Академический Документы
Профессиональный Документы
Культура Документы
Adrenergic Mechanisms
Загружено:
Hailu DinbuИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Adrenergic Mechanisms
Загружено:
Hailu DinbuАвторское право:
Доступные форматы
a2-Adrenergic Mechanisms of Analgesia
575
References
1. Lima, D., Mendes-Ribeiro, J. A., and Coimbra, A. (1991).The spino-latero-reticular system of the rat: Projections from the superficial dorsal horn and structural characterization of marginal neurons involved. Neuroscience 45, 137-152. 2. Menktrey, D., and Basbaum, A. I. (1987).Spinal and trigeminal projections to the nucleus of the solitary tract: A possible substrate for somatovisceral and viscerovisceral reflex activation. J. Comp. Neurol. 255, 439-450. 3. Pacak, K., Palkovits, M., Kopin, I. J., and Goldstein, D. S. (1995).Stress-induced norepinephrine release in the hypothalamic paraventricular nucleus and pituitary-adrenocortical and sympatho-adrenal activity: In vivo microdialysis study. Front. Neuroendocrinol. 16,89-150. 4. Pacak, K., Palkovits, M., Makino, S., Kopin, I. J., and Goldstein, D. S. (1996). Brainstem hemisection decreases corticotropin-releasing hormone mRNA in the paraventricular nucleus but not in the central amygdaloid nucleus. J. Neuroendocrinol. 8, 543-551. 5. Palkovits, M., Baffi, J. S., and Dvori, S. (1995). Neuronal organization of stress response: Pain-induced c-fos expression in brain stem catecholaminergic cell groups. Ann. N. Y. Acad. Sci. 771, 313-326.
Mark J. Millan
Department of Psychopharmacology lnstitut de Recherches Servier 78290 Croissy-sur-Seine (Paris), France
cu2-Adrenergic Mechanisms of Analgesia: Strategies for Improving Their Therapeutic Window and Identification of the Novel, Potent cu2,-Adrenergic Receptor Agonist, S 18616
Adrenergic pathways descending from the brain stem the dorsal horn (DH) of the spinal cord control the access of nociceptive information to the brain (1, 2 ) . The antinociceptive actions of noradrenaline (NAD) in the DH are exerted both presynaptically on terminals of primary afferent fibers (PAFs),thereby inhibAdvances in Pharmacology, Volume 42 Copyright 0 1998 by Academic Press. All rights ot reproduction in any form reserved. 1054-3.589/98 $25.00
576
Mark J. Millan
iting the release of substance P and glutamate, and postsynaptically on projection neurones targetted by PAFs ( 3 ) .The discovery of multiple a-adrenergic receptors (a2ARs) ( a Z A , a z b , azc,and aZD/raZA, orthologous to haZA) raises the question as to their respective roles. a2*ARs predominate in the DH and play a major role in mediating antinociception (2,4). First, preferential ff2A agonists, such as guanfacine, guanabenz, and oxymetazoline, elicit antinociception. Second, their actions are blocked by the azAAR-selectiveantagonist, BRL 44408,but not by the @B/ 2cARantagonists, prazosin, ARC 239,and BRL 41992.Third, a2,AR-targetted gene knockdown (antisense)and gene knockout (null mutation) strategies have confirmed that the antinociceptive actions of a2AR agonists are exerted via azAARs (M.Maze and L. E. Limbird, personal communication).Indeed, clonidine and dexmedetomidine (DMT), which elicit antinociception in both rodents and humans, display high affinity at azAARs. These represent, thus, an attractivedevelopment target, and we have identified a spiro-oxazoline, S 18616 ([7,8](2chlorobenzo)-2-amino-l-aza-3-oxa-[4,5]spirodeca-1,7-diene) possessing high efficacy and extraordinary potency at these sites (Table I). S 18616 displays a modest preference for aZAAR versus aZBand aZCARs. It also shows a marked preference for ( Y ~ ~ versus A R alARs and I2 receptors, while its preference for azAARsversus I1 receptors is also more pronounced than for clonidine. It is active at very low doses upon S.C. (not shown) or oral (see Table I ) administration to mice, with a duration of action of 1216 hr. S 18616 may show superior separation of antinociceptive to motor actions as compared with DMT and clonidine (see Table I), although this requires confirmation. S 18616 does exert sedative properties at higher doses, and the hypnotic-sedative actions of a2AR agonists reflect the engagement of dendritic a2*AR autoreceptors on noradrenergic neurones of the locus ceruleus (1, 2).Further, a2AARs in the brain stem and intermediolateral cell column of the spinal cord mediate the sympathoinhibitory actions of azAARagonists (4). Thus, activation of azAARsunderlies not only the analgesic, but also the hypnotic-sedative and hypotensive actions of aZAAR agonists. Moreover, reflecting an inhibition of ascending noradrenergic neurones, they similarly mediate the anxiolytic actions of a2ARagonists. These roles open several therapeutic avenues for ~ ~ ~ ~ A R - s e l e c agonists, tive including their use in the perioperative environment for the reduction of anesthesia requirements and (owing to their
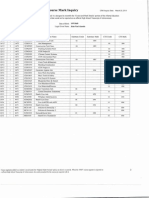
TABLE I In Vitro and In Vivo Activity of S18616
S 18616 DMT Clonidine
0.17 2.1 8.4
1.9 3.8 27.0
0.9 12.9 73
6.5 26 444
79 355 562
4.1 198 29
72
11000 >lo00
1.2 9.4 56
81 80 350
67.5 8.5 6.3
Affinities are for native receptors, except ha2*-and haZcARs(cloned, human) transfected into an Sf9 baccilovirus. For methods, see Millan et al. (2) and Renouard et al. (5).1994. I, imidazoline; IDSO, inhibitory dose 50 (gg/kg, p.0.); FPL, tormalin paw-lick; RR, rotarod.
cu?-Adrenergic Mechanisms of Analgesia
577
hemostabilizing and sympatholytic actions) myocardioprotection (1, 6). However, the induction of hypotension and sedation by azAARagonists raises the question as to whether satisfactory analgesia can be acheived in the absence of intolerable side effects in conscious subjects. This question can be answered only in the clinic with selective, potent, and high-efficacy drugs such as S 18616. Nonetheless, one may also envisage several alternative strategies for improving the therapeutic window of azAR agonists. First, partial agonists may permit the separation of analgesic actions from side effects. This approach presupposes that the efficacy required for induction of analgesia is less than that for induction of hypotension or sedation. However, azAARautoreceptors mediating motor actions are unlikely to be less sensitive than their postsynaptic counterparts mediating antinociception, and a reduction in agonist efficacy risks limiting maximal analgesia. Further, clonidine itself is a partial agonist. This approach has, thus, yet to prove successful. Second, drugs with varying degrees of efficacy may show differential rates of tolerance development, and the analgesic actions of a2AR agonists may adapt more slowly than their secondary actions. Interestingly, there aye indications that motor actions adapt more rapidly than analgesic actions (notably, with S 18616), but hypotensive effects are unlikely to disappear. Further, this is not relevant to acute, first-dose administration. Third, one might, conceivably, build into an azAAR agonist a component of activity palliating its undesirable effects. This would be analogous to antipsychotic agents possessing serotoninergic properties to moderate the extrapyramidal syndrome provoked by dopamine Dz-receptor blockade. Fourth, it may be possible to incorporate into a drug two synergistic mechanisms of analgesic activity. For example, a dual a2AR agonist plus popioidergic mechanism of action might allow for the optimization of analgesic actions while minimizing the side effects associated with stimulation of a2AR and p-opioid receptors, respectively ( I ) .One possible example of such a drug is the weak opioid, tramadolol, which possesses adrenergic properties. Fifth, this strategy does not permit the titration of each of the components of activity separately, and a related approach would be to use an azAR agonist in association with a further analgesic agent in order to similarly augment the therapeutic window. Indeed, systemic or spinal coadministration of a2AR agonists with popioids or local anesthetics affords robust pain relief in the absence of severe side limits (6).Further, there is experimental evidence that a2AR agonists elicit additive or synergistic antinociception (in the absence of intensified side effects) with agonists at muscarinic and serotoninlBreceptors and with antagonists a t the N-methyl-D-aspartate receptor (1, 3). Sixth, the preceding approach incorporates the strategy of local (intrathecal or epidural) administration of a2AR agonists into the DH. Nevertheless, spinal application is not of universal utility and does not necessarily obviate all side effects of azAR agonists. Thus, actions of aZARagonists in the intermediolateral cell column modulate sympathetic outflow, while the occurrence of bradycardia and hypotension at high doses of spinal clonidine in humans may reflect redistribution (via the cerebrospinal fluid or circulation) to the brain stem (4, 6). Indeed, apart from motor effects in the ventral horn, sedation has been seen in some clinical studies with clonidine likewise indicating that the drug may access higher centers. Bolus administration and/or computerized control of injection rates may limit such
578
Mark 1. Millan
problems ( 6 ) . Further, an evaluation of the actions of lipophobic drugs (to minimize redistribution) would be of interest. Seventh, desipramine and other antidepressants inhibiting the re-uptake of NAD are effective analgesic agents, for example, against neuropathic pain, and a component of their activity may be exerted spinally ( 3 ) .These drugs mimic the physiological release of NAD, which presumably acts with all available adrenergic receptor types (possibly including some as yet unknown). This might, arguably, be the most appropriate mode for obtaining analgesia in a manner comparable to that which occurs naturally. Eighth, an opposite approach comprises the development of drugs interacting selectively with specific a2AR subtypes and, as described previously, aZAARs constitute one possible target (2). However, azeARs are found in the thalamus and in human DH, while a2cARs are found in both rat and human DH (albeit at low densities), in PAFs, and in sympathetic ganglia (4). Thus, they also may play a role in modulating nociception. In addition, an additional non-azAAR,possibly a2c, also may contribute to antinociception at the spinal level in rats (2). Finally, the possible importance of a,ARs should not be neglected (4). In conclusion, there exist many potential strategies for an improvement in the therapeutic index of qAR-mediated analgesics. Of these, the development of a2AR subtype-selective ligands remains particularly attractive. Unfortunately, to date, virtually all clinical data have been acquired with clonidine, which is a partial agonist of modest potency and only limited selectivity. There is, thus, an urgent need for novel ligands. In this regard, S 18616 should prove of use in the further exploration of the potential antinociceptive roles of adrenergic mechanisms, and its therapeutic properties will be of interest to evaluate.
Acknowledgments
A. Cordi, J-M. Lacoste, S. Girardon, K. Bervoets, and C. Dacquet are thanked for collaboration.
References
1. Hayashi, Y., and Maze, M. (1993). Alphaz adrenoceptor agonists and anaesthesia. Br. J . Anaesth. 71, 108-118. 2. Millan, M. J., Bervoets, K., Rivet, J-M., Widdowson, P., Renouard, A,, Le MarouilleGirardon, S., and Gobert, A. (1994). Multiple alpha2-adrenergic receptor subtypes. 11. Evidence for a role of rat RazA-ARsin the control of nociception, motor behaviour and hippocampal synthesis of noradrenaline. /. Pharmacol. E x p . Ther. 270, 958-972. 3 . Besson, J-M., and Guilbaud, G., eds. (1992). Towards the Use of Noradrenergic Agonists for the Treatment of Pain. pp. 233. Elsevier, Amsterdam. 4. Nicholas, A. P., Pieribone, V. A., and Hokfelt, T. (1996).The distribution and significance of CNS adrenoceptors examined with in situ hybridization. Trends Pharmacol. Sci. 17, 245-255.
Cellular Transplantation for Intractable Pain
579
5 . Renouard, A., Widdowson, P. S . , and Millan, M. J. (1994). Multiple alpha2-adrenergic receptor subtypes. I. Comparison of ['H]RX821002-labelled rat RalA-adrenergicreceptors in cerebral cortex to human HazA-adrenergic receptors and other populations of alA-adrenergic subtypes J. Pharmacol. E x p . Ther. 270, 946-957. 6. Eisenach, J. C. (1994).Alpha-2 agonists and analgesia. Exp. Opin. Invest. Drugs 3, 10051010.
Jacqueline Sagen
CytoTherapeutics, Inc. Providence, Rhode island 02906
CelIuIar Transp Iantat ion for
Intractable Pain
Implantation of cells directly into the central nervous system (CNS) offers a novel means of providing sustained local delivery of pharmacologically active substances for the long-term management of chronic disorders. Furthermore, the use of cellular implant therapies allows for the delivery and utilization of agents that have short biological half-lives or barriers to CNS penetration. Work in our laboratory over the past 10 years has suggested that cellular transplantation may be a powerful approach for the alleviation of chronic pain. For these studies, adrenal medullary chromaffin were chosen as donor sources, because these cells produce and secrete catecholamines and opioid peptides, agents that reduce pain when administered directly into the spinal subarachnoid space and synergize to produce potent analgesia. In addition to these agents, chromaffin cells have been reported to secrete a variety of neurotrophic factors, cytokines, and other neuropeptides, as well as ascorbate and heme-containing proteins, which may aid in the restoration of spinal cord function in chronic pain syndromes. Donor sources for these studies have included primarily either adrenal medullary tissue allografts or isolated xenogeneic chromaffin cells, although cell lines that can be genetically engineered have been utilized and are a likely avenue for future applications. For preclinical rodent studies, allogeneic tissues can be obtained from adult donors of the same strain by microdissection of adrenal medullary tissue from the adrenal cortex. Previous findings have shown that adrenal medullary tissue can be either transplanted following dissection or maintained in tissue culture for at least 30 days prior to implantation without apparent decrement in antinociceptive potency. The latter approach has been utilized in initial clinical studies, with adrenal medullary tissue derived from human organ donors (1).However, because the practical application of adrenal
Advances zn Pharmacology, Volume 42 Copyrighi Q 1998 by Academic Press. All rights of reproducrion in any form rcserved
1054.3589198 $25.00
Вам также может понравиться
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- IM1 Calculus 2 Revised 2024 PUPSMBДокумент14 страницIM1 Calculus 2 Revised 2024 PUPSMBEunice AlonzoОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- 18-MCE-49 Lab Session 01Документ5 страниц18-MCE-49 Lab Session 01Waqar IbrahimОценок пока нет
- Img 20150510 0001Документ2 страницыImg 20150510 0001api-284663984Оценок пока нет
- CATaclysm Preview ReleaseДокумент52 страницыCATaclysm Preview ReleaseGhaderalОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Leadership and Management in Different Arts FieldsДокумент10 страницLeadership and Management in Different Arts Fieldsjay jayОценок пока нет
- Financial Market - Bsa 2A Dr. Ben E. Bunyi: Imus Institute of Science and TechnologyДокумент3 страницыFinancial Market - Bsa 2A Dr. Ben E. Bunyi: Imus Institute of Science and TechnologyAsh imoОценок пока нет
- SubaruДокумент7 страницSubaruclaude terizlaОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Project Quality Plan (JFJS-788)Документ18 страницProject Quality Plan (JFJS-788)mominОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Subject OrientationДокумент15 страницSubject OrientationPearl OgayonОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Mecha World Compendium Playbooks BWДокумент12 страницMecha World Compendium Playbooks BWRobson Alves MacielОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Arithmetic QuestionsДокумент2 страницыArithmetic QuestionsAmir KhanОценок пока нет
- Grade 3 - Unit 1 Increase and Decrease PatternДокумент7 страницGrade 3 - Unit 1 Increase and Decrease PatternKyo ToeyОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- MH5-C Prospekt PDFДокумент16 страницMH5-C Prospekt PDFvatasaОценок пока нет
- Praise and Worship Songs Volume 2 PDFДокумент92 страницыPraise and Worship Songs Volume 2 PDFDaniel AnayaОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- 2nd Term Project 4º Eso Beauty Canons 2015-16 DefinitivoДокумент2 страницы2nd Term Project 4º Eso Beauty Canons 2015-16 DefinitivopasferacosОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Inspección, Pruebas, Y Mantenimiento de Gabinetes de Ataque Rápido E HidrantesДокумент3 страницыInspección, Pruebas, Y Mantenimiento de Gabinetes de Ataque Rápido E HidrantesVICTOR RALPH FLORES GUILLENОценок пока нет
- Carnegie Mellon Thesis RepositoryДокумент4 страницыCarnegie Mellon Thesis Repositoryalisonreedphoenix100% (2)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Li JinglinДокумент3 страницыLi JinglincorneliuskooОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Maya Deren PaperДокумент9 страницMaya Deren PaperquietinstrumentalsОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- 220245-MSBTE-22412-Java (Unit 1)Документ40 страниц220245-MSBTE-22412-Java (Unit 1)Nomaan ShaikhОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Song Book Inner PagesДокумент140 страницSong Book Inner PagesEliazer PetsonОценок пока нет
- 02 Object Modeling TechniqueДокумент50 страниц02 Object Modeling TechniqueMuhammad Romadhon Batukarang EsdОценок пока нет
- XII CS Material Chap7 2012 13Документ21 страницаXII CS Material Chap7 2012 13Ashis PradhanОценок пока нет
- WWW Studocu Com in N 29646569 Sid 01682568219Документ1 страницаWWW Studocu Com in N 29646569 Sid 01682568219Nivetha SelvamuruganОценок пока нет
- Derma Notes 22pages. DR - Vishwa Medical CoachingДокумент23 страницыDerma Notes 22pages. DR - Vishwa Medical CoachingΝίκος ΣυρίγοςОценок пока нет
- DJ Crypto ResumeДокумент1 страницаDJ Crypto ResumeNitin MahawarОценок пока нет
- I M Com QT Final On16march2016Документ166 страницI M Com QT Final On16march2016Khandaker Sakib Farhad0% (1)
- Quotation of Suny PDFДокумент5 страницQuotation of Suny PDFHaider KingОценок пока нет
- HUMSS - Introduction To World Religions & Belief Systems CGДокумент13 страницHUMSS - Introduction To World Religions & Belief Systems CGAliuqus SirJasper89% (18)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Perdarahan Uterus AbnormalДокумент15 страницPerdarahan Uterus Abnormalarfiah100% (1)