crown is gr du lly pus hed through the overlying tissue l yers into the or l c vity (Fig. 15.32B). The eruption of deciduous or milk teeth occurs 6 to 24 months fter birth. Buds for the perm nent teeth, which lie on the lingu l spect of the milk teeth, re form ed during the third month of development. These buds rem in dorm nt until pprox im tely the sixth ye r of postn t l life (Fig. 15.33). Then En mel Dentin Cementobl sts Periodont l lig ment Cementum A B Bone of socket
Figure 15.32 The tooth just before birth (A)
nd fter eruption (B).
398 P rt Two: Speci l Embryology
they begin to grow, pushing g inst the underside of the milk teeth nd iding i n the shedding of them. As perm nent tooth grows, the root of the overlying de ciduous tooth is resorbed by osteocl sts. Molecul r Regul tion of Tooth Developm ent Teeth re present only in vertebr tes nd p r llel the evolution ry ppe r n ce of the neur l crest. Tooth development represents cl ssic ex mple of n epi theli l-mesenchym l inter ction, in this c se between the overlying epithelium nd underlying neur l crest derived mesenchyme. Regul tion of tooth p tterning fr om incisors to mol rs is gener ted by combin tori l expression of HOX genes ex pressed in the mesenchyme. With respect to e ch tooths individu l development, th e epithelium governs differenti tion to the bud st ge, t which time this regul tory function is tr nsferred to the mesenchyme. Sign ls for development involve growth f ctors including: WNTs, bone morphogenetic proteins (BMPs), nd brobl st growth f ctors (FGFs); the secreted f ctor sonic hedgehog (SHH); nd tr nscripti on f ctors, such s MSX1 nd 2 th t inter ct in complex p thw y to produce cel l differenti tion nd p tterning for e ch tooth. Teeth lso ppe r to h ve sig n ling center th t represents the org nizer for tooth development much like the c tivity of the node during g strul tion (see Ch pter 4). This org nizer region is c lled the en mel knot, nd it ppe rs in
Figure 15.33 Repl cement of deciduous teeth by perm nent teeth in r 9 ye rs.
child of 8 o
Ch pter 15: He d nd Neck 399 circumscribed region of the dent l epithelium t the tips of the tooth buds. I t then enl rges t the c p st ge into tightly p cked group of cells but underg oes poptosis (cell de th) nd dis ppe rs by the end of this st ge (Fig. 15.31). While it is present, it expresses FGF-4, SHH, nd BMP2 nd 4. FGF-4 m y regul t e outgrowth of cusps much s it p rticip tes in limb outgrowth produced by the pic l ectoderm l ridge (AER); while BMP-4 m y regul te the timing of poptosis i n knot cells. CLINICAL CORRELATES
Tooth Abnorm lities N t l teeth h ve erupted by the time of birth. Usu lly they involve the m ndibul r incisors, which m y be bnorm lly formed nd h ve little en mel. Teeth m y be bnorm l in number, sh pe, nd size. They m y be discolored by foreign subst nces, such s tetr cyclines, or be de cient in en mel, conditi on often c used by vit min D de ciency (rickets). M ny f ctors ffect tooth develo pment, including genetic nd environment l in uences. Summ ry Ph rynge l (br nchi l) rches, consisting of b rs of mesenchym l tissue sep r ted by ph rynge l pouches nd clefts, give the he d nd neck their typic l ppe r nce in the fourth week (Fig. 15.3). E ch rch cont ins its own rtery (F ig. 15.4), cr ni l nerve (Fig. 15.7), muscle element, nd c rtil ge b r or skele t l element (Figs. 15.8 nd 15.9; T ble 15.1, p. 366). Endoderm of the ph rynge l pouches gives rise to number of endocrine gl nds nd p rt of the middle e r. In subsequent order the pouches give rise to ( ) the middle e r c vity nd udi tory tube (pouch 1), (b) the strom of the p l tine tonsil (pouch 2), (c) the in ferior p r thyroid gl nds nd thymus (pouch 3), nd (d) the superior p r thyroid gl nds nd ultimobr nchi l body (pouches 4 nd 5) (Fig. 15.10). Ph rynge l clef ts give rise to only one structure, the extern l uditory me tus. Molecul r cont rol of rch development resides in HOX genes, whose ph rynge l rch code is c rr ied to the rches by neur l crest cells migr ting from hindbr in segments known s rhombomeres (Fig. 15.12). This code is then m int ined by inter ctions betwee n crest cells nd rch mesoderm (Fig. 15.13). The thyroid gl nd origin tes from n epitheli l prolifer tion in the oor of the tongue nd descends to its level in front of the tr che l rings in the course of development. The p ired m xill ry nd m ndibul r prominences nd the fronton s l prominence re the rst prominences of the f ci l region. L ter, medi l nd l ter l n s l prominences form round t he n s l pl codes on the fronton s l prominence. All of these structures re imp ort nt, since they determine,
400 P rt Two: Speci l Embryology through fusion nd speci lized growth, the size nd integrity of the m ndible, u pper lip, p l te, nd nose (T ble 15.2, p. 389). Form tion of the upper lip occu rs by fusion of the two m xill ry prominences with the two medi l n s l prominen ces (Figs. 15.22 nd 15.23). The interm xill ry segment is formed by merging of the two medi l n s l prominences in the midline. This segment is composed of ( ) the philtrum, (b) the upper j w component, which c rries the four incisor teeth , nd (c) the p l t l component, which forms the tri ngul r prim ry p l te. The nose is derived from ( ) the fronton s l prominence, which forms the bridge, (b) the medi l n s l prominences, which provide the crest nd tip, nd (c) the l te r l n s l prominences, which form the l e (Fig. 15.23). Fusion of the p l t l s helves, which form from the m xill ry prominences, cre tes the h rd (second ry) nd soft p l te. A series of cleft deformities m y result from p rti l or incomp lete fusion of these mesenchym l tissues, which m y be c used by heredit ry f ct ors nd drugs (diphenylhyd ntoin). The dult form of the f ce is in uenced by deve lopment of p r n s l sinuses, n s l conch e, nd teeth. Teeth develop from epith eli l-mesenchym l inter ctions between or l epithelium nd neur l crest derived mesenchyme. En mel is m de by melobl sts (Figs. 15.31 nd 15.32). It lies on thick l yer of dentin produced by odontobl sts, neur l crest deriv tive. Cemen tum is formed by cementobl sts, nother mesenchym l deriv tive found in the root of the tooth. The rst teeth (deciduous teeth, or milk teeth) ppe r 6 to 24 mont hs fter birth, nd the de nitive or perm nent teeth, which suppl nt the milk teet h, re formed during the third month of development (Fig. 15.33). Problems to Solve 1. Why re neur l crest cells considered such n import nt cel l popul tion for cr niof ci l development? 2. You re c lled s consult nt for child with very sm ll m ndible nd e rs th t re represented by sm ll protu ber nces bil ter lly. The b by h s h d numerous episodes of pneumoni nd is sm ll for its ge. Wh t might your di gnosis be, nd wh t might h ve c used these bnorm lities? 3. A child is born with medi n cleft lip. Should you be concerne d bout ny other bnorm lities? 4. A child presents with midline swelling ben e th the rch of the hyoid bone. Wh t might this swelling be, nd wh t is its b sis embryologic lly?
SUGGESTED READING Fr ncis-West P, L dher R, B rlow A, Gr veson A: Sign ling inte r ctions during f ci l development. Mech Dev 75:3, 1998. Freidberg J: Ph rynge l cleft sinuses nd cysts, nd other benign neck lesions. Pedi tr Clin North Am 3 6:1451, 1989.
Ch pter 15: He d nd Neck 401 Gorlin RJ, Cohen MM, Levin LS (eds): Syndromes of the He d nd Neck. 4th ed. New York, Oxford University, 2002. Hong R, The DiGeorge nom ly (C tch22, DiGeorge/ Veloc rdiof ci l syndrome). Sem Hem tol 35:282, 1998. Ji ng X, Iseki S, M xson R E, Sucov HM, Morriss-K y GM: Tissue origins nd inter ctions in the m mm li n sk ull v ult. Dev Biol 241:106, 2002. Lumsden A, Spr wson N, Gr h m A: Segment l or igin nd migr tion of neur l crest cells in the hindbr in region of the chick em bryo. Development 113:1281, 1991. Nichols DH: Mesenchyme form tion from the trig emin l pl codes of the mouse embryo. Am J An t 176:1931, 1986. Noden DM: Cell mo vements nd control of p tterned tissue ssembly during cr niof ci l development . J Cr niof c Genet Dev Biol 11:192, 1991. Osumi-Y m shit N, Ninomiy Y, Doi H, Eto K: The contribution of both forebr in nd midbr in crest cells to the mesen chyme in the fronton s l m ss of mouse embryos. Dev Biol 164(2):409, 1994. Sulik KK, Cook CS, Webster WS: Ter togens nd cr niof ci l m lform tions: rel tionshi ps to cell de th. Dev Suppl 103:213, 1988. Sulik KK, et l.: Fet l lcohol syndr ome nd DiGeorge nom ly: critic l eth nol exposure periods for cr niof ci l m l form tion s illustr ted in n nim l model. Am J Med Genet 2(suppl):97, 1986. S ulik KK, Schoenwokf GC: Highlights of cr niof ci l morphogenesis in m mm li n em bryos, s reve led by sc nning electron microscopy. Sc nning Electron Microsc 4: 1735, 1985. Thesleff I, Sh rpe P: Sign ling networks regul ting dent l developme nt. Mech Dev 67:111, 1997. Thorogood P: The he d nd f ce. In Thorogood P (ed): Embryos, Genes, nd Birth Defects. New York, Wiley & Sons, 1997. Tr inor PA, Kru ml uf R: Hox genes, neur l crest cells nd br nchi l rch p tterning. Curr Op Ce ll Biol 13:698, 2001. Webster WS, Lipson AH, Sulik KK: Interference with g strul tion during the third week of pregn ncy s c use of some f ci l bnorm lities nd CNS defects. Am J Med Genet 31:505, 1988. Wilkie AOM, Morriss-K y GM: Genet ics of cr niof ci l development nd m lform tion. N ture Rev Genet 2:458, 2001.
ch pter 16 E r In the dult, the e r forms one n tomic l unit serving both he ring nd equilib rium. In the embryo, however, it develops from three distinctly different p rts: ( ) the extern l e r, the soundcollecting org n; (b) the middle e r, sound co nductor from the extern l to the intern l e r; nd (c) the intern l e r, which c onverts sound w ves into nerve impulses nd registers ch nges in equilibrium. Intern l E r The rst indic tion of the developing e r c n be found in embryos of pproxim tely 22 d ys s thickening of the surf ce ectoderm on e ch side of th e rhombenceph lon (Fig. 16.1). These thickenings, the otic pl codes, inv gin te r pidly nd form the otic or uditory vesicles (otocysts) (Fig. 16.2). During l ter development, e ch vesicle divides into ( ) ventr l component th t gives ri se to the s ccule nd cochle r duct nd (b) dors l component th t forms the ut ricle, semicircul r c n ls, nd endolymph tic duct (Figs. 16.3 16.6). Together th ese epitheli l structures form the membr nous l byrinth. SACCULE, COCHLEA, AND O RGAN OF CORTI In the sixth week of development, the s ccule forms tubul r outp ocketing t its lower pole (Fig. 16.3, CE nd G ). This outgrowth, the cochle r d uct, penetr tes the surrounding mesenchyme in spir l 403
404 P rt Two: Speci l Embryology A B Figure 16.1 A. Sc nning electron microgr ph of mouse embryo equiv lent to ppr oxim tely 28 d ys of hum n development. The otic pl codes, s shown in B, re in v gin ting to form the otic pits ( rrows). Arrowhe d, second rch; H, he rt; st r, m ndibul r prominence. B. Region of the rhombenceph lon showing the otic pl c odes in 22-d y embryo.
f shion until t the end of the eighth week it h s completed 2.5 turns (Fig. 16. 3, D nd E ). Its connection with the rem ining portion of the s ccule is then c on ned to n rrow p thw y, the ductus reuniens (Fig. 16.3E ; see lso Fig. 16.8). Mesenchyme surrounding the cochle r duct soon differenti tes into c rtil ge (Fi g. 16.4A). In the 10th week, this c rtil ginous shell undergoes v cuoliz tion, nd two perilymph tic sp ces, the sc l vestibuli nd sc l tymp ni, re formed ( Fig. 16.4, B nd C ). The cochle r duct is then sep r ted from the sc l vestibu li by the vestibul r membr ne nd from the sc l tymp ni by the b sil r membr ne (Fig. 16.4C ). The l ter l w ll of the cochle r duct rem ins tt ched to the su rrounding c rtil ge by the spir l lig ment, where s its medi n ngle is connecte d to nd p rtly supported by long c rtil ginous process, the modiolus, the fut ure xis of the bony cochle (Fig. 16.4B). Initi lly, epitheli l cells of the co chle r duct re like (Fig. 16.4A). With further development, however, they form two ridges: the inner ridge, the future spir l limbus, nd the outer ridge (Fig . 16.4B). The outer ridge forms one row of inner nd three or four rows of outer h ir cells, the sensory cells of the uditory system (Fig. 16.5). They re cove red by the tectori l membr ne, brill r gel tinous subst nce tt ched to the spi r l limbus th t rests with its tip on the h ir cells (Fig. 16.5). The sensory ce lls nd tectori l membr ne together constitute the org n of Corti. Impulses rece ived by this org n re tr nsmitted
Ch pter 16: E r 405 A B C OV D E Figure 16.2 A to C. Tr nsverse sections through the region of the rhombenceph lo n showing form tion of the otic vesicles. A. 24 d ys. B. 27 d ys. C. 4.5 weeks. Note the st to coustic g ngli . D nd E. Sc nning electron microgr phs of mouse embryos equiv lent to st ges depicted in A nd B showing development of the otic vesicles (OV ).
to the spir l g nglion nd then to the nervous system by the uditory bers of cr ni l nerve VIII (Figs. 16.4 nd 16.5). UTRICLE AND SEMICIRCULAR CANALS During th e sixth week of development, semicircul r c n ls ppe r s ttened outpocketings of the utricul r p rt of the otic vesicle (Fig. 16.6, A nd B). Centr l portions of the w lls of these outpocketings eventu lly ppose e ch other (Fig. 16.6, C nd D) nd dis ppe r, giving rise to three semicircul r c n ls (Fig. 16.6; see lso Fig. 16.8). Where s one end of e ch c n l dil tes to form the crus mpull re , the other, the crus non mpull re, does not widen (Fig. 16.6). Since two of the l tter type fuse, however, only ve crur enter the utricle, three with n mpull nd two without. Cells in the mpull e form crest, the crist mpull ris, co nt ining sensory cells for m inten nce of equilibrium. Simil r sensory re s, th e m cul e
406 P rt Two: Speci l Embryology C E A B D F G Figure 16.3 A nd B. Development of the otocyst showing dors l utricul r porti on with the endolymph tic duct nd ventr l s ccul r portion. C to E. Cochle r duct t 6, 7, nd 8 weeks, respectively. Note form tion of the ductus reuniens nd the utriculos ccul r duct. F nd G. Sc nning electron microgr phs of mouse em bryos showing simil r st ges of development of the otocyst s depicted in A nd B. Arrowhe ds, endolymph tic duct; S, s ccule; sm ll rrow, opening of semicircu l r c n l; U , utricle. G lso shows initi l st ges of cochle r duct form tion ( l rge rrow).
custic e, develop in the w lls of the utricle nd s ccule. Impulses gener ted i n sensory cells of the crist e nd m cul e s result of ch nge in position o f the body re c rried to the br in by vestibul r bers of cr ni l nerve VIII. Dur ing form tion of the otic vesicle, sm ll group of cells bre ks w y from its w ll nd forms the st to coustic g nglion (Fig. 16.2C ). Other cells of this g ng lion re derived from the neur l crest. The g nglion subsequently
Ch pter 16: E r 407 C rtil ginous shell Sc l vestibuli B sement membr ne Cochle r duct Spir l lig ment Outer ridge A Cochle r duct (sc l medi ) Vestibul r membr ne Inner ridge
Spir l lig ment Auditory nerve fibers B sil r membr ne Spir l g nglion Sc l tym p ni C Figure 16.4 Development of the sc l tymp ni nd sc l vestibuli. A. The cochle r duct is surrounded by c rtil ginous shell. B. During the 10th week l rge v c uoles ppe r in the c rtil ginous shell. C. The cochle r duct (sc l medi ) is s ep r ted from the sc l tymp ni nd the sc l vestibuli by the b sil r nd vesti bul r membr nes, respectively. Note the uditory nerve bers nd the spir l (cochl e r) g nglion. splits into cochle r nd vestibul r portions, which supply sensory cells of the org n of Corti nd those of the s ccule, utricle, nd semicircul r c n ls, respe ctively. Middle E r TYMPANIC CAVITY AND AUDITORY TUBE The tymp nic c vity, which origin t es in the endoderm, is derived from the rst ph rynge l pouch (Figs. 16.2 nd 16.7 ). This pouch exp nds in l ter l direction nd comes in cont ct with the oor of the rst ph rynge l cleft. The dist l p rt of the pouch, the tubotymp nic recess, widens nd gives rise to the primitive tymp nic c vity, nd the proxim l p rt r em ins n rrow nd forms the uditory tube (eust chi n tube; Fig. 16.7B nd 16.8) , through which the tymp nic c vity communic tes with the n soph rynx.
B Sc l tymp ni Sc l
vestibuli Modiolus
408 P rt Two: Speci l Embryology Figure 16.5 Development of the org n of Corti. A. 10 weeks. B. Approxim tely 5 m onths. C. Full-term inf nt. Note the ppe r nce of the spir l tunnels in the org n of Corti. W lls of centr l portion of outpocketing re pposed Superior semicircul r c n l Crus commune non mpull re C A Utricle B Fl ttened outpocketing Utricle Crus mpull re Apposed w lls of outpocketing L ter l semicircul r c n l Posterior semicircul r c n l Semicircul r c n ls D E F Figure 16.6 Development of the semicircul r c n ls. A. 5 weeks. C. 6 weeks. E. 8 weeks. B, D, nd F. Apposition, fusion, nd dis ppe r nce, respectively, of the centr l portions of the w lls of the semicircul r outpocketings. Note the mpul l e in the semicircul r c n ls.
Ch pter 16: E r 409
Extern l E r EXTERNAL AUDITORY MEATUS The extern l uditory me tus develops from the dors l portion of the rst ph rynge l cleft (Fig. 16.7A). At the beginning of the third month, epitheli l cells t the bottom of the me tus prolifer te, form ing solid epitheli l pl te, the me t l plug (Fig. 16.7B ). In the seventh mont h, this plug dissolves nd the epitheli l lining of the oor of the me tus p rtici p tes in form tion of the de nitive e rdrum. Occ sion lly the me t l plug persists until birth, resulting in congenit l de fness. EARDRUM OR TYMPANIC MEMBRANE The e rdrum is m de up of ( ) ectoderm l epitheli l lining t the bottom of the ud itory me tus, (b) endoderm l epitheli l lining of the tymp nic c vity, nd (c) n intermedi te l yer of connective tissue (Fig. 16.9B) th t forms the brous str t um. The m jor p rt of the e rdrum is rmly tt ched to the h ndle of the m lleus ( Fig. 16.8 nd 16.9B), nd the rem ining portion forms the sep r tion between the extern l uditory me tus nd the tymp nic c vity.
OSSICLES The m lleus nd incus re derived from c rtil ge of the rst ph rynge l rch, nd the st pes is derived from th t of the second rch (Fig. 16.9A). Althou gh the ossicles ppe r during the rst h lf of fet l life, they rem in embedded in mesenchyme until the eighth month (Fig. 16.9B ), when the surrounding tissue di ssolves (Figs. 16.7, 16.8, nd 16.9B). The endoderm l epitheli l lining of the p rimitive tymp nic c vity then extends long the w ll of the newly developing sp ce. The tymp nic c vity is now t le st twice s l rge s before. When the ossic les re entirely free of surrounding mesenchyme, the endoderm l epithelium conne cts them in mesentery-like f shion to the w ll of the c vity (Fig. 16.9B). The supporting lig ments of the ossicles develop l ter within these mesenteries. Si nce the m lleus is derived from the rst ph rynge l rch, its muscle, the tensor t ymp ni, is innerv ted by the m ndibul r br nch of the trigemin l nerve. The st p edius muscle, which is tt ched to the st pes, is innerv ted by the f ci l nerve , the nerve to the second ph rynge l rch. During l te fet l life, the tymp nic c vity exp nds dors lly by v cuoliz tion of surrounding tissue to form the tymp nic ntrum. After birth, epithelium of the tymp nic c vity inv des bone of the d eveloping m stoid process, nd epithelium-lined ir s cs re formed (pneum tiz t ion). L ter, most of the m stoid ir s cs come in cont ct with the ntrum nd ty mp nic c vity. Exp nsion of in mm tions of the middle e r into the ntrum nd m s toid ir cells is common complic tion of middle e r infections.
410 P rt Two: Speci l Embryology Roof of rhombenceph lon Endolymph tic duct Auditory ossicles embedded in loose m esenchyme W ll of inner e r Utricul r portion of otic vesicle S ccul r portion Mesenchym l condens tion 1st ph rynge l cleft Auditory tube A Tubotymp nic recess B Extern l uditory me tus Me t l Primitive tymp nic plug c vity Figure 16.7 A. Tr nsverse section of 7-week embryo in the region of the rhombe nceph lon, showing the tubotymp nic recess, the rst ph rynge l cleft, nd mesench ym l condens tion, foresh dowing development of the ossicles. B. Middle e r show ing the c rtil ginous precursors of the uditory ossicles. Thin yellow line in m esenchyme indic tes future exp nsion of the primitive tymp nic c vity. Note the me t l plug extending from the primitive uditory me tus to the tymp nic c vity. Figure 16.8 E r showing the extern l uditory me tus, the middle e r with its os sicles, nd the inner e r. AURICLE The uricle develops from six mesenchym l prolifer tions t the dors l e nds of the rst nd second ph rynge l rches, surrounding the rst ph rynge l cleft (Fig. 16.10, A nd E ). These swellings ( uricul r hillocks), three on e ch side of the extern l me tus, l ter fuse nd form the de nitive uricle (Fig. 16.10,
Ch pter 16: E r 411 Lig ments Incus M lleus Meckels c rtil ge St pes Styloid process Stylohyoid lig m ent Hyoid bone Incus Petrous bone Perilymph tic sp ce W ll of inner e r Ov l window M lleus E rdrum Intermedi te mesoderm l yer St pes Tymp nic c vity Endoderm l epithelium A B Ectoderm l epithelium
BD nd G ). As fusion of the uricul r hillocks is complic ted, development l bn orm lities of the uricle re common. Initi lly, the extern l e rs re in the lo wer neck region (Fig. 16.10F ), but with development of the m ndible, they scen d to the side of the he d t the level of the eyes. CLINICAL CORRELATES De fness nd Extern l E r Abnorm lities Congenit l de fness, usu lly ssoci ted with de f-mutism, m y be c used by bnorm l development of the membr nous nd bo ny l byrinths or by m lform tions of the uditory ossicles nd e rdrum. In the m ost extreme c ses the tymp nic c vity nd extern l me tus re bsent. Most forms of congenit l de fness re c used by genetic f ctors, but environment l f ctors m y lso interfere with norm l development of the intern l nd middle e r. Rube ll virus, ffecting the embryo in the seventh or eighth week, m y c use severe d m ge to the org n of Corti. It h s lso been suggested th t poliomyelitis, ery throbl stosis fet lis, di betes, hypothyroidism, nd toxopl smosis c n c use con genit l de fness. Extern l e r defects re common; they include minor nd severe bnorm lities (Fig. 16.11). They re signi c nt from the st ndpoint of the psycho logic l nd emotion l tr um they m y c use nd for the f ct they re often sso ci ted with other m lform tions. Thus, they serve s clues to ex mine inf nts c refully for other bnorm lities. All of the frequently occurring chromosom l syn dromes nd most of the less common ones h ve e r nom lies s one of their ch r cteristics.
Figure 16.9 A. Deriv tives of the rst three ph rynge l rches. Note the m lleus nd incus t the dors l tip of the rst rch nd the st pes t th t of the second rch. B. Middle e r showing the h ndle of the m lleus in cont ct with the e rdrum . The st pes will est blish cont ct with the membr ne in the ov l window. The w ll of the tymp nic c vity is lined with endoderm l epithelium.
3 3 4 2 5 1 6 4 5 6 Auricul r hillocks 2 1 B 3 2 1 5 6 2 1 6 4 3 4
Antihelix Tr gus A D Antitr gus gus
E F G Figure 16.10 A. L ter l view of the he d of n embryo showing the six uricul r hillocks surrounding the dors l end of the rst ph rynge l cleft. B to D. Fusion nd progressive development of the hillocks into the dult uricle. E. The six u ricul r hillocks from the rst nd second ph rynge l rches. H, he rt; NP, n s l p l code. F. The hillocks becoming more de ned. Note the position of the e rs with r espect to the mouth nd eyes (e). G. Extern l e r ne rly complete. Growth of the m ndible nd neck region pl ces the e rs in their perm nent position.
C Cymb conch e Helix Conch 5
Ch pter 16: E r 413 A B C D Figure 16.11 A. Microti with pre uricul r pit ( rrow). B. Pre uricul r pits ( r rows). C nd D. Pre uricul r ppend ges (skin t gs). Note the low position of th e t g in D. Pre uricul r ppend ges nd pits (Fig. 16.11) re skin t gs nd sh llow depressi ons, respectively, nterior to the e r. Pits m y indic te bnorm l development o f the uricul r hillocks, where s ppend ges m y be due to ccessory hillocks. L ike other extern l e r defects, both re ssoci ted with other m lform tions. Summ ry The e r consists of three p rts th t h ve different origins, but th t fu nction s one unit. The intern l e r origin tes from the otic vesicle, which in the fourth week of development det ches from surf ce ectoderm. This vesicle divi des into ventr l component, which gives rise to the s ccule nd cochle r duct, nd dors l component, which gives rise to the utricle, semicircul r c n ls, nd endolymph tic duct (Figs. 16.3, 16.6, nd 16.8). The epitheli l structures th us formed re known collectively s the membr nous l byrinth. Except for the coc hle r duct, which forms the org n of Corti, ll structures derived from the memb r nous l byrinth re involved with equilibrium. The middle e r, consisting of th e tymp nic c vity nd uditory tube, is lined with epithelium of endoderm l orig in nd is derived from the rst
414 P rt Two: Speci l Embryology ph rynge l pouch. The uditory tube extends between the tymp nic c vity nd n so ph rynx. The ossicles, which tr nsfer sound from the tymp nic membr ne to the ov l window, re derived from the rst (m lleus nd incus) nd second (st pes) ph ry nge l rches (Fig. 16.9). The extern l uditory me tus develops from the rst ph r ynge l cleft nd is sep r ted from the tymp nic c vity by the tymp nic membr ne (e rdrum). The e rdrum consists of ( ) n ectoderm l epitheli l lining, (b) n i ntermedi te l yer of mesenchyme, nd (c) n endoderm l lining from the rst ph ryn ge l pouch. The uricle develops from six mesenchym l hillocks (Fig. 16.10) lon g the rst nd second ph rynge l rches. Defects in the uricle re often ssoci t ed with other congenit l m lform tions. Problem to Solve 1. A newborn h s bil ter l microti . Should you be concerned b out other m lform tions? Wh t cell popul tion might be involved in the embryolog ic l origin of the defect? SUGGESTED READING Ars B: Org nogenesis of the middle e r structures. J. L ryngol Otol 103:16, 1989. Fritzsch B, Beisel KW: Evolution of the nervous system: evol ution nd development of the vertebr te e r. Br in Res Bull 55:711, 2001. McPhee JR, V n De W ter TR: Epitheli l mesenchym l tissue inter ctions guiding otic c psule form tion: the role of the otocyst. J Embryol Exp Morphol 97:1, 1986. Mich els L: Evolution of the epidermoid form tion nd its role in the development of the middle e r nd tymp nic membr ne during the rst trimester. J Otol ryngol 17: 22, 1988. Mich els L, Soucek S: Auditory epitheli l migr tion on the hum n tymp nic membr ne: 2. The existence of two discrete migr tory p thw ys nd their embr yologic l correl tes. Am J An t 189:189, 1990. OR hilly R: The e rly development of the otic vesicle in st ged hum n embryos. J Embryol Exp Morphol 11:741, 1963.
ch pter 17 Eye Optic Cup nd Lens Vesicle The developing eye ppe rs in the 22-d y embryo s p ir of sh llow grooves on the sides of the forebr in (Fig. 17.1). With closure of the neur l tube, these grooves form outpocketings of the forebr in, the optic vesicles. These vesicles subsequently come in cont ct with the surf ce ectoderm nd induce ch nges in the ectoderm necess ry for lens form tion (Fig. 17.1). Sh ortly there fter the optic vesicle begins to inv gin te nd forms the double-w l led optic cup (Figs. 17.1 nd 17.2A). The inner nd outer l yers of this cup re initi lly sep r ted by lumen, the intr retin l sp ce (Fig. 17.2B; see lso Fi g. 17.4A), but soon this lumen dis ppe rs, nd the two l yers ppose e ch other (see Fig. 17.4). Inv gin tion is not restricted to the centr l portion of the cu p but lso involves p rt of the inferior surf ce (Fig. 17.2A) th t forms the c horoid ssure. Form tion of this ssure llows the hy loid rtery to re ch the inner ch mber of the eye (Figs. 17.3 nd 17.4; see lso Fig. 17.8). During the sevent h week, the lips of the choroid ssure fuse, nd the mouth of the optic cup become s round opening, the future pupil. During these events, cells of the surf ce e ctoderm, initi lly in cont ct with the optic vesicle, begin to elong te nd form the lens pl code (Fig. 17.1). This pl code subsequently inv gin tes nd develop s into the lens vesicle. During the fth week, the lens vesicle loses cont ct with the surf ce ectoderm nd lies in the mouth of the optic cup (Figs. 17.2C , 17.3 , nd 17.4). 415
416 P rt Two: Speci l Embryology A B C M M H H D E Figure 17.1 A. Tr nsverse section through the forebr in of 22-d y embryo ( ppr oxim tely 14 somites), showing the optic grooves. B. Tr nsverse section through the forebr in of 4-week embryo showing the optic vesicles in cont ct with the surf ce ectoderm. Note the slight thickening of the ectoderm (lens pl code). C. Tr nsverse section through the forebr in of 5-mm embryo showing inv gin tion o f the optic vesicle nd the lens pl code. D. Sc nning electron microgr ph showin g front l view of mouse embryo t st ge simil r to th t shown in B. E. Sc nning electron microgr ph of mouse embryo during form tion of the optic vesicl e. The embryo h s been cut s gitt lly to reve l the inside of the br in vesicles nd outpocketing of the optic vesicle ( rrow) from the forebr in. H, hindbr in; nd M, midbr in.
Retin , Iris, nd Cili ry Body The outer l yer of the optic cup, which is ch r c terized by sm ll pigment gr nules, is known s the pigmented l yer of the retin (Figs. 17.3, 17.4, nd 17.7). Development of the inner (neur l) l yer of the op tic cup is more complic ted. The posterior four- fths, the p rs optic retin e, co nt ins cells bordering the intr retin l sp ce (Fig. 17.3) th t differenti te int o light-receptive elements, rods nd cones (Fig. 17.5). Adj cent to this photore ceptive l yer is the m ntle l yer, which, s in the br in, gives rise to neurons nd supporting cells, including the
Ch pter 17: Eye 417 Figure 17.2 A. Ventrol ter l view of the optic cup nd optic st lk of 6-week e mbryo. The choroid ssure on the undersurf ce of the optic st lk gr du lly t pers off. B. Tr nsverse section through the optic st lk s indic ted in A, showing th e hy loid rtery in the choroid ssure. C. Section through the lens vesicle, the o ptic cup, nd optic st lk t the pl ne of the choroid ssure. Figure 17.3 Section through the eye of 7-week embryo. The eye primordium is co mpletely embedded in mesenchyme. Fibers of the neur l retin converge tow rd the optic nerve.
418 P rt Two: Speci l Embryology Figure 17.4 Sc nning electron microgr phs of sections through the eyes of mouse embryos t st ges equiv lent to (A) 6 weeks nd (B) 7 weeks in the hum n. A. The forming lens vesicle, not entirely closed; the two l yers of the optic cup; nd the lumen (L) of the optic st lk. (Comp re with Fig. 17.2C.) B. Lens bers (Lf ) nd neur l (N) nd pigment l yers ( rrow) forming. (Comp re with Fig. 17.3.) outer nucle r l yer, inner nucle r l yer, nd g nglion cell l yer (Fig. 17.5). O n the surf ce is brous l yer th t cont ins xons of nerve cells of the deeper l yers. Nerve bers in this zone converge tow rd the optic st lk, which develops in to the optic nerve (Figs. 17.3 nd 17.5). Hence, light impulses p ss through mos t l yers of the retin before they re ch the rods nd cones. The nterior fth of the inner l yer, the p rs cec retin e, rem ins one cell l yer thick. It l ter d ivides into the p rs iridic retin e, which forms the inner l yer of the iris, nd the p rs cili ris retin e, which p rticip tes in form tion of the cili ry bod y (Fig. 17.6 nd 17.7). Me nwhile, the region between the optic cup nd the over lying surf ce epithelium is lled with loose mesenchyme (Figs. 17.3, 17.4, nd 17. 7). The sphincter nd dil tor pupill e muscles form in this tissue (Fig. 17.6). These muscles develop from the underlying ectoderm of the optic cup. In the dul t, the iris is formed by the pigment-cont ining extern l l yer, the unpigmented intern l l yer of the optic cup, nd l yer of richly v scul rized connective t issue th t cont ins the pupill ry muscles (Fig. 17.6). The p rs cili ris retin e is e sily recognized by its m rked folding (Figs. 17.6B nd 17.7). Extern lly i t is covered by l yer of mesenchyme th t forms the cili ry muscle; on the insi de it is connected to the lens by network of el stic bers, the suspensory lig m ent or zonul (Fig. 17.7). Contr ction of the cili ry muscle ch nges tension in the lig ment nd controls curv ture of the lens.
Ch pter 17: Eye 419
Choroid, Scler , nd Corne At the end of the fth week, the eye primordium is com pletely surrounded by loose mesenchyme (Fig. 17.3). This tissue soon differenti tes into n inner l yer
Lens Shortly fter form tion of the lens vesicle (Fig. 17.2C ), cells of the terior w ll begin to elong te nteriorly nd form long bers th t gr du lly lumen of the vesicle (Figs. 17.3 nd 17.4B). By the end of the seventh week, se prim ry lens bers re ch the nterior w ll of the lens vesicle. Growth of ens is not nished t this st ge, however, since new (second ry) lens bers inuously dded to the centr l core.
Figure 17.5 V rious l yers of the p rs optic retin e in y 25 weeks.
fetus of pproxim tel pos ll the the the l re cont
420 P rt Two: Speci l Embryology Pigment l yer of retin Sinus venosus scler e
Cili ry process Cili ry muscles Sphincter pupill e Anterior lens epithelium Dil tor pupill e Sphincter pupill e Outer pigmented l yer of iris Cili ry proces s A B Inner unpigmented l yer of iris Figure 17.6 Development of the iris nd cili ry body. The rim of the optic cup i s covered by mesenchyme, in which the sphincter nd dil tor pupill e develop fro m the underlying ectoderm. Figure 17.7 Section through the eye of 15-week fetus showing the nterior ch m ber, iridopupill ry membr ne, inner nd outer v scul r l yers, choroid, nd scle r .
Neur l l yer of retin
Ch pter 17: Eye 421 comp r ble with the pi m ter of the br in nd n outer l yer comp r ble with th e dur m ter. The inner l yer l ter forms highly v scul rized pigmented l yer known s the choroid; the outer l yer develops into the scler nd is continuous with the dur m ter round the optic nerve (Fig. 17.7). Differenti tion of mese nchym l l yers overlying the nterior spect of the eye is different. The nteri or ch mber forms through v cuoliz tion nd splits the mesenchyme into n inner l yer in front of the lens nd iris, the iridopupill ry membr ne, nd n outer l yer continuous with the scler , the subst nti propri of the corne (Fig. 17.7) . The nterior ch mber itself is lined by ttened mesenchym l cells. Hence, the c orne is formed by ( ) n epitheli l l yer derived from the surf ce ectoderm, (b ) the subst nti propri or strom , which is continuous with the scler , nd (c) n epitheli l l yer, which borders the nterior ch mber. The iridopupill ry mem br ne in front of the lens dis ppe rs completely, providing communic tion betwee n the nterior nd posterior eye ch mbers. Vitreous Body Mesenchyme not only surrounds the eye primordium from the outside but lso inv des the inside of the optic cup by w y of the choroid ssure. Here it forms the hy loid vessels, which during intr uterine life supply the lens nd f orm the v scul r l yer on the inner surf ce of the retin (Fig. 17.7). In dditi on, it forms delic te network of bers between the lens nd retin . The intersti ti l sp ces of this network l ter ll with tr nsp rent gel tinous subst nce, for ming the vitreous body (Fig. 17.7). The hy loid vessels in this region re oblit er ted nd dis ppe r during fet l life, le ving behind the hy loid c n l. Optic Nerve The optic cup is connected to the br in by the optic st lk, which h s groove, the choroid ssure, on its ventr l surf ce (Figs. 17.2 nd 17.3). In t his groove re the hy loid vessels. The nerve bers of the retin returning to the br in lie mong cells of the inner w ll of the st lk (Fig. 17.8). During the se venth week, the choroid ssure closes, nd n rrow tunnel forms inside the optic st lk (Fig. 17.8B). As result of the continuously incre sing number of nerve be rs, the inner w ll of the st lk grows, nd the inside nd outside w lls of the s t lk fuse (Fig. 17.8C ). Cells of the inner l yer provide network of neurogli th t support the optic nerve bers. The optic st lk is thus tr nsformed into the optic nerve. Its center cont ins portion of the hy loid rtery, l ter c lled t he centr l rtery of the retin . On the outside, continu tion of the choroid nd scler , the pi r chnoid nd dur l yer of the nerve, respectively, surround the optic nerve.
422 P rt Two: Speci l Embryology
A Choroid fissure B C Figure 17.8 Tr nsform tion of the optic st lk into the optic nerve. A. Sixth wee k (9 mm). B. Seventh week (15 mm). C. Ninth week. Note the centr l rtery of the retin in the optic nerve. Molecul r Regul tion of Eye Development PAX6 is the key regul tory gene for eye development. It is member of the PAX (p ired box) f mily of tr nscription f ct ors nd cont ins two DNA binding motifs th t include p ired dom in nd p ire d type homeodom in. Initi lly, this tr nscription f ctor is expressed in b nd in the nterior neur l ridge of the neur l pl te before neurul tion begins. At t his st ge, there is single eye eld th t l ter sep r tes into two optic primordi . The sign l for sep r tion of this eld is sonic hedgehog (SHH ) expressed in th e prechord l pl te (see Fig. 19.32). SHH expression up-regul tes PAX2 in the cen ter of the eye eld nd downregul tes PAX6. L ter this p ttern is m int ined so th t PAX2 is expressed in the optic st lks nd PAX6 is expressed in the optic cup nd overlying surf ce ectoderm th t forms the lens. As development proceeds, it ppe rs th t PAX6 is not essenti l for optic cup form tion. Inste d, this proces s is regul ted by inter ctive sign ls between the optic vesicle nd surrounding mesenchyme nd the overlying surf ce ectoderm in the lens-forming region (Fig. 1 7.9). Thus, brobl st growth f ctors (FGFs) from the surf ce ectoderm promote diff erenti tion of the neur l (inner l yer) retin , while tr nsforming growth f ctor (TGF-), secreted y surrounding mesenchyne, directs formation of the pigmented ( outer) retinal layer. Downstream from these gene products the transcription fact ors MITF and CHX10 are expressed and direct differentiation of the pigmented and neural layer, respectively (Fig. 17.9). Thus, the lens ectoderm is essential fo r proper formation of the optic cup such that without a lens placode no cup inva gination occurs. Differentiation of the lens is dependent upon PAX6, although th e gene is not responsi le for inductive activity y the optic vesicle. Instead, PAX6 acts autonomously in the surface ectoderm to regulate lens development (Fig . 17.10). The process egins with PAX6 expression in the neural plate that upreg ulates the transcription factor SOX2 and also maintains PAX6 expression in the p rospective lens ectoderm. In turn, the optic vesicle secretes BMP-4, which also upregulates and maintains SOX2 expression as well as expression of LMAF, another transcription factor. Next, the expression of two homeo ox genes, SIX3 and
Optic nerve fibers Centr l rtery of retin
Outer l yer of optic st lk Lumen of optic st lk Nerve fibers Hy loid
rtery
Chapter 17: Eye 423 Figure 17.9 Drawing showing molecular regulation of epithelial-mesenchymal inter actions responsi le for patterning eye development. A. Once PAX6 esta lishes the eye eld, ro last growth factors (FGFs), secreted y surface ectoderm (SE) in the prospective lens-forming region overlying the optic vesicle, promote differenti ation of the neural retinal layer; while mem ers of the transforming growth fact or (TGF-) family, secreted y surrounding mesenchyme, promote differentiation of the pigmented retinal layer. These external signals cause regionalization of the inner and outer layers of the optic cup and upregulate downstream genes, includ ing CHX10 and MITF, that regulate continued differentiation of these structures (B and C). In addition to its role in determining the eye elds, PAX6 speci es the l ens placode (LP) region (B) and is also important for retinal development. Figure 17.10 Schematic showing the cascade of gene expression responsi le for ea rly stages of lens development.
424 Part Two: Special Em ryology PROX1, is upregulated y PAX6, while BMP-7 expression in the lens ectoderm is in creased to maintain expression of SOX2 and PAX6. Finally, the com ined expressio n of PAX6, SOX2, and LMAF initiates expression of genes responsi le for formatio n of lens crystalline proteins, while PROX1 expression regulates genes controlli ng cell proliferation. CLINICAL CORRELATES Eye A normalities Colo oma may occur if the choroid ssure fails to close. Normall y this ssure closes during the seventh week of development (Fig. 17.8). When it d oes not, a cleft persists. Although such a cleft is usually in the iris onlycolo oma iridis (Fig. 17.11 A)it may extend into the ciliary ody, the retina, the cho roid, and the optic nerve. Colo oma is a common eye a normality frequently assoc iated with other eye defects. Colo omas (clefts) of the eyelids may also occur. Mutations in the PAX2 gene have een linked with optic nerve colo omas and may p lay a role in the other types as well. Renal defects also occur with mutations i n PAX2 as part of the renal colo oma syndrome (see Chapter 14). The iridopupilla ry mem rane (Fig. 17.11B) may persist instead of eing resor ed during formation of the anterior cham er. In congenital cataracts the lens ecomes opaque during intrauterine life. Although this anomaly is usually genetically determined, man y children of mothers who have had German measles (ru ella) etween the fourth a nd seventh weeks of pregnancy have cataracts. If the mother is infected after th e seventh week of pregnancy, the lens escapes damage, ut the child may e deaf as a result of a normalities of the cochlea. The hyaloid artery may persist to f orm a cord or cyst. Normally the distal portion of this vessel degenerates, leav ing the proximal part to form the central artery of the retina. In microphthalmi a the eye is too small; the eye all may e only two-thirds of its normal volume. Usually associated with other ocular a normalities, Figure 17.11 A. Colo oma iris. B. Persistence of the iridopupillary mem rane.
Chapter 17: Eye 425 microphthalmia frequently results from intrauterine infections such as cytomegal ovirus and toxoplasmosis. Anophthalmia is a sence of the eye. In some cases hist ological analysis reveals some ocular tissue. The defect is usually accompanied y severe cranial a normalities. Congenital aphakia (a sence of the lens) and an iridia (a sence of the iris) are rare anomalies that are due to distur ances in induction and formation of tissues responsi le for formation of these structures . Mutations in PAX6 result in aniridia and may also contri ute to anophthalmia a nd microphthalmia. Cyclopia (single eye) and synophthalmia (fusion of the eyes) comprise a spectrum of defects in which the eyes are partially or completely fus ed (Fig. 17.12). The defects are due to a loss of midline tissue that may occur as early as days 19 to 21 of gestation or at later stages when facial developmen t is initiated. This loss results in underdevelopment of the fore rain and front onasal prominence. These defects are invaria ly associated with cranial defects, such as holoprosencephaly, in which the cere ral hemispheres are partially or c ompletely merged into a single telencephalic vesicle. Factors affecting the midl ine include alcohol, mutations in sonic hedgehog, (SHH) and a normalities in cho lesterol meta olism that may disrupt SHH signaling (see Chapter 19). Figure 17.12 Synophthalmia. The eyes are fused ecause loss of midline structure s prevented the eye elds from separating. Such a ies also have severe cranial de fects, including holoprosencephaly.
426 Part Two: Special Em ryology Summary The eyes egin to develop as a pair of outpocketings that will ecome th e optic vesicles on each side of the fore rain at the end of the fourth week of development. The optic vesicles contact the surface ectoderm and induce lens for mation. When the optic vesicle egins to invaginate to form the pigment and neur al layers of the retina, the lens placode invaginates to form the lens vesicle. Through a groove at the inferior aspect of the optic vesicle, the choroid ssure, the hyaloid artery (later the central artery of the retina) enters the eye (Figs . 17.2 and 17.3). Nerve ers of the eye also occupy this groove to reach the opti c areas of the rain. The cornea is formed y (a) a layer of surface ectoderm, ( ) the stroma, which is continuous with the sclera, and (c) an epithelial layer ordering the anterior cham er (Fig. 17.7). PAX6, the master gene for eye develo pment, is expressed in the single eye eld at the neural plate stage. The eye eld i s separated into two optic primordia y SHH, which up-regulates PAX2 expression in the optic stalks while down-regulating PAX6, restricting this genes expression to the optic cup and lens. Epithelial-mesenchymal interactions etween prospect ive lens ectoderm, optic vesicle, and surrounding mesenchyme then regulate lens and optic cup differentiation (Figs. 17.9 and 17.10). Pro lems to Solve 1. A new orn has unilateral aphakia (a sent lens). What is the em ryological origin of t his defect? 2. In taking a history of a young woman in her 10th week of gestatio n you ecome concerned that she may have contracted ru ella sometime during the fourth to eighth weeks of her pregnancy. What types of defects might e produced in her offspring? 3. Physical examination of a new orn reveals clefts in the lo wer portion of the iris ilaterally. What is the em ryological asis for this de fect? What other structures might e involved? SUGGESTED READING Ashery-Padau R, Gruss P: Pax6 lights up the way for eye develo pment. Curr Op Cell Biol 13:706, 2001. Li HS, et al.: A single morphogenetic eld gives rise to two retina primordia under the in uence of the prechordal plate. Dev elopment 124:603, 1997. Macdonald R, et al.: Midline signaling is required for P ax gene regulation and patterning of the eyes. Development 121:3267, 1995. ORahil ly R: The timing and sequence of events in the development of the human eye and ear during the em ryonic period proper. Anat Em ryol (Berl) 168:87, 1983. Saha M S, Spann C, Grainger RM: Em ryonic lens induction: more than meets the optic ves icle. Cell Differ Dev 28:153, 1989. Stromland K, Miller M, Cook C: Ocular terato logy. Surv Ophthalmol 35:429, 1991.
chapter 18 Integumentary System Skin The skin has a dual origin: (a) A super cial layer, the epidermis, develops f rom the surface ectoderm. ( ) A deep layer, the dermis, develops from the underl ying mesenchyme. EPIDERMIS Initially, the em ryo is covered y a single layer of ectodermal cells (Fig. 18.1A). In the eginning of the second month, this epith elium divides, and a layer of attened cells, the periderm, or epitrichium, is lai d down on the surface (Fig. 18.1B). With further proliferation of cells in the asal layer, a third, intermediate zone is formed (Fig. 18.1C ). Finally, at the end of the fourth month, the epidermis acquires its de nitive arrangement, and fou r layers can e distinguished (Fig. 18.1D): The asal layer, or germinative laye r, is responsi le for production of new cells. This layer later forms ridges and hollows, which are re ected on the surface of the skin in the ngerprint. A thick s pinous layer consists of large polyhedral cells containing ne tono rils. The granu lar layer contains small keratohyalin granules in its cells. The horny layer, fo rming the tough scalelike surface of the epidermis, is made up of closely packed dead cells containing keratin. Cells of the periderm are usually cast off durin g the second part of intrauterine life and can e found in the amniotic uid. 427
428 Part Two: Special Em ryology Figure 18.1 Formation of the skin at various stages of development. A. 5 weeks. B. 7 weeks. C. 4 months. D. Birth. During the rst 3 months of development, the epidermis is invaded y cells arising from the neural crest. These cells synthesize melanin pigment, which can e tra nsferred to other cells of the epidermis y way of dendritic processes. After i rth, these melanocytes cause pigmentation of the skin (Fig. 18.1D). CLINICAL CORRELATES Fingerprints The epidermal ridges that produce typical patterns on the surface o f the ngertips, palms of the hand, and soles of the feet are genetically determin ed. They form the asis for many studies in medical genetics and criminal invest igations (dermatoglyphics). In children with chromosomal a normalities, the epid ermal pattern on the hand and ngers is sometimes used as a diagnostic tool. DERMI S The dermis is derived from lateral plate mesoderm and the dermatomes from somi tes. During the third and fourth months, this tissue, the corium (Fig. 18.1D), f orms many irregular papillary structures, the dermal papillae, which project upw ard into the epidermis. Most of these papillae contain a small capillary or sens ory nerve end organ. The deeper layer of the dermis, the su corium, contains lar ge amounts of fatty tissue. At irth, the skin is covered y a whitish paste, th e vernix caseosa, formed y secretions from se aceous glands and degenerated epi dermal cells and hairs. It protects the skin against the macerating action of am niotic uid.
Chapter 18: Integumentary System 429 Figure 18.2 Ichthyosis in a harlequin fetus with massive thickening of the kerat in layer, which cracks to form ssures etween thickened plaques. CLINICAL CORRELATES Keratinization of the skin Ichthyosis, excessive keratinization of the skin, is characteristic of a group of hereditary disorders that are usually inherited as an autosomal recessive trait ut may also e X-linked. In severe cases, ichthyos is may result in a grotesque appearance, as in the case of a harlequin fetus (Fi g. 18.2). Hair Hairs appear as solid epidermal proliferations penetrating the underlying d ermis (Fig. 18.3A). At their terminal ends, hair uds invaginate. The invaginati ons, the hair papillae, are rapidly lled with mesoderm in which vessels and nerve endings develop (Fig. 18.3, B and C ). Soon cells in the center of the hair ud s ecome spindle-shaped and keratinized, forming the hair shaft, while
430 Part Two: Special Em ryology Figure 18.3 Development of a hair and a se aceous gland. A. 4 months. B. 6 month s. C. New orn. peripheral cells ecome cu oidal, giving rise to the epithelial hair sheath (Fig . 18.3, B and C ). The dermal root sheath is formed y the surrounding mesenchym e. A small smooth muscle, also derived from mesenchyme, is usually attached to t he dermal root sheath. The muscle is the arrector pili muscle. Continuous prolif eration of epithelial cells at the ase of the shaft pushes the hair upward, and y the end of the third month the rst hairs appear on the surface in the region of the eye row and upper lip. The rst hair that appears, lanugo hair, is shed at a out the time of irth and is later replaced y coarser hairs arising from new hair follicles. The epithelial wall of the hair follicle usually shows a small ud penetrating the surrounding mesoderm (Fig. 18.3C ). Cells from these uds for m the se aceous glands. Cells from the gland degenerate, forming a fatlike su st ance secreted into the hair follicle, and from there it reaches the skin. CLINICAL CORRELATES A normalities of Hair Distri ution Hypertrichosis (excessive hairiness) is cause d y an unusual a undance of hair follicles. It may e localized to certain area s of the ody, especially the
Chapter 18: Integumentary System 431 lower lum ar region covering a spina i da occulta defect or may cover the entire ody. Atrichia, the congenital a sence of hair, is usually associated with a nor malities of other ectodermal derivatives, such as teeth and nails.
Mammary Glands The rst indication of mammary glands is found in the form of a an dlike thickening of the epidermis, the mammary line or mammary ridge. In a 7-wee k em ryo, this line extends on each side of the ody from the ase of the foreli m to the region of the hindlim (Fig. 18.4C ). Although the major part of the m ammary line disappears shortly after it forms, a small portion in the thoracic r egion persists and penetrates the underlying mesenchyme (Fig. 18.4A). Here it fo rms 16 to 24 sprouts, which in turn give rise to small, solid uds. By the end o f prenatal life, the epithelial sprouts are canalized and form the lactiferous d ucts, and the uds form small ducts and alveoli of the gland. Initially, the lac tiferous ducts open into a small epithelial pit (Fig. 18.4B ). Shortly after ir th, this pit is transformed into the nipple y proliferation of the underlying m esenchyme. Figure 18.4 A and B. Sections through the developing mammary gland at the third and eighth months, respectively. C. Positions of accessory nipples ( lue line, m ammary line).
432 Part Two: Special Em ryology CLINICAL CORRELATES Mammary Gland A normalities Polythelia is a condition where accessory nipples ha ve formed due to the persistence of fragments of the mammary line (Fig. 18.4C ). Accessory nipples may develop anywhere along the original mammary line, ut usu ally appear in the axillary region. Polymastia occurs when a remnant of the mamm ary line develops into a complete reast. Inverted nipple is a condition in whic h the lactiferous ducts open into the original epithelial pit that has failed to evert. Summary The skin and its associated structures, hair, nails, and glands, are derived from surface ectoderm. Melanocytes, which give the skin its color, are derived from neural crest cells, which migrate into the epidermis. The produ ction of new cells occurs in the germinative layer. After moving to the surface, cells are sloughed off in the horny layer (Fig. 18.1). The dermis, the deep lay er of the skin, is derived from lateral plate mesoderm and from dermatomes of th e somites. Hairs develop from downgrowth of epidermal cells into the underlying dermis. By a out 20 weeks, the fetus is covered y downy hair, lanugo hair, whic h is shed at the time of irth. Se aceous glands, sweat glands, and mammary glan ds all develop from epidermal proliferations. Supernumerary nipples (polythelia) and reasts (polymastia) are relatively common (see Fig. 18.4). Pro lem to Solv e 1. A woman appears to have accessory nipples in her axilla and on her a domen ilaterally. What is the em ryological asis for these additional nipples, and w hy do they occur in these locations? SUGGESTED READING Beller F: Development and anatomy of the reast. In Mitchell G W Jr, Bassett LW (eds): The Female Breast and Its Disorders. Baltimore, Williams & Wilkins, 1990. Fuchs E: Epidermal differentiation: the are essential. J Cell Biol 111:2807, 1990. Hirschhorn K: Dermatoglyphics. In Behrman RE (ed): Nelson Text ook of Pediatrics. 14th ed. Philadelphia, WB Saunders, 1992. Newman M: Supe rnumerary nipples. Am Fam Physician 38:183, 1988. Nordlund JJ, A del-Malek ZA, B oissy R, Rheins LA: Pigment cell iology: an historical review. J Invest Dermato l 92:53S, 1989. Opitz JM: Pathogenetic analysis of certain developmental and gen etic ectodermal defects. Birth Defects 24:75, 1988. Smith LT, Hol rook KA: Em ry ogenesis of the dermis in human skin. Pediatr Dermatol 3:271, 1986.
chapter 19 Central Nervous System The central nervous system (CNS) appears at the eginning of the third week as a slipper-shaped plate of thickened ectoderm, the neural plate, in the middorsal region in front of the primitive node. Its lateral edges soon elevate to form th e neural folds (Fig. 19.1). With further development, the neural folds continue to elevate, approach each other in the midline, and nally fuse, forming the neura l tu e (Figs. 19.2 and 19.3). Fusion egins in the cervical region and proceeds in cephalic and caudal directions (Fig. 19.3A). Once fusion is initiated, the op en ends of the neural tu e form the cranial and caudal neuropores that communica te with the overlying amniotic cavity (Fig. 19.3B). Closure of the cranial neuro pore proceeds cranially from the initial closure site in the cervical region (19 .3A) and from a site in the fore rain that forms later. This later site proceeds cranially, to close the rostralmost region of the neural tu e, and caudally to meet advancing closure from the cervical site (19.3B). Final closure of the cran ial neuropore occurs at the 18- to 20-somite stage (25th day); closure of the ca udal neuropore occurs approximately 2 days later. The cephalic end of the neural tu e shows three dilations, the primary rain vesicles: (a) the prosencephalon, or fore rain; ( ) the mesencephalon, or mid rain; and (c) the rhom encephalon, or hind rain (Fig. 19.4). Simultaneously it forms two exures: (a) the cervical exu re 433
434 Part Two: Special Em ryology C Figure 19.1 A. Dorsal view of a late presomite em ryo at approximately 18 days. The amnion has een removed, and the neural plate is clearly visi le. B. Dorsal view at approximately 20 days. Note the somites and the neural groove and neural folds. C. Scanning electron micrograph of a mouse em ryo at a stage similar to that in B. F, fore rain; M, mid rain; H, hind rain. at the junction of the hind rain and the spinal cord and ( ) the cephalic exure i n the mid rain region (Fig. 19.4). When the em ryo is 5 weeks old, the prosencep halon consists of two parts: (a) the telencephalon, formed y a midportion and t wo lateral outpocketings, the primitive cere ral hemispheres, and ( ) the dience phalon, characterized y outgrowth of the optic vesicles (Fig. 19.5). A deep fur row, the rhom encephalic isthmus, separates the mesencephalon from the rhom ence phalon. The rhom encephalon also consists of two parts: (a) the metencephalon, w hich later forms the pons and cere ellum, and ( ) the myelencephalon. The ounda ry etween these two portions is marked y the pontine exure (Fig.19.5). The lume n of the spinal cord, the central canal, is continuous with that of the rain ve sicles. The cavity of the rhom encephalon is the fourth ventricle, that of the d iencephalon is the third ventricle, and those of the cere ral hemispheres are th e lateral ventricles (Fig. 19.5). The lumen of the mesencephalon connects the th ird and fourth ventricles. This lumen ecomes very narrow and is then known as t he aqueduct of Sylvius. The lateral ventricles communicate with the third ventri cle through the interventricular foramina of Monro (Fig. 19.5).
Chapter 19: Central Nervous System 435 Neural crest Dorsal root ganglion Sympathetic ganglion A Developing suprarenal gland Preaortic ganglion Enteric ganglia B C Urogenital ridge D Figure 19.2 AC. Transverse sections through successively older em ryos showing fo rmation of the neural groove, neural tu e, and neural crest. Cells of the neural crest, migrate from the edges of the neural folds and develop into spinal and c ranial sensory ganglia (AC). D. Scanning electron micrograph of a mouse em ryo sh owing the neural tu e (NT ) and neural crest cells (arrows) migrating from the d orsal region (compare with B and C).
436 Part Two: Special Em ryology Cranial neuropore Neural fold Pericardial Somite Cut edge of amnion Caudal neuropore A B C Figure 19.3 A. Dorsal view of a human em ryo at approximately day 22. Seven dist inct somites are visi le on each side of the neural tu e. B. Dorsal view of a hu man em ryo at approximately day 23. The nervous system is in connection with the amniotic cavity through the cranial and caudal neuropores. C. Scanning electron micrograph of a mouse em ryo at a stage similar to that in A. S, somites. Spinal Cord NEUROEPITHELIAL, MANTLE, AND MARGINAL LAYERS The wall of a recently closed neural tu e consists of neuroepithelial cells. These cells extend over th e entire thickness of the wall and form a thick pseudostrati ed epithelium (Fig. 1 9.6). Junctional complexes at the lumen connect them. During the neural groove s tage and immediately after closure of the tu e, they divide rapidly, producing m ore and more neuroepithelial cells. Collectively they constitute the neuroepithe lial layer or neuroepithelium. Once the neural tu e closes, neuroepithelial cell s egin to give rise to another cell type characterized y a large round nucleus with pale nucleoplasm and a dark-staining nucleolus. These are the primitive ne rve cells, or neuro lasts (Fig. 19.7). They form the mantle layer, a zone around the neuroepithelial layer (Fig. 19.8). The mantle layer later forms the gray ma tter of the spinal cord. The outermost layer of the spinal cord, the marginal la yer, contains nerve ers emerging from neuro lasts in the mantle layer. As a resu lt of myelination of nerve ers, this layer takes on a white appearance and there fore is called the white matter of the spinal cord (Fig. 19.8).
ulge Otic placode
Chapter 19: Central Nervous System 437 Figure 19.4 Scanning electron micrograph of a sagittal section through a mouse e m ryo at approximately 27 days of human development. Three rain vesicles repres ent the fore rain (F ), mid rain (M ), and hind rain (H ). Figure 19.5 Scanning electron micrograph of a sagittal section through a mouse e m ryo at approximately 32 days of human development. The three rain vesicles ha ve segregated into the telencephalon (T ), diencephalon (D), mesencephalon (M), metencephalon (Mt), and myelencephalon (My). Asterisk, outpocketing of the telen cephalon; arrow, rhom encephalic isthmus; arrowheads, roof of the fourth ventric le; o, optic stalk.
438 Part Two: Special Em ryology External limiting mem rane ( asement mem rane) Intermitotic neuroepithelial cells Dividing neuroepithelial cell A Junctional complexes at lumen B Figure 19.6 A. Section of the wall of the recently closed neural tu e showing ne uroepithelial cells, which form a pseudostrati ed epithelium extending over the fu ll width of the wall. Note the dividing cells at the lumen of the tu e. B. Scann ing electron micrograph of a section of the neural tu e of a mouse em ryo simila r to that in A.
Chapter 19: Central Nervous System 439 Pia cell External limiting mem rane Differentiating neuro last Intermitotic neuroepithelial cells Dividing neuroepithelial cell Lumen Junctional complexes Figure 19.7 Section of the neural tu e at a slightly more advanced stage than in Figure 19.6. The major portion of the wall consists of neuroepithelial cells. O n the periphery, immediately adjacent to the external limiting mem rane, neuro l asts form. These cells, which are produced y the neuroepithelial cells in everincreasing num ers, will form the mantle layer. BASAL, ALAR, ROOF, AND FLOOR PLATES As a result of continuous addition of neuro lasts to the mantle layer, each side of the neural tu e shows a ventral and a do rsal thickening. The ventral thickenings, the asal plates, which contain ventra l motor horn cells, form the motor areas of the spinal cord; the dorsal thickeni ngs, the alar plates, form the sensory areas (Fig. 19.8A). A longitudinal groove , the sulcus limitans, marks the oundary etween the two. The dorsal and ventra l midline portions of the neural tu e, known as the roof and oor plates, respecti vely, do not contain neuro lasts; they serve primarily as pathways for nerve ers crossing from one side to the other.
440 Part Two: Special Em ryology Roof plate Alar plate Sulcus limitans Mantle layer Marginal layer Central canal Dorsal median septum Dorsal sensory horn Basal plate A Floor plate Intermediate horn Neuroepithelial layer White matter B Ventral fissure Ventral motor horn C Figure 19.8 A and B. Two successive stages in the development of the spinal cord . Note formation of ventral motor and dorsal sensory horns and the intermediate column. C. Scanning electron micrograph of a section through the spinal cord of a mouse em ryo showing a stage similar to that in A. SG, spinal ganglion. In addition to the ventral motor horn and the dorsal sensory horn, a group of ne urons accumulates etween the two areas and forms a small intermediate horn (Fig . 19.8B). This horn, containing neurons of the sympathetic portion of the autono mic nervous system, is present only at thoracic (T1T12) and upper lum ar levels ( L2 or L3) of the spinal cord. HISTOLOGICAL DIFFERENTIATION Nerve Cells Neuro las ts, or primitive nerve cells, arise exclusively y division of the neuroepitheli al cells. Initially they have a central process extending to the lumen (transien t dendrite), ut when they migrate into the mantle layer, this
Chapter 19: Central Nervous System 441 process disappears, and neuro lasts are temporarily round and apolar (Fig. 19.9 A). With further differentiation, two new cytoplasmic processes appear on opposi te sides of the cell ody, forming a ipolar neuro last (Fig. 19.9 B). The proce ss at one end of the cell elongates rapidly to form the primitive axon, and the process at the other end shows a num er of cytoplasmic ar orizations, the primit ive dendrites (Fig. 19.9C ). The cell is then known as a multipolar neuro last a nd with further development ecomes the adult nerve cell or neuron. Once neuro l asts form, they lose their a ility to divide. Axons of neurons in the asal plat e reak through the marginal zone and ecome visi le on the ventral aspect of th e cord. Known collectively as the ventral motor root of the spinal nerve, they c onduct motor impulses from the spinal cord to the muscles (Fig. 19.10). Axons of neurons in the dorsal sensory Figure 19.9 Various stages of development of a neuro last. A neuron is a structu ral and functional unit consisting of the cell ody and all its processes. Figure 19.10 A. Motor axons growing out from neurons in the asal plate and cent rally and peripherally growing ers of nerve cells in the dorsal root ganglion. B . Nerve ers of the ventral motor and dorsal sensory roots join to form the trunk of the spinal nerve.
442 Part Two: Special Em ryology horn (alar plate) ehave differently from those in the ventral horn. They penetr ate into the marginal layer of the cord, where they ascend to either higher or l ower levels to form association neurons. Glial Cells The majority of primitive s upporting cells, the glia lasts, are formed y neuroepithelial cells after produ ction of neuro lasts ceases. Glia lasts migrate from the neuroepithelial layer t o the mantle and marginal layers. In the mantle layer, they differentiate into p rotoplasmic astrocytes and rillar astrocytes (Fig. 19.11). Another type of suppo rting cell possi ly derived from glia lasts is the oligodendroglial cell. This c ell, which is found primarily in the marginal layer, forms myelin sheaths around the ascending and descending axons in the marginal layer. In the second half of development, a third type of supporting cell, the microglial cell, appears in t he CNS. This highly phagocytic cell type is derived from mesenchyme (Fig. 19.11) . When neuroepithelial cells cease to produce neuro lasts and glia lasts, they d ifferentiate into ependymal cells lining the central canal of the spinal cord. N eural Crest Cells During elevation of the neural plate, a group of cells appears along each edge (the crest) of the neural folds (Fig. 19.2). These neural crest cells are ectodermal Figure 19.11 Origin of the nerve cell and the various types of glial cells. Neur o lasts, rillar and protoplasmic astrocytes, and ependymal cells originate from neuroepithelial cells. Microglia develop from mesenchyme cells. The origin of th e oligodendroglia is not clear.
Chapter 19: Central Nervous System 443 in origin and extend throughout the length of the neural tu e. Crest cells migra te laterally and give rise to sensory ganglia (dorsal root ganglia) of the spina l nerves and other cell types (Fig. 19.2). During further development, neuro las ts of the sensory ganglia form two processes (Fig. 19.10A). The centrally growin g processes penetrate the dorsal portion of the neural tu e. In the spinal cord, they either end in the dorsal horn or ascend through the marginal layer to one of the higher rain centers. These processes are known collectively as the dorsa l sensory root of the spinal nerve (Fig. 19.10B). The peripherally growing proce sses join ers of the ventral motor roots and thus participate in formation of th e trunk of the spinal nerve. Eventually these processes terminate in the sensory receptor organs. Hence, neuro lasts of the sensory ganglia derived from neural crest cells give rise to the dorsal root neurons. In addition to forming sensory ganglia, cells of the neural crest differentiate into sympathetic neuro lasts, Schwann cells, pigment cells, odonto lasts, meninges, and mesenchyme of the phar yngeal arches (see Chapter 5). Spinal Nerves Motor nerve ers egin to appear in the fourth week, arising from nerve cells in the asal plates (ventral horns) of the spinal cord. These ers collect into undles known as ventral nerve roots (F ig. 19.10). Dorsal nerve roots form as collections of ers originating from cells in dorsal root ganglia (spinal ganglia). Central processes from these ganglia f orm undles that grow into the spinal cord opposite the dorsal horns. Distal pro cesses join the ventral nerve roots to form a spinal nerve (Fig. 19.10). Almost immediately, spinal nerves divide into dorsal and ventral primary rami. Dorsal p rimary rami innervate dorsal axial musculature, verte ral joints, and the skin o f the ack. Ventral primary rami innervate the lim s and ventral ody wall and f orm the major nerve plexuses ( rachial and lum osacral). Myelination Schwann cel ls myelinate the peripheral nerves. These cells originate from neural crest, mig rate peripherally, and wrap themselves around axons, forming the neurilemma shea th (Fig. 19.12). Beginning at the fourth month of fetal life, many nerve ers tak e on a whitish appearance as a result of deposition of myelin, which is formed y repeated coiling of the Schwann cell mem rane around the axon (Fig. 19.12C ). The myelin sheath surrounding nerve ers in the spinal cord has a completely diff erent origin, the oligodendroglial cells (Fig. 19.12, B and C ). Although myelin ation of nerve ers in the spinal cord egins in approximately the fourth month o f intrauterine life, some of the motor ers descending from higher rain centers to the spinal cord do not ecome myelinated until the rst year of postnatal life. Tracts in the nervous system ecome myelinated at a out the time they start to function.
444 Part Two: Special Em ryology Figure 19.12 A. Motor horn cell with naked rootlet. B. In the spinal cord oligod endroglia cells surround the ventral rootlet; outside the spinal cord, Schwann c ells egin to surround the rootlet. C. In the spinal cord the myelin sheath is f ormed y oligodendroglia cells; outside the spinal cord the sheath is formed y Schwann cells. POSITIONAL CHANGES OF THE CORD In the third month of development the spinal cord extends the entire length of the em ryo, and spinal nerves pass through the int erverte ral foramina at their level of origin (Fig. 19.13A). With increasing age , however, the verte ral column and dura lengthen more rapidly than the neural t u e, and the terminal end of the spinal cord gradually shifts to a higher level. At irth, this end is at the level of the third lum ar verte ra (Fig. 19.13C ). As a result of this disproportionate growth, spinal nerves run o liquely from t heir segment of origin in the spinal cord to the corresponding level of the vert e ral column. The dura remains attached to the verte ral column at the coccygeal level. In the adult, the spinal cord terminates at the level of L2 to L3, where as the dural sac and su arachnoid space extend to S2. Below L2 to L3, a threadli ke extension of the pia mater forms the lum terminale, which is attached to the p eriosteum of the rst coccygeal verte ra and which marks the tract of regression o f the spinal cord. Nerve ers elow the terminal end of the cord collectively con stitute the cauda equina. When cere rospinal uid is tapped during a lum ar punctu re, the needle is inserted at the lower lum ar level, avoiding the lower end of the cord. Molecular Regulation of Spinal Cord Development At the neural plate st age in the spinal cord region, the entire plate expresses the transcription fact ors PAX3, PAX7, MSX1, and MSX2, all of which contain a homeodomain. This express ion pattern is altered y sonic hedgehog (SHH ) expressed in the notochord and one morphogenetic proteins 4 and 7 (BMP4 and BMP7) expressed in the nonneural ec toderm at the order of the neural plate (Fig. 19.14 A ). The SHH signal repress es expression of PAX3 and PAX7 and MSX1 and MSX2. Thus, SHH ventralizes the neur al tu e. This ventral region then acquires the capacity to form a oor plate, whic h also expresses SHH, and motor neurons in the asal plate. BMP4 and BMP7 expres sion maintains
Chapter 19: Central Nervous System 445 L2 Spinal cord L1 Dura T11 S1 L1 Dorsal root ganglion of 1st sacral nerve C1 S1 Attachment of dura Lengthened root of 1st sacral nerve L3 A B Filum terminale internum S1 Dura C Figure 19.13 Terminal end of the spinal cord in relation to that of the verte ra l column at various stages of development. A. Approximately the third month. B. End of the fth month. C. New orn. and up-regulates PAX3 and PAX7 in the dorsal half of the neural tu e, where sens ory neurons in the alar plate will form (Fig. 19.14B). These two genes are requi red for formation of neural crest cells in the top of the neural folds, ut thei r roles and those of the MSX genes in differentiation of sensory neurons and int erneurons is not clear. However, their expression throughout the neural plate at earlier stages is essential for formation of ventral cell types, despite the fa ct that their expression is excluded from ventral regions y SHH at later stages . Thus, they confer on ventral cell types competence to respond appropriately to SHH and other ventralizing signals. Yet another PAX gene, PAX6, is expressed th roughout the elevating neural folds except in the midline, and this pattern is m aintained after fold closure. However, the role of this gene has not een determ ined (Fig. 19.14 B ). CLINICAL CORRELATES Neural Tu e Defects Most defects of the spinal cord result from a normal closure of the neural folds in the third and fourth weeks of development. The resulting a normalities,
446 Part Two: Special Em ryology BMPs BMPs BMPs S SHH F N S S A PAX3,7 PAX3, 7 S F N F N S PAX3,7 S PAX6 S B F N S PAX6 Figure 19.14 Molecular regulation of spinal cord development. A. Sonic hedgehog (SHH), secreted y the notochord, ventralizes the neural tu e and induces a oor p late region (F ) that also expresses this gene. Bone morphogenetic proteins 4 an d 7 are secreted y the nonneural ectoderm and contri ute to differentiation of the roof and alar plates. B. Initially, PAX3 and 7 and MSX 1 and 2 are expressed uniformly throughout the neural plate. SHH represses expression of these genes in the ventral half of the neural tu e that will ecome the oor and asal plates. Simultaneously, BMPs upregulate and maintain expression of PAX 3 and 7 in the d orsal half of the neural tu e that will form the roof and alar plates. PAX 6 eg ins expression throughout the neural ectoderm as the neural folds elevate and cl ose. The exact roles of the PAX and MSX genes in differentiation of these region s have not een determined. neural tu e defects (NTDs), may involve the meninges, verte rae, muscles, and sk in. Severe NTDs involving neural and non-neural structures occur in approximatel y 1 in 1000 irths, ut the incidence varies among different populations and may e as high as 1 in 100 irths in some areas, such as Northern China. Spina i da is a general term for NTDs affecting the spinal region. It consists of a splitti ng of the verte ral arches and may or may not involve underlying neural tissue. Two different types of spina i da occur: 1) Spina i da occulta is a defect in the verte ral arches that is covered y skin and usually does not involve underlying neural tissue (Fig. 19.15A). It occurs in the lum osacral region (L4 to S1) and is usually marked y a patch of hair overlying the affected region. The defect, which is due to a lack of fusion of the verte ral arches, affects a out 10% of otherwise normal people. 2) Spina i da cystica is a severe NTD in which neural ti ssue and/or meninges protrude through a defect in the verte ral arches and skin to form a cystlike sac (Fig. 19.15). Most lie in the lum osacral region and resu lt in neurological de cits, ut they are usually not associated with mental retard ation. In some cases only uid- lled meninges protrude through the defect (spina i da
with meningocele) (Fig. 19.15B ); in others neural tissue is included
Chapter 19: Central Nervous System 447 Hairs Skin Dura Arachnoid Arachnoid Spinal cord Su arachnoid space A Transverse Dura process B Meningocele C Meningomyelocele Folded neural tissue Spina ifida occulta Neural tissue D Rachischisis E Rachischisis Figure 19.15 Various types of spina i da. in the sac (spina i da with meningomyelocele) (Figs. 19.15C and 19.16A). Occasion ally the neural folds do not elevate ut remain as a attened mass of neural tissu e (spina i da with myeloschisis or rachischisis) (Figs. 19.15, D and E , and 19.1 6B). Hydrocephaly develops in virtually every case of spina i da cystica ecause the spinal cord is tethered to the verte ral column. As the verte ral column len gthens, tethering pulls the cere ellum into the foramen magnum, cutting off the o w of cere rospinal uid. Spina i da cystica can e diagnosed prenatally y ultrasou nd and y determination of -fetoprotein (AFP) levels in m tern l serum nd mniot ic uid. The vertebr c n be visu lized by 12 weeks of gest tion, nd defects in c losure of the vertebr l rches c n be detected. A new tre tment for the defect i s to perform surgery in utero t pproxim tely 28 weeks of gest tion. The b by i s exposed by ces re n section, the defect is rep ired, nd the inf nt is pl ced b ck in the uterus. Prelimin ry results indic te th t this ppro ch reduces the incidence of hydroceph lus, improves bl dder nd bowel control, nd incre ses mo tor development to the lower limbs. Hyperthermi , v lproic cid, nd hypervit mi nosis A produce NTDs, s do l rge number of other ter togens. The origin of mo st NTDs is multif ctori l, nd the likelihood of h ving child with such defe ct incre ses signi c ntly once one ffected offspring is born. Recent evidence pro ves th t folic cid (fol te) reduces the incidence of NTDs by s much s 70% if 400 g is t ken d ily beginning 2 months prior to conception nd continuing throug hout gest tion.
448 P rt Two: Speci l Embryology A B Figure 19.16 Lumbos cr l region of p tients with neur l tube defects. A. P tient with l rge meningomyelocele. B. P tient with severe defect in which the neu r l folds f iled to elev te throughout the lower thor cic nd lumbos cr l region s, resulting in r chischisis. Br in Distinct b s l nd l r pl tes, representing motor nd sensory re s, resp ectively, re found on e ch side of the midline in the rhombenceph lon nd mesen ceph lon. In the prosenceph lon, however, the l r pl tes re ccentu ted nd th e b s l pl tes regress. RHOMBENCEPHALON: HINDBRAIN The rhombenceph lon consists of the myelenceph lon, the most c ud l of the br in vesicles, nd the metenceph lon, which extends from the pontine exure to the rhombenceph lic isthmus (Figs. 1 9.5 nd 19.17). Myelenceph lon The myelenceph lon is br in vesicle th t gives rise to the medull oblong t . It differs from the spin l cord in th t its l ter l w lls re everted (Fig. 19.18, B nd C ). Al r nd b s l pl tes sep r ted by the sulcus limit ns c n be cle rly distinguished. The b s l pl te, simil r to th t of the spin l cord, cont ins motor nuclei. These nuclei re divided into thre e groups: ( ) medi l som tic efferent
Ch pter 19: Centr l Nervous System 449
group, (b) n intermedi te speci l viscer l efferent group, nd (c) l ter l ge ner l viscer l efferent group (Fig. 19.18C ). The rst group cont ins motor neuron s, which form the ceph lic continu tion of the nterior horn cells. Since this s om tic efferent group continues rostr lly into the mesenceph lon, it is c lled t he som tic efferent motor column. In the myelenceph lon it includes neurons of t he hypogloss l nerve th t supply the tongue muscul ture. In the metenceph lon n d the mesenceph lon, the column cont ins neurons of the bducens (Fig. 19.19), t rochle r, nd oculomotor nerves (see Fig. 19.23), respectively. These nerves sup ply the eye muscul ture. The speci l viscer l efferent group extends into the me tenceph lon, forming the speci l viscer l efferent motor column. Its motor neuro ns supply stri ted muscles of the ph rynge l rches. In the myelenceph lon the c olumn is represented by neurons of the ccessory, v gus, nd glossoph rynge l ne rves. The gener l viscer l efferent group cont ins motor neurons th t supply inv olunt ry muscul ture of the respir tory tr ct, intestin l tr ct, nd he rt. The l r pl te cont ins three groups of sensory rel y nuclei (see Fig. 19.18C ). The most l ter l of these, the som tic fferent (sensory) group, receives impulses from the e r nd surf ce of the he d by w y of the vestibulocochle r nd trigemi n l nerves. The intermedi te, or speci l viscer l fferent, group receives impul ses from t ste buds of the tongue nd from the p l te, oroph rynx, nd epiglotti s. The medi l, or gener l viscer l fferent, group receives interoceptive inform tion from the g strointestin l tr ct nd he rt. The roof pl te of the myelencep h lon consists of single l yer of ependym l cells covered by v scul r mesenchy me, the pi m ter (Figs. 19.5 nd
Figure length ved to the cr
19.17 L ter l view of the br in vesicles in n 8-week embryo (crown-rump pproxim tely 27 mm). The roof pl te of the rhombenceph lon h s been remo show the intr ventricul r portion of the rhombic lip. Note the origin of ni l nerves.
450 P rt Two: Speci l Embryology 4th ventricle Mesenceph lon Metenceph lon Al r pl te Abducens nerve Roof pl te B Rhombic lip B s l pl te Choroid plexus Som tic fferent Speci l viscer l fferen t Gener l viscer l fferent Sulcus limit ns Gener l viscer l efferent B s l pl te Al r pl te Att chment of roof pl te Myelenceph lon A Oliv ry nucleus C Som tic efferent (XII) Speci l viscer l efferent (IX, X, XI) Figure 19.18 A. Dors l view of the oor of the fourth ventricle in 6-week embryo fter remov l of the roof pl te. Note the l r nd b s l pl tes in the myelence ph lon. The rhombic lip is visible in the metenceph lon. B nd C. Position nd d ifferenti tion of the b s l nd l r pl tes of the myelenceph lon t different s t ges of development. Note form tion of the nucle r groups in the b s l nd l r pl tes. Arrows, p th followed by cells of the l r pl te to the oliv ry nucle r complex. The choroid plexus produces cerebrospin l uid. Extern l gr nul r l yer 4th ventricle Roof pl te Som tic fferent Rhombic lip Speci l viscer l fferent Gener l viscer l fferent Gener l viscer l efferent Pontine nuclei Som tic efferent (VI) Speci l viscer l efferent (V nd VII) Figure 19.19 Tr nsverse section through the c ud l p rt of the metenceph lon. No te the differenti tion of the v rious motor nd sensory nucle r re s in the b s l nd l r pl tes, respectively, nd the position of the rhombic lips, which pr oject p rtly into the lumen of the fourth ventricle nd p rtly bove the tt chm ent of the roof pl te. Arrows, direction of migr tion of the pontine nuclei.
Ch pter 19: Centr l Nervous System 451 19.18B). The two combined re known s the tel choroide . Bec use of ctive pro lifer tion of the v scul r mesenchyme, number of s clike inv gin tions project into the underlying ventricul r c vity (Figs. 19.18C nd 19.20D). These tuftlik e inv gin tions form the choroid plexus, which produces cerebrospin l uid. Metenc eph lon The metenceph lon, simil r to the myelenceph lon, is ch r cterized by b s l nd l r pl tes (Fig. 19.19). Two new components form: ( ) the cerebellum, coordin tion center for posture nd movement (Fig. 19.20), nd (b) the pons, th e p thw y for nerve bers between the spin l cord nd the cerebr l nd cerebell r cortices. E ch b s l pl te of the metenceph lon (Fig. 19.19) cont ins three grou ps of motor neurons: ( ) the medi l som tic efferent group, which gives rise to Mesenceph lon Posterior colliculus Cerebell r hemisphere Anterior colliculus Cerebell r pl te { Extr ventricul r Intr ventricul r Al r pl te B s l pl te Vermis Nodule Flocculus Posterior medull ry velum Sulcus limit ns Cut edge roof of 4th ventricle Roof pl te of 4th ventricle For men of Luschk For men of M gendie (medi l perture) A B C D Figure 19.20 A. Dors l view of the mesenceph lon nd rhombenceph lon in n 8-wee k embryo. The roof of the fourth ventricle h s been removed, llowing view of its oor. B. Simil r view in 4-month embryo. Note the choroid l ssure nd the l t er l nd medi l pertures in the roof of the fourth ventricle. C. Sc nning elect ron microgr ph of mouse embryo t slightly younger st ge th n in A, showing the cerebell r primordium ( rrow) extending into the fourth ventricle (V ). M, m esenceph lon. D. High m gni c tion of the cerebell r region in C. Choroid plexus ( rrow) in the roof of the fourth ventricle (V ).
452 P rt Two: Speci l Embryology the nucleus of the bducens nerve; (b) the speci l viscer l efferent group, cont ining nuclei of the trigemin l nd f ci l nerves, which innerv te the muscul tu re of the rst nd second ph rynge l rches; nd (c) the gener l viscer l efferent group, whose xons supply the subm ndibul r nd sublingu l gl nds. The m rgin l l yer of the b s l pl tes of the metenceph lon exp nds s it m kes bridge for nerve bers connecting the cerebr l cortex nd cerebell r cortex with the spin l cord. Hence this portion of the metenceph lon is known s the pons (bridge). In ddition to nerve bers, the pons cont ins the pontine nuclei, which origin te in the l r pl tes of the metenceph lon nd myelenceph lon ( rrows, Fig. 19.19). Th e l r pl tes of the metenceph lon cont in three groups of sensory nuclei: ( ) l ter l som tic fferent group, which cont ins neurons of the trigemin l nerve nd sm ll portion of the vestibulocochle r complex, (b) the speci l viscer l fferent group, nd (c) the gener l viscer l fferent group (Fig. 19.19). Cerebel lum The dorsol ter l p rts of the l r pl tes bend medi lly nd form the rhombic lips (Fig. 19.18). In the c ud l portion of the metenceph lon, the rhombic lips re widely sep r ted, but immedi tely below the mesenceph lon they ppro ch e c h other in the midline (Fig. 19.20). As result of further deepening of the p ontine exure, the rhombic lips compress ceph loc ud lly nd form the cerebell r p l te (Fig. 19.20). In 12-week embryo, this pl te shows sm ll midline portion , the vermis, nd two l ter l portions, the hemispheres. A tr nsverse ssure soon sep r tes the nodule from the vermis nd the l ter l occulus from the hemispheres (Fig. 19.20B ). This occulonodul r lobe is phylogenetic lly the most primitive p rt of the cerebellum. Initi lly, the cerebell r pl te consists of neuroepitheli l, m ntle, nd m rgin l l yers (Fig. 19.21A). During further development, num ber of cells formed by the neuroepithelium migr te to the surf ce of the cerebel lum to form the extern l gr nul r l yer. Cells of this l yer ret in their bilit y to divide nd form prolifer tive zone on the surf ce of the cerebellum (Fig. 19.21, B nd C ). In the sixth month of development, the extern l gr nul r l ye r gives rise to v rious cell types. These cells migr te tow rd the differenti ti ng Purkinje cells (Fig. 19.22) nd give rise to gr nule cells. B sket nd stell te cells re produced by prolifer ting cells in the cerebell r white m tter. The cortex of the cerebellum, consisting of Purkinje cells, Golgi II neurons, nd n eurons produced by the extern l gr nul r l yer, re ches its de nitive size fter b irth (Fig. 19.22B ). The deep cerebell r nuclei, such s the dent te nucleus, re ch their n l position before birth (Fig. 19.21D). MESENCEPHALON: MIDBRAIN In the mesenceph lon (Fig. 19.23), e ch b s l pl te cont ins two groups of motor nucle i: ( ) medi l som tic efferent group, represented by the
Ch pter 19: Centr l Nervous System 453 Roof pl te of 4th ventricle M rgin l l yer Mesenceph lon Mesenceph lon Extern l gr nul r l yer A M ntle l yer Neuroepitheli l l yer Purkinje cells B Purkinje cells Gr y cortex of cerebellum Mesenceph lon Choroid plexus Medull (white) C Aqueduct 4th ventricle Dent te nucleus D Anterior medull ry velum Posterior medull ry velum Figure 19.21 S gitt l sections through the roof of the metenceph lon showing dev elopment of the cerebellum. A. 8 weeks ( pproxim tely 30 mm). B. 12 weeks (70 mm ). C. 13 weeks. D. 15 weeks. Note form tion of the extern l gr nul r l yer on th e surf ce of the cerebell r pl te (B nd C). During l ter st ges, cells of the e xtern l gr nul r l yer migr te inw rd to mingle with Purkinje cells nd form the de nitive cortex of the cerebellum. The dent te nucleus is one of the deep cerebe ll r nuclei. Note the nterior nd posterior velum.
Figure 19.22 St ges in development of the cerebell r cortex. A. The extern l gr nul r l yer on the surf ce of the cerebellum forms prolifer tive l yer from wh ich gr nule cells rise. They migr te inw rd from the surf ce ( rrows). B sket nd stell te cells derive from prolifer ting cells in the cerebell r white m tter . B. Postn t l cerebell r cortex showing differenti ted Purkinje cells, the mole cul r l yer on the surf ce, nd the intern l gr nul r l yer bene th the Purkinje cells.
454 P rt Two: Speci l Embryology Figure 19.23 A nd B. Position nd differenti tion of the b s l nd l r pl tes in the mesenceph lon t v rious st ges of development. Arrows in A indic te the p th followed by cells of the l r pl te to form the nucleus ruber nd subst nti nigr . Note the v rious motor nuclei in the b s l pl te. oculomotor nd trochle r nerves, which innerv te the eye muscul ture, nd (b) sm ll gener l viscer l efferent group, represented by the nucleus of EdingerWest ph l, which innerv tes the sphincter pupill ry muscle (Fig. 19.23B). The m rgin l l yer of e ch b s l pl te enl rges nd forms the crus cerebri. These crur ser ve s p thw ys for nerve bers descending from the cerebr l cortex to lower center s in the pons nd spin l cord. Initi lly the l r pl tes of the mesenceph lon p pe r s two longitudin l elev tions sep r ted by sh llow midline depression (F ig. 19.23). With further development, tr nsverse groove divides e ch elev tion into n nterior (superior) nd posterior (inferior) colliculus (Fig. 19.23B ). The posterior colliculi serve s syn ptic rel y st tions for uditory re exes; the nterior colliculi function s correl tion nd re ex centers for visu l impuls es. The colliculi re formed by w ves of neurobl sts migr ting into the overlyin g m rgin l zone. Here they re rr nged in l yers (Fig. 19.23B). PROSENCEPHALON: FOREBRAIN The prosenceph lon consists of the telenceph lon, which forms the cer ebr l hemispheres, nd the dienceph lon, which forms the optic cup nd st lk, pi tuit ry, th l mus, hypoth l mus, nd epiphysis. Dienceph lon Roof Pl te nd Epip hysis. The dienceph lon, which develops from the medi n portion of the prosencep h lon (Figs. 19.5 nd 19.17), is thought to consist of roof pl te nd two l r pl tes but to l ck oor nd b s l pl tes (interestingly, sonic hedgehog, ventr l midline m rker, is expressed in the oor of the dienceph lon, suggesting th t o or pl te does exist). The roof pl te of the dienceph lon consists of single l yer of ependym l cells covered by
Ch pter 19: Centr l Nervous System 455
Hippoc mpus Choroid plexus For men of Monro Corpus stri tum A B Hypoth l mus Figure 19.24 A. Medi l surf ce of the right h lf of the prosenceph lon in 7-we ek embryo. B. Tr nsverse section through the prosenceph lon t the level of the broken line in A. The corpus stri tum bulges out in the oor of the l ter l ventri cle nd the for men of Monro. v scul r mesenchyme. Together these l yers give rise to the choroid plexus of th e third ventricle (see Fig. 19.30). The most c ud l p rt of the roof pl te devel ops into the pine l body, or epiphysis. This body initi lly ppe rs s n epithe li l thickening in the midline, but by the seventh week it begins to ev gin te ( Figs. 19.24 nd 19.25). Eventu lly it becomes solid org n on the roof of the m esenceph lon (see Fig. 19.30) th t serves s ch nnel through which light nd d rkness ffect endocrine nd beh vior l rhythms. In the dult, c lcium is freque ntly deposited in the epiphysis nd then serves s l ndm rk on r diogr phs of the skull. Al r Pl te, Th l mus, nd Hypoth l mus. The l r pl tes form the l te r l w lls of the dienceph lon. A groove, the hypoth l mic sulcus, divides the pl te into dors l nd ventr l region, the th l mus nd hypoth l mus, respectiv ely (Figs. 19.24 nd 19.25). As result of prolifer tive ctivity, the th l mus gr du lly projects into the lumen of the dienceph lon. Frequently this exp nsio n is so gre t th t th l mic regions from the right nd left sides fuse in the mi dline, forming the m ss intermedi , or interth l mic connexus. The hypoth l mus , forming the lower portion of the l r pl te, differenti tes into number of n ucle r re s th t regul te the viscer l functions, including sleep, digestion, b ody temper ture, nd emotion l beh vior. One of these groups, the m mill ry body , forms distinct protuber nce on the ventr l surf ce of the hypoth l mus on e ch side of the midline (Figs. 19.24A nd 19.25A). Hypophysis or Pituit ry Gl nd. The hypophysis, or pituit ry gl nd, develops from two completely different p rt s: ( ) n ectoderm l outpocketing of the stomodeum immedi tely in front of the b uccoph rynge l membr ne, known
Roof pl te of Epith l mus dienceph lon L ter l ventricle Pine l Cerebr l thicken ing P llium hemisphere Th l mus For men of Monro L min termin lis Optic chi sm Hypoth l mic sulcus Choroid plexus M mill ry body Hypoth l mus Infundibulum 3rd ventricle
456 P rt Two: Speci l Embryology Occipit l lobe Cerebr l hemisphere Olf ctory bulb Epiphysis
A Optic chi sm Infundibulum Neop llium L ter l ventricle Hippoc mpus Choroid plexus Corpus stri tum P leop llium Corpus stri tum Th l mus B Hypoth l mus C Figure 19.25 A. Medi l surf ce of the right h lf of the telenceph lon nd dience ph lon in n 8-week embryo. B nd C. Tr nsverse sections through the right h lf of the telenceph lon nd dienceph lon t the level of the broken lines in A. s R thkes pouch, nd (b) downw rd extension of the dienceph lon, the infundibu lum (Fig. 19.26, A nd D). When the embryo is pproxim tely 3 weeks old, R thkes pouch ppe rs s n ev gin tion of the or l c vity nd subsequently grows dors l ly tow rd the infundibulum. By the end of the second month it loses its connecti on with the or l c vity nd is then in close cont ct with the infundibulum. Duri ng further development, cells in the nterior w ll of R thkes pouch incre se r pi dly in number nd form the nterior lobe of the hypophysis, or denohypophysis ( Fig. 19.26B). A sm ll extension of this lobe,
Th l mus M mill ry body L min
termin lis Hypoth l mus
Ch pter 19: Centr l Nervous System 457 A B C D Figure 19.26 A. S gitt l section through the ceph lic p rt of 6-week embryo sh owing R thkes pouch s dors l outpocketing of the or l c vity nd the infundibu lum s thickening in the oor of the dienceph lon. B nd C. S gitt l sections th rough the developing hypophysis in the 11th nd 16th weeks of development, respe ctively. Note form tion of the p rs tuber lis encircling the st lk of the p rs n ervos . D. Highm gni c tion sc nning electron microgr ph of the region of the deve loping hypophysis simil r to th t in A. R thkes pouch ( rrow) nd the infundibulu m ( rrowhe ds) re visible. the p rs tuber lis, grows long the st lk of the infundibulum nd eventu lly sur rounds it (Fig. 19.26C ). The posterior w ll of R thkes pouch develops into the p rs intermedi , which in hum ns seems to h ve little signi c nce. The infundibulum gives rise to the st lk nd the p rs nervos , or posterior lobe of the hypophys is (neurohypophysis) (Fig. 19.26C ). It is composed of neurogli l cells. In ddi tion, it cont ins number of nerve bers from the hypoth l mic re .
458 P rt Two: Speci l Embryology CLINICAL CORRELATES Hypophyse l Defects Occ sion lly sm ll portion of R thkes pouch persists in the roof of the ph rynx s ph rynge l hypophysis. Cr nioph ryngiom s rise from r emn nts of R thkes pouch. They m y form within the sell turcic or long the st lk of the pituit ry but usu lly lie bove the sell . They m y c use hydroceph lu s nd pituit ry dysfunction (e.g., di betes insipidus, growth f ilure). Telencep h lon The telenceph lon, the most rostr l of the br in vesicles, consists of two l ter l outpocketings, the cerebr l hemispheres, nd medi n portion, the l mi n termin les (Figs. 19.4, 19.5, 19.24, nd 19.25). The c vities of the hemisphe res, the l ter l ventricles, communic te with the lumen of the dienceph lon thro ugh the interventricul r for min of Monro (Fig. 19.24). Cerebr l Hemispheres. T he cerebr l hemispheres rise t the beginning of the fth week of development s bil ter l ev gin tions of the l ter l w ll of the prosenceph lon (Fig. 19.24). B y the middle of the second month the b s l p rt of the hemispheres (i.e., the p rt th t initi lly formed the forw rd extension of the th l mus) (Fig. 19.24A) be gins to grow nd bulges into the lumen of the l ter l ventricle nd into the oor of the for men of Monro (Figs. 19.24B nd 19.25, A nd B). In tr nsverse section s, the r pidly growing region h s stri ted ppe r nce nd is therefore known s the corpus stri tum (Fig. 19.25B ). In the region where the w ll of the hemisp here is tt ched to the roof of the dienceph lon, the w ll f ils to develop neur obl sts nd rem ins very thin (Fig. 19.24B). Here the hemisphere w ll consists o f single l yer of ependym l cells covered by v scul r mesenchyme, nd together they form the choroid plexus. The choroid plexus should h ve formed the roof of the hemisphere, but s result of the disproportion te growth of the v rious p rts of the hemisphere, it protrudes into the l ter l ventricle long the choroi d l ssure (Figs. 19.25 nd 19.27). Immedi tely bove the choroid l ssure, the w ll of the hemisphere thickens, forming the hippoc mpus (Figs. 19.24B nd 19.25B ). This structure, whose prim ry function is olf ction, bulges into the l ter l ve ntricle. With further exp nsion, the hemispheres cover the l ter l spect of the dienceph lon, mesenceph lon, nd ceph lic portion of the metenceph lon (Figs. 1 9.27 nd 19.28). The corpus stri tum (Fig. 19.24B), being p rt of the w ll of the hemisphere, likewise exp nds posteriorly nd is divided into two p rts: ( ) dorsomedi l portion, the c ud te nucleus, nd (b) ventrol ter l portion, the lentiform nucleus (Fig. 19.27B). This division is ccomplished by xons p ssing to nd from the cortex of the hemisphere nd bre king through the nucle r m ss of the corpus stri tum. The ber bundle thus formed is known s the intern l c psu le (Fig. 19.27B). At the s me time, the medi l w ll of the
Ch pter 19: Centr l Nervous System 459 Figure 19.27 A. Medi l surf ce of the right h lf of the telenceph lon nd dience ph lon in 10-week embryo. B. Tr nsverse section through the hemisphere nd die nceph lon t the level of the broken line in A. hemisphere nd the l ter l w ll of the dienceph lon fuse, nd the c ud te nucleu s nd th l mus come into close cont ct (Fig. 19.27B ). Continuous growth of the cerebr l hemispheres in nterior, dors l, nd inferior directions results in the form tion of front l, tempor l, nd occipit l lobes, respectively. As growth in the region overlying the corpus stri tum slows,
460 P rt Two: Speci l Embryology
however, the re between the front l nd tempor l lobes becomes depressed nd i s known s the insul (Fig. 19.28A). This region is l ter overgrown by the dj c ent lobes nd t the time of birth is lmost completely covered. During the n l p rt of fet l life, the surf ce of the cerebr l hemispheres grows so r pidly th t gre t m ny convolutions (gyri) sep r ted by ssures nd sulci ppe r on its sur f ce (Fig. 19.28B). Cortex Development. The cerebr l cortex develops from the p llium (Fig. 19.24), which h s two regions: ( ) the p leop llium, or rchip llium , immedi tely l ter l to the corpus stri tum (Fig. 19.25B), nd (b) the neop lli um, between the hippoc mpus nd the p leop llium (Figs. 19.25B nd 19.27B). In t he neop llium, w ves of neurobl sts migr te to subpi l position nd then diffe renti te into fully m ture neurons. When the next w ve of neurobl sts rrives, t hey migr te through the e rlier-formed l yers of cells until they re ch the subp i l position. Hence the e rly-formed neurobl sts obt in deep position in the c ortex, while those formed l ter obt in more super ci l position. At birth the co rtex h s str ti ed ppe r nce due to differenti tion of the cells in l yers. The motor cortex cont ins l rge number of pyr mid l cells, nd the sensory re s re ch r cterized by gr nul r cells. Olf ctory Bulbs. Differenti tion of the olf ctory system is dependent upon epitheli l-mesenchym l inter ctions. These occur between neur l crest cells nd ectoderm of the fronton s l prominence to form t he olf ctory pl codes (Fig. 19.29) nd between these s me crest cells nd the oor of the telenceph lon to form the olf ctory bulbs. Cells in the n s l pl codes d ifferenti te into prim ry sensory neurons of the n s l epithelium whose xons gr ow nd m ke cont ct with second ry neurons in the developing olf ctory bulbs (Fi g. 19.29). By the seventh week, these cont cts re well est blished. As growth o f the br in continues, the olf ctory bulbs nd the olf ctory tr cts of the secon d ry neurons lengthen, nd together they constitute the olf ctory nerve (Fig. 19 .30).
Figure 19.28 Development of gyri nd sulci on the l ter l surf ce of the cerebr l hemisphere. A. 7 months. B. 9 months.
Ch pter 19: Centr l Nervous System 461 W ll of br in N s l pit Medi l n s l prominence Bre kdown of oron s l membr ne Or l c vity Or l c vity A Oron s l membr ne Tongue B Olf ctory bulb Conch e M xill Upper lip Lower lip
Olf ctory bulb Second ry p l te M ndible C D
Figure 19.29 A. S gitt l section through the n s l pit nd lower rim of the medi l n s l prominence of 6-week embryo. The primitive n s l c vity is sep r ted from the or l c vity by the oron s l membr ne. B. Simil r section s in A tow rd the end of the sixth week showing bre kdown of the oron s l membr ne. C. At 7 w eeks, neurons in the n s l epithelium h ve extended processes th t cont ct the oo r of the telenceph lon in the region of the developing olf ctory bulbs. D. By 9 weeks, de nitive oron s l structures h ve formed, neurons in the n s l epithelium re well differenti ted, nd second ry neurons from the olf ctory bulbs to the b r in begin to lengthen. Togther, the olf ctory bulbs nd tr cts of the second ry neurons constitute the olf ctory nerve (see Fig. 19.30). Commissures. In the dult, number of ber bundles, the commissures, which cross the midline, connect the right nd left h lves of the hemispheres. The most impo rt nt ber bundles m ke use of the l min termin lis (Figs. 19.24, 19.27, nd 19.3 0). The rst of the crossing bundles to ppe r is the nterior commissure. It cons ists of bers connecting the olf ctory bulb nd rel ted br in re s of one hemisph ere to those of the opposite side (Figs. 19.27 nd 19.30). The second commissure to ppe r is the hippoc mp l commissure, or fornix commissure. Its bers rise in the hippoc mpus nd converge on the l min termin lis close to the roof pl te o f the dienceph lon. From here the bers continue, forming n rching system immedi tely outside the choroid ssure, to the m mill ry body nd the hypoth l mus. The most import nt commissure is the corpus c llosum. It ppe rs by the 10th week of development nd connects the nonolf ctory re s of the right nd the left cereb r l cortex. Initi lly, it forms sm ll bundle in the l min termin lis. As re sult of continuous exp nsion of the neop llium, however, it extends rst
Definitive cho n
N s l ch mber Primitive cho n
Prim ry p l te
462 P rt Two: Speci l Embryology Figure 19.30 Medi l surf ce of the right h lf of the br in in 4-month embryo s howing the v rious commissures. Broken line, future site of the corpus c llosum. The hippoc mp l commissure is not indic ted. nteriorly nd then posteriorly, rching over the thin roof of the dienceph lon (Fig. 19.30). In ddition to the three commissures developing in the l min term in lis, three more ppe r. Two of these, the posterior nd h benul r commissures , re just below nd rostr l to the st lk of the pine l gl nd. The third, the op tic chi sm , which ppe rs in the rostr l w ll of the dienceph lon, cont ins bers from the medi l h lves of the retin e (Fig. 19.30). Molecul r Regul tion of Br in Development Anteroposterior (cr nioc ud l) p tterning of the centr l nervous system begins e rly in development, during g strul tion nd neur l induction (se e Ch pters 4 nd 5). Once the neur l pl te is est blished, sign ls for segreg ti on of the br in into forebr in, midbr in, nd hindbr in regions re derived from homeobox genes expressed in the notochord, prechord l pl te, nd neur l pl te. The hindbr in h s eight segments, the rhombomeres, th t h ve v ri ble expression p tterns of the Antenn pedi cl ss of homeobox genes, the HOX genes (see Ch pte r 5). These genes re expressed in overl pping p tterns, with genes t the most 3 end of cluster h ving more nterior bound ries nd p r logous genes h ving i dentic l expression dom ins (Fig. 19.31). Genes t the 3 end re lso expressed e rlier th n those t the 5 end, so th t tempor l rel tion
Ch pter 19: Centr l Nervous System 463 Figure 19.31 P tterns of HOX gene expression in the hindbr in nd the p ttern of neur l crest cell migr tion into the ph rynge l rches. HOX genes re expressed in overl pping p tterns ending t speci c rhombomere bound ries. Genes t the 3 e nd of cluster h ve the most nterior bound ries, nd p r logous genes h ve ide ntic l expression dom ins. These genes confer position l v lue long the nterio r-posterior xis of the hindbr in, determine the identity of the rhombomeres, n d specify their deriv tives. to the expression p ttern is est blished. These genes, then, confer position l v lue long the nteroposterior xis of the hindbr in, determine the identity of the rhombomeres, nd specify their deriv tives. How this regul tion occurs is no t cle r, lthough the retinoids (retinoic cid) pl y critic l role in regul ti ng HOX expression. For ex mple, excess retinoic cid shifts HOX gene expression nteriorly nd c uses more cr ni l rhombomeres to differenti te into more c ud l types. Retinoic cid de ciency results in sm ll hindbr in. There is lso diff erenti l response to retinoic cid by the HOX genes; those t the 3 end of the c luster re more sensitive th n those t the 5 end. Speci c tion of the forebr in nd midbr in re s is lso regul ted by genes cont ining homeodom in. However, these genes re not of the Antenn pedi cl ss, whose most nterior bound ry of e xpression stops t rhombomere 3. Thus, new genes h ve ssumed the p tterning rol e for these regions of the
464 P rt Two: Speci l Embryology Figure 19.32 Overl pping expression p tterns of homeobox genes th t specify the identities of the forebr in nd midbr in regions. br in, which evolution rily constitute the new he d. At the neur l pl te st ge, LI M1, expressed in the prechord l pl te, nd OTX2, expressed in the neur l pl te, re import nt for design ting the forebr in nd midbr in re s, with LIM1 suppor ting OTX2 expression. (These genes re lso expressed t the e rliest st ges of g strul tion, nd they ssist in specifying the entire cr ni l region of the epi bl st.) Once the neur l folds nd ph rynge l rches ppe r, ddition l homeobox genes, including OTX1, EMX1, nd EMX2 re expressed in speci c nd in overl pping (nested) p tterns (Fig. 19.32) th t specify the identity of the forebr in nd mi dbr in regions. Once these bound ries re est blished, two ddition l org nizing centers ppe r: the nterior neur l ridge (ANR) t the junction of the cr ni l border of the neur l pl te nd nonneur l ectoderm (Fig. 19.33) nd the isthmus ( Fig. 19.34) between the hindbr in nd midbr in. In both loc tions, brobl st growt h f ctor-8 (FGF-8) is the key sign ling molecule, inducing subsequent gene expre ssion th t regul tes differenti tion. In the ANR t the four-somite st ge, FGF-8 induces expression of br in f ctor 1 (BF1; Fig. 19.33). BF1 then regul tes deve lopment of the telenceph lon (cerebr l hemispheres) nd region l speci c tion with in the forebr in, including the b s l telenceph lon nd the retin . In the isthm us t the junction between the midbr in nd hindbr in territories, FGF-8 is expr essed in ring round the circumference of this loc tion (Fig. 19.34). FGF-8 in duces expression of engr iled 1 nd 2 (EN1 nd EN2 ), two homeobox-cont ining ge nes, expressed in gr dients r di ting nteriorly nd posteriorly from the isthmu s. EN1 regul tes development throughout its expression dom in, including the dor s l midbr in (tectum) nd nterior hindbr in (cerebellum), where s EN2 is involv ed only in cerebell r development. FGF-8 lso induces WNT1 expression in
Ch pter 19: Centr l Nervous System 465 ANR Figure 19.33 Di gr m illustr ting the org nizing center known s the nterior ne ur l ridge (ANR). This re lies in the most nterior region of the neur l pl te nd secretes FGF-8, which induces expression of br in f ctor 1 (BF1) in dj cen t neurectoderm. BF1 regul tes development of the telenceph lon (cerebr l hemisph eres) nd region l speci c tion within the prosenceph lon (PR). Sonic hedgehog (SH H), secreted by the prechord l pl te (P) nd notochord (N), ventr lizes the br i n nd induces expression of NKX2.1, which regul tes development of the hypoth l mus. Bone morphogenetic proteins 4 nd 7, secreted by the dj cent nonneur l ect oderm, control dors l p tterning of the br in. M, mesenceph lon; R, rhombenceph lon. circumferenti l b nd nterior to the region of FGF-8 expression (Fig. 19.34). WN T1 inter cts with EN1 nd EN2 to regul te development of this region, including the cerebellum. In f ct, WNT1 m y ssist in e rly speci c tion of the midbr in re since it is expressed in this region t the neur l pl te st ge. FGF8 is lso e xpressed t this e rly time in mesoderm underlying the midbr inhindbr in junctio n nd m y therefore regul te WNT1 expression nd initi l p tterning of this regi on. The constriction for the isthmus is slightly posterior to the ctu l midbr i n-hindbr in junction, which lies t the c ud l limit of OTX2 expression (Fig. 19 .32). Dorsoventr l (mediol ter l) p tterning lso occurs in the forebr in nd mi dbr in re s. Ventr l p tterning is controlled by SHH just s it is throughout t he rem inder of the centr l nervous system. SHH, secreted by the prechord l pl t e, induces expression of NKX2.1, homeodom in-cont ining gene th t regul tes
466 P rt Two: Speci l Embryology R1 R2 R3 R4 R5 R6 R7 R8 Spin l Cord D T P M N FGF8 WNT1 EN1, 2 SHH Figure 19.34 Org nizing center in the isthmus t the bound ries between the midb r in nd hindbr in. This region secretes FGF-8 in circumferenti l ring th t in duces expression of engr iled 1 nd 2(EN1 nd EN2) in gr dients nteriorly nd p osteriorly from this re . EN1 regul tes development of the dors l midbr in, nd both genes p rticip te in form tion of the cerebellum. WNT1, nother gene induc ed by FGF-8, lso ssists in development of the cerebellum. N, notochord; P, pre chord l pl te. development of the hypoth l mus. Interestingly, SHH sign ling requires cle v ge of the protein. The c rboxy termin l portion executes this process, which lso i ncludes cov lent link ge of cholesterol to the c rboxy terminus of the mino ter min l product. The mino termin l portion ret ins ll of the sign ling propertie s of SHH, nd its ssoci tion with cholesterol ssists in its distribution. Dors l (l ter l) p tterning of the neur l tube is controlled by bone morphogenetic p roteins 4 nd 7 (BMP4 nd BMP7) expressed in the nonneur l ectoderm dj cent to the neur l pl te. These proteins induce expression of MSX1 in the midline nd re press expression of BF1 (Fig. 19.33). Expression p tterns of genes regul ting n terior-posterior (cr nioc ud l) nd dorsoventr l (mediol ter l) p tterning of th e br in overl p nd inter ct t the borders of these regions. Furthermore, v rio us br in regions re competent to respond to speci c sign ls nd not to others. Fo r ex mple, only the cr ni l p rt of the neur l pl te expresses NKX2.1 in respons e to SHH. Likewise, only the nterior neur l pl te produces BF1 in response to F GF-8; midbr in levels express EN2 in response to the s me FGF-8 sign l. Thus, competence to respond lso ssists in specifying region l differences. CLINICAL CORRELATES
Cr ni l Defects Holoprosenceph ly (HPE) refers to spectrum of bnorm lities in which loss of midline structures results in m lform tions of the br in nd f ce. In severe c ses, the l ter l ventricles merge into single telenceph lic ve sicle ( lob r HPE), the eyes re fused, nd there is single n s l ch mber lon g
Ch pter 19: Centr l Nervous System 467 Figure 19.35 Holoprosenceph ly nd fusion of the eyes (synophth lmi ). A loss of the midline in the br in c uses the l ter l ventricles to merge into single c h mber nd the eye elds to f il to sep r te. Mut tions in the gene sonic hedgehog (SHH), which speci es the midline of the centr l nervous system t neur l pl te s t ges, is one c use for this spectrum of bnorm lities. with other midline f ci l defects (Fig. 19.35). In less severe c ses, some divis ion of the prosenceph lon into two cerebr l hemispheres occurs, but there is inc omplete development of midline structures. Usu lly the olf ctory bulbs nd tr ct s nd the corpus c llosum re hypopl stic or bsent. In very mild c ses, sometim es the only indic tion th t some degree of HPE h s occurred is the presence of single centr l incisor. HPE occurs in 1 in 15,000 live births, but is present i n 1 in 250 pregn ncies th t end in e rly misc rri ge. Mut tions in SHH, the gene th t regul tes est blishment of the ventr l midline in the CNS, result in some forms of holoprosenceph ly. Another c use is defective cholesterol biosynthesis le ding to Smith-Lemli-Opitz syndrome. These children h ve cr niof ci l nd limb defects, nd 5% h ve holoprosenceph ly. Smith-Lemli-Opitz syndrome is due to b norm lities in 7-dehydrocholesterol reduct se, which met bolizes 7-dehydrocholes terol to cholesterol. M ny of the defects, including those of the limbs nd br i n, m y be due to bnorm l SHH sign ling, since cholesterol is necess ry for this gene to exert its effects (see p ge 466). Other genetic c uses include mut tion s in the tr nscription f ctors sine occulis homeobox3 (SIX3), TG inter cting f c tor (TGIF) nd the zinc nger protein ZIC2. Yet nother c use of holoprosenceph ly is lcohol buse, which t e rly st ges of development selectively kills midlin e cells.
468 P rt Two: Speci l Embryology Schizenceph ly is r re disorder in which l rge clefts occur in the cerebr l he mispheres, sometimes c using loss of br in tissue. Mut tions in the homeobox g ene EMX2 ppe r to ccount for some of these c ses. Meningocele, meningoenceph l ocele, nd meningohydroenceph locele re ll c used by n ossi c tion defect in th e bones of the skull. The most frequently ffected bone is the squ mous p rt of the occipit l bone, which m y be p rti lly or tot lly l cking. If the opening of the occipit l bone is sm ll, only meninges bulge through it (meningocele), but if the defect is l rge, p rt of the br in nd even p rt of the ventricle m y pen etr te through the opening into the meninge l s c (Figs. 19.36 nd 19.37). The l tter two m lform tions re known s meningoenceph locele nd meningohydroenceph locele, respectively. These defects occur in 1/2000 births. Exenceph ly is ch r cterized by f ilure of the ceph lic p rt of the neur l tube to close. As resu lt, the v ult of the skull does not form, le ving the m lformed br in exposed. L ter this tissue degener tes, le ving m ss of necrotic tissue. This defect is c lled nenceph ly, lthough the br instem rem ins int ct (Fig. 19.38, A nd B). Since the fetus l cks the mech nism for sw llowing, the l st 2 months of pregn ncy re ch r cterized by hydr mnios. The bnorm lity c n be recognized on r di ogr ph, since the v ult of the skull is bsent. Anenceph ly is common bnorm l ity (1/1500) th t occurs 4 times more often in fem les th n in m les. Like spin bi d , up to 70% of these c ses c n be prevented by h ving women t ke 400 g of fol ic cid per d y before nd during pregn ncy. Hydroceph lus is ch r cterized by n bnorm l ccumul tion of cerebrospin l uid within the ventricul r system. In mo st c ses, hydroceph lus in the newborn is due to n obstruction of the queduct of Sylvius ( queduct l stenosis). This prevents the cerebrospin l uid of the l te r l nd third ventricles from p ssing into the fourth ventricle nd from there i nto the sub r chnoid sp ce, where it would be resorbed. As result, uid ccumul tes Figure 19.36 AD. V rious types of br in herni tion due to bnorm l ossi c tion of t he skull.
Ch pter 19: Centr l Nervous System 469 Figure 19.37 Ultr sonogr m (top) nd photogr ph (bottom) of child with menin goenceph locele. The defect w s detected by ultr sound in the seventh month of g est tion nd rep ired fter birth. Ultr sound shows br in tissue ( rrows) extend ing through the bony defect in the skull ( rrowhe ds). in the l ter l ventricles nd presses on the br in nd bones of the skull. Since the cr ni l sutures h ve not yet fused, sp ces between them widen s the he d e xp nds. In extreme c ses, br in tissue nd bones become thin nd the he d m y be very l rge (Fig. 19.39). The Arnold-Chi ri m lform tion is c ud l displ cement nd herni tion of cerebell r structures through the for men m gnum. Arnold-Chi r i m lform tion occurs in virtu lly every c se of spin bi d cystic nd is usu ll y ccomp nied by hydroceph lus. Microceph ly describes cr ni l v ult th t is s m ller th n norm l (Fig. 19.40). Since the size of the cr nium depends on growth of the br in, the
470 P rt Two: Speci l Embryology Figure 19.38 A. Anenceph lic child, ventr l view. This bnorm lity occurs freque ntly (1/1500 births). Usu lly the child dies few d ys fter birth. B. Anenceph lic child with spin bi d in the cervic l nd thor cic segments, dors l view. Figure 19.39 Child with severe hydroceph lus. Since the cr ni l sutures h d not closed, pressure from the ccumul ted cerebrospin l uid enl rged the he d, thinni ng the bones of the skull nd cerebr l cortex.
Ch pter 19: Centr l Nervous System 471 Figure 19.40 Child with microceph ly. This bnorm lity, due to poor growth of th e br in, is frequently ssoci ted with ment l ret rd tion. underlying defect is in br in development. C us tion of the bnorm lity is v rie d; it m y be genetic ( utosom l recessive) or due to pren t l insults such s in fection or exposure to drugs or other ter togens. Imp ired ment l development oc curs in more th n h lf of c ses. Fet l infection by toxopl smosis m y result in cerebr l c lci c tion, ment l ret rd tion, hydroceph lus, or microceph ly. Likewis e, exposure to r di tion during the e rly st ges of development m y produce micr oceph ly. Hyperthermi produced by m tern l infection or by s un b ths m y c us e spin bi d nd exenceph ly. The forementioned bnorm lities re the most serio us ones, nd they m y be incomp tible with life. A gre t m ny other defects of t he CNS m y occur without much extern l m nifest tion. For ex mple, the corpus c llosum m y be p rti lly or completely bsent without much function l disturb nce . Likewise, p rti l or complete bsence of the cerebellum m y result in only s light disturb nce of coordin tion. On the other h nd, c ses of severe ment l ret rd tion m y not be ssoci ted with morphologic lly detect ble br in bnorm liti es. Ment l ret rd tion m y result from genetic bnorm lities (e.g., Down nd Kli nefelter syndromes) or from exposures to ter togens, including infectious gents (rubell , cytomeg lovirus, toxopl smosis). The le ding c use of ment l ret rd t ion is, however, m tern l lcohol buse.
472 P rt Two: Speci l Embryology Figure 19.41 Segment tion p tterns in the br in nd mesoderm th t ppe r by the 25th d y of development. The hindbr in (co rse stipple) is divided into 8 rhombo meres (r1 to r8), nd these structures give rise to the cr ni l motor nerves (m) . P1P4, ph rynge l (br nchi l) rches; t, telenceph lon; d, dienceph lon; m, mese nceph lon. Cr ni l Nerves By the fourth week of development, nuclei for ll 12 cr ni l nerv es re present. All except the olf ctory (I) nd optic (II) nerves rise from th e br instem, nd of these only the oculomotor (III) rises outside the region of the hindbr in. In the hindbr in, prolifer tion centers in the neuroepithelium e st blish eight distinct segments, the rhombomeres. These rhombomeres give rise t o motor nuclei of cr ni l nerves IV, V, VI, VII, IX, X, XI, nd XII (Figs. 19.17 nd 19.41). Est blishment of this segment l p ttern ppe rs to be directed by m esoderm collected into somitomeres bene th the overlying neuroepithelium. Motor neurons for cr ni l nuclei re within the br instem, while sensory g ngli re o utside of the br in. Thus the org niz tion of cr ni l nerves is homologous to th t of spin l nerves, lthough not ll cr ni l nerves cont in both motor nd sens ory bers (T ble 19.1, p. 473474). Cr ni l nerve sensory g ngli origin te from ect oderm l pl codes nd neur l crest cells. Ectoderm l pl codes include the n s l, otic, nd four epibr nchi l pl codes represented by ectoderm l thickenings dors l to the ph rynge l (br nchi l) rches (T ble 19.2, p. 475; see Fig. 15.2). Epib r nchi l pl codes contribute to g ngli for nerves of the ph rynge l rches (V, VII, IX, nd X). P r symp thetic (viscer l efferent) g ngli re derived from ne ur l crest cells, nd their bers re c rried by cr ni l nerves III, VII, IX, nd X (T ble 19.1).
Ch pter 19: Centr l Nervous System TABLE 19.1 473 Origins of Cr ni l Nerves nd Their Composition Br in Region Telenceph lon Dienceph lon Mesenceph lon Type SVA SSA GSE Innerv t ion N s l epithelium (smell) Retin (vision) Sup., inf., med. Rectus, inf. obliq ue, lev tor p lpebr e sup. m. sphincter pupill e, cili ry m. Sup. oblique m. Cr ni l Nerve Olf ctory (I) Optic (II) Oculomotor (III) Trochle r (IV) Trigemin l (V) Metenceph lon (exits mesenceph lon) Metenceph lon GVE (cili ry g nglion) GSE GSA (trigemin l g nglion) GVA (trigemin l g nglion) SVE (br nchiomotor) Abducens (VI) F ci l (VII) Metenceph lon Metenceph lon GSE SVA (genicul te g nglion) GSA (genicul te g nglion) GVA (genicul te g nglion ) SVE (br nchiomotor) GVE Vestibulocochle r (VIII) Metenceph lon SSA (vestibul r nd spir l g ngli ) Glossoph rynge l (IX) Myelenceph lon SVA (inferior g nglion) GVA (superior g nglion) GSA (inferior g nglion) SVE Styloph ryngeus (br nchiomotor) GVE (otic g nglion) P rotid gl nd Skin, mouth, f ci l m., teeth, nt. two thirds of tongue proprioception: skin, m uscles, joints M. of m stic tion, mylohyoid, nt. belly of dig stric, tensor vel ip l tini, post. belly of di g stric m. L ter l rectus m. T ste nt. two thirds of tongue Skin ext. uditory me tus Ant. two thirds of tongue M. of f ci l expre ssion, st peduis, stylohyoid, post. belly of dig stric Subm ndibul r, sublingu l , nd l crim l gl nds Semicircul r c n ls, utricle, s ccule (b l nce) spir l org n of Corti (he ring) Post. one third of tongue (t ste) P rotid gl nd, c rotid b ody nd sinus, middle e r Extern l e r (Continued )
474 P rt Two: Speci l Embryology TABLE 19.1 (Continued) Br in Region Myelenceph lon Type SVA (inferior g nglion) GVA (superior g nglion) Innerv tion P l te nd epiglottis (t ste) B se of tongue, ph rynx, l rynx, tr c he , he rt, esoph gus, stom ch, intestines Extern l uditory me tus Constrictor m. ph rynx, intrinsic m. l rynx, sup. two thirds esoph gus Tr che , bronchi, dig estive tr ct, he rt Sternocleidom stoid, tr pezius m. Solf p l te, ph rynx (with X) M. of tongue (except p l togl ssus) Cr ni l Nerve V gus (X) GSA (superior g nglion) SVE (br nchiomotor) Spin l Accessory Myelenceph lon (XI)
Hypogloss l (XII) Myelenceph lon SVA, Speci l Viscer l Aff rent; SSA, Speci l Som tic Aff rent; SVE, Speci l Visc er l Efferent; GVE, Gener l Viscer l Efferent; GSE, Gener l Som tic Efferent; GS A, Gener l Som tic Aff rent; GVA, Gener l Viscer l Aff rent. Autonomic Nervous System Function lly the utonomic nervous system c n be divide d into two p rts: symp thetic portion in the thor columb r region nd p r sy mp thetic portion in the ceph lic nd s cr l regions. SYMPATHETIC NERVOUS SYSTEM In the fth week, cells origin ting in the neur l crest of the thor cic region mi gr te on e ch side of the spin l cord tow rd the region immedi tely behind the d ors l ort (Fig. 19.42). Here they form bil ter l ch in of segment lly rr ng ed symp thetic g ngli interconnected by longitudin l nerve bers. Together they f orm the symp thetic ch ins on e ch side of the vertebr l column. From their posi tion in the thor x, neurobl sts migr te tow rd the cervic l nd lumbos cr l regi ons, extending the symp thetic ch ins to their full length. Although initi lly t he g ngli re rr nged segment lly, this rr ngement is l ter obscured, p rticu l rly in the cervic l region, by fusion of the g ngli . Some symp thetic neurobl sts migr te in front of the ort to form pre ortic g ngli , such s the celi c nd mesenteric g ngli . Other symp thetic cells migr te to the he rt, lungs, n d g strointestin l tr ct, where they give rise to symp thetic org n plexuses (Fi g. 19.42).
GVE (g ngli
t or ne r viscer ) SVE (br nchiomotor) GSE GSE
Ch pter 19: Centr l Nervous System TABLE 19.2 475 Contributions of Neur l Crest Cells nd Pl codes to G ngli of the Cr ni l Nerve s G nglion Cili ry (viscer l efferent) Origin Neur l crest t forebr in-midbr in j unction Neur l crest t forebr in-midbr in junction, trigemin l pl code Hindbr i n neur l crest, rst epibr nchi l pl code First epibr nchi l pl code Hindbr in neu r l crest Hindbr in neur l crest Otic pl code Otic pl code, hindbr in neur l cre st Hindbr in neur l crest Second epibr nchi l pl code Hindbr in neur l crest Hin dbr in neur l crest Hindbr in neur l crest; third, fourth epibr nchi l pl codes Hindbr in neur l crest Nerve Oculomotor (III) Trigemin l (V) Trigemin l (gener l fferent) F ci l (VII) Vestibulocochle r (VIII) Superior (gener l nd speci l fferent) Inferior (genicul te) (gener l nd speci l fferent) Sphenop l tine (viscer l efferent) Subm ndibul r (viscer l efferent ) Acoustic (cochle r) (speci l fferent) Vestibul r (speci l fferent) Superior (gener l nd speci l fferent) Inferior (petros l) (gener l nd speci l fferent ) Otic (viscer l efferent) Superior (gener l fferent) Inferior (nodose) (gener l nd speci l fferent) V g l p r symp thetic (viscer l efferent) Glossoph rynge l (IX) V gus (X) Once the symp thetic ch ins h ve been est blished, nerve bers origin ting in the visceroefferent column (intermedi te horn) of the thor columb r segments (T1-L1, 2) of the spin l cord penetr te the g ngli of the ch in (Fig. 19.43). Some of t hese nerve bers syn pse t the s me levels in the symp thetic ch ins or p ss thro ugh the ch ins to pre ortic or coll ter l g ngli (Fig. 19.43). They re known s preg nglionic bers, h ve myelin she th, nd stimul te the symp thetic g nglio n cells. P ssing from spin l nerves to the symp thetic g ngli , they form the wh ite communic ting r mi. Since the visceroefferent column extends only from the rs t thor cic to the second or third lumb r segment of the spin l cord, white r mi re found only t these levels. Axons of the symp thetic g nglion cells, the pos tg nglionic bers, h ve no myelin she th. They either p ss to other levels of the symp thetic ch in or extend to the he rt, lungs, nd intestin l tr ct (broken li nes in Fig. 19.43).
476 P rt Two: Speci l Embryology Figure 19.42 Form tion of the symp thetic g ngli . A portion of the symp thetic neurobl sts migr tes tow rd the prolifer ting mesothelium to form the medull of the supr ren l gl nd. Other bers, the gr y communic ting r mi, p ss from the symp thetic ch in to spin l nerves nd from there to peripher l blood vessels, h ir, nd swe t gl nds. Gr y communic ting r mi re found t ll levels of the spin l cord. Supr ren l Gl n d The supr ren l gl nd develops from two components: ( ) mesoderm l portion, w hich forms the cortex, nd (b) n ectoderm l portion, which forms the medull . D uring the fth week of development, mesotheli l cells between the root of the mese ntery nd the developing gon d begin to prolifer te nd penetr te the underlying mesenchyme (Fig. 19.42). Here they differenti te into l rge cidophilic org ns, which form the fet l cortex, or primitive cortex, of the supr ren l gl nd (Fig. 19.44A). Shortly fterw rd second w ve of cells from the mesothelium penetr t es the mesenchyme nd surrounds the origin l cidophilic cell m ss. These cells, sm ller th n those of the rst w ve, l ter form the de nitive cortex of the gl nd ( Fig. 19.44, A nd B). After birth the fet l cortex regresses r pidly except for its outermost l yer, which differenti tes into the reticul r zone. The dult str ucture of the cortex is not chieved until puberty. While the fet l cortex is be ing formed, cells origin ting in the symp thetic system (neur l crest cells) inv de its medi l spect, where they re rr nged in cords nd clusters. These cell s give rise to the medull of the supr ren l gl nd. They st in yellow-brown with chrome s lts nd hence re c lled chrom f n
Ch pter 19: Centr l Nervous System 477 Figure 19.43 Rel tion of the preg nglionic nd postg nglionic nerve bers of the s ymp thetic nervous system to the spin l nerves. Note the origin of preg nglionic bers in the visceroefferent column of the spin l cord. cells (Fig. 19.44). During embryonic life, chrom f n cells re sc ttered widely th roughout the embryo, but in the dult the only persisting group is in the medull of the dren l gl nds. PARASYMPATHETIC NERVOUS SYSTEM Neurons in the br instem nd the s cr l region of the spin l cord give rise to preg nglionic p r symp thetic bers. Fibers from nuc lei in the br instem tr vel vi the oculomotor (III), f ci l (VII), glossoph ryn ge l (IX), nd v gus (X) nerves. Postg nglionic bers rise from neurons (g ngli ) derived from neur l crest cells nd p ss to the structures they innerv te (e.g. , pupil of the eye, s liv ry gl nds, viscer ).
478 P rt Two: Speci l Embryology Figure 19.44 A. Chrom f n (symp thetic) cells penetr ting the fet l cortex of the supr ren l gl nd. B. L ter in development the de nitive cortex surrounds the medul l lmost completely. CLINICAL CORRELATES Congenit l Meg colon (Hirschsprung Dise se) Congenit l meg colon (Hirschsprung d ise se) results from f ilure of p r symp thetic g ngli to form in the w ll of p rt or ll of the colon nd rectum bec use the neur l crest cells f il to migr te. Most f mili l c ses of Hirschsprung dise se re due to mut tions in the RET gene, which codes for cell membr ne tyrosine kin se receptor. This gene on ch romosome 10q11 is essenti l for crest cell migr tion. The lig nd for the recepto r is gli l cell derived neurotrophic growth f ctor (GDNF) secreted by mesenchyme cells through which crest cells migr te. Receptor lig nd inter ctions then regul te crest cell migr tion. Consequently, if there re bnorm lities in the recept or, migr tion is inhibited nd no p r symp thetic g ngli form in ffected re s . The rectum is involved in ne rly ll c ses, nd the rectum nd sigmoid re inv olved in 80% of ffected inf nts. The tr nsverse nd scending portions of the c olon re involved in only 10 to 20%. The colon is dil ted bove the ffected reg ion, which h s sm ll di meter bec use of tonic contr ction of noninnerv ted mu scul ture.
Summ ry The e middle of eur l folds s. 19.2 nd
CNS origin tes in the ectoderm nd ppe rs s the neur l pl te t th the third week (Fig. 19.1). After the edges of the pl te fold, the n ppro ch e ch other in the midline to fuse into the neur l tube (Fig 19.3). The cr ni l end closes pproxim tely
Ch pter 19: Centr l Nervous System 479 t d y 25, nd the c ud l end closes t d y 27. The CNS then forms tubul r str ucture with bro d ceph lic portion, the br in, nd long c ud l portion, the spin l cord. F ilure of the neur l tube to close results in defects such s spin bi d (Figs. 19.15 nd 19.16) nd nenceph ly (Fig. 19.38), defects th t c n be prevented by folic cid. The spin l cord, which forms the c ud l end of the CNS, is ch r cterized by the b s l pl te cont ining the motor neurons, the l r pl t e for the sensory neurons, nd oor pl te nd roof pl te s connecting pl tes between the two sides (Fig. 19.8). SHH ventr lizes the neur l tube in the spin l cord region nd induces the oor nd b s l pl tes. Bone morphogenetic proteins 4 nd 7, expressed in nonneur l ectoderm, m int in nd up-regul te expression of P AX3 nd PAX7 in the l r nd roof pl tes. The br in, which forms the cr ni l p r t of the CNS, consists origin lly of three vesicles: the rhombenceph lon (hindbr in), mesenceph lon (midbr in), nd prosenceph lon (forebr in). The rhombenceph lon is divided into ( ) the myelenceph lon, which forms the medull oblong t (t his region h s b s l pl te for som tic nd viscer l efferent neurons nd n l r pl te for som tic nd viscer l fferent neurons) (Fig. 19.18), nd (b) the me tenceph lon, with its typic l b s l (efferent) nd l r ( fferent) pl tes (Fig. 19.19). This br in vesicle is lso ch r cterized by form tion of the cerebellum (Fig. 19.20), coordin tion center for posture nd movement, nd the pons, the p thw y for nerve bers between the spin l cord nd the cerebr l nd the cerebell r cortices (Fig. 19.19). The mesenceph lon, or midbr in, resembles the spin l co rd with its b s l efferent nd l r fferent pl tes. The mesenceph lons l r pl t es form the nterior nd posterior colliculi s rel y st tions for visu l nd u ditory re ex centers, respectively (Fig. 19.23). The dienceph lon, the posterior p ortion of the forebr in, consists of thin roof pl te nd thick l r pl te in which the th l mus nd hypoth l mus develop (Figs. 19.24 nd 19.25). It p rtici p tes in form tion of the pituit ry gl nd, which lso develops from R thkes pouch (Fig. 19.26). R thkes pouch forms the denohypophysis, the intermedi te lobe, n d p rs tuber lis, nd the dienceph lon forms the posterior lobe, the neurohypoph ysis, which cont ins neurogli nd receives nerve bers from the hypoth l mus. The telenceph lon, the most rostr l of the br in vesicles, consists of two l ter l outpocketings, the cerebr l hemispheres, nd medi n portion, the l min termin lis (Fig. 19.27). The l min termin lis is used by the commissures s connect ion p thw y for ber bundles between the right nd left hemispheres (Fig. 19.30). The cerebr l hemispheres, origin lly two sm ll outpocketings (Figs. 19.24 nd 19 .25), exp nd nd cover the l ter l spect of the dienceph lon, mesenceph lon, n d metenceph lon (Figs. 19.2619.28). Eventu lly, nucle r regions of the telenceph lon come in close cont ct with those of the dienceph lon (Fig. 19.27). The ventr icul r system, cont ining cerebrospin l uid, extends from the lumen in the spin l cord to the fourth ventricle in the rhombenceph lon, through
480 P rt Two: Speci l Embryology the n rrow duct in the mesenceph lon, nd to the third ventricle in the dienceph lon. By w y of the for min of Monro, the ventricul r system extends from the t hird ventricle into the l ter l ventricles of the cerebr l hemispheres. Cerebros pin l uid is produced in the choroid plexus of the third, fourth, nd l ter l ven tricles. Block ge of cerebrospin l uid in the ventricul r system or sub r chnoid sp ce m y le d to hydroceph lus. The br in is p tterned long the nteroposterio r (cr nioc ud l) nd dorsoventr l (mediol ter l) xes. HOX genes p ttern the nt eroposterior xis in the hindbr in nd specify rhombomere identity. Other tr nsc ription f ctors cont ining homeodom in p ttern the nteroposterior xis in the forebr in nd midbr in regions, including LIM1 nd OTX2. Two other org nizing c enters, the nterior neur l ridge nd the rhombenceph lic isthmus, secrete FGF-8 , which serves s the inducing sign l for these re s. In response to this growt h f ctor, the cr ni l end of the forebr in expresses BF1, which regul tes develo pment of the telenceph lon, nd the isthmus expresses engr iled genes th t regul te differenti tion of the cerebellum nd the roof of the midbr in. As it does t hroughout the centr l nervous system, SHH, secreted by the prechord l pl te nd notochord, ventr lizes the forebr in nd midbr in re s. Bone morphogenetic prot eins 4 nd 7, secreted by nonneur l ectoderm, induce nd m int in expression of dors lizing genes. Problems to Solve 1. How re cr ni l nerves nd spin l nerves simil r? How re t hey different? 2. At wh t level is spin l t p performed? From n embryologic l st ndpoint, why is this possible? 3. Wh t is the embryologic l b sis for most n eur l tube defects? C n they be di gnosed pren t lly? Are there ny me ns of pre vention? 4. Pren t l ultr sound reve ls n inf nt with n enl rged he d nd exp nsion of both l ter l ventricles. Wh t is this condition c lled, nd wh t might h ve c used it?
SUGGESTED READING Chi ng C, et l: Cyclopi nd defective xi l p tterning in mi ce l cking sonic hedgehog gene function. N ture 383:407, 1996. Cohen MM, Sulik K K: Perspectives on holoprosenceph ly: P rt II. Centr l nervous system, cr niof c i l n tomy, syndrome comment ry, di gnostic ppro ch, nd experiment l studies. J Cr niof c Genet Dev Biol 12:196, 1992. Cordes SP: Molecul r genetics of cr ni l nerve development in mouse. N t Rev Neurosci 2:611, 2001. Deh rt DB, L noue L , Tint GS, Sulik KK: P thogenesis of m lform tions in rodent model for Smith-L emli-Opitz syndrome. Am J Med Genet 68:328, 1997. G v lis A, Kruml uf R: Retinoi d sign ling nd hindbr in p tterning. Curr Op Genet Dev 10:380, 2000.
Ch pter 19: Centr l Nervous System 481 Geelen JAG, L ngm n J: Closure of the neur l tube in the ceph lic region of the mouse embryo. An t Rec 189:625, 1977. Hinrichsen K, Mestres P, J cob HJ: Morphol ogic l spects of the ph rynge l hypophysis in hum n embryos. Act Morphol Neerl Sc nd 24:235, 1986. Hu D, Helms JA: The role of sonic hedgehog in norm l nd b norm l cr niof ci l morphogenesis. Dev 126:4873, 1999. LeDou rin N, Font ine-Per us J, Couly G: Ceph lic ectoderm l pl codes nd neurogenesis. Trends Neurosci 9: 175, 1986. LeDou rin N, Smith J: Development of the peripher l nervous system fr om the neur l crest. Annu Rev Cell Biol 4:375, 1988. Le M nti AS, Bh sin N, Rho des K, Heemskerk J: Mesenchym l epitheli l induction medi tes olf ctory p thw y form tion. Neuron 28:411, 2000. Loggie JMH: Growth nd development of the utono mic nervous system. In D vis JA, Dobbing J (eds): Scienti c Found tions of Pedi tr ics. Phil delphi , WB S unders, 1974. Lumsden A, Kruml uf R: P tterning the vert ebr te neur xis. Science 274:1109, 1996. Lumsden A, Spr wson N, Gr h m A: Segmen t l origin nd migr tion of neur l crest cells in the hindbr in region of the ch ick embryo. Development 113:1281, 1991. Muller F, OR hilly R: The development of the hum n br in nd the closure of the rostr l neuropore t st ge 11. An t Embry ol 175:205, 1986. Muller F, OR hilly R: The development of the hum n br in from closed neur l tube t st ge 13. An t Embryol 177:203, 1986. OR hilly R, Muller F : The meninges in hum n development. J Neurop thol Exp Neurol 45:588, 1986. Rodi er PM, Reynolds SS, Roberts WN: Beh vior l consequences of interference with CNS development in the e rly fet l period. Ter tology 19:327, 1979. Roessler E, et l.: Mut tions in the hum n sonic hedgehog gene c use holoprosenceph ly. N t Gen et 14:357, 1996. Rubenstein JLR, Be chy PA: P tterning of the embryonic forebr i n. Curr Opin Neurobiol 8:18, 1998. S k i Y: Neurul tion in the mouse: 1. The ont ogenesis of neur l segments nd the determin tion of topogr phic l regions in centr l nervous system. An t Rec 218:450, 1987. Schoenwolf G: On the morphogenes is of the e rly rudiments of the developing centr l nervous system. Sc nning Ele ctron Microsc 1:289, 1982. Schoenwolf G, Smith JL: Mech nisms of neurul tion: tr dition l viewpoint nd recent dv nces. Development 109:243, 1990. Shim mur K, Rubenstein JLR: Inductive inter ctions direct e rly region liz tion of the mous e forebr in. Development 124:2709, 1997. T n be Y, Jessell TM: Diversity nd p t terning in the developing spin l cord. Science 274:1115, 1996. W tkins-Chow DE, C mper SA: How m ny homeobox genes does it t ke to m ke pituitory gl nd? Trend s Genet 14:284, 1998. Wilkie AOM, Morriss-K y GM: Genetics of cr niof ci l devel opment nd m lform tion. N t Rev Genet 2:458, 2001.
Вам также может понравиться
- Mock Papers for MRCPI, 3rd Edition: Four Mock Tests With 400 BOFsОт EverandMock Papers for MRCPI, 3rd Edition: Four Mock Tests With 400 BOFsОценок пока нет
- Test Bank Larsens Human Embryology 5th EditionДокумент22 страницыTest Bank Larsens Human Embryology 5th EditionRichard1LauritsenОценок пока нет
- Synovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandSynovial Chondromatosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Clinical Notes On Upper LimbДокумент10 страницClinical Notes On Upper LimbZllison Mae Teodoro Mangabat100% (1)
- MCQ EmbryoДокумент78 страницMCQ EmbryoAyesha Rajpoot100% (1)
- NUMS-MBBS Curriculum 1st Year 2020Документ108 страницNUMS-MBBS Curriculum 1st Year 2020nadia100% (1)
- Embryology - Updates and Highlights On Classic TopicsДокумент222 страницыEmbryology - Updates and Highlights On Classic TopicsIndera Vyas100% (1)
- Ist Year MbbsДокумент3 страницыIst Year MbbsJaved Gaba0% (1)
- A Text - Book of Histology: Descriptive and Practical. For the Use of StudentsОт EverandA Text - Book of Histology: Descriptive and Practical. For the Use of StudentsОценок пока нет
- Sweet Biochemistry: Remembering Structures, Cycles, and Pathways by MnemonicsОт EverandSweet Biochemistry: Remembering Structures, Cycles, and Pathways by MnemonicsОценок пока нет
- Histology Exam IV Review Part 2Документ26 страницHistology Exam IV Review Part 2ashdmb217Оценок пока нет
- Advances in Pathobiology and Management of Paget’s Disease of BoneОт EverandAdvances in Pathobiology and Management of Paget’s Disease of BoneSakamuri V. ReddyОценок пока нет
- Paget Disease of Bone, A Simple Guide to the Condition, Treatment and Related DiseasesОт EverandPaget Disease of Bone, A Simple Guide to the Condition, Treatment and Related DiseasesОценок пока нет
- Multiple Choice Questions in Anatomy and Neurobiology for UndergraduatesОт EverandMultiple Choice Questions in Anatomy and Neurobiology for UndergraduatesРейтинг: 4.5 из 5 звезд4.5/5 (5)
- Practical PhysiologyДокумент436 страницPractical Physiologyaastha212002100% (1)
- Embryology practice questions and answersДокумент33 страницыEmbryology practice questions and answersElizabeth Gabriel HoyaОценок пока нет
- Langman Medical Embryology Made Easy PDFДокумент19 страницLangman Medical Embryology Made Easy PDFAsma SaleemОценок пока нет
- Upper Limb MCQsДокумент12 страницUpper Limb MCQstafi66Оценок пока нет
- Von Gierke Disease, (Glycogen Storage Disorder I) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandVon Gierke Disease, (Glycogen Storage Disorder I) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Anatomy MCQДокумент3 страницыAnatomy MCQSrinivasa Rao BollaОценок пока нет
- Embryologypracticequestionswithanswers 140707144050 Phpapp02Документ120 страницEmbryologypracticequestionswithanswers 140707144050 Phpapp02oopie0% (1)
- Exercise on Upper Limb Bones and JointsДокумент2 страницыExercise on Upper Limb Bones and JointsLem A SharОценок пока нет
- Principles and Techniques for the Aspiring Surgeon: What Great Surgeons Do Without ThinkingОт EverandPrinciples and Techniques for the Aspiring Surgeon: What Great Surgeons Do Without ThinkingОценок пока нет
- Selected Topics in the History of Biochemistry. Personal Recollections. Part IIIОт EverandSelected Topics in the History of Biochemistry. Personal Recollections. Part IIIРейтинг: 1 из 5 звезд1/5 (1)
- Lowe Syndrome (Oculocerebrorenal syndrome) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandLowe Syndrome (Oculocerebrorenal syndrome) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- PhysiologyДокумент31 страницаPhysiologyraza20Оценок пока нет
- 01 Emryology The BeginningДокумент117 страниц01 Emryology The BeginningOsman Saidu SesayОценок пока нет
- Exam 1 NotesДокумент54 страницыExam 1 NotesAnonymous If9p21kwZKОценок пока нет
- Embryology of The Nervous SystemДокумент188 страницEmbryology of The Nervous SystemMOHAMMAD IBRAHIM AGORОценок пока нет
- Anatomy-1 PDFДокумент50 страницAnatomy-1 PDFSaransh Ghimire100% (1)
- Cell MCQДокумент3 страницыCell MCQkaran79Оценок пока нет
- MCQs & QUs On Fsirst Year First ComДокумент74 страницыMCQs & QUs On Fsirst Year First Commaisara10Оценок пока нет
- 100 Mcqs of AnatomyДокумент13 страниц100 Mcqs of Anatomydrusmansaleem100% (1)
- Bones of Upper and Lower Limbs - RevisionДокумент15 страницBones of Upper and Lower Limbs - RevisionChess Nuts100% (1)
- Embryology Viva ChartsДокумент29 страницEmbryology Viva ChartsAnusha SebastianОценок пока нет
- Histology-World! Histology Testbank-Nervous System 1Документ3 страницыHistology-World! Histology Testbank-Nervous System 1Kat JornadalОценок пока нет
- 4th To 8th WeekДокумент48 страниц4th To 8th WeekjefferyОценок пока нет
- 15 - Anatomy Mcqs HistologyДокумент14 страниц15 - Anatomy Mcqs HistologyNasan ShehadaОценок пока нет
- Medical AnatomyДокумент84 страницыMedical AnatomyhevenpapiyaОценок пока нет
- Important MCQ Colloction For PartДокумент154 страницыImportant MCQ Colloction For PartNazia Ali86% (7)
- Embryology BoneДокумент6 страницEmbryology BoneMarera DomnicОценок пока нет
- Histology-World! Histology Testbank-Cartilage 2aДокумент7 страницHistology-World! Histology Testbank-Cartilage 2aAya AhmedОценок пока нет
- Notes About BiologyДокумент81 страницаNotes About BiologyRichard CoffeyОценок пока нет
- Ganong Physiology 21eДокумент1 страницаGanong Physiology 21eprasun_v0% (1)
- Mitosis Vs MeiosisДокумент40 страницMitosis Vs Meiosiscmillica1176Оценок пока нет
- CLS Aipmt 18 19 XIII Bot Study Package 4 SET 1 Chapter 13Документ20 страницCLS Aipmt 18 19 XIII Bot Study Package 4 SET 1 Chapter 13Hemavarshini selvarajОценок пока нет
- Imbong v. OchoaДокумент187 страницImbong v. OchoaRostum AgapitoОценок пока нет
- Igcse Biology ReproductionДокумент92 страницыIgcse Biology ReproductionEric Chew100% (3)
- Chapter10 Lecture Ppt-Mader13-ModifiedДокумент33 страницыChapter10 Lecture Ppt-Mader13-Modifiedopa472308Оценок пока нет
- QUIZ#5 GeneticsДокумент6 страницQUIZ#5 GeneticsLouiza Angelina LayugОценок пока нет
- 9700 BIOLOGY: MARK SCHEME For The October/November 2015 SeriesДокумент8 страниц9700 BIOLOGY: MARK SCHEME For The October/November 2015 SeriesNerminОценок пока нет
- SIM LectureДокумент17 страницSIM LectureRaymond BunsoyОценок пока нет
- Midterm Examihation, I (Ovember: PUC RrorДокумент2 страницыMidterm Examihation, I (Ovember: PUC Rrorjäšħwâñtħ rОценок пока нет
- Cell Division and ReproductionДокумент4 страницыCell Division and Reproduction423003157Оценок пока нет
- Sri Chaitanya NEET Grand TestДокумент24 страницыSri Chaitanya NEET Grand TestAshutosh PathakОценок пока нет
- Biology Revision TrackerДокумент4 страницыBiology Revision TrackerHisham El KanayatiОценок пока нет
- Cell Cycle and Cell Division-AnswerДокумент5 страницCell Cycle and Cell Division-AnswerSWASTIKA MALOОценок пока нет
- Surat Pernyataan Kelas Bahasa Mandarin (Selasa)Документ1 страницаSurat Pernyataan Kelas Bahasa Mandarin (Selasa)Yanang Surya Putra HardyantoОценок пока нет
- Quiz Bee ReveiwerДокумент5 страницQuiz Bee ReveiwerIrish DomingoОценок пока нет
- Fertilisation Implantation NotesДокумент4 страницыFertilisation Implantation NotesShaun JinОценок пока нет
- Lost Sex - The Evolutionary Biology of Parthenogenesis - I. Schon, Et Al., (Springer, 2009) WWДокумент617 страницLost Sex - The Evolutionary Biology of Parthenogenesis - I. Schon, Et Al., (Springer, 2009) WWDeaconu Bianca100% (1)
- 0610 s03 QP 2 Model Answer FinalДокумент19 страниц0610 s03 QP 2 Model Answer FinalHema MohamedОценок пока нет
- Neet Xii Unit I DДокумент9 страницNeet Xii Unit I Dtechnicalmohit88Оценок пока нет
- Cornell Notes 10.1Документ1 страницаCornell Notes 10.1Morpho23Оценок пока нет
- Spirogyra Undergoes VegetativeДокумент3 страницыSpirogyra Undergoes VegetativeJoshua Prince100% (1)
- Bu2-3 Revision NotesДокумент26 страницBu2-3 Revision Notesveronica burlacuОценок пока нет
- Ds76-Meiosis Review Summative AssessmentДокумент6 страницDs76-Meiosis Review Summative Assessmentapi-110789702Оценок пока нет
- Genetic Engineering: How Genes Work and Novel ProductsДокумент25 страницGenetic Engineering: How Genes Work and Novel ProductsNikko SaiОценок пока нет
- Spatafora Etal 2017 Microbiology Spectrum 5-1-31Документ32 страницыSpatafora Etal 2017 Microbiology Spectrum 5-1-31Sam LenzОценок пока нет
- ICAR Animal Science Short NotesДокумент252 страницыICAR Animal Science Short NotesDr AMEER SUHAIL LOYOLITEОценок пока нет
- Biology 140 Lab 2 Cell DivisionДокумент11 страницBiology 140 Lab 2 Cell DivisionParidhi TiwariОценок пока нет
- Biology Today and Tomorrow With Physiology 5th Edition Starr Solutions Manual 1Документ9 страницBiology Today and Tomorrow With Physiology 5th Edition Starr Solutions Manual 1robert100% (31)
- Accelerated Plant Breeding, Volume 2 Vegetable Crops Springer, 2020Документ457 страницAccelerated Plant Breeding, Volume 2 Vegetable Crops Springer, 2020rommell AlvaradoОценок пока нет
- Bot Practical 10 Variation in Chromosome NumberДокумент4 страницыBot Practical 10 Variation in Chromosome NumberAbdulrehmanОценок пока нет