Академический Документы
Профессиональный Документы
Культура Документы
Tuberculosis Meningitis 2
Загружено:
Arie PrasetyowatiАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Tuberculosis Meningitis 2
Загружено:
Arie PrasetyowatiАвторское право:
Доступные форматы
Tuberculous Meningitis
Definition Tuberculous meningitis (TBM) is a chronic infection of the meninges caused by Mycobacterium tuberculosis. Pathogenesis Dissemination of bacilli to the meninges and brain occurs as a complication of the primary infection, or as a complication of an existing TB lesion (tuberculoma, miliary TB) or reactivation of a latent TB focus. Meningeal infection is then caused when a parameningeal caseous focus ruptures into the brain/spinal substance and subarachnoid space. A severe inflammatory response is elicited by mycobacterial components. A thick exudate, phlebitis, arteritis, thrombosis, infarction and obstruction of CSF flow are common findings. Complications include raised intracranial pressure, cerebral oedema, inappropriate antidiuretic hormone (ADH) secretion, hydrocephalus, brain infarcts, hemi- or quadriplegia, convulsions, deafness, blindness, mental retardation and other neurological sequelae. Diagnostic criteria Early diagnosis and treatment improves the prognosis. Clinical: History of contact with tuberculosis (not always present). Onset may be gradual with vague complaints of headache, irritability, weight loss and drowsiness. Examination may reveal signs of meningeal irritation, signs of raised intracranial pressure, convulsions, cranial nerve palsies, localising signs (such as hemipareses), altered level of consciousness or coma and choroidal tubercles. Degree of involvement is classified into 3 stages. Prognosis relates to the stage of the disease.
Stage 1: Non-specific signs, signs of meningeal irritation, conscious, rational, no focal neurological signs, no hydrocephalus. Stage 2: Confusion and/or focal neurological signs. Stage 3: Stupor, delirium, coma and/or neurological signs (hemiplegia). Investigations: It is often not possible to diagnose TBM on a single CSF examination. Often introduction of antibiotics misleads the findings. Lumbar puncture is hazardous if the patient has a focal neurological deficit or if fundoscopy shows papilloedema. In these circumstances, a C.A.T. brain scan is helpful, if available. Otherwise, it may be safer to start presumptive treatment with anti TB drugs when there are ample historical and clinical more evidences rather than risk lumbar puncture. CSF findings: May vary depending on the stage. Protein is markedly raised, glucose is moderately low, chloride is low and lymphocytes usually predominate. CSF adenosine deaminase may be raised (> 7 units/L). Gram stain is negative and acid-fast bacilli are seldom found. A bromide partition test may be helpful. (CSF bromide partition test ratio < 1.6). Bacilli may be cultured from the CSF but may take up to 46 weeks.
A Mantoux test if negative a BCG enhanced reaction test, and chest X-ray should always be done. A CT scan of the brain may be helpful.
Treatment objectives Early diagnosis and treatment. Eradication of the mycobacteria. Prevention and early treatment of complications. Symptomatic and supportive treatment. Education of parents and caregivers. BCG vaccine to newborn babies.
Treatment guidelines Management Monitor neurological status on a regular basis. Attend to nutritional status. Nasogastric feeding is usually needed initially. CSF shunting procedures or repeated lumbar punctures may be needed as part of the management of hydrocephalus. Monitor liver function. Most of the drugs used are hepatotoxic. Rifampicin + isoniazid (INH) + pyrazinamide + streptomycin Rifampicin, oral, 20 mg/kg/24 hours as a single daily dose. Isoniazid, oral, 20 mg/kg/24 hours as a single daily dose. Pyrazinamide, oral, 40 mg/kg/24 hours as a single daily dose; maximum 2 g per 24 hours. Streptomycin: 20-40mg/kg/24 hours as a single daily IM dose. 4-month Discontinue pyrazinamide. continuation Continue with rifampicin, isoniazid and using the doses phase: above. Steroids: Prednisone, oral, 24 mg/kg/24 hours in 3 divided doses for 46 weeks. Then taper to stop over 1421 days. Hydrocephalus: Acetazolamide, oral, 100 mg/kg/24 hours in 3 divided Refer non- communicating hydrocephalus doses; maximum 1 g/day. for ventriculo- peritoneal shunt urgently. AND Furosemide, oral, 12 mg/kg/24 hours as a single daily dose for at least 46 weeks. Convulsions: Diazepam, slow IV, 0.20.3 mg/kg, to control acute seizures. Maintenance: Phenobarbital, oral, 510 mg/kg/24 hours Comments All patients need physiotherapy Follow-up at clinic/hospital is essential. Rehabilitative measures.
Non-drug treatment
Drug treatment 2-month initial phase:
in 2 divided doses, until the patient is free of convulsions for 14 days. Taper to stop over 1 week. Raised intracranial Elevate head of bed + 15 degrees. Treat severe cerebral oedema/increased pressure or Maintain Paco2 at 2830 mmHg; intubate and ventilate if intracranial pressure if there is an acute cerebral oedema: necessary. deterioration of the level of consciousness. Mannitol, IV, 1g/kg administered over 1 hour. (Do not repeat.) 1 kPa = 7.5 mmHg; 1 mmHg x 0.133 = 1 Furosemide, IV, 1 mg/kg. (Do not repeat.) kPa Avoid fluid overload. Limit total daily fluid intake (IV + oral) not to exceed the maintenance requirements for Evidence that fluid restriction is beneficial is age. inconclusive.
Вам также может понравиться
- Pediatrics MS WordДокумент13 страницPediatrics MS WordSamhitha SharmaОценок пока нет
- Meningo Encephalitis DiscussionДокумент28 страницMeningo Encephalitis DiscussionVindu WadhwaniОценок пока нет
- Tuberculous MeningitisДокумент26 страницTuberculous MeningitispurbandaruОценок пока нет
- Pyogenic MeningitisДокумент46 страницPyogenic MeningitisShahnaaz ShahОценок пока нет
- Bacterial MeningitisДокумент51 страницаBacterial MeningitiscaseinrenninОценок пока нет
- Chapter IIДокумент34 страницыChapter IINycoОценок пока нет
- Cns InfectionДокумент53 страницыCns InfectionBernamai CalamОценок пока нет
- TB MeningitisДокумент13 страницTB Meningitisياسر كوثر هانيОценок пока нет
- TREATMENT Bacterial MeningitisДокумент32 страницыTREATMENT Bacterial MeningitisironОценок пока нет
- Meningitis in ChildrenДокумент27 страницMeningitis in Childrensai saiОценок пока нет
- Practice Essentials: Essential Update: New Guidelines From KDIGOДокумент13 страницPractice Essentials: Essential Update: New Guidelines From KDIGOPratama Aditya BiantoroОценок пока нет
- Empiric Therapy of CNS Infections Acute Bacterial Meningitis ABMДокумент6 страницEmpiric Therapy of CNS Infections Acute Bacterial Meningitis ABMSamsul BahriОценок пока нет
- L6105 - Toxoplasmosis Serebral 2022Документ37 страницL6105 - Toxoplasmosis Serebral 2022zqhg66yynfОценок пока нет
- Brain AbscessДокумент1 страницаBrain AbscessRolando AgustianОценок пока нет
- Brucellosis: ClassificationДокумент3 страницыBrucellosis: ClassificationAbdul-rhman AlmarshoodОценок пока нет
- Toxoplasmosis in HIV PatientsДокумент49 страницToxoplasmosis in HIV PatientsLily SolОценок пока нет
- Meningitis in ChildrenДокумент17 страницMeningitis in ChildrenNurul NajibОценок пока нет
- Epidemiology, Clinical Presentation and ManagementДокумент14 страницEpidemiology, Clinical Presentation and ManagementPrincewill SeiyefaОценок пока нет
- Neonatal Seizures and Management: Dhaka Sishu Hospital BangladeshДокумент19 страницNeonatal Seizures and Management: Dhaka Sishu Hospital BangladeshGoha BashaОценок пока нет
- Q&A OsloДокумент9 страницQ&A OslosyukriОценок пока нет
- TB MeningitisДокумент18 страницTB Meningitisjesa34Оценок пока нет
- Opportunistic Infections: Dr. Baldev S. PrajapatiДокумент69 страницOpportunistic Infections: Dr. Baldev S. PrajapatiZazzZaffaОценок пока нет
- Bab I Pendahuluan Tuberculous Meningitis: Diagnosis and Treatment OverviewДокумент14 страницBab I Pendahuluan Tuberculous Meningitis: Diagnosis and Treatment OverviewInalОценок пока нет
- PEDIA aPSGNДокумент2 страницыPEDIA aPSGNiSmayli (smyle-smayl)Оценок пока нет
- Clinical Features: - Initial Symptoms in Patients With MeningitisДокумент12 страницClinical Features: - Initial Symptoms in Patients With Meningitisyuii_48Оценок пока нет
- Meningococcemia: Neisseria Meningitidis - Is An EncapsulatedДокумент19 страницMeningococcemia: Neisseria Meningitidis - Is An EncapsulatedcarolinecayasaОценок пока нет
- HIV Infection - Opportunistic InfectionsДокумент21 страницаHIV Infection - Opportunistic InfectionszawadiОценок пока нет
- CC Junsay Nicole Xyza T. Learning Interaction FormДокумент10 страницCC Junsay Nicole Xyza T. Learning Interaction FormNicole Xyza JunsayОценок пока нет
- Pediatric Sepsis Topic DiscussionДокумент5 страницPediatric Sepsis Topic Discussionapi-602288180Оценок пока нет
- Meningitis and Encephalitis: Samantha Noll June 11, 2015Документ45 страницMeningitis and Encephalitis: Samantha Noll June 11, 2015galihОценок пока нет
- Group 25 BronchopneumoniaДокумент22 страницыGroup 25 BronchopneumoniaMichael AdjeiОценок пока нет
- Meningitis Beyond The Neonatal AgeДокумент51 страницаMeningitis Beyond The Neonatal AgeBeamlak Getachew WoldeselassieОценок пока нет
- 5 Neurological ManifestationsДокумент30 страниц5 Neurological ManifestationsCalvin ChisangoОценок пока нет
- Neurological EmergenciesДокумент47 страницNeurological EmergenciesStellate Repentance100% (1)
- TB Management Final1Документ23 страницыTB Management Final1Aanchal JainОценок пока нет
- CPPP PP P PP PPPPPPP PPДокумент3 страницыCPPP PP P PP PPPPPPP PPangelieballesterosОценок пока нет
- ENLS Meningitis and Encephalitis ProtocolДокумент20 страницENLS Meningitis and Encephalitis ProtocolFransiskus MikaelОценок пока нет
- CNS InfectionДокумент36 страницCNS InfectionIkaDian PuspitanzaОценок пока нет
- Medicine RotatationbookletДокумент20 страницMedicine RotatationbookletJanelle JosephsОценок пока нет
- MENINGITIS DR Syad Akram Ali 01-12-2014Документ95 страницMENINGITIS DR Syad Akram Ali 01-12-2014Gopireddy Sivakarthik ReddyОценок пока нет
- HIV-Opportunistic Infection (Autosaved)Документ22 страницыHIV-Opportunistic Infection (Autosaved)Jonathan RyanОценок пока нет
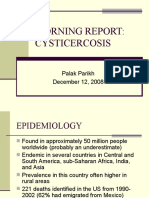
- Morning Report: Cysticercosis: Palak Parikh December 12, 2008Документ29 страницMorning Report: Cysticercosis: Palak Parikh December 12, 2008Jayarani AshokОценок пока нет
- 7902-002 Investigators Meeting Material 08 Feb 2019Документ39 страниц7902-002 Investigators Meeting Material 08 Feb 2019FERNANDO BUSTAMANTE MORALESОценок пока нет
- Meningitis 222Документ28 страницMeningitis 222alemante tafeseОценок пока нет
- HIV Infection and The CNS: Stephen J. Gluckman, M.DДокумент36 страницHIV Infection and The CNS: Stephen J. Gluckman, M.DLuna WhiteОценок пока нет
- Meningitis PresentationДокумент41 страницаMeningitis PresentationO'Mark AndrewsОценок пока нет
- TOXOPLASMOSIS (Internal Medicine)Документ3 страницыTOXOPLASMOSIS (Internal Medicine)Moses Jr KazevuОценок пока нет
- Tuberculosis of Spine: Current Views in Diagnosis and ManagementДокумент13 страницTuberculosis of Spine: Current Views in Diagnosis and ManagementNurul HidayahОценок пока нет
- Clinical Science Session Infeksi SSPДокумент44 страницыClinical Science Session Infeksi SSPraisa cesardaОценок пока нет
- Bacterial Meningitis in AdultsДокумент55 страницBacterial Meningitis in AdultsfjnaressiОценок пока нет
- Meningitis in Children: Shakilu J MD University of DodomaДокумент47 страницMeningitis in Children: Shakilu J MD University of DodomaGimson kanimbaОценок пока нет
- Department of Health and Family Welfare Govt. of West BengalДокумент35 страницDepartment of Health and Family Welfare Govt. of West Bengalswagato deyОценок пока нет
- Q&A Oslo Revisi 61023Документ10 страницQ&A Oslo Revisi 61023syukriОценок пока нет
- Meningitis PDFДокумент10 страницMeningitis PDFAlfatahadi SОценок пока нет
- Nephrotic Syndrome in Children: Supervised By: Dr. Pulung M. Silalahi Sp.A Presented By: Anna ListianaДокумент38 страницNephrotic Syndrome in Children: Supervised By: Dr. Pulung M. Silalahi Sp.A Presented By: Anna ListianaAnna ListianaОценок пока нет
- Nephrotic Syndrome PDFДокумент36 страницNephrotic Syndrome PDFanwar jabariОценок пока нет
- Meningitis - 2018Документ55 страницMeningitis - 2018Abraham Anaely100% (1)
- Tuberculoma: Case ReportДокумент34 страницыTuberculoma: Case ReportitaОценок пока нет
- On Co EmergenciesДокумент6 страницOn Co EmergenciessdfОценок пока нет
- Mabel atДокумент5 страницMabel atAlec SyОценок пока нет
- Section 17 - 30 of Nursing JurisprudenceДокумент3 страницыSection 17 - 30 of Nursing JurisprudenceAlec SyОценок пока нет
- DiarrheaДокумент4 страницыDiarrheaAlec SyОценок пока нет
- Presentation 1Документ9 страницPresentation 1Alec SyОценок пока нет
- Health Care Delivery and Nursing PracticeДокумент36 страницHealth Care Delivery and Nursing PracticeAlec SyОценок пока нет
- Health Care Delivery and Nursing PracticeДокумент36 страницHealth Care Delivery and Nursing PracticeAlec SyОценок пока нет
- Health Care Delivery and Nursing PracticeДокумент36 страницHealth Care Delivery and Nursing PracticeAlec SyОценок пока нет