Академический Документы
Профессиональный Документы
Культура Документы
24insulin & Diabetes
Загружено:
EstiPramestiningtyasИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
24insulin & Diabetes
Загружено:
EstiPramestiningtyasАвторское право:
Доступные форматы
Talking diabetes No.
24
insulin & diabetes
Insulin injections are required when the body produces little or no insulin, as with type 1 diabetes. They are also required for some people with type 2 diabetes when diabetes tablets, together with healthy eating and regular physical activity, are not enough to control blood glucose levels.
What is insulin?
Insulin is a hormone made by special cells, called beta cells, in the pancreas. When we eat, insulin is released into the blood stream where it helps to move glucose from the food we have eaten into cells to be used as energy. Insulin also helps store excess glucose in the liver.
Why must it be injected?
While ways of taking insulin by mouth or as a nasal spray are being developed, they are yet to become readily available. Insulin cannot be given in tablet form as the stomach would digest it, just as it digests food.
What if I have to go on to insulin?
For people with type 2 diabetes, starting on insulin can be a difficult and frightening decision to make. However, the many injection devices and tiny needles available today make injecting insulin much easier than most people imagine. In fact many say that they can feel the finger prick for monitoring blood glucose more than they can feel the needle used to inject insulin. When starting on insulin, your doctor and diabetes educator will help you adjust to the new routine. You may find that even with their help, it may take a while to find exactly the right dose to reduce your blood glucose to acceptable levels and to suit your particular lifestyle.
Are there different types of insulin?
There are five types of insulin ranging from short to long acting as insulin is classified according to how long it works in the body. Some insulins are clear in appearance, others cloudy.
As insulin is classified according to how long it works in the body, there are five types available. Everyone is different and will respond differently to the insulin they take. Therefore, many people need varying amounts of both a short and longer acting insulin.
Revised August 2009 A diabetes information series from State / Territory organisations of Diabetes Australia Copyright 2009
Revised August 2009
insulin & diabetes
The five types of insulin available in Australia
1. Rapid onset-fast acting insulin Rapid acting insulins are CLEAR in appearance. They are very fast acting, starting to work from 1 to 20 minutes, peaking approximately one hour later and lasting from 3 to 5 hours. When using these insulins, it is important to eat immediately after injecting. Rapid onset-fast acting insulins currently available are: > NovoRapid (Insulin aspart) > Apidra (Insulin glulisine) 2. Short acting insulin Short acting insulins are CLEAR in appearance. They begin to lower blood glucose levels within half an hour so you need to have your injection half an hour before eating. These have a peak effect at 2 to 4 hours and last for 6 to 8 hours. Short acting insulins currently available are: > Actrapid > Humulin R > Hypurin Neutral (beef) > Humalog (Insulin lispro)
3. Intermediate acting insulin Intermediate acting insulins are CLOUDY in appearance. They have either protamine or zinc added to delay their action. These insulins begin to work about 1 1/2 hours after injecting, peaking at 4 to 12 hours and lasting for 16 to 24 hours. Before injecting this type of insulin, make sure you check the leaflet inside the pack for instructions on how to prepare the insulin, including to gently shake or rotate the insulin before use. Intermediate acting insulins currently available with protamine added are: > Protaphane > Humulin NPH > Hypurin Isophane (beef)
4. Mixed insulin Mixed insulins are CLOUDY in appearance. They contain pre-mixed combinations of either a rapid onset-fast acting or a short acting insulin and intermediate acting insulin, making it easier by giving two types of insulin in one injection. If the insulin is 30/70 then it contains 30% quick acting and 70% intermediate acting insulin. 50/50 is 50% of each. Before injecting this type of insulin, make sure you check the leaflet inside the pack for instructions on how to prepare the insulin, including to gently shake or rotate the insulin before use. Mixed insulins containing a rapid acting insulin currently available are: > NovoMix 30 (30% insulin aspart, 70% protamine crystallised insulin aspart) > HumalogMix 25 (25% insulin lispro, 75% insulin lispro protamine suspension) > HumalogMix 50 (50% insulin lispro, 50% insulin lispro protamine suspension)
insulin is injected
Mixed insulins containing a short acting insulin currently available are: > Mixtard 30/70 > Mixtard 50/50 > Humulin 30/70
5. Long acting insulin Long acting insulins are injected once or twice a day and last up to 24 hours. They are used to provide background or basal insulin. If you have type 1 diabetes, long acting insulins need to be supplemented with injections of a short or rapid acting insulin. If you have type 2 diabetes that now requires treating with insulin, you may need supplements of short or rapid acting insulin, or remain on tablets with long acting insulin only. Your doctor will advise you. Long acting insulins currently available are: > Lantus (insulin glargine)* > Levemir (insulin detemir)*
Lantus must not be mixed with any other insulin in a syringe. Lantus is available in a disposable pen called a Solostar, as well as in a 3mL cartridge for use with a durable pen device. Levemir is available in a disposable pen called a FlexPen as well as in a 3mL cartridge for use with a durable pen device.
How is insulin given?
There are many different devices available to inject insulin. The main choices include: Insulin syringes Insulin syringes are to be used with insulin vials (10 ml). Syringes are manufactured in 30 unit (0.3 ml), 50 unit (0.5 ml) and 100 unit (1.0 ml) measures. The size of the syringe will depend on the insulin dose eg: it is easier to measure a 10 unit dose in a 30 unit syringe and 55 units in a 100 unit syringe. It is best to use each syringe once only. Needles on the syringes are available in different lengths ranging from 8mm to 13mm. Your doctor or diabetes educator will help you decide which syringe is right for you. Syringes are free for people registered with the National Diabetes Services Scheme (NDSS). Contact your State or Territory Diabetes Organisation for details on 1300 136 588 or visit www.ndss.com.au. Insulin delivery devices Devices are available in different shapes and sizes. An insulin cartridge (3ml, containing 300 units of insulin) fits into the device. When finished, a new cartridge is inserted. Some pen devices, however, are pre-filled with insulin and the whole device is disposable. Your doctor or diabetes educator will advise the one thats right for your needs and lifestyle. Many people find pen devices easier and more convenient to use than syringes. hose who have difficulties with their sight or have problems with arthritis may find T the InnoLet pre-filled device or similar easy to use. Discuss this with your doctor or diabetes educator.
* Listed on PBS. Detemir for type 1 diabetes only.
d through the skin into the fatty tissue known as the sub
Revised August 2009
It is recommended that the needle be changed with each injection. Needles vary in length 5mm, 6mm, 8mm or 12mm. They also vary in thickness (or gauge) 28G, 29G, 30G or 31G. The higher the number the finer the needle. Durable devices: NovoPen 3, NovoPen 3 Demi, AutoPen and HumaPen Luxura Full and Half Dose. Pre-filled (or disposable) devices: InnoLet, FlexPen, NovoLet, Solostar and KwikPen. Needles are free for people registered with the National Diabetes Services Scheme (NDSS). Contact your State or Territory Diabetes Organisation for details on 1300 136 588 or visit www.ndss.com.au. Insulin pump The insulin pump is a small programmable device (about the size of a pager) that holds a reservoir of insulin. The pump is programmed to deliver insulin into the body through thin plastic tubing known as the infusion set or giving set. The pump is worn outside the body, in a pouch or on your belt. The infusion set has a fine needle or flexible cannula that is inserted just below the skin (usually on the abdomen) where it stays in place for two to three days. Only rapid acting insulins are used in the pump. Whenever food is eaten the pump is programmed to deliver a surge of insulin into the body similar to the way the pancreas does in people without diabetes. Between meals a small and steady rate of insulin is delivered. The insulin pump is not suitable for everyone. So, if youre considering using one, you must discuss it first with your diabetes health care team.
Where is insulin injected?
Insulin is injected through the skin into the fatty tissue known as the subcutaneous layer. You do not give it into muscle or directly into the blood. Absorption of insulin varies depending on the part of the body into which you inject. The tummy (abdomen) absorbs insulin the fastest and is the site used by most people. The upper arms, buttocks and thighs are also used by some people. While it is essential to give each injection in a slightly different spot within the one site (such as the tummy), it is not advisable to change sites without first discussing it with your doctor or diabetes educator.
bcutaneous layer
Revised August 2009
What affects the way insulin is absorbed?
Absorption is accelerated by: Injecting into an exercised area such as the thigh High temperatures (eg: shower, bath, hot water bottle, spa, sauna) Massaging the area around the injection site Injecting into muscle (the deeper the injection into muscle, the faster the insulin will be absorbed) Absorption can be delayed by: Smoking Scarring or lumps due to over-use of the same injection site, which causes the flesh to become hard and leads to erratic absorption of insulin Cold insulin (eg: injecting immediately after taking from the fridge) Variation in insulin absorption (either accelerated or delayed) can cause fluctuations in blood glucose levels Not mixing an insulin that requires reconstituting before injecting
Tips about insulin
Storage Keep your unopened insulin vials or pen cartridges on their side in the fridge. Do not allow to freeze. Once opened, insulin may be kept at room temperature (less than 30 degrees) for one month and then thrown away. Insulin can be safely carried in your handbag or pocket. Insulin may be damaged by extreme temperatures. It must not be left where temperatures are over 30 degrees (remember it can get this hot in the glove box of your car) or in direct sunlight. Insulin must not be allowed to freeze. Variation in insulin absorption (either accelerated or delayed) can cause fluctuations in blood glucose levels. Do not use insulin if: The clear insulin has turned cloudy The expiry date has been reached The insulin has been frozen or exposed to high temperatures Lumps or flakes are seen in the insulin Deposits of insulin are seen on the inside of the vial and cannot be dissolved by gently rotating the vial The vial has been open for longer than one month
insulin & diabetes
Whats the best way to dispose of used syringes?
Used syringes, pen needles and lancets must be disposed of in an Australian Safety Standards-approved sharps container which is puncture-proof and has a secure lid. These are usually yellow in colour and are available through pharmacies and your State or Territory Diabetes Organisation. Procedures to dispose of sharps containers vary from State to State. Contact your State or Territory Diabetes Organisation on 1300 136 588, your State Department of Health or Local Council for information. Many countries need insulin. If you have spare in-date insulin, please donate to your State or Territory Diabetes Organisation on 1300 136 588 or send directly to Insulin for Life Inc., PO Box 2010 Ballarat Mail Centre, Vic 3354.
Would you like to join Australias leading diabetes organisation?
> Dietary services > Educational literature > Free magazines > Product discounts > Childrens services > Support groups
For more information phone 1300 136 588 or visit your State/Territory Organisations website: ACT NT SA VIC www.diabetes-act.com.au www.healthylivingnt.org.au www.diabetessa.com.au www.diabetesvic.org.au NSW QLD TAS WA www.diabetesnsw.com.au www.diabetesqld.org.au www.diabetestas.com.au www.diabeteswa.com.au
The design, content and production of this diabetes information sheet has been undertaken by: > Diabetes Australia NSW > Diabetes Australia Victoria > Diabetes Australia Queensland > Diabetes Australia Tasmania > Diabetes ACT > Diabetes SA > Diabetes WA > Healthy Living NT The original medical and educational content of this information sheet has been reviewed by the Health Care and Education Committee of Diabetes Australia Ltd. Photocopying this publication in its original form is permitted for educational purposes only. Reproduction in any other form by third parties is prohibited. For any matters relating to this information sheet, please contact National Publications at dapubs@tpg.com.au or phone 02 9527 1951.
Health professionals: For bulk copies of this resource, contact Diabetes Australia in your State/Territory. Revised August 2009 A diabetes information series from State / Territory organisations of Diabetes Australia Copyright 2009
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Diab Care 0504Документ7 страницDiab Care 0504Ady SetiadyОценок пока нет
- ID Gambaran Kadar Lipid Trigliserida Pada PДокумент5 страницID Gambaran Kadar Lipid Trigliserida Pada PEstiPramestiningtyasОценок пока нет
- Redefining The Diagnosis of Diabetes Using Glycated HemoglobinДокумент2 страницыRedefining The Diagnosis of Diabetes Using Glycated HemoglobinEstiPramestiningtyasОценок пока нет
- 1 PBДокумент3 страницы1 PBEstiPramestiningtyasОценок пока нет
- 1478 7547 7 5Документ12 страниц1478 7547 7 5EstiPramestiningtyasОценок пока нет
- 04 PDFДокумент12 страниц04 PDFEstiPramestiningtyasОценок пока нет
- CG 87 Short GuidelineДокумент102 страницыCG 87 Short GuidelineEstiPramestiningtyasОценок пока нет
- USP 37 (795) Pharm. Comp. Non-Sterile PrepДокумент8 страницUSP 37 (795) Pharm. Comp. Non-Sterile PrepEstiPramestiningtyasОценок пока нет
- Malaria JournalДокумент11 страницMalaria JournalEstiPramestiningtyasОценок пока нет
- Hyper GlycemiaДокумент32 страницыHyper GlycemiaEstiPramestiningtyasОценок пока нет
- Usp 2008 P 2 Supplement 3Документ166 страницUsp 2008 P 2 Supplement 3EstiPramestiningtyas100% (1)
- Disease The British Journal of Diabetes & VascularДокумент6 страницDisease The British Journal of Diabetes & VascularEstiPramestiningtyasОценок пока нет
- Karakteristik Penderita Diabetes Mellitus Dengan Komplikasi Yang Di Rawat Inap Di RSUD Deli Serdang Tahun 2012 Fitriana Butarbutar, Hiswani, JemadiДокумент10 страницKarakteristik Penderita Diabetes Mellitus Dengan Komplikasi Yang Di Rawat Inap Di RSUD Deli Serdang Tahun 2012 Fitriana Butarbutar, Hiswani, JemadiEstiPramestiningtyasОценок пока нет
- FINAL Standalone Management of Hyperglycemia GuidelineДокумент40 страницFINAL Standalone Management of Hyperglycemia GuidelineDavid Tibidor JaraОценок пока нет
- Diabetes Melitus Treatment GuideДокумент104 страницыDiabetes Melitus Treatment GuideBogdan Petrescu0% (1)
- 474C15E9-066F-45ED-9B49-85C5ED9BF548Документ4 страницы474C15E9-066F-45ED-9B49-85C5ED9BF548EstiPramestiningtyasОценок пока нет
- Appl Numeric Math 06Документ15 страницAppl Numeric Math 06EstiPramestiningtyasОценок пока нет
- Vol 5 3 Org3 HeinemannДокумент6 страницVol 5 3 Org3 HeinemannEstiPramestiningtyasОценок пока нет
- Combination Treatment With Insulin and Oral Agents in Type 2 Diabetes MellitusДокумент6 страницCombination Treatment With Insulin and Oral Agents in Type 2 Diabetes MellitusEstiPramestiningtyasОценок пока нет
- Adiposity Compared With Physical Inactivity and Risk of Type 2 Diabetes in WomenДокумент6 страницAdiposity Compared With Physical Inactivity and Risk of Type 2 Diabetes in WomenEstiPramestiningtyasОценок пока нет
- Diabetes Management in General Practice 2013Документ96 страницDiabetes Management in General Practice 2013jukunkОценок пока нет
- Diabetes Melitus Treatment GuideДокумент104 страницыDiabetes Melitus Treatment GuideBogdan Petrescu0% (1)
- Who DMG PDFДокумент65 страницWho DMG PDFShelly Silvia BintangОценок пока нет
- 481 3533 5 PBДокумент13 страниц481 3533 5 PBEstiPramestiningtyasОценок пока нет
- 10 11648 J SJCM 20120101 12Документ6 страниц10 11648 J SJCM 20120101 12EstiPramestiningtyasОценок пока нет
- 1 PBДокумент3 страницы1 PBEstiPramestiningtyasОценок пока нет
- Sulfonylurea 18 5 A RДокумент32 страницыSulfonylurea 18 5 A REstiPramestiningtyasОценок пока нет
- CJD July 2011 Position StatementДокумент3 страницыCJD July 2011 Position StatementJose RobledoОценок пока нет
- 1478 7547 7 5Документ12 страниц1478 7547 7 5EstiPramestiningtyasОценок пока нет
- Diab Care 0504Документ7 страницDiab Care 0504Ady SetiadyОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- MedicalerrorДокумент38 страницMedicalerrorchanda jabeenОценок пока нет
- Assessing The Ear and HearingДокумент32 страницыAssessing The Ear and HearingArlyn Mendenilla0% (1)
- Strengthening Grief Support For Adolescents Coping With A Peer's DeathДокумент19 страницStrengthening Grief Support For Adolescents Coping With A Peer's DeatharisuimasuОценок пока нет
- Persistent Prelethal Stress Leads To Cellular AdaptationДокумент14 страницPersistent Prelethal Stress Leads To Cellular AdaptationMalliga SundareshanОценок пока нет
- Wild and Ancient Fruit - Is It Really Small, Bitter, and Low in Sugar - Raw Food SOSДокумент73 страницыWild and Ancient Fruit - Is It Really Small, Bitter, and Low in Sugar - Raw Food SOSVictor ResendizОценок пока нет
- Pathophysiology of Typhoid FeverДокумент3 страницыPathophysiology of Typhoid FeverKristofer Karlo Cabrera Castillo0% (1)
- Renal Pharmacology 2023Документ116 страницRenal Pharmacology 2023sami MesfinОценок пока нет
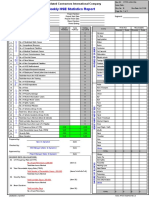
- Hse Statistics Report Pp701 Hse f04 Rev.bДокумент1 страницаHse Statistics Report Pp701 Hse f04 Rev.bMohamed Mouner100% (1)
- Pyometra in A Cat: A Clinical Case Report: November 2021Документ7 страницPyometra in A Cat: A Clinical Case Report: November 2021Ronny Alberto GallegoОценок пока нет
- Acute PoisoningДокумент5 страницAcute PoisoningrlinaoОценок пока нет
- Cervical Speculum ExaminationДокумент41 страницаCervical Speculum ExaminationEdwin Delos Reyes AbuОценок пока нет
- Sandlewood Health BenefitsДокумент7 страницSandlewood Health BenefitskalaimaniОценок пока нет
- Teaching Medical Students Basic Principles of Laboratory MedicineДокумент14 страницTeaching Medical Students Basic Principles of Laboratory MedicineIrish De VeraОценок пока нет
- Lung Cancer Prediction Using Data Mining TechniquesДокумент6 страницLung Cancer Prediction Using Data Mining TechniquesKEZZIA MAE ABELLAОценок пока нет
- PANCE Prep Pearls Cardio Questions PDFДокумент9 страницPANCE Prep Pearls Cardio Questions PDFkat100% (3)
- Anatomy and Physiology of Male Reproductive SystemДокумент8 страницAnatomy and Physiology of Male Reproductive SystemAdor AbuanОценок пока нет
- Nu 712 Health DisparitiesДокумент5 страницNu 712 Health Disparitiesapi-555218722Оценок пока нет
- Arcega ErlindaДокумент7 страницArcega ErlindaIvonne TernidaОценок пока нет
- Abdominal Health AssessmentДокумент11 страницAbdominal Health Assessmentcrisel costalesОценок пока нет
- Holi With Natural ColoursДокумент1 страницаHoli With Natural Coloursankush014Оценок пока нет
- The Nurse Leader's Role: Crisis ManagementДокумент3 страницыThe Nurse Leader's Role: Crisis Managementravsab GaikwadОценок пока нет
- BOMSS Standards For Clinical ServicesДокумент4 страницыBOMSS Standards For Clinical ServiceskintОценок пока нет
- Semey State Medical University: Department of Psychiatry Topic Schizophrenia Raja Ali HassanДокумент45 страницSemey State Medical University: Department of Psychiatry Topic Schizophrenia Raja Ali HassanRaja HassanОценок пока нет
- One Answer To Cancer by William Donald Kelley, D.D.S., M.S.Документ53 страницыOne Answer To Cancer by William Donald Kelley, D.D.S., M.S.Teti Haxhidauti94% (16)
- Respiratory PhysiologyДокумент16 страницRespiratory PhysiologyYsabel Salvador DychincoОценок пока нет
- Demography Using Cemetery DataДокумент5 страницDemography Using Cemetery DatamjbdobleuОценок пока нет
- Community Radio Script - Why We Have COVID Vaccines NowДокумент2 страницыCommunity Radio Script - Why We Have COVID Vaccines NowBenBuilds PHОценок пока нет
- Medsurg 3 Exam 1Документ55 страницMedsurg 3 Exam 1Melissa Blanco100% (1)
- 40 Fed. Reg. 8912 (1975) PDFДокумент19 страниц40 Fed. Reg. 8912 (1975) PDFaweiner100% (1)
- Myths PDFДокумент8 страницMyths PDFLuisa Elena HernandezОценок пока нет