Академический Документы
Профессиональный Документы
Культура Документы
Multidrug-Resistant Tuberculosis (MDR-TB) Is Defined As TB That Is Resistant To Both
Загружено:
sanny_sundariИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Multidrug-Resistant Tuberculosis (MDR-TB) Is Defined As TB That Is Resistant To Both
Загружено:
sanny_sundariАвторское право:
Доступные форматы
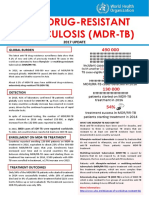
Defining MDR- and XDR-TB
Multidrug-resistant tuberculosis (MDR-TB) is defined as TB that is resistant to both isoniazid [INH] and rifampicin [RMP], two of the first-line drugs used in treating smearpositive pulmonary tuberculosis. Extensively drug-resistant tuberculosis (XDR-TB) is defined by the WHO as MDR-TB with additional resistance to any fluoroquinolone (FQ) and to at least one of three injectable second-line anti-tuberculosis drugs used in treatment (capreomycin [CPM], kanamycin [KM] or amikacin [AMK]).
Some 440,000 cases of multidrug-resistant tuberculosis (MDR-TB) are identified each year, causing at least 150,000 deaths from a disease that should be curable. Extensively drugresistant TB, which has an even higher fatality rate, has now been reported in more than 65 countries.
Drug-resistant TB is the end result of a number of different failures, each of which, on its own, is solvable with existing tools. The Union offers technical assistance in MDR-TB in the field to more than 15 countries yearly and has developed a package, including this technical assistance, training and research to support countries in implementing and developing an MDR-TB project. To address all of the issues and stop the spread of this disease requires a comprehensive, multi-pronged strategy, such as The Union has developed.
When TB is misdiagnosed or the treatment is poorly managed, the doors open to drug resistance.
Consequently training for people at every level of the health care system is central to The Union's approach. More than 300 people including physicians from 35 countries participated in MDR-TB training offered by The Union in 2010. These international and national courses in English, French or Spanish train clinicians to manage MDR-TB cases and cover questions ranging from logistics and procurement to ethics and human rights.
Patients who do not correctly take the medicines required to complete their TB treatment are at high risk for developing drug-resistant tuberculosis and passing on these new strains.
Strong programmes for case detection, diagnosis and patient monitoring are all critical to avoid this scenario. At the request of an NTP, The Union helps review plans, procedures, policies and systems and makes suggestions for improvement. In recognition of the pivotal role of laboratories in diagnosing and monitoring drug-resistant strains of the disease, The Union has also helped develop an international network of TB reference laboratories.
Use of poor quality medicines and drug shortages are also leading causes of drug-resistant TB.
If the quality of first-line TB drugs is not assured or the supply is not adequate to meet the needs of those in treatment patients will not be cured and may develop MDR-TB. They will then require treatment with the more expensive second-line drugs (SLD). The Union works closely with NTPs to support them in the implementation of best practices for ordering, storing and distributing medicines, as well as to assure the quality of the medicines selected for national procurement and to monitor their quality.
Treating drug-resistant TB is much more expensive and can take up to two years creating a strain on both patients and health systems.
Through its operational research and clinical trials programmes, The Union continually seeks new solutions to issues of prevention, treatment and control. The Union also collaborates with international working groups, such as the Green Light Committee, and publishes recommendations on these issues.
Multidrug-Resistant Tuberculosis (MDR TB) Fact Sheet
February 2010 Multidrug-resistant tuberculosis (MDR TB) is a form of tuberculosis that is resistant to two or more of the primary drugs (isoniazied and rifampin) used for the treatment of tuberculosis. Extensively drug-resistant TB (XDR TB) is TB resistant to at least isoniazied and rifampin among the first-line anti-TB drugs and is resistant to any fluoroquinolone and at least one of the three second-line injectable drugs.1 Resistance to one or several forms of treatment occurs when the bacteria develops the ability to withstand antibiotic attack and relays that ability to its offspring. Since that entire strain of bacteria inherits this capacity to resist the effects of the various treatments, resistance can spread from one person to another. On an individual basis, however, inadequate treatment or improper use of the anti-tuberculosis medications remains an important cause of drug-resistant tuberculosis. Drug-resistant TB is difficult and costly to treat and can be fatal.
In 2008, the CDC reported that 8.2 percent of tuberculosis cases in the U.S. were resistant to isoniazid, the first-line drug used to treat TB.2 The CDC also reported that 1.0 percent of tuberculosis cases in the U.S. were resistant to both isoniazid and rifampin.3 Rifampin is the drug most commonly used with isoniazid. Overall, 125 cases of MDR TB cases were reported in 2007, which was an increase from the 116 cases reported in 2006.4 Only 18.4 percent of primary MDR TB cases were in U.S. born persons in 2007. The proportion of MDR TB cases continues to disproportionately affect foreign-born persons in the United States. This group accounted for 26 percent of MDR TB cases in 1993, but 81.6 percent of such cases in 2007.5 The World Health Organization estimates that there were half a million cases of MDR TB worldwide in 2007, the highest ever reported. These cases are not spread proportionately across the globe, as only 27 countries account for 85 percent of all MDR TB cases. Unfortunately, only a small portion of MDR TB cases are treated properly each year; about 1 percent (3,700) in 2007.6 A strain of MDR TB originally develops when a case of drug-susceptible tuberculosis is improperly or incompletely treated. This occurs when a physician does not prescribe proper treatment regimens or when a patient is unable to adhere to therapy. Improper treatment
allows individual TB bacilli that have natural resistance to a drug to multiply. Eventually the majority of bacilli in the body are resistant.7 Once a strain of MDR TB develops it can be transmitted to others just like a normal drugsusceptible strain. Airborne transmission has been the cause of several well-publicized cases of nosocomial (hospital-based) outbreaks of MDR TB in New York City and Florida. These outbreaks were responsible for the deaths of several patients and health care workers, a majority of whom were coinfected with HIV.8 MDR TB has been a particular concern among HIV-infected persons. Some of the factors that have contributed to the number of cases of MDR TB, both in general and among HIVinfected individuals are: 1. Delayed diagnosis and delayed determination of drug susceptibility, which may take several weeks 2. Susceptibility of immunosuppressed individuals for not only acquiring MDR TB but for rapid disease progression, which may result in rapid transmission of the disease to other immunosuppressed patients 3. Inadequate respiratory isolation procedures and other environmental safety conditions, especially in confined areas such as prisons 4. Noncompliance or intermittent compliance with antituberculosis drug therapy.9 MDR TB is more difficult to treat than drug-susceptible strains of TB. The success of treatment depends upon how quickly a case of TB is identified as drug resistant and whether an effective drug therapy is available. The second-line drugs used in cases of MDR TB are often less effective and more likely to cause side effects.10 Tests to determine the resistance of a particular strain to various drugs usually take several weeks to complete. During the delay, the patient may be treated with a drug regimen that is ineffective. Once a strain's drug resistance is known, an effective drug regimen must be identified and begun. Some strains of MDR TB are resistant to seven or more drugs, making the identification of effective drugs difficult. To deal with this problem, it is recommended that newly discovered cases of TB in populations at high risk for MDR TB be treated with four drugs rather than the standard three as part of initial treatment.11 Treatment for MDR TB involves drug therapy over many months or years. Despite the longer course of treatment, the cure rate decreases from over 90 percent for nonresistant strains of TB to 50 percent or less for MDR TB.12 Because it is difficult for some people to successfully complete their tuberculosis treatment, several innovations have been developed. One of these is the use of incentives and enablers, which may be transportation, tokens or food coupons that are given to patients each time they appear at the clinic or doctor's office for treatment. Incentives and enablers are combined with the use of directly observed therapy (DOT). DOT is a system of treatment in which the patient is administered his or her medication by a nurse or other health worker and observed taking the medication.13 FDA has approved Rifater, a medication that combines the three main drugs (isoniazid, rifampin, and pyrazinamide) used to treat tuberculosis into one pill. This reduces the number of pills a patient has to take each day and makes it impossible for the patient to take only one of the three medications, a common path to the development of MDR TB.14 In 2006, a study in Africa revealed the presence of not only multidrug-resistant (MDR) tuberculosis but also what is now known as extensively drug-resistant (XDR) tuberculosis in patients infected with HIV. The Centers for Disease Control and Prevention and the World Health Organization reported the existence of XDR TB in 17 countries, including 4 percent of cases here in the United States.15
For more information on tuberculosis, please review the Tuberculosis Morbidity and Mortality Trend Report in the Data and Statistics section of our website at www.lung.org or call the American Lung Association at 1-800-LUNG-USA (1-800-586-4872).
Вам также может понравиться
- Biology Project On TBДокумент20 страницBiology Project On TBAdnan Fazeel73% (15)
- Mantoux Test: Pirquet Test, or PPD Test For Purified Protein Derivative) Is A Diagnostic Tool ForДокумент5 страницMantoux Test: Pirquet Test, or PPD Test For Purified Protein Derivative) Is A Diagnostic Tool ForGurmeet SinghОценок пока нет
- Medical MCQ Center - Tuberculosis MCQsДокумент4 страницыMedical MCQ Center - Tuberculosis MCQsnarendrakumar9450% (2)
- Ga TB Test Form OscarДокумент1 страницаGa TB Test Form OscarWilliamОценок пока нет
- What Is Multidrug-Resistant Tuberculosis (MDR-TB) and How Do We Control It?Документ2 страницыWhat Is Multidrug-Resistant Tuberculosis (MDR-TB) and How Do We Control It?Dvica SarahОценок пока нет
- WHO Bulletin 2005Документ10 страницWHO Bulletin 2005ajh2675Оценок пока нет
- Baluchestan ProvinceДокумент9 страницBaluchestan ProvinceVincentius Michael WilliantoОценок пока нет
- JH 08003Документ8 страницJH 08003Nur Afni PonsengОценок пока нет
- MDR TB FactsheetДокумент2 страницыMDR TB FactsheetfaradillaОценок пока нет
- Contemporary Data On TB Epidemiology by Nwokotubo Beulah 2Документ26 страницContemporary Data On TB Epidemiology by Nwokotubo Beulah 2Beulah AlexОценок пока нет
- Multi Drug ResistenДокумент2 страницыMulti Drug ResistenNurul W.AОценок пока нет
- Burden of Tuberculosis - Combating Drug Resistance: EditorialДокумент3 страницыBurden of Tuberculosis - Combating Drug Resistance: EditorialmominamalikОценок пока нет
- Molecular AnalysisДокумент29 страницMolecular AnalysisBaranishankarОценок пока нет
- jh08003 PDFДокумент8 страницjh08003 PDFkiranaОценок пока нет
- Case Study For TuberculosisДокумент7 страницCase Study For TuberculosisGabbii CincoОценок пока нет
- MDRTB Case StudyДокумент35 страницMDRTB Case StudyFejlean Angelica AntineoОценок пока нет
- Multi-Drug-Resistant Tuberculosis (MDR-TB) Is Defined: EpidemiologyДокумент3 страницыMulti-Drug-Resistant Tuberculosis (MDR-TB) Is Defined: EpidemiologyJhemar Handa JulhamidОценок пока нет
- Mutidrug Resistant TuberculosisДокумент2 страницыMutidrug Resistant Tuberculosistummalapalli venkateswara raoОценок пока нет
- BY Dr. Tahmina AzharДокумент71 страницаBY Dr. Tahmina Azharscribdnotes123Оценок пока нет
- Surveillance Evaluation Report of Tuberculosis in District Bhawalpur-2018 by DR Ammara TahirДокумент22 страницыSurveillance Evaluation Report of Tuberculosis in District Bhawalpur-2018 by DR Ammara TahirSantosh WadhwaniОценок пока нет
- Multi-Drug-resistant Tuberculosis - Wikipedia, The Free EncyclopediaДокумент8 страницMulti-Drug-resistant Tuberculosis - Wikipedia, The Free Encyclopedianayan555Оценок пока нет
- Akurit 4 TBДокумент14 страницAkurit 4 TBNicolloОценок пока нет
- Prevalence of Rifampicin Resistance Tuberculosis and Associated Factors Among Presumptive TB or MDRДокумент3 страницыPrevalence of Rifampicin Resistance Tuberculosis and Associated Factors Among Presumptive TB or MDRTigray OutlookОценок пока нет
- Overview of Tuberculosis-WithNotesДокумент26 страницOverview of Tuberculosis-WithNotesivanradosinavicОценок пока нет
- Tuberculosis: WHO Global Tuberculosis Report 2014Документ2 страницыTuberculosis: WHO Global Tuberculosis Report 2014blueicelandОценок пока нет
- Tuberculosis: Key FactsДокумент5 страницTuberculosis: Key FactsIdris IkhsanОценок пока нет
- Antimicrobial ResistanceДокумент9 страницAntimicrobial Resistancesattyadev95Оценок пока нет
- Research On Prevalence of TB FinalДокумент9 страницResearch On Prevalence of TB FinalBontuОценок пока нет
- TUBERCULOSISДокумент4 страницыTUBERCULOSISLâm NguyễnОценок пока нет
- Diagnosis & Treatment of Tuberculosis in HIV Co-Infected PatientsДокумент16 страницDiagnosis & Treatment of Tuberculosis in HIV Co-Infected PatientsdevisilalahiОценок пока нет
- No 2Документ6 страницNo 2Raven RavenОценок пока нет
- 411 TB FactsheetДокумент54 страницы411 TB FactsheetKimberly SebekОценок пока нет
- 1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1Документ9 страниц1201 Sanchez Padilla High Prevalence of Multidrug Resistant Tuberculosis Swaziland 2009 2010 Emerging Infectious Diseases 18 1dewi ayu wulandariОценок пока нет
- Multi Drug Resistant TBДокумент28 страницMulti Drug Resistant TBmedeviОценок пока нет
- Tuberculosis Strains, It Continues To Be One of The Diseases With High Mortality RatesДокумент40 страницTuberculosis Strains, It Continues To Be One of The Diseases With High Mortality RatesNikki GarlejoОценок пока нет
- Zhang 2015Документ15 страницZhang 2015Annisa Nurfiatul AiniОценок пока нет
- TuberculosisДокумент6 страницTuberculosisANGELINE CHRYSTABELОценок пока нет
- Drug Resistance of TBДокумент17 страницDrug Resistance of TBGaurav Sharma100% (1)
- WHO Antimicrobial ResistanceДокумент4 страницыWHO Antimicrobial ResistanceDesalegnОценок пока нет
- Vol 42 No 13-EnglishДокумент4 страницыVol 42 No 13-EnglishVijayakanth VijayakumarОценок пока нет
- Linezolid To Treat MDR-/XDR-tuberculosis: Available Evidence and Future ScenariosДокумент5 страницLinezolid To Treat MDR-/XDR-tuberculosis: Available Evidence and Future ScenariosNop PiromОценок пока нет
- Clinical Case of Multidrug-Resistant in King Khalid Hospital, HailДокумент2 страницыClinical Case of Multidrug-Resistant in King Khalid Hospital, HailryoОценок пока нет
- Non-Tuberculosis Mycobacterial Pulmonary Disease (NTM)Документ1 страницаNon-Tuberculosis Mycobacterial Pulmonary Disease (NTM)readyboy89Оценок пока нет
- Disease Is Reduced. The Level of Herd Immunity May Vary With DiseasesДокумент2 страницыDisease Is Reduced. The Level of Herd Immunity May Vary With DiseasesPattyОценок пока нет
- Antimicrobial ResistanceДокумент9 страницAntimicrobial Resistancekzqwrpp484Оценок пока нет
- TheUnion DR TB GuideДокумент2 страницыTheUnion DR TB GuideDhani KurniawanОценок пока нет
- First-Line Anti-Tuberculosis Drug Resistance Pattern: Original ArticleДокумент6 страницFirst-Line Anti-Tuberculosis Drug Resistance Pattern: Original ArticleyasserОценок пока нет
- Survival Status and Treatment Outcome ofДокумент6 страницSurvival Status and Treatment Outcome ofEghar EverydayishellОценок пока нет
- Classification of Drug-Resistant Tuberculosis in An Epidemic AreaДокумент4 страницыClassification of Drug-Resistant Tuberculosis in An Epidemic AreaTika Dwi TamaОценок пока нет
- 1 s2.0 S1198743X16303639 Main PDFДокумент7 страниц1 s2.0 S1198743X16303639 Main PDFMuhammad Addinul HudaОценок пока нет
- Long Walk TBДокумент3 страницыLong Walk TBdellanurainiОценок пока нет
- Scientific BriefДокумент3 страницыScientific BriefRose Virginie Coo GowaОценок пока нет
- TB Elimination: Extensively Drug-Resistant Tuberculosis (XDR TB)Документ3 страницыTB Elimination: Extensively Drug-Resistant Tuberculosis (XDR TB)Hardi CahyantaОценок пока нет
- TuberculosisДокумент4 страницыTuberculosisDr Mangesti Utami PKM Kebaman BanyuwangiОценок пока нет
- What Is Multidrug-Resistant Tuberculosis (MDR-TB) ?Документ63 страницыWhat Is Multidrug-Resistant Tuberculosis (MDR-TB) ?Birhanu AbebeОценок пока нет
- Tuberculosis: Novel Approaches To An Old Disease: EditorialДокумент3 страницыTuberculosis: Novel Approaches To An Old Disease: EditorialYet Barreda BasbasОценок пока нет
- Multidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceДокумент7 страницMultidrug-Resistant Tuberculosis in Children: Evidence From Global SurveillanceAldy RinaldiОценок пока нет
- Prevention and Containment of Antimicrobial Resistance: Sixty-Third Session Bangkok, Thailand 7-10 September 2010Документ17 страницPrevention and Containment of Antimicrobial Resistance: Sixty-Third Session Bangkok, Thailand 7-10 September 2010gabriela_mariangela5929Оценок пока нет
- Palliative and End-Of-Life Care in The Global Response To Multidrug-Resistant TuberculosisДокумент7 страницPalliative and End-Of-Life Care in The Global Response To Multidrug-Resistant TuberculosisSausan ZakiyahОценок пока нет
- Drug-Resistant TB: Deadly, Costly and in Need of A VaccineДокумент6 страницDrug-Resistant TB: Deadly, Costly and in Need of A VaccineSorina ElenaОценок пока нет
- Experimental 11Документ5 страницExperimental 11parmar jalpabenОценок пока нет
- Reviews: Etiology and Management of Genitourinary TuberculosisДокумент11 страницReviews: Etiology and Management of Genitourinary TuberculosisAnderson SousaОценок пока нет
- Research Paper On MDR TBДокумент6 страницResearch Paper On MDR TBgz8qs4dn100% (1)
- Pulmonary Tuberculosis: Anindya .L. Sidarta 03.011.034Документ19 страницPulmonary Tuberculosis: Anindya .L. Sidarta 03.011.034Anindya SidartaОценок пока нет
- RNTCPДокумент24 страницыRNTCPmohanpskohli8310Оценок пока нет
- Emergence of MDR-TBДокумент18 страницEmergence of MDR-TBAmor SantiagoОценок пока нет
- Curs 14 Boala Lyme 2Документ63 страницыCurs 14 Boala Lyme 2n1u1s1h1100% (1)
- Cutaneous TBДокумент45 страницCutaneous TBWarren Lie100% (1)
- Drug Import-LinezolidДокумент13 страницDrug Import-LinezolidShantanu MannaОценок пока нет
- Chapter 2: Transmission and Pathogenesis of TuberculosisДокумент26 страницChapter 2: Transmission and Pathogenesis of TuberculosisMajd Ahmad Abdel RahimОценок пока нет
- RNTCP - Wikipedia, The Free EncyclopediaДокумент5 страницRNTCP - Wikipedia, The Free EncyclopediaakurilОценок пока нет
- Overview Rujukan Horizontal TB SD Okt 22Документ10 страницOverview Rujukan Horizontal TB SD Okt 22Meriya Whuland NugrohoОценок пока нет
- Pedoman Nasional Pengendalian TuberkulosisДокумент111 страницPedoman Nasional Pengendalian TuberkulosisYusriОценок пока нет
- 2020newskin - Ex-US MGIT Trifold Print VersionДокумент6 страниц2020newskin - Ex-US MGIT Trifold Print Versionrofi husaeni fahmiОценок пока нет
- Proposal FiadetaДокумент4 страницыProposal Fiadetajose suni100% (1)
- Faktor Resiko TB ParuДокумент7 страницFaktor Resiko TB ParurivaindragiriОценок пока нет
- Panduan Penanggulangan TBДокумент132 страницыPanduan Penanggulangan TBice mayasopaОценок пока нет
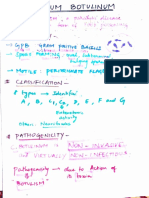
- Clostridium Botulinum MT29Документ5 страницClostridium Botulinum MT29Game GameОценок пока нет
- Dr. Cahyarini - Ppi TB RSP KarsДокумент44 страницыDr. Cahyarini - Ppi TB RSP KarsMohammad SutamiОценок пока нет
- Tuberculosis Treatment: General Principles and ApproachДокумент24 страницыTuberculosis Treatment: General Principles and ApproachRahul PatilОценок пока нет
- Faktor Faktor Yang Mempengaruhi Kejadian TB Paru Dan Upaya Penanggulangannya - Edza Aria Wikurendra, S.KL, M.KL PDFДокумент12 страницFaktor Faktor Yang Mempengaruhi Kejadian TB Paru Dan Upaya Penanggulangannya - Edza Aria Wikurendra, S.KL, M.KL PDFsalsa nОценок пока нет
- Yersinia Pestis: (Great Bubonic Plague)Документ11 страницYersinia Pestis: (Great Bubonic Plague)Andy RosseОценок пока нет
- Jenis Pelayanan L P Jumlah: Program TBДокумент1 страницаJenis Pelayanan L P Jumlah: Program TBFirani AmazonaОценок пока нет
- Peran Pengawas Minum Obat (Pmo) Dalam Keberhasilan Pengobatan Tuberculosis Paru Di Masyarakat (The Role of Direct Observed Treatment in Tuberculosis Treatment Successful at Comm...Документ7 страницPeran Pengawas Minum Obat (Pmo) Dalam Keberhasilan Pengobatan Tuberculosis Paru Di Masyarakat (The Role of Direct Observed Treatment in Tuberculosis Treatment Successful at Comm...petrayohanaОценок пока нет
- Vibrio CholeraeДокумент20 страницVibrio CholeraeChockalingam MeenakshisundaramОценок пока нет
- Data Pasien TB JuliДокумент42 страницыData Pasien TB JuliTsubbatun NajahОценок пока нет
- Laporan Kegiatan Packing Dan Pengantaran Sampel TCM Ke Puskesmas Temindung TAHUN 2022Документ6 страницLaporan Kegiatan Packing Dan Pengantaran Sampel TCM Ke Puskesmas Temindung TAHUN 2022Leha SabrinaОценок пока нет
- Similarity - An Evaluation of Chest X-Ray in The Context of Community-Based Screening of Child Tuberculosis ContactsДокумент17 страницSimilarity - An Evaluation of Chest X-Ray in The Context of Community-Based Screening of Child Tuberculosis ContactsIntan HartandyОценок пока нет
- National Tuberculosis ProgramДокумент37 страницNational Tuberculosis ProgramDon Oliveros ÜОценок пока нет