Академический Документы
Профессиональный Документы
Культура Документы
Asthma Article Careplan
Загружено:
Cristina CenturionИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Asthma Article Careplan
Загружено:
Cristina CenturionАвторское право:
Доступные форматы
Asthma: Implications and Nursing Interventions
By Annie Collins, RN, MSN
The author of this article, Annie Collins describes the importance of applying better treatment management and nursing interventions in order to obtain more substantial outcomes in the health of clients with asthma. This disease is characterized by inflammation and hyper-responsiveness, with narrowing of the airways resulting in airway constriction and reducing oxygen supply. These symptoms can be mild but can also be life threatening in certain cases and result in a decline of their quality of life. When the disease is not well controlled, the patients activities and daily routine are limited and children can even miss school days and adults can miss days of work. Asthma prevalence increased from 2001 to 2010: An estimated 25.7 million persons had asthma in 2010. Certain demographic groups have higher asthma prevalence, like children aged 017 years, females, black people, people of multiple race, Puerto Rican people, and people with a family income below the poverty level. Increasing necessity of medical attention means also increasing on healthcare costs. The author mentions different interventions including accurate diagnosis, ongoing education for clients and their families, and the use of inhaled corticosteroids to reduce inflammatory response, to make the management of asthma more effective. The patients need to know the proper use of short and long-term medications, and the environmental triggers that exacerbate their asthma. The nursing intervention of education should include improving symptom identification by the clients and the use of peak flow meter to set a baseline for assessing lung function. The author states that increased asthma emergency room visits, hospitalizations, mortality and morbidity are associated with delay treatment and the inability of the client, or their families to identify accurately the severity of their symptoms. The writer also mentions that is necessary to adhere to daily medication regimens and daily adjustments if lung function changes, in order to obtain positive health outcomes. The client must be able to determine the level of lung function in order to accurately medicate and use interventions to reduce and prevent acute exacerbations of asthma. Nurses and patients or the patients families need to be aware and have information about the effects of chronic inflammation on the airways. These effects result in airway remodeling characterized by thickening of the sub-epithelial layers in the bronchial tree, and this can be prevented with appropriate therapy and frequent follow-up with a nurse trained in asthma management. The client or parents must understand the role of triggers and how to avoid them, the difference between rescue drugs and control drugs, the importance of inhaled corticosteroids in reducing inflammation and maintenance of the airway mucosa integrity. The routine use of inhaled corticosteroids has been shown to reduce the number of emergency room visits by 80% and the risk of death by 21%.
Despite the fact that there have been national guidelines for asthma management in existence for years, not all nurses or physicians follow them and there is little follow-up and education of the client regarding their individual medication protocols. Asthma remains undertreated by physicians with little use of inhaled corticosteroids, and the consequence of this is that patients in emergency room respond less to bronchodilators because there is airway remodeling resulting from chronic airway narrowing. Community based interventions for children with asthma should encourage all school districts to adopt protocols that include assessment, referral and education to students. School nurses should include not only screening for hearing, vision and other diseases, but also asthma screening. The author says that when asthma is properly managed it can achieve minimal or no chronic symptoms or exacerbations and normal or near normal pulmonary function, and the client can improve their quality of life. It is important to keep a trustful relationship and open communication between the health care provider, parents and children with asthma, and the nurse needs to be current in their knowledge of resources on asthma in order to be able to share them with the families and patients. This will promote reduction in the loss of school days, greater engagement in physical activity, less visits to emergency room, and improved quality of life. Nurses acting as patient advocates have to promote assessment, diagnosis and patients education. Early assessment to prevent airway remodeling, incorporation of national asthma guidelines, individualized management and medication monitoring will help to obtain better outcomes in asthma care.
References
Collins, A. (2007). Asthma: Implications and Nursing Interventions. The Kansas nurse. 82, 6-8. Web Nov 16, 2012. Retrieved from CINAHL Plus with Full Text Database: ( AN: 2009813473) http://lib1.lib.sunysuffolk.edu:2184/ehost/search/advanced?sid=4ed096734c33-4b56-9fed-b30412b35c40%40sessionmgr115&vid=2&hid=103
Вам также может понравиться
- Emergency DrugsДокумент2 страницыEmergency DrugsCristina CenturionОценок пока нет
- Neurological Stressors III Chronic Neurological Disorders: Joy Borrero, RN, MSN and NUR240 Nursing StudentsДокумент38 страницNeurological Stressors III Chronic Neurological Disorders: Joy Borrero, RN, MSN and NUR240 Nursing StudentsCristina CenturionОценок пока нет
- Brother Manual Kh950iДокумент199 страницBrother Manual Kh950iCristina CenturionОценок пока нет
- Nclex MedicationsДокумент39 страницNclex MedicationsCristina Centurion100% (2)
- Sociology 1Документ19 страницSociology 1Cristina CenturionОценок пока нет
- Nclex TermsДокумент48 страницNclex TermsCristina Centurion100% (2)
- Anxiety Class & Copy11-2Документ33 страницыAnxiety Class & Copy11-2Cristina CenturionОценок пока нет
- Cranial Nerves Assessment FormДокумент3 страницыCranial Nerves Assessment FormCristina CenturionОценок пока нет
- Chair ExercisesДокумент5 страницChair ExercisesCristina CenturionОценок пока нет
- Thyroid StormДокумент6 страницThyroid StormCristina CenturionОценок пока нет
- Mood Disorders Class & Copy 11-1Документ43 страницыMood Disorders Class & Copy 11-1Cristina CenturionОценок пока нет
- Cardiac DrugsДокумент35 страницCardiac DrugsCristina Centurion100% (3)
- Nclex Made Incredible Easy - Cardio AnswersДокумент16 страницNclex Made Incredible Easy - Cardio AnswersCristina CenturionОценок пока нет
- Pharmacology OverviewДокумент33 страницыPharmacology OverviewCristina CenturionОценок пока нет
- Sociology: Chapter 1Документ4 страницыSociology: Chapter 1Cristina CenturionОценок пока нет
- Ethical Dilemmas in Nursing - Code GrayДокумент24 страницыEthical Dilemmas in Nursing - Code GrayCristina Centurion100% (1)
- Substance Abuse QuestionsДокумент3 страницыSubstance Abuse QuestionsCristina CenturionОценок пока нет
- Sociology: Chapter 1Документ4 страницыSociology: Chapter 1Cristina CenturionОценок пока нет
- Sociology: Chapter 1Документ4 страницыSociology: Chapter 1Cristina CenturionОценок пока нет
- Substance Abuse NclexДокумент4 страницыSubstance Abuse NclexCristina Centurion100% (3)
- Child Abuse and NeglectДокумент1 страницаChild Abuse and NeglectCristina CenturionОценок пока нет
- Impaired Gas Exchange R/T Ventilation-Perfusion Imbalance Care PlanДокумент2 страницыImpaired Gas Exchange R/T Ventilation-Perfusion Imbalance Care PlanCristina Centurion100% (10)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Healthcare Waste Management EssentialsДокумент10 страницHealthcare Waste Management EssentialsMohamedErrmaliОценок пока нет
- Seddon and Sunderland Nerve Injury ClassificationДокумент8 страницSeddon and Sunderland Nerve Injury ClassificationAndres AcostaОценок пока нет
- Nur81 NCP GastroДокумент4 страницыNur81 NCP GastroJordan Gonzales100% (1)
- NUR 102 - Chapter 14 Fluid and ElectrolytesДокумент32 страницыNUR 102 - Chapter 14 Fluid and ElectrolytesIanna J. L. Pedrosa100% (1)
- Diabetes Mellitus DescritionДокумент5 страницDiabetes Mellitus DescritionTinke WinkeОценок пока нет
- Z50 Transducer Ficha Tecnica SheetДокумент3 страницыZ50 Transducer Ficha Tecnica SheetMarcos CharmeloОценок пока нет
- Imaging of Ventricular Septal Defect - Rizki Yuda PurnomoДокумент18 страницImaging of Ventricular Septal Defect - Rizki Yuda PurnomoRizkiYudaPurnomoОценок пока нет
- Penatalaksanaan Fisioterapi Pada Penderita Gangguan Nyeri Akibat Sindrom Piriformis Dengan Teknik Strain Counterstrain Dan Contract Relax StretchingДокумент7 страницPenatalaksanaan Fisioterapi Pada Penderita Gangguan Nyeri Akibat Sindrom Piriformis Dengan Teknik Strain Counterstrain Dan Contract Relax Stretchingchyntia eryonzaОценок пока нет
- Anti Thyroid DrugsДокумент22 страницыAnti Thyroid DrugsShahid HameedОценок пока нет
- Endoscopic DacryocystorhinostomyДокумент17 страницEndoscopic Dacryocystorhinostomyapi-19500641Оценок пока нет
- Red Cross Medical CertificateДокумент2 страницыRed Cross Medical CertificateScribdTranslationsОценок пока нет
- Retina: Zarieh Dawn L. Novela Medicine 2Документ50 страницRetina: Zarieh Dawn L. Novela Medicine 2Zari NovelaОценок пока нет
- Extrahepatic Biliary AtresiaДокумент3 страницыExtrahepatic Biliary AtresiaTiti Afrianto100% (1)
- Amphotericin B Deoxycholate (Conventional) - Drug Information - UpToDate-1Документ4 страницыAmphotericin B Deoxycholate (Conventional) - Drug Information - UpToDate-1Vh TRОценок пока нет
- Nursing Management of A Patient With Close FractureДокумент15 страницNursing Management of A Patient With Close FractureJoshuaYapОценок пока нет
- Document (4) FNCP PrioritizationДокумент7 страницDocument (4) FNCP Prioritizationrose angelaОценок пока нет
- Chapter 23: Cancer Development Test Bank: Multiple ChoiceДокумент11 страницChapter 23: Cancer Development Test Bank: Multiple ChoiceNurse UtopiaОценок пока нет
- Chapter 31 Dyslipidemia UpdatedДокумент37 страницChapter 31 Dyslipidemia UpdatedMai TarekОценок пока нет
- MORPHINEДокумент39 страницMORPHINEShlok RathodОценок пока нет
- HSYLCSyllabus Beijing 2016Документ5 страницHSYLCSyllabus Beijing 2016Akshay SwaminathanОценок пока нет
- Dissociation Affect Dysregulation Somatization BVDKДокумент22 страницыDissociation Affect Dysregulation Somatization BVDKkanuОценок пока нет
- Nnewfile 2Документ2 страницыNnewfile 2mahariyaОценок пока нет
- Hydrocephalus AND Neural Tube DefectДокумент7 страницHydrocephalus AND Neural Tube DefectTherese ArellanoОценок пока нет
- Emanation of CovidДокумент4 страницыEmanation of Covidmarion sebastianОценок пока нет
- Endocrine Gland Disorders and MetabolismДокумент74 страницыEndocrine Gland Disorders and MetabolismRatnam hospitalОценок пока нет
- Community DentistryДокумент11 страницCommunity DentistryMunir AkhtarОценок пока нет
- Pelvic Traction SlingДокумент3 страницыPelvic Traction SlingArturo Jr Garces RNОценок пока нет
- Fluid and Electrolyte BalanceДокумент83 страницыFluid and Electrolyte BalanceRubinaОценок пока нет
- Clinical Abstract: Bañag, Daraga, Albay Contact Nos.: (Globe) 09271684061 (Smart) 09475160066Документ1 страницаClinical Abstract: Bañag, Daraga, Albay Contact Nos.: (Globe) 09271684061 (Smart) 09475160066kolintang1Оценок пока нет
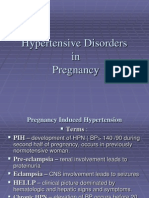
- 001hypertensive Disorders in Pregnancy PDFДокумент23 страницы001hypertensive Disorders in Pregnancy PDFRosechelle Bas SamsonОценок пока нет