Академический Документы
Профессиональный Документы
Культура Документы
Children's Early Warning Tool
Загружено:
Ywagar YwagarИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Children's Early Warning Tool
Загружено:
Ywagar YwagarАвторское право:
Доступные форматы
Tasmanian Health Organisation - North
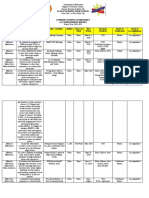
LAUNCESTON GENERAL HOSPITAL SDMS Id No.: P2012/0454-001 LGH Procedure No.: 40/12
Childrens Early Warning Tool (CEWT) Use LGH Procedure
Application: This procedure applies to all staff involved in the care of paediatric patients in the Launceston General Hospital (LGH). The procedure directly affects family members and patients. CEO Tasmanian Health Organisation - North 14 September 2012 Quality Improvement Nurse, Paediatrics and Neonate Units LGH 14 September 2015 1 N/A
Approved by: Effective Date: Custodian and Review Responsibility: Review Date: Version: Replaces:
Background
It is important to alleviate risk to patient safety by implementing best practice and national recommendations as described in the National Consensus Statement: Essential Elements for Recognising and Responding to Clinical Deterioration. The National Safety and Quality Health Service Standards include the standard Recognising and Responding to Clinical Deterioration in Acute Health Care which describes the systems and processes to be implemented by health service organisations to respond effectively to patients when their clinical condition deteriorates.
Procedure
The Childrens Early Warning Tool (CEWT) is used for the early identification and management of clinical deterioration of paediatric patients in LGH. It is a component of the Tasmanian Health Organisation Norths early recognition and response system DANGERS (Doctors and Nurses Emergency Response System). At all times, clinical staff are responsible for the patient and for delivering appropriate treatment for their condition, within their scope of practice. The CEWT observation chart is a tool to support assessment and together with the clinical emergency response system is designed to enable health care workers to confidently call for help when they and their patient need it.
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
1 of 7
The CEWT observation chart must be used for all paediatric patients across LGH, including all paediatric patients in the Department of Emergency Medicine. Exclusions are paediatric patients in the following areas: Intensive Care Unit (ICU) Operating Room Suite (ORS) Day Procedure Unit (DPU)
The CEWT chart is based on a track and trigger scoring system allowing for multiple assessment elements to formulate an escalation process. The numeric CEWT score is colour coded to allow ease of identification for corresponding actions to be taken. The age appropriate CEWT chart must be used: < 1 year 1 4 years 5 11 years 12 years and older
Clinical Alert
The CEWT chart may not be appropriate when a patient has been diagnosed as actively dying or in the terminal phase where an end of life pathway may be suitable.
Observations
All paediatric patients must have a full CEWT score and a pain score taken: on admission once per shift (minimum 8th hourly) and if the patient is deteriorating (increasing score or you are concerned about the patient).
For abnormal observations you must continue to check until normal. Aside from the above, do appropriate observations at an appropriate frequency for the patients clinical status.
Clinical Alert
A full CEWT score = respiratory rate oxygen saturation respiratory distress blood pressure temperature heart rate
If an observation moves into one of the shaded areas on the CEWT chart, add up the patients full score and initiate the actions required for that colour, unless modifications have been made. Where a Clinical Pathway sets out a schedule for varying the frequency of observations, a medical officer (following consultation with the consultant) may document this as consistent with clinical pathway for [insert title of pathway] in the medical record. Varying observation frequency in this manner may only occur provided that this does not reduce frequency further than a minimum of 8 th hourly.
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
2 of 7
Observations must be recorded on the CEWT chart in black or blue ink at the time they are taken. When graphing observations, place a dot (.) in the appropriate box and join to the preceding dot. For blood pressure use the symbols indicated on the chart. All paediatric patients are to be visually checked every 30 minutes (including at night) with rise and fall of chest during respiration observed. Interventions and observations must not be withheld or delayed in an attempt to avoid disturbing the sleeping patient. Any clinical staff member can increase the frequency of observations from the required minimum. A full CEWT score must be documented on patients if a family member or carer is concerned about deterioration in the patients clinical condition. A manual reading should be obtained if the automated blood pressure reading is outside the patients usual range (high or low) or if the patient has an irregular heart rate.
Modifications
Modifications to the parameters for individual patients can only be made by the admitting registrar or consultant. These must be clearly documented on the CEWT chart in the modification section and reviewed at least every 24 hours by the home team registrar or consultant. Changes to the modifications must be clearly documented on a new CEWT chart. Special treatment plans which alter calling criteria such as not for cardio-pulmonary resuscitation or an Advance Care Plan/Directive must also be documented in the patients medical record.
Specific Observation Charts
When a specific observation (e.g. respiratory assessment, neurological observations, blood product transfusion) chart is required, a full set of observations must also be documented on the CEWT chart 8th hourly as a minimum. If any of the observations (regardless of which chart they are recorded on) breach CEWT parameters then the appropriate escalation response and actions must be initiated.
Transfer of Patients
Prior to transfer from any exclusion area listed above to 4K a full CEWT score must be recorded on the CEWT chart. If the observations fall into any of the coloured zones on the chart the patient must be medically reviewed and cleared for transfer and a management plan documented in the medical record. Clinical handover must include any breaches of CEWT parameters and ongoing management. All paediatric patients transferred from ORS, ICU, and DPU must have a full CEWT score assessed 4 hourly until clinically stable.
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
3 of 7
On return to 4K from specialised procedural areas (including ORS, DPU, Cardiac Cath Lab) all post procedure or post anaesthetic observations must be documented on the CEWT chart. Inter-facility transfer requirements at a minimum are to include: Clinical handover using ISOBAR Management plan Relevant clinical charts (copies) Transfer letters from relevant staff Own medications, private Xrays Details of follow-up Relevant results (copies) Discharge medications (if required
Paediatric patients may be required to leave the ward or area to attend diagnostic or other support services within or external to the LGH. Refer to Escorting of Inpatients Within and External to the Launceston General Hospital (LGH): LGH Policy and Radiology Escort of Patients: LGH Policy.
Management Plans
Management plans must be clearly documented by the home team so each health care team member understands their responsibilities, and includes orders for: frequency and type of observations expected nursing and allied health interventions other therapy and interventions investigations and when notification is required re condition change
Escalation Protocol
Clinical staff must identify deteriorating paediatric patients who meet the parameters for initiating the escalation protocol and complete the actions required for that level of escalation. In caring for patients who are deteriorating it is important to: recognise that CEWT parameters have been triggered initiate basic treatment including review of oxygen requirements and patient position, reassurance systematically assess the patient seek senior assistance early as per the escalation actions required increase observation frequency and level of care as per the escalation actions required communicate situation clearly with RN in charge activate emergency call if criteria met
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
4 of 7
There are four escalation levels in response to breaches in the CEWT parameters. For each escalation level the frequency of observations must be increased at a minimum as below and the corresponding actions required on the CEWT chart completed. Interventions by clinical staff in response to a breach of CEWT parameters are to be recorded on the CEWT chart (see chart for instructions).
Score 1-3 Increased Surveillance
1 Consider increasing frequency of observations to a minimum of 4/24 or more frequently if clinically indicated, until observations stable (i.e. when they fall into the white zones of the CEWT chart), then return to patients usual frequency.
Score 4-5 RMO/Intern Review (in consultation with senior nurse)
1 Record observations at least once every 30 minutes to one hour for 2 hours until observations stable then return to patients usual frequency.
Score 6-7 Clinical Review by Paediatric Registrar and Home Team Registrar
1 2 3 4 5 While waiting for review, assess observations at least every 30 minutes or as clinically indicated Following clinical review the patients observations must be assessed as prescribed and documented by the attending medical officer If at any time the patients observations breach Clinical Review parameters then recommence the above process from step 1 Document on CEWT chart and in the medical record that a clinical review has been requested. The home team Registrar must attend within 15 minutes. If the patient is not reviewed within 15 minutes or if clinically indicated initiate a Code Blue emergency call. If the child is under a surgical or medical team and cannot be reviewed by the home team registrar within 15 minutes then they should be reviewed by the Paediatric Registrar or Paediatrician within that time frame, as well as contacting the home team consultant. If the patients condition has improved prior to review they must still be reviewed by the home team Registrar and a management plan documented in the medical record. NOTE for paediatric patients under surgical/medical teams contact the home team registrar within hours (0800-1640), after hours contact the rostered medical/surgical registrar as per the Switchboard Bulletin escalate as per point 5 above if unable to be reviewed by the nominated registrar.
Score 8+ Code Blue Call
1 2 Record observations as clinically indicated If the patient meets the criteria for a Code Blue Call, activate the Code Blue by dialling 222 Clearly State:
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
5 of 7
Code Blue Call and Paediatric and Location NOTE: Within business hours the home team Registrar must be notified by the ward staff and attend the Code Blue.
Communication and Documentation following activation of rapid response system
When escalating care staff must use the communication tool ISOBAR to provide a standardised, sequential approach to give and receive handover. Documentation in the patients medical record following activation of Clinical Review or Code Blue call must include: date/time name of staff notified reason for call time patient is seen for Clinical Review or Code Blue call treatment arising from Clinical Review or Code Blue call outcomes following treatment management plan
Evaluation
Performance measures for CEWT are included in the overarching recognition and response system for THO-North healthcare facilities; these can be found in the DANGERS procedure document. Performance measures will be evaluated six monthly to annually and reports made available to relevant staff within facilities and clinical units to inform improvement to systems. The responsibility for co-ordination of collection and analysis of evaluation data is with the Paediatric Quality Improvement Nurse and Clinical Nurse Educator, Clinical Effectiveness Service, Resuscitation Advisory Group (RAG), and Life Support Coordinator.
Responsibilities/Delegations
All LGH clinical staff and visiting practitioners are responsible for compliance with the requirements outlined in this procedure document. Managers of clinical staff should ensure their staff are able to access and carry out the actions that fulfil the CEWT procedure.
Definitions
Clinical staff: all staff who provide direct patient care (nursing, medical and allied health). Consultant: the senior medical practitioner (visiting medical officer or staff specialist) who has primary responsibility for the patient during the admission.
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
6 of 7
Escalation protocol: the protocol that sets out the response required for different levels of abnormal physiological measurements or other observed deterioration. Must: indicates a mandatory action requiring compliance. Patient: for the purposes of this document a person aged 17 years or younger is considered a paediatric patient unless otherwise specified by the admitting doctor. Track and trigger scoring system: an observation charting system used to record routine periodic measurement of observations graphically so trends can be tracked visually and which incorporates predetermined parameters (triggers) beyond which a standard set of actions is required by health professionals if a patients observations breach this parameter.
Related Documents/Legislation
Escorting of Inpatients Within and External to the Launceston General Hospital: LGH Policy Radiology Escort of Patients: LGH Procedure LGH Code Blue response to medical emergency LGH Procedure Procedure for Doctors and Nurses General Emergency Response System (DANGERS) National Consensus Statement: Essential Elements for Recognising and Responding to Clinical Deterioration National Safety and Quality Health Service Standards
Prepared by Through Through Cleared by
Malcolm Gulliver Michael Sherring Dr Neil Atherton THO-N Executive Committee John Kirwan
Quality Improvement Nurse Clinical Nurse Educator Paediatrician
6348 7654 6348 8972
24 July 2012 24 July 2012 13 September 2012
CEO Tasmanian Health Organisation - North
6348 7043
14 September 2012
AUTHORISED BY CHIEF EXECUTIVE OFFICER ... John Kirwan 17 September 2012 Date
Note: PLEASE DESTROY PRINTED COPIES. The electronic version of this Procedure is the approved and current version and is located on the departments intranet. Any printed version is uncontrolled and therefore not current. Page
7 of 7
Вам также может понравиться
- The Room - SartreДокумент14 страницThe Room - SartreYue Biohazard100% (1)
- Enhancing Nurses Pain Assessment To Improve.11Документ2 страницыEnhancing Nurses Pain Assessment To Improve.11Na d'Nazaie CodeОценок пока нет
- Online Hospital Management SystemДокумент2 страницыOnline Hospital Management Systemyay guruОценок пока нет
- SopДокумент3 страницыSopmrchilliciousОценок пока нет
- 15-Clinical Pathway Audit Tools A Systematic Review - Cari RefДокумент20 страниц15-Clinical Pathway Audit Tools A Systematic Review - Cari RefKang Heru Angon PitekОценок пока нет
- Highest Efficiencies For Various Industrial Applications: PumpsДокумент8 страницHighest Efficiencies For Various Industrial Applications: Pumpsahmed MareiОценок пока нет
- OGJ Worldwide Refining Survey 2010Документ67 страницOGJ Worldwide Refining Survey 2010Zahra GhОценок пока нет
- Hospital To Hospital Transfers Marina Rivers April 12Документ12 страницHospital To Hospital Transfers Marina Rivers April 12Flossie SingletonОценок пока нет
- Generalized SAP BI Unit Test Case TemplatesДокумент6 страницGeneralized SAP BI Unit Test Case TemplateswaseemqaОценок пока нет
- Department of Management Studies: Control ChartsДокумент12 страницDepartment of Management Studies: Control ChartsmaninderОценок пока нет
- LiverpoolIntra-Hospital Transfer of ICU PatientsДокумент8 страницLiverpoolIntra-Hospital Transfer of ICU PatientsInnas DoankОценок пока нет
- Statistical Process Control Using Control ChartsДокумент28 страницStatistical Process Control Using Control ChartsTARUN MAHAWERОценок пока нет
- SPC Charts - Statistical Process Control Charts PDFДокумент6 страницSPC Charts - Statistical Process Control Charts PDFMutahir KhanОценок пока нет
- The Royal Children HospitalДокумент8 страницThe Royal Children HospitalrenystrawberryОценок пока нет
- Domain 16 - Improving The Testing ProcessДокумент21 страницаDomain 16 - Improving The Testing Processapi-19934187Оценок пока нет
- Quality AssuranceДокумент43 страницыQuality Assurancekanika100% (1)
- BEd, Aut-2018Документ25 страницBEd, Aut-2018Karam Ali50% (2)
- Glossary Health TeccnologyДокумент4 страницыGlossary Health TeccnologyreneportilloОценок пока нет
- Strategies To Improve Handoff CommunicationДокумент2 страницыStrategies To Improve Handoff CommunicationJames SimmonsОценок пока нет
- Using Data For ImprovmentДокумент52 страницыUsing Data For ImprovmentasperijonОценок пока нет
- Morbidity and Mortality Conference ManualДокумент22 страницыMorbidity and Mortality Conference Manualkelly_ann23Оценок пока нет
- Hospital Management SystemДокумент3 страницыHospital Management SystemRida beygОценок пока нет
- Bi TestingДокумент11 страницBi TestingwaseemqaОценок пока нет
- Advence Hospital Management System PDFДокумент6 страницAdvence Hospital Management System PDFMd Nazmul IslamОценок пока нет
- Data Warehouse and Business Intelligence Testing: Challenges, Best Practices & The SolutionДокумент15 страницData Warehouse and Business Intelligence Testing: Challenges, Best Practices & The SolutionAnonymous S5fcPaОценок пока нет
- Clinical Audit GuideДокумент13 страницClinical Audit Guidewassie gebiОценок пока нет
- Hospital Management System Final ProjectДокумент37 страницHospital Management System Final Project02 Sanket MahureОценок пока нет
- EvaluationprogramplanДокумент32 страницыEvaluationprogramplanapi-523878990Оценок пока нет
- Asl Testing - Template Test PlanДокумент12 страницAsl Testing - Template Test PlanBalaji ElanchezhiyanОценок пока нет
- Nursing Documentation Audit The Effect oДокумент10 страницNursing Documentation Audit The Effect opita romawatiОценок пока нет
- Assessment and Re-Assessment of Patients According To The Scope of ServiceДокумент9 страницAssessment and Re-Assessment of Patients According To The Scope of Servicegiya nursingОценок пока нет
- Define Medical Audit. Describe The Conditions, Prerequisites & Steps For Conducting Medical Audit in A General HospitalДокумент15 страницDefine Medical Audit. Describe The Conditions, Prerequisites & Steps For Conducting Medical Audit in A General HospitalAbdul RahamanОценок пока нет
- A Meta Analysis of The Effects of Resistance Training On Blood S 2020 MidwifДокумент10 страницA Meta Analysis of The Effects of Resistance Training On Blood S 2020 Midwifriska yolandaОценок пока нет
- A Project Proposal On Hospital Management System in JavaДокумент2 страницыA Project Proposal On Hospital Management System in JavaPirzada SwatiОценок пока нет
- 38 SOP ICT DepartmentДокумент19 страниц38 SOP ICT Departmentelmore kakaОценок пока нет
- Mod2 - Ch3 - Health IndicatorsДокумент13 страницMod2 - Ch3 - Health IndicatorsSara Sunabara100% (1)
- Ways To Improve The Health SystemДокумент18 страницWays To Improve The Health SystemB I N SОценок пока нет
- Principles of Oncology and Outline of ManagementДокумент78 страницPrinciples of Oncology and Outline of ManagementPavan JonnadaОценок пока нет
- Clinical Audit For Medical StudentsДокумент6 страницClinical Audit For Medical StudentsAmal SaeedОценок пока нет
- NABH Assessment - Institutional Ethics CommitteesДокумент4 страницыNABH Assessment - Institutional Ethics CommitteesAmitKumarОценок пока нет
- HIS EnglishДокумент53 страницыHIS Englishkgg1987Оценок пока нет
- Seminar JCI - 9 Feb 2012Документ16 страницSeminar JCI - 9 Feb 2012Mahardika PertiwiОценок пока нет
- Suggested Healthcare GoalsДокумент3 страницыSuggested Healthcare GoalsYousef Al-AmeenОценок пока нет
- Nabl 153Документ14 страницNabl 153Ziaul HaqueОценок пока нет
- Clinical Chart Audit STDДокумент31 страницаClinical Chart Audit STDNoureen ZawarОценок пока нет
- Course Manual - NGNДокумент12 страницCourse Manual - NGNjugulkОценок пока нет
- Job Responsibilities of Different Health People PDFДокумент114 страницJob Responsibilities of Different Health People PDFRuben Paul C RajОценок пока нет
- MDS G2Документ133 страницыMDS G2mohamed radwanОценок пока нет
- Self Assessment Toolkit 4thДокумент107 страницSelf Assessment Toolkit 4thDrPankaj MittalОценок пока нет
- Lecture Modules 1-7 (Healthcare Database Management & Design) (Systems Analysis) (PC)Документ165 страницLecture Modules 1-7 (Healthcare Database Management & Design) (Systems Analysis) (PC)MarkBelarminoОценок пока нет
- Clinic Supervisors Manual PDFДокумент202 страницыClinic Supervisors Manual PDFnawaflehОценок пока нет
- Synthesis PosterДокумент1 страницаSynthesis Posterapi-483044745Оценок пока нет
- HmisДокумент14 страницHmis166873100% (1)
- 2007 International Patient Safety GoalsДокумент1 страница2007 International Patient Safety GoalsElias Baraket FreijyОценок пока нет
- Six Sigma Yellow Belt Project CharterДокумент2 страницыSix Sigma Yellow Belt Project CharterBRUNO ADRIEL ZAMORA FERNÁNDEZОценок пока нет
- Hospital Emergency Response Checklist EngДокумент26 страницHospital Emergency Response Checklist EngRaniОценок пока нет
- Minimum Service Delivery Standards (MSDS) For Hospitals in Sindh ProvinceДокумент3 страницыMinimum Service Delivery Standards (MSDS) For Hospitals in Sindh Provinceimran82aliОценок пока нет
- Implementation Guidelines For The Canadian Emergency Department Triage & Acuity Scale (CTAS)Документ27 страницImplementation Guidelines For The Canadian Emergency Department Triage & Acuity Scale (CTAS)Jery JsОценок пока нет
- Clinical Safety Data Management AE SAE ADR ReportingДокумент10 страницClinical Safety Data Management AE SAE ADR ReportingIvan KolevОценок пока нет
- Process MapДокумент7 страницProcess Mapapi-535002543100% (1)
- Recall Brisbane February 2008Документ7 страницRecall Brisbane February 2008Ywagar YwagarОценок пока нет
- Sydney 2008 MarchДокумент8 страницSydney 2008 MarchYwagar YwagarОценок пока нет
- Walhalla Gold MineДокумент1 страницаWalhalla Gold MineYwagar YwagarОценок пока нет
- Clinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeДокумент14 страницClinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeYwagar YwagarОценок пока нет
- Gold Coast 2008Документ1 страницаGold Coast 2008Ywagar YwagarОценок пока нет
- Draft May 08 WES ProgramДокумент2 страницыDraft May 08 WES ProgramYwagar YwagarОценок пока нет
- GPДокумент3 страницыGPYwagar YwagarОценок пока нет
- Adel 2Документ24 страницыAdel 2Ywagar YwagarОценок пока нет
- Brisbane, 11th October 2008Документ6 страницBrisbane, 11th October 2008Ywagar YwagarОценок пока нет
- Brisbane July 2008 RecallДокумент11 страницBrisbane July 2008 RecallYwagar YwagarОценок пока нет
- Adelaide April 2008Документ16 страницAdelaide April 2008Ywagar YwagarОценок пока нет
- AMC Clinical Exam Recall 8 Sep 2008 Melbourne Retest 1Документ7 страницAMC Clinical Exam Recall 8 Sep 2008 Melbourne Retest 1Ywagar YwagarОценок пока нет
- Clinical Tutorial 2008.11.05Документ31 страницаClinical Tutorial 2008.11.05Ywagar Ywagar100% (1)
- Adelaide, 5 April, 2008: PaediatricsДокумент17 страницAdelaide, 5 April, 2008: PaediatricsYwagar YwagarОценок пока нет
- Adelaide 13th September 2008Документ16 страницAdelaide 13th September 2008Ywagar YwagarОценок пока нет
- Adelaide 13th September 2008Документ16 страницAdelaide 13th September 2008Ywagar YwagarОценок пока нет
- Adelaide 13th September 2008Документ16 страницAdelaide 13th September 2008Ywagar YwagarОценок пока нет
- Melbourne 2008 Nov 8Документ10 страницMelbourne 2008 Nov 8Ywagar YwagarОценок пока нет
- ACln2007!09!08MEL Retest Wd97Документ6 страницACln2007!09!08MEL Retest Wd97Ywagar YwagarОценок пока нет
- Brisbane, 11th October 2008Документ6 страницBrisbane, 11th October 2008Ywagar YwagarОценок пока нет
- MelbДокумент9 страницMelbYwagar YwagarОценок пока нет
- Melb RetestДокумент6 страницMelb RetestYwagar YwagarОценок пока нет
- To ReviseAug 22 AdelaideДокумент4 страницыTo ReviseAug 22 AdelaideYwagar YwagarОценок пока нет
- BrisДокумент9 страницBrisYwagar YwagarОценок пока нет
- Melb RetestДокумент4 страницыMelb RetestYwagar YwagarОценок пока нет
- Melb RetestДокумент2 страницыMelb RetestYwagar YwagarОценок пока нет
- Paediatrics:: Case 1nsionДокумент16 страницPaediatrics:: Case 1nsionYwagar YwagarОценок пока нет
- Syd 1Документ11 страницSyd 1Ywagar YwagarОценок пока нет
- 9 August 08 Melbourne Clinical Exam RecallДокумент6 страниц9 August 08 Melbourne Clinical Exam RecallYwagar YwagarОценок пока нет
- Clinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeДокумент14 страницClinical Recall 17 May 2008 Melbourne: AMC Feedback: Sudden Infant Death SyndromeYwagar YwagarОценок пока нет
- Vertical Transportation in BuildingsДокумент46 страницVertical Transportation in BuildingsHIMA MiniОценок пока нет
- Numerical Modelling of Brine Dispersion in Shallow Coastal WatersДокумент13 страницNumerical Modelling of Brine Dispersion in Shallow Coastal WatersIAEME PublicationОценок пока нет
- Surveys For Maint'Ce ClassДокумент7 страницSurveys For Maint'Ce ClassSuhe EndraОценок пока нет
- La Paz National High SchoolДокумент19 страницLa Paz National High SchoolBon Ivan FirmezaОценок пока нет
- Hello!: I Am Sir DeanДокумент30 страницHello!: I Am Sir DeanDean MalaluanОценок пока нет
- Complications of Diabetes MellitusДокумент46 страницComplications of Diabetes MellitusAbhijith MenonОценок пока нет
- 10 Major Sulfuric Acid Industrial Applications - WorldOfChemicalsДокумент9 страниц10 Major Sulfuric Acid Industrial Applications - WorldOfChemicalsFarhad MalikОценок пока нет
- Lipoma in Submandibular Region - A Case ReportДокумент4 страницыLipoma in Submandibular Region - A Case Reportmaxfac2010Оценок пока нет
- POFL Unit 1 Status QUO pp.1-37Документ38 страницPOFL Unit 1 Status QUO pp.1-37AruОценок пока нет
- DemolitionДокумент25 страницDemolitionusler4u100% (1)
- Financial Problems Are Commonly Faced by EveryoneДокумент2 страницыFinancial Problems Are Commonly Faced by EveryoneGrace Ann Mancao PototОценок пока нет
- Fitting in and Fighting Back: Stigma Management Strategies Among Homeless KidsДокумент24 страницыFitting in and Fighting Back: Stigma Management Strategies Among Homeless KidsIrisha AnandОценок пока нет
- Yuasa NPL Range: VRLA BatteriesДокумент2 страницыYuasa NPL Range: VRLA BatteriesVuro BegaОценок пока нет
- Different Types of FermentationДокумент26 страницDifferent Types of FermentationCats and DogОценок пока нет
- L-6th Sem (Eng Notes) Law Relating To Women and ChildДокумент52 страницыL-6th Sem (Eng Notes) Law Relating To Women and ChildCuriae corporate consultantsОценок пока нет
- Thyroid OphthalmopathyДокумент59 страницThyroid OphthalmopathyLavanya MadabushiОценок пока нет
- Telecommunications GroundingДокумент24 страницыTelecommunications GroundingMike FordealsОценок пока нет
- Machine Design II: Prof. K.Gopinath & Prof. M.M.MayuramДокумент4 страницыMachine Design II: Prof. K.Gopinath & Prof. M.M.Mayurampredrag10Оценок пока нет
- Weigh Bridge Miscellaneous Items DetailsДокумент1 страницаWeigh Bridge Miscellaneous Items DetailsChandan RayОценок пока нет
- How To Self-Decontaminate After A Radiation Emergency - CDCДокумент2 страницыHow To Self-Decontaminate After A Radiation Emergency - CDCZankanotachiОценок пока нет
- Arma 2018 047Документ7 страницArma 2018 047Lígia BrumОценок пока нет
- LaserДокумент12 страницLasercabe79Оценок пока нет
- Increase Credit Limit PDFДокумент1 страницаIncrease Credit Limit PDFemc2_mcvОценок пока нет
- 6 Instrumentation PDFДокумент144 страницы6 Instrumentation PDFWanderley MandruzatoОценок пока нет
- Lead and Manage People TTLMДокумент41 страницаLead and Manage People TTLMHenok Mehari100% (1)
- 2016 Specimen Paper 1 PDFДокумент16 страниц2016 Specimen Paper 1 PDFBioScMentor-1Оценок пока нет
- Assessment 2 Vital Signs Normal ValuesДокумент4 страницыAssessment 2 Vital Signs Normal Valuesthannikkotte12345Оценок пока нет