Академический Документы
Профессиональный Документы
Культура Документы
Adjuvant Analgesic
Загружено:
carl_hoongАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Adjuvant Analgesic
Загружено:
carl_hoongАвторское право:
Доступные форматы
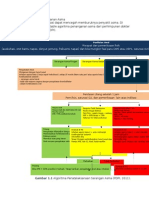
Adjuvant Analgesic Analgesik adjuvant (adjuvant analgesic) adalah obat yang mempunyai sifat analgesic lemah atau tidak
ada sifat analgesic sama sekali apabila diberikan sendiri, namun dapat meningkatkan efek agen analgesic lain. Obat ini dapat dikombinasikan dengan analgesic primer sesuai dengan sistem WHO Analgesic Ladder untuk mengurangi rasa nyeri. Analgesik adjuvant biasanya diberikan kepaada pasien yang menggunakan berbagai obat sehingga keputusan mengenai administrasi dan dosis obat harus dibuat dengan pemahaman yang jelas dari tahap penyakit dan tujuan perawatan. Sebagian analgesic adjuvant mempunyai efek yang bagus pada beberapa situasi nyeri tertentu sehingga diberikan nama multipurpose adjuvant analgesics (antidepressants, corticosteroids, 2-adrenergic agonists, neuroleptics). Ada juga yang spesifik pada kondisi nyeri tertentu saja, seperti pada nyeri neuropatik (anticonvulsants, local anesthetics, Nmethyl-D-aspartate receptor antagonists), nyeri tulang (calcitonin, bisphosphonates, radiopharmaceuticals), nyeri otot (muscle relaxants), atau nyeri pada obstruksi usus (octreotide, anticholinergics). Adjuvant Medications Multipurpose adjuvant analgesics Antidepressants Kedua jenis tertiary amines (amitriptyline, imipramine, doxepin, dan clomipramine) dan secondary amines (nortriptyline dan desipramine) bersifat analgesic. Namun tricyclic antidepressants jarang digunakan pada lanjut usia dan penderita dengan penyakit kronis karena efek samping obat yang sering terjadi seperti cardiotoxicity dan orthostatic hypotension. Obat ini tidak boleh diberikan kepada yang pernah mempunyai riwayat glaucoma, dan pada pasien dengn deficit kognitif. Obat secondary amine tricyclic antidepressants (desipramine dan nortriptyline) lebih kurang efek anti-kolinergik sehingga lebih aman daripada tertiary amines. Terdapat juga antidepresan lain yang memiliki efek analgesic. Namun penelitian yang mendukung penggunaan dan efektivitas masih kurang. Secara umum obat yang tidak tergolong tricyclic jauh labih aman dan lebih dapat ditoleransi daripada obat tricyclic. Maka obat bukan tricyclic dapat diberikan kepada yang tidak bisa toleransi atau tidak menunjukkan perbaikan setelah mengkonsumsi obat tricyclic. Dosis?
Corticosteroids Korticosteroid mempunyai sifat analgesic untuk banyak kodisi nyeri seperti nyeri kanker, nyeri tulang, nyeri neuropatik (kompresi pada struktur saraf), nyeri kepala (peningkatan tekanan intracranial), nyeri sendi (arthralgia) dan nyeri di dalam rongga abdomen. Obat yang sering dipakai adalah dexametason, prednisone dan metilprednisolone. Dalam praktek seharian, kortikosteroid bisa diberikan dalam regimen dosis tinggi atau dosis rendah. Regimen dosis tinggi (dexametason, 100 mg, diikuti 96 mg per hari) diberikan pada pasien dengan kompresi spinal kord atau nyeri berat yang tidak bisa dhilangkan dengan opioid saja. Regimen dosis tinggi dapat diturunkan dosisnya (tapering off) dalam waktu beberapa hari atau beberapa minggu setelah pasien menerima regimen analgesic yang berbeda (opioid atau terapi radiasi) Regimen dosis rendah (dexametason 2-4 mg sekali atau 2 kali sehari) bisa diberikan kepada pasien dengan kanker stadium lanjut yang mengeluh nyeri walaupun sudah diberikan opioid. Dosis kortikostroid harus dikurangi menjadi dosis efektif minimal. Kortikosteroid bisa menambah nafsu makan, mengurangi nausea, malaise dan meningkatkan kualitas hidup. Kortikosteroid juga bias menyebabkan ulkus peptikum. Namun dalam praktek sehari-hari, dokter hanya akan memberikan obat gastro-proteksi (proton pump inhibitor) kalau ada faktor risiko lain yang bisa menyebabkan ulkus peptikum seperti pemberian kombinasi obat NSAIDs dengan kortikosteroid. Alpha-2-Adrenergic Agonists Walaupun klonidin dan tizanidin adalah 2-adrenergic agonists dan dikatagorikan dalam nonspecific multipurpose adjuvant analgesics, namundata-data yang mendukung sangat terbatas dan obat-obat ini juga dikatakan memiliki efek samping seperti hipotensi dan somnolence. Klonidin bisa dimasukkan lewat oral, transdermal atau intraspinal. Namun secara oral klonidin masih kurang efeknya. Intraspinal klonidin lebih baik dalam mengurangi nyeri neuropatik terutama penderita yang intoleran terhadap opioid. Tizanidin adalah agen antispastik. Walaupun tizanidin lebih baik untuk sindrom nyeri myofascial dan nyeri kepala kronis, obat ini tetap digolongkan sebagai multipurpose adjuvant analgesic terutama karena jarangnya terjadinya hipotensi. Dosis?
Neuroleptics Generasi kedua (atypical) dari golongan olanzapine dikatakan dapat menurunkan intensitas nyeri dan pemakaian opioid dalam terapi nyeri. Selain itu, golongan genberasi kedua dari olanzapine akan dapat meningkatkan fungsi kognitif dan juga rasa cemas yang berlebihan, dalam beberapa manajemen nyeri yang diakibatkan oleh kanker.dari beberapa hasil pengamatan,dikatakan bahwa obat-obat yang tergolong neuroleptik, memiliki kemampuan analgetik yang sangat kurang. Mengingat dari efek sampingnya yang sangat banyak seperti tardive diskinesia, neuroleptic malignant sindom, maka golongan neuroleptik ini jarang digunakan sebagai analgesic adjuvant kecuali apabila adanya delirium dan agitasi pada pasien, dimana sifat analgetik yang dimiliki obat jenis neuroleptik ini lebih baik digunakan untuk menurunkan rasa nyeri, dan mengurangi penggunaan dari opioid, hal ini sangat membantu dalam mengatasi delirium. Neuroleptik juga seringkali menyebabkan peningkatan nafsu makan , dimana seringkali dapat membantu terutama pada pasien dengan kanker Analgetik adjuvant untuk nyeri neuropati Anticonvulsants Pada beberapa kasus didapatkan bahwa obat-obat yang tergolong antikonvulsan memiliki pengaruh yang baik dalam mengurangi nyeri neuropati. Obat generasi pertama kini sudah dilengkapi dengan jenis obat-obat antikonvulsi yang baru. Peran awal dari antikonvulsi dimulai dari pengenalan mekanisme kerja gabapentin . efektifitas kerja dari gabapentin mulai diperkenalkan pada beberapa kasus dengan nyeri neuropati yang bersifat non nmalignan, dan akhir-akhir ini gabapentin digunakan secara luas untuk menangani masalah nyeri neuropati, karena toleransi obat yang cukup baik, dan jarang menimbulkan interaksi obat. Gabapentin pada decade ini digunakan sebagai obat yang berperan sebagai lini pertama untuk mengobati nyeri neuropati yang disebabkan oleh penyebab yang sangat buruk, khususnya pada beberapa kondisi medis yang sangat berat. Obat ini harus dimulai dengan dosis 100-300 mg pada saat sebelum tidur dan dapat dinaikkan dosisnya setiap 3 hari. Dosis maksimal adalah 3600 mg per hari, tetapi kadang pasien seringkali mengatakan nyeri dapat dihilangkan dalam dosis yang besar. Percobaan dosis yang adekuat harus ditempuh selama 1sampai 2 minggu pada dosis maksimasl yang dapat dicapai. Adapun efek samping dari obat ini adlah There is good evidence that the anticonvulsant drugs are useful in the management of neuropathic pain. The older drugs, which have been used for decades, are now complemented by a rapidly increasing number of newer agents.
An expanding role for the anticonvulsants began with the introduction of gabapentin. The analgesic efficacy of gabapentin has been established in several types of nonmalignant neuropathic pain, and it is now widely used to treat cancer-related neuropathic pain. Due to its proven analgesic effect in several types of neuropathic pain, its good tolerability, and a rarity of drug-drug interactions, gabapentin is now recommended as a first-line agent for the treatment of neuropathic pain of diverse etiologies, especially in the medically ill population. It should be initiated at a daily dose of 100300 mg at bedtime and can be increased every 3 days. The usual maximum dose is 3,600 mg daily, but occasionally patients report benefits at higher doses. An adequate trial should include 12 weeks at the maximum-tolerated dose. The most common adverse effects are somnolence, dizziness, and unsteadiness. If titrated carefully, gabapentin is usually well tolerated, but in medically ill patients, somnolence can be a limiting factor. Among the older drugs, evidence of efficacy is best for carbamazepine and phenytoin, and both valproate and clonazepam have been widely used. The classic indication for carbamazepine is trigeminal neuralgia, and the use of phenytoin in cancer pain has been described. Due to their frequent side effects (sedation, dizziness, nausea, unsteadiness) and potential for drug-drug interactions, the use of these drugs has declined with the introduction of the newer analgesic anticonvulsants. In summary, selected anticonvulsant drugs may be effective for diverse types of neuropathic pain. Although earlier studies suggested that there might be a preferential role for these drugs in the treatment of neuropathic pain characterized by lancinating or paroxysmal components, this has not been confirmed in trials, and anticonvulsants are now routinely tried for any type of neuropathic pain. Among the anticonvulsants, gabapentin should be administered first due to its proven efficacy in different neuropathic pain syndromes and its good tolerability. Other newer anticonvulsants can be tried successively in patients who either has not responded satisfactorily to, have contraindications to, or have experienced adverse effects to gabapentin and other first-line adjuvant analgesics. Oral and Parenteral Local Anesthetics Local anesthetics have analgesic properties in neuropathic pain. Due to their potential for serious side effects, they have been conventionally positioned as second-line therapies, reserved for the treatment of severe intractable or crescendo neuropathic pain. A brief intravenous infusion of lidocaine has been shown to be effective in nonmalignant neuropathic pain. Despite negative results obtained in randomized controlled
trials in neuropathic cancer pain, clinical experience justifies considering its use. Brief infusions can be administered at varying doses within the range of 15 mg/kg infused over 2030 minutes. In the medically frail patient, it is prudent to start at the lower end of this range and provide repeated infusions at successively higher doses. A history of significant cardiac disease may relatively contraindicate this approach and should be evaluated before it is administered. Although prolonged relief of pain following a brief local anaesthetic infusion may occur, relief usually is transitory. If lidocaine appears to be effective but pain recurs, longterm systemic local anaesthetic therapy can be accomplished using an oral local anaesthetic, typically mexiletine. For rare patients with refractory neuropathic cancer pain who respond only to intravenous lidocaine infusion, long-term subcutaneous administration has been reported to provide sustained relief. The predictive value of a brief lidocaine infusion for the subsequent effectiveness of an oral local anaesthetic has not been established for pain. Given the limited number of supportive studies, mexiletine and other oral local anaesthetics are used as second-line agents for neuropathic pain that has not responded to trials of anticonvulsant or antidepressant analgesics. Controlled studies of mexiletine have demonstrated a relatively high rate of adverse effects (nausea, vomiting, tremor, dizziness, unsteadiness, and paresthesias) and discontinuation due to toxicity in almost one-half of patients N-methyl-D-Aspartate Receptor Blockers Interactions at the N-methyl-D-aspartate (NMDA) receptor are involved in the development of CNS changes that may underlie chronic pain and modulate opioid mechanisms, specifically tolerance. Antagonists at the NMDA receptor may offer another novel approach to the treatment of neuropathic pain in cancer patients. At the present time, there are four commercially available NMDA receptor antagonists in the U.S.the antitussive, dextromethorphan; the dissociative anesthetic, ketamine; the antiviral drug, amantadine; and a drug approved for the treatment of Alzheimers disease, memantine. Most of these drugs have been shown to have analgesic effects in nonmalignant neuropathic pain. Ketamine, administered by intravenous infusion or orally, is effective in relieving cancer pain and reducing opioid requirements. Clinicians who are experienced in the use of parenteral ketamine may, therefore, consider this option in patients with refractory pain. The side-effect profile of ketamine can be daunting, however, particularly in the medically frail.
Typically, ketamine therapy for pain has been initiated at low doses given subcutaneously or intravenously, such as a starting dose of 0.10.15 mg/kg by brief infusion or 0.10.15 mg/kg/hour by continuous infusion. The dose can be gradually escalated, with close monitoring of pain and side effects. For patients with refractory pain and limited life expectancies, long-term therapy can be maintained using continuous subcutaneous infusion or repeated subcutaneous injections. Oral administration also has been used, but experience is more limited with that approach. The ratio of doses needed to maintain effects when converting from parenteral to oral dosing is uncertain. Based on anecdotal data, some authors have suggested a 1:1 ratio, or an oral dose equivalent to 30%40% of the parenteral dose. It is also recommended to lower the opioid dose when starting ketamine. In patients undergoing surgery for bone malignancy, dextromethorphan was shown to augment analgesia and lessen analgesic requirements. Other studies and clinical experience have yielded mixed results. If prescribed, a prudent starting dose is 4560 mg/day, which can be gradually escalated until favourable effects occur, side effects supervene, or a conventional maximal dose of 1 g is achieved. Amantadine is a noncompetitive NMDA antagonist, and limited data suggest that it might reduce pain, allodynia, and hyperalgesia in chronic neuropathic pain and surgical neuropathic cancer pain. Currently available data are, however, too meagre to support recommending its use. Memantine is an NMDA antagonist recently marketed in the U.S. for the treatment of Alzheimers disease. Although it could theoretically possess some analgesic properties, controlled trials published so far have been disappointing. Other Systemic Drugs Baclofen Baclofen, an agonist at the gamma aminobutyric acid type B (GABAB) receptor, has established efficacy in trigeminal neuralgia and is often considered for a trial in any type of neuropathic pain. The effective dose range is very wide (20 mg/day to >200 mg/day orally), and titration from a low initial dose is necessary. The possibility of a serious withdrawal syndrome on abrupt discontinuation must be avoided by a gradual dose taper. Cannabinoids Cannabinoids have antinociceptive effects in animal models and oral delta-9tetrahydrocannabinol has been shown to be effective in cancer pain. Not all data are positive, and more studies on the various cannabinoids are needed.
Benzodiazepines The evidence for analgesic effects from benzodiazepines is limited and conflicting, and overall provides little support for the conclusion that these drugs are analgesic for neuropathic pain. Nonetheless, a trial of clonazepam can still be justified in refractory neuropathic pain on the basis of anecdotal experience, especially in the case of the common coexistence of pain and anxiety. Psychostimulants There is substantial evidence that psychostimulant drugs dextroamphetamine, methylphenidate, and caffeine have analgesic effects. Although pain is not considered a primary indication for these drugs, the potential for analgesic effects may influence the decision to recommend a trial. In cancer patients, methylphenidate can reduce opioidinduced somnolence, improve cognition, treat depression, and alleviate fatigue. Treatment is typically begun at 2.55 mg in the morning and again at midday, if necessary, to keep the patient alert during the day and not interfere with sleep at night. Doses are increased gradually until efficacy is established. Modafinil, a newer psychostimulant with a unique mechanism, is also used to reduce opioid-induced somnolence in cancer patients. It is usually started at 100 mg/day and then increased. Although there are currently no scientific data supporting its use to reduce opioid-induced sedation, atomoxetine, a selective norepinephrine reuptake inhibitor approved for the treatment of attentiondeficit/hyperactivity disorder, has been used successfully in clinical practice. The analgesic properties of modafinil and atomoxetine have not yet been studied. Topical Analgesics Topical drugs are applied directly to the skin, as a patch, gel, or cream and have their pharmacologic activity directly under the skin site without any significant amount of drug entering the blood stream. Thus, true topical drugs should not produce any systemic side effects, that is, side effects caused by the drug's effects throughout the body. Currently, only one topical drug has an FDA approved indication for pain treatment -- a topical lidocaine patch (Lidoderm) -- for the treatment of postherpetic neuralgia. This patch can be tried for many types of nerve pain. A widely used topical pain reliever is capsaicin, which is available as an over-thecounter cream. There have been some studies that show pain relief with capsaicin and others that do not. This drug is being used to treat nerve pain and arthritis pain. Capsaicin is the ingredient in chili pepper that produces its pungent taste. When applied topically, it causes
the depolarization of the nociceptors and release of substance P. Regular use eventually leads to depletion of substance P from the terminals of afferent C-fibers, potentially leading to decreased pain perception. In cancer patients, capsaicin cream has been shown to be effective in reducing neuropathic postsurgical pain (such as postmastectomy pain). There are two commercially available concentrations (0.025% and 0.075%), and an initial trial usually involves application of the higher concentration three to four times daily. A trial of several weeks is needed to adequately judge effects. Many patients experience severe burning pain after the first applications (related to the initial release of substance P), which usually decreases gradually over a few days if the cream is applied regularly. Some patients tolerate the lower concentration cream better, or tolerate application only if preceded by a topical local anesthetic or ingestion of an analgesic. Adjuvant analgesics specific for bone pain Calcitonin Calcitonin may have several pain-related indications in the palliative care setting, including pain from bone metastasis. The most frequent routes of administration are subcutaneous and intranasal. If subcutaneous boluses are used, they should be preceded by skin testing with 1 IU to screen for hypersensitivity reactions, especially in patients with a history of reactions to salmon or seafood. The optimal dose is not known. A trial may be initiated at a relatively low dose, which then can be gradually increased if tolerated. The intranasal formulation avoids the need for subcutaneous injections, facilitating the use of this drug in home care. It is administered once daily, with an initial dose of 200 IU in one nostril, alternating nostrils every day. There are no data from which to judge the dose-response relationship for pain; escalation of the dose once or twice is reasonable if the first response is unfavorable. Apart from infrequent hypersensitivity reactions associated with subcutaneous injections, the main side effect is nausea. The likelihood and severity of this effect may be reduced by gradual escalation from a low starting dose. It usually subsides after a few days and is less frequent with the intranasal form. Periodic monitoring of calcium and phosphorus is prudent during treatment. Bisphosphonates Bisphosphonates are analogues of inorganic pyrophosphate that inhibit osteoclast activity and, consequently, reduce bone resorption in a variety of illnesses. The analgesic efficacy of these compounds, particularly pamidronate, has been well established.
Pamidronate has been extensively studied in populations with bone metastases. Its analgesic effects have been shown in breast cancer and multiple myeloma. The dose usually recommended is 6090 mg i.v. (infused over 24 hours) every 34 weeks. There are dosedependent effects, and a poor response at 60 mg can be followed by a trial of 90 or 120 mg. The reduction of skeletal morbidity (pathological fractures, need for bone radiation or surgery, spinal cord compression, hypercalcemia) described with the administration of pamidronate in multiple myeloma and breast cancer patients is another incentive to use it as an adjuvant. Adverse effects, including hypocalcemia and a flu-like syndrome, are dose related and typically transitory. Nephrotoxicity occurs rarely, usually following relatively rapid infusions, and typically is transitory; the drug can be used in those with impaired renal function. Zoledronic acid is a new bisphosphonate that is approximately two to three times more potent than pamidronate. It has been shown to reduce pain and the occurrence of skeletal-related events in breast cancer, prostate cancer, and multiple myeloma, as well as a variety of solid tumors, including lung cancer. It is effective in both osteoblastic and osteolytic lesions. It is as effective as pamidronate, and its use is more convenient, as it can be infused safely over 15 minutes at a dose of 4 mg every 3 weeks. The side effects are similar to those encountered with pamidronate, and the dose does not have to be adjusted in patients with mild-to-moderate renal failure. Radiopharmaceuticals Radionuclides that are absorbed at areas of high bone turnover have been evaluated as potential therapies for metastatic bone disease. Strontium-89 and samarium-153, which are commercially available in the U.S., may be effective as monotherapy or as an adjunct to conventional radiation therapy. Given the potential for myelosuppression associated with their use, these drugs usually are considered when pain is refractory to other modalities. Adjuvant analgesics used for musculoskeletal pain The so-called muscle relaxants include drugs in a variety of classes, including antihistamines (e.g., orphenadrine), tricyclic compounds structurally similar to the tricyclic antidepressants (e.g., cyclobenzaprine), and others (e.g., carisoprodol, metaxalone, methocarbamol). Although these drugs can relieve musculoskeletal pain, these effects may not be specific, and there is no evidence that they relax skeletal muscle in the clinical setting. Although they have been shown to reduce musculoskeletal pains, their risk:benefit ratio relative to the NSAIDs
or opioids is unknown. The most common adverse effect is sedation, which can be additive to other centrally acting drugs, including opioids. Treatment should be initiated with relatively low initial doses. The potential for abstinence, as well as abuse by predisposed patients, warrants caution when discontinuing therapy or administering these drugs to those with a substance abuse history. If a muscle spasm is present and is believed to be responsible for the pain, drugs with established effects on skeletal muscle should be tried in place of the muscle relaxants. These include diazepam (Valium) or other benzodiazepines, the 2-adrenergic agonist tizanidine or the GABAB agonist baclofen. Injections of botulinum toxin can be considered for refractory musculoskeletal pain related to muscle spasms, including those occurring after radiation therapy. Adjuvant analgesics used for pain caused by bowel obstruction The management of symptoms associated with malignant bowel obstruction may be challenging. If surgical decompression is not feasible, the need to control pain and other obstructive symptoms, including distension, nausea, and vomiting, becomes paramount. The use of opioids may be problematic due to dose-limiting toxicity (including gastrointestinal toxicity) or the intensity of breakthrough pain. Anecdotal reports suggest that anticholinergic drugs, the somatostatin analogue octreotide, and corticosteroids may be useful adjuvant analgesics in this setting. The use of these drugs may also ameliorate nonpainful symptoms and minimize the number of patients who must be considered for chronic drainage using nasogastric percutaneous catheters. Octreotide The somatostatin analogue octreotide inhibits the secretion of gastric, pancreatic, and intestinal secretions, and reduces gastrointestinal motility. These actions, which can occur more rapidly than similar effects produced by anticholinergic drugs, probably underlie the analgesia and other favorable outcomes that have been reported in case series and one randomized trial in patients with bowel obstruction. Octreotide has a good safety profile and its considerable expense may be offset in some situations by the avoidance of gastrointestinal drainage procedures.
Anticholinergic Drugs Anticholinergic drugs could theoretically relieve the symptoms of bowel obstruction by reducing propulsive and nonpropulsive gut motility and decreasing intraluminal secretions. Two small series demonstrated that a continuous infusion of hyoscine butylbromide (scopolamine) at a dose of 60 mg daily can control symptoms from nonoperable malignant bowel obstruction, including pain. Glycopyrrolate has a pharmacological profile similar to that of hyoscine butylbromide, but may produce fewer side effects because of a relatively low penetration through the blood-brain barrier; this drug, however, has not been systematically evaluated in a population with symptomatic bowel obstruction. Corticosteroids The symptoms associated with bowel obstruction may improve with corticosteroid therapy. The mode of action is unclear, and the most effective drug, dose, and dosing regimen are unknown. Dexamethasone has been used in a dose range of 860 mg/day, and methylprednisolone has been administered in a dose range of 3050 mg/day. The potential for complications during long-term therapy, including an increased risk of bowel perforation, may limit this approach to patients with short life expectancies.
Other Adjuvant Analgesics Baclofen is on the market as a muscle relaxant and is used to treat nerve pain syndromes. There is very good evidence that it works in trigeminal neuralgia. Drugs that block a specific receptor involved in the experience of pain, the N-methylD-aspartate (NMDA) receptor, may also be analgesic in nerve pain. These include dextromethorphan (the cough suppressant, but at higher doses than those needed to block cough), ketamine (an anesthetic), and amantadine. There are many drugs that are called "muscle relaxants" and are used to treat minor musculoskeletal pains. These include carisoprodol (Soma), cyclobenzaprine (Flexeril), metaxolone (Skelaxin), and others. These drugs do not actually relax skeletal muscle, but they can relieve pain, and they are commonly used.
Вам также может понравиться
- Interaksi Obat Tramadol Dengan OndancetronДокумент1 страницаInteraksi Obat Tramadol Dengan OndancetronNyoman Gina Henny KristiantiОценок пока нет
- Parkinson terapi tatalaksanaДокумент4 страницыParkinson terapi tatalaksanaMuhammad ArdiansyahОценок пока нет
- Obat Relaksan OtotДокумент20 страницObat Relaksan Ototmeufe0% (1)
- Penatalaksanaan KomprehensifДокумент4 страницыPenatalaksanaan KomprehensifFaradila Isnaini100% (2)
- Konsensus Dispepsia TerbaruДокумент5 страницKonsensus Dispepsia Terbarueva taulabiОценок пока нет
- Pemeriksaan Klonus Dan Sindrom NyeriДокумент4 страницыPemeriksaan Klonus Dan Sindrom NyeriDaan AnisaОценок пока нет
- Sistem ekstrapiramidal dan krisis okulogirikДокумент4 страницыSistem ekstrapiramidal dan krisis okulogirikRizqi Amir100% (2)
- Analisa Resep AsmaДокумент21 страницаAnalisa Resep AsmaRirin Frisilia100% (1)
- KetorolacДокумент25 страницKetorolacSurya Nirmala DewiОценок пока нет
- AnsiolitikДокумент7 страницAnsiolitikAlvi MuldaniОценок пока нет
- Farmakokinetik KortikosteroidДокумент9 страницFarmakokinetik KortikosteroidnadyaratuafОценок пока нет
- Kasus II Demam TifoidДокумент4 страницыKasus II Demam TifoidwulansucinОценок пока нет
- Obat Pelumpuh Otot (Anestesi)Документ15 страницObat Pelumpuh Otot (Anestesi)Mala100% (1)
- Amino LebanДокумент7 страницAmino LebanKikiiОценок пока нет
- 06 - 224diagnosis Dan Tatalaksana Meningitis BakterialisДокумент5 страниц06 - 224diagnosis Dan Tatalaksana Meningitis BakterialisZeewy DeiruyoОценок пока нет
- Perhitungan DosisДокумент12 страницPerhitungan Dosisphia29100% (1)
- AtracuriumДокумент11 страницAtracuriumPutrii JoanОценок пока нет
- LAPORAN PARKINSONДокумент16 страницLAPORAN PARKINSON89ILAОценок пока нет
- CiprofloxacinДокумент2 страницыCiprofloxacinStacy Harper100% (1)
- OBAT-OBAT FARMAKOTERAPIДокумент15 страницOBAT-OBAT FARMAKOTERAPIFedri Baysar100% (1)
- Presus Obs - KejangДокумент22 страницыPresus Obs - Kejangadha_noer01Оценок пока нет
- BAB1Документ13 страницBAB1Nurhanani RidzuanОценок пока нет
- 5 Pilar Penanganan DiareДокумент1 страница5 Pilar Penanganan Diarefani melindaОценок пока нет
- Penatalaksanaan ParkinsonДокумент3 страницыPenatalaksanaan ParkinsonDarulisman SamadОценок пока нет
- Algoritma Penanganan AsmaДокумент2 страницыAlgoritma Penanganan Asmaanaesaburi sahid100% (1)
- FENTANYLДокумент4 страницыFENTANYLxerwane100% (2)
- H2 Antagonis dan AntasidaДокумент4 страницыH2 Antagonis dan AntasidaHerdiko Shalatin100% (1)
- Bismuth SubsalisilatДокумент2 страницыBismuth SubsalisilatRahma Agustina100% (1)
- Analgetik Opioid Dan Non OpioidДокумент26 страницAnalgetik Opioid Dan Non OpioidBarri Ratlisyah AliОценок пока нет
- Edukasi AsmaДокумент2 страницыEdukasi AsmaR Anrico MuhammadОценок пока нет
- Anamnesis Kasus PneumoniaДокумент4 страницыAnamnesis Kasus PneumoniaMalvino GiovanniОценок пока нет
- CME 234-Ensefalopati Hepatikum Minimal PDFДокумент5 страницCME 234-Ensefalopati Hepatikum Minimal PDFlaily nurhayatiОценок пока нет
- Diagnosa Dan Penatalaksanaan LaringitisДокумент6 страницDiagnosa Dan Penatalaksanaan LaringitisMuhamad Ibnu Sina100% (1)
- Farmakokinetik Dan Farmakodinamik MeropenemДокумент7 страницFarmakokinetik Dan Farmakodinamik MeropenemMaria FernandezОценок пока нет
- Terapi BPPVДокумент11 страницTerapi BPPVErvandy Rangganata100% (1)
- AlprazolamДокумент2 страницыAlprazolamtugba1234Оценок пока нет
- AmpleДокумент9 страницAmplereniprativiОценок пока нет
- Asm Tranex Dan Vit KДокумент8 страницAsm Tranex Dan Vit KKumara JpОценок пока нет
- Dosis ManitolДокумент3 страницыDosis Manitolmutya yulindaОценок пока нет
- Penanganan Adiksi Golongan BenzodiazepinДокумент13 страницPenanganan Adiksi Golongan BenzodiazepinQariahMaulidiahAminОценок пока нет
- Patofisiologi Mual MuntahДокумент2 страницыPatofisiologi Mual MuntahIs May Niyar100% (1)
- XeroftalmiaДокумент25 страницXeroftalmiaamaliaturrahmah100% (1)
- TIVAДокумент28 страницTIVAZahra PuspitaОценок пока нет
- NeurologiДокумент102 страницыNeurologichindysihombingОценок пока нет
- Keracunan Adjuvan Analgesik, Psikotropik Dan Hipnotik - SedatifДокумент39 страницKeracunan Adjuvan Analgesik, Psikotropik Dan Hipnotik - SedatifRizki Dyah RahmawatiОценок пока нет
- Obat Analgetik Berdasarkan Ilmu FarmakologiДокумент16 страницObat Analgetik Berdasarkan Ilmu FarmakologiAdriana GarciaОценок пока нет
- Skenari 1 FARMASIДокумент1 страницаSkenari 1 FARMASISeptya AyuОценок пока нет
- Dika-Manajemen Nyeri Dalam Perawatan PaliatifДокумент9 страницDika-Manajemen Nyeri Dalam Perawatan PaliatifJuvander IvanОценок пока нет
- Farmakologi Manajemen NyeriДокумент3 страницыFarmakologi Manajemen NyeriTita Puspita DewiОценок пока нет
- Kombinasi Tramadol Paracetamol Analgesik MultimodalДокумент5 страницKombinasi Tramadol Paracetamol Analgesik MultimodalHayudhiaОценок пока нет
- Analgesik, Antidepresan, dan OAINS dalam Pengobatan NyeriДокумент7 страницAnalgesik, Antidepresan, dan OAINS dalam Pengobatan NyeriDaffa AdhitamaОценок пока нет
- Praktikum Farmakol AnalgetikaДокумент19 страницPraktikum Farmakol AnalgetikaDian NovitaОценок пока нет
- FarmasiДокумент9 страницFarmasiMADEDESIMARIANIОценок пока нет
- Tatalaksana NyeriДокумент25 страницTatalaksana NyeriayudevitaОценок пока нет
- AnalgetikДокумент17 страницAnalgetikRefta Sekar DeviОценок пока нет
- Algoritma Dan Analgetik Akut AbdomenДокумент15 страницAlgoritma Dan Analgetik Akut AbdomenLibert ValentineОценок пока нет
- Makalah Analgesik PeriferДокумент12 страницMakalah Analgesik PeriferFaedah Karim FM'sОценок пока нет
- Contoh Makalah AnalgetikДокумент10 страницContoh Makalah AnalgetikKettyОценок пока нет
- Materi Panduan Manajemen Nyeri 2Документ12 страницMateri Panduan Manajemen Nyeri 2Tika RenwarinОценок пока нет
- Fisiologi Sirkulasi ParuДокумент4 страницыFisiologi Sirkulasi Parucarl_hoongОценок пока нет
- Trauma Kepala Ringan Anak DidikДокумент6 страницTrauma Kepala Ringan Anak Didikcarl_hoongОценок пока нет
- Lapsus Wangaya AdikДокумент23 страницыLapsus Wangaya Adikcarl_hoongОценок пока нет
- Kasus Gizi BurukДокумент10 страницKasus Gizi Burukcarl_hoongОценок пока нет