Академический Документы
Профессиональный Документы
Культура Документы
Health Assessment
Загружено:
rlinaoАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Health Assessment
Загружено:
rlinaoАвторское право:
Доступные форматы
ATENEO DE DAVAO UNIVERSITY College of Nursing HEALTH ASSESSMENT Procedures Guidelines in preparing for a Physical Examination: 1.
Always dress in a clean, professional manner; make sure your name pin or ID is visible. 2. Remove all jewelry that can interfere with the physical examination, such as bracelets and rings. 3. Be sure that your fingernails are short and your hands are warm for maximum patient comfort. 4. Be sure your hair will not fall forward and touch the patient. 5. Arrange for a well-lit, warm and private room. 6. Assemble and arrange all needed equipment. 7. Introduce yourself to the patient. 8. Instruct the patient to undress privately; Inform the patient of when you will return to start the examination. 9. Have the patient void before the examination. 10. Wash your hands in front of the patient to show your concern for cleanliness. 11. Observe Standard Precautions and Transmission-Based Precautions, as indicated. 12. Ensure that the patient is accessible from both sides of the examination bed or table. 13. If a bed is used, raise the height so that you do not have to bend over to perform the examination. 14. Position the patient as indicated of the body system being assessed. 15. Enlist the patients cooperation by explaining what you are about to do, where it will be done, and how it may feel. 16. Use your hands or warm water to warm all instruments before use. 17. If the patient complains of fatigue, continue the examination later (if possible). 18. Avoid making crude or negative remarks; be cognizant of your facial expressions when dealing with malodorous or dirty patients or with disturbing findings (e.g., infected wounds or disfigurement). 19. Conduct the examination in a systematic fashion every time. Consistency decreases the likelihood of forgetting to perform a particular assessment. 20. Thank the patient when the physical examination is concluded; inform the patient of what will happen next. 21. Document examination findings in the appropriate section of the patient record.
Appropriate Positions:
A. Semi-fowlers 45-degree angle: Used in assessing the skin;head and neck; eyes, ears, nose, mouth, and throat; thorax and lungs; heart and peripheral vasculature;musculoskeletal;neurological; patients who cannot tolerate sitting up at a 90-degree angle. B. Sitting (High-Fowlers) Used in assessing the skin;head and neck; eyes, ears, nose, mouth, and throat; thorax and lungs; heart and peripheral vasculature;musculoskeletal;neurological; C. Horizontal recumbent (Supine) Breasts; heart and peripheral vasculature; abdomen; musculoskeletal D. Dorsal recumbent Female genitalia; anterior thorax and lungs; breasts; axillae; heart and peripheral vasculature; abdomen; musculoskeletal E. Side lying Skin; thorax and lungs; bedridden patients who cannot sit up F. Lithotomy Female genitalia and rectum G. Knee-chest Rectum and prostate H. Sims Rectum and female genitalia I. Prone Skin; posterior thorax and lungs; hips
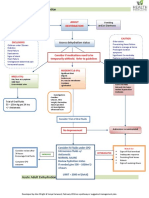
Format of Assessment/Legend: E- Examination N-Normal findings A-Abnormal findings P-Pathophysiology GENERAL SURVEY Initial observations involve collecting information about the patients: a. Physical presence b. Psychological presence c. Signs and Symptoms of distress
EXAMINATION A. Physical Presence Observe the patients: 1. Stated age versus apparent age. 2. General appearance 3. Body fat.
NORMAL FINDINGS
The patients stated chronological age should be congruent with the apparent age. The patient should exhibit body symmetry, no obvious deformity, and a well appearance. Body fat should be evenly distributed. Body fat composition is difficult to estimate accurately without the use of immersion tanks or calipers. Limbs and trunk should appear proportional to body height; posture should be erect. Walking gait as well as other body movements should be smooth and effortless. All body parts should demonstrate controlled, purposeful movement.
4. Stature. 5. Motor activity
B. Psychological Presence Observe the patients 1. Dress, grooming, and personal hygiene. The patient should appear clean and neatly pressed. Clothing choice should be appropriate to the weather. Norms and standards for dress and cleanliness may vary between cultures.
2. Mood and manner. 3. Speech.
The patient should be generally cooperative and pleasant. The patient should respond to questions and commands easily, and the patients speech should be clear and understandable. Pitch, rate, and volume should vary normally. The patient should appear awake and alert. Facial expressions should be appropriate to what is happening in the environment. Facial expression should change naturally.
4. Facial expressions.
C. Distress Observe for: 1. Labored breathing or speech; wheezing or coughing. 2. Painful facial expression, sweating, or physical protection of a painful area. Breathing should be effortless and without coughing or wheezing. Speaking should not leave the patient breathless. The patients face should be relaxed, and the patient should be willing to move all body parts freely. There should be no life-threatening conditions.
3. Serious or life-threatening occurrences such as seizure activity, active and severe bleeding, gaping wounds, and open fractures.
4. Signs of emotional distress or anxiety, The patient should not be perspiring excessively which may include but are not limited to or showing signs of emotional distress, such as tearfulness, nervous tics or laughter, lack of nail biting or avoiding eye contact. eye contact, excessive nail biting, inability to pay attention, autonomic responses such as diaphoresis, changes in breathing patterns, or cold, clammy hands.
ASSESSMENT OF THE SKIN, HAIR, and NAILS
General Approach to Skin, Hair, and Nails Assessment 1. Ensure that the room is well lit. Daylight is the best source of light, especially when determining skin color. If daylight is unavailable, however, overhead fluorescent lights should be used. 2. Use a hand-held magnifying glass to aid in inspection when simple visual inspection is inadequate. 3. Explain to the patient each step of the assessment process before initiating the assessment. 4. Ensure patient comfort by keeping the room at an appropriate temperature. 5. Warm hands by washing them in warm water before the assessment. 6. Ask the patient to undress completely and to put on a gown, leaving the back untied. 7. Perform the assessment in cephalocaudal fashion. 8. For episodic illness, the skin examination is incorporated into the regional physical exam.
EQUIPMENT Magnifying glass Good source of natural light Penlight Clean gloves Small centimeter ruler Inspection of the skin Examination Findings In each area, observe for color, bleeding, COLOR ecchymosis, erythema, vascularity, lesions, moisture, temperature, texture, turgor, and Normal: edema. The skin is normally a uniform whitish-pink or brown color, depending on the race of the 1. Facing the patient, inspect the color of the patient. Dark-skinned persons may normally skin of the face, eyelids, ears, nose, lips, and have freckling on the gums, tongue borders, mucous membranes. and lining of the cheeks; the gingival may appear blue in color. 2. Inspect the anterior and lateral aspects of the neck, then behind the ears.
3. Inspect the arms and the dorsal and palmar surfaces of the hands. Pay special attention to the webs between the fingers. 4. Have the patient assume a supine position, with the arms placed over the head. 5. Lower the patients gown to uncover the chest and the breasts. 6. Inspect the intramammary folds and ridges. Pendulous breasts may need to be raised to perform this inspection. 7. Assess the axillae and re-cover the chest and breasts with the gown. 8. Raise the gown to uncover the abdomen and the anterior aspects of the lower extremities; cover the genital area with an extra towel. 9. Inspect the abdomen, anterior aspects of the lower extremities, dorsal and plantar surfaces of the feet, and toe webs. 10. Don the gloves and uncover the genital area. 11. Inspect the inguinal folds and genitalia. 12. Remove gloves. 13. Have the patient assume a side-lying position on the examination table so that the patients back is facing you. 14. Inspect the back and the posterior neck and scalp. Specifically look for nevi or other lesions. 15. Inspect the posterior aspects of the lower extremities. 16. Don clean gloves, raise the gluteal cleft, and inspect the gluteal folds, and the perianal area; remove and discard the gloves. 17. Cover the patient and assist back to a sitting position. Wash hands.
Abnormal: Cyanosis: dusky blue fingers, lips or mucous membranes; bluish tint. Jaundice: yellow-green to orange cast or coloration of the skin, sclera, mucous membranes, fingernails, and palmar and/or plantar surfaces in light skinned individuals; yellow staining in the sclera, hard palate, and palmar or plantar surfaces in dark-skinned individuals. Carotenemia: orange-yellow coloration of the palmar and plantar surfaces and forehead but no involvement of the mucous membrane. Polycythemia: bright red to ruddy sustained appearance appearance evident on the integument, mucous membranes, palmar or plantar surfaces. Albinism: white cast to the skin, including the hair and eyebrows. Vitiligo: patchy, symmetrical areas of white on skin. Butterfly rash: an erythematous, confluent, eruption in a butterfly-like distribution over the face. BLEEDING,ECCHYMOSIS AND VASCULARITY Normal: There are normally no areas of bleeding, ecchymosis, or increased vascularity. Abnormal: Spontaneous bleeding from the mucous membranes, previous venipuncture sites, or lesions due to clotting disorders, trauma or use of antithrombolytic agents.
Petechiae: Violaceous discoloration of less than 0.5 cm in diameter that does not blanch; in dark-skinned individuals, evaluate for petechiae in the mucous membranes and axillae. Purpura: Confluent petechiae or confluent echymossis over any part of the body. Ecchymosis: Violaceous discoloration of varying size, also called a black-and-blue mark; deeper in color in dark-skinned individuals. Venous stars: Linear or irregularly shaped blue vascular patterns that do not blanch. Cherry angiomas: Bright red circumscribed areas that may darken with age. Port-wine stain or nevus flammeus: Burgundy, red, or purple macular vascular patch located along the course of the peripheral nerve Gas gangrene or clostridial myonecrosis: Dark brown or blackened areas of the skin that are edematous and painful and that may drain a thin liquid having a sweet, foul odor. Spider angiomas: Bright red or star-shaped with central pulsation. LESIONS Normal: No skin lesions should be present except for freckles, birthmarks, or moles (nevi), which may be flat or elevated.
Palpation of the Skin Examination Moisture: Using the dorsal surfaces of the hands and Normal: fingers, palpate all nonmucous membrane The skin is normally dry, with a minimum of skin surfaces for moisture. perspiration. Moisture on the skin will vary from one body area to another, with perspiration normally present on the hands, axillae, and face, and between the skin folds. Moisture also varies with changes in the environment, muscular activity, body temperature, stress, and activity levels. Body temperature is regulated by the skins production of perspiration, which evaporates to cool the body. Abnormal: Xerosis: excessive dryness of the skin Diaphoresis: profuse perspiration Temperature: Using the dorsal surfaces of the hands and Normal: fingers, palpate all nonmucosal skin surfaces for Skin surface temperature should be warm and temperature. equal bilaterally. The hands and feet may be slightly cooler than the rest of the body. Abnormal: Hypothermia: generalized or localized cooling of the skin. Hyperthemia: generalized or localized excessive warming of the skin. Tenderness: Normal: Palpate the skin surface for tenderness using Skin surfaces should be nontender. the dorsal surfaces of the hands and fingers. Abnormal: Tenderness over the skin structures can be discrete and localized or generalized. Discrete tenderness may indicate a localized infection Findings
such as cellulites, or generalized tenderness can indicate systemic illness such as lymphoma or allergic reaction. Normal: Texture: Use the finger pads to evaluate the texture of Skin should normally feel smooth, even, and the skin. firm, except where there is significant hair growth. A certain amount of roughness can be Evaluate surfaces such as over the abdomen normal. and the medial surfaces of the arms first. Abnormal: Compare these with the areas that are covered Roughness may result from use of wool with hair. clothing, cold weather, use of soap, scleroderma, hypothyroidism, occupational exposures. Soft, silk-like texture may be due to hyperthyroidism. Turgor: Palpate the skin turgor or elasticity, which reflects the skins state of hydration. 1. Between your thumb and forefinger, pinch a small section of the patients skin. The anterior chest, under the clavicle, and the abdomen are optimal to assess. 2. Slowly release the skin. 3. Observe the speed with which the skin returns to its original contour when released. Edema: Palpate the skin for edema, or accumulation of fluid in the intercellular spaces. 1. Firmly imprint your thumb against a dependent portion of the body, such as the arm, hand, leg, foot, ankle, or sacrum. 2. Release the pressure. 3. Observe for the indentation on the skin. 4. Rate the degree of edema: 0+ No pitting edema 1+ Mild pitting edema. 2 mm Normal: Edema is not normally present. Abnormal: Edema:puffy tight skin; localized or generalized. Normal: When the skin is released, it should rapidly return to its original contour. Abnormal: Decreased skin turgor: skin remains pinched when initially released and slowly returns to its original contour. This may be due to dehydration, the aging process, scleroderma. Increased skin turgor: skin returns to its original contour too quickly. This may indicate a connective tissue disease.
depression that disappears rapidly. 2+ Moderate pitting edema. 4 mm depression that disappears in 10-15 seconds. 3+ Moderately severe pitting edema. 6 mm depression that may last more than 1 minute. 4+ Severe pitting edema. 8 mm depression that can last more than 2 minutes.
Inspection of the Hair Examination COLOR Findings
Normal: Inspect the scalp hair, eyebrows, eyelashes, Hair varies from dark black to pale black, or and body hair for color. brown, depending on the amount of melanin present. As melanin production diminishes, hair turns gray. Hair color may be chemically changed. Abnormal: Patches of gray hair that are isolated or occur in conjunction with scarring. This may be due to nerve damage, trauma. DISTRIBUTION Normal: Evaluate the hair distribution on the body, The body is covered in vellus hair. Terminal hair eyebrows, face and scalp. is found in the eyebrows, eyelashes, and scalp, and after, puberty, in the axillae and pubic areas. Males may experience a certain degree of normal balding and may also develop terminal facial and chest hair. Abnormal: Absence of pubic hair, unless purposefully removed may indicate endocrine disorders. Male or female pattern baldness (alopecia areata): circumscribed bald area may be due to genetic predisposition, androgenic effects on the hair follicle, chemotherapy, infection. Hirsutism: excess facial and body hair
Trichotillomania: areas of broken-off hairs in irregular patterns accompanied by scaling but no infection which may due to hair twisting or manipulation. Tinea capitis: ringworm. Broken-off hairs accompanied by scaliness and follicular inflammation due to fungal infection.
LESIONS Normal: Don the gloves and lift the scalp hair by The scalp should be pale white to pink in lightsegments. skinned individuals and light brown in dark skinned individuals. There should be no signs of Evaluate the scalp for lesions and signs of infestation or lesions. Seborrhea, commonly infestation. known as dandruff may be present minimally. Abnormal: Head lice (pediculosis capitis): white dandrufflooking areas that are difficult to remove; associated itching.
Palpation of the Hair Examination TEXTURE Normal: Hair may feel thin, straight, coarse, thick, or curly. It should be shiny and resilient when Note the condition of the hair, from the scalp, to traction is applied and should not come out in the end of the hair. clumps in your hands. Between your fingertips, palpate the hair. Abnormal: Brittle hair that easily breaks off which may indicate malnutrition, hyperthyroidism, use of chemicals, infections secondary to damage of hair follicles. Findings
Inspection and Palpation of the Nails Examination COLOR Findings
Normal: Inspect the fingernails and toenails, noting the The nails normally have a pink cast in lightcolor of the nails. skinned individuals and a brown cast in darkskinned individuals. Capillary refill is an indicator Check capillary refill by depressing the nail until of peripheral circulation. Normal capillary refill blanching occurs. may vary by age, but color should return to normal within 2-3 seconds. Release the nail and evaluate the time required for the nail to return to its previous color. Abnormal: Leukonychia: White striations or dots may Perform a capillary refill check on all four indicate trauma, infection, vascular diseases, extremities. psoriasis, anemia, cirrhosis, hypercalcemia Melanochyia: brown nail plate indicating Addisons disease,malaria Splinter hemorrhage: red or brown linear streaks which may be due to subacute bacterial endocarditis, mitral stenosis. Onychomycosis: a yellow or white hue in a hyperkeratotic nail bed due to a fungal infection. SHAPE AND CONFIGURATION Normal: Assess the fingernails and toenails for shape, The nail surface should be smooth and slightly configuration and consistency. rounded to flat. Curved nails are a normal variant. Nail thickness should be uniform View the profile of the middle finger and throughout, with no splintering or brittle edges. evaluate the angle of the nail base. The angle of the nail base should be approximately 160 degrees. Longitudinal ridging Have the patient bring the distal phalanxes is a normal variant. There is a diamond-shaped together. Note the position of the nailbeds in opening at the base of the nailbeds in nails that relation to each other. are normal. Abnormal: Clubbing: nail base angle greater than 160. Nailbeds do not meet medially and do not have a diamond-shaped opening at their base. These may indicate hypoxia, lung cancer.
TEXTURE Normal: Between your thumb and index finger, palpate The nail base should be firm to palpation. the nail base. Abnormal: Note the consistency. Spongy nail base is indicative of clubbing due to disorders causing impaired tissue oxygenation over a prolonged period.
Assessment of the Eye Equipment: Opthalmoscope Penlight Clean gloves Snellen Chart Vision occluder Cotton-tipped applicator VISUAL ACUITY The assessment of visual acuity (cranial nerve II) is performed using a Snellen chart and an occluder to cover the patients eye.
Examination Distance Vision 1. 2.
Findings
3. 4. 5.
6. 7.
Normal: Ask the patient to stand or sit facing the The person who has a visual acuity of 20/20 is Snellen chart at a distance of 20 feet. considered to have normal visual acuity. If the patient normally wears glasses, ask that they be removed. If the glasses Abnormal: are used strictly for reading, do not Inability to read the chart with an uncorrected have the patient wear the glasses for visual acuity of 20/30 in one eye; vision in both examination. Contact lenses may be left eyes is different by two lines or more; absent in the eyes. acuity. This may be due to myopia or Instruct the patient to cover the left eye nearsightedness; corneal opacities that are with the occluder and read as many either congenital, from lesions that have scarred lines on the chart as possible. the cornea, cataracts, hypertension, diabetes Note the number at the end of the last mellitus/ line the patient was able to read. If the patient is unable to read the letters at the top of the chart, move the patient closer to the chart. Note the distance at which the patient is able to read the top line. Repeat the test with the patient occluding the right eye. If the patient normally wears glasses, the test should be repeated with the patient wearing the glasses and it should be noted (corrected or uncorrected).
DISTRIBUTION Evaluate the hair distribution on the body, eyebrows, face and scalp.
Вам также может понравиться
- Assessment of The IntegumentaryДокумент3 страницыAssessment of The IntegumentaryMona ArabiaОценок пока нет
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideОт EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideОценок пока нет
- IV TherapyДокумент15 страницIV Therapyprincessmonique_208609100% (2)
- EthicoMoral Aspects of NursingДокумент18 страницEthicoMoral Aspects of NursingGemarie Adarlo CastilloОценок пока нет
- Breast AssessmentДокумент2 страницыBreast AssessmentTeanu Jose Gabrillo TamayoОценок пока нет
- Nurses Note DONEДокумент1 страницаNurses Note DONEjhenssineОценок пока нет
- Assessment of Lungs and ThoraxДокумент58 страницAssessment of Lungs and ThoraxShahmeerОценок пока нет
- Head, Mouth, Nose, Throat, Neck and Regional Lymph Nodes: Kristin Clephane, MSN, RN, CPNДокумент44 страницыHead, Mouth, Nose, Throat, Neck and Regional Lymph Nodes: Kristin Clephane, MSN, RN, CPNMike100% (1)
- 118 Skills Lab-Week 1-Responses To Altered Ventilatory FunctionsДокумент8 страниц118 Skills Lab-Week 1-Responses To Altered Ventilatory FunctionsKeisha BartolataОценок пока нет
- Female and Male GenitaliaДокумент5 страницFemale and Male GenitaliaMary Mae BuellaОценок пока нет
- Done By:: Hind Al-Suwais Nwal Al-EnezeДокумент21 страницаDone By:: Hind Al-Suwais Nwal Al-EnezeHINDОценок пока нет
- Nursing Review Bullet For Funda (-Credits To OWNER-)Документ4 страницыNursing Review Bullet For Funda (-Credits To OWNER-)Camille Honeyleith Lanuza FernandoОценок пока нет
- Fluids and ElectrolytesBlood TransfusionДокумент6 страницFluids and ElectrolytesBlood TransfusionMaria Erica Jan MirandaОценок пока нет
- Kozier Chapter 17 Health Wellness Well BeingДокумент10 страницKozier Chapter 17 Health Wellness Well BeingpauchanmnlОценок пока нет
- LWW BATES 17 CranialMotorSystem Transcript FINALДокумент8 страницLWW BATES 17 CranialMotorSystem Transcript FINALRachel Lalaine Marie SialanaОценок пока нет
- Nursing Theories and History HandoutsДокумент5 страницNursing Theories and History Handoutsvinax89Оценок пока нет
- Fluids Electrolytes Acid Base DisordersДокумент6 страницFluids Electrolytes Acid Base DisordersJerikaDolorPadilloPatricioОценок пока нет
- Checklist Mouth Throat Nose SinusesДокумент2 страницыChecklist Mouth Throat Nose SinusesShades ofyellowОценок пока нет
- IV FluidsДокумент17 страницIV FluidsTiffany NicolèОценок пока нет
- NUR100 Sherpath Oxygenation and PerfusionДокумент17 страницNUR100 Sherpath Oxygenation and Perfusioncaloy2345caloyОценок пока нет
- Post Test Health Assessment Chapter 12Документ5 страницPost Test Health Assessment Chapter 12Christianne CapuaОценок пока нет
- Theoretical Foundation of Nursing - Florence NightingaleДокумент9 страницTheoretical Foundation of Nursing - Florence NightingaleAshley Nicole BeltranОценок пока нет
- Catheterization DemoДокумент48 страницCatheterization Demojonna casumpangОценок пока нет
- Nursing Process Diagnosis Plan Implementation EvaluationДокумент59 страницNursing Process Diagnosis Plan Implementation EvaluationYemaya84Оценок пока нет
- Postoperative Nursing CareДокумент2 страницыPostoperative Nursing CareYeana AlonОценок пока нет
- Residual: No More Positive S/SX, Just WithdrawnДокумент10 страницResidual: No More Positive S/SX, Just WithdrawnRosie CuasitoОценок пока нет
- Physical AssessmentДокумент90 страницPhysical AssessmentReann LeeОценок пока нет
- Abdominal AssessmentДокумент2 страницыAbdominal AssessmentJan Jamison ZuluetaОценок пока нет
- Assessing The AbdomenДокумент18 страницAssessing The Abdomenmartinezrose32Оценок пока нет
- Thorax, Skin, Hair, Nails ObjectivesДокумент3 страницыThorax, Skin, Hair, Nails Objectivesctramel001100% (1)
- Communicablediseases 110227001506 Phpapp02 PDFДокумент30 страницCommunicablediseases 110227001506 Phpapp02 PDFCrystal Ann Monsale TadiamonОценок пока нет
- PHARMACOLOGYДокумент19 страницPHARMACOLOGYIligan, JamaicahОценок пока нет
- Fluids and Electrolytes-2Документ82 страницыFluids and Electrolytes-2Jem Loterte100% (1)
- Pyschiatric Nursing SummarizeДокумент39 страницPyschiatric Nursing SummarizeKyssel Seyer100% (1)
- Compilation of Reviewer For Fundamentals of Nursing PDF FreeДокумент49 страницCompilation of Reviewer For Fundamentals of Nursing PDF FreeTyler VintОценок пока нет
- Maternal and Child Health Nursing (NCM 101 Lect) Part 2Документ2 страницыMaternal and Child Health Nursing (NCM 101 Lect) Part 2yunjung0518100% (1)
- Vital Signs-Temp, PRДокумент54 страницыVital Signs-Temp, PRmags_abad09Оценок пока нет
- Or NursingДокумент14 страницOr NursingDharren Rojan Garvida Agullana100% (1)
- Fundamentals of NursingДокумент44 страницыFundamentals of Nursingtheglobalnursing100% (2)
- Chapter 09 - Visual and Auditory ProblemsДокумент7 страницChapter 09 - Visual and Auditory ProblemscariОценок пока нет
- Assessment of Thorax and LungsДокумент8 страницAssessment of Thorax and LungsMikkaela FedelisОценок пока нет
- Fluids Electrolytes - Acid-Base BalanceДокумент11 страницFluids Electrolytes - Acid-Base BalanceJhosita Flora Laroco100% (1)
- Gastro Intestinal Disorders:: Kawasaki DiseaseДокумент6 страницGastro Intestinal Disorders:: Kawasaki DiseaseJoanna TaylanОценок пока нет
- FIXATorsДокумент26 страницFIXATorsKevin P. FelicianoОценок пока нет
- Ears Lecture GuideДокумент56 страницEars Lecture GuidemajОценок пока нет
- Head To Toe Assessment Guide ToolДокумент3 страницыHead To Toe Assessment Guide Toolkezia_lillyОценок пока нет
- Aging Perspective and Demography Ncm114 Gerontology Aging PerspectivesДокумент19 страницAging Perspective and Demography Ncm114 Gerontology Aging PerspectivesLeslie CruzОценок пока нет
- Physical Examination Evaluation Format: Patient's ProfileДокумент6 страницPhysical Examination Evaluation Format: Patient's Profileyangi dokaОценок пока нет
- Maternal Ob NotesДокумент103 страницыMaternal Ob NotesBoris OrbetaОценок пока нет
- Types of LeadershipДокумент13 страницTypes of LeadershipMary Roan RonatoОценок пока нет
- Skin - Hair.Nails Head & Neck Eyes. Ears. Nose. Sinuses Mouth. PharynxДокумент92 страницыSkin - Hair.Nails Head & Neck Eyes. Ears. Nose. Sinuses Mouth. PharynxAT4-11 HUMSS 2 CEDRICK ILAO100% (1)
- Pruritus PRURITIS Pruritis (Itching) Is One of The Most CommonДокумент2 страницыPruritus PRURITIS Pruritis (Itching) Is One of The Most CommonFreeNursingNotesОценок пока нет
- Assessment of The Eyes, Ears, Nose, and Mouth: Mr. Andre Carlo C. de VeyraДокумент42 страницыAssessment of The Eyes, Ears, Nose, and Mouth: Mr. Andre Carlo C. de VeyraFranz Earl Niño AlbesaОценок пока нет
- What Is A Theory?Документ51 страницаWhat Is A Theory?Ca SobrementeОценок пока нет
- Eye DisordersДокумент7 страницEye DisordersClara De GuzmanОценок пока нет
- Concept 3 Notes - Anatomy Basics For StudentsДокумент39 страницConcept 3 Notes - Anatomy Basics For StudentsKaranОценок пока нет
- FUNDAMENTALS OF NURSING NCM 100.odtДокумент1 страницаFUNDAMENTALS OF NURSING NCM 100.odtCharissa Magistrado De LeonОценок пока нет
- AH2 Hesi ReviewДокумент46 страницAH2 Hesi ReviewJamie Antonini Grant100% (1)
- Administering Oral Medications: Melendez, Anna Carmela PДокумент19 страницAdministering Oral Medications: Melendez, Anna Carmela PAnna Carmela P. MelendezОценок пока нет
- Patient List For January 14, 2021: Room 301 - Dela Cerna, EulogioДокумент3 страницыPatient List For January 14, 2021: Room 301 - Dela Cerna, EulogiorlinaoОценок пока нет
- Gawang Pilipino: Ang JeepneyДокумент1 страницаGawang Pilipino: Ang JeepneyrlinaoОценок пока нет
- Metabolism ConceptДокумент76 страницMetabolism ConceptrlinaoОценок пока нет
- HOUSEKEEPINGДокумент37 страницHOUSEKEEPINGrlinaoОценок пока нет
- Health Assessment - Rle (Simulation)Документ10 страницHealth Assessment - Rle (Simulation)rlinaoОценок пока нет
- Acute Pain Related To Effects of Labor and Delivery ProcessДокумент3 страницыAcute Pain Related To Effects of Labor and Delivery ProcessrlinaoОценок пока нет
- Yearbook 2021Документ123 страницыYearbook 2021rlinaoОценок пока нет
- CHN NCP Format, by Araceli Maglaya (4 Edition Vs 5 Edition)Документ1 страницаCHN NCP Format, by Araceli Maglaya (4 Edition Vs 5 Edition)rlinaoОценок пока нет
- Partograph ExercisesДокумент2 страницыPartograph ExercisesrlinaoОценок пока нет
- EndorsementДокумент1 страницаEndorsementrlinaoОценок пока нет
- Eyes and EarsДокумент9 страницEyes and EarsrlinaoОценок пока нет
- Partograph ExercisesДокумент2 страницыPartograph ExercisesrlinaoОценок пока нет
- Total Fertility RateДокумент3 страницыTotal Fertility Rateeay2k13Оценок пока нет
- Philippine Nurses Association, Inc.: Member of The International Council of NursesДокумент2 страницыPhilippine Nurses Association, Inc.: Member of The International Council of NursesrlinaoОценок пока нет
- Case ScenariosДокумент1 страницаCase ScenariosrlinaoОценок пока нет
- A Case Study On Renal CancerДокумент5 страницA Case Study On Renal CancerrlinaoОценок пока нет
- Digital Fundraising Rhythm and Cadence Worksheet - LINAOДокумент2 страницыDigital Fundraising Rhythm and Cadence Worksheet - LINAOrlinaoОценок пока нет
- Roy Cresencio R. Linao JR., RN, MNДокумент4 страницыRoy Cresencio R. Linao JR., RN, MNrlinaoОценок пока нет
- Anatomical PositionsДокумент36 страницAnatomical PositionsrlinaoОценок пока нет
- Barthel IndexДокумент4 страницыBarthel IndexrlinaoОценок пока нет
- Sample Evaluative ToolДокумент5 страницSample Evaluative ToolrlinaoОценок пока нет
- Day - 2 - Date - Se P T e Mber 2 6, 2 0 2 0 Area - Shift - 7 A M - 3 P M Clinical Instructor: S I R Roy L I N AoДокумент4 страницыDay - 2 - Date - Se P T e Mber 2 6, 2 0 2 0 Area - Shift - 7 A M - 3 P M Clinical Instructor: S I R Roy L I N AorlinaoОценок пока нет
- Therapeutic CommunicationДокумент12 страницTherapeutic CommunicationrlinaoОценок пока нет
- Patient: Ivanna Alyanna MalasinДокумент1 страницаPatient: Ivanna Alyanna MalasinrlinaoОценок пока нет
- Digital FundraisingДокумент9 страницDigital FundraisingrlinaoОценок пока нет
- Ward Class Questions For Level 2Документ1 страницаWard Class Questions For Level 2rlinaoОценок пока нет
- Geria Test Questions For MoodleДокумент15 страницGeria Test Questions For MoodlerlinaoОценок пока нет
- Spinal Traction QuizДокумент3 страницыSpinal Traction QuizrlinaoОценок пока нет
- Oral Presentation Rubrik 2015Документ10 страницOral Presentation Rubrik 2015rlinaoОценок пока нет
- Change Process HP Post Grad PDFДокумент52 страницыChange Process HP Post Grad PDFrlinaoОценок пока нет
- PhilHealth Circular No. 14 S. 2018 - CF4Документ3 страницыPhilHealth Circular No. 14 S. 2018 - CF4Toche Doce100% (1)
- Crystal Aromatherapy Lesson 1Документ9 страницCrystal Aromatherapy Lesson 1crystals21Оценок пока нет
- Langerhans-Cell Histiocytosis: Review ArticleДокумент13 страницLangerhans-Cell Histiocytosis: Review ArticleHanifah ArroziОценок пока нет
- Medical Surgical Nursing ReviewДокумент97 страницMedical Surgical Nursing ReviewBernadeth Josefa BorelaОценок пока нет
- Interpretation of Histograms and Its Correlation WДокумент5 страницInterpretation of Histograms and Its Correlation WrezqiОценок пока нет
- 10 Hip Replacement SurgeryДокумент13 страниц10 Hip Replacement SurgeryDIA PHONG THANGОценок пока нет
- Surgeon-Performed Ultrasound As A Diagnostic Tool in AppendicitisДокумент6 страницSurgeon-Performed Ultrasound As A Diagnostic Tool in Appendicitisansar ahmedОценок пока нет
- Diana Sanchez V City & County of DenverДокумент48 страницDiana Sanchez V City & County of DenverEllyn SantiagoОценок пока нет
- Flip Chart 06 IUDДокумент12 страницFlip Chart 06 IUDLamyaa Ali HasanОценок пока нет
- Urinary Tract Infection: DR Badriya Al-Mahrouqi 12/11/2017Документ51 страницаUrinary Tract Infection: DR Badriya Al-Mahrouqi 12/11/2017NinaОценок пока нет
- Skin, Hair, and Nails, Forslind, 2005Документ469 страницSkin, Hair, and Nails, Forslind, 2005Tessa M.100% (1)
- Health Policy Memo MgenoviaДокумент5 страницHealth Policy Memo Mgenoviaapi-302138606Оценок пока нет
- Duty Report RIWДокумент41 страницаDuty Report RIWRiyan W. PratamaОценок пока нет
- Techniques For Parasite Egg Identification in Faecal SamplesДокумент9 страницTechniques For Parasite Egg Identification in Faecal SamplesDr.Kedar Karki ,M.V.Sc.Preventive Vet.Medicine CLSU Philippines100% (2)
- Hamstring Injuries in Football PDFДокумент276 страницHamstring Injuries in Football PDFulfahrifОценок пока нет
- Chapter 7: Emotional and Behavioural Problems: DR Jessie EarleДокумент28 страницChapter 7: Emotional and Behavioural Problems: DR Jessie EarlejajmajОценок пока нет
- Dehydration Pathway 2016Документ3 страницыDehydration Pathway 2016rochmandrg dokter gigiОценок пока нет
- CyberTherapy & Rehabilitation, Issue 3 (3), Winter 2010.Документ52 страницыCyberTherapy & Rehabilitation, Issue 3 (3), Winter 2010.Giuseppe RivaОценок пока нет
- D. Motola Et Al 2017Документ8 страницD. Motola Et Al 2017reclinpharmaОценок пока нет
- Theraputic UltrasoundДокумент64 страницыTheraputic UltrasoundRoshni KhanОценок пока нет
- 200 Terms & Definition From Pharmacology. WatermarkedДокумент17 страниц200 Terms & Definition From Pharmacology. Watermarkedsuresh adgaonkar100% (1)
- Biopharmaceutics and Clinical Pharmacokinetics - 20210831 - 212949Документ22 страницыBiopharmaceutics and Clinical Pharmacokinetics - 20210831 - 212949Md. Abu Bakar Siddique TayefОценок пока нет
- Pharmacy Practice Sample ReportДокумент26 страницPharmacy Practice Sample Reportsaransh misraОценок пока нет
- Manual Neo 900Документ76 страницManual Neo 900Bismarck Pablo Ibañez Piotti67% (3)
- 1 Gme Regulations 1997 Amended Upto May 2018Документ114 страниц1 Gme Regulations 1997 Amended Upto May 2018seethahereОценок пока нет
- 04-09-12 EditionДокумент28 страниц04-09-12 EditionSan Mateo Daily JournalОценок пока нет
- Reasons For Extraction of Primary Teeth in Jordan-A Study.: August 2013Документ5 страницReasons For Extraction of Primary Teeth in Jordan-A Study.: August 2013Mutia KumalasariОценок пока нет
- Windy WigaДокумент2 страницыWindy WigaWindy wigaОценок пока нет
- Drug Card BenadrylДокумент1 страницаDrug Card BenadrylAdrianne Bazo100% (1)
- International Journal of PharmaceuticsДокумент6 страницInternational Journal of PharmaceuticsSjis11362Оценок пока нет