Академический Документы
Профессиональный Документы
Культура Документы
Steroid
Загружено:
Firdaus KamalОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Steroid
Загружено:
Firdaus KamalАвторское право:
Доступные форматы
Guidelines on Indications of Use of Steroids Types of Steroids Replacement Therapy glucocorticoid (hydrocortisone) mineralocorticoid (fludrocortisone) Anti-inflammatory Therapy Short
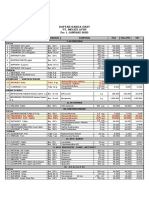
Short acting: hydrocortisone Intermediate acting: prednisolone; methylprednisolone; triamcinolone Long acting: dexamethasone Routes of Administration Systemic : oral, transrectal, IV, IM Local: topical, intranasal, intraocular, intraarticular Availability of International Guidelines on Use of Steroid No one-for-all guideline Glucocorticoid Replacement Therapy : Guidelines published by Royal College of Physicians of London, UK ; not available from Endocrine Society, USA. Systemic Use of Glucocorticoid: Guidelines available for EULAR (European League for Rheumatology) Local Use of Steroid: guidelines on individual disease, general guidelines not available Royal College of Physicians of London Guidelines on Glucocorticoid Replacement Therapy Recommended Daily Dose for Glucocorticoid Hydrocortisone (cortisol) 15-30mg Cortisone acetate 25-37.5mg Prednisolone 5-7.5mg Dexamethasone 0.5mg Recommended Daily Dose of Mineralocorticoid Fludrocortisone 100-200mcg Monitoring hydrocortisone replacement Hypoadrenalism is a rare condition and should be managed by a specialist Biochemical monitoring enables detection of minor degrees of under- or over-replacement Symptoms of hypo- or over-replacement are vague 24 h urine free cortisol measurement should be in the normal range; mid-day and evening plasma cortisol should be >50nmol/l Long-term Follow Up Regular review Steroid card/bracelet/medallion indicating the diagnosis and replacement therapy Advice for concurrent illness management and augmentation of replacement dose; IV therapy for surgery/hospitalisation College of Physicians London, UK recommend patients on glucocorticoid replacement long-term FU by endocrinologist EULAR evidence-based recommendations on the management of systemic glucocorticoid therapy in rheumatic diseases Top Number 1 Recommendation 1 a The ADVERSE effects of glucocorticoid therapy should be considered and discussed with the patient before glucocorticoid therapy is started 1 b This advice should be reinforced by giving information regarding glucocorticoid management
1 c If glucocorticoids are to be used for a more prolonged period of time, a glucocorticoid card is to be issued to every patient, with the date of commencement of treatment, the initial dosage and the subsequent reductions and maintenance regimens
EULAR Recommendation on Systemic Steroid Initial steroid dose/dosage reduction/long-term dosing depends on underlying rheumatic disease, disease activity, patient response Comorbidity should be evaluated: hypertension, DM, peptic ulcer, fractures and osteoporosis, cataract/glaucoma, infection, dyslipidaemia, NSAID Monitoring: body weight, BP, oedema, lipid, glucose, ocular pressure, cardiac insufficiency Prevention of bone loss with anti-resorptives+calcium+Vitamin D (assess of steroid dose/duration/BMD) Children should be monitored for growth IV Steroid during surgery if systemic steroid is used for >1 month Gastric protection if concomittent use of NSAID Intra-articular Steroid Injection First use dated back to 1951 by Hollander et al for arthritic joints; evidence for effectiveness was based on anecdotal studies rather than placebo-controlled trials Few facts but mostly opinions about diagnosis, which lesions to treat, optimal steroid choice, dosage, injection techniques, intervals, frequency Triamcinolone; methylprednisolone; dexamathesone. Insoluble/long-acting steroid remained in the joint, contact with inflamed synovial surface, taken up by synovial cells and absorbed into blood stream Similar side-effects as systemic steroids although the percentage of patients having side-effects is less Recommendation: injection by trained personnel, e.g. rheumatologist, orthopaedic surgeon, orthopaedic physiotherapists practitioners in certain countries Common Indications for Local Steroid Injection Trigger finger Carpel tunnel syndrome De Quervains tenosynovitis Joint Arthritis Chronic spinal pain/facet joint pain Sacroiliac joint arthritis Osteoarthritis Rheumatoid arthritis Side-effects of Steroid Injection Therapy Systemic Side-effects Facial Flushing Menstrual Irregularity Hyperglycaemia Suppress pituitary-adrenal axis Emotional upset Anaphylaxis Local Side-effects Post-injection flare of pain Skin depigmentation
Subcutaneous atrophy Bleeding Infection Steroid Arthropathy Tendon rupture/atrophy Soft tissue calcification
Prolonged steroid injection is associated with osteonecrosis Injection frequency into major joints in lower limbs at no less than 3-4 month intervals. This is based on consensus rather than evidence Joint sepsis is a known complication but rare (1 in 17,000-77,000) Injection should be given by trained personnel Use of Topical Corticosteroids according to British National Formulary Indications: inflammatory condition of the skin other than infection. Common indications: eczema, contact dermatitis, insect sting, eczema of scabies Contraindications: infection (bacteria/viral/fungal), rosacea Use of systemic and potent steroid in psoriasis should be avoided or given only under specialist supervision BNF Formulary Guide: potency grouped as Mild/Moderate/Potent/Very Potent Potent topical steroid should generally be avoided on the face and skin flexures except under special circumstances by specialist supervision Intralesional steroid injection should be reserved by severe cases/localised lesions, eg keloid scars, hypertrophic lichen planus, alopecia areata Side-effects with topical Steroid Spread/worsening of untreated infection Thinning of skin Irreversible striae and telangiectasia Contact dermatitis Perioral dermatitis Acne, worsening of acne rosacea Depigmentation Hypertichosis Caution with Topical Steroid No more frequently than twice daily, apply thinly to the affected area only Use the least potent formulation which is fully effective Avoid prolonged use on the face and keep away from eyes Caution in children and during pregnancy Suppression of pituitary adrenal axis and even cause Cushings syndrome with prolonged use in large area
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Nausea and Vomiting: Key ConceptsДокумент35 страницNausea and Vomiting: Key ConceptsMila ErnilaОценок пока нет
- CorticosteroidsДокумент63 страницыCorticosteroidsRiddhi Jain100% (2)
- Ozur DexДокумент3 страницыOzur DexMohammad Abdullah BawtagОценок пока нет
- Daftar Harga Obat - Pt. Molex Ayus - Januari 2023Документ4 страницыDaftar Harga Obat - Pt. Molex Ayus - Januari 2023Muhammad AdninОценок пока нет
- Lung Cancer Case StudyДокумент48 страницLung Cancer Case StudySahal M.Shuaib100% (4)
- Ivig GAMMARAS - FullДокумент13 страницIvig GAMMARAS - FullNisa UcilОценок пока нет
- Generic Name Brand Name Dosage Indications Mechanisms of Action Adverse Effects Nursing ResponsibilitiesДокумент10 страницGeneric Name Brand Name Dosage Indications Mechanisms of Action Adverse Effects Nursing ResponsibilitiesJennalyn CasapaoОценок пока нет
- Tobradex Eye Drops: Consumer Medicine InformationДокумент5 страницTobradex Eye Drops: Consumer Medicine InformationFranc VenturaОценок пока нет
- CorticoДокумент5 страницCorticoDR AbidОценок пока нет
- Idsa Covid 19 GL TX and MGMT v4.4.1Документ173 страницыIdsa Covid 19 GL TX and MGMT v4.4.1Galaxy SatwaОценок пока нет
- Perbandingan Dexa Dan MethylprednisoloneДокумент2 страницыPerbandingan Dexa Dan MethylprednisoloneRai Jaine DarmantaОценок пока нет
- Anatomy and Physiology Related To Multiple Myelom1Документ15 страницAnatomy and Physiology Related To Multiple Myelom1Diane Kate Tobias Magno100% (1)
- Pharmacokinetics: of OphthalmicДокумент4 страницыPharmacokinetics: of OphthalmicWina Siska Purnama BurmanОценок пока нет
- Steroid Side Effects - How To Reduce Corticosteroid Side Effects - HSSДокумент8 страницSteroid Side Effects - How To Reduce Corticosteroid Side Effects - HSSAtif RehmanОценок пока нет
- Mascc Antiemetic Guidelines English v.1.2.1Документ55 страницMascc Antiemetic Guidelines English v.1.2.1cricriОценок пока нет
- January 2021 Addendum To The Demonstration of The Falsified Romanian Drug and Human Trafficking Mafia Documents at ECHR September 2020Документ247 страницJanuary 2021 Addendum To The Demonstration of The Falsified Romanian Drug and Human Trafficking Mafia Documents at ECHR September 2020Tudor RanetiОценок пока нет
- PONV Prophylaxis GuidelinesДокумент7 страницPONV Prophylaxis GuidelinesAbby WardОценок пока нет
- Pharma 4 QДокумент1 страницаPharma 4 QMARIA PAULINA AMANTEОценок пока нет
- (Đề có 12 trang) : There are three parts in this listening test. You will hear each part twiceДокумент12 страниц(Đề có 12 trang) : There are three parts in this listening test. You will hear each part twiceTún PhạmОценок пока нет
- Multiple Myeloma ManuscriptДокумент36 страницMultiple Myeloma ManuscriptGabriel GuerreroОценок пока нет
- Guidline Mual Muntah Kemotrapi PDFДокумент10 страницGuidline Mual Muntah Kemotrapi PDFTyas TyaОценок пока нет
- Charlier Et Al. Lancet Infectious Diseases 2017Документ47 страницCharlier Et Al. Lancet Infectious Diseases 2017werwrОценок пока нет
- Drug LiteratureДокумент7 страницDrug LiteraturePatricia Anne BerganciaОценок пока нет
- Betnesol InjectionДокумент7 страницBetnesol Injectionhiral mistryОценок пока нет
- Drug StudyДокумент4 страницыDrug StudyJunel Paolo SilvioОценок пока нет
- Drugs Generally Used On Veterinary Clinics in IndiaДокумент17 страницDrugs Generally Used On Veterinary Clinics in IndiaDEV3LLS100% (1)
- Maxitrol (Neomycin and Polymyxin B Sulfates and Dexamethasone Ophthalmic Ointment) Sterile Description: MaxitrolДокумент6 страницMaxitrol (Neomycin and Polymyxin B Sulfates and Dexamethasone Ophthalmic Ointment) Sterile Description: Maxitroldjilal430Оценок пока нет
- Drug StudyДокумент7 страницDrug StudyNicxx GamingОценок пока нет
- End-of-Life Care For Brain Tumor PatientsДокумент36 страницEnd-of-Life Care For Brain Tumor PatientsNisha PradeepaОценок пока нет
- GP Factsheet - Steroids and The EyeДокумент6 страницGP Factsheet - Steroids and The EyeBima RizkiОценок пока нет