Академический Документы
Профессиональный Документы
Культура Документы
Adverse Effects of Blood Transfusion
Загружено:
ay254Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Adverse Effects of Blood Transfusion
Загружено:
ay254Авторское право:
Доступные форматы
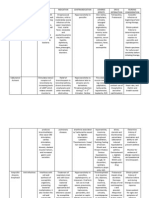
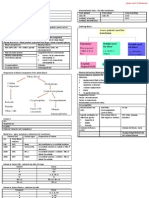
ADVERSE EFFECTS OF BLOOD TRANSFUSION
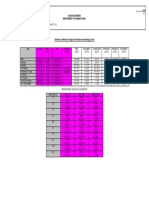
DEFINITION Any adverse outcome associated with the infusion of blood and its components CLASSIFICATION Transfusion reactions can be classified as 1) Immunologic and nonimmunologic 2) Immediate (usually <24hr) and delayed (days-years) 3) Haemolytic and nonhaemolytic TRANSFUSION REACTIONS IMMEDIATE Immunologic Haemolytic NHFTR Allergic TRALI
Problems Acute intravascular haemolysis of transfused red cells. (IHTR) Cause ABO incompatible transfusion. Usually IgM antibodies. When? Clinical Features Often during first few ml of infusion. Fever, pain at iv site, back or chest, red urine, diffuse bleeding, hypotension 5-10 days after red cell transfusion 75% of Rh D negative patients exposed to Rh D positive blood will develop anti-RhD How dangerous? Mortality 10% due to DIC and acute renal failure. . Treatment Avoidance Treat: see below Prevent: avoid clerical errors; ensure proper sample and recipient identification Treat: No treatment for antibodies per se. Avoid: Inform the Blood Bank of this incident Patient requires Rh-D negative or other antigen-negative
DELAYED Immunologic Haemolytic GVHD Nonimmunologic Iron overload Disease transmission
Nonimmunologic Bacterial Contamination Circulatory overload
Delayed extravascular haemolysis of transfused red cells. (DHTR)
Patient has lgG antibodies to donor red cell antigens usually Rhesus
Reduced survival of transfused red cells so transfusion may be less clinically effective. The destruction of red cells occurs extravascular in the reticuloendothelial system.
blood Non-Haemolytic Febrile Reactions (NHFTR) to transfusion of platelets and red cells. Antibodies to transfused white cells. Usually from previous pregnancies or transfusions. Within an hour or less. About 2% of all transfusion episodes. Multiple transfused or multiparous patients. Rise in temperature >1C from baseline, chills, rigors Unpleasant, especially if the patient requires regular transfusions. Treat: Temporarily stop infusion. Paracetamol. Avoid: Pretransfusion antipyretics; Use leukocyte- reduced or depleted cellular components if recurrent. Life threatening. Acute respiratory distress with CXRpulmonary edema, fever, chills, dyspnea, cyanosis Unpleasant. Treat: Stop transfusion, respiratory support, diuretics and high dose steroids.
Transfusion Related Acute Lung Injury (TRALI). Non-cardiogenic pulmonary oedema.
Donor plasma has antibodies to patient leukocyte antigens permeability of pulmonary vessels pulmonary edema Patient has antibodies that react with plasma proteins in transfused blood components.
During or soon after transfusion. Greater risks if large volumes of donor plasma given e.g. whole blood or plasma exchange with donor plasma. 1% of transfusions Itching, urticaria Rarely anaphylaxis, cardiac arrest
Urticaria (allergic reaction).
Treat: Temporarily stop infusion and give antihistamine. More aggressive treatment if severe reactionepinephrine, oxygen Avoid: Pretransfusion antihistamine; washed RBC components if severe or recurrent
Problems Transfusion hemosiderosis (Iron overload)
Cause One unit of red cells contains 250 mg of iron. It accumulates after several transfusions Too rapid and/or excessive blood transfusion
When? Clinical Features Clinical problems after several years of regular transfusion. e.g. Thalassaemics Elderly patients and those with cardiopulmonary compromise are susceptible. Patients with chronic anaemia are at risk due to an expanded plasma volume. -2-
How dangerous? Liver damage Endocrine problems Cardiac dysfunction
Treatment Avoidance Use iron chelating agent to increase iron excretion
Circulatory overload (Hypervolemia)
Dependent on clinical scenario.
Prevent: Avoid transfusion unless absolutely indicated especially in patients with chronic anaemia. Treat according to standard clinical practice.
Diseases transmitted by blood products
Hepatitis B, C; HIV; HTLV-1; CMV; malaria; vCJD
Window period Clinical features related to underlying disease
Hepatitis with liver failure AIDS etc
Prevent: Donor screening and deferral, limit use of blood, leukoreduction of blood, recombinant blood products, viral inactivation of plasma Treat: Discontinue transfusion. Manage septicemia. Prevent: Donor screening and proper cleansing of donor arm
Bacterial contamination (Infective shock)
Whole blood, red cells or platelets contaminated with bacteria eg Yersinia enterocolitica, Staphylococcus
Usually during infusion of first 100 ml of contaminated pack.
Renal failure, shock Very high mortality if high bacterial count
PATHOPHYSIOLOGY OF IHTR Antigen-antibody complex Complement activation lysis of red cells haemoglobinuria Activation of coagulation Bradykinin capillary permeability & dilation Hypotension DIC Renal failure
-3-
Вам также может понравиться
- Phelebotomy Answers 01 2018Документ61 страницаPhelebotomy Answers 01 2018Aaron Wallace100% (1)
- Disturbances in OxygenationДокумент10 страницDisturbances in OxygenationjenrylОценок пока нет
- Anatomy of The SkinДокумент28 страницAnatomy of The Skinay254Оценок пока нет
- Quality Assurance in The Blood BankДокумент41 страницаQuality Assurance in The Blood Bankgauravmahajan4480% (5)
- Blood Transfusion FinalДокумент8 страницBlood Transfusion FinalejkohОценок пока нет
- NGT Enteral Feeding CareДокумент8 страницNGT Enteral Feeding CareSheng GosepОценок пока нет
- Blood TransfusionДокумент55 страницBlood Transfusionanand7504100% (2)
- Delivery Room,.Документ3 страницыDelivery Room,.Yukki CuartoОценок пока нет
- Transfusion Reaction - DRGSPДокумент42 страницыTransfusion Reaction - DRGSPGaurav PawarОценок пока нет
- Hematologic DisorderДокумент86 страницHematologic Disorderasnake Dagnew100% (1)
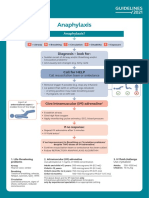
- Refractory Anaphylaxis Algorithm 2021Документ1 страницаRefractory Anaphylaxis Algorithm 2021ay254Оценок пока нет
- Dermatitis101 Diagnosis Treatment EczemaДокумент45 страницDermatitis101 Diagnosis Treatment EczemaUkhti NounaniarnurseОценок пока нет
- Muscle Origins and InsertionsДокумент9 страницMuscle Origins and Insertionsnoisytaost92% (12)
- Intra-Abdominal Hypertension GuideДокумент40 страницIntra-Abdominal Hypertension GuideBayu Surya Dana100% (1)
- IV Fluid Therapy GuideДокумент3 страницыIV Fluid Therapy GuideMary Anthonette Arenas EstradaОценок пока нет
- Transfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1Документ33 страницыTransfusion Reaction and Coombs Test: Moderator:-Dr Sanjay Agrwal Presenter: - DR Pratima Singh PG Jr-1UmikaguptaОценок пока нет
- Understanding DIC: Risks, Pathophysiology, Diagnosis & ManagementДокумент31 страницаUnderstanding DIC: Risks, Pathophysiology, Diagnosis & ManagementKristine Kringle33% (3)
- The Triage ProcessДокумент3 страницыThe Triage ProcessepingОценок пока нет
- Diagrammatic Description of Blood Preparation ProcessesДокумент17 страницDiagrammatic Description of Blood Preparation ProcessesJes CmtОценок пока нет
- Laboratory Test InterpretationДокумент73 страницыLaboratory Test Interpretationjosieangel11Оценок пока нет
- Anaphylaxis Algorithm 2021Документ1 страницаAnaphylaxis Algorithm 2021Shawn Gaurav JhaОценок пока нет
- Anaphylaxis Algorithm 2021Документ1 страницаAnaphylaxis Algorithm 2021Shawn Gaurav JhaОценок пока нет
- BC 700 BC 720 BrochureДокумент2 страницыBC 700 BC 720 Brochure郑伟健Оценок пока нет
- Cardio and Hema - DR PueyoДокумент161 страницаCardio and Hema - DR Pueyoapi-3735995100% (2)
- The Difference Between Osmolality and OsmolarityДокумент2 страницыThe Difference Between Osmolality and OsmolaritySri FadhillaОценок пока нет
- Five Minute Personality Test PDFДокумент1 страницаFive Minute Personality Test PDFSekar MuruganОценок пока нет
- Ebola Presentation Ab-5 2Документ21 страницаEbola Presentation Ab-5 2api-302080035Оценок пока нет
- Simple Schematic Diagram of PneumoniaДокумент1 страницаSimple Schematic Diagram of PneumoniaTyrel LozanoОценок пока нет
- Drugs For GUTДокумент11 страницDrugs For GUTAyesha LiaqatОценок пока нет
- CASE ANALYSIS - Chronic TympanomastoiditisДокумент5 страницCASE ANALYSIS - Chronic TympanomastoiditisTerry Mae Atilazal SarciaОценок пока нет
- Fluorescent Treponemal Antibody Absorption FTA ABS TestДокумент22 страницыFluorescent Treponemal Antibody Absorption FTA ABS TestMekar PalupiОценок пока нет
- Fluid ElectrolyteДокумент115 страницFluid ElectrolytePaul EbenezerОценок пока нет
- Immediate Hemolytic Transfusion ReactionДокумент2 страницыImmediate Hemolytic Transfusion ReactionleoОценок пока нет
- Basic of Fluid Therapy ImaДокумент69 страницBasic of Fluid Therapy Imal Made ArtawanОценок пока нет
- Course in The WardДокумент4 страницыCourse in The WardNejie Zarrah DiazОценок пока нет
- Allergic RhinitisДокумент20 страницAllergic RhinitisMichaelPTОценок пока нет
- HPV Virus Causes Recurrent Respiratory Papillomatosis in BoyДокумент21 страницаHPV Virus Causes Recurrent Respiratory Papillomatosis in BoyDaffa IbnurasyОценок пока нет
- Ebola Virus: Deadly Hemorrhagic FeverДокумент16 страницEbola Virus: Deadly Hemorrhagic FeverSisilia AlfinaОценок пока нет
- Pathophysiology of ArrhythmiasДокумент15 страницPathophysiology of ArrhythmiasJonathan MontecilloОценок пока нет
- Discharge PlanДокумент1 страницаDischarge PlanKamille Bianca Macapagal ÜОценок пока нет
- Acute Glomerulonephritis Case StudyДокумент6 страницAcute Glomerulonephritis Case StudyjakerzОценок пока нет
- Drug StudyДокумент4 страницыDrug StudyArdy PadamadaОценок пока нет
- Letter Consent To Participate FormДокумент5 страницLetter Consent To Participate FormkeithОценок пока нет
- Infectious DiseasesДокумент2 страницыInfectious DiseasesChuckie Miguel Axalan BacolodОценок пока нет
- Causes, Symptoms and Treatment of Pneumonia in ChildrenДокумент4 страницыCauses, Symptoms and Treatment of Pneumonia in ChildrenPrincessMagnoliaFranciscoLlantoОценок пока нет
- Acute AppendicitisДокумент23 страницыAcute AppendicitisSandie Daniel GabalunosОценок пока нет
- ImmunedisorderДокумент3 страницыImmunedisorderDyan LazoОценок пока нет
- Fact Sheet 6 - Genetic Counselling: Page 1 of 2 WWW - Genetics.edu - Au Updated 15 June 2016Документ2 страницыFact Sheet 6 - Genetic Counselling: Page 1 of 2 WWW - Genetics.edu - Au Updated 15 June 2016Yuliandini Pangestika WiyonoОценок пока нет
- Concept Map Template NURS 3073Документ3 страницыConcept Map Template NURS 3073Savanna ChambersОценок пока нет
- Case Analysis Colorectal CancerДокумент4 страницыCase Analysis Colorectal CancerKhie-An Ocampo0% (1)
- PneumoniaДокумент4 страницыPneumoniaroscelle100% (1)
- Objectives For Hospital ExperienceДокумент5 страницObjectives For Hospital ExperienceJorie RocoОценок пока нет
- ER to Discharge CourseДокумент3 страницыER to Discharge CourseAljon S. TemploОценок пока нет
- Aplastic Anemia: Rare Blood Disorder Causes FatigueДокумент11 страницAplastic Anemia: Rare Blood Disorder Causes FatigueToni Shiraishi-Aque RuizОценок пока нет
- Nanda Nursing Diagnosis Examples:: Vague Uneasy Feeling ofДокумент3 страницыNanda Nursing Diagnosis Examples:: Vague Uneasy Feeling ofYOLANDA P. DELCASTILLOОценок пока нет
- GROUP 3 - CASE STUDY - TraumaДокумент5 страницGROUP 3 - CASE STUDY - TraumaDinarkram Rabreca EculОценок пока нет
- University of The Southern Caribbean Maracas Royal Road, Maracas, St. JosephДокумент12 страницUniversity of The Southern Caribbean Maracas Royal Road, Maracas, St. JosephTISHANNA GLASSGOWОценок пока нет
- Dengue FeverДокумент39 страницDengue FeverMuhammad Alauddin Sarwar100% (15)
- What Is AsthmaДокумент13 страницWhat Is AsthmaMuchlissatus Lisa MedicalbookОценок пока нет
- CPM 10th Ed Community Acquired PneumoniaДокумент23 страницыCPM 10th Ed Community Acquired PneumoniaJan Mikhail FrascoОценок пока нет
- LOSARTANДокумент3 страницыLOSARTANAubrey Unique EvangelistaОценок пока нет
- NursingCare PlanДокумент8 страницNursingCare PlanSunSearra Kennedy RuffinОценок пока нет
- Grabe Ka FinalДокумент57 страницGrabe Ka FinalJoanne Bernadette AguilarОценок пока нет
- Cardiac NSG DiagnosisДокумент5 страницCardiac NSG DiagnosisShreyas WalvekarОценок пока нет
- Triage Process in Emergency MedicineДокумент31 страницаTriage Process in Emergency MedicineGab PagalilauanОценок пока нет
- CHICKEN POX Genesis CarandangДокумент10 страницCHICKEN POX Genesis CarandangGenEsis CarandangОценок пока нет
- ChickenpoxДокумент16 страницChickenpoxJeet ThuraiОценок пока нет
- Health and Nutrition: HyperlipidemiaДокумент20 страницHealth and Nutrition: HyperlipidemiaRinoy R BhagoraОценок пока нет
- MeaslesДокумент32 страницыMeaslesYum C100% (2)
- HPB Adverse Transfusion ReactionДокумент26 страницHPB Adverse Transfusion ReactionFransiscus RivaldyОценок пока нет
- Blood Transfusion Guide for Immediate ReactionsДокумент8 страницBlood Transfusion Guide for Immediate ReactionsJohann OrtizОценок пока нет
- Quality Standards Primary Care Equipment and Drug ListsДокумент10 страницQuality Standards Primary Care Equipment and Drug Listsay254Оценок пока нет
- Quality Standards for Primary Care Resuscitation TrainingДокумент10 страницQuality Standards for Primary Care Resuscitation Trainingay254Оценок пока нет
- Emergency Treatment of Anaphylaxis May 2021 - 0Документ61 страницаEmergency Treatment of Anaphylaxis May 2021 - 0Glades AlvarezОценок пока нет
- Key Recommendations For Clinical Practice: Airway And/or Breathing And/or Circulation ProblemsДокумент5 страницKey Recommendations For Clinical Practice: Airway And/or Breathing And/or Circulation ProblemsShawn Gaurav JhaОценок пока нет
- British Standards of Hair RestorationДокумент10 страницBritish Standards of Hair Restorationay254Оценок пока нет
- Local Anaesthetic Systemic Toxicity V6Документ10 страницLocal Anaesthetic Systemic Toxicity V6ay254Оценок пока нет
- Hair Loss v0.5 PathwayДокумент1 страницаHair Loss v0.5 PathwayAdi PurnomoОценок пока нет
- Emergency Medicines - PHA 59 - April 2017Документ31 страницаEmergency Medicines - PHA 59 - April 2017ay254Оценок пока нет
- Anatomy and Functions of the Digestive TractДокумент27 страницAnatomy and Functions of the Digestive Tractay254Оценок пока нет
- Nicky - Human Milk BankДокумент2 страницыNicky - Human Milk BankKaye Tubungbanua - MatunogОценок пока нет
- Aféresis Fresenius AmicusДокумент15 страницAféresis Fresenius AmicusNimsi AstiviaОценок пока нет
- Pediatric Normal Laboratory ValuesДокумент15 страницPediatric Normal Laboratory ValuesAkhmad Dani AwaludinОценок пока нет
- Complete Blood CountДокумент21 страницаComplete Blood CountKrisha Vitto100% (1)
- Case 1: 25 Yr Old Patient With History of FatigueДокумент79 страницCase 1: 25 Yr Old Patient With History of FatigueMira WryczaОценок пока нет
- Daftar Harga Alkes & Reagensia E-CatalogДокумент3 страницыDaftar Harga Alkes & Reagensia E-CatalogPT SNAFAОценок пока нет
- RH IncompatibilityДокумент6 страницRH IncompatibilityEly TaОценок пока нет
- Blood Groups and Blood TransfusionДокумент18 страницBlood Groups and Blood TransfusionAbdul HafeezОценок пока нет
- MILER DISC Aplicationn Platelet CountДокумент2 страницыMILER DISC Aplicationn Platelet CountanggaririnОценок пока нет
- Blood Transfusion TherapyДокумент38 страницBlood Transfusion TherapyAnn Merlin JobinОценок пока нет
- Principles of Blood TransfusionДокумент2 страницыPrinciples of Blood TransfusionGerardLum100% (3)
- Patient-Doctor DialogueДокумент6 страницPatient-Doctor DialogueAlexis Angel DiMaria Muñoz QОценок пока нет
- Transfusion Medicine in Exotic Pets: Marla Lichtenberger, DVM, DACVECCДокумент8 страницTransfusion Medicine in Exotic Pets: Marla Lichtenberger, DVM, DACVECCAlice HellerОценок пока нет
- Clinpath-04.-Disorders of Hemostasis and Blood CoagulationДокумент11 страницClinpath-04.-Disorders of Hemostasis and Blood CoagulationCharisse Angelica MacedaОценок пока нет
- Flow cytometry and red cell indices analysisДокумент4 страницыFlow cytometry and red cell indices analysisKINGSCOMPUTERS CYBERОценок пока нет
- Childrens FBC Reference Ranges PDFДокумент1 страницаChildrens FBC Reference Ranges PDFCerianne BodionganОценок пока нет
- Practical Physiology Gm 2023 1 Часть ! -12 30 Марта-1Документ118 страницPractical Physiology Gm 2023 1 Часть ! -12 30 Марта-1Shubham RaoОценок пока нет
- Interference in Coagulation Testing: Focus On Spurious Hemolysis, Icterus, and LipemiaДокумент10 страницInterference in Coagulation Testing: Focus On Spurious Hemolysis, Icterus, and LipemiaMichael John AguilarОценок пока нет
- ABO Blood Group SystemДокумент3 страницыABO Blood Group SystemGwyneth Marie DayaganОценок пока нет
- Anticoagulant Types, Preparation and Mechanisms of ActionДокумент15 страницAnticoagulant Types, Preparation and Mechanisms of Actionmulugeta fentaОценок пока нет
- Overview of the coagulation systemДокумент9 страницOverview of the coagulation systemaksinuОценок пока нет
- Banana Milk Mujigae Harga - Google SearchДокумент1 страницаBanana Milk Mujigae Harga - Google SearchLILI WILDHANIОценок пока нет
- C4 Procedure For Serum and Plasma SepartionДокумент2 страницыC4 Procedure For Serum and Plasma SepartionLinguumОценок пока нет
- RH Factor PGДокумент3 страницыRH Factor PGapi-375530349Оценок пока нет