Академический Документы
Профессиональный Документы
Культура Документы
Guidelines For Management of Suspected Rabies Exposures
Загружено:
Wira Febrisandi IrsanОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Guidelines For Management of Suspected Rabies Exposures
Загружено:
Wira Febrisandi IrsanАвторское право:
Доступные форматы
Ministry of Health and Long-Term Care
Ministre de la Sant et des Soins de longue dure
GUIDELINES FOR MANAGEMENT OF SUSPECTED RABIES EXPOSURES
January, 2010 All suspected incidents must be reported to the local medical officer of health [Health Protection and Promotion Act, Reg. 557, s. 2 (1)] who can provide consultation and the necessary biologicals. The following is a condensed version of the Rabies Vaccine chapter in the Canadian Immunization Guide (Seventh Edition, Public Health Agency of Canada, 2006, pp.285-97) and the National Advisory Committee on Immunizations Recommendations Regarding the management of Bat Exposures to Prevent Human Rabies (CCDR, November 2009). Text in italics has been added or substituted by the Ministry of Health and Long-Term Care based on the Rabies Prevention and Control Protocol, 2009). Please note that this document ONLY summarizes post-exposure prophylaxis guidelines. For information about pre-exposure management and vaccination of high-risk occupational categories, please see the relevant chapter in the Canadian Immunization Guide.
Post-exposure management
1. Species of animal Squirrels, hamsters, guinea-pigs, gerbils, chipmunks, rats, mice or other rodents, rabbits and hares are only rarely found to be infected with rabies and are not known to have caused human rabies in North America; post-exposure prophylaxis should be considered only if the animals behaviour was highly unusual. 2. Type of exposure Three broad categories of exposure are recognized as warranting post-exposure prophylaxis: bite, nonbite and bat exposures. Bite: This is defined as any penetration of the skin by teeth. Non-bite: This category includes contamination of scratches, abrasions or cuts of the skin or mucous membranes by saliva or other potentially infectious material, such as the brain tissue of a rabid animal. Petting a rabid animal or handling its blood, urine or feces is not considered to be an exposure, but such contact should be avoided. Being sprayed by a skunk is also not considered an exposure. Exposures incurred in the course of caring for humans with rabies could theoretically transmit the infection. No case of rabies acquired in this way has been documented, but post-exposure prophylaxis should be considered for exposed individuals. Bat exposures: With respect to human exposures to bats, post-exposure prophylaxis (PEP) is recommended only: OR when there is direct contact with a bat (the bat should be observed to touch or land on the person) AND either of the following cannot be eliminated: a bat bite or scratch or saliva from a live bat entered an open wound or mucous membranes. when a bat bite or scratch has occurred,
Guidelines for Management of Suspected Rabies Exposures, MOHLTC, January 2010 In an adult, a bat landing on clothing would be considered reason for PEP administration only if a bite, scratch, or saliva exposure into a wound or mucous membrane could not be ruled out. Therefore, if a bat lands on the clothing of a person who can be sure that a bite or scratch did not occur and that the bats saliva did not contact an open wound or mucous membranes, then PEP is not required. In a child, any direct contact with a bat (i.e. the bat landing on or touching the child) should be considered a reason for PEP administration, including contact through clothes, as a history to rule out a bite, scratch or mucous membrane exposure may not be reliable. When a bat is found in the room with a child or adult who is unable to give a reliable history, assessment of direct contact can be difficult. Factors indicating that direct contact may have occurred in these situations include the individual waking up crying or upset while the bat was in the room, or observation of an obvious bite or scratch mark. Extreme care should be taken to ensure that there is no further exposure to the bat if it is captured or handled. In the event that the bat is captured, it should be submitted for rabies testing. Unless exposure to the bat is in the persons head or neck region, PEP can be delayed for up to 48 hours until the rabies test result on the bat is obtained. If PEP was initiated, it can be discontinued if the bat tests negative for rabies. Please note that spelunker exposure in caves will require special consideration. Rarely, transmission has been recorded when virus was inhaled, or infected grafts/organs were transplanted into patients. Post-exposure prophylaxis is warranted and recommended in rare instances of non-bite exposure, such as inhalation of aerosolized virus by spelunkers exploring caves inhabited by infected bats or by laboratory technicians homogenizing tissues infected with rabies virus. 3. Investigation of the incident Each incident of possible exposure requires a full investigation. This should include an assessment of the risk of rabies in the animal species involved and, in a low prevalence area such as Canada, the behaviour of the particular domestic animal implicated. An unprovoked attack is more likely to indicate that the animal is rabid. Nevertheless, rabid cats and dogs may become uncharacteristically quiet. Bites inflicted on a person attempting to feed or handle an apparently healthy animal should generally be regarded as provoked. Domestic pets with up-to-date rabies vaccination are unlikely to become infected with rabies. If vaccinated animals exhibit signs suggestive of rabies they must be carefully evaluated by a veterinarian. Any animal that has bitten a human and/or is suspected of being rabid should be reported to the local medical officer of health and to the nearest Canadian Food Inspection Agency (CFIA) veterinarian. These veterinarians are familiar with the regulations concerning rabies and, if necessary, will collect and ship appropriate specimens to a federal laboratory for diagnosis. Further information and advice is obtainable from the CFIA regional offices or local district office on the CFIA Web site (http://inspection.gc.ca/english/anima/heasan/offbure.shtml) or by consulting the blue pages of the local telephone directory. Signs of rabies cannot be reliably interpreted in wild animals. These animals should immediately be humanely killed in a way that does as little damage as possible to the head, which should be submitted for laboratory examination. Rabies virus is readily demonstrable in brains of animals that have neurologic symptoms. Stray or ownerless dogs or cats that seem healthy should be observed for evidence of rabies for 10 days if feasible, but if isolation and observation are not feasible, the animal should be euthanized and tested for rabies. Exotic pets (other than ferrets) should be treated as wild animals because the incubation period and period of rabies virus shedding in these animals are unknown. Recent information regarding the pathogenesis of rabies in domestic ferrets has prompted them to be considered in the same category as domestic dogs and cats rather than wild carnivores.
Guidelines for Management of Suspected Rabies Exposures, MOHLTC, January 2010
Management of people after possible exposure to rabies
Immediate washing and flushing of the wound with soap and water is imperative and is probably the most effective procedure in the prevention of rabies. Suturing the wound should be avoided if possible. Tetanus prophylaxis and antibacterial drugs should be given as required. The recommendations in the following table are intended as a guide and may need to be modified in accordance with the specific circumstances of the exposure. Table 12. Post-exposure Prophylaxis for Persons Not Previously Immunized Condition of animal of time of exposure Healthy and available for 10 days observation
Animal species Dog, cat or ferret
Management of exposed person 1. Local treatment of wound 2. At first sign of rabies in animal, give RabIg (local and intramuscular) and start HDCV or PCECV, unless bite wound to the head or neck (generally begin immediately see text below for other considerations)
Rabid or suspected to be rabid*. Unknown or escaped
1. Local treatment of wound 2. RabIg (local and Intramuscular) and HDCV or PCECV
Skunk, bat, fox, coyote, raccoon and other carnivores. Livestock, rodents or lagomorphs (hares and rabbits)
Regard as rabid* unless geographic area is known to be rabies free
1. Local treatment of wound 2. RabIg (local and intramuscular) and HDCV or PCECV**
Consider individually. Consult appropriate public health and CFIA officials. Bites of squirrels, chipmunks, rats, mice, hamsters, gerbils, other rodents, rabbits and hares may warrant post-exposure rabies prophylaxis if the behaviour of the biting animal was highly unusual.
Rablg = (human) rabies immune globulin, HDCV = human diploid cell vaccine (Imovax), PCECV = purified chick embryo cell culture vaccine (RabAvert) * If possible, the animal should be humanely killed and the brain tested for rabies as soon as possible; holding for observation is not recommended. Discontinue vaccine if fluorescent antibody test of animal brain is negative. ** See text for potential bat exposure.
Schedule and dosage
Post-exposure prophylaxis of previously unimmunized individuals Five doses of 1.0 mL of HDCV or PCECV should be given, the first dose (on day 0) as soon as possible after exposure and additional doses on each of days 3, 7, 14 and 28 after the first dose. Vaccine should be administered intramuscularly into the deltoid muscle (never in the gluteal region) or the anterolateral upper thigh in infants. An appropriate dose of RabIg, as described below, should also be given on day 0. Neutralizing antibodies develop 7 days after immunization and persist for at least 2 years. Post-exposure prophylaxis should be started as soon as possible after exposure and should be offered to exposed individuals regardless of the elapsed interval. When notification of an exposure is delayed, prophylaxis may be started as late as 6 or more months after exposure. Based on a risk assessment, and where the specimen is received at the lab within 48hrs of exposure, treatment may be withheld until the Fluorescent Antibody Test (FAT) result is available. The FAT report can be obtained within 6 to 24 hours from receipt of an animal specimen at the laboratory. If the suspect animal is 3
Guidelines for Management of Suspected Rabies Exposures, MOHLTC, January 2010 a cat, dog or ferret and is available for observation, then immunization may be withheld pending the animals status after the 10-day observation period. However, if the bite wound is to the head and neck region, prophylaxis should generally begin immediately and not be delayed, unless a risk assessment would support a 10-day observation period instead. Considerations that may support delaying initiation of prophylaxis and instead observing the animal for a 10day period include: if the animal is a domestic pet; if the animal is fully vaccinated; if the bite was provoked; and if there is very low prevalence of rabies in the area. If a rabies exposure is considered likely then post-exposure prophylaxis should never be delayed. The vaccine series may be discontinued after consultation with public health/infectious disease experts if the FAT of the brain of an animal killed at the time of attack is negative. However, if suspicion of rabies in the animal remains high, even in the presence of a negative test, the immunization series should be continued. The recommended dose of human RabIg is 20 IU/kg body weight. This formula is applicable to all age groups, including children. Preferably, the full dose of RabIg should be thoroughly infiltrated into the wound and surrounding area. If not anatomically feasible, any remaining volume of RabIg should be injected, using a separate needle and syringe, intramuscularly at a site distant from vaccine administration. When more than one wound exists, each should be locally infiltrated with a portion of the RabIg using a separate needle and syringe if possible. In such instances, the RabIg may be diluted 2- to 3-fold in a solution of 0.9% sodium chloride in order to provide the full amount of human RabIg required for good infiltration of sites at risk of rabies. If the site of the wound is unknown, the entire dose should be administered intramuscularly. Because of interference with active antibody production, the recommended dose should not be exceeded. Under no circumstances should vaccine be administered in the same syringe or at the same site as RabIg. Protective antibodies are present immediately after passive vaccination with RabIg, but they have a half-life of only approximately 21 days. Since vaccine-induced antibodies begin to appear within 1 week, there is no value in administering RabIg more than 8 days after initiating an approved vaccine course. RabIg is supplied in 2 ml vials containing 150 IU/ml. Use the following formulae to calculate the dose required and use the table to determine how many vials to order: 20 IU/kg x (client wt in kg) 150 IU/mL = dose in mL 9.09 IU/lb x (client wt in lb) 150 IU/mL = dose in mL TOTAL WEIGHT To 33 lbs To 15 Kg 34 66 lbs 15 - 30 Kg 67 99 lbs 30 - 45 Kg 100 132 lbs 45 - 60 Kg 133 165 lbs 60 - 75 Kg # OF VIALS 1 2 3 4 5 TOTAL WEIGHT 166 198 lbs 75 - 90 Kg 199 231 lbs 90 - 105 Kg 232 264 lbs 105 120 Kg 265 297 lbs 120 135 Kg 298 330 lbs 135 150 Kg # OF VIALS 6 7 8 9 10
Post-exposure prophylaxis of previously immunized individuals Post-exposure prophylaxis for people who have previously received rabies vaccine differs according to which preparation of vaccine was received. 1. Two doses of HDCV or PCECV, one injected immediately and the other 3 days later, without RabIg, are recommended for exposed individuals with the following rabies immunization history: Completion of an approved course of pre-or post-exposure prophylaxis with HDCV or PCECV; Completion of immunization with other types of rabies vaccine or with HDCV or PCECV according to unapproved schedules as long as neutralizing rabies antibody has been demonstrated in serum (see serologic testing below). 4
Guidelines for Management of Suspected Rabies Exposures, MOHLTC, January 2010 2. A complete course of HDCV or PCECV plus RabIg is recommended for those who may have received rabies vaccines in the past but do not fulfill the criteria listed in point 1. A serum sample may be collected before vaccine is given, and if an acceptable antibody ( 0.5 IU/ml) is demonstrated, the course may be discontinued, provided that at least two doses of vaccine have been given. If in doubt, consultation with an infectious diseases or public health physician is recommended.
Route of administration
RabIg is always given intramuscularly. If possible, the full dose of RabIg should be thoroughly infiltrated into the wound and surrounding area. If this is not anatomically feasible, any remaining volume of RabIg should be injected, using a separate needle and syringe, intramuscularly at a site distant from vaccine administration. Rabies vaccine for post-exposure prophylaxis must be administered intramuscularly. Both HDCV and PCECV are approved in Canada for intramuscular (IM) use.
Serologic testing
Healthy people immunized with an appropriate regimen do not require routine post-immunization antibody determinations. Determination of post-immunization antibody titre may be advisable for those whose immune response may be reduced by illness, medication or advanced age. Corticosteroids, immunosuppressive agents and immunosuppressive illnesses may interfere with the antibody response. Where antibody levels are required, a sample of 5cc whole clotted blood, or serum therefrom, should be submitted to the nearest regional public health laboratory or directly to the Central Public Health Laboratory, 81 Resources Road, Toronto, Ontario M9P 3T1, telephone: (416) 235 5725. There is no charge for this test. To establish laboratory priority, please indicate the purpose of the sample. An acceptable antibody response is a titre of 0.5 IU/mL by the rapid fluorescent-focus inhibition test.
Other considerations
Vaccine interchangeability: wherever possible, an immunization series should be completed with the same product. However, if this is not feasible, RabAvert and Imovax Rabies are considered interchangeable in terms of indications for use, immunogenicity, efficacy and safety.
FOR MORE INFORMATION: www.phac-aspc.gc.ca/publicat/cig-gci/index.html (Canadian Immunization Guide, 7th Edition) www.vaccineshoppecanada.com/secure/pdfs/CA/IMOVAX_E.pdf (HDCV/Imovax product monograph) www.merckfrosst.ca/mfcl/en/corporate/products/rabavert.html (PCEC / RabAvert product monograph) www.vaccineshoppecanada.com/secure/pdfs/ca/imogam_e.pdf (RabIg/Imogam product monograph) http://www.mnr.gov.on.ca/en/Business/Rabies/index.html (Ministry of Natural Resources rabies in Ontario) http://www.inspection.gc.ca/english/anima/disemala/rabrag/rabrage.shtml (Canadian Food Inspection Agency rabies in Canada) http://www.cdc.gov/rabies (Centre for Disease Control and Prevention) http://www.who.int/rabies/en/ (World Health Organization)
Вам также может понравиться
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- George WashingtonДокумент12 страницGeorge Washingtonsubathra samiveluОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- Broken DollsДокумент77 страницBroken DollsGene FogertyОценок пока нет
- 9 A Bond of BloodДокумент411 страниц9 A Bond of BloodEva CórdovaОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Milk Production TamilnaduДокумент14 страницMilk Production TamilnaduGomatheeswariОценок пока нет
- Mindmap BedahДокумент120 страницMindmap BedahKavin Maalan SadasseevanОценок пока нет
- Level 2 Diploma Health and Social Care: Unit 22 - Undertake Agreed Pressure Area CareДокумент6 страницLevel 2 Diploma Health and Social Care: Unit 22 - Undertake Agreed Pressure Area CareJayne AshleyОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Notes On Sva N TensesДокумент8 страницNotes On Sva N TensesNur SheilaОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- F Y) Y, 0 y 3: Fuad Adrian Iskandar 1606843722 PR-I Matematika Terapan (Statistik)Документ2 страницыF Y) Y, 0 y 3: Fuad Adrian Iskandar 1606843722 PR-I Matematika Terapan (Statistik)Nadia KarimaОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Primary and Secondary LesionsДокумент7 страницPrimary and Secondary LesionsCoral Srinivasa Ramalu50% (2)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- مقدمة علم التشريحДокумент64 страницыمقدمة علم التشريحsayfmohammed719Оценок пока нет
- Her Dawggie Valentine by Tonya Ramagos Cont No GДокумент20 страницHer Dawggie Valentine by Tonya Ramagos Cont No GRachel MorseОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Your First 24 Hours in IslamДокумент11 страницYour First 24 Hours in IslamAbdulRehman100% (1)
- Get To Know Detachable Clipper Blades - Ivan Zoot - Clipper Guy Says...Документ8 страницGet To Know Detachable Clipper Blades - Ivan Zoot - Clipper Guy Says...Ivan Zoot100% (4)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Manobo Religious Believes and PracticesДокумент3 страницыManobo Religious Believes and PracticesKurt ZepedaОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
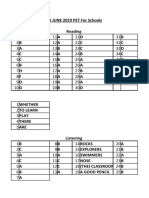
- Keys For Pet Exam PackДокумент34 страницыKeys For Pet Exam PackEleftheria AggeleaОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- 11 Axis FormationДокумент61 страница11 Axis Formationapi-3800038100% (1)
- Modifiers 02Документ2 страницыModifiers 02jaysakeОценок пока нет
- Phrase - Handout 6 - ExercisesДокумент9 страницPhrase - Handout 6 - ExercisesVeasna ChannОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Tehnik - Tehnik MenjahitДокумент6 страницTehnik - Tehnik MenjahitBang mantoОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Kasus Myasis Yang Disebabkan Oleh Chrysomya Bezziana Di Pulau JawaДокумент8 страницKasus Myasis Yang Disebabkan Oleh Chrysomya Bezziana Di Pulau JawaIswandiIbnAmirОценок пока нет
- Level-1 S S SharebookДокумент1 страницаLevel-1 S S Sharebookcastillofloresmarlen396Оценок пока нет
- Frog's Muscular SystemДокумент9 страницFrog's Muscular SystemRon Olegario95% (22)
- Intervention For Voice Disorders PDFДокумент14 страницIntervention For Voice Disorders PDFSiti muhajarohОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- TweetsДокумент134 страницыTweetsAilene VasileОценок пока нет
- Alemayehu Regassa Senbetu, EthiopiaДокумент8 страницAlemayehu Regassa Senbetu, EthiopiaAlemayehu RegassaОценок пока нет
- SN2 Jan 2007Документ20 страницSN2 Jan 2007metawarОценок пока нет
- Endocrine System GlandsДокумент40 страницEndocrine System GlandsSolita PorteriaОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- 6 - Immune Deficiency Diseases 2Документ8 страниц6 - Immune Deficiency Diseases 2Belle Galao GepteОценок пока нет
- Bang MasturbationforpeopleofallgendersandabilitiesДокумент132 страницыBang MasturbationforpeopleofallgendersandabilitiesOlya TsarevОценок пока нет
- Louisiana Hunting Regulations 2010 - 2011Документ47 страницLouisiana Hunting Regulations 2010 - 2011wstОценок пока нет