Академический Документы
Профессиональный Документы
Культура Документы
SCERespMedSampleQs PDF
Загружено:
Zoya AnnamИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
SCERespMedSampleQs PDF
Загружено:
Zoya AnnamАвторское право:
Доступные форматы
Specialty Certificate in Respiratory Medicine Sample Questions
Question 1 A 30-year-old man presented to the chest clinic with a chronic productive cough and increasing breathlessness. He gave a history of recurrent chest infections since childhood. He and his partner had recently been referred for fertility treatment. On examination, he had finger clubbing and scattered crackles throughout both lung fields. What is the most likely diagnosis? A B C D E bronchiectasis cystic fibrosis primary ciliary dyskinesia pulmonary fibrosis pulmonary tuberculosis
Updated Dec-11
Question 2 A 60-year-old man, with type 2 diabetes mellitus, was admitted with a 4-day history of cough, chest pain and loss of diabetic control. Investigations showed a right-sided empyema. What is the most likely infecting organism? A B C D E Bacteroides sp. Enterobacteriaceae Staphylococcus aureus Streptococcus milleri Streptococcus pneumoniae
Updated Dec-11
Question 3 A 45-year-old man presented with a 1-year history of snoring and unrefreshing sleep. There was a history of witnessed apnoeic episodes. His Epworth sleepiness score was 7/24. His body mass index was 29 kg/m2 (1825). His overnight sleep study demonstrated a 4% desaturation index of seven events per hour. Which management option is most likely to improve his sleep quality? A B C D E continuous positive airway pressure mandibular repositioning splint non-invasive ventilation uvuloplasty weight reduction advice
Updated Dec-11
Question 4 A 56-year-old man presented with shortness of breath. Investigations: actual 0.96 2.24 3.52 5.89 4.25 1.0 SR* 2.9 0.6 +3.9 +1.3 2.5 2.8
forced expired volume in 1 s (FEV1) (L) forced vital capacity (FVC) (L) residual volume (RV) (L) total lung capacity (TLC) (L) transfer factor for CO (TLCO) (mmol/min/kPa) transfer coefficient (KCO) (mmol/min/kPa/L)
*SR is the standardised residual and represents the number of standard deviations the actual value is from the predicted value. The normal range for the SR of all lung function parameters is 1.64 to +1.64. What is the most likely diagnosis? A B C D E atrial septal defect with a left-to-right shunt emphysema pulmonary haemorrhage pulmonary vasculitis usual interstitial pneumonitis
Updated Dec-11
Question 5 A 65-year-old smoker attended the outpatient clinic with a 2-week history of pressure in the head. On examination, he had clinical signs of superior vena caval obstruction. A CT scan of the chest showed that the superior vena cava was compressed by a tumour in the right upper lobe of the lung, and there was also evidence of a clot within the vessel. A bronchoscopy showed a tumour in the right upper lobe bronchus and biopsies confirmed that this was a small cell carcinoma of the bronchus. What is the most appropriate management? A B C D E anticoagulation chemotherapy high-dose corticosteroids radiotherapy to the mediastinum stenting of the superior vena cava
Updated Dec-11
Question 6 A 34-year-old man was admitted to hospital with a history of sudden onset of chest pain and severe breathlessness. He was a lifelong non-smoker. A chest X-ray was performed (see image).
According to British Thoracic Society guidelines, what is the most appropriate next management step? A B C D E chest tube insertion high-flow oxygen non-invasive ventilation simple aspiration thoracic surgery
Updated Dec-11
Question 7 A 30-year-old man presented with erythema nodosum. Clinical examination of the chest was unremarkable. Which feature on high-resolution CT scan would favour a diagnosis of sarcoidosis? A centrilobular nodules along bronchovascular structures with an upper zonal predominance B diffuse ground-glass change with soft centrilobular nodules throughout lung C patchy ground-glass shadowing with no zonal predominance D peripheral consolidation with an upper zonal predominance E subpleural honeycombing with a lower zonal predominance
Updated Dec-11
Question 8 A 55-year-old woman with scleroderma presented with a 3-month history of increasing shortness of breath. Which feature on high-resolution CT scan would favour a histological diagnosis of non-specific interstitial pneumonia? A centrilobular nodules along bronchovascular structures with an upper zonal predominance B diffuse ground-glass change with soft centrilobular nodules throughout lung C patchy ground-glass shadowing with no zonal predominance D peripheral consolidation with an upper zonal predominance E subpleural honeycombing with a lower zonal predominance
Updated Dec-11
Question 9 A 66-year-old woman presented with a 4-week history of progressive breathlessness and discomfort over the right chest. Thirty years previously, she had undergone mantle radiotherapy for Hodgkins lymphoma. She had never smoked. Clinical examination showed evidence of radiotherapy change to the skin and signs of a right pleural effusion. Breast examination was normal. A chest X-ray confirmed the presence of a large right pleural effusion. Aspiration yielded straw-coloured fluid, with a protein content of 45 g/L and cytology revealed some atypical cells and lymphocytes. What is the most likely cause of the effusion? A B C D E adenocarcinoma of the lung breast cancer Meigs syndrome mesothelioma recurrent lymphoma
Updated Dec-11
Question 10 A 26-year-old woman with stable Crohns disease was admitted with a 4-day history of dyspnoea and haemoptysis. She required an FiO2 of 0.5 to maintain arterial saturation at 93% (9498) with a normal PCO2. Investigations: haemoglobin MCV white cell count platelet count erythrocyte sedimentation rate international normalised ratio serum creatinine serum albumin serum C-reactive protein CT scan of chest 88 g/L (115165) 90 fL (8096) 10.0 109/L (4.011.0) 522 109/L (150400) 102 mm/1st h (<20) 1.2 (<1.4) 67 mol/L (60110) 36 g/L (3749) 290 mg/L (<10) see image
What investigation is most likely to establish a diagnosis? A B C D E anti-glomerular basement membrane antibodies bronchoalveolar lavage echocardiography open lung biopsy transbronchial lung biopsy
Updated Dec-11
Question 11 A 42-year-old woman was referred with small-volume haemoptysis of less than a teaspoonful of blood-streaked sputum on three occasions. She had also coughed up green sputum. Her weight was stable and exercise tolerance unlimited. She was not taking any regular treatment. She had moved to the UK from Jamaica 23 years previously. She denied exposure to tuberculosis. She had smoked approximately 15 cigarettes per day for 30 years. Clinical examination was unremarkable. Investigations: forced vital capacity forced expiratory volume in 1 s peak expiratory flow rate chest X-ray CT scan of thorax 2.5 L (96% predicted) 2.1 L (93% predicted) 460 L/min (108% predicted) hyperinflated lung fields thin-walled cysts and small nodules mostly in the upper lobes bilaterally
What is the most likely explanation of the CT findings? A B C D E chronic obstructive pulmonary disease hypersensitivity pneumonitis lymphangioleiomyomatosis Pneumocystis jirovecii pneumonia pulmonary Langerhans cell histiocytosis
Updated Dec-11
Question 12 A fit 63-year-old woman was found to have a right lower lobe bronchial carcinoma that was thought to be operable. She wanted to know what the surgical mortality was for a lobectomy. What is the best estimate of 30-day mortality for lobectomy in England? A B C D E <2% 24% 56% 78% 910%
Updated Dec-11
Question 13
A 28-year-old man was referred to the chest clinic with intermittent breathlessness on exertion. He was an ex-smoker, with a 5 pack-year history. He kept a budgerigar. Investigations: chest X-ray ECG actual forced expiratory volume in 1 s (FEV1) forced vital capacity FEV1/FVC ratio functional residual capacity residual volume total lung capacity 3.9 L 5.2 L 75 3.04 L 1.6 L 7.3 L normal normal % predicted 95 100 98 95 98 110 113 standardised residual 0.4 0.6 0.2 0.2 0.1 0.9 1
transfer factor for CO (TLCO) 12.7 mmol/min/kPa
What is the most appropriate next investigation? A B C D E avian precipitins bronchodilator challenge echocardiography exercise testing high-resolution CT scan of thorax
Updated Dec-11
Question 14
A 64-year-old man was admitted with fever and rigors. He had a dry cough with no expectoration and reported no weight loss. He had no foreign travel apart from a holiday in the USA 1 year previously. He had been found to have transitional cell carcinoma of the bladder 3 months previously and was treated with a transurethral partial resection of bladder followed by intravesicular BCG. He had also had a normal chest X-ray 1 year previously. Investigations: haemoglobin white cell count neutrophil count platelet count serum sodium serum potassium serum creatinine interferon- release assay for tuberculosis bronchial washings 136 g/L (130180) 9.7 109/L (4.011.0) 6.3 109/L (1.57.0) 364 109/L (150400) 143 mmol/L (137144) 4.4 mmol/L (3.54.9) 123 mol/L (60110) non-reactive no acid- and alcohol-fast bacilli seen; culture negative see image
CT scan of chest
What is the most likely diagnosis? A B C D E disseminated BCG infection histoplasmosis metastatic transitional cell carcinoma miliary tuberculosis pulmonary sarcoidosis
Updated Dec-11
Question 15
A 25-year-old Caucasian woman was referred to the chest clinic with a productive cough. There was no history of fever or night sweats. She gave a history of 3-kg weight loss over the previous 6 months. She was a childminder and a non-smoker. She had been on one family holiday in the previous year to California. On examination, crackles were heard in both apices. No finger clubbing was noted. Investigations: haemoglobin white cell count neutrophil count platelet count chest X-ray 146 g/L (115165) 8.7 109/L (4.011.0) 4.3 109/L (1.57.0) 164 109/L (150400) see image a
image a
Updated Dec-11
CT scan of chest
see image b
image b
What is the most likely explanation for her CT scan appearances? A B C D E aspergillosis lung abscess organising pneumonia sarcoidosis tuberculosis
Updated Dec-11
Question 16
A 35-year-old woman was admitted with an acute asthmatic attack. On examination, she was using her accessory muscles and had polyphonic wheezes throughout her chest. She was treated with nebulised -adrenoceptor agonists and, within a few minutes, she said that her breathing felt much easier. On auscultation of her chest, there was much less wheeze. If the diameter of her bronchi increased by a factor of two after treatment, by what factor is the resistance of her airway most likely to decrease? A B C D E 2 4 8 16 32
Updated Dec-11
Question 17 A 49-year-old woman presented with a 4-week history of periodic retrosternal discomfort. She denied weight loss or any systemic symptoms. Investigations: CT scan of chest see image
What is the most likely diagnosis? A B C D E bronchogenic cyst lymphoma seminoma teratoma thymoma
Updated Dec-11
Question 18 A 49-year-old woman presented with an 8-week history of increasing breathlessness following a flu-like illness. Her cough had now improved. She did not report any weight loss. She had a history of moderately severe rheumatoid arthritis, for which she was taking methotrexate weekly. She had a 10 pack-year smoking history. On examination, a left-sided effusion was detected. Diagnostic pleural aspiration revealed turbid-looking fluid. Following simple bench centrifugation, the pleural fluid remained turbid (a clear supernatant did not appear). What is the most likely nature of the effusion? A B C D E chylothorax empyema malignant effusion pseudochylothorax rheumatoid effusion
Updated Dec-11
Question 19 A 75-year-old man was referred because of an abnormal chest X-ray. He had first presented 2 weeks previously to his general practitioner with a cough productive of yellow sputum. By the time of consultation, he had recovered completely and was feeling well. He reported no loss of appetite or weight. He had previously worked at a granite quarry. He had never smoked. On examination, there were no crackles or wheeze, and no finger clubbing. Investigations: chest X-ray small dense nodules bilaterally, mainly in the upper zones
What is the most likely diagnosis? A B C D E asbestosis kaolinosis progressive massive fibrosis silicosis stannosis
Updated Dec-11
Question 20 A 77-year-old man was referred because of progressive dyspnoea when walking uphill. He had a 2-month history of fatigue, anorexia and a 3-kg weight loss following a chest infection. He had a 25 pack-year smoking history. He was taking no respiratory medication. He had been treated for Parkinsons disease for 5 years. He was under review for prostatic outflow symptoms and had a mildly raised prostatespecific antigen. He had worked in the roofing industry from the age of 16 years. His mother had died from pulmonary tuberculosis when he was 6 years of age. On examination, he looked well, had no finger clubbing and was haemodynamically stable. There was decreased air entry on the left side of the chest and a dull percussion note. Investigations: chest X-ray see image
What is the most likely diagnosis to explain the chest X-ray findings? A B C D E adverse effects of anti-parkinsonian medication asbestos-related pleural disease chest trauma healed tuberculosis metastatic prostate cancer
Updated Dec-11
Question 21 A 65-year-old man wished to travel to Europe on a 3-hour flight 4 weeks after an acute exacerbation of chronic obstructive pulmonary disease. His general practitioner referred him to the clinic for in-flight oxygen assessment. Investigations: oxygen saturation at rest breathing air PO2 after hypoxic challenge test using 15% FiO2 for 15 min: forced expiratory volume in 1 s (FEV1) What is the most appropriate advice? A B C D E he may fly with in-flight oxygen at a flow rate of 2 L/min he may fly with in-flight oxygen at a flow rate of 4 L/min he may fly without the need for in-flight oxygen he should undergo a walk test as a prelude to flying reassess in 3 weeks 9394% (9498)
7.8 kPa 43% of predicted
Updated Dec-11
Question 22 A 77-year-old man presented with haemoptysis and weight loss. He had been a moderate cigarette-smoker for most of his adult life. Investigations: CT scan 4-cm mass in left lower lobe; 2cm station 7 lymph nodes squamous cell carcinoma in left lower lobe no pathological uptake outside the chest
fibreoptic bronchoscopy
FDG-PET scan
What is the most appropriate next staging investigation of his lung cancer? A B C D E endobronchial ultrasound (EBUS)-guided biopsy explorative thoracotomy left parasternal mediastinotomy mediastinoscopy percutaneous CT-guided biopsy
Updated Dec-11
Question 23 A 79-year-old man presented with weight loss and left-sided chest pains. He said that his symptoms had been present for at least 3 months. He had since stopped smoking. On examination, he was comfortable at rest and appeared cachectic. His oxygen saturation was 94% (9498) breathing air. Investigations: haemoglobin platelet count serum total protein fasting plasma glucose CT scan of thorax pleural pH pleural protein pleural glucose pleural cytology 105 g/L (130180) 480 109/L (150400) 60 g/L (6176) 5.0 mmol/L (3.06.0) left-sided pleural effusion 7.15 46 g/dL 1.5 mmol/L (>2.2) lymphocytes predominant; no malignant cells
What is the most appropriate next step in his management? A B C D E bronchoscopy interferon- release assay pleural biopsy rheumatoid factor tuberculin test
Updated Dec-11
Question 24 A 65-year-old man, weighing 75 kg, was admitted to the critical care unit after emergency abdominal aortic aneurysm repair. There was no medical history of note. What intervention is most likely to reduce his risk of acquiring ventilator-associated pneumonia? A B C D E early introduction of parenteral nutrition introduction of sucralfate as stress ulcer prophylaxis intubation of endotracheal tube using nasal route ventilation in prone position weekly replacement of ventilator tubing
Updated Dec-11
Question 25 A 39-year-old man gave a 3-month history of weight loss and feeling generally unwell. He had X-linked agammaglobulinaemia and was being treated with regular intravenous infusions of immunoglobulin. He also had bronchiectasis and was taking high-dose amoxicillin. Investigations: chest X-ray increased shadowing throughout both lung fields diffuse ground-glass shadowing throughout both lungs with evidence of bilateral lower lobe bronchiectasis
high-resolution CT scan of chest
What is the most likely diagnosis? A B C D E an exacerbation of his bronchiectasis drug-induced pneumonitis lymphocytic interstitial pneumonia lymphoma Pneumocystis jirovecii pneumonia
Updated Dec-11
Question 26 A 47-year-old woman presented with a 1-year history of increasing wheeze and shortness of breath. She was a smoker (25 pack years) and had started working at a local bakery as a cleaner 2 years previously. Her wheeze had improved on holiday and was better on her days off. On examination, she had nasal congestion and marked expiratory wheeze. What is the most likely diagnosis? A B C D E atopic asthma chronic bronchitis hypersensitivity pneumonitis irritant-induced asthma occupational asthma
Updated Dec-11
Answers: 1. B 2. D 3. B 4. B 5. B 6. D 7. A 8. C 9. A 10. A 11. E 12. B 13. D 14. A 15. E 16. D 17. E 18. D 19. D 20. B 21. C 22. A 23. C 24. B 25. C 26. E
Updated Dec-11
Вам также может понравиться
- PANCE Prep Pearls Pulmonary Questions PDFДокумент8 страницPANCE Prep Pearls Pulmonary Questions PDFkatОценок пока нет
- Aesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Документ60 страницAesthetic Dermal Filler Injections For Facial Rejuvenation (PDFDrive)Drhisham AttiaОценок пока нет
- Part 1 Sample Questions MRCPДокумент33 страницыPart 1 Sample Questions MRCPCharan Pal Singh100% (1)
- Respiratory QuestionДокумент79 страницRespiratory QuestionTofik Mohammed100% (2)
- PASSMEDICINE MCQs-RESPIRATORY MEDICINEДокумент111 страницPASSMEDICINE MCQs-RESPIRATORY MEDICINEHashim Ahmad75% (4)
- MRCP Part 2 Sample Questions PDFДокумент83 страницыMRCP Part 2 Sample Questions PDFamesbОценок пока нет
- MRCP Part 2 Sample Questions PDFДокумент83 страницыMRCP Part 2 Sample Questions PDFamesbОценок пока нет
- Aerosols and the Lung: Clinical and Experimental AspectsОт EverandAerosols and the Lung: Clinical and Experimental AspectsStewart W. ClarkeОценок пока нет
- SCEDermatologySampleQs PDFДокумент21 страницаSCEDermatologySampleQs PDFZoya Annam0% (1)
- SCEDermatologySampleQs PDFДокумент21 страницаSCEDermatologySampleQs PDFZoya Annam0% (1)
- Part 1 Sample Questions MRCPДокумент33 страницыPart 1 Sample Questions MRCParvindОценок пока нет
- SCE ED Sample QuestionsДокумент25 страницSCE ED Sample QuestionsZoya Annam100% (2)
- Guide To Genetic CounselingДокумент24 страницыGuide To Genetic Counselingmady_elenutza0% (1)
- MKSAP13-Pulmonary Medicine and Critical CareДокумент85 страницMKSAP13-Pulmonary Medicine and Critical CaresarfirazОценок пока нет
- Final written M.B.B.Ch. EXAMINATION IN MEDICINE PAPER IДокумент16 страницFinal written M.B.B.Ch. EXAMINATION IN MEDICINE PAPER IIsmail SialaОценок пока нет
- 100 BCQ MRCP QuestionsДокумент31 страница100 BCQ MRCP QuestionsMatin Ahmad Khan100% (1)
- Pathology BДокумент5 страницPathology Bttdjhg2p6kОценок пока нет
- EMQs For Medical Students Volume 3 2eДокумент16 страницEMQs For Medical Students Volume 3 2ePasTestBooks50% (2)
- MRCP 2Документ26 страницMRCP 2riyaz414Оценок пока нет
- Breast Lump Prognosis Prediction/TITLEДокумент30 страницBreast Lump Prognosis Prediction/TITLETony DawaОценок пока нет
- Sce Geriatric Medicine Sample QsДокумент67 страницSce Geriatric Medicine Sample QsZoya Annam100% (7)
- Sce Geriatric Medicine Sample QsДокумент67 страницSce Geriatric Medicine Sample QsZoya Annam100% (7)
- BiopharmaceuticsДокумент52 страницыBiopharmaceuticsDharma ShantiniОценок пока нет
- Child Abuse and NeglectДокумент89 страницChild Abuse and NeglectdrvarshaОценок пока нет
- Labor Pain ManagementДокумент1 страницаLabor Pain ManagementKenneth Sy100% (5)
- Infusion Pumps, Large-Volume - 040719081048Документ59 страницInfusion Pumps, Large-Volume - 040719081048Freddy Cruz BeltranОценок пока нет
- Buteyko Meets DR MewДокумент176 страницButeyko Meets DR MewAnonymous hndaj8zCA100% (1)
- RESP MEDICINE For PlabДокумент73 страницыRESP MEDICINE For PlabJanie-Vi GorospeОценок пока нет
- Lung QuizДокумент14 страницLung QuizConcepcion R. AquinoОценок пока нет
- Sce Nephrology Sample QsДокумент59 страницSce Nephrology Sample QsJwaltzPadlanОценок пока нет
- Respiratory QuizДокумент32 страницыRespiratory Quiztajamulhussainshah0% (1)
- Pulmon Ology MCQ SДокумент280 страницPulmon Ology MCQ SSai ShankerОценок пока нет
- Internal MedicineДокумент146 страницInternal MedicineSh. RamОценок пока нет
- Sce Gastro Sample QsДокумент36 страницSce Gastro Sample QsZoya Annam100% (8)
- Sce Gastro Sample QsДокумент36 страницSce Gastro Sample QsZoya Annam100% (8)
- My Masterclass Create Exam My History My DetailsДокумент100 страницMy Masterclass Create Exam My History My DetailsMuntasir BashirОценок пока нет
- Frac P Respiratory QuestionsДокумент4 страницыFrac P Respiratory QuestionsDr-fadi AlkhasawnehОценок пока нет
- LUNGSДокумент11 страницLUNGSRussell Talan CilotОценок пока нет
- Casi Clinici Medicine and Critical CareДокумент85 страницCasi Clinici Medicine and Critical CarePaolo OnidaОценок пока нет
- Pages From Harrison's - Self - Assessment - and - Board-2Документ66 страницPages From Harrison's - Self - Assessment - and - Board-2abutalebheba95Оценок пока нет
- Lungs MCQДокумент10 страницLungs MCQMuhammad Mudassir SaeedОценок пока нет
- Histopathology Part 1 Sample QuestionsДокумент8 страницHistopathology Part 1 Sample Questionsdr shahzadОценок пока нет
- Recurrent Pneumonia Caused by Rare Granular Cell TumorДокумент7 страницRecurrent Pneumonia Caused by Rare Granular Cell TumorJoshua MendozaОценок пока нет
- Quizlet LungsДокумент20 страницQuizlet LungsPrinceОценок пока нет
- Lung Cancer CaseДокумент13 страницLung Cancer CaseAbdirahman Ali YabarОценок пока нет
- Aku 2Документ70 страницAku 2rehan hayderОценок пока нет
- Jurnal Bronchitis Dengan AsmaДокумент5 страницJurnal Bronchitis Dengan AsmaMauLan SaputraОценок пока нет
- Med Respi T&D QuestionsДокумент14 страницMed Respi T&D QuestionsD PatelОценок пока нет
- Evolution From "Typical" To "Atypical" Radiological Appearances-Report of Two Patients of SarcoidosisДокумент5 страницEvolution From "Typical" To "Atypical" Radiological Appearances-Report of Two Patients of SarcoidosisAdie BrianОценок пока нет
- Asthma and Lung MassДокумент4 страницыAsthma and Lung MassAzmachamberAzmacareОценок пока нет
- 11 - Less Common Pulmonary Diseases - Live Session RecordingДокумент21 страница11 - Less Common Pulmonary Diseases - Live Session RecordingjimmyneumologiaОценок пока нет
- A Case of Benign, Multiple MetastasesДокумент2 страницыA Case of Benign, Multiple MetastasesCesar Antonio Ulloa BarbaranОценок пока нет
- Practice Questions: Respiratory SystemДокумент6 страницPractice Questions: Respiratory SystemTraceyОценок пока нет
- A 56 Year Old Woman With Multiple Pulmonary CystsДокумент8 страницA 56 Year Old Woman With Multiple Pulmonary CystsAchmad Dodi MeidiantoОценок пока нет
- End Blok Respi SoalДокумент6 страницEnd Blok Respi Soalanz_4191Оценок пока нет
- Internal Medicine Case StudiesДокумент56 страницInternal Medicine Case StudiesLwayОценок пока нет
- Bronchiectasis: Case & ReviewДокумент40 страницBronchiectasis: Case & ReviewKhaled S. HarbОценок пока нет
- Case Report Displasia BronkopulmonerДокумент5 страницCase Report Displasia BronkopulmonerVivi DeviyanaОценок пока нет
- Mcqs Resp 3Документ4 страницыMcqs Resp 3jhhОценок пока нет
- Laryngeal: Obstruction Relieved by PantingДокумент3 страницыLaryngeal: Obstruction Relieved by PantingIndah D. RahmahОценок пока нет
- Section II - Chest Radiology: Figure 1AДокумент35 страницSection II - Chest Radiology: Figure 1AHaluk Alibazoglu100% (1)
- Medicine RespiratoryДокумент80 страницMedicine Respiratoryan kitОценок пока нет
- Unusual Case of Tuberculous Pleural Effusion and Abdominal MassДокумент4 страницыUnusual Case of Tuberculous Pleural Effusion and Abdominal MassRofi IrmanОценок пока нет
- Lung Cancer in ChildДокумент4 страницыLung Cancer in Childtonirian99Оценок пока нет
- PulmonologyДокумент175 страницPulmonologyJohanna GarciaОценок пока нет
- Neu Motor AxДокумент6 страницNeu Motor AxZay SiagОценок пока нет
- Metastasepulmo 1Документ6 страницMetastasepulmo 1rajawinangunОценок пока нет
- Bula Ca PDFДокумент2 страницыBula Ca PDFFadhli Muhammad KurniaОценок пока нет
- Essentials in Lung TransplantationОт EverandEssentials in Lung TransplantationAllan R. GlanvilleОценок пока нет
- Fast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseОт EverandFast Facts: Blastic Plasmacytoid Dendritic Cell Neoplasm: Shedding light on a rare diseaseОценок пока нет
- Sce Rheum at Ology Sample QДокумент42 страницыSce Rheum at Ology Sample QZoya AnnamОценок пока нет
- Sce Acute Med Sample QsДокумент39 страницSce Acute Med Sample QsZoya AnnamОценок пока нет
- SCE ID Sample QuestionsДокумент30 страницSCE ID Sample Questionstabi_thegr8Оценок пока нет
- Part 2 Sample Questions ExplanationsДокумент25 страницPart 2 Sample Questions ExplanationsJoyee BasuОценок пока нет
- Part 2 Sample Questions Answer KeysДокумент4 страницыPart 2 Sample Questions Answer KeysZoya AnnamОценок пока нет
- Sce Rheum at Ology Sample QДокумент42 страницыSce Rheum at Ology Sample QZoya AnnamОценок пока нет
- Dr. Ayesha Latif's Guide to Airway ManagementДокумент32 страницыDr. Ayesha Latif's Guide to Airway ManagementAyesha LatifОценок пока нет
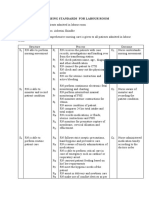
- Nursing Standards for Labour RoomДокумент3 страницыNursing Standards for Labour RoomRenita ChrisОценок пока нет
- NCM 103 Aliasas AtelectasisДокумент3 страницыNCM 103 Aliasas AtelectasisDARREN EDMARKОценок пока нет
- "Bioterrorism": Delhi Pharmaceutical Sciences and Research UniversityДокумент6 страниц"Bioterrorism": Delhi Pharmaceutical Sciences and Research UniversityNeeru ChaudharyОценок пока нет
- SurgeryДокумент3 страницыSurgeryBanu KubendiranОценок пока нет
- Prasugrel and RosuvastatinДокумент7 страницPrasugrel and RosuvastatinMohammad Shahbaz AlamОценок пока нет
- Family Nursing Care PlanДокумент26 страницFamily Nursing Care PlanAmira Fatmah QuilapioОценок пока нет
- Prevalence of Soil Transmitted Helminths infection in adults in North SulawesiДокумент4 страницыPrevalence of Soil Transmitted Helminths infection in adults in North SulawesiSahrul hamidОценок пока нет
- ENL 110 APA In-Text-Citations and References ActivityДокумент5 страницENL 110 APA In-Text-Citations and References ActivityNajat Abizeid SamahaОценок пока нет
- History and P.E. of The Integumentary SystemДокумент6 страницHistory and P.E. of The Integumentary SystempazucenaОценок пока нет
- Jdvar 08 00237Документ3 страницыJdvar 08 00237Shane CapstickОценок пока нет
- Research Paper Brianna BartonДокумент11 страницResearch Paper Brianna Bartonapi-530899175Оценок пока нет
- U.S. clinical observerships help IMGs gain experienceДокумент8 страницU.S. clinical observerships help IMGs gain experienceAkshit ChitkaraОценок пока нет
- Andocor BrochureДокумент19 страницAndocor BrochureAffan AhmadОценок пока нет
- Penicillin Allergy DelabelingДокумент31 страницаPenicillin Allergy Delabelingapi-506607906Оценок пока нет
- NCP Impaired Skin IntegrityДокумент3 страницыNCP Impaired Skin IntegrityMiar QuestОценок пока нет
- F-I Drug HandbookДокумент55 страницF-I Drug HandbookGeanieveve ElnasОценок пока нет
- Thesis On HPV VaccineДокумент8 страницThesis On HPV Vaccinegjftqhnp100% (2)
- Manage Ophthalmia NeonatorumДокумент2 страницыManage Ophthalmia NeonatorumEjay BautistaОценок пока нет
- Guía OxigenoterapiaДокумент39 страницGuía OxigenoterapiaSMIBA MedicinaОценок пока нет
- Major & Mild NCD Terminology UpdatesДокумент30 страницMajor & Mild NCD Terminology Updatesrachelle anne merallesОценок пока нет
- Effects of Healthcare Environmental Design On Medical Outcomes PDFДокумент11 страницEffects of Healthcare Environmental Design On Medical Outcomes PDFAgnes Cheverloo Castillo100% (1)
- SA Psych MAY 2016 FIn Final WebДокумент82 страницыSA Psych MAY 2016 FIn Final WebAKNTAI002Оценок пока нет