Академический Документы
Профессиональный Документы
Культура Документы
The Chronic Cerebrospinal Venous Insufficiency Syndrome
Загружено:
huahuahua1Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
The Chronic Cerebrospinal Venous Insufficiency Syndrome
Загружено:
huahuahua1Авторское право:
Доступные форматы
AZ Series: No.
18
The chronic cerebrospinal venous insufciency syndrome
P Zamboni and R Galeotti
Vascular Disease Centre, Interventional Radiology Unit, University of Ferrara, Italy
Abstract
Chronic cerebrospinal venous insufciency (CCSVI) is a syndrome characterized by stenosies of the internal jugular and/or azygous veins (IJVs-AZ) with opening of collaterals and insufcient drainage proved by reduced cerebral blood ow and increased mean transit time in cerebral MRI perfusional study. The present review is aimed to give a comprehensive overview of the actual status of the art of the diagnosis and treatment of this condition. As far as the origin of venous narrowing is concerned, phlebographic studies of the IJVs and AZ systems demonstrated that venous stenoses were likely to be truncular venous malformations; mostly, they are intraluminal defects such as malformed valve, septa webs. CCSVI condition has been found to be strongly associated with multiple sclerosis (MS), a disabling neurodegenerative and demyelinating disease considered autoimmune in nature. In several epidemiological observations performed at different latitudes on patients with different genetic backgrounds, the prevalence of CCSVI in MS ranges from 56% to 100%. To the contrary, by using venous MR and/or different Doppler protocols, CCSVI was not detected with the same prevalence. Two pilot studies demonstrated the safety and feasibility in Day Surgery of the endovascular treatment of CCSVI by means of balloon angioplasty (PTA). It determines a signicant reduction of postoperative venous pressure. Restenosis rate was found out elevated in the IJVs, but negligible in the AZ. However, PTA seems to positively inuence clinical and QoL parameters of the associated MS and warrants further randomized control trials. Keywords: chronic cerebrospinal venous insufciency; multiple sclerosis; echoDoppler; venous PTA
Anatomy of the cerebrospinal venous system
The cerebrospinal venous system is a threedimensional structure that is often asymmetric and considerably represents a more variable pattern than the arterial anatomy.1,2 The intracranial venous system is mainly composed of parenchymal veins draining into the dural sinuses. The former can be subdivided into two systems:1,2
The supercial (cortical) system reaches dural
sinuses by cortical veins and drains blood mainly from cortex and subcortical white matter; The deep cerebral venous system (DCVs) is composed by the internal cerebral veins, the basal vein of Rosenthal and the great cerebral vein of Galen and their tributaries, and drains the deep white and gray matter surrounding the lateral and third ventricles.
Correspondence: P Zamboni MD, University of Ferrara, 44100 Ferrara, Italy. Email: zmp@unife.it Accepted 3 June 2010
The cerebral veins collect blood into the dural sinuses and in turn redirected toward the main extracranial venous outow routes: the internal jugular veins (IJVs) and the vertebral veins (VVs) system (Figure 1). The anatomical pathways of jugular drainage are well established. The main jugular blood drainage pathway leads from the
DOI: 10.1258/phleb.2010.009083. Phlebology 2010;25:269279
A Z Series: No. 18
P Zamboni and R Galeotti. CCSVI
improves the aspiration of blood toward the right atrium. In addition to vis a tergo and vis a fronte, postural mechanisms play a main role in ensuring a correct cerebral venous return. Several ultrasound studies of healthy volunteers demonstrated that the pattern of cerebral venous drainage changes, even under physiological conditions, depending on the body position.1,2,4 7 In the prone position, the outow through the IJVs is favoured; this assumption was based on angiographic studies and cerebral blood ow analyses with nitrous oxide, labelled erythrocytes and thermodilution techniques.1 Moreover, the supine posture favours cerebral venous outow through the IJVs, whereas passing to the upright position transfers most of the encephalic drainage to the VVs.4 7
Figure 1 Schematic of the cerebrospinal venous system with the location and relative prevalence of extracranial and extravertebral venous stenosis. DMCVs, deep middle cerebral veins; TS, transversal sinus; CV, condylar veins; VV, vertebral veins; IJV, internal jugular vein; VP, vertebral plexus; SVC, superior vena cava: AZY, azygous vein
Echo-colour Doppler as a tool for assessing the physiology of cerebral venous return
The echo-colour Doppler (ECD) is an ideal tool for assessing cerebral venous return. Given the inuence of posture on venous outow, ECD permits to turn rapidly the subject with the help of a tilt chair. It is intuitive that this cannot be easily done by the means of MR. The different signicance of the gravitational gradient in ensuring venous return requires investigating the subject with the head, respectively, either at 908 or at 08. Moreover, ECD permits assessing the ow direction by activating the thoracic pump. The detection of ve parameters related to the above described physiology of cerebral venous return have been proposed:6,8 (1) Flow direction in the cervical veins: It has been reported that ow is monodirectional in the IJVs/VVs. Flow is always increased by the activation of the pump asking the subject to breath. Flow direction is usually assessed during the apnoea phase; (2) Flow direction in the intracranial veins: The cerebral veins are not easy to be insonated. By using the temporal window the basal vein of Rosenthal is one of the more constant segments to be detected, in consequence of the anatomical relationship with the P2 segment posterior cerebral artery. The normal ow is expected in the opposite direction to the transducer position.9 Below the classical temporal window, the intracranial venous compartment can also be studied in the supra-condylar projection. Such a window permits assessing the direction of ow in the inferior petrosus
transverse sinuses via the sigmoid sinuses into the IJVs, which meet the superior cava vein via the brachiocephalic vein. Valve fractioning of the blood column is possible only at the distal portion of the IJVs, where valves were found in 93% of postmortem studies, and in 87% of Bmode investigations, mainly on the right side.3 The VVs system is a freely communicating, valveless system present throughout the entire spinal column and may be divided into an internal intraspinal part, the epidural veins and an extraspinal paravertebral part.1,2 The system communicates with deep thoracic and lumbar veins, intercostal veins, the azygous vein (AZ) and hemiazygous veins. The AZ represents the nal collector of such an enormous plexus, and in turn drains into the superior vena cava, as well as into the inferior vena cava, via the anastomosis of the hemiazygous veins with the left renal vein (Figure 1).
Physiology of cerebral venous return
The blood leaves the brain by using the back propulsion of the residual arterial pressure (vis a tergo), complemented by anterograde respiratory mechanisms (vis a fronte).1,2,4 7 The latter consists of the thoracic pump increased venous outow during inspiration, thanks to increased thoracic negative pressure, which
270 Phlebology 2010;25:269279
P Zamboni and R Galeotti. CCSVI
A Z Series: No. 18
sinus and/or spheno-parietal sinus. In both, the normal ow is elicited by inspiration and directed backward. These are the more easily accessible venous segments by the means of the trancranial ECD technique;9 11 (3) B-mode anomalies/stenosis of the IJVs: Out of the valves of the distal portion of the internal jugular, usually open, in normal cases there are no other intraluminal leaets. Valves are closed whenever central venous pressure rises. Ultrasonography easily demonstrated the valve leaets in 87% of patients.3 Finally, it is frequent that the observation of some asymmetry comparing the cross-sectional area (CSA) of the two IJVs; however, in normal volunteers the smallest CSA measured in the IJVs was never less than 0.4 cm2; (4) Blocked outow in the cervical veins: Blood ow velocity in the cervical veins is increased by activation of the thoracic pump. Temporary outow block can be seen in the cervical veins in healthy subjects, but never reported in all the postural and respiratory conditions; (5) CSA in the IJV: As reported above, under normal physiological conditions, the CSA of the IJV is wider in supine position. This parameter can be assessed in B-mode in transversal access, giving the elliptical shape of the cervical veins.
(3) Type C pattern (14%) is characterized by bilateral stenosis in both IJVs, with a normal azygous system; (4) Type D pattern (18%) is characterized by the multilevel involvement of the azygous and lumbar systems. Association with the IJVs was observed in approximately 50% of cases, causing an additional obstruction in these patients. As far as the collaterals or substitute circles is concerned when venous ow is deviated into collaterals to bypass an obstacle, there exists an anatomic bypass called a vicarious shunt.2,6,14 This type of shunt is desirable because it bypasses blocked veins and thereby reduces resistance to drainage. Blood ows regularly in the substitute circle under the effects of distal cardiac residual pressure and proximal thoracoabdominal aspiration. The main collateral pathways activated in the course of CCSVI are the condylar venous system, the pterygoid plexus and the thyroid veins.2,6 Additionally, the suboccipital cavernous sinus and the hemiazygous-lumbar venous anastomosis with the left renal vein may also become prominent substitute circles. Collateral circulation prevents brain oedema and intracranial hypertension,2,4 and ensures a correct but slower, and thus insufcient, venous drainage.12,14
The chronic cerebrospinal venous insufciency syndrome
Chronic cerebrospinal venous insufciency (CCSVI) is a syndrome characterized by stenosies of the IJVs and AZ venous system with opening of collaterals2,7 and insufcient drainage proved by increased mean transit time in a cerebral magnetic resonance imaging (MRI) perfusional study.12 Phlebographic studies of the IJVs and AZ systems demonstrated that venous stenoses were truncular venous malformations (Figures 7 and 8), and quite recently were inserted in the Consensus Document of the UIP on venous malformations.13 The CCSVI syndrome showed four main patterns of distribution of the venous stenosis:7 (1) Type A pattern (30%) is characterized by signicant stenosis either of the proximal azygous or of one of the two IJVs, with a compensatory controlateral IJV that appears with an ample cross-sectional area; (2) Type B pattern (38%) is characterized by signicant stenoses of both IJVs and the proximal azygous;
CCSVI a paradigm shift in the physiology of cerebral venous return
Extracranial and extravertebral venous narrowing characterizing the CCSVI syndrome deeply modies the physiology of cerebral venous return. This can be assessed by investigating the ve ECD parameters related to cerebral venous return described above: (1) Flow direction in the cervical veins: CCSVI can be characterized by the detection of reux in the cervical veins. This is usually a long-lasting reux expressing a reverse ow in order to permit a drainage through collateral circle.14 The parameter is positive when reux in one of the IJVs and/or in one of the VVs is assessed in both sitting and supine posture, through activation of the thoracic pump, without the need of Valsalva.7,8 These ndings suggest stenoses in the IJV and/or in the AZ, respectively (Figure 2, right); (2) Flow direction in the intracranial veins: The parameter is positive when reux, indicating a ow in the direction opposite to the physiological
Phlebology 2010;25:269279 271
A Z Series: No. 18
P Zamboni and R Galeotti. CCSVI
Figure 2 Left: reux detected by the means of echo-colour Doppler at the level of the IJV, with activation of cervical substitute circles (SC). Right: the corresponding phlebographic imaging with distal IJV stenosis. IJV, internal jugular vein
one, is detected in the vein of Rosenthal and in other deep cerebral veins, and/or in the dural sinusis. Flow direction in the cranial veins is not often simple to be identied. Multi-angle Doppler, like QDP system (MyLab Vinco, Esaote Biosound, Genoa, Italy) may facilitate the detection of B-directional ow (Figure 3). This nding suggests the waste of cerebral venous return, in consequence of the hampered outow;7,8,15
(3) B-mode anomalies\stenosis of the IJVs: The parameter is positive when the B-mode detects stenoses in the IJVs in the form of hypoplasia, annulus, webs, septum or malformed valves (Figure 4);7,16 (4) Blocked outow in the cervical veins: The parameter is positive when the absence of Doppler signal is detected in the IJV and/or in the VV, even after forced inspiration, in both sitting and supine posture; or alternatively,
Figure 3 Transcranial colour-Doppler of the cavernous sinus: The cloud of colours in the middle panel can be deciphered by means of a multiangle Doppler system, respectively into a ow directed physiologically backward at inspiration (INSP), and toward the frontal side, pathologic reux, at expiration (EXP)
272
Phlebology 2010;25:269279
P Zamboni and R Galeotti. CCSVI
A Z Series: No. 18
The inter-observer variability rate between trained and not trained ECD operators, assessed using the same equipment (MyLab Vinco, Esaote Biomedica, Genoa, Italy), was 0.47 (95% CI 0.27 0.68), whereas the inter-observer agreement between trained operators was 0.80 (95% CI 0.59 1.01). Finally, the intra-observer variability rate in trained operators was 0.93 (95% CI 0.80 1.06).17 The conclusion is that ECD diagnostic accuracy is largely dependent on specic training. Recently, for each of the ve ECD parameters a contribution score was assigned. These scores, combined, gave an overall severity measure, the venous haemodynamics insufciency severity score or VHISS, ranging from 0 to 16.18
Figure 4 High resolution B-mode imaging plus Power Doppler of the jugula junction clearly depict a complete obstruction of the vein due to intraluminal septum
Truncular venous malformations of the CCSVI syndrome
Patients fullling the Doppler screening criteria for CCSVI underwent selective venography of the lumbar veins, left renal vein, AZ and IJVs via catheterization of the left iliac femoral venous axis.7 As far as the morphology is concerned, we considered the following malformations:16
in one posture but with reux detection in the other position. Blocked outow is related to stenosis distal to the point of assessment (Figure 5, right);7,8 (5) CSA in the IJV: The CSA of the IJV is measured both in supine and sitting posture. Thus, the parameter is assigned if the CSA in sitting posture should be greater. This happens frequently in CCSVI MS; alternatively, often the CSA in the IJV appears almost at despite the change in posture (Figure 6, left). Operationally, a subject is considered affected by CCSVI if two or more of the proposed physiological parameters should be positive and, nowadays, ECD can be considered a screening device.
Annulus refers to signicant circumferential
stenosis of the whole venous wall;
Septum/valve malformation refers to anomalous valve apparatus causing signicant ow obstacles at the level of the junction of the IJVs with the brachiocephalic/anonymous trunk; Hypoplasia refers to under-developed long venous segments; Twisting refers to severe stenosies in consequence of a twisted venous segment;
Figure 5 Left: normal ow in the vertebral artery (V and blocked outow in the vertebral vein (VV). Right: A) This nding corresponded to membraneous obstruction of the outlet of the AZ into the SVC. AZ, azygous vein; SVC, superior vena cava
Phlebology 2010;25:269279
273
A Z Series: No. 18
P Zamboni and R Galeotti. CCSVI
Figure 6 Left: increased cross-sectional area (CSA) measured in the IJVs of healthy controls passing from the sitting to the supine posture. Right: at or even negative CSA variation measured in the majority of CCSVI-MS patients. IJV, internal jugular vein; CCSVI-MS, chronic cerebrospinal venous insufciency multiple sclerosis
Membranous obstruction refers to a membrane
almost occluding a vein; Agenesis refers to the complete anatomical absence of a venous segment.
extracranial and extravertebral cerebrospinal veins are given, and the more typical malformations are shown in the gures.
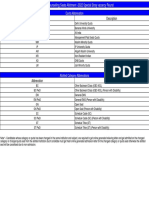
Annulus, septum, membranous obstruction, hypoplasia and agenesis are truncular malformations previously described in other venous segments (cava, iliac, deep veins of the lower limbs).13 In Figure 7 there are some examples of venous stenosing lesions morphologically quite similar to those described in the IJVs/AZ in course of CCSVI. In contrast, twisting of the AZ is a truncular malformation never been described so far (Figure 8). In Table 1 the distribution of the different truncular lesions in the
Association of the CCSVI syndrome with neurological disorders
Blocked extracranial venous blood outow causes a high rate of cerebral venous reux in multiple sclerosis (MS) patients, as demonstrated in previous studies.8,10 This detected reux, propagated from the chest and neck veins into the parenchymal veins of the brain, was found strongly associated to the more common cause of disability in young
Figure 7 Left: annulus of the IJV between the venous valve (VV) and the brachio cephalic trunk (BCT). Right: twisting of the AZY just below the arch with dilation and reux toward the spine. AZY, azygous vein; IJV, internal jugular vein
274
Phlebology 2010;25:269279
P Zamboni and R Galeotti. CCSVI
A Z Series: No. 18
Figure 8 Parallel between truncular venous malformation in the jugular veins and in other venous segments. (a) Membranous obstruction of the superior vena cava in primary Budd-Chiari syndrome (courtesy of BB Lee, Washington, USA). (b) The same lesion in up-side-down fashion observed in the IJV. (c) Closed truncular stenosis of the left IJV quite similar to that depicted in (d) at the level of the external iliac vein. IJV, internal jugular vein
people, namely to MS. It has been demonstrated that extracranial reux was also transmitted up to the DCV system in 50% of MS cases. Extracranial blockages and haemodynamic disturbances of the cerebral veins are particularly associated to MS. CCSVI was not found in patients affected by other neurodegenerative diseases, such as Alzheimer, Parkinson and amyotrophic lateral sclerosis,4,6,9 11,15 but was detected in a miscellaneous of other neurological disorders.19 Cerebral vein haemodynamics in healthy subjects are characterized by a laminar, mono-directional ow with low velocity,10 15 and it has been established that steady laminar shear stress promotes a release of factors from endothelial cells that inhibit migration of leukocytes.20,21 In contrast, altered haemodynamics have been documented by transcranial ECD in veins anatomically related to MS lesions, characterized by a high rate of reverse ow with a chaotic displacement of blood at the activation of the thoracic pump.6 8,15 Reuxing oscillatory ow favours the expression of adhesion molecules on endothelial cells, becoming a previously overlooked inammatory mechanism in MS.20,21 Finally, the score of severity of anomalous
venous haemodynamics (VHISS) is strongly correlated to a signicant reduction of the cerebrospinal uid ow dynamics in consequence of increased transmural pressure in CCSVI.18
The CCSVI prevalence in MS
Duplex scanning, despite the need of a formal training, is the perfect tool for screening for CCSVI.17 It provides information on the prevalence of CCSVI in MS, and in healthy people at different geographical regions and among populations with different genetic backgrounds. For instance the prevalence in MS ranges between 56% and 100%, indicating that CCSVI is one of the major risk factors for the development of MS. Particularly, in the USA a prevalence of 56% versus 22% was found in the normal population;19 in Middle Orient of 84% versus 0%; and in Central/Eastern Europe of 90% without data on healthy controls.22,23 To the contrary, by using MR venography and/or different from the above echo-colour-Doppler protocols, some authors did not nd evidence of different prevalence of CCSVI in MS patients respective
Table 1 Morphology, location and relative rate of the stenosing venous truncular malformations found out in 65 consecutive patients16 Annulus (%) AZ Distal AZ Lumbar IJVr IJVl 0 0 0 28 52 Septum/valve malformation (%) 14 0 0 46 43 Hypoplasia (%) 9 5 2 6 6 Twisting (%) 0 18 0 0 0 Membranous obstruction (%) 48 0 0 0 0 Agenesis (%) 0 0 8 0 0
Distal AZ is intended below the arch
AZ, azygous vein; IJV, internal jugular vein Hypoplasia can be combined with other malformations in the AZ and in the IJVl
Phlebology 2010;25:269279
275
A Z Series: No. 18
P Zamboni and R Galeotti. CCSVI
to controls.24,25 Particularly, the Doppler methodology proposed by Doepp et al. seems to be inadequate because measures more than 40% differences in cerebral venous outow among healthy controls.25,26 Given that both the autoimmune model and the CCSVI model have robust data and theory to back them up, it may well be that both CCSVI and externally driven, central nervous system (CNS) autoimmunity are important contributors to MS. The above recently released data from ongoing CCSVI studies seem to favour an MS disease model which integrates both CCSVI and CNS autoimmunity.
signicantly lower net CSF ow (P 0.038), which was highly associated with the VHISS (r 0.77, r2 0.60, P , 0.0007). This nding is consisting with increased venous pressure in the superior saggital sinus. This study demonstrates that venous outow disturbances in the form of CCSVI signicantly impact on CSF pathophysiology in patients with MS.18
Neurological outcome measures in MS
Several validated outcome measures are currently used to assess treatment effect in MS. Clinical measures are the Kurtzke Expanded Disability Status Scale (EDSS) and the Multiple Sclerosis Funtional Composite (MSFC). EDSS is a method of quantifying disability in MS.34 The EDSS categorizes a persons level of disability. EDSS scores range from 0 to 10, with higher scores indicating more severe disability. It is an important tool in clinical practice, because it is widely used and photographs the clinical situation. The EDSS score is based upon neurological testing and examination of functional systems, which are areas of the CNS which control bodily functions. The functional systems are: Pyramidal (ability to walk); Cerebellar (coordination); Brain stem (speech and swallowing); Sensory (touch and pain); Bowel and bladder functions; Visual; Mental; Other (includes any other neurological ndings due to MS). (ii) MSFC is more sophisticated and less utilized in clinical practice, but preferable in clinical trials.35,36 MSF is a multidimensional clinical outcome measure consisting of quantitative timed tests of leg function/ambulation (Timed 25-Foot Walk T25FW), arm function (Nine-Hole Peg Test 9HPT) and cognitive function (Paced Auditory Serial Addition Test PASAT) expressed as a single score along a continuous scale.35 Tests were administrated using a standardized protocol according to MSFC guidelines.36 The MSFC score was derived from three components: (1) the average scores from the four trials on the 9HPT (the two trials for each hand are averaged, converted to the reciprocals of the mean times for each hand and then the two reciprocals are (i)
Histology of MS plaques related to CCSVI
In chronic venous disorders (CVDs) of the leg, it is well established that the same altered venous haemodynamic conditions negatively affect tissue drainage, with development of chronic inammation, iron deposition and various degrees of tissue injury.27 At the microcirculatory level, erythrocyte sludge facilitates the transmigration of these cells and subsequent extravascular haemolysis, leading to increased pericapillary iron deposition.27 Histological studies demonstrate the peculiar disposition of the iron stores in MS constantly encircling the venous wall.28 30 Iron stores are arranged in hemosiderin deposits as well as in ferritin-like structures inside the macrophage, curiously resembling perivenous iron stores commonly observed in peripheral venous disease.27 Starting from histology, an impressive parallel has been delineated between the inammatory process activated in course of CVD, and that profoundly studied in MS.6 Interestingly, pericapillary brin cuffs, a well-known marker of venous hypertension, have also been demonstrated in CCSVI associated with MS.27 30 Pressure in the AZ and in the IJVs measured signicantly higher in CCSVI-MS respect to controls, testifying the haemodynamic signicance of venous obstruction.7 These ndings are consistent with a role of venous hypertension in the complex pathogenesis of MS, only hypothesized to date.31,32 Raised venous pressure can stretch vein walls sufciently to separate the tight junctions between endothelial cells forming the bloodbrain barrier.33 Colloids and erythrocytes could then pass through the exposed porous basement membranes participating to the inammatory process. In addition, VHISS is strongly associated to a parallel impairment of the cerebro-spinal uid (CSF) dynamics measured by the means of advanced MR techniques. The CCSVI-MS patients showed a
276 Phlebology 2010;25:269279
P Zamboni and R Galeotti. CCSVI
A Z Series: No. 18
averaged); (2) the average scores of two 25FW trials; and (3) the number correct from the PASAT-3. For each component a z-score was then created using test results from the baseline visit. A z-score is a standardized score obtained by subtracting the baseline mean from the test result then dividing by the baseline SD. The composite score was calculated by adding the z-scores obtained and dividing the sum by 3, as described in the following formula: MSFC score (zarm, average zleg, average + zcognitive)/3.0. The negative value of the 25FW z-score was used to make the direction of change the same as the other components. A decrease or an increase in the MSFC score represents, respectively, deterioration or improvement in neurological functions. MS quality-of-life (QoL) questionnaire is another validated tool to assess not only physical performances but also disabilitating symptoms such as chronic fatigue and mental status as well. It was specically projected taking into account disabilities and disease course of MS.37 There are also neurophysiological measurements, such as motor-evoked potentials. The pyramidal pathway is frequently affected early on in MS and impaired motor performance is a major cause of disability. Pyramidal tract function can be assessed using transcranial magnetic stimulation (TMS). TMS supports the diagnosis of MS, detecting corticospinal tract involvement and monitoring its course with or without treatment.38 Finally, the MRI measures are considered very important. Although it is unlikely that one single
outcome measure can capture all aspects of the MS disease process, there is potential for MR imaging outcomes to evaluate inammatory and degenerative components within clinical trials. They include the number of active plaques in the brain and in the spinal cord, corresponding to the number of lesions assessed in T1 enhanced gadolinium, the T2 lesions volume and the measurement of atrophy based on global brain volume and/or segmentary brain.39
CCSVI endovascular treatment
Endovascular treatment of CCSVI was reported to be feasible in day surgery with a minor and negligible complication rate.16,40 It consisted of percutaneous transluminal angioplasty (PTA) performed in the majority of cases (Figure 9). Stenting procedures was used in selected cases of AZ twisting.16 Postoperative venous pressure was signicantly lower in the IJVs, and in the AZ as well (P , 0.001). However, the cumulative patency rate at 18 months in the IJVs was 53%, whereas in the AZ was 96%, absolutely more satisfactory. Clinical outcome measures of the associated MS were signicantly improved by PTA treatment, especially in the group characterized by a relapsing-remitting clinical course: rates of relapsefree patients passed from 27% to 50% postoperatively (P , 0.001), and that MRI Gad+ active lesions from 50% to 12% (P , 0.0001). In addition, MSFC at one year improved signicantly, as well physical and mental QoL.
Figure 9 (a) Closed stenosis of the right IJV; (b) The balloon inated during the PTA; (c) Postoperative result IJV, internal jugular vein; PTA, percutaneous transluminal angioplasty
Phlebology 2010;25:269279
277
A Z Series: No. 18
P Zamboni and R Galeotti. CCSVI
The result of this open label prospective study was highly positive in the neurological outcome of MS patients. It presents several limitations, yet. The main shortcomings of this pilot study are represented by the lack of a control group, and the unblinded clinical evaluation. However, the reduction of Gad+ active lesion at the MRI is a blinded and signicant measure. It seems that endovascular treatment could add further advantages with respect to current therapy, because all the patients were under the treatment Food and Drug Administration approved drugs for MS. In a further pilot study two groups of CCSVI-MS patients were evaluated. The rst group underwent to the PTA at baseline, whereas the second group had a delayed endovascular treatment six months later. This study conrmed the safety of PTA because again no major complications occurred. MS outcome measure is currently under evaluation. Further subanalysis of the rst trial demonstrated a signicant reduction of chronic fatigue, one of the more dibilitating symptoms in MS. Chronic fatigue is still the orphan of any effective treatment. The dramatic reduction of fatigue perception following PTA appears to be a symptom peculiar to CCSVI in the highly complex symptomatic picture of MS.41 Moreover, it has been reported that treatment of the associated CCSVI made a parallel improvement in both clinical and neurophysiological TMS parameters. The demonstration of a modication of the cerebrovenous function with both clinical manifestation and via TMS suggests that the hampered cerebral venous return may contribute to the motor clinical manifestation of MS.38 The results of such pilot studies warrant subsequent randomized control trials.
10
11
12
13
14
15
16
17
18
19
References
1 Schaller B. Physiology of cerebral venous blood ow: from experimental data in animals to normal function in humans. Brain Res Rev 2004;46:243 60 Zamboni P, Consorti G, Galeotti R, et al. Venous collateral circulation of the extracranial cerebrospinaloutow routes. Curr Neurovasc Res 2009;3:204 12 Lepori D, Capasso P, Fournier D, Genton CY, Schnyder P. High-resolution ultrasound evaluation of internal jugular venous valves. Eur Radiol 1999;9:1222 6 Ursino M, Lodi CA. A simple mathematical model of the interaction between intracranial pressure and cerebral hemodynamics. J Appl Physiol 1997;82:1256 69 Menegatti E, Zamboni P. Doppler haemodynamics of cerebral venous return. Curr Neurovasc Res 2008;5:260 5 Singh AV, Zamboni P. Anomalous venous blood ow and iron deposition in multiple sclerosis. J Cereb Blood Flow Metab 2009;29:1867 78 20
21
22
5 6
23
Zamboni P, Galeotti R, Menegatti E, et al. Chronic cerebrospinal venous insufciency in patients with multiple sclerosis. J Neurol Neurosurg Psychiatry 2009;80:392 9 Zamboni P, Menegatti E, Galeotti R, et al. The value of cerebral Doppler venous haemodynamics in the assessment of multiple sclerosis. J Neurol Sci 2009;282:21 7 Stolz DE, Kaps M, Kern A, Babacan SS. Reference data from 130 volunteers transcranial color-coded duplex sonography of intracranial veins and sinuses. Stroke 1999;30:1070 5 Valdueza JM, Schmierer K, Mehraein S, Einhaupl KM. Assessment of normal ow velocity in basal cerebral veins. A transcranial Doppler ultrasound study. Stroke 1996;27:1221 5 Baumgartner RW, Nirkko AC, Muri RM, Gonner F. Transoccipital power-based color-coded duplex sonography of cerebral sinuses and veins. Stroke 1997;28:1319 23 Law M, Saindane AM, Ge Y, et al. Microvascular abnormality in relapsing-remitting multiple sclerosis: perfusion MR imaging ndings in normal-appearing white matter. Radiology 2004;231:645 52 Lee BB, Bergan JB, Gloviczki P, et al. Guidelines for diagnosis and treatment of venous malformations. A consensus document of The International Union of Phlebology. Int Angiol 2009;28:43451 Franceschi C. The unsolved puzzle of multiple sclerosis and venous function. J Neurol Neurosurg Psychiatry 2009;80:358 Zamboni P, Menegatti E, Bartolomei I, et al. Intracranial venous haemodynamics in multiple sclerosis. Curr Neurovasc Res 2007;4:252 8 Zamboni P, Galeotti R, Menegatti E, et al. A prospective open-label study of endovascular treatment of chronic cerebrospinal venous insufciency. J Vasc Surg 2009;50:1348 58 Menegatti E, Galeotti R, Genova V, et al. Colour Doppler in multiple sclerosis: diagnostic accuracy and reproducibility. Int Ang 2010;29:121 6 Zamboni P, Menegatti E, Weinstock-Guttman B, et al. The severity of chronic cerebrospinal venous insufciency in patients with multiple sclerosis is related to altered cerebrospinal uid dynamics. Funct Neur 2009;24:133 8 Zivadinov R, Marr K, Cutter G, et al. Combined Transcranial and Extracranial Venous Doppler Evaluation (CTEVD) study. Description of the Design and Interim Results of an Epidemiological Study of the Prevalence of Chronic Cerebrospinal Venous Insufciency in MS and Related Diseases. Abstract presented at the American Academy of Neurology Annual Meeting, Toronto, 2010 Bergan JJ, Schmid-Schonbein GW, Smith PD, Nicolaides AN, Boisseau MR, Eklof B. Chronic venous disease. N Engl J Med 2006;355:488 98 Sorescu GP, Song H, Tressel SL, et al. Bone morphogenic protein 4 produced in endothelial cells by oscillatory shear stress induces monocyte adhesion by stimulating reactive oxygen species production from a nox1-based NADPH oxidase. Circ Res 2004;95:773 9 Simka M, Kostecki J, Zaniewski M, Majewski E, Hartel M. Extracranial Doppler sonographic criteria of chronic cerebrospinal venous insufciency in the patients with multiple sclerosis. Int Angiol 2010;29:109 14 Al-Omari MH, Rousan LA. Internal jugular vein morphology and hemodynamics in patients with multiple sclerosis. Int Angiol 2010;29:115 20
278
Phlebology 2010;25:269279
P Zamboni and R Galeotti. CCSVI
A Z Series: No. 18
24
25
26
27
28
29
30
31
32 33
Sundstrom P, Wahlin A, Ambarki K, et al. Venous and cerebrospinal uid ow in multiple sclerosis: A casecontrol study. Ann Neurol 2010;68:255 9 Doepp F, Paul F, Valdeuza JM, et al. No cerebrocervical venous congestion in patients with multiple sclerosis. Ann Neurol 2010;68:173 83 Valdeuza JM, von Munster T, Hoffman O, et al. Postural dependency of the cerebral venous outow. Lancet 2000;355:200 1 Zamboni P. Iron-dependent inammation in venous disease and proposed parallels in multiple sclerosis. J R Soc Med 2006;99:589 93 Adams CW. Perivascular iron deposition and other vascular damage in multiple sclerosis. J Neurol Neurosurg Psychiatry 1988;51:260 5 Adams CW, Poston RN, Buk SJ. Pathology, histochemistry and immunocytochemistry of lesions in acute multiple sclerosis. J Neurol Sci 1989;92:291 306 Adams CW. Vascular aspects of multiple sclerosis. In: A Colour Atlas of Multiple Sclerosis and Other Myelin Disorders. London: Wolfe Medical Publication, 1989:184 7 Schelling F. Damaging venous reux into the skull or spine: relevance to multiple sclerosis. Med Hypotheses 1986;21:141 8 Talbert DG. Raised venous pressure as a factor in multiple sclerosis. Med Hypotheses 2008;70:1112 7 West JB, Tsukimoto K, Matheu-Costello O, Prediletto R. Stress failure in pulmonary capillaries. J Appl Physiol 1991;70:1731 42
34
35
36
37
38
39
40
41
Kurtzke JF. Rating neurological impairment in multiple sclerosis: an expanded disability scale (EDSS). Neurology 1983;33:1444 52 Cutter GR, Baier ML, Rudick RA, et al. Development of a multiple sclerosis functional composite as a clinical trial outcome measure. Brain 1999;122:871 82 Fisher JS, Rudick R, Cutter G, et al. The Multiple Sclerosis Functional Composite measure (MSFC): an integrated approach to MS clinical outcome assessment. Mult Scler 1999;5:244 50 Vickrey BG, Hays RD, Harooni R, et al. A health-related quality of life measure for multiple sclerosis. Qual Life Res 1995;4:187 206 Bermel RA, Fisher E, Cohen JA. The use of MR imaging as an outcome measure in multiple sclerosis clinical trials. Neuroimaging Clin N Am 2008;18:687 701 Zamboni P, Galeotti R, Weinstock-Guttman B, et al. Endovascular Treatment for Chronic Cerebrospinal Venous Insufciency in Multiple Sclerosis. A Longitudinal Pilot Study. Abstract Presented at the 22nd Annual Meeting American Venous Forum, Amelia Island, FL, February 1013, 2010 Malagoni AM, Galeotti R, Menegatti E, et al. Is chronic fatigue the symptom of venous insufciency associated with multiple sclerosis? A longitudinal pilot study. Int Angiol 2010;29:176 82 Plasmati R, Pastorelli F, Fini N, et al. Chronic cerebro-spinal venous insufciency: report of transcranial magnetic stimulation follow-up study in a patient with multiple sclerosis. Int Angiol 2010;29:189 92
Phlebology 2010;25:269279
279
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- South Neocon-2010: ConferenceДокумент11 страницSouth Neocon-2010: ConferenceMANJUNATHA SОценок пока нет
- William TДокумент7 страницWilliam Ttony_chrisОценок пока нет
- How Does Hypnosis WorkДокумент11 страницHow Does Hypnosis WorkchoileoОценок пока нет
- PONV Prophylaxis Guidelines: Risk Factor OR 95% CIДокумент4 страницыPONV Prophylaxis Guidelines: Risk Factor OR 95% CIHerly NurrahmaОценок пока нет
- Newborn ScreeningДокумент40 страницNewborn Screeningjosephabram051590Оценок пока нет
- Pediatric Schedule 3Документ12 страницPediatric Schedule 3Luis NepomucenoОценок пока нет
- MCQ On MeaslesДокумент27 страницMCQ On Measlesnikhil73% (11)
- Review Article UDC 616.8-009:616.31Документ7 страницReview Article UDC 616.8-009:616.31Bernarda MrakОценок пока нет
- FINAL Use and Application of Topical FluoridesДокумент7 страницFINAL Use and Application of Topical FluoridesmahmoudОценок пока нет
- SnuconeДокумент80 страницSnuconeimplantologyОценок пока нет
- Final Result of PG 2022 Special Stray Vacancy RounДокумент43 страницыFinal Result of PG 2022 Special Stray Vacancy Rounu19n6735Оценок пока нет
- APC Free Journal List External-Embargo-List - ElsevierДокумент47 страницAPC Free Journal List External-Embargo-List - ElsevierSYED ALI HUSSAINОценок пока нет
- APAAACI 2018 Delegate BrochureДокумент10 страницAPAAACI 2018 Delegate BrochureSuprapto WОценок пока нет
- Copy (2) of ThesisДокумент20 страницCopy (2) of Thesiscaridadlintao100% (1)
- The Significance of Surface PH in Chronic WoundsДокумент4 страницыThe Significance of Surface PH in Chronic WoundskixfrondaОценок пока нет
- 2017 Knox County Junior Cheerleading Registration FormДокумент2 страницы2017 Knox County Junior Cheerleading Registration FormJay MillerОценок пока нет
- Maternal Cardiovascular and Hemodynamic Adaptations To PregnancyДокумент13 страницMaternal Cardiovascular and Hemodynamic Adaptations To PregnancyAnchalia ChandrakumaranОценок пока нет
- Membership of The Royal College of PhysiciansДокумент3 страницыMembership of The Royal College of PhysiciansMatin Ahmad KhanОценок пока нет
- The New FIGO Staging SystemДокумент4 страницыThe New FIGO Staging Systemcraniophage95Оценок пока нет
- Tissue Engineering CWK 1Документ16 страницTissue Engineering CWK 1skc_b37851Оценок пока нет
- Dka GuidelineДокумент16 страницDka GuidelineGhada HusseinОценок пока нет
- CTGДокумент11 страницCTGMustafa Abd-Al SahibОценок пока нет
- Monteggia FractureДокумент11 страницMonteggia FractureRonald Ivan WijayaОценок пока нет
- A Double-Plating Approach To Distal Femur Fracture. INJURY2017Документ6 страницA Double-Plating Approach To Distal Femur Fracture. INJURY2017Eduardo Gonzalez100% (1)
- Ioracon 2011 Write UpДокумент6 страницIoracon 2011 Write Upzorodocknife7354Оценок пока нет
- Endometriosis Classification An UpdateДокумент8 страницEndometriosis Classification An UpdateZurya UdayanaОценок пока нет
- Headache Orofacial Pain and Bruxism - Selvaratnam PDFДокумент377 страницHeadache Orofacial Pain and Bruxism - Selvaratnam PDFLukas100% (1)
- ChattisgarhДокумент43 страницыChattisgarhNILOFAR RAWANIОценок пока нет
- Medical Gas Design Guide Chapter 6 - Medical Vacuum (Suction)Документ226 страницMedical Gas Design Guide Chapter 6 - Medical Vacuum (Suction)jhonacostaОценок пока нет
- LamotrigineДокумент109 страницLamotriginemunzirОценок пока нет