Академический Документы
Профессиональный Документы
Культура Документы
LCM, X Sa, X Xlladsvmde
Загружено:
Czarina Jeri Mae MejillaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
LCM, X Sa, X Xlladsvmde
Загружено:
Czarina Jeri Mae MejillaАвторское право:
Доступные форматы
The respiratory system is situated in the thorax, and is responsible for gaseous exchange between the circulatory system
and the outside world. Air is taken in via the upper airways (the nasal cavity, pharynx and larynx) through the lower airways (trachea, primary bronchi and bronchial tree) and into the small bronchioles and alveoli within the lung tissue. Move the pointer over the coloured regions of the diagram; the names will appear at the bottom of the screen) The lungs are divided into lobes; The left lung is composed of the upper lobe, the lower lobe and the lingula (a small remnant next to the apex of the heart), the right lung is composed of the upper, the middle and the lower lobes. Mechanics of Breathing To take a breath in, the external intercostal muscles contract, moving the ribcage up and out. The diaphragm moves down at the same time, creating negative pressure within the thorax. The lungs are held to the thoracic wall by the pleural membranes, and so expand outwards as well. This creates negative pressure within the lungs, and so air rushes in through the upper and lower airways. Expiration is mainly due to the natural elasticity of the lungs, which tend to collapse if they are not held against the thoracic wall. This is the mechanism behind lung collapse if there is air in the pleural space (pneumothorax).
Physiology of Gas Exchange Each branch of the bronchial tree eventually sub-divides to form very narrow terminal bronchioles, which terminate in the alveoli. There are many millions of alveloi in each lung, and these are the areas responsible for gaseous exchange, presenting a massive surface area for exchange to occur over. Each alveolus is very closely associated with a network of capillaries containing deoxygenated blood from the pulmonary artery. The capillary and alveolar walls are very thin, allowing rapid exchange of gases by passive diffusion along concentration gradients. CO2 moves into the alveolus as the concentration is much lower in the alveolus than in the blood, and O2 moves out of the alveolus as the continuous flow of blood through the capillaries prevents saturation of the blood with O2 and allows maximal transfer across the membrane.
Precipitating factors: >lifestyle >bacteria: staphylococcus pneumoniae
Predisposing factors: >age >sex
staphylococcus pneumoniae enters the respiratory system through inhalation/aspiration Activation of defense mechanism Penetration in the sterile lower respiratory tract Proliferation in the Alveoli Colonization of lungs by the bacteria Exudates that come from the bateria erode from the lung infection vasodilation Increase blood flow Accumulation of edematous fluids Pleural effusion Inflamed and fluid filled alveolar sac Decrease CO2 Lung consolidation hypoxia Impaired CO2 and O2 exchange >increased RR Occluded airway Increase mucus production Irritation of airways Increase goblet cells
>cough >crackles
Hyperventilation Airway constriction
DOB
Parapneumonic effusion is defined as pleural effusion associated with lung infection (ie, pneumonia). These effusions result from the spread of inflammation and infection to the pleura. Much less commonly, infections in other adjacent areas, such as the retropharyngeal, vertebral, abdominal, and retroperitoneal spaces may spread to the pleura resulting in the development of effusion. Early in the course of parapneumonic effusion, the pleura becomes inflamed; subsequent leakage of proteins, fluid, and leukocytes into the pleural space forms the effusion. At the time of formation, the pleural effusion is usually sterile with a low leukocyte count. With time, bacteria invade the fluid, resulting in empyema, which is defined as the presence of grossly purulent fluid in the pleural cavity. The development of pleural empyema is determined by a balance between host resistance, bacterial virulence, and timing of presentation for medical treatment
Parapneumonic effusion It is a common complication of bacterial pneumonia (about 40%). Most parapneumonic effusions are small and resolve with appropriate antibiotic therapy. Thoracentesis should be done if the effusion layers out to a thickness equal to or greater than 10 mm on the lateral decubitus chest radiograph to determine as early as possible if a chest tube should be placed. Pathophysiology: The spectrum of parapneumonic effusions has been divided into three stages, although they are not sharply defined and represent a point on a continuous spectrum.
1. The exudative stage which results from a focus of parenchymal infection leading
to increased pulmonary interstitial fluid. Some of this fluid crosses the visceral pleura and accumulates as a small sterile pleural effusion. The pleural fluid is an exudate with primarily PMNs, a normal glucose level, and a normal pH level. Antibiotics begun in this stage will affect resolution of both the pneumonic and pleural process. The initial sterile free flowing exudative parapneumonic effusions may rapidly progress (within a day) to the second stage. 2. The fibropurulent stage characterized by infection of sterile pleural fluid. Pleural fluid further accumulates and contains many PMNs, bacteria, and cellular debris. Fibrin deposits cover both the visceral and parietal pleura. Fibrin membrane partitions result in loculated effusion. This loculation makes complete pleural space drainage difficult. During this stage, the pleural fluid pH and glucose levels become low, LDH levels increase, and bacterial organisms or frank pus may be present. 3. The organization stage. Fibroblasts grow into the exudate from both the visceral and parietal pleural surface to produce an inelastic membrane called the pleural peel. These untreated effusions may also drain spontaneously through the chest wall (empyema necessitans) or into the lung to produce a bronchopleural fistula.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Tobacco Cessation PlanДокумент11 страницTobacco Cessation PlanEsteban García EcheverryОценок пока нет
- SCIT 1408 Applied Human Anatomy and Physiology II - Urinary System Chapter 25 BДокумент50 страницSCIT 1408 Applied Human Anatomy and Physiology II - Urinary System Chapter 25 BChuongОценок пока нет
- Bahasa InggrisДокумент6 страницBahasa InggrisSofi SusantoОценок пока нет
- The Effect of Tobacco Smoking Among Third Year Student Nurse in The University of LuzonДокумент6 страницThe Effect of Tobacco Smoking Among Third Year Student Nurse in The University of LuzonNeil Christian TadzОценок пока нет
- Complications of DiabetesДокумент3 страницыComplications of Diabetesa7wfОценок пока нет
- A Sonographic Sign of Moderate ToДокумент5 страницA Sonographic Sign of Moderate ToDivisi FER MalangОценок пока нет
- Pigeons: Animal SciencesДокумент15 страницPigeons: Animal SciencesSafi Ul RehmanОценок пока нет
- Nursing Management of HypertensionДокумент152 страницыNursing Management of HypertensionEnfermeriaAncam100% (3)
- Nowadays Young People Spend Too Much of Their Free Time in Shopping MallsДокумент3 страницыNowadays Young People Spend Too Much of Their Free Time in Shopping MallsYacine BenHmeidaОценок пока нет
- Abnormal Psychology Final Practice QuestionsДокумент16 страницAbnormal Psychology Final Practice QuestionsJames WilkesОценок пока нет
- What Is Malnutrition?: WastingДокумент6 страницWhat Is Malnutrition?: WastingĐoan VõОценок пока нет
- Is It True That GanodermaДокумент2 страницыIs It True That GanodermaRohit SharmaОценок пока нет
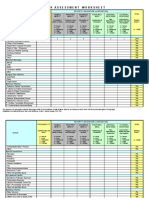
- IC Risk Assessment Worksheet - Kangas-V2.1-Aug.2010 1Документ4 страницыIC Risk Assessment Worksheet - Kangas-V2.1-Aug.2010 1Juon Vairzya AnggraeniОценок пока нет
- DSM OcdДокумент2 страницыDSM Ocdnmyza89Оценок пока нет
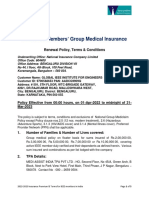
- GIEEE TGMP Policy Terms For 2022-23Документ5 страницGIEEE TGMP Policy Terms For 2022-23Janardhan Reddy TОценок пока нет
- Quiz 632 General Science For SSC ExaminationsДокумент4 страницыQuiz 632 General Science For SSC ExaminationsDibyendu SahuОценок пока нет
- A Comparative Clinical Evaluation of Eranda Taila Matra Basti With Combination of Mefenamic Acid and Dicyclomine in The Management of Udavartini W.S.R To Primary DysmenorrheaДокумент8 страницA Comparative Clinical Evaluation of Eranda Taila Matra Basti With Combination of Mefenamic Acid and Dicyclomine in The Management of Udavartini W.S.R To Primary DysmenorrheaEditor IJTSRDОценок пока нет
- Physiology of The Cell: H. Khorrami PH.DДокумент89 страницPhysiology of The Cell: H. Khorrami PH.Dkhorrami4Оценок пока нет
- Week 6 Nursing Care of The Family With Reproductive DisordersДокумент27 страницWeek 6 Nursing Care of The Family With Reproductive DisordersStefhanie Mae LazaroОценок пока нет
- Neurobiology of Sleep: Madhu Kalia4Документ5 страницNeurobiology of Sleep: Madhu Kalia4Julian ReyesОценок пока нет
- Conduction Blocks in Acute Myocardial Infarction: A Prospective StudyДокумент6 страницConduction Blocks in Acute Myocardial Infarction: A Prospective StudyJack JacksonОценок пока нет
- Celecoxib, Etoricoxib, DiclofenacДокумент13 страницCelecoxib, Etoricoxib, Diclofenacbaitur rohmahОценок пока нет
- ZFN, TALEN, and CRISPR-Cas-based Methods For Genome EngineeringДокумент9 страницZFN, TALEN, and CRISPR-Cas-based Methods For Genome EngineeringRomina Tamara Gil RamirezОценок пока нет
- Prioritization - FNCPДокумент10 страницPrioritization - FNCPJeffer Dancel67% (3)
- Resource Material - Day 1 Primary Register Activity - ANC Register - 0Документ3 страницыResource Material - Day 1 Primary Register Activity - ANC Register - 0Ranjeet Singh KatariaОценок пока нет
- 1 To 3Документ49 страниц1 To 3Vikki NandeshwarОценок пока нет
- CHCCCS015 Student Assessment Booklet Is (ID 97088) - FinalДокумент33 страницыCHCCCS015 Student Assessment Booklet Is (ID 97088) - FinalESRОценок пока нет
- Carbon Monoxide PoisoningДокумент31 страницаCarbon Monoxide PoisoningDheerajОценок пока нет
- Adult Failure To ThriveДокумент5 страницAdult Failure To Thriveasmika danaОценок пока нет
- Environmental Studies-FIRST UNIT-vkmДокумент59 страницEnvironmental Studies-FIRST UNIT-vkmRandomОценок пока нет