Академический Документы
Профессиональный Документы
Культура Документы
Clavicle Fracture
Загружено:
sridharОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Clavicle Fracture
Загружено:
sridharАвторское право:
Доступные форматы
Acute Clavicle Fractures
Carl J. Basamania, MD, FACS Chief, Adult Reconstructive Shoulder Surgery Division of Orthopaedic Surgery Duke University Medical Center
a fracture of the clavicle has been greatly underrated in respect to pain and disability. the usual or routine treatment is perhaps far short of satisfying, relieving therapy.
Carter R. Rowe, 1968
Clavicle fractures are very common, accounting for 5-15% of all fractures and nearly half of all shoulder fractures. Middle third fractures are by far the most common, accounting for 80% of all clavicle fractures with lateral third fractures accounting for about 10-15% and medial third fractures accounting for about 5% 23.
It used to be thought than most clavicle fractures occurred as the result of a direct blow to the clavicle. However, the clavicle is typically fractured by a fall on to the lateral aspect of the shoulder
24
. Less commonly, it can also be fractured by a
direct blow as seen in seat belt fractures or in sports such as lacrosse. There are reported cases of stress fractures of the clavicle, typically in overhead athletes. Midshaft clavicle fractures tend to occur in younger individuals while lateral third fractures tend to occur in older individuals. Earlier literature suggested that the rate of healing with non-operative treatment was quite high
19, 28
approximately 99% were felt to heal without complication.
However, no recent study has been able to reproduce these results. In fact, most recent studies have shown a nonunion rate of 15-25% 10, 21, 26 . More importantly, when looking at patient satisfaction, 30 - 50% of patients who had sustained a
clavicle fracture, even as long as ten years previously, felt that they had not fully recovered and were dissatisfied with the result 21. Most clavicle fractures are multiplanar injuries; that is, the fracture displacement occurs in multiple planes: angulation, shortening and medial rotation. This is due to the weight of the arm and the pull of the various muscles about the shoulder, particularly the anterior muscles such as the pectoralis.
Fracture Classification
There are numerous classification systems for clavicle fractures 21, 24, 28; however, it is really only important to describe them as displaced or nondisplaced and comminuted or simple. Lateral third fractures are usually referred to as Type II or III fractures; however, in this case, it is important only to recognize whether or not the stabilizing CC ligaments are involved. If the ligaments are involved, as would typically be the case in a fracture in the region of the coracoid, the fracture is inherently unstable, whereas fractures occurring in the lateral most aspect of the clavicle or lateral to the CC ligament insertions are inherently stable. It is important to note that in skeletally immature patients, lateral clavicle fractures are usually periosteal sleeve avulsions and can be treated nonoperatively since they have considerable potential for remodeling, even towards the end of the growth period.
Clinical Evaluation
Clavicle fractures typically do not present as a diagnostic dilemma since the injury is rather obvious in most cases. There is usually a clear history of some form of either direct or indirect injury to the shoulder. The patient typically presents splinting the injured side due to the pain. There is usually tenting of the skin over the fracture site; however, open fractures of the clavicle are quite rare. It is of utmost importance to assess for other associated injuries due to the trauma
4, 14, 18
. These can be classified as injuries to the surrounding bone and soft tissue,
lung, vascular structures and the brachial plexus. A careful neurovascular exam should be documented in all clavicle fractures. The obvious nature of the clavicle
fracture should not detract from other boney injuries such as those to the scapula and underlying ribs.
Radiographic Evaluation Many physicians accept a single AP radiographic view to assess injuries to the
clavicle; however, it is impossible to assess fracture displacement on a single radiograph. Unfortunately, it is not possible to obtain orthogonal views (views at right angles to each other) of the clavicle. The next best technique is to obtain an AP and 45 degree cephalic tilt AP radiograph. The contour and displacement can best be seen on the 45-degree cephalic tilt view.
Lateral third clavicle fractures must include an axillary radiograph to assess
posterior displacement of the medial fragment relative to the lateral fragment.
It is not possible to assess accurately shortening of a clavicle fracture on plain
radiographs. This is because the shortening occurs obliquely to the plane of the radiograph. In fact, short of 3D CT reconstructions with side-to-side comparisons, shortening can only be measured clinically.
Treatment
The statement that all clavicle fractures heal well is probably one of the greatest fallacies in all of orthopaedics
19, 28
. Many clavicle fractures can be treated non-
operatively. However, as more and more studies have suggested a poorer outcome with non-operative treatment, it is important to recognize those that may require operative intervention 10, 21, 26. For those fractures that are nondisplaced or are minimally displaced (100% or less displacement and less than 15-20mm of shortening), patients can be treated in a sling or a figure of eight harness. Studies have suggested that there is no difference in these two treatment modalities 1; however, both have significant limitations. First, the figure of eight harness tends to be very awkward to put on and maintain. It should be adjusted frequently to keep proper tension on the brace. Secondly, the figure of eight harness itself usually lies directly over the fracture
and can actually exacerbate the discomfort rather than alleviate it. The advantage of the figure of eight harness is that it frees up both upper extremities for day-today activities. It can also be used quite successfully in treating medial third clavicle fractures. The primary problem with the sling is that it is typically worn with the arm internally rotated and this can exacerbate the shortening and rotation of the fracture. If used, the sling is better if the arm is held in a neutral position; i.e., with the forearm pointing straight ahead. An attempt at closed reduction of clavicle fractures is not only painful but also probably futile. At best, patients will remain in the position they present with on first evaluation. Repeat exams and radiographs are justified to make sure a minimally or non-displaced fracture remains so. In the case of lateral third fractures, a Kenny Howard brace, which forces the clavicle downward and the shoulder/arm upward, can be tried; however, compliance with this brace is very poor. Ironically, patients who do comply with wearing of this brace can be at risk for skin breakdown under the brace. There are certain cases where operative intervention is indicated 10, 21,26: 1. Neurovascular injury or compromise that is progressive or that fails to reverse with closed reduction of the fracture 2. Severe displacement caused by comminution with resultant angulation and tenting of the skin severe enough to threaten its integrity and that fails to respond to a closed reduction 3. An open fracture that will require operative debredment 4. Multiple trauma, when mobility of the patient is desirable and closed methods of immobilization are impractical or impossible 5. A "floating" shoulder, with a displaced clavicular fracture and an unstable scapular fracture, with compromise of the acromioclavicular and coracoacromial ligaments. 6. Factors that render the patient unable to tolerate closed immobilization, such as the neurological problems of Parkinsonism, seizure disorders, or other neurovascular disorders
7. The very rare patient for whom the cosmetic lump over the healed clavicle would be intolerable A relative indication for operative intervention is displacement of the fracture fragments more than 100% (the width of the clavicle) and shortening more than 20mm. Most poor outcomes after non-operative treatment of clavicle fractures occur in patients who have more this much displacement. In addition, patients who have a butterfly fragment that is flipped 90 degrees on the 45-degree cephalic tilt radiograph tend to have poorer outcomes and should be considered for operative intervention 21.
Operative Treatment
There are two primary forms of operative treatment of midshaft clavicle fractures: plate and screw fixation and intramedullary fixation. Due to the significant forces placed on the clavicle, most other types of fixation, such as circlage wires, are inadequate, and should not be considered. One type of fixation that is contraindicated in clavicle fractures is smooth wire fixation. For some reason, smooth wires have a very significant tendency to migrate and the literature is replete with cases of smooth wires migrating from the shoulder to almost unimaginable locations such as the lung, abdomen, and spine
15, 17, 20, 29
Both intramedullary fixation and plate fixation have been shown to have good outcomes in treating clavicle fractures. The choice is more related to the experience and comfort level of the surgeon in regards to operating in this area. The primary advantage of plate and screw fixation is that most orthopaedic surgeons are comfortable with using this technique. The primary disadvantage is that this type of surgery has to be performed through a rather large, non-cosmetic incision with the risk of compromise of the bones blood supply due to soft tissue stripping. Removal of the plate and screws requires a second major procedure that can leave the clavicle with multiple stress rises and can place the patient at risk for later re-fracture 3.
The primary advantage of intramedullary fixation is that it can be accomplished through a small, cosmetic incision and the hardware can later be removed under
local anesthesia. The primary disadvantage of this type of fixation is that most surgeons are unfamiliar with this technique and that fact that there is less rotational control of the fragments with the intramedullary fixation 9. Lateral third clavicle fractures represent a special dilemma: most occur in older patients from standing height falls; however, the nonunion rate from nonoperative treatment is rather high 25, 27. Some surgeons suggest that many of these nonunions are relatively asymptomatic; however, most surgeons feel that operative intervention is indicated due to the high nonunion rate 5, 7, 13, 30. Fixation of lateral third fractures can be difficult due to the location of the fracture and the difficulty in getting enough adequate purchase with the fixation devices. Plate and screw fixation is very difficult to achieve unless the plate extends out on to the acromion 16. Because of this, most surgeons prefer suture circlage or coracoclavicular screw fixation 2, 30. Pin or smooth wire fixation through the acromion and into the clavicle can be used; however, this is rather weak fixation and carries the risk of damage to the acromioclavicular joint and smooth pin migration 8. With suture fixation, sutures are passed around the coracoid the around or through the medial clavicle fragment to achieve and hold the reduction. Although relative easy to do, there is a risk of the sutures sawing through the clavicle or coracoid if non-absorbable sutures are used. Absorbable sutures can be used; however, these may weaken and fail before adequate healing has taken place. With coracoclavicular screw fixation, a screw is passed through the medial fragment into the coracoid. This is a very strong form of fixation when properly placed; however, it is technically more difficult and the screw should be removed once healing is achieved, necessitating a second operative procedure. Late treatment of lateral third nonunions usually consists of excision of the distal fragment. The medial fragment must be stabilized with a ligament transfer due to the earlier injury to the CC ligaments. Failure to do so can result in significant instability of the clavicle. Intraarticular distal clavicle fractures can be treated with rest until there is evidence of radiographic and clinical healing. If the patient has later symptoms,
they can be treated with a simple distal clavicle resection. Stability of the remaining clavicle should be assessed at the time of surgery.
References: 1. Andersen K, Jensen PO, Lauritzen J. Treatment of clavicular fractures. Figure-of-eight bandage versus a simple sling. Acta Orthop Scand 1987 Feb;58(1):71-4. 2. Ballmer FT, Gerber C. Coracoclavicular screw fixation for unstable fractures of the distal clavicle. A report of five cases. J Bone Joint Surg Br 1991 Mar;73(2):291-4. 3. Bostman O, Manninen M, Pihlajamaki H. Complications of plate fixation in fresh displaced midclavicular fractures. J Trauma 1997 Nov;43(5):77883. 4. Dath R, Nashi M, Sharma Y, Muddu BN. Pneumothorax complicating isolated clavicle fracture. Emerg Med J 2004 May;21(3):395-6. 5. Edwards DJ, Kavanagh TG, Flannery MC. Fractures of the distal clavicle: a case for fixation. Injury 1992;23(1):44-6. 6. Emond SD, Tayoun P, Bedolla JP, Camargo CA, Jr. Injuries in a 1-day recreational cycling tour: Bike New York. Ann Emerg Med 1999 Jan;33(1):56-61. 7. Eskola A, Vainionpaa S, Patiala H, Rokkanen P. Outcome of operative treatment in fresh lateral clavicular fracture. Ann Chir Gynaecol 1987;76(3):167-9. 8. Fann CY, Chiu FY, Chuang TY, Chen CM, Chen TH. Transacromial Knowles pin in the treatment of Neer type 2 distal clavicle fracturesA prospective evaluation of 32 cases. J Trauma 2004 May;56(5):1102-5. 9. Grassi FA, Tajana MS, D'Angelo F. Management of midclavicular fractures: comparison between nonoperative treatment and open intramedullary fixation in 80 patients. J Trauma 2001 Jun;50(6):1096-100. 10. Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middlethird fractures of the clavicle gives poor results. J Bone Joint Surg Br 1997 Jul;79(4):537-9. 11. Iannotti MR, Crosby LA, Stafford P, Grayson G, Goulet R. Effects of plate location and selection on the stability of midshaft clavicle
osteotomies: a biomechanical study. J Shoulder Elbow Surg 2002 Sep;11(5):457-62. 12. Jubel A, Andermahr J, Prokop A, Isenberg J, Rehm KE. [Minimal invasive biological osteosynthesis of the clavicle with a titanium nail]. Kongressbd Dtsch Ges Chir Kongr 2002;119:485-90. 13. Kao FC, Chao EK, Chen CH, Yu SW, Chen CY, Yen CY. Treatment of distal clavicle fracture using Kirschner wires and tension-band wires. J Trauma 2001 Sep;51(3):522-5. 14. Kendall KM, Burton JH, Cushing B. Fatal subclavian artery transection from isolated clavicle fracture. J Trauma 2000 Feb;48(2):316-8. 15. Leppilahti J, Jalovaara P. Migration of Kirschner wires following fixation of the clavicle--a report of 2 cases. Acta Orthop Scand 1999 Oct;70(5):517-9. 16. Mizue F, Shirai Y, Ito H. Surgical treatment of comminuted fractures of the distal clavicle using Wolter clavicular plates. J Nippon Med Sch 2000 Feb;67(1):32-4. 17. Naidoo P. Migration of a Kirschner Wire from the clavicle into the abdominal aorta. Arch Emerg Med 1991 Dec;8(4):292-5. 18. Natali J, Maraval M, Kieffer E, Petrovic P. Fractures of the clavicle and injuries of the sub-clavian artery. Report of 10 cases. J Cardiovasc Surg (Torino) 1975 Sep;16(5):541-7. 19. Neer CS II: Nonunion of the clavicle. JAMA 172:10061011, 1960. 20. Nordback I, Markkula H. Migration of Kirschner pin from clavicle into ascending aorta. Acta Chir Scand 1985;151(2):177-9. 21. Nowak J. Clavicular Fractures: Epidemiology, Union, Malunion, Nonunion. Uppsala, Sweden: Acta Universitatis Upsalaiensis; 2002. 22. Poigenfurst J, Rappold G, Fischer W. Plating of fresh clavicular fractures: results of 122 operations. Injury 1992;23(4):237-41. 23. Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg 2002 Sep;11(5):452-6. 24. Robinson CM. Fractures of the clavicle in adults. Epidemiology and classification. J Bone Joint Surg Br 1998;80-B(3):476-84.
25. Robinson CM, Cairns DA. Primary nonoperative treatment of displaced lateral fractures of the clavicle. J Bone Joint Surg Am 2004 Apr;86A(4):778-82. 26. Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am 2004 Jul;86-A(7):1359-65. 27. Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis 2002;61(1-2):32-9. 28. Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop 1968 May;58:29-42. 29. Subbotin VM, Sukhanov SG. [Migration of a foreign body into the aorta following osteosynthesis of the clavicle]. Grud Serdechnososudistaia Khir 1991 Feb;(2):56. 30. Yamaguchi H, Arakawa H, Kobayashi M. Results of the Bosworth method for unstable fractures of the distal clavicle. Int Orthop 1998;22(6):366-8.
Вам также может понравиться
- Lower Limb Evaluation Format Lower Limb Fracture Assesstment FormДокумент12 страницLower Limb Evaluation Format Lower Limb Fracture Assesstment FormsridharОценок пока нет
- IIITDM Yoga HandbookДокумент24 страницыIIITDM Yoga HandbookBenoit HsuОценок пока нет
- Hepatitis B VirusДокумент47 страницHepatitis B VirusDiah Puspita RiniОценок пока нет
- Liver Enzymes (AST-ALT)Документ3 страницыLiver Enzymes (AST-ALT)sridharОценок пока нет
- 10-11 Gbs General Neuro 2nd YearДокумент29 страниц10-11 Gbs General Neuro 2nd YearsridharОценок пока нет
- 01-13 2 End Diastolic Pneumatic Compression Boot As A Treatment of PVD or LymphedemaДокумент4 страницы01-13 2 End Diastolic Pneumatic Compression Boot As A Treatment of PVD or LymphedemasridharОценок пока нет
- Nerve Conduction Velocity StudiesДокумент12 страницNerve Conduction Velocity StudiessridharОценок пока нет
- Guidelines For Pre Submission Seminar-LPUДокумент1 страницаGuidelines For Pre Submission Seminar-LPUsridharОценок пока нет
- PNFДокумент39 страницPNFsridhar100% (1)
- Patterns of PNFДокумент39 страницPatterns of PNFsridhar100% (1)
- Brachial Plexus InjuryДокумент43 страницыBrachial Plexus InjurysridharОценок пока нет
- Ankle MobilizationДокумент16 страницAnkle MobilizationsridharОценок пока нет
- Adverse Reaction To DrugsДокумент22 страницыAdverse Reaction To DrugssridharОценок пока нет
- Inflammatory My Opa ThiesДокумент10 страницInflammatory My Opa ThiessridharОценок пока нет
- Brachial Plexus InjuryДокумент43 страницыBrachial Plexus InjurysridharОценок пока нет
- Imaging Findings and Clinical Correlation: Cerebral Herniation SyndromesДокумент64 страницыImaging Findings and Clinical Correlation: Cerebral Herniation SyndromessridharОценок пока нет
- Sudden Infant Death SyndromeДокумент20 страницSudden Infant Death SyndromesridharОценок пока нет
- Brachial Plexus InjuryДокумент43 страницыBrachial Plexus InjurysridharОценок пока нет
- Imaging Findings and Clinical Correlation: Cerebral Herniation SyndromesДокумент64 страницыImaging Findings and Clinical Correlation: Cerebral Herniation SyndromessridharОценок пока нет
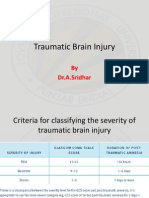
- Traumatic Brain InjuryДокумент26 страницTraumatic Brain InjurysridharОценок пока нет
- Thoracic Spine AnatomyДокумент5 страницThoracic Spine AnatomysridharОценок пока нет
- Tardieu ScaleДокумент2 страницыTardieu ScalesridharОценок пока нет
- Application FormatДокумент2 страницыApplication FormatsridharОценок пока нет
- Windlass Effect Ankle JointДокумент35 страницWindlass Effect Ankle JointsridharОценок пока нет
- Skanda Shasti KavachamДокумент6 страницSkanda Shasti KavachamsriramanaОценок пока нет
- Vinayagar Agaval - Avvaiyar PDFДокумент17 страницVinayagar Agaval - Avvaiyar PDFkckejaman100% (1)
- College of NursingДокумент1 страницаCollege of NursingsridharОценок пока нет
- Infra RedДокумент7 страницInfra RedsridharОценок пока нет
- Clavicle FractureДокумент4 страницыClavicle FracturesridharОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- General PrinciplesДокумент61 страницаGeneral PrinciplesAnda Madalina ZahariaОценок пока нет
- Approach To FractureДокумент17 страницApproach To FractureRebecca WongОценок пока нет
- NBPME Part II 2008 Practice Tests 1-3Документ49 страницNBPME Part II 2008 Practice Tests 1-3Vinay Matai50% (2)
- Musculoskeletal TraumaДокумент20 страницMusculoskeletal TraumawidanОценок пока нет
- Treatment and Rehabilitation of Fractures (Stanley Hoppenfeld)Документ1 страницаTreatment and Rehabilitation of Fractures (Stanley Hoppenfeld)小蓮花Оценок пока нет
- 06 Principles of Orthopaedic Traction SystemsДокумент12 страниц06 Principles of Orthopaedic Traction SystemsNiyati RathodОценок пока нет
- Rib Fracture Repair Cost-BenefitДокумент4 страницыRib Fracture Repair Cost-Benefitdella oktaviani100% (1)
- UME Radiology Musculoskeletal Imaging (Review)Документ52 страницыUME Radiology Musculoskeletal Imaging (Review)Nguyễn Hoàng SơnОценок пока нет
- Classification of FracturesДокумент50 страницClassification of Fracturesmohammad farhanОценок пока нет
- Laukota's Paper PDFДокумент7 страницLaukota's Paper PDFislamellabbanОценок пока нет
- Colles Fracture & Knee DislocationДокумент38 страницColles Fracture & Knee DislocationNap91Оценок пока нет
- Interpreting The Orthopaedic X-Rays - NewДокумент29 страницInterpreting The Orthopaedic X-Rays - NewSanju427Оценок пока нет
- Bioelectricity and Microcurrent TherapyДокумент11 страницBioelectricity and Microcurrent TherapyGustavo Cabanas100% (2)
- First Aid Personal Hygiene and Sanitation 2Документ23 страницыFirst Aid Personal Hygiene and Sanitation 2Wen Legazpi100% (1)
- Pathophysiology of FractureДокумент2 страницыPathophysiology of FractureEunice CuñadaОценок пока нет
- Dental Procedure CodesДокумент42 страницыDental Procedure CodesTonderai KurewaОценок пока нет
- Principle of Fracture & Dislocation ManagementДокумент118 страницPrinciple of Fracture & Dislocation ManagementBryan LeongОценок пока нет
- A Comprehensive Overview On Osteoporosis and Its Risk FactorsДокумент21 страницаA Comprehensive Overview On Osteoporosis and Its Risk Factorsdenta aeОценок пока нет
- 7.5 Statistical Data-Safety RecordsДокумент2 страницы7.5 Statistical Data-Safety RecordsKlemens SuhartonoОценок пока нет
- Bone Healing Radiology of Normal and Diseased BoneДокумент40 страницBone Healing Radiology of Normal and Diseased BoneAhmed SalmanОценок пока нет
- Cancer massage therapy contraindicationsДокумент15 страницCancer massage therapy contraindicationsMya AlissandraОценок пока нет
- Case Study On Normal Vaginal DeliveryДокумент40 страницCase Study On Normal Vaginal DeliveryPabhat Kumar100% (1)
- Conservative Treatment of Clavicle FracturesДокумент21 страницаConservative Treatment of Clavicle FracturesErwan Ahmad DОценок пока нет
- PIN SITE CARE USING CHLORHEXIDINEДокумент10 страницPIN SITE CARE USING CHLORHEXIDINEBabang YasОценок пока нет
- Treatment and Rehabilitation of Fractures (Stanley Hoppenfeld)Документ1 страницаTreatment and Rehabilitation of Fractures (Stanley Hoppenfeld)小蓮花Оценок пока нет
- Grade 9-Pe and Health 3RD QuarterДокумент6 страницGrade 9-Pe and Health 3RD QuarterJemar Cadion ArotaОценок пока нет
- Orthopedics Toronto NotesДокумент47 страницOrthopedics Toronto Noteskyliever78% (9)
- Geriatric Rehab Device Choices: Cane, Crutches, Walker or Forearm Supports for 78yo F after Knee ReplacementДокумент31 страницаGeriatric Rehab Device Choices: Cane, Crutches, Walker or Forearm Supports for 78yo F after Knee ReplacementsmrutiptОценок пока нет
- R. Kleining (Auth.), Hans K. Uhthoff MD, FRCS (C), Elvira Stahl BA, FAAAS, FAMWA (Eds.) - Current Concepts of External Fixation of Fractures-Springer-Verlag Berlin Heidelberg (1982)Документ432 страницыR. Kleining (Auth.), Hans K. Uhthoff MD, FRCS (C), Elvira Stahl BA, FAAAS, FAMWA (Eds.) - Current Concepts of External Fixation of Fractures-Springer-Verlag Berlin Heidelberg (1982)Jose Enrique FonsecaОценок пока нет
- Final Surgery Exam Vi Sem 2021Документ37 страницFinal Surgery Exam Vi Sem 2021Mohammed ShafiОценок пока нет