Академический Документы
Профессиональный Документы
Культура Документы
Peritoneal Dialysis WK 6
Загружено:
Reem NurИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Peritoneal Dialysis WK 6
Загружено:
Reem NurАвторское право:
Доступные форматы
Ateneo de Zamboanga University
College of Nursing NURSING SKILLS OUTPUT (NSO) Report No. 2 PERITONEAL DIALYSIS
Description: Peritoneal dialysis is a dialysis procedure performed to correct an imbalance of fluid or of electrolytes in the blood or to remove toxins, drugs, or other wastes normally excreted by the kidney. The peritoneum is used as a diffusible membrane. Purpose: 1. To relieve symptoms of renal failure temporarily until the person regains kidney function. 2. To sustain life in the person with irreversible kidney disease until a successful kidney transplant is done. 3. It provides the patient more independence and mobility than hemodialysis.
Materials/ Equipment needed: Transfer Set Dialysis Solution Cycler Container/ drain Solution Storage Heater bag Fluid meter
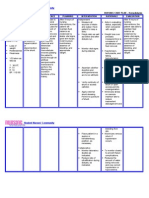
Procedure Pre-Dialysis Care 1. Document vital signs including temperature, orthostatic blood pressures (lying, sitting, and standing), apical pulse, respirations, and lung sound. (These baseline data help assess fluid volume status and tolerance of the dialysis procedure. Hypertension, abnormal heart or lung sounds, or dyspnea may indicate excess fluid volume. Poor respiratory function may affect the ability to tolerate peritoneal dialysis. Temperature measurement is vital, because infection is the most common complication of peritoneal dialysis). 2. Weigh daily or between dialysis runs as indicated. Weight is an accurate indicator of fluid volume status. Note BUN, serum electrolyte, creatinine, pH, and hematocrit levels prior to peritoneal dialysis and periodically during the procedure. These values are used to assess the efficacy of treatment. 3. Measure and record abdominal girth. Increasing abdominal girth may indicate retained dialysate, excess fluid volume, or early peritonitis. 4. Maintain fluid and dietary restrictions as ordered. Fluid and diet restrictions help reduce hypervolemia and control azotemia. 5. Have the client empty the bladder prior to catheter insertion. Emptying the bladder reduces the risk of inadvertent puncture. 6. Warm the prescribed dialysate solution to body temperature (98.6 F or 37 C) using a warm water bath or heating pad on low setting. Dialysate is warmed to prevent hypothermia. 7. Explain all procedures and expected sensations. Knowledge helps reduce anxiety and elicit cooperation.
Intradialysis Care 8. Use strict aseptic technique during the dialysis procedure and when caring for the peritoneal catheter. Peritonitis is a common complication of peritoneal dialysis; sterile technique reduces the risk. 9. Add prescribed medications to the dialysate; prime the tubing with solution and connect it to the peritoneal catheter, taping connections securely and avoiding kinks. This allows dialysate to flow freely into the abdominal cavity and prevents leaking or contamination. 10. Instill dialysate into the abdominal cavity over a period of approximately 10minutes. Clamp tubing and allow the dialysate to remain in the abdomen for the prescribed dwell time. 11. Keep drainage tubing clamped at all times during instillation and dwell time. Dialysate should flow freely into the abdomen if the peritoneal catheter is patent. Dialysis, the exchange of solutes and water between the blood and dialysate, occurs across the peritoneal membrane during the dwell time. 12. During instillation and dwell time, observe closely for signs of respiratory distress, such as dyspnea, tachypnea, or crackles. Place in Fowlers or Semi-Fowlers position and slow the rate of instillation slightly to relieve respiratory distress if it develops. Respiratory compromise may result from overly rapid filling or overfilling of the abdomen or from a diaphragmatic defect that allows fluid to enter the thoracic cavity. 13. After prescribed dwell time, open drainage tubing clamps and allows dialysate to drain by gravity into a sterile container. 14. Note the clarity, color, and odor of returned dialysate. Blood or feces in the dialysate may indicate organ or bowel perforation; cloudy or malodorous dialysate may indicate an infection. 15. Accurately record amount and type of dialysate instilled (including any added medications), dwell time, and amount and character of the drainage. When more dialysate drains than has been instilled, excess fluid has been lost (output). If less dialysate is returned than has been instilled, a fluid gain has occurred (intake). 16. Monitor BUN, serum electrolyte, and creatinine levels. These values are used to assess the effectiveness of dialysis. 17. Troubleshoot for possible problems during dialysis. a) Slow dialysate instillation. Increase the height of the container and reposition the client. Check tubing and catheter for kinks. Check abdominal dressing for wetness, indicating leakage around the catheter. Slow dialysate flow may be related to a partially obstructed tube or catheter. b) Excess dwell time. Prolonged dwell time may lead to water depletion or hyperglycemia. c) Poor dialysate drainage. Lower the drainage container, reposition, and check for tubing kinks. Post-dialysis Care 18. Assess vital signs, including temperature. Comparison of pre and post-dialysis vital signs helps identify beneficial and adverse effects of the procedure. 19. Time meals to correspond with dialysis outflow. Scheduling meals while the abdomen is empty of dialysate enhances intake and reduces nausea. 20. Teach the client and family about the procedure. The client may elect to use peritoneal dialysis at home to manage end-stage renal disease and prevent uremia.
Diagram/Illustration
Reference: RECOMMENDED TEXT: Lippincott Manual of Nursing Practic1e by LWW, pp699
July 27, 2012 Date
NUR, REEM. A BSN IV - D
Antonia R. Quilos RN, MN Clinical Instructor
Вам также может понравиться
- Anatomy & Physiology PeritoneumДокумент42 страницыAnatomy & Physiology Peritoneumkets143Оценок пока нет
- CCRN-PCCN Review RenalДокумент11 страницCCRN-PCCN Review RenalGiovanni MictilОценок пока нет
- 313 - Disorders of Renal and Urinary SystemsДокумент8 страниц313 - Disorders of Renal and Urinary SystemsChrissy Mendoza100% (2)
- Dialysis Definition and FactsДокумент6 страницDialysis Definition and FactsAilen Rose PuertasОценок пока нет
- Hemodialysis and Peritoneal DialysisДокумент57 страницHemodialysis and Peritoneal Dialysisirene joy91% (11)
- Chest Tube ThoracostomyДокумент6 страницChest Tube ThoracostomyRhea Lyn LamosteОценок пока нет
- Liver Biopsy and AbdominalДокумент25 страницLiver Biopsy and AbdominalAfiq Mubasyyir AmranОценок пока нет
- DialysisДокумент5 страницDialysisAnusha Verghese100% (1)
- Hirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandHirschsprung’s Disease, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- DIALYSIS ReportingДокумент10 страницDIALYSIS ReportingGlenelyn Grace InfanteОценок пока нет
- Nursing Management of Patient Undergoing Peritoneal DialysisДокумент27 страницNursing Management of Patient Undergoing Peritoneal DialysisHemantОценок пока нет
- HemodyalisisДокумент148 страницHemodyalisisRatnaSuryatiОценок пока нет
- Assisting in Gastric LavageДокумент5 страницAssisting in Gastric LavageJannen Casas100% (1)
- Peritoneal Dialysis (PD) : Dr. Dwi Edi Wahono, SPPDДокумент62 страницыPeritoneal Dialysis (PD) : Dr. Dwi Edi Wahono, SPPDM. Tarmizi TaherОценок пока нет
- Manual Liberty SelectДокумент2 страницыManual Liberty SelectMarcos AcioliОценок пока нет
- 8 Irrigating A ColostomyДокумент5 страниц8 Irrigating A ColostomyAnn Jalover PerezОценок пока нет
- Nasogastric & Gavage - NsoДокумент5 страницNasogastric & Gavage - NsojamesОценок пока нет
- CYSTOCLYSIS3Документ9 страницCYSTOCLYSIS3Alvin OccianoОценок пока нет
- Drug DialysabilityДокумент61 страницаDrug DialysabilityMohamed Essam ElraggalОценок пока нет
- NSO Gastric LavageДокумент3 страницыNSO Gastric Lavagetry dokkОценок пока нет
- Percutaneous Transhepatic CholangiographyДокумент3 страницыPercutaneous Transhepatic CholangiographyRonel UsitaОценок пока нет
- Gastric LavageДокумент2 страницыGastric LavageIrish Eunice FelixОценок пока нет
- Rahman Institute of Nursing and Paramedical Sciences, Radhanagar, Guwahati Demonstration ON Peritoneal DialysisДокумент7 страницRahman Institute of Nursing and Paramedical Sciences, Radhanagar, Guwahati Demonstration ON Peritoneal DialysisPuy Puy ChhangteОценок пока нет
- Peritoneal DialysisДокумент3 страницыPeritoneal DialysisSumit YadavОценок пока нет
- CefuroximeДокумент2 страницыCefuroximeReem NurОценок пока нет
- DT Peritoneal Dialysis DektaДокумент21 страницаDT Peritoneal Dialysis Dektailham nugrohoОценок пока нет
- Procedure - Gastric LavageДокумент2 страницыProcedure - Gastric LavageJose Paul RaderОценок пока нет
- NGT Feeding ChecklistДокумент1 страницаNGT Feeding ChecklistJoycee BoОценок пока нет
- Peritoneal DialysisДокумент37 страницPeritoneal Dialysisger668Оценок пока нет
- Nso ErcpДокумент3 страницыNso Ercptry dokkОценок пока нет
- Hypertension NclexДокумент5 страницHypertension Nclexハニファ バランギОценок пока нет
- Colostomy IrrigationДокумент3 страницыColostomy IrrigationJikko Verra GarciaОценок пока нет
- Assisting in Application of Plaster of ParisДокумент2 страницыAssisting in Application of Plaster of ParisGopi RajОценок пока нет
- Intravenous Pyelography: Week 5Документ2 страницыIntravenous Pyelography: Week 5Shaina Angelique SaliОценок пока нет
- Bacillary DysenteryДокумент32 страницыBacillary Dysenteryapi-199163990% (1)
- Ateneo de Zamboanga University College of Nursing NCM 112j RLEДокумент3 страницыAteneo de Zamboanga University College of Nursing NCM 112j RLEsenyorakath0% (1)
- TahbsoДокумент4 страницыTahbsomichZ_13Оценок пока нет
- Water Sealed DrainageДокумент2 страницыWater Sealed DrainagefairwoodsОценок пока нет
- Nursing Care PlanДокумент8 страницNursing Care PlanVincent QuitorianoОценок пока нет
- Cerebral Aneurysm Case Analysis and Concept MapДокумент5 страницCerebral Aneurysm Case Analysis and Concept Mapate NarsОценок пока нет
- Surgical Management For Cryptorchidism With Nursing ManagementsДокумент4 страницыSurgical Management For Cryptorchidism With Nursing ManagementsAprille Claire MoralesОценок пока нет
- CystocylsisДокумент7 страницCystocylsisJennifer DimapilisОценок пока нет
- Nasogastric Tube FeedingДокумент4 страницыNasogastric Tube FeedingAru VermaОценок пока нет
- Diagnostic Test For Endocrine DisordersДокумент15 страницDiagnostic Test For Endocrine DisordersRichard Deo R. Alave100% (1)
- Angiotensin Converting Enzyme (ACE) InhibitorsДокумент4 страницыAngiotensin Converting Enzyme (ACE) InhibitorsPutri Mulia HasibuanОценок пока нет
- A Case Presentation On CholedocholithiasisДокумент11 страницA Case Presentation On CholedocholithiasisPaul Vincent EspereОценок пока нет
- CNN Practice QuestionsДокумент5 страницCNN Practice QuestionsUri Perez MontedeRamosОценок пока нет
- Urinalysis: PurposeДокумент6 страницUrinalysis: PurposebobtagubaОценок пока нет
- Acute Cholecystitis Ppt. DR Dilip S. RajpalДокумент42 страницыAcute Cholecystitis Ppt. DR Dilip S. Rajpaldiliprajpal73100% (1)
- Measuring Intake and OutputДокумент1 страницаMeasuring Intake and OutputCJ AngelesОценок пока нет
- Types and Collection of Urine SpecimenДокумент12 страницTypes and Collection of Urine SpecimengireeshsachinОценок пока нет
- NSO Breast Self ExamДокумент4 страницыNSO Breast Self ExamGio Mangaya-ayОценок пока нет
- Potassium ChlorideДокумент2 страницыPotassium ChlorideSetiram Zenitram50% (2)
- Module 2 - Case 1Документ9 страницModule 2 - Case 1Joselyn M. LachicaОценок пока нет
- HemodialysisДокумент2 страницыHemodialysisRA Ferrer de RomaОценок пока нет
- HernioplastyДокумент6 страницHernioplastyCherry Delos ReyesОценок пока нет
- Case Study - Dengue Fever V - S UtiДокумент12 страницCase Study - Dengue Fever V - S UtiHarlene Joyce ReyОценок пока нет
- BaclofenДокумент2 страницыBaclofenamiraОценок пока нет
- Imbalanced Nutrition: Less Than Body Requirements R/T Diarrhea Due To Excessive OutputДокумент2 страницыImbalanced Nutrition: Less Than Body Requirements R/T Diarrhea Due To Excessive OutputMark BarengОценок пока нет
- Kabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseДокумент24 страницыKabiven: (Amino Acids, Electrolytes, Dextrose and Lipid Injectable Emulsion), For Intravenous UseDivine Mercy De JulianОценок пока нет
- ARTHROCENTESISДокумент2 страницыARTHROCENTESISJairene Dave Martinez CambalonОценок пока нет
- PeritonitisДокумент6 страницPeritonitisDiane ArgoteОценок пока нет
- Dela Rosa 2A MCN-Module 05Документ2 страницыDela Rosa 2A MCN-Module 05Atsu MiyaОценок пока нет
- Care of Patient With: Chest DrainageДокумент29 страницCare of Patient With: Chest DrainageMSc. PreviousОценок пока нет
- Post Op Worksheet FinalДокумент5 страницPost Op Worksheet FinalRiza Angela BarazanОценок пока нет
- Risk For Bleeding - Cirrhosis NCPДокумент2 страницыRisk For Bleeding - Cirrhosis NCPPaula AbadОценок пока нет
- Discharge Plan Post SeizureДокумент2 страницыDischarge Plan Post SeizureVecky TolentinoОценок пока нет
- 13 Surgery (Perioperative Client) Nursing Care Plans - NurseslabsДокумент31 страница13 Surgery (Perioperative Client) Nursing Care Plans - NurseslabsRena SafitriОценок пока нет
- Question Text: Clear My ChoiceДокумент13 страницQuestion Text: Clear My ChoiceLylibette Anne H. CalimlimОценок пока нет
- Nursing Care Plan 1Документ3 страницыNursing Care Plan 1gagandipkS100% (1)
- Preoperative Skin PreparationДокумент16 страницPreoperative Skin PreparationSyahri DzikriОценок пока нет
- Reteplase (MIRel)Документ23 страницыReteplase (MIRel)Jhoann JamanilaОценок пока нет
- Renal Dialysis PeritonealДокумент7 страницRenal Dialysis Peritonealmardsz100% (2)
- Write Up - Data Analysis & InterpretationДокумент10 страницWrite Up - Data Analysis & InterpretationReem NurОценок пока нет
- HemodialysisДокумент3 страницыHemodialysisReem NurОценок пока нет
- Stress and Academic PerformanceДокумент29 страницStress and Academic PerformanceReem NurОценок пока нет
- Antiprotozoal AgentsДокумент4 страницыAntiprotozoal AgentsReem NurОценок пока нет
- Teknik CapdДокумент2 страницыTeknik CapdtitoОценок пока нет
- 01 Diagnosis and Treatment of Peritonitis in PD Patients ECO 33732 PDFДокумент19 страниц01 Diagnosis and Treatment of Peritonitis in PD Patients ECO 33732 PDFagustОценок пока нет
- Facebook Faqs Website Faqs (Included) : Laboratory / Radiology InquiriesДокумент13 страницFacebook Faqs Website Faqs (Included) : Laboratory / Radiology InquiriesChristian SanchezОценок пока нет
- LiWorld in Peritoneal DialysisДокумент3 страницыLiWorld in Peritoneal DialysisAnthropophobe NyctophileОценок пока нет
- © Medi - Lectures DR Shubham UpadhyayДокумент27 страниц© Medi - Lectures DR Shubham Upadhyayashu13bОценок пока нет
- Peritoneal Dialysis - Associated Peritonitis: Suggestions For Management and Mistakes To AvoidДокумент9 страницPeritoneal Dialysis - Associated Peritonitis: Suggestions For Management and Mistakes To AvoidAbidi HichemОценок пока нет
- Fluid and Electrolytes, Burns, G.UДокумент56 страницFluid and Electrolytes, Burns, G.Uapi-3735995100% (4)
- SDJ 2023 Last AnnДокумент11 страницSDJ 2023 Last AnnAstutiningrum Puspa DamayantiОценок пока нет
- BONENT CPDN Exam Content PDFДокумент6 страницBONENT CPDN Exam Content PDFVashistmohan A.P.Оценок пока нет
- PDP 1Документ2 страницыPDP 1api-264038055Оценок пока нет
- What Is Peritoneal DialysisДокумент34 страницыWhat Is Peritoneal DialysisKen MagallanesОценок пока нет
- Kidney Failure (Reference Summary) : AnatomyДокумент3 страницыKidney Failure (Reference Summary) : AnatomyUSMP FN ARCHIVOSОценок пока нет
- DR Merikhi PETДокумент33 страницыDR Merikhi PETAnitha SuprionoОценок пока нет
- CAPD - StaySafe Training Manual PDFДокумент16 страницCAPD - StaySafe Training Manual PDFChris LeeОценок пока нет
- Peritoneal Dialysis in Children: Keia Sanderson, Joshua Zaritsky and Bradley A. WaradyДокумент20 страницPeritoneal Dialysis in Children: Keia Sanderson, Joshua Zaritsky and Bradley A. WaradyNi Ketut sugiatiОценок пока нет
- National Dialysis Program National Dialysis ProgramДокумент56 страницNational Dialysis Program National Dialysis ProgramsaravananОценок пока нет
- Pembicara: Dr. Orfeas Liangos - Coburg GermanyДокумент6 страницPembicara: Dr. Orfeas Liangos - Coburg GermanyRicky VirnardoОценок пока нет
- Course f2f 312 Peritoneal DialysisДокумент10 страницCourse f2f 312 Peritoneal DialysisyumulОценок пока нет