Академический Документы
Профессиональный Документы
Культура Документы
Decreased Fetal Movement
Загружено:
Ywagar YwagarИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Decreased Fetal Movement
Загружено:
Ywagar YwagarАвторское право:
Доступные форматы
Launceston General Hospital Clinical Guideline WACSClinProc1.
12/10 Title: Replaces: Description: Target Audience: Key Words: Policy Supported: Purpose: The rationale for maternal monitoring of fetal movement is based on the assumption that early recognition of decreased fetal movement makes it possible for the clinician to intervene at a stage when the fetus is still compensated, and thus prevent progression to fetal or neonatal death. Women should be advised to contact their antenatal care provider if they feel a major and persistent decrease in usual activity, or if there are fewer than 10 movements over two hours at times when the fetus is usually active and the mother is focusing upon counting. Maternal concern of decreased fetal movement overrides any definition based on the number of kicks. The recommended time frame for initiation of clinical assessment is within 2 hours if fetal movements are absent and within 12 hours if they are decreased. The prevalence and significance of reduced fetal movement in the second trimester are largely unknown, while third trimester reduced fetal movement has been linked with adverse pregnancy outcomes related to fetal hypoxia and malnutrition. Women with third trimester reduced fetal movement are more likely to have pregnancies complicated by impaired fetal growth, preterm birth, and fetal or neonatal death than women with normal fetal movement. A decrease in perceived fetal movement does not necessarily mean the fetus is compromised. The perception of low fetal activity may be due to early gestational age, decreased amniotic fluid, maternal drug ingestion, fetal position, or a fetal sleep pattern. Fetal activity may be reduced with maternal illness or when amniotic fluid volume is decreased. The prevalence of perceived reduced fetal movement increases with nulliparity, obesity and smoking. Assessment of reduced fetal movement less than 24 weeks gestation: Review antenatal record for risk factors Auscultate fetal heart with doppler Provide reassurance, education and document in antenatal record and hand held record Discharge, after consultation with the senior midwife/registrar, for follow up with usual antenatal care provider. If fetal heart unable to be detected, the registrar, consultant or trained provider should then perform an ultrasound scan to visual the fetal heart
1 Decreased Fetal Movement Feb-11 WACSClinProc1.12/10
Decreased Fetal Movement Reduced Fetal Movement WACSClinProc1.12/07 Management of women with reduced fetal movement Midwives and medical officers, QVMU Reduced fetal movement
Assessment of reduced fetal movement greater than 24 weeks gestation: Review antenatal record for risk factors Maternal observations Abdominal palpation and symphysis fundal height (SFH) measure Auscultate fetal heart rate with a doppler. If over 30 weeks gestation perform an antenatal cardiotocograph (CTG). Consider antenatal CTG if less than 30 weeks gestation and risk factors present. Antenatal CTG only provides an assessment of immediate fetal condition Ultrasound scan assessment of fetal biometry, amniotic fluid volume and morphology (preferably within 24 hours) should be performed where maternal perception of decreased fetal movement persists despite a normal CTG For women with their first presentation, no risk factors and a reassuring CTG, consult with the senior midwife/registrar, provide education and complete documentation. Where concern remains over decreased fetal movement in the presence of normal clinical assessment (CTG and ultrasound) women should be advised to return for follow-up assessment within 24 hours. If recurrent presentation, with or without risk factors, SFH not within 2cm or CTG not reassuring then formal ultrasound scan (preferably within 24 hours) required for growth, AFI and UA dopplers. Registrar or Consultant to review and develop management plan. If fetal heart rate unable to be located then ultrasound scan to be performed by the registrar or consultant. If CTG is non-reassuring then referral to the registrar or consultant is required. Testing for fetal maternal haemorrhage is recommended. Fetal Movement Chart There is not enough evidence to recommend or not recommend formal fetal movement counting at present. There is indirect evidence that fetal movement counting may be beneficial. Limited data suggests that women prefer daily counting to repeated counting periods during the day.
2 Decreased Fetal Movement Feb-11 WACSClinProc1.12/10
Attachments Attachment 1 Performance Indicators: Review Date: Stakeholders: Developed by:
Reduced Fetal Movement Algorithm Evaluation of compliance with guideline to be achieved through medical record audit annually by clinical Quality improvement Midwife WACS Annually verified for currency or as changes occur, and reviewed every 3 years Midwives and medical staff WACS Dr A Dennis Co-Director (Medical) Sue McBeath Co-Director (Nursing & Midwifery) Womens & Childrens Services
Dr A Dennis Co-Director (Medical) Womens & Childrens Services
Sue McBeath Co-Director (Nursing & Midwifery) Womens & Childrens Services
Date: _15 June 2010_____
REFERENCES Froen, J 2006, Evaluation of decreased fetal movement, UpToDate, Online: http://uptodateonline.com/utd/content/topic.do?topicKey=antenatl/24547&selectedTitle=1~ 39&source=search_result Mangesi, L & Hofmeyr, G 2006, Fetal movement counting for assessment of fetal wellbeing, Cochrane Review, Online: http://www.mrw.interscience.wiley.com/cochrane/clsysrev/articles/CD004909/frame.html Olesen, A & Svare, J 2004, Decreased fetal movements: background, assessment, and clinical management, Acta Obstetrics and Gynecology Scandinavia, vol. 83, pp.818-826. Preston, S, Mahomed, K, Chadha, Y, Flenady, V, Gardener, G, Macphail, J, Conway, L, Koopmans, L, Stacey, T, Heazell, A, Fretts, R and Froen, F for the Fetal Movement Study Group and the International FEMINA collaboration. Clinical practice guidelines for management of decreased fetal movements. Consultation edition. Brisbane, August 2009. www.stillbirthalliance.org.au
3 Decreased Fetal Movement Feb-11 WACSClinProc1.12/10
ATTACHMENT 1 Algorithm for Women with Reduced Fetal Movement Review antenatal history for risk factors
Discuss with the Arrange USS for > 24 weeks gestation senior AFI, UA doppler, midwife/registrar growth within 24 CTG if over 30 weeks gestation hours. (as per Antenatal Electronic Fetal Documentation Monitoring Guideline Encourage WACSClinProc1.7) woman Review and to return ASAP if management plan perception of DFM developed Consider CTG if under 30 weeks by persists registrar or
< 24 weeks gestation Auscultate FH with doppler. If fetal heart reassuring: Reassure, document and discharge to usual antenatal care provider USS by consultant if unable to locate FHR with doppler.
First presentation No risk factors SFH within 2 cm Reassuring CTG
Repeat presentation
&/or
FH not detected
Non reassuring CTG
Risk factors
&/or
SFH not within 2 cm
&/or
CTG non reassuring Real time USS by registrar or consultant Urgent referral to registrar or consultant
4 Decreased Fetal Movement Feb-11 WACSClinProc1.12/10
Вам также может понравиться
- Nursing the NeonateОт EverandNursing the NeonateMaggie MeeksОценок пока нет
- Diagnosis of Preterm Labor and Overview of Preterm BirthДокумент15 страницDiagnosis of Preterm Labor and Overview of Preterm BirthKenny IncsОценок пока нет
- Fetal AssessmentДокумент59 страницFetal AssessmentBasharKeewanОценок пока нет
- Preterm Labor and DeliveryДокумент21 страницаPreterm Labor and DeliverydenekeОценок пока нет
- Fetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsОт EverandFetal Physiological Measurements: Proceedings of the Second International Conference on Fetal and Neonatal Physiological MeasurementsPeter RolfeОценок пока нет
- Dr. Rimonta F Gunanegara, SpogДокумент58 страницDr. Rimonta F Gunanegara, SpogJanetty TjandraОценок пока нет
- Fetal Healt Survillence SCOGДокумент55 страницFetal Healt Survillence SCOGCésar Gardeazábal100% (1)
- Neurological Deseases in PregnancyДокумент6 страницNeurological Deseases in PregnancyOdi KaiОценок пока нет
- 9fetal Well Being in PregnancyДокумент10 страниц9fetal Well Being in PregnancyuouoОценок пока нет
- Assessment of Fetal Well BeingДокумент46 страницAssessment of Fetal Well BeingAumrin Fathima100% (1)
- Low Birth Weight Baby and HyalineДокумент42 страницыLow Birth Weight Baby and Hyalineakhmad rizky subkiОценок пока нет
- Factors Affecting Maternal Perception of Fetal MovementsДокумент9 страницFactors Affecting Maternal Perception of Fetal MovementsNoraОценок пока нет
- 2023 OB/GYN Coding Manual: Components of Correct CodingОт Everand2023 OB/GYN Coding Manual: Components of Correct CodingОценок пока нет
- Miscarriage Early Pregnancy LossДокумент10 страницMiscarriage Early Pregnancy LossiwennieОценок пока нет
- Embryology and Congenital Anomalies of The Female Genital SystemДокумент42 страницыEmbryology and Congenital Anomalies of The Female Genital Systemvrunda joshiОценок пока нет
- Fetal Growth Restriction - ACOG 2019Документ23 страницыFetal Growth Restriction - ACOG 2019Adhitya Yudha MaulanaОценок пока нет
- Jurnal Inggris PDFДокумент4 страницыJurnal Inggris PDFTom PrasОценок пока нет
- Rhesus Iso ImmunizationДокумент12 страницRhesus Iso Immunizationapi-3705046Оценок пока нет
- Handbook of Current and Novel Protocols for the Treatment of InfertilityОт EverandHandbook of Current and Novel Protocols for the Treatment of InfertilityMichael H. DahanОценок пока нет
- Antepartum HaemorrhageДокумент48 страницAntepartum HaemorrhageRutashobya Manara TopManyota100% (1)
- Abnormal Cardiotocography - "CTG"Документ47 страницAbnormal Cardiotocography - "CTG"Ahmad Mustaqim SulaimanОценок пока нет
- 2019 PreeclampsiaДокумент19 страниц2019 PreeclampsiaMalexandra S CandoОценок пока нет
- Case History Ob & Gyne 4Документ6 страницCase History Ob & Gyne 4maksventileОценок пока нет
- Malformation of Female Reproductive SystemДокумент170 страницMalformation of Female Reproductive SystemKriti BanstolaОценок пока нет
- Abortion and Sterilization: Medical and Social AspectsОт EverandAbortion and Sterilization: Medical and Social AspectsJane E. HodgsonОценок пока нет
- Nancy E Fay MD Facog Division of Reproductive MedicineДокумент32 страницыNancy E Fay MD Facog Division of Reproductive MedicineAdityo MulyonoОценок пока нет
- Management of Neonatal HypoglycemiaДокумент14 страницManagement of Neonatal Hypoglycemiaece142Оценок пока нет
- Management of Preterm LaborДокумент2 страницыManagement of Preterm LaborpolygoneОценок пока нет
- Presentation Aids and HivДокумент27 страницPresentation Aids and HivLamnunnem HaokipОценок пока нет
- Keehbauch Menopause HRT 4.2.16 SCДокумент55 страницKeehbauch Menopause HRT 4.2.16 SCMuhammad AzkaОценок пока нет
- Nausea and Vomiting of Pregnancy and Hyperemesis GravidarumДокумент27 страницNausea and Vomiting of Pregnancy and Hyperemesis GravidarumxxdrivexxОценок пока нет
- Oxytocics and TocolyticsДокумент6 страницOxytocics and TocolyticsFarheen khanОценок пока нет
- Occipito-Posterior Position of The Fetal HeadДокумент8 страницOccipito-Posterior Position of The Fetal HeaduouoОценок пока нет
- Normal Labour in Obstetric2Документ17 страницNormal Labour in Obstetric2Tejasvi ChavdaОценок пока нет
- Bleeding During PregnancyДокумент8 страницBleeding During Pregnancyfernandezrachelle44Оценок пока нет
- Hemorrhagic Disease of Newborn PDFДокумент2 страницыHemorrhagic Disease of Newborn PDFIndah Paradifa SariОценок пока нет
- Pelvic TuberculosisДокумент11 страницPelvic TuberculosisAmalia Zulfa AmandaОценок пока нет
- Myop in PregnancyДокумент4 страницыMyop in PregnancySamuel WilliamsОценок пока нет
- Physiologicalchangesinpregnancy 170323142156Документ69 страницPhysiologicalchangesinpregnancy 170323142156madhu.B100% (1)
- MK Fetal Lie and Presentation (OBGY)Документ9 страницMK Fetal Lie and Presentation (OBGY)Moses Jr KazevuОценок пока нет
- Tmbool's Notes in Obstetrics and GynecologyДокумент113 страницTmbool's Notes in Obstetrics and GynecologyFrom HumanОценок пока нет
- Genital FistulaeДокумент15 страницGenital Fistulaesangeetha francisОценок пока нет
- Hypertension in Pregnancy PoltekesДокумент41 страницаHypertension in Pregnancy PoltekesKhoerunnisa SeptianiОценок пока нет
- Instrumental DeliveryДокумент25 страницInstrumental DeliveryAhmed ElmohandesОценок пока нет
- Puerpera L Mental DisordersДокумент13 страницPuerpera L Mental DisordersclarheenaОценок пока нет
- Ovarian TorsionДокумент48 страницOvarian Torsionmaria ilyasОценок пока нет
- Amniotic Fluid EmbolismДокумент18 страницAmniotic Fluid EmbolismmanjuОценок пока нет
- AFE, RUPTURE OF UTERUS, (Autosaved)Документ31 страницаAFE, RUPTURE OF UTERUS, (Autosaved)maezu100% (1)
- Infections of Female Genital TractДокумент67 страницInfections of Female Genital TractSana AftabОценок пока нет
- Division of Perinatology Department of Child Health Medical School University of Sumatera UtaraДокумент37 страницDivision of Perinatology Department of Child Health Medical School University of Sumatera UtaraJosephine IrenaОценок пока нет
- Queenan's Management of High-Risk Pregnancy: An Evidence-Based ApproachОт EverandQueenan's Management of High-Risk Pregnancy: An Evidence-Based ApproachОценок пока нет
- HELLP SyndromeДокумент3 страницыHELLP SyndromeWidyawati TjahjadiОценок пока нет
- Impey Obs and Gynae Revision Notes PDFДокумент9 страницImpey Obs and Gynae Revision Notes PDFRoiseОценок пока нет
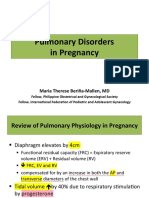
- Pulmonary Disorders in PregnancyДокумент49 страницPulmonary Disorders in PregnancyMara Medina - BorleoОценок пока нет
- Walhalla Gold MineДокумент1 страницаWalhalla Gold MineYwagar YwagarОценок пока нет
- Draft May 08 WES ProgramДокумент2 страницыDraft May 08 WES ProgramYwagar YwagarОценок пока нет
- Sydney 2008 MarchДокумент8 страницSydney 2008 MarchYwagar YwagarОценок пока нет
- Clinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeДокумент14 страницClinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeYwagar YwagarОценок пока нет
- Gold Coast 2008Документ1 страницаGold Coast 2008Ywagar YwagarОценок пока нет
- Clinical Tutorial 2008.11.05Документ31 страницаClinical Tutorial 2008.11.05Ywagar Ywagar100% (1)
- Recall Brisbane February 2008Документ7 страницRecall Brisbane February 2008Ywagar YwagarОценок пока нет
- GPДокумент3 страницыGPYwagar YwagarОценок пока нет
- Adelaide 13th September 2008Документ16 страницAdelaide 13th September 2008Ywagar YwagarОценок пока нет
- Adelaide April 2008Документ16 страницAdelaide April 2008Ywagar YwagarОценок пока нет
- AMC Clinical Exam Recall 8 Sep 2008 Melbourne Retest 1Документ7 страницAMC Clinical Exam Recall 8 Sep 2008 Melbourne Retest 1Ywagar YwagarОценок пока нет
- Brisbane July 2008 RecallДокумент11 страницBrisbane July 2008 RecallYwagar YwagarОценок пока нет
- Adel 2Документ24 страницыAdel 2Ywagar YwagarОценок пока нет
- Adelaide, 5 April, 2008: PaediatricsДокумент17 страницAdelaide, 5 April, 2008: PaediatricsYwagar YwagarОценок пока нет
- Melbourne 2008 Nov 8Документ10 страницMelbourne 2008 Nov 8Ywagar YwagarОценок пока нет
- MelbДокумент9 страницMelbYwagar YwagarОценок пока нет
- ACln2007!09!08MEL Retest Wd97Документ6 страницACln2007!09!08MEL Retest Wd97Ywagar YwagarОценок пока нет
- Adelaide 13th September 2008Документ16 страницAdelaide 13th September 2008Ywagar YwagarОценок пока нет
- Adelaide 13th September 2008Документ16 страницAdelaide 13th September 2008Ywagar YwagarОценок пока нет
- Melb RetestДокумент6 страницMelb RetestYwagar YwagarОценок пока нет
- Paediatrics:: Case 1nsionДокумент16 страницPaediatrics:: Case 1nsionYwagar YwagarОценок пока нет
- Brisbane, 11th October 2008Документ6 страницBrisbane, 11th October 2008Ywagar YwagarОценок пока нет
- To ReviseAug 22 AdelaideДокумент4 страницыTo ReviseAug 22 AdelaideYwagar YwagarОценок пока нет
- Melb RetestДокумент2 страницыMelb RetestYwagar YwagarОценок пока нет
- BrisДокумент9 страницBrisYwagar YwagarОценок пока нет
- Brisbane, 11th October 2008Документ6 страницBrisbane, 11th October 2008Ywagar YwagarОценок пока нет
- 9 August 08 Melbourne Clinical Exam RecallДокумент6 страниц9 August 08 Melbourne Clinical Exam RecallYwagar YwagarОценок пока нет
- Syd 1Документ11 страницSyd 1Ywagar YwagarОценок пока нет
- Melb RetestДокумент4 страницыMelb RetestYwagar YwagarОценок пока нет
- Clinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeДокумент14 страницClinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeYwagar YwagarОценок пока нет
- Euroncap 2017 Audi q5 DatasheetДокумент13 страницEuroncap 2017 Audi q5 DatasheetCosmin AnculiaОценок пока нет
- Introduction On Photogrammetry Paul R WolfДокумент33 страницыIntroduction On Photogrammetry Paul R Wolfadnan yusufОценок пока нет
- Mass, Weigth and Density IGCSEДокумент6 страницMass, Weigth and Density IGCSEsapiniОценок пока нет
- Feeg2003 L21Документ9 страницFeeg2003 L21jiales225Оценок пока нет
- A Ongc HRM Summer ProjectДокумент58 страницA Ongc HRM Summer ProjectAmit SunsaraОценок пока нет
- Key-Sentence Writing 1Документ23 страницыKey-Sentence Writing 1Thảo VyОценок пока нет
- Evolution of MISДокумент4 страницыEvolution of MISHarshitha PadmashaliОценок пока нет
- Job Hazard Analysis Form: Section A: Task InformationДокумент3 страницыJob Hazard Analysis Form: Section A: Task InformationHasnei NОценок пока нет
- Expansion ScrewsДокумент32 страницыExpansion ScrewsJomar PortadoОценок пока нет
- Colegio de San Gabriel Arcangel of Caloocan, IncДокумент7 страницColegio de San Gabriel Arcangel of Caloocan, IncKIRITO SALINASОценок пока нет
- Traina 250Wp PDFДокумент2 страницыTraina 250Wp PDFSherifImamОценок пока нет
- Mixing L 6-7Документ60 страницMixing L 6-7hyde2520015754Оценок пока нет
- Fuel Tank Truck Afd-091005-058Документ40 страницFuel Tank Truck Afd-091005-058cascade1100% (1)
- MH2732-Robotics Lab ManualДокумент50 страницMH2732-Robotics Lab Manualramzi ayadiОценок пока нет
- Ffu 0000034 01Документ8 страницFfu 0000034 01Karunia LestariОценок пока нет
- Vortex Based MathematicsДокумент14 страницVortex Based Mathematicssepsis19100% (2)
- Neo Neurophone Patrick FlanaganДокумент2 страницыNeo Neurophone Patrick FlanaganalexanderjfernandesОценок пока нет
- Wahabism - Bala SurajoДокумент17 страницWahabism - Bala SurajoAbu Muhammad50% (2)
- P1 - Duct Design IntroductionДокумент30 страницP1 - Duct Design IntroductionAndryx MartinezОценок пока нет
- Perbedaan Fermentasi Dan Respirasi Anaerob (Campbell Biology 12th Ed.)Документ4 страницыPerbedaan Fermentasi Dan Respirasi Anaerob (Campbell Biology 12th Ed.)Oppof7 OppoОценок пока нет
- Prof Budi Wiweko - Protokol Dan Pemantauan Stimulasi Ovarium SederhanaДокумент36 страницProf Budi Wiweko - Protokol Dan Pemantauan Stimulasi Ovarium SederhanaAnisanang BanjarОценок пока нет
- Ancient CivilizationsДокумент9 страницAncient CivilizationsMarienne LaoОценок пока нет
- CompAir 4-Pages SmartAir MasterДокумент4 страницыCompAir 4-Pages SmartAir MasterKaisar Ahmed BhuyanОценок пока нет
- Unit 2 - CT2Документ45 страницUnit 2 - CT2Jagrit DusejaОценок пока нет
- Gujarat-Ports Sector ReportДокумент17 страницGujarat-Ports Sector ReportK. Ashok Vardhan ShettyОценок пока нет
- Designing Hopping Animal PDFДокумент3 страницыDesigning Hopping Animal PDFAntonio Francisco Muñoz100% (1)
- 49728393Документ17 страниц49728393MarcoОценок пока нет
- Full Download Test Bank For Financial Reporting Financial Statement Analysis and Valuation 8th Edition PDF Full ChapterДокумент36 страницFull Download Test Bank For Financial Reporting Financial Statement Analysis and Valuation 8th Edition PDF Full Chaptervespersrealizeravzo100% (18)
- GENII - Nissan Patrol GQ & GU - RE4 4 Speed Diesel & Petrol - Lock Up Instructions-1Документ14 страницGENII - Nissan Patrol GQ & GU - RE4 4 Speed Diesel & Petrol - Lock Up Instructions-1Trav GilesОценок пока нет
- Detector de Fum Si Temperatura Apollo XP95-55000-885Документ2 страницыDetector de Fum Si Temperatura Apollo XP95-55000-885dorobantu_alexandruОценок пока нет