Академический Документы
Профессиональный Документы
Культура Документы
Veterinary Pathology Online: Equine Viral Arteritis
Загружено:
meawchiИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Veterinary Pathology Online: Equine Viral Arteritis
Загружено:
meawchiАвторское право:
Доступные форматы
Veterinary Pathology Online
http://vet.sagepub.com/ Equine Viral Arteritis
F. Del Piero Vet Pathol 2000 37: 287 DOI: 10.1354/vp.37-4-287 The online version of this article can be found at: http://vet.sagepub.com/content/37/4/287
Published by:
http://www.sagepublications.com
On behalf of:
American College of Veterinary Pathologists, European College of Veterinary Pathologists, & the Japanese College of Veterinary Pathologists.
Additional services and information for Veterinary Pathology Online can be found at: Email Alerts: http://vet.sagepub.com/cgi/alerts Subscriptions: http://vet.sagepub.com/subscriptions Reprints: http://www.sagepub.com/journalsReprints.nav Permissions: http://www.sagepub.com/journalsPermissions.nav
>> Version of Record - Jul 1, 2000 What is This?
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
Vet Pathol 37:287296 (2000)
REVIEW ARTICLE Equine Viral Arteritis
F. DEL PIERO
Department of Pathobiology, School of Veterinary Medicine, University of Pennsylvania, New Bolton Center, Kennett Square, PA Abstract. Equine viral arteritis (EVA) can cause prominent economic losses for the equine industry. The purpose of this review is to provide the pathologist some familiarity with the clinical history, lesions, pathogenesis, and diagnosis of EVA. EVA is caused by an arterivirus (equine arteritis virus, EAV), and the vascular system is the principal but not unique viral target. EVA has variable presentations, including interstitial pneumonia, panvasculitis with edema, thrombosis and hemorrhage, lymphoid necrosis, renal tubular necrosis, abortion, and inammation of male accessory genital glands. EAV antigen (EAVAg) can be demonstrated within the cytoplasm of epithelial cells such as alveolar pneumocytes, enterocytes, adrenal cortical cells, trophoblasts, thymus stroma, renal tubular cells, and male accessory genital gland cells. It can be also demonstrated within endothelia, in vascular, myometrial, and cardiac myocytes, macrophages, dendritelike cells of lymphoid organs, and chorionic mesenchymal stromal cells. In young and adult horses, following colonization of macrophages, the virus spreads systemically using circulating monocytes and enters the endothelium and tunica media of blood vessels, histiocytes, and dendritelike cells. Eventually, the virus multiplies within renal tubular cells. Lesions are uncommon in the aborted fetus; if present, they are mild, and EAVAg is frequently not detectable within fetal tissues and placenta. The clinical presentation and lesions of EVA may resemble those of other diseases. Complete pathologic examination associated with immunohistochemistry, virus isolation, and, especially in cases of abortion, serology will guarantee a directed and accurate diagnosis. Key words: Abortion; arterivirus; equine viral arteritis; nephritis; panvasculitis; pneumonia.
Equine viral arteritis (EVA) is a global infectious disease of horses and is characterized by panvasculitis inducing edema, hemorrhage, and abortion in pregnant mares.15,16,27 EVA can cause severe economic losses for the equine industry. The purpose of this review is to provide the pathologist some familiarity with the clinical history, lesions, pathogenesis, and diagnosis of EVA. EVA can be confused with other equine diseases and must be considered in sporadic and epizootic respiratory syndromes, foal death associated with respiratory and/or enteric signs, or sudden death in foals. Although not frequent, velogenic isolates of equine arteritis virus (EAV) can induce severe and fatal disease in adults. Natural outbreaks of EVA characterized by transient clinical signs and abortion in pregnant mares contrast with experimental disease, which features high mortality and prominent systemic vascular necrosis. Blood vessel cells are the major, but not exclusive, target of EAV. Lung, intestine, kidney, the reproductive tract, and occasionally the placenta are important viral replication sites, which favor the spread of the virus. Complete pathologic examination associated with the available ancillary procedures will help guarantee a directed and accurate diagnosis.
The Virus EAV is an enveloped, spherical, positive-stranded RNA virus with a diameter of 5070 nm. The virion is comprised of an isometric core surrounded by a lipid-containing envelope from which delicate spikes protrude. The viral genomic RNA, which is encapsulated by a single nucleocapsid protein, is contained within the core particle. Within the viral envelope at least three integral membrane proteins are incorporated. EAV is a non-arthropod-borne virus classied as a member of the new order Nidovirales, including also the bigeneric family Coronaviridae, within the family Arteriviridae with porcine respiratory and reproductive syndrome virus, simian hemorrhagic fever virus, and lactate dehydrogenase elevating virus.5,14 Genetically, EAV is similar to coronaviruses but has a dissimilar viral structure and a complement-xing antigen but no hemagglutinins.6 Genetic diversity is recognized among eld isolates.1 EAV was rst isolated from fetal lung collected during an epizootic of abortion in Bucyrus, Ohio (USA).4,16 In Bucyrus, horses of both sexes and various age groups experienced an acute and febrile infectious disease charac-
287
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
288
Del Piero
Vet Pathol 37:4, 2000
terized by mucopurulent rhinitis, stiffness, depression, and edema of conjunctiva and limbs.9,15 The virus was isolated on primary kidney cells.15 Only one strain of EAV is recognized, the Bucyrus strain; however, various isolates have different degrees of virulence.39 Clinical Features and Carrier State Clinical signs may be absent or may include pyrexia, depression, anorexia, leukopenia, limb edema, stiffness of gait, rhynorrhea and epiphora, conjunctivitis, and rhinitis. Edema of the periorbital and supraorbital areas, midventral regions, scrotum, prepuce, and mammary gland, urticarial rash, and abortion also occur. Less frequently, severe respiratory distress, ataxia, mucosal papular eruptions, submaxillary lymphadenopathy, and intermandibular and shoulder edema may be observed.52,55 EAV can be associated with epidemic abortion,8,51,52 is occasionally fatal in adults,35,47 and more frequently can be fatal for foals.13,18,21,54,56 When neonates are not protected by passive maternal immunity, they may present with sudden death or severe respiratory distress followed by death.55 Affected intact males may become long-term carriers and may shed EAV in the semen.53 Stallions shedding EAV in their semen serve as a reservoir for the virus within the equine population. Additionally, infected stallions and semen have resulted in restrictions for international movement of horses and semen. Clinical Pathology
Clinical laboratory results and serology
characterized by dyspnea, tachypnea, hypoxemia, and hypercapnia. The condition in this foal was initially reported in the literature as a case of bronchopulmonary dysplasia.18 Subsequent reanalysis of the case revealed that the foal was infected with EAV, and a correction was published.13,56 Cytologic abnormalities in bronchoalveolar lavage and tracheal aspirate reported for this foal included formed fragments of granular material, mucus, brin, a few small macrophages, and epithelial cells demonstrating cilia loss with retention of a prominent terminal bar and squamous metaplasia. In addition, there were papillary clusters of squamoid or cuboidal cells with focal loss of cilia. These cytologic ndings corresponded to proliferative bronchointerstitial pneumonia with intraalveolar macrophages and a few neutrophils, brin and hyaline membrane formation, type 2 pneumocytic hypertrophy, and hyperplasia. Most foals with EVA die without cytologic evaluation of tracheal and bronchial aspirates. This case is the only one with such an evaluation and likely represents ndings in severe cases. Because the EAV pulmonary antigen is not as abundant as the antigen in EHV-1 infection,10,11,41 its identication within the cytologic specimens may be difcult. However, renal tubular necrosis occurring during the late phase of the EAV infection is associated with orid intraepithelial intracytoplasmic viral growth,13,15 making the urine sample a potential candidate for in vivo immunocytochemical testing. In addition to buffy coat and rhinopharyngeal swab, part of the uid obtained with the tracheal lavage and urine should be submitted for ancillary virologic testing. Anatomic Pathology EAV-associated gross and histologic lesions have been described in naturally infected13,18,21,27,35,45,47,54,56 and experimentally infected7,15,17,22,36,39,45 equids. The EAV isolates differ in virulence and consequently induce lesions that differ in severity.39 EAV antigen (EAVAg) can be identied in various tissues and organs either associated with lesions or occasionally in the absence of them.9,13,35,36,56 EAVAg can be identied within the cytoplasm of the infected cell using equine polyclonal9 and murine monoclonal35 antibodies in fresh and xed tissues.
Gross lesions
Clinical pathology ndings reported in affected foals include hypoxia, hypercapnia, respiratory acidosis sometimes complicated by metabolic acidosis, neutropenia/neutrophilia, lymphopenia/lymphocytosis, thrombocytopenia, and hyperbrinogenemia.13,18,54,56 However, abnormal values may be inconsistent, are highly variable, and are not diagnostic for EVA. Arterial blood gas values in affected foals are diagnostic of severe disease of the respiratory system, but these abnormalities may be seen in a variety of neonatal diseases of horses, including bacterial sepsis and other viral diseases such as equine herpesvirus 1 (EHV-1) infection. In one report,4 experimentally infected mature horses were consistently leukopenic. The horses in this study presented with a biphasic leukopenia and neutropenia. Lymphopenia was consistently present postinfection (PI) in this group of experimentally infected horses.
Cytology
Cytology of pulmonary washings has been described in one foal with severe pulmonary disease
Gross lesions are the expression of the vascular pathologic changes. Edema, congestion, and hemorrhage of the subcutaneous tissues, lymph nodes, and viscera are the most frequent gross lesions in horses that die after natural or experimental EAV infection (Fig. 1). The body cavities may contain moderate to abundant amounts of yellowish clear exudate. Congestion and lymphadenomegaly, edema, and hemor-
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
Vet Pathol 37:4, 2000
Equine Viral Arteritis
289
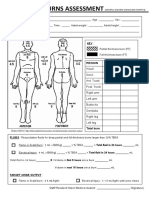
Fig. 1. Lung, liver, and stomach; foal with EVA. Severe and diffuse edema of lung, Glisson hepatic capsule, and gastric mucosa, with petechiae. Bar 8 cm. (Courtesy of J. M. King, Department of Pathology, College of Veterinary Medicine, Cornell University, Ithaca, NY.) Fig. 2. Small muscular artery; foal with EVA. Fibrinoid necrosis of the tunica media and perivascular edema with lymphocytic inltrate. HE. Bar 80 m. Fig. 3. Lung; foal with EVA. Interstitial pneumonia with hypertrophied type 2 pneumocytes containing intracytoplasmic EAV antigen. Hematoxylin and avidinbiotin immunoperoxidase. Bar 20 m. Fig. 4. Small muscular artery; foal with EVA. Vascular intimal and medial necrosis with perivascular lymphocytic inltrate and edema. EAV antigen is diffusing from the endothelium to the tunica media. Hematoxylin and avidinbiotin immunoperoxidase. Bar 120 m. Fig. 5. Kidney; mare with EVA. Severe diffuse interstitial lymphocytic nephritis with tubular necrosis and abundant EAV antigen contained in renal tubules and intraluminal casts. Hematoxylin and avidinbiotin immunoperoxidase. Bar 300 m. Fig. 6. Chorioallantois; equine fetus with EVA. A syncytial trophoblast cell contains abundant intracytoplasmic EAV antigen. Hematoxylin and avidinbiotin immunoperoxidase. Bar 25 m.
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
290
Del Piero
Vet Pathol 37:4, 2000
rhages can be observed along the course of the colonic and cecal vessels but also are evident systemically. On the cut surface of lymph nodes, there may be a prominent subcapsular sinus and dilated medullary sinuses. Lungs, especially those of infected neonates (Fig. 1), are wet and increased in weight, with a prominent lobular pattern. The trachea may contain froth. On occasion, lungs can be multifocally or diffusely reddish because of congestion and hemorrhage. The uterine endometrial surface of aborting mares may be swollen and diffusely congested, sometimes with hemorrhages.
Microscopic lesions
The histologic lesions are observed in various systems of horses with EAV infection. The blood vessels are the principal target. Blood vessels. All organs, including the skin, may contain vascular changes. Mild lesions include vascular and perivascular edema with occasional lymphocytic inltrate and endothelial cell hypertrophy. Severe changes include vasculitis with brinoid necrosis of the tunica media, abundant vascular and perivascular lymphocytic and lesser granulocytic inltration (Fig. 2) with karyorrhexis, frequent loss of endothelium, and formation of large brinocellular stratied thrombi. Occasionally, vascular portal vasculitis consists of severe inammatory cell inltrate that erodes the hepatocellular periportal limiting plate. Within vessels, EAVAg localizes in endothelium, medial myocytes (Fig. 4), and pericytes. Marginating macrophages containing intracytoplasmic EAVAg may be seen, occasionally associated with infected endothelial cells. Rarely, cardiac vasculitis with myocyte necrosis and associated EAVAg can be observed. Ultrastructurally,17 infected endothelial cells appear hypertrophied, with expansion of cytoplasmic matrix in the absence of increased cytoplasmic organelles. Endoplasmic cisternae are distended, and mitochondria are increased in volume and their cristae are affected by degenerative changes. Specic cytoplasmic alterations associated with viral colonization of endothelial cells include dense crystalloid viral particles contained within endoplasmic cysternae and membranes of endoplasmic reticulum and vacuoles containing virions. These viral particles average 58 nm in diameter and are characterized by a 25-nm core and a less dense external membrane. Capillary lumina are often obliterated by swollen endothelial cells, platelet thrombi, or neutrophils. The nervous system is generally not affected, although cerebral vascular necrosis has been reported in fetuses. Lungs. Lungs may be affected by mild to severe interstitial pneumonia (Figs. 1, 3) characterized by alveolar inltration with macrophages and lesser numbers of neutrophils, hyaline membrane formation, and
uid-lled alveoli. There is hypertrophy and hyperplasia of alveolar pneumocytes, which become rounded with a vesicular nucleus. In addition, there is pulmonary arteritis and phlebitis. Usually EAVAg localizes within the cytoplasm of pneumocytes (Fig. 3) and within alveolar macrophages. Later in the infection, EAVAg becomes identiable within vascular endothelium and then extends to the cytoplasm of vascular myocytes. Lymphoid tissue. Within lymphoid organs, it is possible to observe lymphoid follicle necrosis, edema, and slight hemorrhage with histiocytic erythrophagocytosis. Lymph node sinuses may contain prominent and sometimes highly pleomorphic histiocytic cells and lymphocytes. EAVAg is contained within stromal dendritelike cells and within the macrophages of the lymph node sinuses and spleen. Intestine. In adults, distention of the submucosal lymphatics of the large intestine, with mild crypt and lamina propria necrosis, may be observed. In foals, where the pulmonary lesions generally prevail, it is also possible to observe a pneumoenteric syndrome with pathologic changes involving crypts, intestinal mucosal blood vessels, and gastrointestinal tractassociated lymphoid tissue. Infarcts may be present in cecum and colon. In these cases, EAVAg may localize within enterocytes and vascular endothelial cells. Adrenal glands. The adrenal gland may present with multifocal vasculitis, hemorrhages, and infarcts. The EAVAg can localize within cortical epithelial cells and capillary endothelium of cortex and medulla. Kidneys. Renal lesions, which can be severe, occur when infection is at an advanced stage and consist of tubular necrosis, lymphocytic interstitial nephritis (Fig. 5), glomerular tuft disorganization, and hypercellularity. The viral antigen can localize within morphologically intact and necrotic tubular epithelial cells, intratubular cellular hyaline casts (Fig. 5), and glomerular endothelial and perhaps mesangial cells. Sometimes, in absence of morphologic changes and before the occurrence of the tubular lesions, it is possible to observe abundant intracytoplasmic viral antigen within stellate and fusiform cells located within the renal interstitium. Skin. The dermis may be involved with vasculitis, making skin biopsy suitable for diagnostic histopathology and immunohistochemistry. The vasculitis may be associated with thrombosis and ulcerative dermatitis. Female reproductive tract and fetus. Fetuses and fetal membranes are often expelled without premonitory signs of abortion and can be autolyzed or well preserved.10,16,35 Lesions in the fetus are only occasionally detected7,10,29 and when present are represented by mild perivascular lymphocytic inltrate and mild interstitial pneumonia. Rarely, they can be severe and
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
Vet Pathol 37:4, 2000
Equine Viral Arteritis
291
consist of vasculitis involving the allantochorion, brain, liver, spleen, and lung.29 EAVAg is inconsistently detectable within tissues of aborted fetuses and when present is localized within the cytoplasm of the areolar trophoblast (Fig. 6), allantochorionic mesenchyma, thymus epithelium, splenic reticular cells, endothelium of visceral blood vessels, and enterocytes.10,13,36 In mares experiencing abortion following experimental infection,7 the uterine epithelial cells are swollen, with fragmentation of cytosolic network, swollen granular mitochondria, residual bodies, and large phagolysosomes containing dense and nely granular material, membranes, and vescicles. The uterine propria submucosa may be edematous with inltration of neutrophils and macrophages and endothelial cell swelling. The myometrium may contain necrotic myocytes with ribosome clusters, macrophages, and swollen endothelial cells. Male reproductive tract. EVA lesions associated with the male reproductive tract were studied in experimentally infected prepubertal and peripubertal colts.22 Colts euthanized between the 7th and the 14th day following viral inoculation had thoracic and abdominal effusions, lymphadenopathy, and diffuse edema of the genital organs. Histologically, necrotizing vasculitis involving testes, epididymides, vasa deferentia, ampullae, prostate glands, and vesicular and bulbourethral glands were observed. This vasculitis was characterized by severe brinoid necrosis of small muscular arteries with edema and hemorrhage. Colts examined between the 28th and 180th day PI had lymphocytic and plasmacytic inltrate within the lamina propria and tunica muscularis of the epididymides and accessory genital glands. One of the prepubertal foals, persistently infected for 15 months following viral inoculation, had marked lymphoplasmacytic inltration of ampullae.
Experimental infection
The terminal lesions are considered extensions of the developmental lesions with subcutaneous edema and abundant quantities of uid in the peritoneal and pleural cavities. All the lymph nodes of the body are swollen and hemorrhagic to some degree. Infarcts have been described in the cecum and colon. Severe submucosal edema and hemorrhage are frequent ndings, and hemorrhage of the adrenal cortex has been observed. Microscopically, there is severe necrosis of the germinal centers of lymph nodes, with associated hemorrhage. Severe necrosis of the mucosa, submucosal edema, and necrotizing panvasculitis with neutrophils and lymphocytes mainly involving the small muscular arteries also has been reported. Multifocal thrombosis and infarction involving cecum and colon and hemorrhage of the renal medulla are seen. In the renal cortex, there is mild glomerulitis with swelling and disorganization of the glomerular tufts. Chronic lesions are seen in horses from day 12 following virus inoculation. Lesions consist of mild swollen lymph nodes and excess of uid within peritoneal and thoracic cavities. Microscopic lesions are dramatic and consist of generalized arteritis and severe glomerulonephritis with tubular necrosis and hyaline casts. Lesions of natural EVA are rarely as severe as those observed following experimental infection. Pathogenesis It is possible to determine the pathogenesis of EAV infection in horses by following the distribution of viral antigen and lesions in experimental2,9,36,40 and natural10,13,35,56 infections (Fig. 7). Twenty-four hours PI or later, the virus invades the respiratory epithelium (Fig. 3) and alveolar macrophages. By 48 hours PI, the virus can be found in the satellite lymph nodes, especially bronchial lymph nodes. At 3 days PI, the virus replicates in bronchopulmonary lymph nodes, endothelium, and circulating monocytes. Systemic distribution of the virus follows, with localization within macrophages and dendritelike cells of lymphoid tissue. Approximately 68 days PI, the virus localizes within endothelium and medial myocytes of blood vessels and mesothelium. At day 10 PI, the most severe damage occurs to blood vessels. After 10 days PI, there is decrease of EAVAg in all the locations except the tunica media of small muscular arteries (Fig. 3). The last site to be invaded apparently is the renal tubular epithelium (Fig. 5), where the virus may persist for an additional 2 weeks. Infective EAV is no longer detectable in most tissues 28 days after experimental infection, except in the reproductive tracts of some colts and stallions.19,43 The vascular lesions observed in EAV infection, particularly medial necrosis, may be due to a combi-
Lesions observed following experimental infection have been arbitrarily divided into three groups: developmental, terminal, and chronic but active.45 Lesions were subdivided on the basis of the progression of the macroscopic and histologic changes. The developmental lesions, observed from the 4th through the 6th day PI, consist of excessive pleural and peritoneal uid, congestion and enlargement of the lymph nodes, and edema along the course of the colonic and cecal vessels. Histologically, distention of the submucosal lymphatics of the large intestine, with mild necrosis of the mucosal epithelium, is evident. In addition, subcapsular and interstitial edema and congestion of lymph nodes, adrenal cortices, and kidneys have been reported.
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
292
Del Piero
Vet Pathol 37:4, 2000
Fig. 7.
Pathogenesis of EVA.
nation of factors. Virus localization may have a direct cytopathic effect on endothelium and medial myocytes.13 The endothelial cell damage could induce anoxia17 or thrombosis. As previously speculated,7 abortion may occur by myometritis. Reduction of blood ow to the fetus may occur due to blood vessel compression by endometrial edema or alteration of vascular tone by various inammatory mediators. Serum progesterone levels constantly diminish from 6 to 48 hours before abortion and are not detectable at necropsy. This decreased progesterone production from a hypoxic placenta, combined with a local release of prostaglandins, may trigger chorionic detachment.7 Vasculitis with associated thrombosis may also play a role inducing ischemia. Chorionic detachment and expulsion of an infected or un-
infected fetus may follow (Fig. 8). In the infected fetus, EAVAg can be identied within the trophoblastic epithelium and mesenchyma and shortly after within pneumocytes, alveolar macrophages, thymic epithelium, and enterocytes. Diagnosis The diagnosis of EVA is based on demonstration of lesions and the etiologic agent and/or seroconversion.
Serology and virology
The detection of seroconversion with complementdependent virus neutralization performed using the Bucyrus strain in EAV-infected animals is a reliable method for identing EAV infection in horses. Some foals13,54 have presuckle positive serology tests for
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
Vet Pathol 37:4, 2000
Equine Viral Arteritis
293
Fig. 8.
Pathogenesis of EAV abortion.
EAV, suggestive of in utero infection. Postsuckle testing would be invalid because of passive transfer of maternal immunity in seroconverted mares.13 Tissue culture cell lines generally used to isolate EAV are RK-13 cells, Vero cells, and equine lung cells. In addition to immunohistochemistry, other molecular techniques, such as reverse transcription polymerase chain reaction, have been used to identify the presence of EAV, especially in regard to genital transmission of the virus.46,49 The application of these techniques to identify viral RNA in tissues may be very useful for diagnostic purposes and further studies, although sensitivity and specicity for routine diagnostic use still need to be proven.
Differential diagnoses
There are several infectious and a few noninfectious diseases that should be considered as differential diagnoses for EVA. EHV-1 and, sporadically, equine herpesvirus 4 induce late abortion and stillbirth in horses.57,60 In neonates it is difcult to distinguish between EHV and EAV pneumonia macroscopically, whereas at the mi-
croscopic level the difference is rather clear. EHV-1 induces necrotizing bronchiolitis and interstitial pneumonia with intranuclear viral inclusions, chromatin margination, and fragmentation. Large quantities of intranuclear and intracytoplasmic EHV antigen can be immunocytochemically observed within epithelial cells, macrophages, and pulmonary endothelial cells of fetuses.11,42 In addition, EHV-1infected fetuses and neonatal foals may present with multifocal coagulative necrosis of various organs, in particular liver, intestine, and lymphoid organs, which are also the ideal specimens for histologic and immunocytochemical diagnosis.58 EHV-1 induces encephalomyelopathy secondary to vasculitis,26 with virus antigen localizing within endothelial cells, myocytes, and pericytes.12,59 Encephalomyelitis has not been associated with EAV infection. EHV-1 also may rarely induce nonneurologic fatal disease in young adult horses with severe vasculitis that is difcult to distinguish histologically from EVA infection (F. Del Piero, unpublished). Equine adenovirus37 is a rare cause of death in horses and almost exclusively involves Arabian and Thoroughbred foals affected by combined immunodeciency characterized by severe atrophy of the lymphoid
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
294
Del Piero
Vet Pathol 37:4, 2000
tissues. Foals die because of a severe necrotizing bronchopneumonia. Large intranuclear basophilic Cowdry type B viral inclusions are seen within the bronchial epithelium and are also occasionally located within the exocrine pancreas. The identiable viral antigen is present in smaller quantities than in EHV-1 and EAV infection and is almost exclusively intranuclear. Inuenza orthomyxovirus infections accompanied by bacterial infections cause interstitial and bronchopneumonia.28 Vasculitis is not a characteristic feature. The orthomyxovirus antigen is abundant within the cytoplasm and nucleus and can be detected in pulmonary specimens.50 The acute and subacute forms of lentivirus-induced equine infectious anemia present with gross and histologic lesions33 that, with the exception of bone marrow hyperplasia and dyserythropoiesis, the absence of vasculitis, and the possible occurrence of granulomatous meningoencephalomyelitis,38 could be mistaken for EVA. Viral RNA can be identied systemically in cells of macrophage lineage.44 The orbivirus of African horse sickness causes acute pulmonary, retroorbital, and muscle edema with ascites, hydrothorax, and hydropericardium. Histologically, the edema may be associated with mild perivascular mononuclear inltrate, which may resemble an arterivirus lesion. The virus is localized within the cytoplasm of endothelium and macrophages.3,34,61 The morbillivirus of Hendra disease41 may cause a fatal infection and induces hemorrhagic pneumonia with typical endothelial cell syncytia. Vascular lesions resembling EVA can be systemically distributed, particularly in the kidney. The viral antigen is localized within endothelial cells, and lamentous paramyxovirus structures may be identied ultrastructurally.24 Getah virus, of the alphavirus subgroup of the Togaviridae, can cause fever, rhinorrhea, and occasional exanthema, limb edema, lymphopenia or monocytosis, and abortion and must be included among the differential diagnoses for EVA.30 Purpura hemorrhagica31 and septic shock may induce systemic hemorrhages and occasionally vascular changes48 resembling the severe lesions of the rare fatal EVA cases. The toxic plant hoary alyssum (Berteroa incana) induces fever, hemolysis, limb edema, laminitis, gastroenteritis, and abortion and can mimic EVA clinical presentation and gross lesions.20,25 Differential diagnoses should also include infectious and noninfectious abortion, and each of these forms will present more or less characteristic lesions.23,32,57 Conclusions Although not frequently diagnosed as a cause of abortion, neonatal mortality, and disease in adults,
EVA is an important and perhaps emerging disease that can result in severe economic losses for the equine industry. Complete pathologic examination associated with the available ancillary procedures will guarantee a directed and accurate diagnosis. Acknowledgements
I am very grateful to Mrs. A. Wensky-Roberts of the Image Lab for the photography.
References
1 Belak S, Stade T, Bjorklund H, Ros Bascunana C, Ciabatti IM, Scicluna MT, Amaddeo D, McCollum WH, Paton DJ, Autorino GL, Timoney PJ, Klingeborn B: Genetic diversity among eld isolated of equine arteritis virus. Proc Int Conf Equine Infect Dis 8:177183, 1999 2 Breese SS Jr, McCollum WH: Electron-microscopic studies of tissues of horses infected by equine arteritis virus. Proc Int Conf Equine Infect Dis 3:273281, 1972 3 Brown CC, Meyer RF, Grubman MJ: Presence of African horse sickness virus in equine tissues, as determined by in situ hybridization. Vet Pathol 31:689694, 1994 4 Bryans JT, Doll ER, Crowe MEW, McCollum WH: The blood picture and thermal reaction in experimental viral arteritis of horses. Cornell Vet 47:4252, 1957 5 Cavanagh D: Nidovirales: a new order comprising Coronaviridae and Arteriviridae. Arch Virol 142:629633, 1997 6 Cavanagh D, Brien DA, Brinton M, Enjuanes L, Holmes KV, Horzinek MC, Lai MMC, Laude H, Plaggemann PGW, Siddel S, Spaan WJM, Taguchi F, Talbot PJ: Revision of the taxonomy of the coronavirus, togavirus and arterivirus genera. Arch Virol 135:227237, 1994 7 Coignoul FL, Cheville NF: Pathology of maternal genital tract, placenta and fetus in equine viral arteritis. Vet Pathol 21:333340, 1984 8 Cole JR, Hall RF, Gosser HS, Hendricks JB, Pursell AR, Senne DA, Pearson JE, Gipson CA: Trasmissibility and abortogenic effect of equine viral arteritis in mares. J Am Vet Med Assoc 189:769771, 1986 9 Crawford TD, Henson JB: Immunouorescent, light-microscopic and immunologic studies of equine viral arteritis. Proc Int Conf Equine Infect Dis 3:282302, 1972 10 Del Piero F: Comparison of equine arteritis virus and equine herpesvirus 1 ndings in aborted fetuses. J Equine Vet Sci 19:562, 1999 11 Del Piero F, Dubovi EJ: The diagnosis of equine herpesvirus 1 (EHV-1) abortion and neonatal infection with emphasis on immuno-peroxidase histochemical ndings. Vet Pathol 35:444, 1998 12 Del Piero F, Wilkins PA, de Lahunta A, Nelson C, Dubovi EJ: Fifteen cases of equine herpesvirus 1 (EHV-1) encephalomyelopathy in horses: pathological and immuno-peroxidase histochemical ndings. Vet Pathol 35: 441, 1998 13 Del Piero F, Wilkins PA, Lopez JW, Glaser AL, Dubovi EJ, Schlafer DH, Lein DH: Equine viral arteritis in newborn foals: clinical, pathological, serological, microbio-
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
Vet Pathol 37:4, 2000
Equine Viral Arteritis
295
14
15
16 17 18 19 20
21 22
23
24 25 26
27 28 29 30 31
logical and immunohistochemical observations. Equine Vet J 29:178185, 1997 de Vries AAF, Horzinek MC, Rottier PJM, de Groot RJ: The genome organization of the Nidovirales: similarities and differences between arteri-, toro-, and coronaviruses. Semin Virol 8:3347, 1997 Doll ER, Bryans JT, McCollum WH, Crowe MEW: Isolation of a lterable agent causing arteritis of horses and abortion by mares. Its differentiation from the equine abortion (inuenza) virus. Cornell Vet 47:341, 1957 Doll ER, Knappenberger RE, Bryans JT: An outbreak of abortion caused by the equine arteritis virus. Cornell Vet 47:6975, 1957 Estes PC, Cheville NF: The ultrastructure of vascular lesions in equine viral arteritis. Am J Pathol 58:235252, 1970 Freeman KP, Cline JM, Simmons R, Wilkins PA, Cudd TA, Perry BJ: Recognition of broncopulmonary dysplasia in a newborn foal. Equine Vet J 21:292296, 1989 Fukunaga Y, Imagawa H, Tabuchi E: Clinical and virological ndings on experimental equine viral arteritis in horses. Bull Equine Res Inst 18:110113, 1981 Geor RJ, Becker RL, Kanara EW, Hovda LR, Sweeney WH, Winter TF, Rorick JK, Ruth GR, Hope E, Murphy MJ: Toxicosis in horses after ingestion of hoary alyssum. J Am Vet Med Assoc 201:6367, 1992 Golnik W, Michalska Z, Michalak T: Natural equine viral arteritis in foals. Schweiz Arch Tierheilkd 123:523533, 1981 Holyoak GR, Giles RC, McCollum WH, Little TV, Timoney PJ: Pathological changes associated with equine arteritis virus infection of the reproductive tract in prepubertal and peripubertal colts. J Comp Pathol 109:281 293, 1993 Hong CB, Donahue JM, Giles RC Jr, Petrites-Murphy MB, Poonacha KB, Roberts AW, Smith BJ, Tramontin RR, Tuttle PA, Swerczeck TW: Equine abortion and stillbirth in central Kentucky during 1988 and 1989 foaling seasons. J Vet Diagn Invest 5:560566, 1993 Hooper PT, Ketterer PJ, Hyatt AD, Russel GM: Lesions of experimental equine morbillivirus pneumonia in horses. Vet Pathol 34:312322, 1997 Hovda LR, Rose ML: Hoary alyssum (Berteroa incana) toxicity in a herd of broodmare horses. Vet Hum Toxicol 35:3940, 1993 Jackson TA, Osburn BI, Cordy DR, Kendrick JW: Equine herpesvirus 1 infection of horses: studies on the experimentally induced neurologic disease. Am J Vet Res 38:709719, 1977 Jones TC, Doll ER, Bryans JT: The lesions of equine viral arteritis. Cornell Vet 47:5268, 1957 Jones TC, Maurer FD: The pathology of equine inuenza. Am J Vet Res 4:1531, 1943 Johnson B, Baldwin C, Timoney P, Ely R: Arteritis in equine fetuses aborted due to equine viral arteritis. Vet Pathol 28:248250, 1991 Kamada M, Kumanomido T, Wada R, Fukunaga Y, Imagawa H, Sugiura T: Intranasal infection of Getah virus in experimental horses. J Vet Med Sci 53:855858, 1991 King AS: Studies on equine purpura hemorrhagica: 3.
32 33 34
35
36
37 38 39 40
41
42
43
44 45
46
47
Morbid anatomy and histology. Br Vet J 105:3554, 1949 Kirkbride CA: Laboratory Diagnosis of Livestock Abortion, 3rd ed., pp. 202254. Iowa State University Press, Ames, IA, 1990 Konno S, Yamamoto H: Pathology of equine infectious anemia. Proposed classication of pathologic types of the disease. Cornell Vet 60:393449, 1970 Laegreid WW, Burrage TG, Stone-Marschat M, Skowronek A: Electron microscopic evidence for endothelial infection by African horse sickness virus. Vet Pathol 29: 554556, 1992 Lopez JW, Del Piero F, Glaser A, Finazzi M: Immunoperoxidase histochemistry as a diagnostic tool for detection of equine arteritis virus antigen in formalin xed tissues. Equine Vet J 28:7779, 1996 MacLachlan NJ, Balasuriya UB, Rossitto PV, Hullinger PA, Patton JF, Wilson WD: Fatal experimental equine arteritis virus infection of a pregnant mare: immunohistochemical staining of viral antigens. J Vet Diagn Invest 8:367374, 1996 McChesney AE, England JJ: Adenoviral infection in foals. J Am Vet Med Assoc 166:8385, 1975 McClure JJ, Lindsay WA, Taylor W, Ochoa R, Issel CJ, Coulter SJ: Ataxia in four horses with equine infectious anemia. J Am Vet Med Assoc 180:279283, 1982 McCollum WH: Pathologic features of horses given avirulent equine arteritis virus intramuscularly. Am J Vet Res 42:12181220, 1981 McCollum WH, Prickett ME, Bryans JT: Temporal distribution of equine arteritis virus in respiratory mucosa, tissues and body uids of horses infected by inhalation. Res Vet Sci 12:459464, 1971 Murray K, Selleck P, Hooper P, Hyatt A, Gould A, Gleeson L, Westbury H, Hiley L, Selvey L, Rodwell B, Ketterer P: A morbillivirus that caused fatal disease in horses and humans. Science 268:9497, 1995 Murray MJ, Del Piero F, Jeffrey SC, Davis MS, Furr MO, Dubovi EJ, Mayo JA: Neonatal equine herpesvirus type 1 infection on a Thoroughbred breeding farm. J Vet Intern Med 12:3641, 1998 Neu SM, Timoney PJ, McCollum WH: Persistent infection of the reproductive tract in stallions experimentally infected with equine arteritis virus. Proc Int Conf Equine Infect Dis 5:14, 1987 Oaks JL, McGuire TC, Ulibarri C, Crawford TB: Equine infectious anemia virus is found in tissue macrophages during subclinical infection. J Virol 72:72637269, 1998 Prickett ME, McCollum WH, JT Bryans: The gross and microscopic pathology observed in horses experimentally infected with the equine arteritis virus. Proc Int Conf Equine Infect Dis 3:265272, 1972 Ramina A, Dalla Valle L, De Mas S, Tisato E, Zuin A, Renier M, Cuteri V, Valente C, Cancellotti FM: Detection of equine arteritis virus in semen by reverse transcriptase polymerase chain reactionELISA. Comp Immunol Microbiol Infect Dis 22:187197, 1999 Redaelli GD, Codazza P, Finazzi M, Agrimi P, Fanchini G, Proverbio E: Osservazioni epizootologiche, cliniche ed anatomo-istopatologiche sul primo focolaio di arterite
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
296
Del Piero
Vet Pathol 37:4, 2000
48 49
50
51
52 53
equina negli allevamenti italiani [First outbreak of equine viral arteritis in Italy: epidemiological, clinical and pathological ndings]. Clin Vet 103:566571, 1980 Rooney JR, Robertson JL: Equine Pathology, 1st ed., pp. 357358. Iowa State University Press, Ames, IA, 1996 Starick E: Rapid and sensitive detection of equine arteritis virus in semen and tissue samples by reverse transcription-polymerase chain reaction, dot blot hybridisation and nested polymerase chain reaction. Acta Virol 42:333339, 1998 Sutton GA, Viel L, Carman PS, Boag BL: Study of the duration and distribution of equine inuenza virus subtype 2 (H3N8) antigens in experimentally infected ponies in vivo. Can J Vet Res 61:113120, 1997 Timoney PJ: Clinical, virological and epidemiological features of the 1984 outbreak of equine viral arteritis in the Thoroughbred population in Kentucky, USA. Proc Int Conf Thoroughbred Breed Organ: Equine Viral Arteritis 1984:2433, 1984 Timoney PJ, McCollum WH: Equine viral arteritis. Vet Clin North Am Equine Pract 9:295309, 1993 Timoney PJ, McCollum WH, Murphy TW: The carrier state in equine arteritis virus infection in the stallion with specic emphasis on the venereal mode of virus transmission. J Reprod Fertil 35(Suppl 1):95, 1987
54 Vaala WE, Hamir AN, Dubovi EJ, Timoney PJ, Ruiz B: Fatal congenitally acquired infection with equine arteritis virus in a neonatal Thoroughbred. Equine Vet J 24:155 158, 1992 55 Wilkins PA: Equine viral arteritis. In: 5 Minute Consult: Equine. (in press) 56 Wilkins PA, Del Piero F, Lopez J, Cline M: Immunohistochemical diagnosis of equine arteritis infection in a foal. Equine Vet J 27:398, 1995 57 Whitwell KE: Investigations into fetal and neonatal losses in the horse. Vet Clin North Am Large Anim Pract 2: 313331, 1980 58 Whitwell KE: An assessment of the criteria used to diagnose virus abortion: a review of 100 cases. J Reprod Fertil 32(Suppl 1):110, 1982 59 Whitwell KE, Blunden AS: Pathological ndings in horses dying during an outbreak of the paralytic form of equid herpesvirus type 1 (EHV-1) infection. Equine Vet J 24:1319, 1992 60 Whitwell KE, Smith KC, Sinclair R, Mumford JA: Foetal lesions in spontaneous EHV-4 abortion in mares. Proc Int Conf Equine Infect Dis 7:354, 1994 61 Wohlsein P, Pohlenz JF, Davidson FL, Salt JS, Hamblin C: Immunohistochemical demonstration of African horse sickness viral antigen in formalin-xed equine tissues. Vet Pathol 34:568574, 1997
Request reprints from Dr. F. Del Piero, Department of Pathobiology, School of Veterinary Medicine, University of Pennsylvania, New Bolton Center, 382 West Street Road, Kennett Square, PA 19348-1692 (USA). E-mail: fdp@vet.upenn.edu.
Downloaded from vet.sagepub.com at Universiti Malaysia Kelantan on October 29, 2012
Вам также может понравиться
- Veterinary Virology PDFДокумент96 страницVeterinary Virology PDFShem Peter Mutua Mutuiri100% (1)
- Activity 3.1.2 Rapid Pathogen IdentificationДокумент8 страницActivity 3.1.2 Rapid Pathogen Identificationsahsdjkh7Оценок пока нет
- Reoviridae Birnaviridae: General and Systemic Virology (MICRO - 303)Документ11 страницReoviridae Birnaviridae: General and Systemic Virology (MICRO - 303)Muhammad Arslan UsmanОценок пока нет
- CoccidosisДокумент288 страницCoccidosisMegersaОценок пока нет
- Ruminant Diseases of Respiratory System. CypresДокумент5 страницRuminant Diseases of Respiratory System. CypresDonnabelContignoОценок пока нет
- Equine Viral ArteritisДокумент13 страницEquine Viral ArteritisMohammedОценок пока нет
- Interstitial Lung Disease Associated With Equine Infectious Anemia Virus Infection in HorsesДокумент10 страницInterstitial Lung Disease Associated With Equine Infectious Anemia Virus Infection in HorsesFredy MoralesОценок пока нет
- EPIDEMIOLOGYДокумент3 страницыEPIDEMIOLOGYEdgarОценок пока нет
- Lab Tests To Check The Post Mortem AbnormalitiesДокумент13 страницLab Tests To Check The Post Mortem AbnormalitiesusamatayyabОценок пока нет
- Poxviridae: In: A Concise Review of Veterinary Virology, Carter G.R., Wise D.J. and Flores E.F. (Eds.) - A3410.1005Документ10 страницPoxviridae: In: A Concise Review of Veterinary Virology, Carter G.R., Wise D.J. and Flores E.F. (Eds.) - A3410.1005Mestesanu ElisabetaОценок пока нет
- PRRS Guide Web Bulletin - OIEДокумент7 страницPRRS Guide Web Bulletin - OIESimone Rosa DidonéОценок пока нет
- Exotic Diseases of Poultry - A ReviewДокумент19 страницExotic Diseases of Poultry - A Reviewthanh ba matОценок пока нет
- Rift Valley Fever: C H A P T E R 2 - 1 - 1 4Документ20 страницRift Valley Fever: C H A P T E R 2 - 1 - 1 4WormInchОценок пока нет
- Equine Viral ArteritisДокумент14 страницEquine Viral ArteritisKristen PykeОценок пока нет
- B108 - Enzootic Bovine Leukosis: Nature of The DiseaseДокумент3 страницыB108 - Enzootic Bovine Leukosis: Nature of The DiseaseDilip GuptaОценок пока нет
- Classical Swine Fever: (Hog Cholera)Документ25 страницClassical Swine Fever: (Hog Cholera)Vini Vidi ViciОценок пока нет
- A Concise Guide To The Microbial and Parasitic Diseases of HorsesДокумент82 страницыA Concise Guide To The Microbial and Parasitic Diseases of HorsesLeo PerezОценок пока нет
- Under Natural ConditionsДокумент3 страницыUnder Natural ConditionsSantosh BhandariОценок пока нет
- AvianPneumovirus APV PDFДокумент7 страницAvianPneumovirus APV PDFRayza Lubis0% (1)
- Resumo Seneca Virus - Seneca Valley VirusДокумент12 страницResumo Seneca Virus - Seneca Valley VirusviroticaОценок пока нет
- Proceedings of The 16th Italian Association of Equine Veterinarians CongressДокумент4 страницыProceedings of The 16th Italian Association of Equine Veterinarians CongressCabinet VeterinarОценок пока нет
- Feline Panleukopenia: Directed By: DR - Nadir Khosa DVM, Uvas, LahoreДокумент11 страницFeline Panleukopenia: Directed By: DR - Nadir Khosa DVM, Uvas, LahoreVetlife DvpОценок пока нет
- Japanese Encephalitis: NB: Version Adopted by The World Assembly of Delegates of The OIE in May 2010Документ11 страницJapanese Encephalitis: NB: Version Adopted by The World Assembly of Delegates of The OIE in May 2010WormInchОценок пока нет
- AA 219 - Lecture 6Документ52 страницыAA 219 - Lecture 6EddyОценок пока нет
- Prrs Guide Web BulletinДокумент7 страницPrrs Guide Web BulletinJocelyn LunaОценок пока нет
- Viro Final 2Документ10 страницViro Final 2Muhammad Arslan UsmanОценок пока нет
- Lager 1996Документ8 страницLager 1996mari combsОценок пока нет
- Pyometrainsmallanimals: Ragnvi HagmanДокумент23 страницыPyometrainsmallanimals: Ragnvi HagmansalomonОценок пока нет
- Delost Introduction To Diagnostic Microbiology 390 392Документ3 страницыDelost Introduction To Diagnostic Microbiology 390 392Keanne GanironОценок пока нет
- Vet Pathol 2011 2011 ACVP Annual Meeting E1 E51Документ52 страницыVet Pathol 2011 2011 ACVP Annual Meeting E1 E51Haroon RashidОценок пока нет
- 2.03.14 Newcastle DisДокумент14 страниц2.03.14 Newcastle DisdiparayogagalihОценок пока нет
- Newcastle Disease: C H A P T E R 2 - 3 - 1 4Документ14 страницNewcastle Disease: C H A P T E R 2 - 3 - 1 4Roby R. AryoputrantoОценок пока нет
- FMD Oie 2012Документ29 страницFMD Oie 2012dilipreddygОценок пока нет
- Togaviridae Flaviviridae AND Bunyaviridae: General and Systemic Virology (MICRO - 303)Документ8 страницTogaviridae Flaviviridae AND Bunyaviridae: General and Systemic Virology (MICRO - 303)Muhammad Arslan UsmanОценок пока нет
- Viro Final 6Документ10 страницViro Final 6Muhammad Arslan UsmanОценок пока нет
- Literature Review On Newcastle DiseaseДокумент8 страницLiterature Review On Newcastle Diseasenaneguf0nuz3100% (1)
- Japanese Encephalitis: OIE Terrestrial Manual 2008 231Документ9 страницJapanese Encephalitis: OIE Terrestrial Manual 2008 231Iin NovitaОценок пока нет
- Newcastle Disease ThesisДокумент5 страницNewcastle Disease Thesiskatieduboseatlanta100% (2)
- Overview of Infectious Laryngotracheitis in Poultry: Veterinary ManualДокумент2 страницыOverview of Infectious Laryngotracheitis in Poultry: Veterinary ManualSamapanОценок пока нет
- Proceeding of The SEVC Southern European Veterinary ConferenceДокумент4 страницыProceeding of The SEVC Southern European Veterinary ConferenceHartina SamosirОценок пока нет
- Fowl PoxДокумент3 страницыFowl PoxakhmadfuadiОценок пока нет
- Experimental Infection With A Virulent 1234Документ3 страницыExperimental Infection With A Virulent 1234Iulian RoșuОценок пока нет
- Microbial Fish Diseases 2011Документ79 страницMicrobial Fish Diseases 2011Saraturituri100% (2)
- Epizootic Haemorrhagic Disease: CHAPTER2.1.4BДокумент11 страницEpizootic Haemorrhagic Disease: CHAPTER2.1.4BWormInchОценок пока нет
- Avian Encephalomyelitis (AE)Документ36 страницAvian Encephalomyelitis (AE)shylendarОценок пока нет
- Ecthyma Contagiosum (Human Orf)Документ2 страницыEcthyma Contagiosum (Human Orf)Deba P SarmaОценок пока нет
- Birnaviridae - Infectious Bursal DiseaseДокумент9 страницBirnaviridae - Infectious Bursal DiseaseELIJAH EUMIR CUNANANОценок пока нет
- Feline Infectious Peritonitis ABCD Guidelines On PДокумент12 страницFeline Infectious Peritonitis ABCD Guidelines On Pxn5q8nckvkОценок пока нет
- Prrs (Porcine Reproductive and Respiratory Syndrome) : GijaponДокумент43 страницыPrrs (Porcine Reproductive and Respiratory Syndrome) : GijaponFrance GijaponОценок пока нет
- Newcastle Disease 2016Документ23 страницыNewcastle Disease 2016RavenMirronОценок пока нет
- Corona Virus: Q1: Coronavirus Life CycleДокумент6 страницCorona Virus: Q1: Coronavirus Life CycleTufail KhanОценок пока нет
- Detection of Viral Antigen in Placenta and Fetus of Cattle Acutely Infected With Bovine Viral Diarrhea VirusДокумент9 страницDetection of Viral Antigen in Placenta and Fetus of Cattle Acutely Infected With Bovine Viral Diarrhea VirusDarwin Leonardo Garzon MОценок пока нет
- NEWCASTLE DISEASE - Diseases of Poultry - The Poultry SiteДокумент3 страницыNEWCASTLE DISEASE - Diseases of Poultry - The Poultry SiteHerman Ndau100% (1)
- Avian Influenza (Ai) : Poultry Pathology (Path-510)Документ52 страницыAvian Influenza (Ai) : Poultry Pathology (Path-510)Abdullah AzeemОценок пока нет
- Reprinted in The IVIS Website With The Permission of The Meeting OrganizersДокумент2 страницыReprinted in The IVIS Website With The Permission of The Meeting OrganizersLucienne GonzalesОценок пока нет
- Avian EncephalomyelitisДокумент6 страницAvian Encephalomyelitisstraihan234Оценок пока нет
- Haemophilus Parasuis (Glasser'S Disease)Документ4 страницыHaemophilus Parasuis (Glasser'S Disease)AndreasKarapatakisОценок пока нет
- Vesicular StomatitisДокумент5 страницVesicular StomatitisSeby SebastianОценок пока нет
- Models of Protection Against HIV/SIV: Models of Protection Against HIV/SIVОт EverandModels of Protection Against HIV/SIV: Models of Protection Against HIV/SIVGianfranco PancinoОценок пока нет
- Screenshot 2021-06-23 at 11.36.48 AMДокумент116 страницScreenshot 2021-06-23 at 11.36.48 AMSmitha ShekarОценок пока нет
- Advice Following Nasal Surgery Fes Sep20Документ8 страницAdvice Following Nasal Surgery Fes Sep20Adela MarcovОценок пока нет
- Quiz I Categorical Data AnalysisДокумент2 страницыQuiz I Categorical Data Analysisfatima fatimaОценок пока нет
- Refractive ErrorsДокумент15 страницRefractive ErrorsMubasher 783Оценок пока нет
- Perforasi Pada Penderita Apendisitis Di RSUD DR.H.Abdul Moeloek LampungДокумент7 страницPerforasi Pada Penderita Apendisitis Di RSUD DR.H.Abdul Moeloek LampungKikiОценок пока нет
- Mother To Child Transmition of HIVДокумент23 страницыMother To Child Transmition of HIVGenoveva Maditias Dwi PertiwiОценок пока нет
- Sharon Denise Gross: 513 Grazing Field Drive, Tuscaloosa, AL 35405 (C) 205-242-3670 (W) 205-554-2000 Ext. 3617 (E) (E)Документ6 страницSharon Denise Gross: 513 Grazing Field Drive, Tuscaloosa, AL 35405 (C) 205-242-3670 (W) 205-554-2000 Ext. 3617 (E) (E)api-469030612Оценок пока нет
- Hand Foot & Mouth DiseaseДокумент23 страницыHand Foot & Mouth DiseaseKabang Moa100% (1)
- Drug Study-Ceftriaxone ClindamycinДокумент2 страницыDrug Study-Ceftriaxone ClindamycinDavid VillanuevaОценок пока нет
- How A Breath Is Delivered: OutlineДокумент16 страницHow A Breath Is Delivered: OutlineLesly Peinado TorresОценок пока нет
- Pharmaceutical Dosage Forms: by S.Bohlooli, PHDДокумент36 страницPharmaceutical Dosage Forms: by S.Bohlooli, PHDvignesh murugesanОценок пока нет
- Prevalence of ADHD and Autism Spectrum Disorder in Children With Hypermobility Spectrum Disorders or Hypermobile Ehlers-Danlos Syndrome - A Retrospective StudyДокумент10 страницPrevalence of ADHD and Autism Spectrum Disorder in Children With Hypermobility Spectrum Disorders or Hypermobile Ehlers-Danlos Syndrome - A Retrospective StudyKarel GuevaraОценок пока нет
- Chloe Ting - 2021 Summer Shred Challenge - Free Workout ProgramДокумент1 страницаChloe Ting - 2021 Summer Shred Challenge - Free Workout ProgramAnniie GuerreroОценок пока нет
- Oral Pathology Key PointsДокумент4 страницыOral Pathology Key PointsRohit Bansal100% (1)
- 10 Diagnosa PenyakitДокумент3 страницы10 Diagnosa PenyakitDiny Rachma Putri HОценок пока нет
- Drug Study: Drug Name Contraindications ResponsibilityДокумент2 страницыDrug Study: Drug Name Contraindications ResponsibilityJOVEMEA LIRAYОценок пока нет
- Boyd & Griffin Classification (1949)Документ14 страницBoyd & Griffin Classification (1949)João Pedro ZenattoОценок пока нет
- Tomografia UrotacДокумент12 страницTomografia Urotacnoeg_909929Оценок пока нет
- The Study of Drug Resistance in Bacteria Using Antibiotics: June 2019Документ6 страницThe Study of Drug Resistance in Bacteria Using Antibiotics: June 20197'A'06Aditya BeheraОценок пока нет
- Burn Assessment CMU PDFДокумент2 страницыBurn Assessment CMU PDFmegamindОценок пока нет
- Mod 4 Combined PacopДокумент138 страницMod 4 Combined PacopJacosby WorcestershireОценок пока нет
- Effect of Nonsurgical Periodontal Therapy. I. Moderately Advanced Periodontitis. Badersten A, Nilvéus R, Egelberg J. J Clin Periodontol. 1981 Feb8 (1) 57 72 PDFДокумент17 страницEffect of Nonsurgical Periodontal Therapy. I. Moderately Advanced Periodontitis. Badersten A, Nilvéus R, Egelberg J. J Clin Periodontol. 1981 Feb8 (1) 57 72 PDFMashal AmirОценок пока нет
- Ajor Epressive Isorder: Marshall Cates, Angela Passero, and Jacqueline FeldmanДокумент16 страницAjor Epressive Isorder: Marshall Cates, Angela Passero, and Jacqueline FeldmanbencleeseОценок пока нет
- فسلجة دم الطيورДокумент604 страницыفسلجة دم الطيورMustafa AL-Asadsy100% (1)
- Inistitutional Assessementknowledge Test For Comprhenssive NursingДокумент19 страницInistitutional Assessementknowledge Test For Comprhenssive NursingkassahunОценок пока нет
- Therapeutic UltrasoundДокумент18 страницTherapeutic UltrasoundPhysio Ebook100% (1)
- Microsoft Word - Schuessler Salts FlyerДокумент2 страницыMicrosoft Word - Schuessler Salts Flyer4379100% (2)
- Conversion DisorderДокумент2 страницыConversion DisorderThe Lullaby100% (1)
- Role of Pain Placebo Analgesia: Gordont, Fields FДокумент4 страницыRole of Pain Placebo Analgesia: Gordont, Fields Fmaurina rizkiОценок пока нет