Академический Документы
Профессиональный Документы
Культура Документы
Eclampsia: Pathophysiology
Загружено:
NuriinayaОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Eclampsia: Pathophysiology
Загружено:
NuriinayaАвторское право:
Доступные форматы
Eclampsia
- Courtney Reynolds, MD, William C. Mabie, MD, & Baha M. Sibai, MD
Eclampsiaoccurs in 0.2-0.5% of all deliveries, with occurrence being influenced by the same factors as inpreeclampsia. In rare instances,eclampsiadevelops before 20 weeks' gestation. About 75% of eclampticseizuresoccur before delivery. About 50% of postpartum eclampticseizuresoccur in the first 48 hours after delivery, but they may occur as late as 6 weeks postpartum.
Pathophysiology
The pathogenesis of eclampticseizuresis poorly understood. Seizures have been attributed to platelet thrombi, hypoxia due to localized vasoconstriction, and foci of hemorrhage in the cortex. There is also a mistaken tendency to equateeclampsiawith hypertensive encephalopathy. There is a poor correlation between occurrence ofseizuresand severity of hypertension. Seizures may occur with insignificant blood pressure elevations that are only slightly higher than readings recorded 24 hours previously. The hallmarks of hypertensive encephalopathy (retinal hemorrhages, exudates, and papilledema) are very infrequent ineclampsia, where funduscopic changes are minimal.
Clinical Findings
There is usually no aura preceding the seizure, and the patient may have one, two, or manyseizures. Unconsciousness lasts for a variable period of time. The patient hyperventilates after the tonic-clonic seizure to compensate for the respiratory and lactic acidosis that develops during the apneic phase. Fever is rare but is a poor prognostic sign. Seizure-induced complications may include tongue biting, broken bones, head trauma, or aspiration. Pulmonary edema and retinal detachment have also been noted followingseizures.
Treatment
A. Prenatal Treatment
Hypertensive States of Pregnancy
Hypertensive States of Pregnancy Preeclampsia L Classification L Pathogenesis LPathophysiology L Clinical Findings L Differential Diagnosis LComplications L Prevention L Treatment L Prognosis Eclampsia Chronic Hypertension L Clinical Findings LComplications L Treatment L Prognosis
1.Control ofseizures- In many centers outside the United States, anticonvulsants are not used prophylactically. For References example, in the United Kingdom it is thought that the maternal risk ofeclampsia, although variable, can be predicted. Anticonvulsant drugs such as diazepam, phenytoin, and chlormethiazole are used sparingly. In the United States, obstetricians believe the risk ofeclampsiato be unpredictable and not correlated with symptoms ofpreeclampsia, blood pressure readings, deep tendon reflexes, or the degree of proteinuria. Most authorities recommend giving anticonvulsants to all patients in labor who have hypertension with or without proteinuria or edema. Since many women will be treated who are at low risk forseizures, the drug must be safe for mother and fetus. Fifty years of experience with magnesium sulfate has shown it to be effective and safe. The mechanism of the anticonvulsant action of magnesium sulfate is unknown. Its use has been criticized on the grounds that it does not cross the blood-brain barrier and does not have a central nervous system inhibitory effect. While early studies failed to show a significant increase in cerebrospinal fluid (CSF) magnesium concentrations during therapy, more recent studies have shown about a 20% increase in CSF magnesium levels, and these levels parallel those in the serum. Magnesium sulfate decreases the amount of acetylcholine released at the neuromuscular junction, resulting in peripheral neuromuscular blockade at high magnesium concentrations; however, this does not account for its anticonvulsant effect. A recent study demonstrated that magnesium sulfate had a central anticonvulsant effect on electrically-stimulated hippocampalseizuresin rats. The researchers speculated that since magnesium ion blocks calcium entry into neurons through the N-methyl-D-aspartate (NMDA) receptor-operated calcium channel, magnesium sulfate might be acting through this mechanism. On the other hand, another study found that magnesium sulfate was ineffective in altering seizure discharge in pentylenetetrazole-induced status epilepticus in rats. These researchers argued that because magnesium blocks calcium entry through the NMDA receptor-operated calcium channel in a voltage-dependent manner, it would be ineffective in neurons that are continuously depolarizing as in status epilepticus. Finally, Doppler studies of brain blood flow in preeclamptic women suggest that magnesium sulfate vasodilates the smaller-diameter intracranial vessels distal to the middle cerebral artery and may exert its main effect in the prophylaxis and treatment ofeclampsiaby reversing vasospastic cerebral ischemia. Other actions are transient mild hypotension during intravenous loading, transient mild decrease in uterine activity during active labor, tocolytic effect in premature labor, and potentiation of depolarizing and nondepolarizing muscle relaxants. Magnesium sulfate has unpredictable effects on fetal heart rate variability (increased, decreased, or unchanged). Maternal dose-related effects at various serum levels are: 10 mg/dL, loss of deep tendon reflexes; 15 mg/dL, respiratory paralysis; and 25 mg/dL, cardiac arrest. The therapeutic level is between 4.8 and 8.4 mg/dL. This range is empiric, based on levels obtained with an intramuscular dose usually found to be effective. Magnesium sulfate is usually given intravenously as a loading dose of 6 g over 20 minutes followed by a constant infusion of 2 g/h. If plasma levels are lower than 5 mg/dL, the maintenance dose is increased to 3 g/h. Patients may haveseizureswhile receiving magnesium sulfate. If a seizure occurs within 20 minutes after the loading dose, the convulsion is usually short, and no treatment is indicated. If the seizure occurs more than 20 minutes after the loading dose, an additional 2-4 g of magnesium sulfate may be given. Usually a magnesium level drawn acutely reveals subtherapeutic levels, but occasionally this is not so. In such cases, diazepam, 5-10 mg given intravenously, or amobarbital, up to 250 mg given intravenously, may be used. The patient should be checked every 4 hours to be sure that deep tendon reflexes are present, respirations are at least 12/min, and urine output has been at least 100 mL during the preceding 4 hours. The antidote for magnesium sulfate overdose is 10 mL of 10% calcium chloride or calcium gluconate given intravenously. The remedial effect occurs within seconds. Phenytoin is not as effective as magnesium for the prevention of eclampticseizures; however, it may be used safely in settings in which there is a risk in using magnesium, such as patients with myasthenia gravis.
Diazepam causes respiratory depression, hypotonia, poor feeding, and thermoregulatory problems in the newborn. Also, the sodium benzoate preservative competes with bilirubin for albumin binding, thus predisposing the infant to kernicterus. 2.Control of hypertension- There is controversy about whether or not uteroplacental blood flow is autoregulated. Most evidence indicates that the uterine vasculature is maximally vasodilated at all times. Therefore, most physicians believe that reductions in maternal blood pressure tend to decrease uteroplacental perfusion and caution against treatments that will cause large, precipitate drops in mean arterial pressure. Antihypertensive drugs are usually given if the diastolic blood pressure exceeds 110 mm Hg. The goal is to bring the diastolic blood pressure into the 90-100 mm Hg range. a. Hydralazine- The drug of choice is hydralazine, a direct arteriolar vasodilator that causes a secondary baroreceptor-mediated sympathetic discharge resulting inTachycardiaand increased cardiac output. This latter effect is important because it increases uterine blood flow and blunts the hypotensive response, making it difficult to give an overdose. If late decelerations of fetal heart rate do occur after hydralazine administration, they usually respond to fluid-loading, administration of oxygen, turning the patient on her side, and discontinuing oxytocin. Hydralazine is metabolized by the liver, and in patients with slow acetylation, it has a longer duration. The dose is 5 mg given intravenously every 15-20 minutes. The onset of action is 15 minutes, the peak effect occurs within 30-60 minutes, and the duration of action is 4-6 hours. Side effects include flushing, headache, dizziness, palpitations,angina, and an idiosyncratic lupuslike syndrome in patients taking more than 200 mg/d chronically. In more than 95% of cases ofpreeclampsia, hydralazine will be effective in controlling blood pressure. Other agents have been substituted for hydralazine, most commonly labetalol, nifedipine, and diazoxide. b. Labetalol- Labetalol is a nonselective beta blocker and postsynaptic 1-adrenergic blocking agent available for both oral and intravenous administration. Intravenous labetalol is given every 10 minutes as follows: the first dose is 20 mg, the second is 40 mg, and subsequent doses are 80 mg - to a maximum cumulative dosage of 300 mg or until blood pressure is controlled. It may also be given as a constant infusion. Onset of action is in 5 minutes, peak effect is in 10-20 minutes, and duration of action ranges from 45 minutes to 6 hours. Uteroplacental blood flow appears to be unaffected by intravenous labetalol. Initial experience indicates it to be well-tolerated by mother and fetus. c. Nifedipine- Nifedipine, a calcium channel blocker, can be administered in a bite-and-swallow technique to lower blood pressure acutely. It is a powerful arteriolar vasodilator with the main problem being overshoot hypotension. For this reason, it probably should not be used in patients with intrauterine growth retardation or abnormal fetal heart rate patterns. Profound hypotension may be reversed by volume administration or intravenous calcium. Although nifedipine appears to have much potential, it requires further assessment of its use in pregnancy. d. Sodium nitroprusside- Sodium nitroprusside causes equal degrees of vasodilatation in arteries and veins without autonomic or central nervous system effects. Its onset of action is 1.5-2 minutes, the peak effect occurs in 1-2 minutes, and the duration of action is 3-5 minutes. It is an excellent drug for minuteto-minute control in an intensive care unit setting. It may be titrated against a segmental epidural block for labor orcesarean section. It is recommended that the drug not be administered intravenously over a period longer than 30 minutes in the undelivered mother because of the risk of cyanide and thiocyanate toxicity in the fetus. e. Trimethaphan- Trimethaphan, a ganglionic blocker, is used acutely by anesthesiologists to lower blood pressure prior to laryngoscopy and intubation for general anesthesia. A reported fetal side effect is meconium ileus. f. Nitroglycerin- Nitroglycerin given intravenously is a predominantly venular vasodilator that appears to be safe for the fetus. It is only a moderately powerful antihypertensive agent.
Fluids such as 5% dextrose in Ringer's lactate, 125-150 mL/h, are given intravenously. ASwanGanzcatheter is helpful in patients with pulmonary edema, massive hemorrhage, or oliguria unresponsive to a 1000-mL fluid challenge. Analgesia with intravenous meperidine or butorphanol is given in small doses every 1-2 hours. Local anesthesia with or without pudendal block may be used for vaginal delivery. The use of epidural anesthesia in patients withpreeclampsiais somewhat controversial. The problem is sudden hypotension due to pooling of blood in the venous capacitance vessels secondary to sympathetic blockade. However, with the almost universal use of epidural anesthesia forcesarean section, it has been widely used in preeclamptic patients. If there is no evidence of fetal compromise (by fetal heart rate criteria), if there is no coagulopathy present, if the patient is prehydrated, and if a segmental activation technique is used by an experienced anesthesiologist, epidural anesthesia may be used for labor and delivery or forcesarean section. If these criteria are not met, then balanced general anesthesia is preferred forcesarean section. Spinal anesthesia is considered contraindicated for women with severepreeclampsia.
C. Postpartum Treatment
Some of the constraints of therapy no longer apply once delivery has occurred, eg, sodium nitroprusside or diuretics may be used. Since 25% of eclampticseizuresoccur postpartum, patients withpreeclampsiaare maintained on magnesium sulfate for 24 hours after delivery. Phenobarbital, 120 mg/d, is sometimes used in patients with persistent hypertension in whom spontaneous postpartum diuresis does not occur or in whom hyperreflexia persists after 24 hours of magnesium sulfate. Alternatively, magnesium sulfate may not be continued for 36-48 hours. Hypertension may not resolve until 6 weeks postpartum. If the diastolic blood pressure remains consistently above 100 mm Hg for 24 hours postpartum, any number of antihypertensive agents could be given, including a diuretic, calcium channel blocker, ACE inhibitor, central alpha agonist, or beta-blocker. The blood pressure should be checked in the standing position to avoid the possibility of orthostatic hypotension. At follow-up after 1 week, the need for continuing antihypertensive therapy may be reevaluated.
Prognosis
Maternal deaths due topreeclampsia-eclampsia are rare in the United States, but death may be caused by cerebral hemorrhage, aspiration pneumonia, hypoxic encephalopathy, thromboembolism, hepatic rupture, renal failure, or anesthetic accident. It is important to stress that iatrogenic complications increase if multiple drugs are given. If the patient truly hadpreeclampsia, the risk of recurrence is less likely (33%) than if she had chronic hypertension mistaken forpreeclampsia. In the latter situation, the risk of recurrence is quite high (70%). In studies that include multiparas withpreeclampsia, the recurrence rate in the nextpregnancyis as high as 70%. In one study of primigravidas witheclampsia, only 33% had some hypertensive disorder in any subsequent pregnancy; in most cases, the condition was not severe, but 2% did have recurrence ofeclampsia. The effect ofpreeclampsia-eclampsia on subsequent development of chronic hypertension is debatable. Confusion may result from a mistaken diagnosis ofpreeclampsiain women with underlying renal disease or chronic hypertension. In one study of women witheclampsiaduring their firstpregnancywho were followed for more than 40 years, no increase was seen in the incidence of hypertension or deaths due to cardiovascular disease or other causes. Multiparas witheclampsiahad a much higher incidence of subsequent hypertension and deaths due to cardiovascular disease and other causes. It seems reasonable to conclude that the risk of recurrenteclampsiain subsequent pregnancies is not high enough to recommend against future pregnancies.Preeclampsiadoes not cause permanent damage, predispose to chronic hypertension, or adversely affect the long-term health of the mother.
http://www.health.am/pregnancy/eclampsia/
Вам также может понравиться
- CS ShockДокумент5 страницCS ShockJuliusSerdeñaTrapal0% (5)
- Week - 4 - Lecture (1) NCLEX SHORT CUT STUDYДокумент71 страницаWeek - 4 - Lecture (1) NCLEX SHORT CUT STUDYdatudeОценок пока нет
- SimulationДокумент5 страницSimulationJessFriend100% (1)
- Ob FinalДокумент43 страницыOb FinalPrincess LotusОценок пока нет
- Chapter 55Документ8 страницChapter 55DelindaEvansОценок пока нет
- Comparative Pharmacology For AnesthetistДокумент162 страницыComparative Pharmacology For AnesthetistGayatri PalacherlaОценок пока нет
- Cardiovascular Test Questions: "I Will Observe The Color of My Urine and Stool"Документ36 страницCardiovascular Test Questions: "I Will Observe The Color of My Urine and Stool"Melodia Turqueza GandezaОценок пока нет
- TROPONIN T & I Cardiac EnzymesДокумент2 страницыTROPONIN T & I Cardiac EnzymesIanОценок пока нет
- E. UrinaryДокумент16 страницE. UrinaryGloryJaneОценок пока нет
- Cardiovascular Test Questions: "I Will Observe The Color of My Urine and Stool"Документ36 страницCardiovascular Test Questions: "I Will Observe The Color of My Urine and Stool"Melodia Turqueza GandezaОценок пока нет
- Study Notes For Upper GI ProblemsДокумент5 страницStudy Notes For Upper GI ProblemsPrince K. Tailey100% (1)
- 3rd SpacingДокумент1 страница3rd Spacingmidnightdream254589Оценок пока нет
- U World Cardiac FinalДокумент15 страницU World Cardiac FinalAcohCChaoОценок пока нет
- Community Acquired Pneumonia CAP 1.28.21Документ1 страницаCommunity Acquired Pneumonia CAP 1.28.21Illaizah EdictoОценок пока нет
- CHP 66 Common Problems of Critical Care PatientsДокумент18 страницCHP 66 Common Problems of Critical Care Patientshops23Оценок пока нет
- Conduction System: Rhythm Identification and TreatmentДокумент12 страницConduction System: Rhythm Identification and Treatmenthops23Оценок пока нет
- SURG - Hepatobiliary, Pancreas, SpleenДокумент230 страницSURG - Hepatobiliary, Pancreas, SpleenJoan Timbol100% (1)
- Case Study Fluids ElectrolytesДокумент3 страницыCase Study Fluids ElectrolytesDawn Marie Manza-OpanchaОценок пока нет
- MS Final 46 Blood or Lymphatic DisorderДокумент4 страницыMS Final 46 Blood or Lymphatic DisorderZachary T Hall0% (1)
- Gastro Intestinal Disorders:: Kawasaki DiseaseДокумент6 страницGastro Intestinal Disorders:: Kawasaki DiseaseJoanna TaylanОценок пока нет
- Electrical Activity EKG EKG Pattern Name/ComplexДокумент2 страницыElectrical Activity EKG EKG Pattern Name/ComplexGloryJaneОценок пока нет
- Principles of NutritionДокумент34 страницыPrinciples of Nutritionfakhribabiker100% (1)
- Cardiac Conditions Cardiac Dysrhythmias: B. Sinus BradycardiaДокумент5 страницCardiac Conditions Cardiac Dysrhythmias: B. Sinus BradycardiaIrish Eunice FelixОценок пока нет
- Medical Surgical by Nursing CribДокумент7 страницMedical Surgical by Nursing Cribnursegian13100% (1)
- CorrectsДокумент46 страницCorrectsnursing_hallОценок пока нет
- Schedule of Virtual Classes For Nclex RN 2020Документ3 страницыSchedule of Virtual Classes For Nclex RN 2020Jasmine ClaireОценок пока нет
- Dele PrioДокумент10 страницDele PriomonmonОценок пока нет
- 1.113.medication Administration TimingДокумент14 страниц1.113.medication Administration TimingSophiaОценок пока нет
- Exam ReviewДокумент4 страницыExam ReviewMya Thomas100% (1)
- Addison Vs CushingsДокумент1 страницаAddison Vs CushingsChris ZantiraОценок пока нет
- Concept Map Et Al 11-04-15Документ7 страницConcept Map Et Al 11-04-15api-353656227Оценок пока нет
- Coronavirus (COVID-19) Quiz Review For NursesДокумент11 страницCoronavirus (COVID-19) Quiz Review For Nurseshasan ahmdОценок пока нет
- Shock and SIRSДокумент85 страницShock and SIRSBryan Mae H. DegorioОценок пока нет
- Pharmacology: General Anaesthetic AgentsДокумент65 страницPharmacology: General Anaesthetic AgentsSharifa DarayanОценок пока нет
- EditДокумент80 страницEditkaye patОценок пока нет
- Neurologic NCLEX Practice Test Part 1Документ6 страницNeurologic NCLEX Practice Test Part 1ojoj2206Оценок пока нет
- NCLEX QuestionsДокумент5 страницNCLEX QuestionsTindo Esa SariОценок пока нет
- Labor DeliveryДокумент10 страницLabor Deliverydhodejun lizhaldeОценок пока нет
- First Aid HandoutДокумент3 страницыFirst Aid HandoutMaria Alyssa NaranjoОценок пока нет
- Ch34 PharmДокумент8 страницCh34 PharmShaneka WilliamsОценок пока нет
- Asthma and COPD NCLEXДокумент17 страницAsthma and COPD NCLEXPotchiee PfizerОценок пока нет
- Nclex ReviewДокумент9 страницNclex ReviewGabriel 'gabo' AquinoОценок пока нет
- Critical Care Nurses' Knowledge RegardingManagement of Patients WithAtrial Fibrillation at Baghdad CityДокумент5 страницCritical Care Nurses' Knowledge RegardingManagement of Patients WithAtrial Fibrillation at Baghdad CityIOSRjournalОценок пока нет
- Group 5 - Hemodialysis - Chronic Kidney FailureДокумент31 страницаGroup 5 - Hemodialysis - Chronic Kidney FailureKimberly Abella CabreraОценок пока нет
- NclexДокумент4 страницыNclexihatetouОценок пока нет
- Medical Surgical Nursing 4 BulletsДокумент5 страницMedical Surgical Nursing 4 BulletsQueen ElizabethОценок пока нет
- Nclex Exam 14Документ9 страницNclex Exam 14Ya Mei LiОценок пока нет
- Drugs Med-SurgTest 3Документ6 страницDrugs Med-SurgTest 3Sarah PlunkettОценок пока нет
- Case Study Exam 1Документ7 страницCase Study Exam 1Tro WactОценок пока нет
- Antineoplastic DrugsДокумент16 страницAntineoplastic DrugstheintrovОценок пока нет
- DelegationДокумент3 страницыDelegationVanessa AbboudОценок пока нет
- 106 Finals Reviewer Quizlet and NurselabsДокумент62 страницы106 Finals Reviewer Quizlet and NurselabsCreciabullecerОценок пока нет
- Clotting Concept Analysis Diagram and ExplanationДокумент2 страницыClotting Concept Analysis Diagram and ExplanationJulius Haynes100% (1)
- DRUG SUMMARY TABLE - Anticoagulantes y AntiagregantesДокумент3 страницыDRUG SUMMARY TABLE - Anticoagulantes y AntiagregantesManuel BetancurОценок пока нет
- The Metabolic and Endocrine Systems NotesДокумент9 страницThe Metabolic and Endocrine Systems NotesCarl Elexer Cuyugan Ano100% (2)
- D. Preparing The Medication For Bolus AdministrationДокумент17 страницD. Preparing The Medication For Bolus AdministrationseanОценок пока нет
- CH 59 Care of Patients With Problems of The Biliary System and PancreasДокумент28 страницCH 59 Care of Patients With Problems of The Biliary System and Pancreasjrflores1284Оценок пока нет
- Pathology of Stroke: Dr. Isnaniah, Sp. SДокумент51 страницаPathology of Stroke: Dr. Isnaniah, Sp. SFiladelfia sariОценок пока нет
- Chapter 11: Parenteral Administration: Intradermal, Subcutaneous, and Intramuscular Routes Test BankДокумент7 страницChapter 11: Parenteral Administration: Intradermal, Subcutaneous, and Intramuscular Routes Test BankLuna TunaОценок пока нет
- Trauma and Emergency NursingДокумент9 страницTrauma and Emergency Nursingchinthaka18389021Оценок пока нет
- Meat Plant FeasabilityДокумент115 страницMeat Plant FeasabilityCh WaqasОценок пока нет
- Adsorbents and Adsorption Processes For Pollution ControlДокумент30 страницAdsorbents and Adsorption Processes For Pollution ControlJoao MinhoОценок пока нет
- Ventricular Septal DefectДокумент8 страницVentricular Septal DefectWidelmark FarrelОценок пока нет
- Chapter 2 Unfinished RRLДокумент22 страницыChapter 2 Unfinished RRLGM XylerОценок пока нет
- Analysis of Pure Copper - A Comparison of Analytical MethodsДокумент12 страницAnalysis of Pure Copper - A Comparison of Analytical Methodsban bekasОценок пока нет
- How To Do Banana Milk - Google Search PDFДокумент1 страницаHow To Do Banana Milk - Google Search PDFyeetyourassouttamawayОценок пока нет
- Intershield803 MDSДокумент4 страницыIntershield803 MDSSahanОценок пока нет
- Lichens - Naturally Scottish (Gilbert 2004) PDFДокумент46 страницLichens - Naturally Scottish (Gilbert 2004) PDF18Delta100% (1)
- Pengaruh Kualitas Anc Dan Riwayat Morbiditas Maternal Terhadap Morbiditas Maternal Di Kabupaten SidoarjoДокумент9 страницPengaruh Kualitas Anc Dan Riwayat Morbiditas Maternal Terhadap Morbiditas Maternal Di Kabupaten Sidoarjohikmah899Оценок пока нет
- Mil STD 792fДокумент13 страницMil STD 792fdoradoanОценок пока нет
- Report On Analysis of TSF Water Samples Using Cyanide PhotometerДокумент4 страницыReport On Analysis of TSF Water Samples Using Cyanide PhotometerEleazar DequiñaОценок пока нет
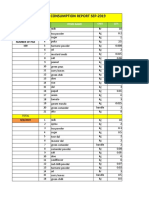
- Daily Staff Food Consumption Reports Sep-2019Документ4 страницыDaily Staff Food Consumption Reports Sep-2019Manjit RawatОценок пока нет
- 3 Activities For Adults To Practice Modeling SELДокумент10 страниц3 Activities For Adults To Practice Modeling SELDavid Garcia PerezОценок пока нет
- Characteristics of Testable HypothesesДокумент30 страницCharacteristics of Testable HypothesesMarivic Diano67% (3)
- Registration Statement (For Single Proprietor)Документ2 страницыRegistration Statement (For Single Proprietor)Sherwin SalanayОценок пока нет
- Science and TechnologyДокумент21 страницаScience and TechnologyPat MillerОценок пока нет
- Neopuff PDFДокумент4 страницыNeopuff PDFoechimОценок пока нет
- RRC Group D Notification 70812Документ11 страницRRC Group D Notification 70812admin2772Оценок пока нет
- Case Study of Milk ProductionДокумент46 страницCase Study of Milk Productionmian21100% (2)
- Eric Koech CV - Docx..bakДокумент7 страницEric Koech CV - Docx..bakPeter Osundwa KitekiОценок пока нет
- Minyak Atsiri Sereh WangiДокумент4 страницыMinyak Atsiri Sereh Wangicindy paraditha kasandraОценок пока нет
- Sanctuary Policy PomonaДокумент3 страницыSanctuary Policy PomonaGabriel EliasОценок пока нет
- Weld Metal Overlay & CladdingДокумент2 страницыWeld Metal Overlay & CladdingbobyОценок пока нет
- Bedwetting TCMДокумент5 страницBedwetting TCMRichonyouОценок пока нет
- TC 10 emДокумент7 страницTC 10 emDina LydaОценок пока нет
- Phardose Lab Prep 19 30Документ4 страницыPhardose Lab Prep 19 30POMPEYO BARROGAОценок пока нет
- User ManualДокумент21 страницаUser ManualKali PrasadОценок пока нет
- Ds0h Ufaa68 ProposalДокумент11 страницDs0h Ufaa68 Proposaledward baskaraОценок пока нет
- Class Two Summer Vacation AssignmentДокумент1 страницаClass Two Summer Vacation AssignmentshahbazjamОценок пока нет