Академический Документы
Профессиональный Документы
Культура Документы
Causes of Knee Problems in The Elderly
Загружено:
Śáńtőśh MőkáśhíИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Causes of Knee Problems in The Elderly
Загружено:
Śáńtőśh MőkáśhíАвторское право:
Доступные форматы
CAUSES OF KNEE PROBLEMS IN THE ELDERLY The knee is the largest joint in the body and bears much
of the body's weight when walking and running. Because it takes the most stress, it is also more prone to injuries and degeneration. According to Mayo Clinic physicians, almost one in every three Americans over the age of 45 will report some type of knee pain, and the potential to experience knee pain rises with age. Many of the problems that the elderly experience in their knees start with poor muscle development or inadequate stretching that begins in their 50s. Osteoarthritis Sometimes called degenerative arthritis, this condition is fairly common in people over the age of 50, and the incidence rises considerably as people approach age 70. According to Mayo Clinic physicians, osteoarthritis will cause a variety of degrees of pain when standing or walking. Individuals will experience swelling, stiffness and creaking or popping sounds from the knee. Most people who suffer from osteoarthritis will also experience a loss of flexibility in the knee joint so that they do not have full range of motion. These symptoms are a result of breakdown in the cartilage of the knee that happens with use and increasing age. Varicose Veins Treatment Laser Treatment for Varicose Veins. India's best Center 02223525001 www.varicoseveinsindia.com Sponsored Links Meniscus Tear The menisci are "C" shaped discs that help to support the fit between the large thigh bone and shin bone. They help to distribute the weight and absorb the shock during walking or running. According to the Stretching Institute, a meniscus tear can be the result of injury or degeneration. Because the meniscus doesn't receive any blood supply, recovery from this type of condition is very difficult. Degenerative tears to the meniscus are associated with the breakdown of collagen fibers in the meniscus in the elderly. Bursitis The bursae are small sacs of fluid that cushion the outside of the knee joint so that the tendons and ligaments move smoothly over the joint. With repeated injury or increased age, the bursae can become inflamed and cause problems. Injury to the bursae is common when an individual hits the knee against a hard object, such as a desk or cabinet. According to the Mayo Clinic, the symptoms will include warmth, swelling, redness, tenderness, aching and pain at rest and when going up or down the stairs. If an infection is present, there can also be fever. Chondromalacia Patella This condition is common in the elderly who develop it as a result of arthritis in the kneecap. It causes pain and tenderness at the front of the knee when sitting for long periods of time, getting up from a chair or climbing stairs. The sufferer may also experience a grating or grinding sensation when the knee is straightened or extended. Tendinitis According to Dr. Mark King from Dynamic Chiropractic, patellar tendinitis is an inflammation of the tendons that keep the kneecap in place. Individuals may experience pain either above or below the
kneecap. The type of tendinitis more commonly experienced in people over age 35 is located above the kneecap. This condition can be aggravated when the individual has weak gluteal muscles or stiff hips. Both of these situations place more stress on the knee joint and is common in the elderly who do not spend time stretching.
Sleep disorders in the elderly
Email this page to a friendShare on facebookShare on twitterBookmark & SharePrinter-friendly version Sleep disorders in the elderly involve any disrupted sleep pattern, such as problems falling or staying asleep, too much sleep, or abnormal behaviors with sleep. Causes Sleep problems are common in the elderly. In general, older people need 30 to 60 minutes less sleep than younger people. Their sleep is less deep and more choppy than sleep in younger people. A healthy 70 year old may wake up four times during the night without it being due to disease. Some causes or contributors to sleep disturbances in older adults include: Alzheimer's disease Chronic disease, such as congestive heart failure Depression (depression is a common cause of sleep problems in people of all ages) Neurological conditions Pain caused by diseases such as arthritis Prescription drugs, recreational drugs, or alcohol Sedentary lifestyle Stimulants such as caffeine Urination at night
Symptoms Difficulty falling asleep Difficulty telling the difference between night and day Early morning awakening Waking up often during the night
Exams and Tests The health care provider will take a history and perform a physical exam to look for medical causes and determine which type of sleep disorder is causing the problem. Treatment Relieving chronic pain and controlling medical conditions such as frequent urination may improve sleep in some people. Treating depression can also improve sleep. Sleeping in a quiet place and drinking a glass of warm milk before bed may improve the symptoms. Other ways to promote sleep include following these healthy lifestyle tips: Avoid large meals shortly before bedtime. Avoid stimulants such as caffeine. Get regular exercise early in the day. Go to bed and wake up at the same time every day. (Don't take naps.) Use the bed only for sleep or sexual activity.
If you can't fall asleep after 20 minutes, get out of bed and do a quiet activity such as reading or listening to music. Avoid using sleeping pills to help you sleep, if possible. They can lead to dependence and can make sleep problems worse over time if you don't use them correctly. Your health care provider should assess your risks of daytime sleepiness, mental (cognitive) side effects, and falls before you begin taking sleep medications. If you need sleeping pills, Ambien, Lunesta, Sonata, and Rozerem can be safe when used properly. It is best to NOT take sleeping pills several days in a row or for more than 2 - 4 days a week. Alcohol can make the side effects of all sleeping pills worse and should be avoided.
WARNING: The FDA has asked manufacturers of certain sleep medicines to put stronger warning labels on their products so that consumers are more aware of the potential risks. Possible risks while taking such medicines include severe allergic reactions and dangerous sleep-related behaviors, including sleepdriving. Ask your doctor about these risks.
Common Causes of Vision Loss in Elderly Patients DAVID A. QUILLEN, M.D., Pennsylvania State University College of Medicine, Hershey, Pennsylvania Am Fam Physician. 1999 Jul 1;60(1):99-108. Vision loss among the elderly is a major health care problem. Approximately one person in three has some form of vision-reducing eye disease by the age of 65. The most common causes of vision loss among the elderly are age-related macular degeneration, glaucoma, cataract and diabetic retinopathy. Age-related macular degeneration is characterized by the loss of central vision. Primary open-angle glaucoma results in optic nerve damage and visual field loss. Because this condition may initially be asymptomatic, regular screening examinations are recommended for elderly patients. Cataract is a common cause of vision impairment among the elderly, but surgery is often effective in restoring vision. Diabetic retinopathy may be observed in the elderly at the time of diagnosis or during the first few years of diabetes. Patients should undergo eye examinations with dilation when diabetes is diagnosed and annually thereafter. The elderly population in the United States is increasing rapidly. By the year 2030, approximately 70 million Americans will be over 65 years of age. Loss of vision among the elderly is a major health care problem: approximately one in three elderly persons has some form of vision-reducing eye disease by the age of 65.1 Vision impairment is associated with a decreased ability to perform activities of daily living and an increased risk for depression.2 This article reviews the four most common causes of vision impairment in the elderly: age-related macular degeneration, glaucoma, cataract and diabetic retinopathy.3,4 Presenting symptoms of these four causes are summarized in Table 1. Age-Related Macular Degeneration Age-related macular degeneration (AMD) is the leading cause of loss of vision in people over 65 years of age. AMD is characterized by degeneration of the macula, the area of the retina responsible for central vision (Figure 1). Risk factors for AMD include advancing age, family history of AMD and cardiovascular risk factors such as hypertension and cigarette smoking. AMD can be divided into two categories: nonexudative (or dry) AMD and exudative (or wet) AMD.
Вам также может понравиться
- MCGM PF SlipДокумент2 страницыMCGM PF SlipŚáńtőśh Mőkáśhí100% (3)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Group 4Документ34 страницыGroup 4Śáńtőśh MőkáśhíОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Corruption Is One of The Biggest Threat ToДокумент2 страницыCorruption Is One of The Biggest Threat ToŚáńtőśh MőkáśhíОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Display Raj PatraДокумент2 страницыDisplay Raj PatraŚáńtőśh MőkáśhíОценок пока нет
- To Do On Daily Basis: MccafeДокумент1 страницаTo Do On Daily Basis: MccafeŚáńtőśh MőkáśhíОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Swami Vivekananda: Bengali: BengaliДокумент1 страницаSwami Vivekananda: Bengali: BengaliŚáńtőśh MőkáśhíОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Badminton: Cleanliness SloganДокумент3 страницыBadminton: Cleanliness SloganŚáńtőśh MőkáśhíОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Rohan Dilip Milkhe: Residential & Permanent AddressДокумент2 страницыRohan Dilip Milkhe: Residential & Permanent AddressŚáńtőśh MőkáśhíОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The India of My DreamsДокумент1 страницаThe India of My DreamsŚáńtőśh MőkáśhíОценок пока нет
- Car Revese HornДокумент8 страницCar Revese HornŚáńtőśh MőkáśhíОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Curriculum Vitae: Sushant Suresh VajeДокумент3 страницыCurriculum Vitae: Sushant Suresh VajeŚáńtőśh MőkáśhíОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Water Supply and Sanitation: Railway Advantages: 1. DependableДокумент2 страницыWater Supply and Sanitation: Railway Advantages: 1. DependableŚáńtőśh MőkáśhíОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- App 27802794462079Документ2 страницыApp 27802794462079Śáńtőśh MőkáśhíОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Curriculum Vitae: Personal ProfileДокумент2 страницыCurriculum Vitae: Personal ProfileŚáńtőśh MőkáśhíОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
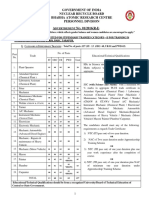
- Government of India Nuclear Recycle Board Bhabha Atomic Research Centre Personnel Division A N - 01/2016 (R-I)Документ7 страницGovernment of India Nuclear Recycle Board Bhabha Atomic Research Centre Personnel Division A N - 01/2016 (R-I)Śáńtőśh MőkáśhíОценок пока нет
- Shivaji MaharajДокумент2 страницыShivaji MaharajŚáńtőśh MőkáśhíОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Baithe KhelДокумент1 страницаBaithe KhelŚáńtőśh MőkáśhíОценок пока нет
- Philip SerraoДокумент1 страницаPhilip SerraoŚáńtőśh MőkáśhíОценок пока нет
- Mobile Phone Radiation: Analysis of DataДокумент2 страницыMobile Phone Radiation: Analysis of DataŚáńtőśh MőkáśhíОценок пока нет
- Seasonal Goods DemandДокумент45 страницSeasonal Goods DemandŚáńtőśh MőkáśhíОценок пока нет
- Finding and AnalysisДокумент4 страницыFinding and AnalysisŚáńtőśh MőkáśhíОценок пока нет
- Curriculum Vitae: Personal ProfileДокумент2 страницыCurriculum Vitae: Personal ProfileŚáńtőśh MőkáśhíОценок пока нет
- 92 63Документ1 531 страница92 63Śáńtőśh MőkáśhíОценок пока нет
- Low Vision: Care of The Patient WithДокумент39 страницLow Vision: Care of The Patient WithDattatri ReddyОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Health 2 - Part B-Older Adult Community Health AssignmentДокумент23 страницыHealth 2 - Part B-Older Adult Community Health AssignmentNicole PattenОценок пока нет
- Challenges Faced by Visually Impaired Students at Makerere and Kyambogo UniversitiesДокумент12 страницChallenges Faced by Visually Impaired Students at Makerere and Kyambogo UniversitiesDesire ramsОценок пока нет
- 1503182828PWBD Certificate - FORM VI PDFДокумент2 страницы1503182828PWBD Certificate - FORM VI PDFMadhu PanchadarlaОценок пока нет
- Blind Persons Aid For Indoor Movement Using RFIDДокумент6 страницBlind Persons Aid For Indoor Movement Using RFIDSajid BashirОценок пока нет
- Children With Special Needs-SsaДокумент130 страницChildren With Special Needs-SsaPeetamber ShambhooОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Kaufman-Scarborough - 2000 - Seeing Through The Eyes of The Color-Deficient Shopper Consumer Issues For Public PolicyДокумент4 страницыKaufman-Scarborough - 2000 - Seeing Through The Eyes of The Color-Deficient Shopper Consumer Issues For Public PolicyDante EdwardsОценок пока нет
- Exceptionality Name Definition & Alberta Ed. CodeДокумент20 страницExceptionality Name Definition & Alberta Ed. Codeapi-316248639Оценок пока нет
- Educ Chapter 6 Lesson - CompressДокумент19 страницEduc Chapter 6 Lesson - CompressMhay Pale BongtayonОценок пока нет
- Understanding Disabilities and VulnerabilitiesДокумент32 страницыUnderstanding Disabilities and VulnerabilitiesdawitОценок пока нет
- 9a Q1 L2 HWДокумент3 страницы9a Q1 L2 HWNGUYỄN THẾ VIỆT QUANGОценок пока нет
- Synopsis of Blind SchoolДокумент2 страницыSynopsis of Blind Schoolarc_nilesh786Оценок пока нет
- Intelligent Face Recognition and Navigation System Using Neural Learning For Smart Security in Internet of ThingsДокумент12 страницIntelligent Face Recognition and Navigation System Using Neural Learning For Smart Security in Internet of Thingssmriti127Оценок пока нет
- Article 1Документ23 страницыArticle 1Palaganesh NaiduОценок пока нет
- Narrative Report LexiДокумент3 страницыNarrative Report LexiLen-Len CobsilenОценок пока нет
- New Microsoft Office Word DocumentДокумент26 страницNew Microsoft Office Word DocumentHarish BhavandlaОценок пока нет
- It's A Beautiful Spring Day 17, 19Документ2 страницыIt's A Beautiful Spring Day 17, 19Anowar Hossain100% (1)
- AIPGMEE 2006 Question PaperДокумент96 страницAIPGMEE 2006 Question PaperpavaniОценок пока нет
- TNEA 2019 Info BookletДокумент37 страницTNEA 2019 Info BookletTest UserОценок пока нет
- Special Equipment Amount (SEA) : Education FundingДокумент24 страницыSpecial Equipment Amount (SEA) : Education FundingbmvoОценок пока нет
- Blind Soccer ProposalДокумент17 страницBlind Soccer ProposalHlayisekaОценок пока нет
- Primary - Kast Great Final ResearchДокумент39 страницPrimary - Kast Great Final Researchmubarek oumer100% (1)
- General Objective of The StudyДокумент28 страницGeneral Objective of The StudykasimОценок пока нет
- Accessibility and Usability Guidelines For WebsitesДокумент36 страницAccessibility and Usability Guidelines For WebsitesSergei BalaboninОценок пока нет
- The Persons With Disabilities 1995Документ27 страницThe Persons With Disabilities 1995siva ramanОценок пока нет
- Introduction To Inclusive EducationДокумент137 страницIntroduction To Inclusive EducationFeven SolomonОценок пока нет
- Maternity LeaveДокумент5 страницMaternity Leavenaveen kumarОценок пока нет
- Better Education For All Global Report October 2009Документ186 страницBetter Education For All Global Report October 2009Tatiana PiatakovaОценок пока нет
- Blind SchoolДокумент14 страницBlind SchoolHasnan ChouhanОценок пока нет
- Fashiin Show AnchoringДокумент3 страницыFashiin Show AnchoringShubhanshi AgarwalОценок пока нет
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDОт EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDРейтинг: 5 из 5 звезд5/5 (3)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionОт EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionРейтинг: 4 из 5 звезд4/5 (404)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (32)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)