Академический Документы
Профессиональный Документы
Культура Документы
Arf, CRF, BC
Загружено:
Jacqueline de AsisИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Arf, CRF, BC
Загружено:
Jacqueline de AsisАвторское право:
Доступные форматы
Renal Failure (Acute & Chronic) & Bladder Cancer
Consolidated by: Howell Thomas M. Alamo, MSN
Acute renal failure (ARF) is the abrupt deterioration of renal function that results in the accumulation
of fluids, electrolytes, and metabolic waste products. It is usually accompanied by a marked decrease in urinary output. Although ARF is often reversible, if it is ignored or inappropriately treated, it can lead to irreversible kidney damage and chronic renal failure. CATEGORIES OF ACUTE RENAL FAILURE A. prerenal (hypoperfusion of kidney) -occur as a result of impaired blood flow that leads to hypoperfusion of the kidney and a drop in the GFR. Common clinical situations are volume-depletion states (hemorrhage or GI losses), impaired cardiac performance (myocardia infarction, heart failure, or cardiogenic shock), vasodilation (sepsis or anaphylaxis). B. intrarenal (actual damage to kidney tissue) are the result of actual parenchymal damage to the glomeruli or kidney tubules. - burns, crush injuries, and infections, as well as nephrotoxic agents, may lead to acute tubular necrosis and cessation of renal function.Severe transfusion reactions Medications may also predispose a patient to intrarenal damage, especially nonsteroidal anti-inflammatory drugs (NSAIDs) and ACE inhibitors. C. postrenal (obstruction to urine flow). Postrenal causes of ARF are usually the result of an obstruction somewhere distal to the kidney. Pressure rises in the kidney tubules; eventually, the GFR decreases. PHASES OF ACUTE RENAL FAILURE initiation, oliguria, diuresis, and recovery. a. initiation period begins with the initial insult and ends when oliguria develops. b. oliguria period is accompanied by a rise in the serum concentration of substances usually excreted by the kidneys (urea, creatinine, uric acid, organic acids, and the intracellular cations [potassium and magnesium]). In this phase uremic symptoms first appear and life-threatening conditions such as hyperkalemia develop. c. In the diuresis period, the third phase, the patient experiences gradually increasing urine output, which signals that glomerular filtration has started to recover. The patient must be observed closely for dehydration during this phase d. The recovery period signals the improvement of renal function .May take 3 to 12 months. Laboratory values return to the patients normal level. What to ask during ASSESSMENT? HISTORY Taking. When you elicit the patients history, look for a disorder that can lead to prerenal, intrarenal, or postrenal ARF. Question the patient about recent illnesses, infections, or injuries, and take a careful medication history with attention to maximum daily doses and selfmedication patterns. Determine the patients urinary patterns and document information such as frequency of voiding, approximate voiding volume, and pattern of daily fluid intake. Evaluate the patient for a recent history of gastrointestinal (GI) problems, such as anorexia, nausea, and changes in bowel patterns. Some patients have a recent history of weight gain, edema, headache, confusion, and sleepiness. PHYSICAL EXAMINATION. The patient appears seriously ill and often drowsy, irritable, confused, and combative because of the accumulation of metabolic wastes. In the oliguric phase, the patient may show signs of fluid overload such as hypertension, rapid heart rate, peripheral edema, and crackles when you listen to the lungs. Patients in the diuretic phase appear dehydrated, with dry mucous membranes, poor skin turgor, flat neck veins, and orthostatic hypotension. The patient may have increased bleeding tendencies, such as petechiae, ecchymosis of the skin, and bloody vomitus (hematemesis). What to Expect in the DIAGNOSTIC PROCEDURES Test Normal Result Abnormality Urinalysis Clear, Reddish-brown urine, + colorless,straw,yellow RBC, +WBC or amber colored Blood urea 5-20 mg/dL Elevated nitrogen Serum Creatinine 0.5-1.1 mg/dL Elevated
Explanation Acute damage to kidneys causes loss of rbc and wbc and protein into the urine Kidneys cannot excrete wastes Kidneys cannot excrete
24-hr urine creatinine
F- 85-125 ml/min M- 95-135 ml/min
50 % decrease
wastes Acute damage to kidneys limits ability to clear creatinine
Other tests: Complete blood count; x-ray of kidney, ureter, bladder; blood urea nitrogen; creatinine; renal ultrasound; serum levels of Na, Mg, K, ABG PRIMARY NURSING DIAGNOSIS Fluid volume deficit rt excessive urinary output, vomiting, hemorrahage PLANNING AND IMPLEMENTATION Collaborative During the oliguric-anuric stage, diuretic therapy with furosemide (Lasix) or ethacrynic acid (Edecrin) may be attempted to convert oliguric ARF to nonoliguric ARF, which has a better renal recovery rate. During the diuretic phase, fluid volume replacement may be ordered to compensate for the fluid loss and to maintain adequate arterial blood flow to the kidneys. A daily record of intake, output, and weights assists the physician in making treatment decisions. Electrolyte replacement is based on the patients serum electrolyte values. The physician attempts to limit hyperkalemia because of its potentially lethal effects on cardiac function. Note the excretory route for medications so that the already damaged kidneys are not further damaged by nephrotoxins. The patients response to medications is important; drug dosages may need to be decreased because of decreased renal excretion. In addition, timing of medications may need to be changed because of increased excretion during dialysis. Hemodialysis, peritoneal dialysis, or alternative dialysis methods may be used to manage ARF. Indications for dialysis include fluid overload, hyperkalemia, metabolic acidosis, uremic intoxication, and the need to remove nephrotoxic substances such as metabolites or drugs. The diet for the patient with ARF is usually high in carbohydrates to prevent protein breakdown and low in protein to provide essential amino acids but to limit increases in azotemia (increased urea in the body). For patients who lose sodium in the urine, the diet is high in sodium; for patients with sodium and water retention, the diet is low in sodium and may also contain a fluid restriction. Potassium restrictions are frequently ordered, based on laboratory values. Medication Diuretics Dopamine Phosphate binders Dosage Varies by drug 1-3mcg/kg/min IV 15-30 ml with meals tid Description Furosemide;mannitol Vasodilator Aluminum hydroxide Rationale Convert oliguric phase to nonoliguric ohase Increase renal blood flow and urine output Increase GI excretion of phosphorus
Independent Rest and recovery are important nursing goals. By limiting an increased metabolic rate, the nurse limits tissue breakdown and decreases nitrogenous waste production. A quiet, well-organized environment at a temperature comfortable for the patient ensures rest and recovery. To help the patient deal with fluid restrictions, use creative strategies to increase the patients comfort and compliance. Give medications with meals or in minimal IV volumes to maximize the amount of fluid available for patient use. Several factors place the patient with ARF at risk for impaired skin integrity. Uremia results in itching and dryness of the skin. If the patient experiences pruritus, help the patient clip the fingernails short and keep the nail tips smooth. Use skin emollients liberally, avoid harsh soaps, and bathe the patient only when necessary. Frequent turning and range-of-motion exercises assist in preventing skin breakdown. If the patient is taking medications that cause frequent stools, clean the perineum and buttocks frequently to maintain skin integrity. Note that one of the most common sources of postrenal ARF is an obstructed urinary catheter drainage system. Before contacting the physician about a decreasing urinary output in an acutely or critically ill patient, make sure that the catheter is patent. If institutional policy permits, irrigate the Foley catheter using sterile technique with 30 mL of normal saline to check for obstruction. Note any kinks in the collecting system. If institutional policy permits, replace the indwelling Foley catheter with a new catheter and urinary drainage system to ensure it is functioning adequately. Signs that postrenal ARF is caused by obstruction in the urinary catheter include a sudden cessation of urinary output in a patient whose urinary output has previously been high or average and a urinary output with normal specific gravity and normal urinary sodium. The patient with ARF is often irritable and confused. Recognize that the irritability is part of the disease process. Keep the environment free of unnecessary clutter to reduce the chance of falls. If the patient is on bedrest, maintain the bed in the low position and keep the side rails up. Keep the patients call light within easy reach and the patients belongings on a bedside table close to the bed.
The patient with ARF is anxious, not only because of the ambiguity of the prognosis but also because he or she may be in an acute care environment for treatment. Provide the patient with ongoing, repeated information about what is happening and why. Ongoing reassurance for both the patient and the significant others is essential. Chronic renal failure (CRF) refers to irreversible renal dysfunction as manifested by the inability of the kidneys to excrete sufficient fluid and waste products from the body to maintain health. What to do ask during HISTORY taking? The patient may report a history of ARF although usually the patient does not become symptomatic until he or she has a GFR less than 35% of normal. The patient likely complains of oliguria and weight gain. Ask the patient about the color of the urine, whether it is clear or cloudy, and whether it is frothy. The patient may also complain of a metallic taste in the mouth, anorexia, and stomatitis. Elicit a gastrointestinal (GI) history with particular attention to nausea, vomiting, hematemesis, diarrhea, and constipation. Elicit the patients description of any central nervous system (CNS) symptoms. Blurred vision is common. Patients may have impaired decision making and judgment, irritability, decreased alertness, insomnia, increased extremity weakness, and signs of increasing peripheral neuropathy (decreased sensation in the extremities, hands, and feet; pain; and burning sensations). Patients often report changes in other body systems as well. Some have idiopathic bone and joint pain in the absence of a diagnosis of arthritis. Others suffer from loss of muscle mass and nocturnal leg cramping. Men may be impotent or notice gynecomastia, and women may mention amenorrhea. Both may have decreased libido. What to doduringPHYSICAL EXAMINATION. CRF affects all body systems. Patients with CRF have significant cardiovascular involvement. Hypertension is usually noted in the patient with CRF and may indeed be its cause. Patients often have rapid, irregular heart rates; distended jugular veins; and if pericarditis is present, a pericardial friction rub and distant heart sounds. Respiratory symptoms include hyperventilation, Kussmaul breathing, dyspnea, orthopnea, and pulmonary congestion. Rales may signify fluid overload. Frothy sputum combined with shortness of breath may indicate some degree of pulmonary edema. The renal effects of CRF are pronounced. You may smell a urine-like odor on the breath and notice a yellow-gray cast to the skin. If the patient is producing any urine at all, it may be dilute, with casts or crystals present. The skin is fragile and dry, and there may be uremic frost on the skin or open areas owing to severe scratching (pruritus) by the patient. The patient may have bruising; petechiae; brittle nails; dry, brittle hair; gum ulcerations; or bleeding. If the patient has been followed for CRF, there may already be access sites created in preparation for dialysis. Assess the sites for patency (an arteriovenous fistula should have a palpable thrill and audible bruit) and signs of infection. When you assess the CNS, you may find that the patient has difficulty with ambulation because of altered motor function, gait abnormalities, bone and joint pain, and peripheral neuropathy. The patients mental status may range from mild behavioral changes to profound loss of consciousness and seizures. Electrolyte imbalances may result in signs of hypocalcemia muscle cramps, and twitching. What to Expect in the DIAGNOSTIC PROCEDURES Test Normal Result Abnormality Blood urea 5-20 mg/dL Elevated nitrogen Serum Creatinine 0.5-1.1 mg/dL Elevated
Explanation Kidneys cannot excrete wastes Kidneys cannot excrete wastes 24-hr urine F- 85-125 ml/min < 95 % decrease Acute damage to kidneys creatinine M- 95-135 ml/min limits ability to clear creatinine Other tests: Urinalysis, Complete blood count; x-ray of kidney, ureter, bladder; blood urea nitrogen; creatinine; renal ultrasound; serum levels of Na, Mg, K, ABG PRIMARY NURSING DIAGNOSIS Fluid volume excess related to compromised regulatory mechanisms PLANNING AND IMPLEMENTATION Collaborative Patients who have progressed to ESRD require either dialysis or renal transplantation. Other procedures, such as venovenodialysis, are also used in some institutions.
Surgical interventions for the patient with CRF consist of creating peritoneal or vascular access for dialysis or renal transplantation. The diet for the CRF patient is generally restricted in fluids, protein, sodium, and potassium. It is usually high in calories, particularly carbohydrates. The fluid restriction is generally the amount of the previous days urine plus 500 to 600 mL. Medication Dosage Description Rationale Antihypertensives Varies by drug ACEinhibitors, BetaTreat the underlying adrenergic antagaonists hypertension Diuretics Varies by drug Loop and thiazide Control fluid overloadearly in diuretics the disease if the patient is not anuric Sodium 352-650 mEq/L PO tid Alkalinizing agent Supplements sodium bicarbonate bicarbonate when serum level falls below 18-20 mEq/L KayexalateOrally or enema; 15 0.5-1.0 mEq/L of K is Ecahnges sodium for Sodium g/60 mL in 20-100 mL removed with each potassium in the GIT, polystyrene sorbitol to facilitate enema but an leading to the elimination of sulfonate passage of resin thru equivalent NA is potassium the intestinal tract retained INDEPENDENT To help the patient deal with fluid restrictions, use creative strategies to increase the patients comfor t and compliance. Use ice chips, frozen lemon swabs, hard candy, and diversionary activities. Give medications with meals or with minimal fluids to maximize the amount of fluid that is available for patient use. Skin care is important because of the effects of uremia. Uremia results in itching and dryness of the skin. If the patient experiences pruritus, help the patient clip the fingernails short and keep the nail tips smooth. Teach the patient to use skin emollients liberally, to avoid harsh soaps, and to bathe only when necessary. You may need to speak to the physician to request an as-needed dose of an oral antihistamine such as diphenhydramine(Benadryl). If the patient is hospitalized, frequent turning and range-of-motion exercises assist in preventing skin breakdown. If the patient is taking medications that cause frequent stools, teach the patient to clean the perineum and buttocks frequently to maintain skin integrity. The patient needs to plan the weeks activities to incorporate the level of fatigue, the dialysis routine, and any desired activities. Counseling relative to role function, family processes, and changes in body image is important. Sexuality counselling may be required. Reassure the patient that adaptation to a chronic illness with an uncertain future is not easy for either the patient or the significant others. Participate when asked in discussions related to feasibility of home dialysis, placement on the transplant list, and decisions related to acceptance or refusal of dialysis treatment. Encourage decisions that increase feelings of control for the patient. If the patient undergoes a renal transplantation, provide preoperative and postoperative care as for any patient with abdominal surgery. Monitoring of fluids is more important for these patients than for other surgical patients because a decrease in output may be an early sign of rejection. Other signs include weight gain, edema, fever, pain over the site, hypertension, and increased white blood cell count. Emotional support is important for the patient and family, both preoperatively and postoperatively, because both positive and negative outcomes produce emotional turmoil. BLADDER CANCER ASSESSMENT What to ask during HISTORY taking. Gross, painless, intermittent hematuria is the most frequently reported symptom. Occult blood may be discovered during a routine urinalysis. Dysuria and urinary frequency are also reported. Burning and pain with urination are present only if there is infection. Other symptoms may include suprapubic pain after voiding, bladder irritability, dribbling, and nocturia. What to do during PHYSICAL EXAMINATION. The physical examination is usually normal. A bladder tumor becomes palpable only after extensive invasion into surrounding structures. PRIMARY NURSING DIAGNOSIS Risk for altered urinary elimination related to the obstruction of urinary flow
PLANNING AND IMPLEMENTATION Collaborative Patients with higher-stage invasive disease are usually treated with radical curative surgery, whereas patients with lower-stage noninvasive disease can be controlled with more conservative measures. Papillary tumors, even when noninvasive, have a high rate of recurrence. CONSERVATIVE. Superficial bladder tumors can be treated effectively with conservative measures that consist of surgical removal of the tumor by transurethral resection of the bladder (TURB) followed by electrical destruction or fulguration, intravesical instillation of chemotherapy or immunotherapy, and frequent follow-up cystoscopic examination. Superficial bladder tumors can also be destroyed with the neodymium:yttrium-aluminum-garnet (Nd:YAG) laser. Patients with multiple superficial bladder tumors receive intravesical instillation of chemotherapy and immunotherapy such as bacillus Calmette-Gurin (BCG) vaccine. This vaccine is made from a strain of Mycobacterium bovis, and helps to prevent a relapse. SURGICAL. Partial or segmental cystectomy may be recommended for patients with diffuse unresectable tumors or tumors that fail to respond to intravesical therapy. Because tumors are likely to continue to spread and metastasize to distant sites, procedures such as radical cystectomy with creation of a urinary diversion, external radiation therapy, or a combination of preoperative radiation therapy followed by radical cystectomy and urinary diversion are recommended. POSTOPERATIVE. Postoperatively, direct nursing care toward providing comfort, preventing complications from major abdominal surgery, and promoting urinary drainage. Monitor the patients vital signs, dressings, and drains for symptoms of hemorrhage and infection. Monitor the color of the stoma, as well as the amount and color of the urine in the collection pouch, every 4 hours. RADIATION. External beam radiation therapy can be used as both adjuvant and definite treatment for bladder cancer. Radiation therapy with a curative intent may be a treatment option for patients who are opposed to a cystectomy and urinary diversion. Independent For patients who require radical cystectomy with urinary diversion, offer support and reinforcement of the information. Be sure what to expect. Involve another family member in the preoperative education. If it is needed, arrange a preoperative visit by someone who has adjusted well to a similar diversion.
Вам также может понравиться
- Nasogastric Tube Insertion, Feeding and RemovalДокумент13 страницNasogastric Tube Insertion, Feeding and RemovalJacqueline de Asis100% (2)
- PositioningДокумент10 страницPositioningJacqueline de AsisОценок пока нет
- Exercises: Click To Edit Master Subtitle StyleДокумент9 страницExercises: Click To Edit Master Subtitle StyleJacqueline de AsisОценок пока нет
- Exercises: Click To Edit Master Subtitle StyleДокумент9 страницExercises: Click To Edit Master Subtitle StyleJacqueline de AsisОценок пока нет
- In Behalf On My Wife and IДокумент1 страницаIn Behalf On My Wife and IJacqueline de AsisОценок пока нет
- Exercises: Click To Edit Master Subtitle StyleДокумент9 страницExercises: Click To Edit Master Subtitle StyleJacqueline de AsisОценок пока нет
- Exercises: Click To Edit Master Subtitle StyleДокумент9 страницExercises: Click To Edit Master Subtitle StyleJacqueline de AsisОценок пока нет
- Intake and Output MonitoringДокумент12 страницIntake and Output MonitoringJacqueline de Asis100% (2)
- Acute Resp FailureДокумент30 страницAcute Resp FailuresridharОценок пока нет
- Exercises: Click To Edit Master Subtitle StyleДокумент9 страницExercises: Click To Edit Master Subtitle StyleJacqueline de AsisОценок пока нет
- PositioningДокумент10 страницPositioningJacqueline de AsisОценок пока нет
- IO SheetДокумент2 страницыIO SheetJacqueline de AsisОценок пока нет
- Arf, CRF, BCДокумент5 страницArf, CRF, BCJacqueline de AsisОценок пока нет
- Exercises: Click To Edit Master Subtitle StyleДокумент9 страницExercises: Click To Edit Master Subtitle StyleJacqueline de AsisОценок пока нет
- Anxiety DisordersДокумент1 страницаAnxiety DisordersJacqueline de AsisОценок пока нет
- Arf, CRF, BCДокумент5 страницArf, CRF, BCJacqueline de AsisОценок пока нет
- Bladder CancerДокумент35 страницBladder CancerHealth Education Library for PeopleОценок пока нет
- Vital SignsДокумент32 страницыVital SignsJacqueline de AsisОценок пока нет
- Neuro Ana and PhysioДокумент2 страницыNeuro Ana and PhysioJacqueline de AsisОценок пока нет
- 6th Central Pay Commission Salary CalculatorДокумент15 страниц6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Living With LossДокумент26 страницLiving With LossJacqueline de AsisОценок пока нет
- Mood DisordersДокумент36 страницMood DisordersJacqueline de AsisОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- 4 Patpka#-Yvxv, : Circuit-Breaker IZMДокумент42 страницы4 Patpka#-Yvxv, : Circuit-Breaker IZMJames IzquierdoОценок пока нет
- MIP17 - HSE - PP - 001 Environment Management Plan (EMP) 2021 REV 3Документ40 страницMIP17 - HSE - PP - 001 Environment Management Plan (EMP) 2021 REV 3AmeerHamzaWarraichОценок пока нет
- InterbarkadaДокумент8 страницInterbarkadaJay Vincent DiamanteОценок пока нет
- Korean Vocabulary ListttДокумент31 страницаKorean Vocabulary ListttAireeneMhaePanenОценок пока нет
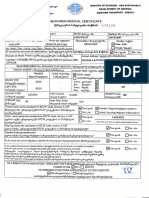
- Seafarer Medical CertificateДокумент2 страницыSeafarer Medical CertificateKoki ToОценок пока нет
- Kera Ritual Menu - With DensifiqueДокумент8 страницKera Ritual Menu - With Densifiquee.K.e.kОценок пока нет
- 1823 - Part - A - DCHB - Kamrup Metropolitan PDFДокумент224 страницы1823 - Part - A - DCHB - Kamrup Metropolitan PDFSaddam FaruqueОценок пока нет
- Sharon Jones Amended ComplaintДокумент35 страницSharon Jones Amended ComplaintMichael_Lee_RobertsОценок пока нет
- FAO-JECFA Monographs Vol 10Документ154 страницыFAO-JECFA Monographs Vol 10Vu Thi Phuong Thuy - QAОценок пока нет
- KMC3063 - Unit 3 - Bowenian Family TherapyДокумент38 страницKMC3063 - Unit 3 - Bowenian Family TherapyJane Rabi TinkaiОценок пока нет
- ADHERENCE and INVASION ASSAYS A092Документ2 страницыADHERENCE and INVASION ASSAYS A092Samrah Anwar0% (2)
- Basic Maternity ConceptsДокумент14 страницBasic Maternity ConceptsDivine Grace Arreglo AbingОценок пока нет
- The Superheroes of PharmaДокумент13 страницThe Superheroes of PharmaMPAОценок пока нет
- Smartphones and Sleep - MediaДокумент2 страницыSmartphones and Sleep - Mediaivan7tatОценок пока нет
- GayДокумент15 страницGayjulyerwanni100% (2)
- Guide To Clinical Audit Antibiotic Use in Urinary Tract InfectionДокумент10 страницGuide To Clinical Audit Antibiotic Use in Urinary Tract Infectionihtisham1Оценок пока нет
- Dosage and SolutionsДокумент3 страницыDosage and SolutionsNicole PageОценок пока нет
- 07 RPM Chapter Feb 2021 V9 508 Clean FinalДокумент143 страницы07 RPM Chapter Feb 2021 V9 508 Clean FinalShubhamОценок пока нет
- Microbiome Labs Total Gut RestorationДокумент2 страницыMicrobiome Labs Total Gut RestorationKrishna DasОценок пока нет
- AsthmaДокумент10 страницAsthmaAcohCChaoОценок пока нет
- Karyotype WorksheetДокумент4 страницыKaryotype WorksheetKellieM.8406Оценок пока нет
- Albumin CPДокумент4 страницыAlbumin CPLAB. GATOT SUBROTOОценок пока нет
- Biology Questions CholeraДокумент12 страницBiology Questions CholeraLucas100% (1)
- Week 3 PATIENTS RIGHTS AND RESPONSIBILITIES 19-20Документ32 страницыWeek 3 PATIENTS RIGHTS AND RESPONSIBILITIES 19-20maha abdallahОценок пока нет
- IntralipidДокумент3 страницыIntralipidGwyn RosalesОценок пока нет
- New Form 6 Leave Form TEACHERSДокумент2 страницыNew Form 6 Leave Form TEACHERSmarites mercedОценок пока нет
- Branchial Cleft CystДокумент4 страницыBranchial Cleft CystCharmila SariОценок пока нет
- Waste ManagementДокумент34 страницыWaste ManagementSivaRamanОценок пока нет
- Innovative Ideas To Reduce Post Covid DifficultiesДокумент5 страницInnovative Ideas To Reduce Post Covid DifficultiesBrindhaОценок пока нет
- Network Hospital Grading Proforma: General InformationДокумент6 страницNetwork Hospital Grading Proforma: General InformationSanket SahareОценок пока нет