Академический Документы
Профессиональный Документы
Культура Документы
FKG3 Tambahan - Hormone Thyroid
Загружено:
vil66Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
FKG3 Tambahan - Hormone Thyroid
Загружено:
vil66Авторское право:
Доступные форматы
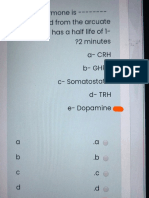
Thyroid Physiology and Pharmacology
Overview o Thyroid
o
Two hormones types released:
thyroxine and triiodothyronine calcitonin
o 11 11 11 11
Thyroxine and triiodothyronine are important in:
growth development maintaining normal body temperature energy metabolism regulation Receptors:
Thyrotropin (TSH, a pituitary hormone) modulates thyroid function by binding to TSH receptors (TSH-R) TSH-R: localization and properties:
o
basolateral membrane of thyroid follicular cells.
Iodide:
Metabolism: Iodide intake: gastrointestinal tract absorption from food, water, or medication.
Iodide:
o o o
rapid absorption enters extracellular pool thyroid removes amount required for hormone secretion
excess iodide: urinary excretion
Non-Physiological Thyroid Simulation:
o
Graves' disease:
Greenspan, F.S., and Dong, B. J.. Histamine, Thyroid and Antithyroid Drugs, in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp 619-633.
Wartofsky, L., Diseases of the Thyroid, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, pp 20122034
Thyroid Hormones
Chemistry of thyroid hormones: o Active isomer -- levo (L-form) -- thyroxine, triiodothyronine, reverse iodothyronine (reverse T4) Pharmacokinetics:
o
T4 -- well absorbed from the ileum and duodenum following oral administration-- about 80% absorbed on average Modification of absorption:
food drugs (e.g., sucralfate, iron, aluminum-containing antacids)
o o
T3 -- almost completely absorbed (95%) following oral administration T4 and T3 absorption may be impaired by myxedema (may require parenteral administration {IV}, as a result) Factors that alter T4 and T3 clearance:
hyperthyroidism: increases hypothyroidism: decreases Drugs (hepatic microsomal enzymes inducers): Clearance is enhanced; Euthyroid state may be maintained because of thyroid hyperfunction.
phenobarbital carbamazepine (Tegretol) phenytoin (Dilantin) rifampin
Increases in the number of TBG binding sites (due to pregnancy, estrogen use, oral contraceptive use)
more thyroid hormone is bound; elimination rate declines (only free hormone can be eliminated); normal hormone concentration would be eventually restored
1. 2.
Mechanism of Hormone Action: Unbound T4 and T3 diffuse into the cell (passive diffusion, possibly active transport) Inside cell: 3. T4 converted to T3 4. T3 is transported to the cell nucleus where T3 binds to a specific T3 nuclear receptor
Thyroid hormones: metabolic actions o nuclear receptor activation results in increased RNA and protein synthesis: examples -
increased Na/K ATPase causes increased ATP turnover, increased oxygen consumption --calorigenic effect
Thyroid Hormone Effects*
Physiological system
Hyperthyroidism (thyrotoxicosis)
Hypothyroidism
skin --appendages
warm, moist skin; sweating; fine, thin hair; Plumber's pale, cool, puffy skin; brittle nails; pretibial hair and nails dermopathy (Graves' disease) Upper lid retraction (wide stare); Eyelid drooping; periorbital periorbital edema; edema; puffy, nonpitting exophthalmos, facies; large tongue diplopia (Graves' disease) decreased peripheral increased peripheral resistance, increased resistance, decreased cardiac output, cardiac output, stroke
Eyes, face
Cardiovascular
stroke volume, heart volume, heart rate, pulse rate, pulse pressure; pressure; congestive heart congestive heart failure (low output); failure (highbradycardia (low voltage output); increased ECG with prolonged PR contractility,. interval, flat T wave); arrhythmogenic; pericardial effusion angina Respiratory dyspnea; reduced vital capacity increased appetite; increased bowel movement frequency; hypoproteinemia Nervousness, hyperkinesia, variable emotional states Weakness; fatigue; hypercalcemia, osteoporosis, increased deep tendon reflex hypoventilation (CO2 retention) pleural effusions decreased appetite, decreased bowel movement frequency; ascites
Gastrointestinal
CNS
lethargy, neuropathy
Musculoskeletal
muscle fatigue, reduced deep tendon reflex, increased alkaline phosphatase, LDH, AST
Renal
Increased renal blood Decreased renal blood flow; flow; increased GFR; decreased GFR; reduced mild polyuria water excretion anemia (increased RBC turnover); increased erythropoiesis decreased fertility; menstrual irregularity; enhanced gonadal steroid metabolism increased basal rate; negative nitrogen balance, hyperglycemia; increased free fatty acids, decreased cholesterol and triglycerides; anemia (decrease production rate, decreased iron absorption, decreased folate acid absorption, autoimmune pernicious anemia),decreased erythropoiesis infertility;hypermenorrhea, decreased libido; impotence, decreased gonadal steroid metabolism decreased basal rate; delayed insulin degradation, with increased sensitivity; enhanced cholesterol and triglyceride levels; decreased hormone degradation; decreased requirements for fat-and
Hematopoietic
Reproductive
Metabolic
increased hormone degradation; increased water-soluble vitamins; requirement for fat- decreased drug and water-soluble detoxification. vitamins; enhanced drug detoxification * * Adapted from Table 38-4, Greenspan, F.S., and Dong, B. J.. Histamine, Thyroid and Antithyroid Drugs, in Basic and Clinical Pharmacology, (Katzung, B. G., ed) AppletonLange, 1998, p 625. Greenspan, F.S., and Dong, B. J.. Histamine, Thyroid and Antithyroid Drugs, in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp 619-633. Wartofsky, L., Diseases of the Thyroid, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, pp 20122034
Thyroid preparations: o Synthetic:
o
levothyroxine liothyronine liotrix
Animal origin:
dessicated thyroid-- never justifiable; many disadvantages {protein antigenicity; product instability and variable hormone concentration; difficulty and lab assessment}
Preparations of choice: synthetic levothyroxine:
Applications:
thyroid replacement suppression therapy
11 11 11 11 11 11
Rationale:
low-cost stability non-allergenic (no foreign protein) serum levels readily obtained long half-life (seven days) -- supports once-daily dosing since T4 is converted to T3 inside the cell, T4 administration produces both hormones
o
Liothyronine -- more active than levothyroxine but not recommended because of:
11 11 11
shorter half-life (multiple dosing) more costly
higher hormonal activity enhances cardiotoxicity (T3 -- contraindicated in patients with cardiac disease)
11
most appropriate use: short-term TSH suppression
Antithyroid Drugs:
Overview o Purpose:
reduction of thyroid activity reduction of hormone effects
Approach:
use drugs that change tissue response to thyroid hormones destroy the the thyroid with surgical or radiation interventions
Definition:
"goitrogens" -1. compounds that suppress T3 and T4 secretion 2. thereby increasing TSH 3. increased TSH levels produces thyroid gland enlargement (goiter)
Antithyroid drugs include:
thioamides iodides radioactive iodine
Thioamides:
o
Major drugs for thyrotoxicosis:
Propylthiouracil
rapidly absorbed bioavailability: 50 -- 80% (incomplete absorption/large firstpass effect) metabolism: glucuronidation by the liver; excreted by the kidney short half-life (1.5 hours) but accumulated by the thyroid crosses placental barrier (increased protein binding compared to methimazole makes propylthiouracil preferable for use in pregnancy since less free drug is available to cross into the fetus)
Methimazole
(about 10 times more active than propylthiouracil) well absorbed accumulated by the thyroid
11
crosses the placental barrier
Mechanism of Action: thioamides
Major action: inhibits thyroidal peroxidase-catalyzed reactions, blocking iodine organification: -- thus preventing hormone synthesis. Propylthiouracil and methimazole (too a much reduced degree) inhibit peripheral deiodination of T4 and T3
11 11
Slow onset of pharmacological effect
Toxicity:
Frequency of adverse effects: 3-12%. Most common: maculopapular pruritic rash Most serious potential reaction: agranulocytosis -- risk 0.3% 0.6 % of patients; reversible upon discontinuation; cross sensitivity between propylthiouracil and methimazole possibly increased risk in:
o o
elderly patients receiving high-dose methimazole
Anion Inhibitors
o
Competitive inhibition:
Perchlorate Pertechnetate Thiocyanate
Major clinical use -- potassium perchlorate ( not often used because of the possibility of causing aplastic anemia)
blockade of thyroid gland reuptake of I- in patients with iodide-induced hyperthyroidism
Iodides
o o
rarely used now as monotherapy Actions on the thyroid:
inhibit organification inhibit hormone release-- major action
Mechanism: perhaps inhibition of thyroglobulin proteolysis
decreased thyroidal size and vascularity may induce hyperthyroidism (jodbasedow) may precipitate hypothyroidism
Clinical Considerations:
may be useful in short-term management of thyroid storm maybe helpful in preoperative preparation for surgery (due to reduction in gland vascularity, size, and fragility) Major disadvantages:
11
iodide therapy increases intraglandular iodine concentration
may delay initiation of thioamides treatment may delay use of radioactive iodine treatment
chronic iodide used in pregnancy: avoid -- iodide crosses the placenta and may cause fetal goiter
11
iodide as monotherapy: not appropriate; iodide block lasts only 2-8 weeks; withdrawal at this time may exacerbate thyrotoxicosis
11
Iodide use, if at all, should be initiated only after thioamide treatment and not used if radioactive iodine therapy is planned
Iodinated Radiographic Contrast Media
o o
Useful in management of hyperthyroidism (off label use) Ipodate and iopanoic acid inhibit T4 to T3 conversion in:
kidney liver pituitary gland brain
o o 11 11
additional mechanism: iodine release-mediated inhibition of hormone release Clinical Use:
adjunctive treatment of thyroid storm alternatives if thioamides and iodides are contraindicated
o
Toxicity:similar to iodides; relatively nontoxic.
Radioactive Iodine:
o o
131
I is the radioactive isotope used for treating thyrotoxicosis.
Mechanism of Action:
rapidly absorbed, concentrated in the thyroid incorporated into thyroid follicles beta emission is the basis for therapeutic efficacy Thyroid parenchymal destruction occurs within a few weeks.
o 11 11 11 11
Therapeutic Advantages for radioiodine:
good efficacy easy to administer low expense pain free treatment
o
Contraindication:
131
I-- not administered to pregnant women or nursing mother;131I crosses placental barrier and excreted in breast milk.
Adrenergic receptor blocking drugs:
o
Rationale: reduction of sympathetic manifestations in thyrotoxicosis:
Applicable drugs:
beta adrenoceptor blockers guanethidine
Agent of choice: propranolol (Inderal, nonselective beta-receptor antagonist)
Hypothyroidism
Overview: hypothyroidism 1. cause: inadequate thyroid hormone synthesis 2. Cretinism -- when hypothyroidism is present from birth and accompanied by developmental abnormalities 3. Myxedema: severe hypothyroidism associated with:
deposition of hydrophilic mucopolysaccharides in the dermis (ground substance) and other tissues-- causing:
facial feature thickening doughy skin induration
Pretibia myxedema
Adult hypothyroidism: Pretibial myxedema in the foot and lower extremity skin 1999 KUMC Pathology and the University of Kansas, used with permission; courtesy of Dr. James Fishback, Department of Pathology, University of Kansas Medical Center.
Hypothyroidism: Causes/Classification Thyroid
Thyroprivic* Congenital development defect
Goitrous Biosynthesis defect (genetic) Transmitted by the mother (antithyroid drugs) Iodine deficiency Drug-induced {e.g. salicylates,
Idiopathic (primary) Postablative {postsurgical,131I} Postradiation {e.g. for lymphoma}
lithium,iodides, phenylbutazone,iodoantipyrine}
chronic thyroiditis (Hashimoto's disease); interleukin 2
Suprathyroid (Trophoprivic) Pituitary Panhypopituitarism Isolated low TSH levels Hypothalamic Congenital defect Infection (e.g. encephalitis) Neoplasm; Infiltrative (sarcoidosis)
Hypothyroidism: pathogenesis 1. inadequate thyroid hormone synthesis causes TSH hypersecretion which results in goiter 2. if this compensatory physiological response is insufficient, goitrous hypothyroidism occurs o Causes of goitrous hypothyroidism (North America)
most common cause: Hashimoto's disease
Mechanism: A. defective binding of iodide B. abnormal secretion of iodoproteins
Iodide-induced goiter with or without hypothyroidism: intrinsic defect inorganic binding mechanism
Euthyroid patients with Graves' disease {particularly following surgery or radioiodine therapy}, patients with Hashimoto's disease, and normal fetuses are particularly susceptible to iodide-induced goiter.
(Right) Struma lymphomatosa in Hashimoto thyroiditis, gross. Note: diffuse, pale yellow infiltrate affecting the entire thyroid. The yellow infiltrate is caused by an influx of lymphocytes, which may form follicles. Normal thyroid (Left) 1999 KUMC Pathology and the University of Kansas, used with permission; courtesy of Dr. James Fishback, Department of Pathology, University of Kansas Medical Center.
Hypothyroidism: Clinical presentation o Neonates (note that cretinism may be present at birth, but usually is apparent within the first few months after birth as a function of the extent of thyroid failure)
manifestations:
physiologic jaundice constipation somnolence feeding problems
Since early clinical diagnosis may be difficult and early treatment is necessary to ensure normal intellectual development,all neonates should be screened for hypothyroidism by measuring serum T4 or TSH
Young Children:
coarse features, protruding tongue, broad, flat nose, widely set eyes, dry skin, coarse hair. impaired mental development, retarded bone age, epiphyseal dysgenesis, delayed dentition.
Older Child:
retardation of linear growth, delayed puberty poor school performance
Adult:
fatigue, lethargy, constipation, cold intolerance, slowing of intellectual and motor activity lessened appetite; increased weight dry skin; dry hair (may fall out) deeper, hoarser voice With Advanced Disease: (florid myxedema)
dull, expressionless facies, sparse hair, periorbital puffiness , large tongue, rough and doughy skin (cool, pale) enlarged heart (dilation, pericardial effusion) adynamic ileus Without treatment: myxedema coma possible with respiratory depression and increased PCO2
Laboratory Tests:
single most useful: serum TSH
increased levels in thyroprivic and goitrous normal or undetectable in pituitary or hypothalamic hypothyroidism
in hypothalamic hypothyroidism: TSH hypersecretion is associated with hypersecretion of other pituitary hormones
All hypothyroidism:
decreased serum T4 and free T4I serum T3 may be decreased less than serum serum T4
Some other abnormal laboratory results:
increase serum cholesterol (hypothyroidism of thyroid origin)
increased creatinine phosphokinase increased aspartate transaminase indications of pernicious anemia
Pharmacological treatment:
o
Synthetic hormones:
levothyroxine, preferred liothyronine liotrix (combination of new L-thyroxine and liothyronine)
Neonatal, infantile, and juvenile hypothyroidism: early full replacement therapy vital to improve likelihood of:
normal intellectual development normal growth
If neonatal, infantile, and juvenile presentations result from pituitary and hypothalamic hypothyroidism, treatment with hydrocortisone should precede thyroid replacement therapy:
Rationale:acute adrenocortical insufficiency may because by the increase in metabolic rate with increase glucocorticoid clearance following thyroid hormonal treatment
Adults:
rapid treatment desirable especially in patients with:
11 11
myxedema coma
hypothyroid patients needing to undergo emergency surgery (these patients have extreme sensitivity to CNS depressants);
IV levothyroxine with hydrocortisone may be appropriate
to patients with myxedema coma and systemic illness may have reduced ability to convert T4 to T3. In these cases supplemental liothyronine may be added to levothyroxine.
*- Thyroprivic: refering to lack of thyroidhormone (e.g. removal of the gland or suppression of glandular function)
Thyrotoxicosis:
Definition:clinical, physiological, biochemical consequences when tissues respond to excess thyroid hormone Most important causes: those associated with prolonged hormone overproduction by the thyroid. Causes:
o
Extra-pituitary unregulated thyroid stimulation: 1. Graves' disease 2. Hashimoto's disease 3. trophoblastic tumor
o o o o
Chronic thyroiditis Excessive TSH secretion by pituitary tumor (rare) Autonomous thyroid gland hyperfunction Ingestion of meat contaminated with animal thyroids ("hamburger toxicosis")
Hyperthyroidism is only associated with conditions in which thyroidal hyperfunction leads to thyrotoxicosis.
Graves' disease
Three major presentations: o hyperthyroidism with diffuse goiter
o o
dermopathy ophthalmopathy
Thyroid Pathology :
o o o
soft, enlarged, vascular Parenchymal hypertrophy/hyperplasia Lymphocytic infiltration (suggesting the immunological nature of the disease)
"Diffuse toxic goiter of Graves disease, gross, showing symmetric, non-nodular hypervascular enlargement of the thyroid" 1999 KUMC Pathology and the University of Kansas, used with permission; courtesy of Dr. James Fishback, Department of Pathology, University of Kansas Medical Center.
Graves' disease: other involvements o generalized lymphoid hyperplasia and infiltration
o o
spleenic or thymic enlargement Thyrotoxicosis associated with:
skeletal muscle fiber degeneration cardiac enlargement diffuse liver fibrosis with fatty infiltration skeletal decalcification body tissue loss
1. 2.
Ophthalmopathy:characterized by -inflammatory orbital content infiltrate (lymphocytes, mast cells, plasma cells)
enlargement of orbital musculature (lymphocytes infiltration, mucopolysaccharides, edema, fat)
3.
eventually -- muscle fiber degeneration; loss of striations; fibrosis Dermopathy:
dermal thickening (lymphocytes infiltration; mucopolysaccharides)
Clinical Presentations:-- Thyrotoxicosis
o
Common manifestations (thyrotoxicosis)
nervousness, insomnia, tremors, frequent bowel movements, heat intolerance, sweating, emotional instability weight loss despite adequate or increased appetite muscle weakness oligomenorrhea/amenorrhea in premenstrual women dyspnea palpitations exacerbation of angina/cardiac failure (older patients)
Ocular Presentations: -- distinct from ophthalmopathy associated with Graves' disease; ocular signs mainly due to excessive sympathetic stimulation
characteristics stare (widening palprebral fissures) lid lag infrequent blinking failure to wrinkle brow upon upward gaze
Cardiovascular effects:
wide pulse pressure sinus tachycardia atrial arrhythmias (particularly atrial fibrillation) systolic murmurs occasionally heart failure
Clinical Presentations: Graves' disease
o
Common manifestations:
hyperfunctioning goiter
asymmetric, lobular
ophthalmopathy
Two components: spastic and mechanical
spastic-- stare, lid lag, lid retraction
proptosis (sensitive to antiadrenergic agents) including: 1. ophthalmoplegia 2. periorbital swelling 3. conjunctivitis 4. corneal ulceration, optic neuritis, optic atrophy
Diagnosis:
in addition to physical manifestations described earlier:
undetectable TSH Usually increased values of T4 and T3.
Thyroid Storm:
o o o o
Fulminating increase in symptoms of thyrotoxicosis "Medical storm" is now likely to be seen in undertreated patients. Precipitated by surgery or complicating illness, often sepsis. Presenting syndrome:
extreme irritability coma or delirium high fever, 41oC tachycardia hypotension vomiting diarrhea
Treatment:
manage dehydration: IV glucose/Saline, vitamin B complex glucocorticoids (possible reduction in adrenal reserve; increase glucocorticoid requirement and thyrotoxicosis digitalis may be required to control elevated ventricular rates in the presence of atrial fibrillation Block hormone synthesis by large dose propylthiouracil; followed by large doses of iodine, oral or parenteral; sodium ipodate may be used instead of iodine
Propranolol (adrenergic antagonist) important in the absence of CHF Combination treatment with propylthiouracil, iodine, dexamethasone is likely to result in serum T3 levels returning to normal within one to two days.
Greenspan, F.S., and Dong, B. J.. Histamine, Thyroid and Antithyroid Drugs, in Basic and Clinical Pharmacology, (Katzung, B. G., ed) Appleton-Lange, 1998, pp 619-633. Wartofsky, L., Diseases of the Thyroid, In Harrison's Principles of Internal Medicine 14th edition, (Isselbacher, K.J., Braunwald, E., Wilson, J.D., Martin, J.B., Fauci, A.S. and Kasper, D.L., eds) McGraw-Hill, Inc (Health Professions Division), 1998, pp 20122034
Вам также может понравиться
- 7Документ6 страниц7Sungo GridsawanОценок пока нет
- 0132554909Документ22 страницы0132554909vil66Оценок пока нет
- Dentj 38 3 07Документ5 страницDentj 38 3 07vil66Оценок пока нет
- ContentsДокумент104 страницыContentsvil66Оценок пока нет
- Hapoong FamilyДокумент1 страницаHapoong Familyvil66Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Biocheistry Viva Question BankДокумент5 страницBiocheistry Viva Question BankNIHAR UTHALEОценок пока нет
- Chapter 38 Endocrine System FunctionДокумент2 страницыChapter 38 Endocrine System FunctionPaige Nicole GauthreauxОценок пока нет
- Hyperthyroidism: A Stepwise Approach To ManagementДокумент8 страницHyperthyroidism: A Stepwise Approach To ManagementLikha UlandariОценок пока нет
- Chapter 18 Endocrine SystemДокумент40 страницChapter 18 Endocrine SystemlolasparkleОценок пока нет
- EEF467 Tutorial Sheet 1Документ5 страницEEF467 Tutorial Sheet 1NK-NGAMОценок пока нет
- Endocrine SystemДокумент41 страницаEndocrine SystemMerrin EncarnacionОценок пока нет
- Untitled2 PDFДокумент15 страницUntitled2 PDFVANESSA AMELIOОценок пока нет
- Thyroid NodulesДокумент43 страницыThyroid NodulesRaker AMSAОценок пока нет
- Product CatalogueДокумент20 страницProduct CatalogueNguyễn Khang KhangОценок пока нет
- Unit 3 Part 4 Organ-Specific Autoimmune DisordersДокумент23 страницыUnit 3 Part 4 Organ-Specific Autoimmune DisordersReman AlingasaОценок пока нет
- Subclinical Hyperthyroidism UptoDateДокумент17 страницSubclinical Hyperthyroidism UptoDatesamuel_thamОценок пока нет
- Hyperthyroidism CaseДокумент52 страницыHyperthyroidism CaseEncee Mian100% (2)
- QR Management of Thyroid Disorders (MEMS) 20200721Документ16 страницQR Management of Thyroid Disorders (MEMS) 20200721DОценок пока нет
- 2nd Journal - Andre Parmonangan Panjaitan - 013Документ7 страниц2nd Journal - Andre Parmonangan Panjaitan - 013Andre Parmonangan PanjaitanОценок пока нет
- Assessment of Thyroid FunctionДокумент7 страницAssessment of Thyroid FunctionDewi Paramita YuniarahmiОценок пока нет
- HyperthyroidismДокумент73 страницыHyperthyroidismZNEROL100% (1)
- SBA Questions (No Answers)Документ65 страницSBA Questions (No Answers)minayokiОценок пока нет
- Pex 04 01Документ7 страницPex 04 01Aulia Azizah KosmanОценок пока нет
- QuestionsДокумент35 страницQuestionsYasmeen AtiehОценок пока нет
- Graves DiseaseДокумент6 страницGraves Diseaseabida.syeda.718Оценок пока нет
- Asesmen Keterampilan Berpikir Tingkat Tinggi PDFДокумент23 страницыAsesmen Keterampilan Berpikir Tingkat Tinggi PDFFitria HandayaniОценок пока нет
- TSH Levels Low To High Ranges, Symptoms, and WhaДокумент1 страницаTSH Levels Low To High Ranges, Symptoms, and WhaErwin Dela GanaОценок пока нет
- Patient Type: OPD: TSH Test ReportДокумент1 страницаPatient Type: OPD: TSH Test ReportVeenu SehrawatОценок пока нет
- Endocrine NotesДокумент9 страницEndocrine NotesLucky GomezОценок пока нет
- Anatomy and Physiology of The Endocrine System: Presenté ParДокумент64 страницыAnatomy and Physiology of The Endocrine System: Presenté ParYackson FrankОценок пока нет
- Thyroid and Antithyroid PharmaДокумент31 страницаThyroid and Antithyroid PharmaxaviermargaridaОценок пока нет
- Abim Lab ValuesДокумент4 страницыAbim Lab ValuesBell GatesОценок пока нет
- All Endocrine PharmacologyДокумент143 страницыAll Endocrine PharmacologyabenezergebrekirstosОценок пока нет
- NBME 11 Answers To All SectionsДокумент101 страницаNBME 11 Answers To All SectionsBenjaminTan100% (5)
- Physiology of ThyroidДокумент9 страницPhysiology of ThyroidAbby EvangelistaОценок пока нет