Академический Документы
Профессиональный Документы
Культура Документы
Compilation For Med Comprehensive Quiz
Загружено:
Mheg AnОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Compilation For Med Comprehensive Quiz
Загружено:
Mheg AnАвторское право:
Доступные форматы
Compilation for Med Comprehensive Quiz Dr.
Peralta Name Age Birthday Religion Sex Race Marital status Occupation Address Referring physician Date and number of admissions Informant Percentage reliability Dr. Peralta: Inspection = most important Percussion = least important because of remote Remote diagnosis = patient and physician are separated = using laboratory procedures Mc Donalds Triad = predictor for serial killer 1. Bed wetting/ enuresis 2. Cruelty to animals 3. Arson/fire setting o o PEUTZ JEGHERS SYNDROME HEREDITARY INTESTINAL POLYPOSIS SYNDROME Hamartomatous polyps in GIT MOTIVATION GETS YOU GOING, BUT HABIT GETS YOU THERE! - Zig Ziglar THREE PROCESSES IN THE STUDY OF THE PATIENT THE CLINICAL PROCESS THE INTELLECTUAL PROCESS THE DIAGNOSTIC PROCESS THE CLINICAL PROCESS THE STUDY OF THE PATIENT IT IS PHYSICAL DIAGNOSIS COMPOSED OF THREE PHASES: FIRST PHASE DATA COLLECTION & RECORDING PATIENT HISTORY TAKING PERFORMANCE OF PHYSICAL EXAMINATION SYSTEMATIC RECORDING OF DATA SECOND PHASE ANALYSIS OF DATA SYNTHESIS OF DIAGNOSIS FORMULATION OFPROGNOSIS THIRD PHASE
MANAGEMENT AND THERAPY OF THE DISEASE /DIAGNOSIS
Medical History A good clinician is a good Observer done during interview with the patient Communicator patient should understand you Listener Historian Attributes Of A Sign Or Symptom 1. Onset - To know the duration then classify as acute or chronic - Formulation of impressions 2. Precipitating or Aggravating Factors - Provoking factors - Palliative - -----relieving factor - Example: dysuria: sex, fluid intake; withholding urination 3. Quality - Character - What is it like? - Example: pain: squeezing, dull, burning, compressing, sharp, splitting, boring , throbbing - How about LBM? Watery, brownish, with mucus, foul smelling (fishy, fruity) 4. Quantity - Volume to be measured by cc or mL - To know the extent of injury (e.g. LBM) - Avoid using teaspoonful or basinful or cupful or handful - E.g. phlegm: volume (per expectoration), color (greenish, whitish, brownish) - E.g. Diarrhea: 10x for the past 2 hours; volume is 500 cc 5. Radiation Regarding pain or murmur; from one area or location to another Eg. Chest pain radiating to axilla/shoulder 6. Severity How bad is it? Ask for a rating on a scale of 1 10 (10 being most severe) 7. Timing Frequency ( every hour, every after meals) In terms of what time of the day or night 8. Location Localize Where exactly in terms of anatomical location or landmark o Gyne History Had pap smears Any history of gynaecological diseases OB history Give scoring: GP (TPAL) = G (Gravida): number of pregnancies
THE INTELLECTUAL PROCESS SIX LEVELS OF INTELLECTUAL FUNCTIONING: 1. KNOWLEDGE 2. COMPREHENSION 3. APPLICATION 4. ANALYSIS 5. SYNTHESIS 6. EVALUATION > THE DIAGNOSTIC PROCESS THE TECHNIQUE TO MAKING A DIAGNOSIS BY NEWTON S. STERN (HANDOUT) DATA COLLECTION PITFALLS 1. OMISSION OF IMPORTANT QUESTIONS 2. OMISSION OF PERTINENT NEGATIVES 3. FAILURE TO ELICIT TEMPORAL RELATIONSHIPS 4. FAILURE TO FOLLOW UP IMPORTANT LEADS STRUCTURE PITFALLS: 1. BEGINNING TOO FAST & NOT PUTTING HE PATIENT AT EASE 2. ALLOWING PATIENT TO RAMBLE 3. NEEDLESS REPETITIONS OF QUESTIONS & FORGETING ANSWERS 4. POOR TRANSITIONS, HOPPING FROM ONE TOPIC TO ANOTHER 5. COVERING SENSITIVE TOPICS OR DELICATE AREAS TOO EARLY VALIDATION OF DATA: 1. USING TECHNICAL TERMS NOT UNDERSTOOD BY PATIENT 2. NOT ALLOWING PATIENT TO FINISH HIS ANSWERS 3. 4. SWAMPING PATIENT WITH TOO MANY QUESTIONS FAILING TO FIND OUT PXS INTERPRETATION OF SYMPTOMS
PHYSICIANS ATTITUDE: 1. ACTING TOO FRIENDLY OR NOT FRIENDLY ENOUGH 2. ACTING PRE-OCCUPIED & NOT LISTENING 3. NOT ENOUGH EYE CONTACT 4. NOT ENOUGH INTEREST IN EMOTIONAL FACTORS 5. TOO MUCH INTEREST IN EMOTIONAL FACTORS IDENTIFYING DATA (14) o NAME, AGE, BIRTHDAY, RELIGION o SEX, RACE(white, black, yellow, brown) o MARITAL STATUS, OCCUPATION, ADDRESS, REFERRING PHYSICIAN, DATE & NUMBER OF ADMISSIONS, INFORMANT, % RELIABILITY Dr. Tolentino:
= P(Para): number of pregnancies that passed the age of viability (24 weeks AOG) = T (Term) = P (Preterm) = A (Abortion) = L (Living) Record pregnancies, deliveries and results Family planning acceptor? What? How many sexual partner and the last sexual intercourse Major sources of inaccurate observation 1. Oversight a. Overlooking b. Failure c. Mistake **the key to a thorough and accurate physical examination is developing a systematic sequence of examination 2. Forgetfulness a. Carelessness b. Inattentiveness **admit the patient ASAP in the ER or discharge the patient in the OPD **jot down important data on your notes 3. Bias a. Propensity for some fixed thing b. Secondary to preconceived notions Dealing with patients who are: o Silent or unconscious or comatose a. Cant get history unless the one who brought the patient knows the history b. Silent patient psyche patient, deaf and mute o Talkative o Anxious a. Limited information o Crying a. Let them cry o Confusing o Angry or disruptive o Poor historian Dealing with patients who are o With language barrier o With reading problems visual problem; illiterate o With impaired hearing o With limited intellect o With personal problems Ideal Examining Room: o Natural light is preferable Physical Examination: Maneuvers: Fundamental procedures 1. Inspection: Seeing eyes 2. Palpation: feeling hand fingers and palm 3. Percussion: tapping fingers
4.
Auscultation: hearing ears Smelling nose
1. INSPECTION - First procedure in PE - Sense of sight is used - Least mechanical Often or frequently slighted or not given too much importance - Yield most physical signs among the 4 manuevers - Hardest or most difficult to learn 2. Palpation: - Tool is Hand Sensitive Parts of the Hand 1. Tactile sense - Tips of fingers most sensitive to fine tactile 2. Temperature sense - Dorsum of the hand or fingers - Skin is thinner; more blood supply compared to palm 3. Vibratory sense - Use palmar aspect 4. Sense of position and consistency - Use grasping fingers Types of Fever 1. Continuous Fever o Slight fluctuation 2. Remittent Fever o Marked Fluctuation 3. Intermittent o Fever in the morning afternoon normal then morning fever again for 24 hours 4. Relapsing Fever o Takes days before you have fever again o Days of fever and days of normal Grades of fever Normal: 36.5 C ---- 37 C Low: 37.1 C 38.4 C Moderate; 38.5 C 39 C High: 39.1 C 40 C Hyperpyrexia: > 40 C Subnormal: 36.4 C and below Centigrade to Fahrenheit C x 9/5 + 32 Fahrenheit to Centigrade F 32 X 5/9 Types of Breathing a) inspiratory dyspnea Stridulous breathing there is an accompanying crowing sound or stridor 1. Stertorous or noisy breathing\ Due to vibration of the soft palate Usual cause of snoring
2. 3. 4. 5. 6. 7. -
Rattling and gurgling sound produced by passage of air through the secretions that accumulate in trachea and larger bronchi Commonly called death rattle Hyperpnea Increase in depth of respiration Hyperventilation Increase in depth and rate of respiration Meningitic or irregular respiration Gross irregularity or rate rhythm and depth or respiration Seen in meningitis or other CNS diseases Hippocratic Respiration Described as fish mouthing Cheyne-Stokes Breathing Periods of deep breathing (Hyperpnea) alternate with periods of apnea Children and aging people Heart failure Uremia Drug induced respiratory depression o Opioids ex) morphine Brain Damage Biots Respiration Also called ataxic breathing
Hamwis Formula Female: 5 feet = 100 lbs + 5 lbs. for every inch excess of 5 feet Male: 5 feet = 106 lbs. + 6 lbs. for every inch excess of 5 feet Tannhauser Formula Height in cm 100 o Minus 10% for both male and female = ideal body weight in kg BMI >25 = overweight BMI > 30 = obese BMI > 19 but <25 = healthy weight BLOOD PRESSURE: - Palpatory first inorder to avoid missing the AUSCULTATORY GAP period of silence between the systolic and diastolic pressure JNC VII Classification
Systolic Normal preHPN Stage 1 Stage 2 <120 120-139 140-159 >/= 160
Diastolic <80 80-89 90-99 >/= 100
Pulse Pressure - Difference between systolic and diastolic pressure - Normal 30-40 mmHg Widened Pulse Pressure HPN atherosclerosis of the aorta Aortic regurgitation Thyrotoxicosis PDA Arteriovenous fistula Beri-beri heart Coarctation of the aorta Emotional states Fever and vigorous exercise Narrowed Pulse Pressure Tachycardia Severe aortic stenosis Constrictive pericarditis Pericardial effusion Ascites Heart failure
Patients Profile 1. To summarize the patients life 2. To get some idea of his present position in his environment 3. To discover what stimuli in his environment may be contributing to his disease a. Life history o Manner of birth and birthplace o Position in the family o Socio-economic status of the family o Changes in residence o Education and jobs held b. o o c. o o o o d. o Marital Status (if married) Compatibility Adjustment Occupation Nature of present and previous work Adjustment to working situation Interpersonal relationship Presence of occupational hazards
Complete Problem List - Terminology or a way in which a problem is stated will vary according to: i. Quality and quantity of information collected ii. Experience and ability of the physician - Temporary Problem persists - Active Problem - Subtitle: = More common in OB and Surgery Ex. #1. Hypogastric pain (Date) #2. S/P NSVD 1) vaginal bleeding 2) episiorrhapy Types: - 1. Resolved - 2. Redefined - 3. Combined with other Problems - 4. Inactivated - 5. Left Open DM, HPN III. Initial Plan a. 1. Diagnostics (Dx) i. Listed here are the rule outs ii. Priority of rule outs Ex. Summary of Subjective and Objective Impression: Differential Dx; to r/o; Dx - CXR b. 2. Therapeutics (Tx) 1. Plans for specific drug/s or therapy including exact dosage 2. Parameter to be followed in order to determine response to therapy 3. Plans for discovering or monitoring side effects of therapy c. 3. Patients Education (PE) i. What the patient and or his family have been told about the problem ii. Shows the grasp of the physician in the case d. Physicians Order A. Routine orders 1. Patients condition 2. Activity 3. Diet 4. General Medications 5. Vital Signs B. POMR orders 6. Per proble IV. Follow-up notes/Progress notes A. Narrative Progress Notes S: Subjective described by the patient
Finances Whether the patients financial status maybe contributing to his present illness o Whether his illness will impose financial burden or difficulty in him o o Personality Type Reaction to environment
Mean Arterial Pressure (MAP) CO x SVR + CVP 2 x Diastolic Pressure + Systolic Pressure 3 Diastolic Pressure + Pulse Pressure 3 Problem-Oriented Medical Information System (PROMIS) Matching Type o A. POMR o B. Audit of the Record o C. Educational Program A.) POMR 1. Defined Data Base 2. Problem List 3. Iniitial Plan 4. Follow-up notes/Progress notes Defined Data Base Before a data base is collected you must state exactly each piece of information you will seek - Defined data base: A. Problem specific data base B. Comprehensive data base o Parts: A. Patient Profile B. History C. PE D. Laboratory I. o
e.
f.
Habits o Regularity of eating and sleeping o Exercise o Use of tobacco or cigarette o Drugs taken regularly Religion o Affiliation and attitude towards religion
g.
II. Complete Problem List - Categories: 1. Anatomic defects, fracture femur right, imperforate anus, hymen, Tetralogy of Falot 2. Physiologic - arrhythmia, HPN, Jaundice 3. Symptom or sign 4. Etiologic 5. Demographic 6. Social - financial difficulty 7. Psychiatric 8. Allergies 9. Risk factors smoking, alcoholism, obesity 10. Operations 11. Proven Diagnosis histopath results, x-rays 12. Abnormal laboratory findings executive check-up
O: Objective PE or lab finding A: Assessment Interpretation of S & O data P: Plan measure to undertake *Stable patient: at least 1 SOAP for the day * Rapidly progressing: more than 1 SOAP *basis for demerit C. Summary Statements - Discharge summary - SOCP format S- subjective - Significant historical and symptomatic information prior to and during hospital course O- objective - Significant physical and lab findings C- course of confinement - Discussion of relevant lab, changing PE, therapy and response P- plan - Clinical Abstract - Death Summary Dr. Lagdao: Eyes, Ears, neck HEAD the most complaint in head is HEADACHE Facies: Lionine fascies of Leprosy Facies for nephritic patient - Periorbital edema in children with nephritic syndrome Eyes: Complaint: Iridescent vision = corneal edema = halos around light Diplopia = chronic otitis media temporal lobe abscess Headache Error of Refraction (EOR) no headache Epiphora- (+) blockade in the drainage of tears or nasolacrimal duct B. Flow Sheet
Rinnes test Bings test Webers test Drawing: lymph nodes Retina o DM vs Hypertension o Retinopathy Grading HTR Hemorrhages
Tyndall effect Diascopy o Red or purple purpuric lesions o Erythema Shape of individual lesions Arrangement of multiple lesions Serious skin signs in sick patients
- deMussets sign - Head bobbing aortic insufficiency - Stellwags sign - Blank stare of a Hyperthyroidism - Macular star Hypertension - Hair loss/parasites Scalp & hair disorders o Alopecia small part Stress Abnormal secretions B. Lacrimation- with stimulation overproduction of tears C. Epiphora- (+) blockade in the drainage of tears or nasolacrimal duct Dr. Lagdao
Dr. Kishi-Generao Stratum corneum is thicker Number and size of melanosomes determines skin color Melanocytes in dark skin synthesize larger melanosomes than those produced in light skin Larger melanosomes are also produced with chronic sun exposure Vitiligo Langerhans cell o Langehans cell histiocytosis Adnexa: Eccrine Sweat Unit o Most abundant on the palms, soles, forehead and axilla o Cholinergic innervations Apocrine Sweat unit o Serves no known function in humans Sebaceous glands o Outgrowth from the upper portion of the hair follicle o At all skin sites except palms and soles Phases of scalp hair growth Hair follicles o Black person big melanosomes o White person smaller melanosomes o Red hair round melanosomes o White hair decreased melanocytes Nails o Injury in the nail 3-6 months needed to have a new nail o Cuticle is the most important part o Terrys nails Obstructive etiology in the lungs Vasculature of the skin o Hemangioma At birth regress spontaneously without melanoma o Vascular malformation will not be removed Nerves of the skin o Meissner corpuscles touch and pressure o Vater-Pacini corpuscles Pressure Subcutaneous tissue o Lipoatrophy HIV Description of lesions
Dr. Abiog Numerical pain rating scale Visual pain rating scale Causes of Edema Chief complaint - table Manual muscle testing Scoliosis instruments Gait and posture Abnormalities of gait and posture Acute arterial occlusive disorder o Six Ps of sudden arterial occlusion Ankle brachial index o normal values osteogenesis imperfecta painful shoulders colles fracture smiths fracture paronychia felon ganglion cyst upper limb disorders o wrist and hand test for lateral epicondylitis o cozens sign test for de Quervains tenosynovitis o finkelsteins test test for medial epicondylitis o resistive test ape hand deformity in median nerve lesion papal benedictian sign or bishops hand deformity grading of MSR clinical evaluation of the limb and spine cornerstone of all clinical impressions: basis for all diagnoses and treatment history taking functional history chief complaint o primary reason o expressed in patients own words o conveys more than disease symptomatology o implied disability o handicap and subsequent loss associated with clinical symptoms analyzing the pain o muscle cramping, dull, aching, stiffening o bone dull, deep, boring, nagging o fracture sharp, severe, intolerable o joint myriads of adjectives
swelling o o o o
character paresthesia weakness peripheral vascular disease o pain in caves after walking several blocks functional history body mass index ideal body weight 3 degrees of undernutrition WHO classification of obesity Updated Asia-Pacific Classification of obesity Waist hip ratio o Normal values o 0.7 women Optimal levels of estrogen o 0.9 men Auscultation and percussion play a minor role Inspection most basic of all procedures Table of WHR Deformity evaluation and documentation o Almost all topics o Scoliosis o Kyphosis o Hyperlordosis o Spondylolisthesis Forward slipping o Gibbus deformity Congenital kyphosis o Retrolithiasis Polio Varus and valgus Limb deficiencies o Phocomelia o Polydactyly Physical examination and possible causes - table o CREST syndrome o SQ Apparent and true lib length Goniometry Movement of muscle and nerves Manual muscle testing table Gait analysis table Posture Common sites for monitoring pulses Diagnosis of peripheral vascular diseases o Chronic insufficiency of arteries and veins Examination of the spine Back pain Neck pain with HA and vertigo Taut band Suboccipital triangle syndrome
duration soft flunctuant, warm, acute chronic leathery thickening timing of appearance after injury
Erbs palsy Klumpkes palsy Scoliosis o Structura o Nonstructural Lower limb disorders Ankylosing spondylitis
Dr. Revilla Anatomical landmarks Circumference of the chest Lungs o Lobes o Size o Anatomy o Fissures Cough and fever o Smoking in HPI General data Symptoms of respiratory system Dyspnea o Bronchitis o Pneumonia o COPD o Pneumoconiosis o Anaphylactic shock o Malignancy o pneumothorax Chest pain o Muscles most common Hemoptysis 5As of Tobacco cessation Table on cough and cold Smoking Bronchial asthma Post nasal drip syndrome Acute pulmonary embolism Pleuritic pain Restrictive lung disease Hyperpnea Kussmauls breathing Bradypnea Inspection o Barrel chest o Flail chest Palpation o Tactile fremitus o Consolidation Percussion o Plexor o Pleximeter o Sounds different organs o One of the most important techniques in PE Auscultation
Most important examination technique for assessing air flow through the tracheobronchial tree o Pathologic example Table summary Bronchophony Egophony Whispered petroliloquy Deformities of the thorax Airless lungs lobar Pneumonia Wheezes and rhonchi Stridor Palpable masses of the breast SMR or Tanner staging of the breast Breast mass lesions Breast o Lymphatics Major Lymphatic drainage Pectoral nodes Multiple choice o Clinical Brest Self Exam and Mammography Schedule of check up? True or false yata Most common pattern of palpating o Common Breast Masses Yung table Matching type o Viable signs of Breast Cancer Table ulit Matching type o Tanner Sexual Maturity Staging Matching type Chest o Characteristics of breath sounds Matching type o Percussion notes and their characteristics Matching type o Physical Findings in Selected Chest Disorders Cases o Hemoptysis Massive hemoptysis and Nonmassive hemoptysis Multiple choice o Heart Sounds S1/S2: closure of ___ o Reverse paradoxic splitting o Wide fixed splitting Seen in ASD o Pericardial knock Hallmark of constrictive pericarditis Dr. Olarte Down syndrome o
Most common heart defect: di ko sure yung sagot Sa isang hand-out: VSD Dun sa ida: ASD or endocardial cushion defect Turners syndrome o Most common heart defect: Aortic coarctation De Mussets sign o Aortic regurgitation o
2nd Semester Prelims Period Dr. Irmscher Arterial Pressure Control System o Chemoreceptor reflex responds to hydrogen ion and carbon dioxide o CNS ischemic response most potent Methods of BP measurement o Sphygmomanometer and Methods A > B type of exam o Korotkoff sounds Phases Hypertension o JNC 7 Yung table Ankle Brachial Index o Normal level Temperature Pulse dissociation o Typhoid Jugular Pressure and Pulses o Abnormalities kung sang sakit nakikita A wave X descent V wave D wave H wave Dr. Tolentino Peripheral Vascular Disorders 10 Ps o Pain o Pallor o Poikilothermia o Pitting edema o Paresthesia o Paralysis o Pulselessness o Peripheral ulcers o o Lymphedema o Meiges disease Lymphedema praecox o Milroys disease congenital Tests for Competence in Great Saphenous Veins o Perthes test Essay o Ochsner-Mahorner Thrombophlebitis o Phlegmasia alba dolens
o Phlegmasia cerulean dolens DVT: Early Physical signs - Identification o Pratts sign o Louvels sign o Bancrofts sign and Moses sign o Lowenbergs sign o Ramirezs sign o Liskers sign o Homans sign Diseases of the arteries Erythromelalgia Raynauds disease o 3 stages Prehyperemic Hyperemic Posthyperemic Aneurysm o Signs of aneurysm Dr. Tolentino What do you need for a good abdominal examination o Enumeration 9 items Sitophobia: fear of eating because of subsequent or associated abdominal discomfort o Identification Symptoms of Abdominal problems o Matching type Contour of Abdomen o Scaphoid, flat, distended o Enumeration Pseudocyesis o Identification Sister Mary Joseph nodules o Identification o May be the only sign of metastizing intraabdominal malignancy Cullens and Grey-Turner sign o Enumeration: signs of hemorrhagic pancreatitis Bowel sounds: Transition time of stool o 18-150 hours? Fibrillary Hum o Secondary to muscle contraction o Identification Blumberg sign, Markle sign, Rovsings sign o Identification Palpation of a ticklish abdomen o How essay yata Palpation of the Spleen: Middletons method o Essay Virchows node o Other names: enumeration Puddle sign o Essay
Dr. Olarte First heart sound closure of the mitral valve Mitral closure precedes tricuspid closure Varied intensity of S1 Atrial fibrillation regular irregularity of the heart beat Atrial flutter with varying degrees of block Complete AV bock no relationship of LV contraction and RA/LA contraction Ventricular tachycardia Closure of the aortic valve - A2 Wide fixed splitting ASD Extra diastolic heart sound o Third heart sound or S3 Congestive heart failure Advanced mitral or tricuspid regurgitation o Fourth heart sound Stiff ventricle Ventricular hypertrophy Pulmonic or aortic stenosis Summation gallop Tachycardia Diastole S3 and S4 coalesce Quadruple rhythm Pericardial knock Constrictive pericarditis o Extrasystolic heart sounds Classification Vascular dilatation of the pulmonary aorta Valvular deformed and rapidly asxending aortic or pulmonary valve reaches its elastic limit Midsytolic click Mitral or tricuspid valve prolapsed o Extradiastolic heart sounds MS due to RHD Extracardiac systolic and diastolic heart sounds o Pericardial friction rub High pitched Entire cardiac cycle Infectious pericarditis Murmur o Location Aortic area 2-3rd RICS PSL Pulmonic 2-3 LICS PSL
Tricuspid lower left sterna border
Aortic stenosis o Radiate into the carotid arteries bilaterally o Narrow pulse pressure o High frequency murmur o Radiate towards the neck Pulmonic stenosis o Transmitted towards the neck or left shoulder Pansystolic or holosystolic murmurs o Mitral regurgitation o Tricuspid regurgitation o Ventricular septal defect Mitral regurgitation o High pitched and blowing o Radiates toward the left axilla Tricuspid regurgitation o High pitched and blowing Carvallo sign o Intensity of murmur increases with inspiration Aortic regurgitation o High pitched blowing murmur o DeMussets sign Head bobbing with each heart beat o Ewarts sign Pericardial effusion Same findings o Austin Flint Low pitched Severe AR Pulmonic regurgitation o Graham Steel murmur Pulmonary hypertension Mitral stenosis o Low pitched and rumbling Differential diagnosis of continuous thoracic murmurs o Cervical venous hum Disappears on compression of jugular vein 2ndsem Prelims quiz 1 Arterial Pulse or Pressure Dr. Irmscher Arterial Pulse or Pressure A measurement of the function of the left side of the heart Factors which determine: 1. Cardiac output 2. Total Peripheral vascular resistance
Determinants of Cardiac output and Total peripheral resistance 1. Total blood volume affects CO 2. Viscosity of blood affects TPR 3. Compliance of artery affects TPR Pacemaker of the Heart SA node gives the impulse or automaticity 1. Arterial Pressure Control System Baroreceptor reflex Found in the: o Arch of the aorta o Carotid sinus Respond to stretching Most immediate Carotid massage of external carotid artery pulse will decrease or slow down Chemoreceptor reflex Carotid bodies Respond to chemicals such as hydrogen ion and carbon dioxide CNS ischemic response Most potent stimulate SNS activity to overcome decrease in blood pressure
Direct -
Methods of BP measurement Insert a needle in a blood vessel in getting direct pressure
2.
Indirect Made by Korotkoff Noninvasive Sphygmomanometer o Mercury more acceptable in documenting blood pressure o Aneroid o Digital METHODS o Palpatory systolic pressure is usually taken o Auscultatory get both systolic and diastolic pressure o Oscillometric Mechanical aneroid meter BP =CO x TPR CO is measured using systolic blood pressure Depends on the stiffness of the blood vessel o If blood vessel is stiff it results in elevated diastolic blood pressure Indirectly, TPR = diastolic blood pressure Parts of the BP apparatus 1. Bulb inflates the inflatable bag inside the cuff which should cover 80% of the arm 2. Cuff covers 2/3 of the arm o If the arm diameter is more than 35 cm you must use the 14 cm cuff o Normally 12 cm cuff is used Effect of placing the wrong cuff: Too big: false low reading Too small: false high reading 3. Exhaust To decrease or increase pressure in the cuff 4. Mercury More accurate because gravity is constant PROCEDURE When getting the blood pressure: Rested around 5 minutes Has not smoked cigar or drank coffee within the last 30 minutes Patient position: sitting or lying with the brachial artery at the level of the heart
3.
Long term Control Renin-Angiotensin mechanism Aldosterone pressure regulating mechanism Longer mechanism involved in chronic hypertension Aorta pressure flow or point will run around 4 meters per second The smaller the artery, the higher the velocity o Radial 0.1 second from the heart beat Palpable arteries 1. Brachial artery most common which is used for getting blood pressure o Where medial sclerosis is checked or stiffening of blood vessels o For calcified vessels, make use of the thumb 2. Radial artery o Thumb side 3. Ulnar artery little finger side 4. Popliteal artery 5. Dorsalispedis o Normally absent bilaterally but never present unilaterally obstruction 6. Posterior tibial artery posterior to the medial malleolus 7. Carotid artery last to disappear with a patient with shock
Rationale: for every 13.6 cm elevation, you decrease the blood pressure or systolic pressure or arterial pulse around 10 mmHg o Lowering of arm, you increase blood pressure o Lower extremities higher blood pressure due to gravity Apply the cuff o Bladder should cover the top of the brachial artery o 1 inch from the elbow o Tie the cuff tightly but can insert at least 1 finger Do palpatory method o Radial pulse o Inflate BP cuff gently until the disappearance of the radial pulse o Pulsation is more on systolic pressure Deflate the cuff o Deflate it up to 0 mmHg Auscultatory method o Use a stethoscope o Ideally: Length: 12 inches No ear leaks Ear piece should be pointed inward towards the ear canal With diaphragm or bell Bell is ideally used Put diaphragm under the cuff Put the stethoscope on top of brachial artery o Inflate 30 mmHg higher than palpatory method Release air 2 mmHg per heartbeat o
Conditions:Sound until 0 mmHg Elderly Aortic regurgitation o Use phase 4 as diastolic pressure even in children Documentation of blood pressure Record phase 1 systolic pressure and phase 5 diastolic pressure Repeat this 2 minutes apart o Baseline use extremity with higher blood pressure Check if patient has coarctation of the aorta o Hypertension = coarctation of aorta o Extremity distal to the obstruction elevated blood pressure o Extremity proximal to the obstruction decrease and very slow pulse Documentation of hypertension Recheck the blood pressure after a week Hypertension A. Essential 90% B. Secondary o Renal most commom o Endocrine Primary aldosteronism Cushings syndrome Pheochromocytoma surgically corrected form of hypertension Oral contraceptive JNC 7 Category Normal: Prehypertension: HTN Stage 1 HTN Stage 2 SBP <120 120-139 140-159 160 DBP <80 80-89 90-99 100
CVD CAD Renal disease Vascular disease Advance hypertension Retinopathy
Low risk No CV risk factors, TOD or ACC Medium risk 1-2 CV Risk Factors, No TOD or ACC High risk 3 or more CV Risk Factors, with TOD or ACC or DM Hypotension Hypovolemia o External fluid losses o Internal sequestration First manifestation: increased Heart Rate Losses 20% of volume Cardiogenic o cannot pump adequate pressure to supply Obstruction to blood flow o Neuropathic - SCI o Drug induced o Spinal cord injury o Orthostatic decrease in sympathetic tone Valsalva Strain Maintained 10 sec Release Increase in BP Decrease BP, decrease pulse pressure, increase heart rate Decrease BP BP overshoots HR too much sympathetic activity
Korotkoff sounds PHASE 1 Loudest sound A clear sharp snapping sound Appears suddenly and grows louder Recorded as systolic pressure Auscultatory Gap o Period of silence in between two beats Normal rhythm normal korotkoff sounds PHASE 2 Sound is softened and becomes prolonged into a murmur PHASE 3 Sound becomes crisper and increased in intensity PHASE 4 Distinct abrupt muffling of the sound PHASE 5 Sound completely disappears Recorded as the diastolic pressure
Risk Stratification Major risk factors for CVD Smoking Dyslipidemia Men > 55 Women > 65 Diabetes mellitus Family history Target Organ Damage (TOD) hypertensive urgency Goal: lower BP gradually LVH Proteinuria Ultrasound or radio evidence of atherosclerosis Narrowing of retinal vessels Associated Clinical complications (ACC)
Ejection fraction - Force of blood ejected by the heart During inspiration: blood is directed to the pulmonary circulation Strain with closed glottids:increase in blood pressure <50/40 (LVEDP = 35 mmHg) Decrease BP, (no sympathetic activity) o BP goes up straining after release goes down o No korotkoff sound <30/10 LVEDP 40mmHg BP remains elevated, no overshoot or brady square wave Frank-Starlings Law Heart will pump what it is given to it
Ankle Brachial Index (ABI) Getting systolic pulse in the ankle/brachial Normal 0.9-1.1 Mild 0.4-0.8 Revascularization <0.4 Calcified veins > 1.2 Revascularization if obstruction is big Calcified veins Very high readings Medial sclerosis blood vessels are calcified o BP more than 300 mmHg o Real BP intravascularly very low volume Pseudohypertension High blood pressure but low volume BP in coarctation High Blood pressure - Proximal extremity Low blood pressure in lower extremity Maynes sign o Elevation of the arm = Exaggerated drop of 15 mmHg Hill Sign o Increase of: 20 MILD 20-40 MODERATE 40-60 SEVERE
Prolonged (tardus) Coarctation of aorta Very slow pulse o
PulsusBiferens/Dicrotic/Bifid Seen in: o Combined aortic stenosis and aortic regurgitation o Pistol shot (traubes/duroziezs- 2 murmurs produced by diastolic and systolic) Pulsusparadoxus o Tamponade o Any obstruction of the heart, except pregnancy, results to pulsusparadoxus JUGULAR PRESSURE AND PULSES 1. 2. 3. Pressure o Arterial pulse 16x that of venous pulse Abdominal compression o Aka Hepatojugular reflux Inspiration o Carotid not affected o Jugular- decrease in level; pulsation increases Descent (S, VS, S2) o A, C, & V: positive o H, D, Y: negative o Arterial pulse end after S2 o Venous pulse end before s2 o A: atrial contraction Pressure in jugular Contaction: increase in + wave Relaxation leading to X descent (- wave) o Followed by C: closure of tricuspid o Then major descent: X prime Produced by: o When the ventricles contract , free wall goes to septum; base goes downejects blood in the ventricle o Base of R ventricletricuspid valve>>goes down producing X during contraction o Filling of atrium, D wave>>closed tricuspid valve Blood flows until the tricuspid valve opens and have another negative descent o H wave
Filling of both the atria and ventricles Positive wave Another cycle begins atrial contractions
Abnormalities A wave o Giant A wave o Obstruction of outflow (atrium) o Tricuspid stenosis o Atrial myoma o PS/ PHPN (peripheral HPN) o Cannon A wave o AV dissociation o No A wave o Atrial fibrillation X descent o Decrease or (-) o HF o Tricuspid regurgitation o Atrial myxoma o Increase o ASD: increase volume o Pulm HPN o Tamponade V wave o Increase o ASD (rapid atrial filling) o Tricuspid Regurgitation severe: ventricularization o CHF, sever PHPN Inc o o o Dec/ o
4.
Characteristics of Arterial Pulse Rate: Rapid (frequens) tachycardia Above 100bpm Slow (rarus) bradycardia Below 60bpm
Rhythm Irregular (irregularis) Wide QRS Atrial fibrillation Irregular R-R intervals Size Large(magnus) AR(aortic regurgitation), FEVER, ANEMIA, THYROTOXICOSIS Wide: bounding pulse Small (parvus) o AS, MS, CHF, PERICARDIAL EFFUSION
H wave o
Restriction of RV expansion (constrictive pericarditis) Restrictive cariomyopathy Tricuspid Stenosis
Twinckes sign o Apply pressure in nailbeds until demarcation of blood + tricuspid regurgitation or fever: movement of margin of blood Dr. Tolentino PERIPHERAL VASCULAR DISORDERS Functions: Lymphatics o Drains fluid lymph from bodily tissues return to venous circulation o Problem with drainage: obstruction due to:
Wave type Quick (celer) Mitral Regurgitation, VSD Volume overload
Infection Tumor -
o o o
Frostbite Immersion foot Chilblain (Pernio)
Lymph nodes o Important in the spread of cancerous cells Capillaries o Found in the nail beds: between lunula and nail beds Capillary pressures 1. Hydrostatic pressure Forces fluid out into the tissue spaces aided by interstitial colloid oncotic pressure 2. Colloid Oncotic pressure plasma proteins pulls fluid back into the vascular tree Veins o Drains blood to the heart Arteries Important in the determination of BP and reflect contractility of blood vessels
Pain on exposure to heat o Erythromelalgia or Erythermalgia (Weir Mitchells disease) Uncomfortable in warm environment, often plunging their extremities into ice water for relief Coldness and Paresthesia Coldness: o Arterial obstruction: the extremity is cold because the blood supply is inadequate o Venous obstruction: extremity may be cold due to associated arteriospasm and the blood remains in the extremity longer and loses more heat: dissipation Paresthesia o Occurs both with arterial and venous disease but is more common with arterial lesions o Has stocking-glove distribution distribution due to pressure on arterial supply o Tingling sensation when blood flows after occlusion o
When patient sits with leg in a dependent position, a cyanotic rubor occurs within 2-3 minutes (Burgers test) In dependent position the veins should fill in 10-15 seconds Delayed filling (beyond 20 sec) of veins on the dorsum of foot that were collapsed when legs were elevated
B. -
Chronic venous insufficiency have small purpuric lesion on the skin around the ankles. Iron pigment remains in the skin producing a brown mottling or pigmentation about the ankles Iron pigments are from the RBC
PROBLEM WITH ARTERIES: PROBLEM WITH SUPPLY AND MANIFESTATIONS DISORDERS OF: Lymphatics, capillaries andveins are usually due to organic lesion Arterial disease may either be organic or functional (vasoconstriction)
Ulcers (peripheral): common finding PVD o Raynauds phenomenon: side of the fingers near the base of the nail o Arteriosclerosis obliterans: pressure points on the feet hind, sole, and for bedridden patients: sacrum o Chronic venous insufficiency: above the medial malleolus o Ischemic ulcers: lateral surface of the legs Atrophy: common in arterial lesions o May lead to loss of skin appendages (hair follicles, oil glands and sweat glands) o Toenails andfingernails develop longitudinal ridges, thicken and curve over the tips of toes and fingers o **Pruritus manifestation of Dry skin Gangrene o Wet gangrene: Involved area may be purulent, moist and edematous If due to: Venous obstruction Infection Superficial arterial lesion o Dry gangrene: Involved area is atrophic and mummified due to arterial obstruction
C. -
Skin discoloration Acute arterial obstruction: Pallor Chronic arterial insufficiency: Cyanosis when the extremity is dependent and sometimes arteriosclerosis Erythromelalgia: marked vasodilatation extremities are red and hot Raynauds phenomenon: cyanosis as the arteriospasm and venospasm begin and marked pallor when the arteriospasm is severe. During phase of vasodilation, the extremities are red Mottling: due to uneven distribution of blood. May occur because of vasoconstriction or organic obstruction with uneven distribution of collateral circulation o 2 vasospastic disease causing mottling of the skin *Acrocyanosis *Levidoreticularis
MANIFESTATIONS THAT BRING THE PATIENT FOR CONSULATION: Symptoms and signs: A. Pain Most frequent Arterial insufficiency: o Pain is brought by exertion and relieved by rest (Intermittent claudication) cause of pain: Ischemia or angina when muscles lack oxygen it produces lactic acid -
Chronic venous insufficiency: o Severe muscle cramps in the calves and feet, which awakens patient from sleep Pain on exposure to cold o Raynauds disease
PHYSICAL EXAMINATION 1. INSPECTION Most important maneuver + palpation of the pulses Anxiety may cause vasoconstriction and pallor Color: o If arterial circulation is impaired: When foot is elevated to 90 deg , the veins empty and the skin has pale cadaverous appearance
pitting edema o in the dorsum of the foot o PE: best site to check: anterior tibia or shin bone presence of bones
run finger over the bone and feel presence of depression dorsum of the foot: presence of soft tissues
Thrombophlebitis Compressing tumors CHF Portal obstruction Arteriovenous fistula
Positive test: slow filling with occlusion, but release of compression is followed by quick filling from above (1-10 sec) Indicates: Incompetence of the great saphenous vein Double positive: rapid filling during compression , together with added increment of blood from above when pressure is released Indicates: incompetence in both the saphenous vein and its femoral communication
a. b.
DISEASE OF THE LYMPHATIC Lymphedema lymohanigitis
*Varicose veins without venous insufficiency is asymptomatic *Varicose veins with venous insuffuenciency: 1. Aching pain in the calves that is relieved by elevation of the extremities 2. Experience night-time cramps 3. Relief of pain by sharply dorsiflexing the foot or arising from bed and walking 4. Edema 5. Pruritus; due to stretching of the skin by the edema 6. Paresthesia 7. Skin ulceration * Varicosities are most common in leg veins TEST FOR COMPETENCE IN GREAT SAPHENOUS VEINS PERCUSSION TEST: o Patient standing and the varicose vein s filled with blood, palpate a segment of vein below the knee while sharply percussing the vein above the knee. o The receiving finger should feel an impulse only when the valves are incompetent o This is to test valvular competence of superficial and deep veins BRODIE-TRENDELENBURG TEST o Test for competence in Saphenofemoral complex Elevate the lower extremity to vertical Stroke the blood from the veins toward the heart until they are empty Apply tourniquet around the midthigh, snugly enough to occlude the superficial veins With tourniquet in place have the patient stand Note the time taken for venous filling from below, in any case, release the tourniquet within 60 sec Normally: Arterial blood flow from below fills the veins in about 35 sec; no further release should occur after the release of the tourniquet. Negative test: slow filling with occlusion, and no added increment of blood after release of compression Indicates: competence in both the great spahenous and communication with femoral vein -
Lymphedema primary o congenital (Milroys disease) o lymphedema praecox (Meiges disease) o lymphedema tarda secondary o recurrent lymphangitis o tuberculosis o filariasis - most common o phlebitis o Neoplasm (malignant invasion) o Surgery - nod e resection and dissection Radical mastectomy: no drainage o Radiation therapy
Lymphedema Painless swelling of one or both extremities skin ulceration is common marked pitting edema skin of edematous leg may have a rosy hue Lymphangitis Acute Lymphangitis most common disorder characterized by superficial red streaks along the course of the lymphatic vessels VEINS DISEASE OF THE VEINS 2 most common: o Varicose veins o Thrombophlebitis Less common: o Phlebosclerosis o Phlebofibrosis o Spontaneous rupture of the veins
PERTHES TEST Have the patient walk about 5 minutes. Then inspect the varicosities Apply tourniquet to the midthigh when the patIent is standing and the veins are filled with blood Have him walk for 5 minutes If the veins collapse below the tourniquet, the deep veins are patent and the communication veins are competent If the venous caliber remains unchanged, incompetence is present in both saphenous and communicating vein In the veins increase in prominence and pain occurs, the deep veins are occluded Test for obstruction of deep veins OCHSNER-MAHORNER Modification of Perthes test Locate the level of incompetence in communicating veins After midthigh, the tourniquet is applied at the knee and at the midcalf B. THROMBOPHLEBITIS Obstructive disease of the veins Acute: o Associated with localized pain, tenderness, swelling and fever o If it involves an extremity: Edema and dependent cyanosis Chronic: o pain and tenderness are slight and less reddening and heat in the underlying skin Phlegmasia alba dolens o Sudden thrombophlebitis of the femoral vein excruciating pain, massive edema of the extremity and pallor (less intense) from arterial spasm, more cyanosis, femoral vein tender, no anesthesia produced Phlegmasiacaeruleadolens
A. VARICOSE VEINS Primary varicosities: Often familial and is usually associated with congenital defects of the veins and their valves 2-3 times as frequent in women as in men Secondary varicosities: Pregnancy Trauma
o o
Involvement of the entire venous return of an extremity Extreme pain, massive edema, deep cyanosis of the entire limb
Deep vein thrombophlebitis o Silent thrombophlebitis o Phlebothrombosis o Usually applied in thrombosis of the deep veins of the legs o Most important consequence of the disorder is pulmonary embolism DVT: Early Physical signs Symptoms: o Pain or sense of fullness in the leg aggravated by standing or walking Signs: o Restlessness, fever, tachycardia o Cyanosis especially when the leg is dependent o Pitting edema o Venous engorgement of the feet o Elevated skin temperature around ankle or calf Pratts sign Presence of 3 dilated veins over the tibia, called sentinel vv Venous distention should persist when the legs are elevated to 450 Persistent congestion or dilatation Louvels sign Cough or sneeze pain in hte calf Pain in the leg along the course of the thrombosed vein Pain disappears with digital compression of the vein proximal to the obstruction
Ramirezs Sign Calf pain with passive congestion Patient in supine position Knees slightly flexed Sphygmomanometer cuff wrapped above the knee and inflated to 40 mm Hg Resulting venous pressure provokes pain at the site of thrombophlebitis If pressure is sustained for 5 minutes , intensity of pain is increase Pain disappear promptly when the pressure is released Liskers sign Bone tenderness Percuss the subcutaneous surface of tibia, medial to crest, using the tip of flexed finger Bone tenderness is present in about 65% of persons with deep-vein thrombosis Homans sign Calf spasm Knee flexed Forceful and abrupt dorsiflexion of the ankle Pain in calf or popliteal region in about 35% of patients with deep vein thrombosis Also positive in 1. Herniated low intervertebral disk 2. Other lumboscaral affectation -
Symptoms produced because of impaired or restricted blood supply to tissues: Muscle weakness Fatigue Atrophy Intermittent claudication Hair loss Skin ulceration Gangrene FIBROMUSCULAR DYSPLASIA Hyperplastic disorder affecting medium-sized and small arteries Occurs predominantly in females Usually involves renal and carotid arteries but can affect extremity vessels Medial dysplasia : most common type ARTERIOSCLEROSIS OBLITERANS Obstructive degenerative disease Occlusion of large and small arteries by atheromata Highest incidence in 6th and 7th decades of life Primary symptom: intermittent claudication ( site: distal to occlusion) LERICHES SYNDROME Atherosclerotic occlusion of the aortic bifurcation causing hip claudication, impotence, decreased muscle mass in the buttocks and legs PE: no pulses on the lower extremities If collateral circulation is adequate, hair loss and atrophy do not occur THROMBOANGIITIS OBLITERANS Buergers disease Inflammatory occlusive vascular disorder involving small and medium-sized arteries and veins in the distal upper and lower extremities Most frequently in men under age 40 Prevalence higher in Asians Cause: unknown There is a definite relationship to cigarette smoking Clinical feature: triad of intermittent claudication, Raynauds phenomenon and migratory superficial vein thrombophlebitis TAKAYASUS DISEASE A.K.A Pulseless disease Young female arteritis Reverse coarctation RAYNAUDS DISEASE Vasoconstrictive disorder of the arteries and arterioles involving hands and feet precipitated by nervousness and exposure to cold More common in women between 20 and 40 years
Superficial thrombophlebitis o May mask the coincidental occurrence of deep-vein disease o Ultrasonic examination greatly simplifies diagnostication of this condition DISEASES OF THE ARTERIES Arterial disorders Occlusive Partial Complete Nonocclusive A-V fistulas Aneurysms Arterial deficit in tissues 2 etiologic factors: 1. Mechanism of arterial occlusion Compression of the vessel Vasospasm Narrowing of the lumen by intimal thickening Plugging of the lumen by thrombus or embolus 2. Intrinsic disease of the artery that promotes occlusion
Bancrofts sign and Moses sign Calf tenderness with digital compression Consists of compressing the calf forward against the tibia and comparing the resulting with that elicited by transverse compression while the gastrocnemius is lifted from the tibia by grasping both sides of the muscles Thrombophlebitis causes more pain in forward compression Lowenbergs sign Calf tenderness with cuff compression Sphygmomanometer cuff is wrapped around each calf and simultaneous inflation of the 2 Most normal persons tolerate pressures of 180 mm Hg The more sensitive calf is the site of thrombosis -
Fingers are involved more than toes Classic color changes sequence of pallor, cyanosis and rubor when induced by exposure to cold
Palpation: thrill may be felt Palpable pulsation is common in thin, nervous patients Auscultation: systolic murmur
RAYNAUDS PHENOMENON associated with other diseases Cold exposure Trench foot Immersion foot Chilblain ( pernio ) Frostbite Cold exposure: 3 stages: 1. Prehyperemic stage 2. Hyperemic stage 3. Posthyperemic stage Acrocyanosis No discomfort except for cosmetic effect Cyanosis in abolished when part is elevated or when patient sleeps Erythromelalgia Burning sensation in the lower extremities associated with local warmth and a reddish or cyanotic color of the skin during times of exposure to increased heat A-V fistula or aneurysm Abnormal communication between an artery and an adjacent vein Usually the result of trauma Elevated skin temperature in the area of aneurysm Aneurysm Most are due to arteriosclerosis Aneurysm of thoracic Aorta: those that occur in the ascending part of the arch of the aorta Signs of Aneurysm: Inspection o Heaving o Pupil may be dilated or contracted on one side Palpation o Over the larynx may demonstrate tracheal tug Auscultation o Continuous humming-top murmur is usually present when there is communication between the aneurysm and vena cava or the pulmonary artery Aneurysm of the Abdominal Aorta: Inspection: epigastrium = pulsatile mass
Venous drainage of the lower extremities: 3 groups: Deep and superficial veins Popliteal Femoral o Vena committantes of anterior and posterior tibial artery Superficial veins Small saphenous vein Great saphenous vein Tributaries: perforating communicating vein of deep and superficial Dr. Tolentino For abdominal examination o Good light o Relaxed patent o Proper draping o Full exposure from above xiphoid process to symphysis pubis o Patient should not have full bladder o Arms on the side or folded across the chest o Back flat on bed o Knees slightly flexed or pillows under knees o Warm hands, stethoscope and fingernails Sitophobia Dysphagia Odynophagia Variants of vomiting Hematochezia Scybalous stools Matching type o Inspection o Percussion o Palpation o Auscultation Cullens sign Grey-Turners sign Sister Mary-Joseph nodules Diastesis recti Lack or absence of normal sounds Succession splash Fibrillary hum Blumbergs sign Markle sign Rovsings sign Murphys sign Courvoisiers law
Middletons method Hernia o Irreducible or incarcerated strangulated o Richters hernia Virchows nodes o Sentinel node o Signal node o Troisiers node Essay o Fluid wave o Shifting dullness o Puddle sign Ovarian cyst Review of the heart o All the signs - IDENTIFICATION
Dr. Oribio Signs and symptoms of different endocrine problems Dr. Ursua History taking o Physician-patient relationship o Establish rapport History of Present Illness Variables that influence the status of the patient Patient gynecologic history Ovulatory vs anovulatory cycle OB score Characteristic of menstrual flow Menstrual irregularities Complete sexual history Sign and symptom Signs and symptoms more commonly seen in Gyne patient Dr. Irmscher Male Genitalia True or False FSH stimulate sertoli cells to release mullerian inhibiting substance that in turn inhibits the production of mullerian duct or the female counterpart LH/hCG: stimulates the Leydig Cells to produce testosterone Formation of testosterone in the presence of Y chromosome Urination and Potency are the most common complaint Herpes lesions are hard, solitary Matching Type Phimosis: difficulty retracting the prepuce Behcels: ulceration of the glans penis Chordee: fibrous band between the glans and the frenulum Hypospadia: meatal opening on ventral side Chancroid: bubo Peyronie: fibrous intracavernous flap; crooked penile shaft (fibrosis) Priapism: painful erection
Fracture of the Shaft: injury to the corpus cavernosum Contusion: painless Edema: due to renal failure translated to Nephrotic syndrome during the quiz Conditions with Transillumination 1. Hydrocoele 2. Spermatocoele True about Torsion of the spermatic cord Sudden twisting Affects the Left Side Surgical emergency Leg on the affects side is flexed (+) Prehns Sign True of Indirect Hernia Passes thru the inguinal canal scrotum Prone to strangulation Most commonly seen in adults Except: Hasselbachs seen in Direct Signs
Disappearance of median furrow: BPH Nodularity: cancer Tender prostate with induration: TB -
Dr. Tolentino Hematopoietic and Lymphatic systems Reticulocyte count o More than 3% o Recent blood loss o Hemolytic disorder Melanotic spots around the lips and oral mucous membranes o Peutz-Jeghers syndrome Drugs associated with aplastic anemia o Antibacterials Chloramphenicol Sulfamethoxypyridazine Sulfisoxazole Penicillin Tetracyclins o Diuretics Acetazolamide Chlorohtiazide Sickle cell hemoglobin or hemoglobin S o Most common hemoglobinopathy o Aseptic necrosis of the femoral head o Gait abnormality o Fish mouth deformity Necrosis of the femoral head o Hemoglobin G Allele of hemoglobin S Hereditary spherocytosis and elliptocytosis
Increased incidence of gallstones composed of bilirubin Pernicious anemia o Lack intrinsic factor o Unable to absorb vitamin B12 Lead poisoning o Wristdrop o Periphera neuropathies occur commonly Agnogenic myeloid metaplasia o Hematopoiesis develops in extramedullary tissues Iron deficiency anemis o Most common anemic disorder Koilonychias o Flattening of the nail beds Gaisbocks syndrome or stress polycythemia o Decrease in plasma volume o Relative polycythemia An absolute increase in red cell mass is most commonly observed in persons who suffer from chronic hypoxemia due to chronic obstructive pulmonary disease or in children and young adults with significant right-to-left shunts of cardiac origin Inguinal adenopathy o Best detected with the patient in the recumbent position Tuberculous lymhadenitis o Scrofula o Kings Evil o Involves cervical nodes Sarcoidosis o Disorder of unknown etiology produces noncaseating granulomas Sjogrens disease o Schirmers test Cut a strip of Whatman #40 filter paper 15 mm long and 5 mm wide Make a small fold at one end and place this in the conjuctival sac Strip is allowed to remain the conjuctival sac for 2 minutes after which the length of filter paper wetted by the lacrimal secretions is measured The test is positive if less than 5 mm of paper has been wetted Lymphomas o Pruritus is a relatively frequent manifestation of Hodgkins disease and may be a presenting manifestation Multiple myeloma o Solitary plasmacytoma or as diffuse transformation of the plasma cell series o Punched out lesions Types of immune reactions table o
o Complement fixation o I negative o II positive o III positive o IV negative Differences between hemohilioid and purpuric states Purpura o Capillary o Cutaneous and mucosal o Unusual Hemophilioid o Small artery o Muscle, joints o Common Glossary of nomenclature of coagulation factors o Name of deficiency state other than factor deficiency V Proaccelerin Labile factor AC Globulin XIV Jaundice o Accumulation of bilirubin in the bloodstream causes yellow pigmentation of the plasma, leading to discoloration of heavily perfused tissues o Serum bilirubin levels accumulate when its productin from heme exceeds its metabolism and excretion o Imbalance Excess release of bilirubin precursors into the bloodstream Physiologic processes that impair hepatic uptake Metabolism Excretion of this metabolite o Hyperbilirubnemia jaundice or icterus skin and sclerae o Detectable at lower bilirubin levels in patients with fair skin and profound anemia o Obscured in individuals with dark skin or edema o Sclera tissue is rich in elastin which hs a high affinity for bilirubin o Darkening of the urine o Renal excretion of bilirubin in the form of bilirubin glucuronide o Greenish hue oxidation of circulating bilirubin to biliverdin o Conjugated hyperbilirubinemia cirrhosis o Carotenemia yellow skin Beta carotene
90% - unconjugated form, nonpolar circulating as an albumin bound complex o Conjugated form, polar primarily glucuronide, water soluble, excreted by the kidney o 80% senescent red blood cells o Life span 120 days destroyed by reticuloendothelial cells o Ineffective erythropoiesis resulting from destruction of maturing erythroid cells Second major source o Sulfonamides and salicylates compete with bilirubin for binding sites on albumin permitting the released pigment to enter tissues such as CNS o Neonatal hyperbilirubinemia Neurotoxic o Conjugated bilirubin Reversible Noncovalent binding Less stable Irreversible Covalent irreversible complex with albumin Delta bilirubin or biliprotein 1 gram of hemoglobin = 1.34 ml of oxygen Myelophthisic anemia o Bone marrow invasion by malignant derangements due to replacement of erythropoetic tissue Pernicious anemia o Beefy red tongue Aplastic anemias o Choramphenicol o Aspirin o Phenylbutazone o phenytoin Traumatic disorders o Prosthetic heart valves Hemolytic disorder incidental to mechanical trauma to red cells Lead poisoning o Pain scale o Moonshine whiskey o Wristdrop Iron deficiency anemias o Angular stomatitis o Koilonychias or flattening of nail beds o Most common anemic disorder Spontaneous bleeding less than 20,000 per cumm Fibrinogen Prothrombin Thromboplastin Factor V o
Factor X
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Oral Biopsy: Oral Pathologist's Perspective: Review ArticleДокумент7 страницOral Biopsy: Oral Pathologist's Perspective: Review ArticleRafa LopezОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
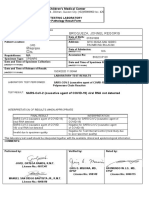
- Broqueza, Jonnel Regoris: Philippine Children's Medical CenterДокумент1 страницаBroqueza, Jonnel Regoris: Philippine Children's Medical CenterRica RegorisОценок пока нет
- Rent AgreementДокумент4 страницыRent Agreementkhushbu chitreОценок пока нет
- ESHRE Guideline EndometriosisДокумент27 страницESHRE Guideline EndometriosisRodiani MoekroniОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Health Assessment Made Incredibly Visual Incredibly Easy Series 2nd Edition PDFDrive 9 18Документ10 страницHealth Assessment Made Incredibly Visual Incredibly Easy Series 2nd Edition PDFDrive 9 18mianpenarandaОценок пока нет
- Departm Ent of Education: R e P U B Lic of Tlje JH JilippineffДокумент7 страницDepartm Ent of Education: R e P U B Lic of Tlje JH JilippineffJoyce CarilloОценок пока нет
- Laparoscopic Course: General Principles of Laparoscopy: Specific Aspects of Transperitoneal Access (R.Bollens)Документ4 страницыLaparoscopic Course: General Principles of Laparoscopy: Specific Aspects of Transperitoneal Access (R.Bollens)Anuj MisraОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- SPESIFIKASI ETERNITY Anesthesia Machine AM834Документ2 страницыSPESIFIKASI ETERNITY Anesthesia Machine AM834si tuyulОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- 1-Collection, Storage and Transportataion of MicrobiologicalДокумент49 страниц1-Collection, Storage and Transportataion of MicrobiologicalSummi NizОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Minerva Anestesiol 2017 GruenewaldДокумент15 страницMinerva Anestesiol 2017 GruenewaldMarjorie Lisseth Calderón LozanoОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- WORKSHOP No 3Документ21 страницаWORKSHOP No 3Jennifer Mabel Almeida BrionesОценок пока нет
- Echinochrome A and Cytokine Storm SyndromeДокумент11 страницEchinochrome A and Cytokine Storm SyndromeNicolas Fernandez RubilarОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Family Therapy and Systemic PracticeДокумент4 страницыFamily Therapy and Systemic PracticeUyên TrươngОценок пока нет
- A Modified Supine Position Facilitates Bladder Function in Patient Undergoing Percutaneous Coronary InterventionДокумент8 страницA Modified Supine Position Facilitates Bladder Function in Patient Undergoing Percutaneous Coronary InterventionVelicia MargarethaОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- Advanced Drug Delivery Reviews: Sadaf Aghevlian, Amanda J. Boyle, Raymond M. ReillyДокумент17 страницAdvanced Drug Delivery Reviews: Sadaf Aghevlian, Amanda J. Boyle, Raymond M. ReillyKamila MartinОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Asthma Reading Task Text A and B Oet Reading NotesДокумент16 страницAsthma Reading Task Text A and B Oet Reading NotesSakshi RanbhiseОценок пока нет
- Rubella Quantitative IgG - IMMULITE 2000 SystemsДокумент40 страницRubella Quantitative IgG - IMMULITE 2000 SystemsMaria Ruth Moreno VargasОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- DiabetesMellitus enДокумент2 страницыDiabetesMellitus enRajesh KumarОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- OncologyДокумент3 страницыOncologyMichtropolisОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Dialysis SkillsДокумент2 страницыDialysis Skillssheelaaku100% (1)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Carboplatin MonographДокумент9 страницCarboplatin Monographmerkuri100% (1)
- Commonly Billed Codes: Spinal Cord StimulationДокумент21 страницаCommonly Billed Codes: Spinal Cord StimulationKrishna KumarОценок пока нет
- Novel Coronavirus Vocabulary - 2020 03 PDFДокумент5 страницNovel Coronavirus Vocabulary - 2020 03 PDFLena MustafaОценок пока нет
- MCQ Final 2014Документ19 страницMCQ Final 2014JohnSon100% (1)
- Lesson 3 - The Circulatory and Respiratory SystemsДокумент26 страницLesson 3 - The Circulatory and Respiratory SystemsEmieleah Lorenzo PauigОценок пока нет
- Uterine Leiomyomas (Fibroids) - Epidemiology, Clinical Features, Diagnosis, and Natural History - UpToDateДокумент48 страницUterine Leiomyomas (Fibroids) - Epidemiology, Clinical Features, Diagnosis, and Natural History - UpToDateRuben Orduño RizoОценок пока нет
- ACTIVATE-Butea SuperbaДокумент22 страницыACTIVATE-Butea Superbaowenangela100% (1)
- Drug Study Ceftriaxone SodiumДокумент3 страницыDrug Study Ceftriaxone SodiumPrincess Queenie OlarteОценок пока нет
- Congential 3 Musculoskeletal 3 Neurological 3 Abusive DisordersДокумент7 страницCongential 3 Musculoskeletal 3 Neurological 3 Abusive DisordersNichole CollinsОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Final Report Sero Survey0409Документ160 страницFinal Report Sero Survey0409BSL-2Оценок пока нет