Академический Документы
Профессиональный Документы
Культура Документы
Physiological Consideration in Oral Formulation Development Gastrointestinal Tract (GIT) in Relevance With Controlled Drug Release PDF
Загружено:
Farah FauziaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Physiological Consideration in Oral Formulation Development Gastrointestinal Tract (GIT) in Relevance With Controlled Drug Release PDF
Загружено:
Farah FauziaАвторское право:
Доступные форматы
Teaching Note: Controlled Drug Release Technology Class 2013
Physiological Consideration in Oral Formulation Development
Gastrointestinal Tract (GIT) in Relevance with Controlled Drug Release: Characteristics, Function, pH, Transit Time, Mucus Membrane Farah Fauzia (0906640791) The rate and extent of absorption of drugs is highly depending on the route of administration; the most common for controlled-release: oral administration. The efficiency will be greatly affected by the physiology of gastrointestinal tract (GIT).
GIT Basic Characteristics Long muscular tube (Figure 1); specialized areas for digest and storage [1]. Designed for the absorption of nutrients; involves fluid secretion to ensure optimum environment for enzymes to work [1]. GIT dividing: preparative & primary storage region (mouth & stomach); secretory & absorptive region (mid-gut); water reclamation system and wasteproduct storage system (colon) [1] (summary: Figure 2). Mouth (Oral Cavity) [1, 2] Guard the GIT by moistening the food. Comprises the lips, cheek, tongue, hard palate, soft palate, and floor of the mouth (Figure 3); The lining is oral mucosa, includes buccal, sublingual, gingival, palatal, and labial mucosa. Overall route is in Figure 4. Potential for drug delivery; advantages: bypass the first pass effect of GIT, avoid pre-systemic elimination in GIT; not using GIT route; Oral mucosal drug delivery: 1) local delivery, 2) systemic delivery: by buccal (immobile surface; Figure 5) or sublingual mucosa (more permeable). Roles in drug delivery: pH, fluid volume, enzyme activity, permeability of mucosa; affected by saliva secretion. Saliva: viscous, watery fluid; lubricate oral cavity, facilitate swallowing, prevent teeth demineralization; 1-2 L discharged per day; composition and pH varies with the rate of secretion (Figure 6); favorable for drug release especially from hydrophilic polymer based. Esophagus [1, 3] Approximately 40 cm (in adult); has a surface of squamous epithelium with a protective function. Transit time taking only around 10-14 s; drug shape factors affecting it.
1 Farah Fauzia (0906640791) Bioprocess Engineering Universitas Indonesia
Teaching Note: Controlled Drug Release Technology Class 2013
Stomach (Gastric) [1, 3-5] First GIT organ located in abdomen (Figure 7); one of GIT reservoirs; digest food and deliver chime to the intestine. Volume swells to accommodate meal without mixing; capacity up to 1.5 L, 50-100 ml in fasted state; capacity can affect the absorption. Lined by epithelium covered by impermeable gastric mucus layer; secrete bicarbonate and create pH gradient (key features: Figure 7). Varied pH, with 1 2.5, generally similar as HCl solution of 1, 1.2, or 1.8; favorable for ionized drugs; co-administration of drug with water or food can affect the pH; acidic pH kill most microbes. Supply calories to small intestine by controlling rate of emptying according to food type; classification: (1) liquid, (2) digestible solids, (3) indigestible solids; summary in Figure 9; liquid emptied first, digestible solids are next, and indigestible solids are emptied later in the fasted state through migration myoelectric complex (MMC) process (Figure 10); varied emptying time, 5 min 2 hour, with half emptying time ~80.5 min Intestine [1, 4, 5] 6-7 m long (longest route); designed for food digestion and macromolecules assimilation; primary area for drug absorption (10-20 times of colon). Divided into three parts: duodenum (20-30 cm); jejunum (2.5 m); and ileum (3.5 m); has mucosa with great surface area (~200 m2 in adult), with 5 million of villi which is covered by epithelium (Figure 11). Varied transit time (0.5 9.5 hour); pH range 6.15 7.35; 6.8 7.88 in different region; varied microflora resembles both in stomach and colon). Is the primary area of the GIT for drug absorption (10-20 times of colon). Colon [1, 4, 5] Large intestine; 1.5 m long; a reservoir for reabsorption of water Environment differs along its length (Figure 12); transit time is varied, typically in a range of 6 to 32 hour; pH range of neutral Home to a large concentration of bacterial species, because of near neutral pH; offer opportunity for targeted delivery (example: some polysaccharides which are colon-microflora-biodegradable) GIT Mucus Layer [2, 6, 7] First membrane barriers in GIT to be encountered; constitutes of water, mineral salts, free proteins, lipids, and DNA. Viscoelastic and translucent; secreted throughout the GIT; prevents direct adhesion to the epithelial cells and retards the transport of active molecules Potential for drug and nutrient absorption through adhesion mechanism
2 Farah Fauzia (0906640791) Bioprocess Engineering Universitas Indonesia
Teaching Note: Controlled Drug Release Technology Class 2013
Mucin molecules Key macromolecular of mucus; large glycoprotein molecule (Figure 13) Govern viscoelastic properties of mucus; negatively charged, hydrophobic, varied structure & arrangement: concentration, pH and temperature dependent Serve as delivery vehicle as lubricant; play major role in adhesion of mucoadhesive drug delivery systems Mucus layer properties Viscoelastic: two types of mucus; different thickness (Figure 14). Hydrophobic: protect epithelium from proton of gastric liquid. Varied acidity: pH gradient across the mucus to ensure neutral pH. Mucosa physiological characteristics are varied (Figure 15). Mucoadhesion Attachment of a carrier to the mucus in bioadhesion; via mucoadhesive system; complex process; potential for improving controlled-release Mucoadhesives polymer: (1) first generation: hydrophilic, non-specific, pHdependent. Examples: chitosan, alginate, CMC; (2) second generation: able to target specific mucosal surface. Examples: lecithin. References 1. Wilson, C.G., The Organization of the Gut and the Oral Absorption of Drugs: Anatomical, Biological and Physiological Considerations in Oral Formulation Development, in Controlled Release in Oral Drug Delivery, C.G. Wilson and P.J. Crowley, Editors. 2011, Springer Science+Business Media: New York. p. 27-48. 2. Patel, V.F., F. Liu, and M.B. Brown, Advances in oral transmucosal drug delivery. J Control Release, 2011. 153(2): p. 106-16. 3. Hejazi, R. and M. Amiji, Chitosan-based gastrointestinal delivery systems. Journal of Controlled Release, 2003. 89(2): p. 151-165. 4. Cook, M.T., et al., Microencapsulation of probiotics for gastrointestinal delivery. J Control Release, 2012. 162(1): p. 56-67. 5. Sinha, V.R. and R. Kumria, Microbially triggered drug delivery to the colon. European Journal of Pharmaceutical Scienes, 2003. 18: p. 3-18. 6. Lafitte, G., Structure of the gastorintestinal mucus layer and implications for controlled release and delivery of functional food ingredients, in Delivery and Controlled Release Bioactives in Foods and Nutraceuticals, N. Garti, Editor 2008, Woodhead Publishing Limited: England. p. 26-47. 7. Madhav, N.V., et al., Orotransmucosal drug delivery systems: a review. J Control Release, 2009. 140(1): p. 2-11.
3 Farah Fauzia (0906640791) Bioprocess Engineering Universitas Indonesia
Teaching Note: Controlled Drug Release Technology Class 2013
Appendix
Figure 1 Illustration of the plan of the GIT showing arrangement of mucosa and muscles [1]
Figure 2 Characteristic of the GIT, showing the pH at the different parts [4]
Figure 3 Schematic representation of the different linings of mucosa in mouth [2]
Teaching Note: Controlled Drug Release Technology Class 2013
Figure 4 Buccal routes of delivery [1]
Figure 5 Schematic diagram of buccal mucosa [2]
Figure 6 The change in saliva pH and osmolality with increasing flow [1]
Figure 7 Diagram of the features of the GIT showing location in the abdomen [1]
Figure 8 Key gastric features [1]
Teaching Note: Controlled Drug Release Technology Class 2013
Figure 9 Emptying of tablet components with a meal. Dissolving drug will follow the liquid emptying curve [1]
Figure 10 The migrating myoelectric complex (MMC) or housekeeper sequence [1]
Figure 11 Structure of intestinal villus [1]
Teaching Note: Controlled Drug Release Technology Class 2013
Figure 12 Schematic of colon transit [1]
Figure 13 Structure and composition of a basic unit of mucin [7]
Figure 14 Thickness of the entire mucus layer in the GIT [6]
Figure 15 Table of comparison of different mucosa [2]
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- VOL-VCA EN Proefexamen PDFДокумент15 страницVOL-VCA EN Proefexamen PDFKonstantins Slatins100% (1)
- Gas Cylider Technical Regulation PDFДокумент37 страницGas Cylider Technical Regulation PDFVinod Varadan SОценок пока нет
- Project ReportДокумент67 страницProject ReportDivyanshu DkОценок пока нет
- Solar RefrigerationДокумент13 страницSolar RefrigerationNivash RamОценок пока нет
- MITOCHONDRIAДокумент3 страницыMITOCHONDRIAAbid RazaОценок пока нет
- Haefele AH A4 Mar 15 8.12-8.24Документ13 страницHaefele AH A4 Mar 15 8.12-8.24khurram1810Оценок пока нет
- Inorganic Chemistry Book2Документ272 страницыInorganic Chemistry Book2bhaks1976Оценок пока нет
- Braskem Braskem PP PCD 0140BR Polypropylene Impact CopolymerДокумент2 страницыBraskem Braskem PP PCD 0140BR Polypropylene Impact CopolymerBFCОценок пока нет
- (5403) Sheet Surface Chemistry Theory eДокумент24 страницы(5403) Sheet Surface Chemistry Theory eboom rangОценок пока нет
- SERIES 7000 Paste Slakers: Fully Automated Lime Slaking SystemsДокумент4 страницыSERIES 7000 Paste Slakers: Fully Automated Lime Slaking Systemssoumyarm942Оценок пока нет
- Energy and Power Ib2Документ24 страницыEnergy and Power Ib2Gkid GkidОценок пока нет
- Chapter 3.1 - CoagulationДокумент51 страницаChapter 3.1 - CoagulationHanif NifОценок пока нет
- Surface Water Treatment Operator Certification Manual - Tratamiento de Aguas ResidualesДокумент311 страницSurface Water Treatment Operator Certification Manual - Tratamiento de Aguas ResidualesJhon Jairo Mazuera GuzmanОценок пока нет
- BC Prescription Regulation TableДокумент2 страницыBC Prescription Regulation TableJuliaОценок пока нет
- Is 6262 1971Документ19 страницIs 6262 1971just_4_u_dear_in9549Оценок пока нет
- 17BEM0049DA1Документ12 страниц17BEM0049DA1Vedant KarnatakОценок пока нет
- Energy Notes 1Документ4 страницыEnergy Notes 1api-491081853Оценок пока нет
- LPG Standards PDFДокумент115 страницLPG Standards PDFhandoyo_eko20017573Оценок пока нет
- Design of Unistrut Farming SystemДокумент256 страницDesign of Unistrut Farming Systemjudaspriest21100% (1)
- Vacuum Regulator Gas Feed Systems Theory and MaintenanceДокумент62 страницыVacuum Regulator Gas Feed Systems Theory and Maintenancezhigang dingОценок пока нет
- Amino Crosslinkers: Product Guide - Cymel Resins - WorldwideДокумент20 страницAmino Crosslinkers: Product Guide - Cymel Resins - WorldwidejoseОценок пока нет
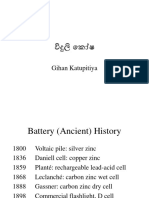
- BatteriesДокумент29 страницBatteriesgihan5dhananjaya5katОценок пока нет
- Kinetics of Inclusion Body Production in Batch and High Cell Density Fed-Batch Culture of Escherichia Coli Expressing Ovine Growth HormoneДокумент12 страницKinetics of Inclusion Body Production in Batch and High Cell Density Fed-Batch Culture of Escherichia Coli Expressing Ovine Growth HormoneSabhajeet YadavОценок пока нет
- Iso 19229 2019Документ10 страницIso 19229 2019laythОценок пока нет
- Acids, Bases and Salts MCQS: (D) (Ii) and (Iv)Документ12 страницAcids, Bases and Salts MCQS: (D) (Ii) and (Iv)Atharva BhokareОценок пока нет
- EBT 335 Polymer Blends: Presented By: PL TehДокумент23 страницыEBT 335 Polymer Blends: Presented By: PL TehTarani TharanОценок пока нет
- Biochemistry Unit ConversionДокумент4 страницыBiochemistry Unit ConversionTran Trong NghiaОценок пока нет
- Friedrich MohsДокумент7 страницFriedrich MohsJohnMadeОценок пока нет
- Origin and Evolution of LifeДокумент40 страницOrigin and Evolution of LifeMary Grace BesinОценок пока нет
- 5031 Acid Base WorksheetДокумент5 страниц5031 Acid Base WorksheetSaima Usman/TCHR/MGBОценок пока нет