Академический Документы
Профессиональный Документы
Культура Документы
Medicaid Expansion Cost Grassroots in Michigan Research
Загружено:
apackof2Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Medicaid Expansion Cost Grassroots in Michigan Research
Загружено:
apackof2Авторское право:
Доступные форматы
Medicaid Expansion Cost.
As proponents attempt to convince states that the cost of the Medicaid expansion will be covered by the federal government, the facts remain the same. To start with, the enhanced match is only for the expansion population, not the existing Medicaid population. In addition, it does not apply to administrative costs, which add about 5 percent to benefit payments. Finally, the full 100 percent enhanced match is temporary, with states picking up 10 percent of the new costs in 2020 and thereafter. Jack McHugh MAC Center At a time when Medicaid is already overwhelming current state budgets, it would be counter- productive for states to voluntarily add to those liabilities. In addition, there are numerous other cost pressures states need to consider when assessing the expansion. First, states will see increased enrollment among the nonexpansion population as the law also expands eligibility by changing how income is measured and corrals those eligible, but not enrolled, into the program. Second, states will face pressure from their hospitals to backfill $18 billion in federal payment cuts for uncompensated care. Third, the PPACA lifts Medicaid reimbursement for primary care physicians to Medicare levels, with federal funding of the differencebut only for two years. Once the federal funding expires, states will face pressure to maintain those levels and to increase payments to other physicians accept-ing Medicaid. Moreover, regardless of HHSs recent claim that it has backed away from previous proposals to shift Medicaid funding to a blended rate, the fiscal challenges facing Medicaid at the state and federal level make future financing adjustments to Medicaid unavoidable. Jack McHugh MAC Center Control. While the HHS Secretary has touted offering flex- ibility to the states, the law and HHS regulations offer states no meaning- ful policy discretion. Specifically, the law extends the maintenance of effort (MOE) restriction from the stimulus law that prevents states from making key changes to their Medicaid programs. Moreover, the recent HHS decision to eliminate any possibility of a state expanding its Medicaid program short of the 138 percent federal poverty level (FPL) further underscores that flexibility was more talk than action. Coverage.
Medicaid is inferior health care As with the exchanges, proponents stress the importance of Medicaid in expanding cover- age. Unlike the federal default in the exchange, there is no federal default for the Medicaid expansion. However, rather than throwing more people into a broken program, states should focus on improving the current program and developing sustainable alternatives for meeting the needs of the proposed expansion population. Fighting Back to Minimize the Damage of Bad Decisions Sometimes opposing bad policysuch as by declining to run exchanges or expand Medicaid while important, is not enough. In those instances, lawmakers need to work to minimize the impact of bad policies that they are unable to fully reverse. They also need to insist on transparency, accountability, and a level playing field, so as to create public awareness of the true consequences of bad policies and build support for future reforms. Still a Risky Proposition for the States Enormous uncertainty still surrounds the health care law. With less than one year remaining before the major provisions of Obamacare take effect, it is no surprise that barely more than one-fifth of states have publically agreed to both establish a state exchange and expand their Medicaid Heritage Fiundation As far as Medicaid I think it would be appropriate to point out the original govt projections on how much that was going to cost and how much it really ended up costing! History always repeats itself with these govt programs because nothing is ever learned from it. Here is a timeline going to 2009 http://www.kff.org/medicaid/timeline/pf_entire.htm This is from an paper (attached) from 1988 however, When Medicaid was enacted, its major purpose was to consolidate several grant programs that already were administered by the states. It was believed initially that Medicaid would add only $250 million to the health care expenditures of the federal government.3 Exhibit 1 depicts the growth in Medicaid expenditures over the past twenty years. In the first year of operation, the combined federal and state outlays were $1.5 billion. By 1975, spending had increased to $14.2 billion, and in 1987 the expenditures exceeded $47 billion.4 Enrollment has increased as well. In 1968 there were only 4.5 million recipients. Enrollment peaked at 24 million in 1977 and since has dropped to approximately 23.2 million in 1987. Medicaid currently accounts for over 10 percent of our nations total health care expenditures. According to the Kaiser Health Foundation Medicaid and CHIP stats Michigan has 20% of her total population enrolled in Medicaid (2009) Michigans Medicaid spending from 1990 -2010 has increased 8% ranking her as 23rd in the nation for Medicaid spending. In contrast our Midwestern neighbors Indiana has increased 5% and Illinois 6.6%
The state of Michigan spend $3,153,326,988 (2010) compared to $1,454,600,107 in Indiana and was the 9th highest in the country Michigan took NO pro-active containment actions for eligibility requirements BEFORE Affordable Care Act (ACA) regulations became law (Maintenance of eligibility requirements enacted as part of the Affordable Care Act (ACA) prohibit states from imposing eligibility and enrollment standards for Medicaid and CHIP that are more restrictive than those that were in place at the time the ACA was passed (March 23, 2010) Michigan has taken NO Medicaid Cost Containment Actions in 2012 or 2013 in areas where they could, such as LTC: Cost containment initiatives for long term care services. In Pharmacy Cost Containment Actions, Michigan has only implemented three of seven possible containments
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Hotel Association vs. RN KapoorДокумент2 страницыHotel Association vs. RN KapoorMEHUL KUMAR0% (2)
- Pit Bull Warning Flyer - Responsible Citizens For Public Safety (RC4PS)Документ1 страницаPit Bull Warning Flyer - Responsible Citizens For Public Safety (RC4PS)apackof2Оценок пока нет
- 13 Years Us Dog Bite Fatalities 2005 2017 DogsbiteДокумент9 страниц13 Years Us Dog Bite Fatalities 2005 2017 Dogsbiteapackof2Оценок пока нет
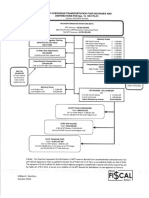
- Michigan 2018-2019 Transportation Fund Revenues and DistributionsДокумент1 страницаMichigan 2018-2019 Transportation Fund Revenues and Distributionsapackof2100% (1)
- Michigan 2018-2019 Transportation Fund Revenues and DistributionsДокумент1 страницаMichigan 2018-2019 Transportation Fund Revenues and Distributionsapackof2100% (1)
- Michigan 2018-2019 Transportation Fund Revenues and DistributionsДокумент1 страницаMichigan 2018-2019 Transportation Fund Revenues and Distributionsapackof2100% (1)
- Fiscal Brief Allocation of Federal Aid To LRA Feb19-1Документ5 страницFiscal Brief Allocation of Federal Aid To LRA Feb19-1apackof2Оценок пока нет
- Brochure Trifold - Responsible Citizens For Public Safety (RC4PS)Документ2 страницыBrochure Trifold - Responsible Citizens For Public Safety (RC4PS)apackof2Оценок пока нет
- Bill "Sanders" NowlingДокумент1 страницаBill "Sanders" Nowlingapackof2Оценок пока нет
- Gov. Snyder EXECUTIVE ORDER No. 2014-12Документ3 страницыGov. Snyder EXECUTIVE ORDER No. 2014-12apackof20% (1)
- Ballot Language To Amend Constitution To Increase The Sales TaxДокумент1 страницаBallot Language To Amend Constitution To Increase The Sales Taxapackof2Оценок пока нет
- My Grandfather Naturalization ApplicationДокумент1 страницаMy Grandfather Naturalization Applicationapackof2Оценок пока нет
- A Summary of House Joint Resolution Uu, Senate Bill 847, and House Bills 4593, 5492, and 5493Документ4 страницыA Summary of House Joint Resolution Uu, Senate Bill 847, and House Bills 4593, 5492, and 5493apackof2Оценок пока нет
- Michigan Proposal 1 of 2015Документ1 страницаMichigan Proposal 1 of 2015Beverly TranОценок пока нет
- Calley VotesДокумент3 страницыCalley Votesapackof2Оценок пока нет
- Michigan Same Sex Marriage JudgementДокумент31 страницаMichigan Same Sex Marriage JudgementpkampeОценок пока нет
- House Joint Resolution UU - Transportation Funding PackageДокумент4 страницыHouse Joint Resolution UU - Transportation Funding Packageapackof2Оценок пока нет
- Public Input On State Supt SearchДокумент1 страницаPublic Input On State Supt Searchapackof2Оценок пока нет
- PROP 1 InformationДокумент5 страницPROP 1 Informationapackof2Оценок пока нет
- Sandra Kahn Questionnaire and QualificationsДокумент4 страницыSandra Kahn Questionnaire and Qualificationsapackof2Оценок пока нет
- Credentials ChallengeДокумент5 страницCredentials Challengeapackof2Оценок пока нет
- John Hayhoe ExposedДокумент17 страницJohn Hayhoe Exposedapackof2Оценок пока нет
- Bobbi Schostack Endorments MIGOP ChairДокумент20 страницBobbi Schostack Endorments MIGOP Chairapackof2Оценок пока нет
- Testimony by The National Motorist Association On HB 4925Документ1 страницаTestimony by The National Motorist Association On HB 4925apackof2Оценок пока нет
- Ronna Romney McDaniels Questionnaire and QualificationsДокумент4 страницыRonna Romney McDaniels Questionnaire and Qualificationsapackof2Оценок пока нет
- Senate Passed Medicaid Expansion Sub For HB 4714Документ40 страницSenate Passed Medicaid Expansion Sub For HB 4714apackof2Оценок пока нет
- MIGOP Saint Clair County Part Resolution Against Medicaid Expansion Part 8Документ1 страницаMIGOP Saint Clair County Part Resolution Against Medicaid Expansion Part 8apackof2Оценок пока нет
- 2013-2014 State CommitteeДокумент3 страницы2013-2014 State Committeeapackof2Оценок пока нет
- Mary Sears Questionnaire and QualificationsДокумент5 страницMary Sears Questionnaire and Qualificationsapackof2Оценок пока нет
- MIGOP 5th Congressional District Resolution Against Medicaid Expansion Part 8Документ1 страницаMIGOP 5th Congressional District Resolution Against Medicaid Expansion Part 8apackof2Оценок пока нет
- The 14th Congressional District Republican Committee Resolution Opposing The Expansion of Medicaid and The Implementation of Health Care ExchangesДокумент1 страницаThe 14th Congressional District Republican Committee Resolution Opposing The Expansion of Medicaid and The Implementation of Health Care Exchangesapackof2Оценок пока нет
- Affidavit of Desistance OmbudsmanДокумент3 страницыAffidavit of Desistance OmbudsmanNinJj Mac100% (1)
- Bureaucracy of PakistanДокумент10 страницBureaucracy of PakistanJaweria AlamОценок пока нет
- Section 66a of It ActДокумент2 страницыSection 66a of It ActNeeraj BhargavОценок пока нет
- Law Litreture & FilmsДокумент38 страницLaw Litreture & FilmsSaksham BarsaiyaОценок пока нет
- Verification of Swedish Citizenship 2022Документ2 страницыVerification of Swedish Citizenship 2022Sava BozicОценок пока нет
- USA Today - March 10, 2022Документ39 страницUSA Today - March 10, 2022Alina YefimenkoОценок пока нет
- A.N. Sen, P.N. Bhagwati and Ranganath Misra, JJДокумент10 страницA.N. Sen, P.N. Bhagwati and Ranganath Misra, JJSowmya JogimuttОценок пока нет
- AC085Документ29 страницAC085PraveenОценок пока нет
- Current-Affairs 2013 Complete GuideДокумент167 страницCurrent-Affairs 2013 Complete GuideRaghuОценок пока нет
- 590657Документ202 страницы590657Bhaskar100% (2)
- Sponsorship FormДокумент2 страницыSponsorship FormRussominho ZewdeОценок пока нет
- Legal Research by ONGДокумент72 страницыLegal Research by ONGyvette soonОценок пока нет
- Memo in Opposition To TROДокумент7 страницMemo in Opposition To TROcraigery82Оценок пока нет
- Counsel For Plaintiff Todd Feinstein and Interim Lead Class CounselДокумент3 страницыCounsel For Plaintiff Todd Feinstein and Interim Lead Class CounselgloprestiОценок пока нет
- Life SciencesДокумент1 страницаLife Sciencesarka prava LahiriОценок пока нет
- Don FrankДокумент3 страницыDon FrankDeKalb OfficersОценок пока нет
- Vodoviz - ENP Course - Visa Liberalisation Towards Ukraine As An ENP ToolДокумент14 страницVodoviz - ENP Course - Visa Liberalisation Towards Ukraine As An ENP ToolWeronika WodowizОценок пока нет
- Eo#2020 001Документ2 страницыEo#2020 001Ma. Christina Libo-onОценок пока нет
- Garcillano v. HORДокумент2 страницыGarcillano v. HORJoshua AbadОценок пока нет
- Report ABRAJANOДокумент5 страницReport ABRAJANOMikee RamirezОценок пока нет
- Saratoga Springs City Employee Salaries (Page 2)Документ1 страницаSaratoga Springs City Employee Salaries (Page 2)Emily DonohueОценок пока нет
- Group 2 Activity 3: HE O LLДокумент13 страницGroup 2 Activity 3: HE O LLJoel100% (2)
- Work EthicsДокумент14 страницWork EthicsArshad Mohd100% (1)
- Political and Constitutional Development SalmaДокумент12 страницPolitical and Constitutional Development SalmaKhan Ume Salma Danish100% (1)
- National Policy On Gender in Basic Education: Federal Ministry of Education Nigeria JANUARY 2006Документ31 страницаNational Policy On Gender in Basic Education: Federal Ministry of Education Nigeria JANUARY 2006Dahiru AbbaОценок пока нет
- Republic v. Holy TrinityДокумент14 страницRepublic v. Holy TrinityReal TaberneroОценок пока нет
- vr1 Verification Request Form v3 2106162192016461440Документ2 страницыvr1 Verification Request Form v3 2106162192016461440Richu PaliОценок пока нет
- Last One Year Current Affairs Ebook July 2023 Edition English MediumДокумент147 страницLast One Year Current Affairs Ebook July 2023 Edition English MediumExcellence of Execution100% (1)
- 2005 09 05 - DR1Документ1 страница2005 09 05 - DR1Zach EdwardsОценок пока нет