Академический Документы
Профессиональный Документы
Культура Документы
Neonatal Cardiac Arrhythmias: Intensive Care Nursery House Staff Manual
Загружено:
Kranti PrajapatiИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Neonatal Cardiac Arrhythmias: Intensive Care Nursery House Staff Manual
Загружено:
Kranti PrajapatiАвторское право:
Доступные форматы
Intensive Care Nursery House Staff Manual
Neonatal Cardiac Arrhythmias
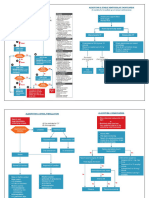
INTRODUCTION: Identification and treatment of arrhythmias in newborns is challenging and differs from older children, and the natural history of arrhythmias presenting in the neonatal period is often dramatically different. METHODS OF DIAGNOSIS AND THERAPY: For management of arrhythmias, consult Cardiology team. 1. Diagnostic methods: 15 lead electrocardiogram (standard 12 lead plus V3R, V4R, V7) Heart rate determination (ECG strip, count number of QRS complexes in 6 sec x 10) Blood pressure (intra-arterial or indirect) 2. Treatment: Electrical (See below for drug therapy) Artificial pacing : -Temporary transvenous pacing -Esophageal pacing Cardioversion: -Setting: 0.5 - 2.0 Joules/kg -Mode: synchronous for narrow QRS; asynchronous for ventricular fibrillation IMMEDIATE MANAGEMENT OF ARRHYTHMIAS: Tachyarrhythmia narrow-QRS wide-QRS Bradyarrhythmia
stable vagal maneuvers adenosine, propranolol or digoxin
unstable synchronized cardioversion
stable Procainamide, lidocaine in VT
unstable synchronized cardioversion no response asynchronous mode
unstable A B C*, O2, atropine & isoproterenol, temporary transvenous pacing
*A B C, airway, breathing, circulation
105
Copyright 2004 The Regents of the University of California
Neonatal Cardiac Arrhythmias
A. Tachy-arrhythmias with narrow QRS: I. Diagnosis
Atrial flutter
Reentry tachycardias Findings on ECG
-"Sawtooth" flutter waves -AV block does not terminate atrial rhythm -Atrial rate up to 500 in newborns -Variable AV conduction common -P follows QRS, typically on upstroke of T -Superior or rightward P wave axis -AV block always terminates tachycardia -Typically terminates with P wave -After termination, WPW have pre-excitation -Incessant - P wave precedes QRS -Inverted P waves in II, III, AVF -AV block always terminates tachycardia -May terminate with QRS or P wave -No pre-excitation after termination -P usually not visible, superimposed on QRS -AV block usually terminates tachycardia.
Treatment
-Unstable: esophageal pacing or electrical cardioversion -Stable: digoxin, propranolol, or digoxin + procainamide
Accessory pathway mediated tachycardia (WPW)
-Unstable: esophageal pacing or electrical cardioversion -Stable: vagal maneuvers. adenosine propranolol or digoxin -No response: procainamide or flecainide
Permanent form of junctional reciprocating tachycardia (PJRT)
Atrioventricular node reentry
Atrial and sinoatrial reentry
-P present, precedes next QRS -Terminates with QRS rather than P -AV block does not terminate atrial rhythm -P axis may be superior or inferior -"Irregularly irregular" -No two RR intervals exactly the same -P waves difficult to see, bizarre and chaotic
-Unstable: electrical cardioversion -Stable: propranolol, procainamide or amiodarone -Unstable: electrical cardioversion -Stable: digoxin + procainamide
Atrial fibrillation
II. Increased automaticity
Sinus tachycardia -Normal P wave axis -P waves precede QRS -Due to extrinsic factor such as heart failure, fever, anemia, catecholamines, theophylline -Incessant -Abnormal P axis which predicts location of focus -P wave precedes QRS -Continues in presence of AV block -Incessant -Usually with atrio-ventricular dissociation and slower atrial than ventricular rate. -Capture beats with no fusion. -Treat causative extrinsic factor
Atrial ectopic tachycardia
-Unstable: IV amiodarone -Stable: propranolol, sotalol or amiodarone, or digoxin + procainamide. -Unstable: cooling, IV amiodarone -Stable: propranolol, sotalol or amiodarone
Junctional ectopic tachycardia
106
Copyright 2004 The Regents of the University of California
Neonatal Cardiac Arrhythmias
B. Tachy-arrhythmias with wide QRS: Diagnosis
Ventricular tachycardia (VT)
Findings on ECG
-Often with AV dissociation -Capture beats with narrower QRS than other beats; fusion beats -Complete chaotic rhythm -Rapid and irregular rhythm
Treatment
-Unstable: electrical cardioversion -Stable: lidocaine, procainamide
Ventricular fibrillation
SVT with pre-existing bundle branch block
Antidromic SVT in WPW
-QRS morphology similar to that in sinus rhythm -QRS morphology is that of right or left bundle branch block -QRS morphology similar to pre-excited sinus rhythm, but wider -Never with AV dissociation
(1) asynchronous cardioversion 2j/kg (2) asynchronouss cardioversion 2j/kg (3)asynchronous cardioversion 4j/kg (4)lidocaine + asynch. cardioversion. -Unstable: esophageal pacing or electrical cardioversion -Stable: vagal maneuvers, adenosine, propranolol or digoxin -No response: procainamide or flecainide
C. Bradyarrhythmias: Diagnosis
Sinus bradycardia
Findings on ECG
Treatment
-Vigorous resuscitation and supportive care -A B C -O2 -Treat underlying causes -Unstable: A B C O2 Atropine, isoproterenol infusion Temporary transvenous pacing -Stable: Treat underlying causes -Permanent pacemaker in AV block with ventricular rate < 55 (newborn)
-Slow atrial rate with normal P waves -1:1 conduction -Due to underlying causes such as hypoxia, acidosis, increased intracranial pressure, abdominal distension, hypoglycemia, hypothermia, digoxin, propranolol Atrioventricular block -Atrioventricular dissociation -Regular R-R intervals Complete atrioventricular block -Regular P-P intervals -Atrial rate > ventricular rate -P which occur after T have no effect on R-R interval -Infants of maternal lupus 2nd degree atrioventricular block - Mobitz type I (Wenckebach) -Progressive PR interval prolongation followed by a blocked beat -Usually indicates block in the AV node - Mobitz type II - No characteristic PR prolongation as seen in type I. - Usually not reversible with medications. - Type II has worse prognosis than type I. - Sinus P waves intermittently disappear due to block of impulses leaving the node. -Premature P wave superimposed on the previous T wave, deforming it
Sinus exit block Premature atrial contractions
-Usually does not need treatment.
107
Copyright 2004 The Regents of the University of California
Вам также может понравиться
- Neonatal Cardiac Arrhythmias: Intensive Care Nursery House Staff ManualДокумент3 страницыNeonatal Cardiac Arrhythmias: Intensive Care Nursery House Staff ManualAhmed MohammedОценок пока нет
- Heart Dysrhythmias Cheat Sheet ExplainedДокумент5 страницHeart Dysrhythmias Cheat Sheet ExplainedpcmundotОценок пока нет
- Nclex RN Review Notes 2018 Triple eДокумент30 страницNclex RN Review Notes 2018 Triple eEndla SriniОценок пока нет
- NCM 112 MSN Prelim Topic 4 Cardiac Rhythm DisordersДокумент5 страницNCM 112 MSN Prelim Topic 4 Cardiac Rhythm DisordersKim Erida QuezonОценок пока нет
- Bradycardia and TachycardiaДокумент66 страницBradycardia and TachycardiaKarissaОценок пока нет
- Ecg Dysrythmias Nursing Responsibilitu Sinus Node 1.) Sinus BradycardiaДокумент2 страницыEcg Dysrythmias Nursing Responsibilitu Sinus Node 1.) Sinus BradycardiaNickha LazoОценок пока нет
- This Study Resource Was Shared Via: Sinus BradycardiaДокумент3 страницыThis Study Resource Was Shared Via: Sinus BradycardiaPascal St Peter NwaorguОценок пока нет
- Atrial Arrhythmias Definition and Pathology Significance Etiology Clinical Manifestations InterventionДокумент5 страницAtrial Arrhythmias Definition and Pathology Significance Etiology Clinical Manifestations Interventionmakyofrancis20Оценок пока нет
- Cardiac Arrhythmias Guide: Tachycardias and Supraventricular RhythmsДокумент83 страницыCardiac Arrhythmias Guide: Tachycardias and Supraventricular Rhythmsmargareth hoyan SilabanОценок пока нет
- Cardiac Dysrhythmia Chart Med Surg NUR4 PDFДокумент3 страницыCardiac Dysrhythmia Chart Med Surg NUR4 PDFlml100% (1)
- NCM 118 - Lesson 11 (Arrhythmia)Документ5 страницNCM 118 - Lesson 11 (Arrhythmia)Bobby Christian DuronОценок пока нет
- 40 - Arrythmias (PICU COURSE)Документ44 страницы40 - Arrythmias (PICU COURSE)surasuarezlopezОценок пока нет
- Workshop Pit IV THN 2017Документ57 страницWorkshop Pit IV THN 2017anettepardedeОценок пока нет
- Arrhythmia: CausesДокумент21 страницаArrhythmia: CausesDagmawit GirmaОценок пока нет
- The ECG Made Easy by John R. HamptonДокумент1 страницаThe ECG Made Easy by John R. HamptonLpОценок пока нет
- Understanding Tachycardia and Bradycardia ClassificationsДокумент18 страницUnderstanding Tachycardia and Bradycardia ClassificationsZega AgustianОценок пока нет
- ELECTROCARDIOGRAM by Aldrin Jayson AlmadenДокумент23 страницыELECTROCARDIOGRAM by Aldrin Jayson AlmadenItsMe AJОценок пока нет
- Drugs used to treat cardiac arrhythmiasДокумент74 страницыDrugs used to treat cardiac arrhythmiasGunel Sadiqova100% (1)
- Cardiac Life Support Cme Latest Edited VersionДокумент53 страницыCardiac Life Support Cme Latest Edited VersionSyed Shahrul Naz SyedОценок пока нет
- Cardiac Life Support Cme Latest Edited VersionДокумент53 страницыCardiac Life Support Cme Latest Edited VersionSyed Shahrul Naz SyedОценок пока нет
- Arrhythmias: BY Zarish FazilДокумент64 страницыArrhythmias: BY Zarish FazilZarish Amanat100% (1)
- Cardiology-5 DysrhythmiaДокумент16 страницCardiology-5 DysrhythmiaMahmoud RamadanОценок пока нет
- ACLS For TachycardiaДокумент31 страницаACLS For TachycardiaTausif HaqueОценок пока нет
- EKG Arrhythmia Identification and Treatment GuideДокумент28 страницEKG Arrhythmia Identification and Treatment GuideJason LinОценок пока нет
- ECG Mastery Improving Your ECG Interpretation SkillsДокумент23 страницыECG Mastery Improving Your ECG Interpretation SkillsHitesh Deora100% (2)
- 3881 - Prosedur Pendaftaran Internship Per November 2016Документ57 страниц3881 - Prosedur Pendaftaran Internship Per November 2016Munawir_Syam91Оценок пока нет
- Cardiology Notes USMLE Step CKДокумент135 страницCardiology Notes USMLE Step CKArianna BetancourtОценок пока нет
- Sinus Rhythm and Sinus and Atrial DysrhythmiasДокумент41 страницаSinus Rhythm and Sinus and Atrial Dysrhythmiasclaudia brongОценок пока нет
- Electrocardiogram Interpretation and Nursing InterДокумент4 страницыElectrocardiogram Interpretation and Nursing InterJulia Rae Delos SantosОценок пока нет
- Curs 7 - Bradiaritmii TahiaritmiiДокумент88 страницCurs 7 - Bradiaritmii Tahiaritmiijhonny12321Оценок пока нет
- Ecg Arrhythmia: Dr. Lowry Yunita, SPJP, FihaДокумент48 страницEcg Arrhythmia: Dr. Lowry Yunita, SPJP, FihaMaria JozilynОценок пока нет
- NCM 118Документ8 страницNCM 118Zanie CruzОценок пока нет
- Atrioventricular Nodal Reentry Tachycardia (AVNRT)Документ24 страницыAtrioventricular Nodal Reentry Tachycardia (AVNRT)Radya Agna100% (1)
- Width of The QRS Complex: - Wide VT, SVT With Aberrant Conduction - Narrrow SVTДокумент11 страницWidth of The QRS Complex: - Wide VT, SVT With Aberrant Conduction - Narrrow SVTWidelmark FarrelОценок пока нет
- DYSRHYTHMIASДокумент9 страницDYSRHYTHMIASgudobenОценок пока нет
- Antiarrhythmic Agents Lecture NotesДокумент6 страницAntiarrhythmic Agents Lecture NotesErnest Patrick MatiasОценок пока нет
- Arrythmias and EKGs 2Документ20 страницArrythmias and EKGs 2Nur Ima ErvianaОценок пока нет
- Basic EKG ECG Rhythms CheatsheetДокумент1 страницаBasic EKG ECG Rhythms CheatsheetAhmad83% (6)
- 26) Approach To Pediatric ArrhythmiasДокумент44 страницы26) Approach To Pediatric ArrhythmiasJude AlyousefОценок пока нет
- W2 Emergency ECG (DR Refli)Документ47 страницW2 Emergency ECG (DR Refli)indahflsaragihОценок пока нет
- Arrhythmias: Sing Khien Tiong Gpst1Документ34 страницыArrhythmias: Sing Khien Tiong Gpst1preethi preethaОценок пока нет
- Atria Arrythmia TestДокумент8 страницAtria Arrythmia TestAnnette SandovalОценок пока нет
- Approach To ArrhythmiasДокумент1 страницаApproach To ArrhythmiasADITYA SARANGIОценок пока нет
- CardiologyДокумент149 страницCardiologyMuhammad SyafiqОценок пока нет
- Unit Learning Outcome: Course MapДокумент3 страницыUnit Learning Outcome: Course MapBunnie AlphaОценок пока нет
- Atrial-Rhythm 230518 191520-1Документ2 страницыAtrial-Rhythm 230518 191520-1Maxinne GorospeОценок пока нет
- TACHYARRHYTMIASДокумент40 страницTACHYARRHYTMIASRoy Sandy PermanaОценок пока нет
- MCEM B CVS TachycardiaДокумент12 страницMCEM B CVS TachycardiaRajin MaahiОценок пока нет
- How To: Read ECG?Документ63 страницыHow To: Read ECG?Let BОценок пока нет
- Peri Operative Arryhthmias: Dr. Juzny Alkatiri, SPPD, SPJPДокумент102 страницыPeri Operative Arryhthmias: Dr. Juzny Alkatiri, SPPD, SPJPAstari Pratiwi NuhrintamaОценок пока нет
- Arrhythmia Types and Features Cheat SheetДокумент2 страницыArrhythmia Types and Features Cheat SheetNur Fatima SanaaniОценок пока нет
- Diagnosis Dan Tatalaksana Awal SVTДокумент47 страницDiagnosis Dan Tatalaksana Awal SVTZuly Vita AulyaОценок пока нет
- Detect VT vs SVT with Wide QRSДокумент1 страницаDetect VT vs SVT with Wide QRSLwin Maung Maung ThikeОценок пока нет
- Quick Ekg ReferenceДокумент23 страницыQuick Ekg Referencekowaikowar100% (1)
- EKG Interpretation Basics Guide: Electrocardiogram Heart Rate Determination, Arrhythmia, Cardiac Dysrhythmia, Heart Block Causes, Symptoms, Identification and Medical Treatment Nursing HandbookОт EverandEKG Interpretation Basics Guide: Electrocardiogram Heart Rate Determination, Arrhythmia, Cardiac Dysrhythmia, Heart Block Causes, Symptoms, Identification and Medical Treatment Nursing HandbookОценок пока нет
- Syncope CasesОт EverandSyncope CasesRoberto García-CiveraОценок пока нет
- Transport in MammalsДокумент109 страницTransport in Mammalsgalaxytwy100% (1)
- Microsoft Word - CC2046 EWC Health Reflection GuidelineДокумент2 страницыMicrosoft Word - CC2046 EWC Health Reflection GuidelinegalaxytwyОценок пока нет
- II. Mechanisms For ArrhythmiasДокумент29 страницII. Mechanisms For ArrhythmiasgalaxytwyОценок пока нет
- .Noitamrofni Erom Rof 0059-404-008 Ta ERAC LlacДокумент2 страницы.Noitamrofni Erom Rof 0059-404-008 Ta ERAC LlacgalaxytwyОценок пока нет
- HRC2009, Birmingham, October 20th 2009Документ48 страницHRC2009, Birmingham, October 20th 2009galaxytwyОценок пока нет
- Ventricular ArrhythmiasДокумент6 страницVentricular ArrhythmiasgalaxytwyОценок пока нет
- Ventricular ArrhythmiasДокумент6 страницVentricular ArrhythmiasgalaxytwyОценок пока нет
- TalkingwomenДокумент1 страницаTalkingwomengalaxytwyОценок пока нет
- Plan 1Документ11 страницPlan 1galaxytwyОценок пока нет