Академический Документы
Профессиональный Документы
Культура Документы
NCP For Schizo
Загружено:
Richelene Mae CanjaИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
NCP For Schizo
Загружено:
Richelene Mae CanjaАвторское право:
Доступные форматы
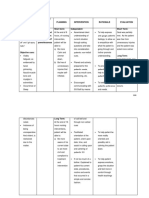
Nursing Care Plan for Schizophrenic Patient
Assessment Subjective: Ako si chong pogi! Marami akong girlpren
Diagnosis Disturbed Thought Process related to Delusion of grandeur
Planning Short Term Goal:
Intervention
Evaluation Short Term Goal Evaluation: After 4 hours of nursepatient interaction and intervention patient is able to respond to environmental stimuli appropriately.
Independent: Within 4 hours of nurse patient interaction and 1. 1. Assess the patient's intervention patient will ability to carry out the be able to respond activities of daily appropriately to living, paying special environmental stimuli attention to his nutritional status. 2. 3. 2. Monitor his weight if Long Term Goal: he isn't eating. If he thinks that his food is After 8 weeks of nursepoisoned, allow him to patient interaction and fix his own food when intervention patient will possible, or offer him be able to know reality foods in closed and will have lesser containers that he can delusion of grandeur. open. If you give liquid medication in a unitdose container, allow the patient to open the container. 4. 5. 3. Maintain a safe environment, minimizing stimuli. 6. 7. 4.Administer medication as ordered
Objective: Distractibility Egocentric Inaccurate Interpretation Memory Deficit
Analysis: Schizophrenia is a mental illness in which patients experience symptoms such as delusions, (mistaken beliefs) hallucinations, and disorganized behavior. It is the change in the amount of patterning of incoming stimuli accompanied by a diminished exaggerated, distorted or impaired response to such stimuli.
Long Term Goal: After 7 weeks of nursepatient interaction and intervention patient is able to recognize reality and has lesser delusion of grandeur.
to decrease symptoms and anxiety. Use physical restraints according to your facility's policy to ensure the patient's safety and that of others. 8. 9. 5. Adopt an accepting and consistent approach with the patient. Don't avoid or overwhelm him. Keep in mind that short, repeated contacts are best until trust has been established. 10. 6. Reward positive behavior to help the patient improve his level of functioning. 7. Engage the patient in reality-oriented activities that involve human contact: inpatient social skills training groups, outpatient day care, and sheltered workshops. 8. Provide reality-based
explanations for distorted body images or hypochondriacal complaints. Clarify private language, autistic inventions, or neologisms, explaining to the patient that what he says isn't understood by others. If necessary, set limits on inappropriate behavior. 9. If the patient is hallucinating, explore the content of the hallucinations. If he has auditory hallucinations, determine if they're command hallucinations that place the patient or others at risk. Tell the patient you don't hear the voices but you know they're real to him. Avoid arguing about the hallucinations; if possible, change the subject. 10. Don't tease or joke with the patient.
Choose words and phrases that are unambiguous and clearly understood. For instance, a patient who's told, That procedure will be done on the floor, may become frightened, thinking he is being told to lie down on the floor. 11. Don't touch the patient without telling him first exactly what you're going to do. For example, clearly explain to him, I'm going to put this cuff on your arm so I can take your blood pressure. If necessary, postpone procedures that require physical contact with facility personnel until the patient is less suspicious or agitated. 12. Remember, institutionalization may produce new symptoms and handicaps in the patient that aren't part
of his diagnosed illness, so evaluate symptoms carefully. 13. Mobilize community resources to provide a support system for the patient and reduce his vulnerability to stress. Ongoing support is essential to his mastery of social skills. 14.Encourage compliance with the medication regimen to prevent relapse. Also monitor the patient carefully for adverse effects of drug therapy, including drug-induced parkinsonism, acute dystonia, akathisia, tardive dyskinesia, and malignant neuroleptic syndrome. Make sure you document and report such effects promptly.
Вам также может понравиться
- Care Plan For SchizophreniaДокумент6 страницCare Plan For SchizophreniaAllea Likestolaugh Brown100% (2)
- NCP PsychosisДокумент3 страницыNCP Psychosisinagasi100% (7)
- NCP BSN 3rd Yr Psychiatric WardДокумент9 страницNCP BSN 3rd Yr Psychiatric WardMary Margarett BoadoОценок пока нет
- Schizophrenia Care Plan RNДокумент8 страницSchizophrenia Care Plan RNlisa75% (4)
- Schizophrenia Symptoms, Nursing Diagnoses, Interventions and OutcomesДокумент9 страницSchizophrenia Symptoms, Nursing Diagnoses, Interventions and Outcomesاسيرالاحزان100% (1)
- A NCP SchizoДокумент5 страницA NCP SchizoJoseph Wilson Macasa50% (4)
- 4 NCP SchizophreniaДокумент9 страниц4 NCP SchizophreniaHazel Banday100% (4)
- NursingDx ImpairedVerbalComm SchizophreniaДокумент8 страницNursingDx ImpairedVerbalComm Schizophreniajmanipon_1100% (1)
- Schizophrenia NCPДокумент4 страницыSchizophrenia NCPGladys Barcelona91% (55)
- NCPДокумент1 страницаNCPNneka Andrea Datiles0% (2)
- Nursing Care Plan - SchizophreniaДокумент3 страницыNursing Care Plan - SchizophreniaJasmin Jacob76% (46)
- Paranoid Schizophrenia NCPДокумент8 страницParanoid Schizophrenia NCPCherubim Lei DC Flores67% (3)
- Nursing Care Plan - SchizophreniaДокумент2 страницыNursing Care Plan - SchizophreniaJasmin Jacob80% (5)
- Nursing Care Plans SchizДокумент27 страницNursing Care Plans SchizClariza Castro76% (17)
- NCP Psyche2Документ6 страницNCP Psyche2Nica RTОценок пока нет
- Schizophrenia NCPДокумент2 страницыSchizophrenia NCPNicole cuencos100% (2)
- Disturbed Thought ProcessesДокумент2 страницыDisturbed Thought ProcessesJason Avellano100% (3)
- Nursing Care PlanДокумент2 страницыNursing Care PlanJewelyn Bronda100% (2)
- Nursing Patient Interaction HistoryДокумент7 страницNursing Patient Interaction Historynoronisa talusobОценок пока нет
- NCP Disturbed Thought ProcessДокумент2 страницыNCP Disturbed Thought ProcessCesara Lacorte80% (5)
- NCP DisturbedThoughtProcessesДокумент1 страницаNCP DisturbedThoughtProcessesJoan KarlaОценок пока нет
- Nursing Care Plan for Improving Social InteractionДокумент3 страницыNursing Care Plan for Improving Social InteractionMae Ceaesar50% (2)
- Improve Memory and Reduce Frustration with Targeted Nursing InterventionsДокумент1 страницаImprove Memory and Reduce Frustration with Targeted Nursing InterventionsHarmony Grace0% (1)
- NCPДокумент8 страницNCPTrixia Diaz67% (3)
- NCP PsychДокумент2 страницыNCP PsychJray Inocencio50% (4)
- NCP Assessment Diagnosis Planning Short-Term GoalДокумент4 страницыNCP Assessment Diagnosis Planning Short-Term GoalJessieRamosAnicetoОценок пока нет
- Defensive coping nursing diagnosisДокумент3 страницыDefensive coping nursing diagnosisRoch Oconer100% (1)
- SCHIZOPHRENIA Nursing Care PlanДокумент1 страницаSCHIZOPHRENIA Nursing Care Planrinkai130% (1)
- NCP FinalДокумент22 страницыNCP FinalAlmira Ahamad100% (1)
- Nursing Care Plan 1 Risk For Violence, Self DirectedДокумент9 страницNursing Care Plan 1 Risk For Violence, Self Directeddbryant010193% (14)
- Xi. Nursing Care PlansДокумент4 страницыXi. Nursing Care PlansNic Ji100% (1)
- Submitted By: Charisa S. Simbajon BSN IvДокумент8 страницSubmitted By: Charisa S. Simbajon BSN IvCharisa Simbajon100% (1)
- NCP SchizДокумент12 страницNCP SchizKristine Reyes - MerleОценок пока нет
- Social isolation nursing diagnosis schizophreniaДокумент3 страницыSocial isolation nursing diagnosis schizophreniaChuck Smith100% (11)
- ND - Disturbed Thought ProcessДокумент2 страницыND - Disturbed Thought ProcessHu DawiОценок пока нет
- NCP (Psychiatric)Документ6 страницNCP (Psychiatric)Erl Joy Montaño Cañete100% (1)
- Nursing Care Plan PsychДокумент12 страницNursing Care Plan Psychblarehead88% (24)
- NCP DEPRESSION DIAGNOSISДокумент4 страницыNCP DEPRESSION DIAGNOSIS'SheenMarkReal'Оценок пока нет
- Improving Social Interaction in a Child with Impaired Social SkillsДокумент2 страницыImproving Social Interaction in a Child with Impaired Social Skills4kscribd80% (5)
- Nursing Care Plan For A Patient With SchizophreniaДокумент14 страницNursing Care Plan For A Patient With SchizophreniaMary Luz De GuzmanОценок пока нет
- Cues Objectives Nursing Interventions Rationale Evaluation Subjective: StoДокумент3 страницыCues Objectives Nursing Interventions Rationale Evaluation Subjective: StoSuzette Rae TateОценок пока нет
- Assessing Auditory Hallucinations in SchizophreniaДокумент3 страницыAssessing Auditory Hallucinations in SchizophreniaJames Lozano83% (6)
- NCP SchizophreniaДокумент7 страницNCP SchizophreniaSteffi Raye Madrid50% (2)
- Care Plan 27Документ10 страницCare Plan 27Oroma TobiasОценок пока нет
- N C PДокумент3 страницыN C PTrixia Diaz100% (1)
- Crisis Intervention: Psychiatric Nursing Nursing Care PlanДокумент13 страницCrisis Intervention: Psychiatric Nursing Nursing Care PlanKatherine 'Chingboo' Leonico Laud100% (4)
- Impaired Social Interaction Related To Fear of Being Scrutinized and Embarrassed by OthersДокумент9 страницImpaired Social Interaction Related To Fear of Being Scrutinized and Embarrassed by Othersnathalie cotengОценок пока нет
- NCP Impaired Social InteractionДокумент2 страницыNCP Impaired Social Interactionzenzamora87% (31)
- Jean Pearl R. Caoili Bsn3 NCB Diagnosis: Paranoid Schizophrenia Psychiatric Nursing Care Plan Assessment Explanation of The Problem Goals/ Objectives Interventions Rationale EvaluationДокумент9 страницJean Pearl R. Caoili Bsn3 NCB Diagnosis: Paranoid Schizophrenia Psychiatric Nursing Care Plan Assessment Explanation of The Problem Goals/ Objectives Interventions Rationale Evaluationpj casteОценок пока нет
- Psychiatric-Mental Health Nursing Sample QuestionsДокумент8 страницPsychiatric-Mental Health Nursing Sample QuestionsBenedict AlvarezОценок пока нет
- NCP For SchizoДокумент6 страницNCP For SchizoGILIANNE MARIE JIMENEAОценок пока нет
- Aggressive Behaviors - ExtendedДокумент7 страницAggressive Behaviors - ExtendedTeresa SilvaОценок пока нет
- Management of AgitationДокумент8 страницManagement of AgitationMahmoud Ahmed MahmoudОценок пока нет
- Nursing Care Plans For Delusional DisorderДокумент4 страницыNursing Care Plans For Delusional Disorderkirill61195% (22)
- Amos 3021finalevaluationДокумент14 страницAmos 3021finalevaluationapi-271045768Оценок пока нет
- IM Communication Skills Teaching-Sem 8Документ13 страницIM Communication Skills Teaching-Sem 8Cynthia SooОценок пока нет
- Hawken, 2005, Strategies For Dealing With The Challeging Patient (Paper) PDFДокумент4 страницыHawken, 2005, Strategies For Dealing With The Challeging Patient (Paper) PDFAlice AugustinОценок пока нет
- Nursing Documentation Using the DAR Method for Patient with FeverДокумент15 страницNursing Documentation Using the DAR Method for Patient with FeverSergio Rivas100% (3)
- Module 3 - Responding EffectivelyДокумент2 страницыModule 3 - Responding EffectivelyjessafesalazarОценок пока нет
- Goal:: Nursing Interventions For SchizophreniaДокумент3 страницыGoal:: Nursing Interventions For SchizophreniaKrystel Joy AuroОценок пока нет
- Secure DownloadДокумент69 страницSecure DownloadRichelene Mae CanjaОценок пока нет
- Anti Discrimination LawДокумент5 страницAnti Discrimination LawRichelene Mae CanjaОценок пока нет
- Power Point in PsychoДокумент6 страницPower Point in PsychoRichelene Mae CanjaОценок пока нет
- Fluid, Electrolyte, and Acid-Base BalanceДокумент42 страницыFluid, Electrolyte, and Acid-Base BalanceRichelene Mae CanjaОценок пока нет
- Final Hum3Документ2 страницыFinal Hum3Richelene Mae CanjaОценок пока нет
- First Days of School WongДокумент428 страницFirst Days of School WongAustin Clark100% (4)
- HMEC5333 Learning KitДокумент34 страницыHMEC5333 Learning KitTutor EvonОценок пока нет
- Revised Bloom's Taxonomy: Three Learning DomainsДокумент34 страницыRevised Bloom's Taxonomy: Three Learning Domainsitacademy100% (1)
- Sexual Disorders Across Life SpanДокумент53 страницыSexual Disorders Across Life SpanCJ AngelesОценок пока нет
- Paul BloomДокумент4 страницыPaul BloomKadir KAYAОценок пока нет
- Workbook 99 Bad Boy TraitsДокумент67 страницWorkbook 99 Bad Boy TraitsAyoubELBakiriОценок пока нет
- PersonalDevelopment - Q1 - Mod 6 - 7 - Emotional-Intelligence - v5Документ33 страницыPersonalDevelopment - Q1 - Mod 6 - 7 - Emotional-Intelligence - v5KryssssОценок пока нет
- SG Cowen's Rigorous Candidate Recruitment ProcessДокумент15 страницSG Cowen's Rigorous Candidate Recruitment ProcessKardenОценок пока нет
- Community HelpersДокумент3 страницыCommunity HelperskaylaroliverОценок пока нет
- Brain Function Assessment and Neurotherapy for Sexual AbuseДокумент23 страницыBrain Function Assessment and Neurotherapy for Sexual AbuseneuropsicojcОценок пока нет
- Stressors Among SHS TeachersДокумент76 страницStressors Among SHS TeachersDexter FernandezОценок пока нет
- Nursing Leadership DIRECTING Quizlet PrintДокумент6 страницNursing Leadership DIRECTING Quizlet PrintNiña Mae QuitorasОценок пока нет
- Hypothesis Is A Tentative Explanation That Accounts For A Set of Facts and Can Be Tested by Further InvestigationДокумент9 страницHypothesis Is A Tentative Explanation That Accounts For A Set of Facts and Can Be Tested by Further InvestigationScreaMonster PicОценок пока нет
- The Impact of Korean Drama Now A Days Social ResearchДокумент6 страницThe Impact of Korean Drama Now A Days Social ResearchAngel AbalosОценок пока нет
- A Unified Theory of Development - A Dialectic Integration of Nature and NurtureДокумент18 страницA Unified Theory of Development - A Dialectic Integration of Nature and NurtureDaniel MontalvoОценок пока нет
- Cidam 1st Half PR1Документ4 страницыCidam 1st Half PR1Feed Back ParОценок пока нет
- MBTIДокумент2 страницыMBTIUma Arby100% (1)
- Teens Brain Under ConstructionДокумент12 страницTeens Brain Under ConstructionDoru-Mihai Barna100% (2)
- Applying Empowerment Approach in Community DevelopmentДокумент16 страницApplying Empowerment Approach in Community DevelopmentMaria Rose BadayosОценок пока нет
- Omde 601Документ2 страницыOmde 601api-241955651Оценок пока нет
- Motor Control Motor LearningДокумент56 страницMotor Control Motor LearningJune EpeОценок пока нет
- Competency DictionaryДокумент22 страницыCompetency Dictionarynaveednoor28Оценок пока нет
- Chapter 01 ArtsДокумент16 страницChapter 01 ArtsCarmela Ayessa PiguerraОценок пока нет
- Hubungan Antara Kemampuan Pengelolaan Emosi Dengan Perilaku Agresif Peserta Didik Di SMP Negeri 23 PadangДокумент8 страницHubungan Antara Kemampuan Pengelolaan Emosi Dengan Perilaku Agresif Peserta Didik Di SMP Negeri 23 PadangChoiria FuОценок пока нет
- Consumer Behavior Hawkins Chap 2Документ64 страницыConsumer Behavior Hawkins Chap 2jack100% (1)
- Constructivist Learning Theory SurveyДокумент3 страницыConstructivist Learning Theory SurveyMadiha SumbalОценок пока нет
- 2017 - BA Psych Honours Prospectus PDFДокумент12 страниц2017 - BA Psych Honours Prospectus PDFMegon HeatherОценок пока нет
- Media & Info Literacy Lesson PlanДокумент2 страницыMedia & Info Literacy Lesson Planseijuro hiko87% (15)
- Chapter-1 Managing Cultural Diversity-An IntroductionДокумент37 страницChapter-1 Managing Cultural Diversity-An IntroductionSakshi GargОценок пока нет
- The Effects of Inclusive Education On The Self-ConДокумент7 страницThe Effects of Inclusive Education On The Self-Consumbarhijab storeОценок пока нет