Академический Документы
Профессиональный Документы
Культура Документы
Laparoscopic Versus Open Appendectomy in Adults With Complicated Appendicitis - Systematic Review and Meta-Analysis
Загружено:
Juan Carlos SantamariaИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Laparoscopic Versus Open Appendectomy in Adults With Complicated Appendicitis - Systematic Review and Meta-Analysis
Загружено:
Juan Carlos SantamariaАвторское право:
Доступные форматы
World J Surg DOI 10.
1007/s00268-010-0669-z
Laparoscopic Versus Open Appendectomy in Adults with Complicated Appendicitis: Systematic Review and Meta-analysis
Georgios Markides Daren Subar Kallingal Riyad
te Internationale de Chirurgie 2010 Socie
Abstract Background The goal of the present study was to critically review and identify the strength of available evidence in the literature on the use of laparoscopic appendectomy (LA) in complicated appendicitis (CA). Methods The Cochrane Library and Controlled Trials Registry, MEDLINE (Ovid), PubMed, Web of knowledge, and SCOPUS databases were electronically searched, using the keywords appendectomy, laparoscopy, appendicitis. complicated appendicitis. gangrenous appendicitis, perforated appendicitis, with English language as a limit. Backward chaining was also employed. The NHS Public Health Resource Unit Critical Appraisal Skills Programme Tools were used for critical appraisal. Results Twelve retrospective case-control studies were included in the review. Overall methodological quality was moderate to poor, with heterogeneity, absence of randomization and blinding, and presence of important methodological aws. Meta-analysis showed that LA in CA has reduced surgical site infection (SSI) rates compared to open appendectomy (OA), odds ratio (OR) 0.23, 95% condence intervals (CI): 0.140.37 (level 3a evidence), and no difference with regard to intra-abdominal abscess
(IAA) complication rates OR: 1.02, (level 3a evidence). Conclusions When compared to appendectomy is advantageous in CA with no signicant additional risk evidence).
95% CI 0.561.86 OA, laparoscopic with regard to SSIs, of IAA (level 3a
Introduction Evidence-based practice is the cornerstone for best medical practice. It is the process of systematically nding, appraising and using contemporaneous research ndings as the basis of clinical decisions [1]. In the face of a clinical problem such as the choice between laparoscopic appendectomy (LA) and open appendectomy (OA) best evidence derived from level 1 quantitative research like welldesigned randomized double-blinded control trials should be used to decide on the best management. In the absence of such trials, evidence from lower down in the hierarchical evidence ladder should be carefully considered. Acute appendicitis is a surgical condition with incidence of 1.17 per 1,000 [2] and lifetime risk of 8.6% in males and 6.7% in females [3]. Complicated appendicitis (CA) occurs once the appendix has become gangrenous and/or has perforated with various degrees of peritonitis. The rate of CA is slowly increasing [4] and has been reported at an incidence of 1230% [5]. It is associated with higher morbidity rateswound infection rates 20% versus 5% in noncomplicated appendicitis (nCA) [6]and mortality rates5% versus 0.8% in nCA [7]. Since 1894, after the description of a series of case studies by McBurney, OA via the McBurney approach has been the gold standard procedure for appendectomy [8]. In the early 1980s Semm [9] described the rst laparoscopic
G. Markides (&) Department of General Surgery, Royal Oldham Hospital, Oldham, UK e-mail: g.markides@yahoo.co.uk D. Subar Department of General Surgery, Stepping Hill Hospital, Stockport, UK K. Riyad Department of General Surgery, Royal Blackburn Hospital, Blackburn, UK
123
World J Surg
appendectomy. Subsequent technological advances and improvement of surgical laparoscopic techniques and expertise have given ground for trying to introduce this procedure as the mainstay of treatment for appendicitis. A recent systematic review and meta-analysis has shown that the advantages of LA in nCA appear to focus on the reduction of postoperative pain, wound infection rates, and in-hospital stay compared to OA, and that it has distinct diagnostic advantages in females of reproductive age [10]. The use of LA in CA though has been controversial and associated with increased rates of intra-abdominal abscess (IAA) complications [10, 11]. More recent studies have refuted the above nding, suggesting reduced postoperative wound infection rates of LA compared to OA in CA, and are actually recommending LA as the mainstay of treatment for these patients [12, 13]. The aim of the present study was therefore to systematically review the literature on the effectiveness of LA in relation to conventional OA in the management of adult patients with complicated acute appendicitis, with a subsequent meta-analysis.
Data abstraction and validity assessment Data on study methodology, participant characteristics, intervention characteristics, and primary outcomes were independently extracted and tabulated by two reviewers with a predened data extraction form. Attempts to contact authors were made if there were missing data or unclear information in the studies, and data were adjusted accordingly. The studies were subsequently assessed independently by two reviewers for methodological quality using the Critical Appraisal Skills Tools for randomized controlled trials and case-control studies [14, 15], with criteria marked as met, unclear, and not met. Overall risk of bias was assessed with established methods and graded as A (low risk), B (moderate risk), and C (high risk) [16]. Data analysis The RevMan 5 statistical package [17] was employed to perform odds ratio (OR) analysis and to assess statistical heterogeneity via I2, with statistical signicance at p \ 0.05 and I2 \ 30%, respectively, and to assess publication bias via funnel plot graphical representation. Meta-analysis was conducted with the Mantel-Haenszel statistical method for dichotomous variables, and Inverse Variance was used for continuous variables. Separate analyses were performed for each bias risk group and for all groups combined together. Final recommendations were graded based on the Oxford Centre of Evidence Based Medicine level of evidence and grades of recommendation guidelines [18].
Methods Types of studies Our search included both randomized controlled trials and observational studies. Eligibility criteria included all studies comparing LA to OA in adult patients with CA, with (a) postoperative surgical site infection (SSI) rates, and/or (b) postoperative IAA rates, and/or (c) postoperative analgesia, and/or time to oral intake, and/or length of stay in hospital, as end points. Studies with insufcient data to form 2 9 2 tables for use in odds ratio (OR) analysis and 95% condence interval (CI) or studies not providing adequate data to obtain mean values and standard deviation for continuous variables were excluded from the relevant calculations. Search and selection strategies The Cochrane Library and Controlled Trials Registry, MEDLINE (Ovid) (1966November 2008), PubMed, EMBASE (1966November 2008), Web of knowledge, and SCOPUS databases were electronically searched for appendectomy, laparoscopy, laparoscopic appendectomy, and appendicitis, complicated appendicitis, gangrenous appendicitis with perforated appendicitis. The search was limited to studies published in the English language, and was completed with reference follow-up. The citations and/or abstracts or full text of all potentially relevant studies were independently reviewed and selected by two reviewers, and any disagreements were resolved with discussion.
Results The initial literature search identied 381 studies. Based on the inclusion criteria, 362 studies were excluded, with a selection of 19 studies for more detailed review. Seven of those studies were subsequently excluded [1925] (Fig. 1), including one conference abstract with limited study methodology information, leaving 12 retrospective observational/ case-controlled studies for systematic review. A summary of the studies methodology, intervention characteristics, and measured outcomes is provided later in Tables 1, 2 and 3.
Discussion Summary of studies Randomization, concealment of allocation, and blinding are inherently absent from the methodological design of the included studies. In the absence of a standardized care protocol, patients were allocated to either operative group
123
World J Surg Fig. 1 Article selection ow chart
Potentially relevant studies identified and screened for retrieval n = 381
Studies excluded n = 362 Not satisfying eligibility criteria
Studies retrieved for more detailed evaluation n = 19 Studies excluded n = 2 Retrospective case-series n = 2 Potentially appropriate studies to be included in the meta-analysis n = 17
Studies included in meta-analysis n = 12 (retrospective case-control studies)
Studies excluded from meta-analysis n = 5 Serious methodological flaw with high bias risk directly affecting outcome n=4 Inadequate data for analysis n=1
Studies withdrawn, by outcome, n = 0 Studies with usable information, by outcome, n = 12
based on the surgeons discretion. This is an important bias because it reects the surgeons experience with LA, the presence of co-morbidities, and the patients clinical condition, all of which may have inuenced placement into either of the patient group [2628]. Another of the problems encountered in the appraisal of the studies is the case denition for CA. Most studies dene this as a perforated appendix with or without abscess formation, with or without peritonitis. Four of the studies [13, 2931] include gangrenous appendix in their case denition, presumably because it is difcult macroscopically to distinguish between a perforated and a nonperforated gangrenous appendix, allowing for variation in the interpretation of results between these groups of studies. Initial diagnosis of CA in all but two cases [12, 30] is made subjectively based on clinical opinion, and macroscopic histological conrmation is provided in only four of the studies [13, 3133]. Validity of the case denition in the remaining studies is therefore compromised. In an attempt to avoid this problem, Fukami et al. [12] used CT (computed tomography) scanning to conrm CA prior to group allocation. A drawback of this denition though would be that patients with perforation but minimal abdominal uid that cannot be diagnosed by CT scanning were excluded from the study thus creating a potential selection bias and less general applicability of the studys results (reduced external validity). An alternative is provided by Yau et al. [30], who diagnose CA laparoscopically rst and then proceed to separate the two groups. This appears to be a reasonable way to reach a good case denition, as the diagnostic effects of an initial laparoscopy in suspected
appendicitis have been well established [10]. It does though introduce the bias of an initial diagnostic laparoscopy. Two of the studies [34, 35] do not report any patient characteristics and should be viewed with great caution with regard to generalizing their results to a normal population. In the remaining studies statistical testing of these independent variables varies signicantly (Table 1) with external validity implications. Yau et al. [30] are the only authors who used exclusion criteria regarding age. It is difcult to judge from the reported ages how big the pediatric contribution is to these studies, as some information is presented as median age standard deviation and some as mean age, rather than medians with the interquartile ranges. From a cautious review, it appears that the majority of patients included are adults as the range of reported median and mean ages is 3648 and 3040 years, respectively, between groups. The exception to this is the study by Pokala et al. [29], which reports the inclusion of 24 pediatric cases in a total study population of 104. In recognition of that, the authors later test the two populations separately, but they potentially compromise the signicance of the studys ndings because of a change in the patient number group ratio (from 43:61 to 28:52). Intervention characteristics The level of surgical experience and the learning curve are two important independent variables requiring consideration. A higher surgical level of experience in LA could mean a reduced number of converted cases to OA and potentially lower complication rates. Even though the
123
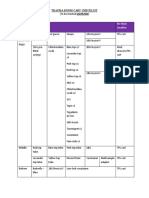
Table 1 Summary of studies Sample size LA n = 146 3.4%ITT not used OA n = 84 All patients with CA from hospital records May 1995May 2007 NS between groups: age, gender, co-morbidities not tested Inclusion criteria Independent variables Conversion rate & ITT Findings SS between groups: lower rate of SSIs, longer OT, analgesic use, TTOI, pLOS in LA group, NS between groups: IAA, other post-op complications LA n = 34 0%N/A OA n = 39 NS between groups: age, gender, obesity, coAll CA patients undergoing OA in rst 3 years and all CA morbidities patients undergoing LA in last 3 years Jan 1999Dec 2004 SS between groups: lower rate of SSIs, analgesic use, TTOI, duration of drainage, pLOS in LA group NS between groups: OT, IAA, hernia, stula formation NS between groups: OT, TTOI (solids), pLOS, SSI, IAA
123
LA n = 50 OA n = 98 All patients with CA from hospital records Jan 2005Aug 2005 S between groups: more 16%ITT not used females of reproductive age, (conversions treated as higher co-morbidity, obese separate group) and unknown abdominal pain pts in LA group LA n = 43 OA n = 61 All patients with CA from hospital records Jan 2003Feb 2006 18.6%ITT used S between groups: more pediatric cases in LA group (separate analysis contacted), NS between groups: gender, ASA group LA n = 175 OA n = 244 LA n = 99 OA n = 130 All patients with CA from hospital records Jan 2001Dec 2003 All patients with CA from hospital records Jan 1999Jan 2004 NS between groups: age, gender 13.7%ITT used SS between groups: longer OT, higher IAA rate in LA group NS between groups: overall complications and SSI SS between groups: shorter OT, LOS and SSI in LA group NS between groups: IAA rates NS between groups: age, gender 8%ITT used SS between groups: longer OT, shorter antibiotic requirements, shorter TTOI and LOS, lower SSI in LA group NS between groups: postoperative analgesia, reoperation rates, IAA LA n = 1,763 1997 Not reported Not given SS between groups: shorter LOS in LA group NS between groups: SSI, postoperative complications OA n = 12,644 All patients with appendicitis from U.S. national database stratication for CA
Study
Exposure measurement
Katsuno et al. [31]
Retrospective case note review
Fukami et al. [12]
Retrospective case note review
Kirshtein et al. [13] Retrospective case note review
Pokala et al. [29]
Retrospective case note review
Yau et al. [30]
Retrospective case note review
Lin et al. [37]
Retrospective case note review
Guller et al. [35]
NIS database
World J Surg
Table 1 continued Sample size Inclusion criteria Independent variables Conversion rate & ITT Findings
World J Surg
Study
Exposure measurement LA n = 85 Jan 1992Jun 1999 All patients with perforated appendicitis OA n = 146 NS between groups: age, gender 40%ITT used SS between groups: less postoperative analgesia and complications, reduced TTOI and LOS in LA group NS between groups: OT LA n = 28 OA n = 24 LA n = 217 OA n = 82 19911999 LA LA n = 80 OA n = 45 LA n = 77 Jan 1994Aug 1997 All patients with acute appendicitis Not reported OA n = 122 All patients with perforated appendix Jul 1991Jun 1999 NS between groups: age, gender, BMI All patients with CA Aug 1989Mar 1999 for OA Not reported 52 prospective patients Not tested 36%ITT not used, groups tested individually NS between groups: OT, IAA, SSI, pLOS
So et al. [36]
Retrospective case note review
Piksun et al. [32]
Prospective case note collection
Wullstein et al. [34] Retrospective case note review
21% (3560% in 1991; SS between groups: SSI lower 23.4% in 19981999) in LA ITT used NS between groups: IAA 45% (16% in latter years)ITT not used SS between groups: SSI NS between groups: OT, LOS, IAA SS between groups: OT NS between groups: LOS, IAA
Stoltzing et al. [33] Retrospective case note review
Khalili et al. [44]
Retrospective case note review
ITT not used
LA laparoscopic appendectomy, ASA American Society of Anesthesiologists score, BMI body mass index, OA open appendectomy, CA complicated appendicitis, uCA uncomplicated appendicitis, ITT intention to treat, SS statistically signicant, NS statistically nonsignicant, OT operating time, TTOI time to oral intake, LOS length of stay in hospital, pLOS postoperative length of stay in hospital, SSI surgical site infection, IAA intra-abdominal abscess
123
Table 2 Summary of studies intervention characteristics
Surgeons Procedure Meso-appendix & appendix resection Coagulation ? suture loops or staples Used McBurneys or paramedian Yes Retrieval bag Procedure LA OA Primary wound Antibiotic closure
123
1 experienced 3 trochars, 10-5surgeon ? surgical trainees 5 mm, ?type of endoscope 6 experienced surgeons for LA, at least 2 other surgeons for OA 3 trochars, 10-105 mm, exible endoscope used Used McBurneys or paramedian Yes Electrocautery or ultrasound dissector ? endolinear cutter Gridiron or paramedian Secondary closure in contaminated cases Not reported Preoperative and postoperative use as clinically indicated Preoperative and postoperative use as clinically indicated 9 surgeons ?experience 3 trochars, 45 deg Coagulation or Used in endoscope clips ? suture loops or 67% staples Preoperative and postoperative use as clinically indicated Not reported Not reported Not reported Not Not reported reported Used Gridiron Not reported Surgical residentsat least 3 years experience 3 trochars, 10-55 mm, ?type of endoscope Electrocautery or ultrasound dissector ? suture loops Electrocautery or clips or Used harmonic scalpel ? clips or endoloop Not reported Not reported Preoperative and postoperative use as clinically indicated 4 experienced surgeons 3 trochars, 10-33 mm, ?type of endoscope McBurneys, paramedian or midline Yes Preoperative and postoperative use as clinically indicated Not reported Not reported Not Not reported reported Used usually Gridiron or midline Not reported Not reported ? number, less experienced surgeons (n \ 20) associated with higher conversion rates 12 surgeons ?experience 3 trochars, 12-55 mm, ?type of endoscope Electrocautery, clips or stapler ? endoloop or stapler Yes but in 4 cases Preoperative and postoperative use as clinically indicated 3 trochars, 10-5?clips ? stapler 12 mm, ?type of endoscope Used Not given Yes Preoperative and postoperative 5 days and then as clinically indicated Used McBurneys Not reported ?surgeons ?experience Learning curve 3 trochars, 12-5Clips or stapler ? clips 12 mm, ?type of or endoloop endoscope Preoperative and postoperative use as clinically indicated
Study
CA diagnosis
Katsuno et al. [31]
Intraoperative
Fukami et al. [12]
CT scan
Kirshtein et al. [13]
?clinical
Pokala et al. [29] Clinical ? CT scan conrmation of CA
Yau et al. [30]
Laparoscopically
Lin et al. [37]
Intra-abdominal pus
Guller et al. [35] ?clinical
So et al. [36]
Clinical
Piksun et al. [32] ?clinical
Wullstein et al. [34]
?clinical
World J Surg
World J Surg
nding is not statistically tested, So et al. [36] do actually report that less experienced laparoscopic surgeons (performing fewer than 20 laparoscopic procedures) had a higher rate of conversion. Trying to compensate for this problem and only allowing experienced surgeons to perform LA, though, would positively bias the results in favor of LA and reduce external validity. This is because in the normal hospital environment of a general hospital there is a variation in the level of laparoscopic experience among both senior surgeons and trainees. As OA is a procedure performed both during day and night by all these levels of surgeons, LA should be assessed under similar circumstances. Similarly, a surgeon at the start of his or her learning curve in performing LA, would be more likely to have a higher rate of conversion to OA, as well as a higher rate of complications. Including a large number of these cases in the analysis sample could potentially bias the results against LA. Such a learning curve is reported by Katsuno et al. and Wullstein et al. [31, 34]. The inclusion of this individual surgeon learning curve in the studies under some circumstances may be acceptable and can be assumed to represent a normal variation around hospitals as inexperienced surgeons learn LA. This though should only occur after a plateau has been reached where, theoretically, all the senior surgeons in an institution have mastered the art of laparoscopy. Results from studies near the introduction of LA would therefore be mostly applicable to clinical practice during that particular time period, with recent results being more applicable to current practice. The earlier studies included in the present appraisal, such as the ones by So et al. [36] and Wullstein et al. [34], both of which include an early institutional learning curve from the early 1990s and should therefore be reviewed carefully with regard to current practice. Randomization of surgeons laparoscopic experience in the LA group should therefore be the most appropriate approach. The number of surgeons performing each procedure should also be sufcient that individual surgeon bias is not introduced, affecting the results and external validity. In the studies included herein there is a wide variation in the numbers of recruited surgeons and their laparoscopic experience, both between groups and between studies (Table 2). The effect of this performance bias can potentially be seen in the studies by Yau et al. [30] and Lin et al. [37], groups that only use experienced laparoscopic surgeons in their studies, reporting relatively low conversion rates compared to the other studies (Table 1). A lower conversion rate could mean an underestimation of wound infections in the LA group because the use of intention to treat (ITT) analysis places patients undergoing LA that required conversion to OA, which means a bigger abdominal wall incision, into the LA group. In these
Preoperative and postoperative use as clinically indicated Pararectal incision Not reported or lower midline laparotomy 3 trochars, 10-5Electrocautery, clips or 12 mm, ?type of stapler endoscope Used
Primary wound Antibiotic closure
Meso-appendix & appendix resection
Retrieval bag
Not reported CT cross tomography scan, CA complicated appendicitis, uCA uncomplicated appendicitis Learning curve Khalili et al. [44] Clinical Not reported Not reported
Procedure
LA
CA diagnosis
Surgeons
Table 2 continued
Stoltzing et al. [33]
Study
Clinical
?surgeons
?experience
Not Not reported reported
Procedure
OA
Not reported
Not reported
123
Table 3 Summary of studies measured outcomes Postoperative analgesia (days) LA: 8.9*, OA: 16.6 ?timing Enteritis, OA: 1/84 Pneumonia, OA: 2/84 Hernia, LA: 1/34 Fistula, OA: 1/39 LA: 11.7*, LA: 8.8%*, LA: 5.9%, OA: 25.8, OA: OA: 5.1% pLOS 48.6% LA: 24%*, LA: 4.3%, OA: 6.4% OA: 4.8% Small bowel obstruction, LA: 2/146, OA: 4/84 1 appt TTOI (days) LOS (days) SSI IAA Other postoperative complications Follow-up Notes Oral intake commenced after bowels opened, 1 experienced surgeon with team, learning curve included
123
PO laxoprofen sodium, LA: 4.2, OA: 6.4* 36 patients 43.6% OA pts performed under spinal anaesthesia ?timing pr diclofenac, LA: 2.1, OA: 7.5* Not reported Pulmonary emboli, OA: 1/48 Wound dehiscence, OA: 1/48 Postoperative LA: 6, OA: LA: 2.3%, LA: 14%*, ileus, LA: 6 OA: 8.2% OA: 0% 14%, OA: 11% Small bowel obstruction, LA: 1/43, OA: 1/61 Medical complications, LA: 2/43, OA: 4/61 Mortality, OA: 1/61 Not reported im pethidine, LA: 1.7, OA: 1.5 LA: 3.2*, OA: 5 LA: 6.3*, OA: 9.3 LA: 15%*, OA: 40% Not measured LA: 5*, OA: 6 LA: 0.6%*, LA: 5.7%, OA: 10% OA: 4.3% LA: 3%, OA: 4% Not reported Intra-abdominal bleeding, LA: 1/99 Enterocutaneous stula, OA: 3/130 Not reported NS, p = 0.8 NS No p value provided LA: 14%, OA: 25% LA: 0%, OA: 1.4% Re-operation, LA: 4/85, OA: 14/146 30 day Not reported for subgroups No 2835 days 1 followup visit Very signicant selection bias - low socioeconomic status & high co-morbidity pts for OA 30 days 24/104 were paediatric patients To solids, LA: 5, OA: LA: 2%, LA: 1, OA: 4, pLOS OA: 2% 1 LA: 7%, OA: 6% Abdominal wall haematoma, LA: 1/42 30 days ITT analysis not used ? Signicantly more females of reproductive age & higher co-morbidity in LA group Stratied analysis used Pt characteristics unavailable LA: 3.7*, OA: 5, MedV LA: 5.2, OA: 5.9 im pethidine, LA: 2.9, OA: 3.2 po naproxen, LA: 4, OA: 2.9 LA: 3.9*, OA: 4.6
Study
OT (min)
Katsuno et al. [31]
LA: 117* im pentazosine, LA: 2.7*, LA: 0.8, OA: 1.2 OA: 3.6 OA: 96
Fukami et al. [12] (n = 73)
LA: 97.9, im pentazosine, LA: 2.6*, OA: 92 LA: 0.7, OA: 0.9 OA: 5.1
Kirshtein et al. [13] LA: 45, (n = 90) OA: 34
Pokala et al. [29] (n = 104)
LA: 101*, Not reported OA: 82
Yau et al. [30] (n = 224)
LA: 55*, OA: 70
Lin et al. [37] (n = 229)
LA: 96*, OA: 68
Guller et al. [35] (n = 8,839)
Not Not reported reported
So et al. [36] (n = 231)
LA: 73, OA: 71
World J Surg
Table 3 continued TTOI (days) LOS (days) SSI IAA Other postoperative complications Not reported No Follow-up Notes
World J Surg
Study
OT (min)
Postoperative analgesia (days) LA: 22%, OA: 38% OA: 9.2, OA: 10.5 LA: 0%, OA: 14% LA: 28%, OA: 29%
Piksun et al. [32] (n = 42)
LA: 115, Not reported OA: 106
5 perforated cases converted due to lack of surgical experience ITT analysis not used for 10 converted cases
Wullstein et al. [34] Not Not reported (n = 299) reported
Not reported
Not reported
LA: 10.5%*, OA: 34% Fistula, LA: 1/217, OA: 1/82
LA: 4.6%, OA: 6%
No
Pt characteristics unavailable High initial conversion rate (27% total)learning curve
Trochar hernia, LA: 2/217 Haematoma, LA: 2/217, OA: 1/82
Stoltzing et al. [33] LA: 75, Not reported (n = 125) OA: 70, Conv: 90, MedV Ileus, LA: 5%, OA: 2% Mortality, OA: 5/45 Total, LA: LA: 11%, LA: 6%, 10, OA: OA: 18%, OA: 4% 11, Conv: some 11, MedV laparotomies LA: 6.3, OA: 6.4 Not reported LA: 5%, OA: 5% Not reported Not reported
No
Signicant selection bias as initially pts with suspected CA selected for OA ? longer symptom duration in LA No ITT not used. Pt characteristics unavailable
Khalili et al. [44] (n = 276)
LA: 86, OA: 70
Not reported
im intramuscular, pr per rectum, po per oral, PRN pro-re-nata (as required), MedV median value
* Statistically signicant difference (p \ 0.05)
123
World J Surg
studies recommendations would strongly favor LA over OA. Standardization of the laparoscopic and open interventions within studies can reduce internal validity errors and improve the studies external validity [38]. All of the nine studies that give information on the interventions report the number and size of trochars used with small inter-study variation (Table 2). The type of endoscope used is only reported by Fukami et al. [12]. Even though the rigid endoscope is the most commonly used instrument for these operations, failure to disclose the type used may affect the studys external validity, as other centers may use different types of endoscopes. Indeed, Fukami et al. [12] describe LA in CA with a exible endoscope at very good success rates and reduced complication rates. The method of ligation and resection of the mesoappendix and the appendix is also reported (Table 2) with some interstudy and intrastudy variation that can affect the rates of intra-abdominal complications and comparison within and between studies. A systematic review is being conducted by the Cochrane group comparing all the surgical techniques used to close the appendix base, and these ndings should provide some evidence of the signicance of variations in these studies. The use of a retrieval bag for the removal of the perforated or gangrenous appendix from the abdominal cavity can, theoretically, limit the spread of infection within the abdominal cavity and at the abdominal skin wound site. All of the studies report use of the retrieval bag. Fukami et al. [12], however, used this technique in only 28 of their 42 LA cases. This variation could introduce a signicant bias with regard to the ndings of the study, as one of the main assessment areas between LA and OA is postoperative complications. The authors themselves note that 4 of the 6 LA infective complications in their series occurred in patients undergoing LA where the retrieval bag was not used. The inclusion of these cases in the LA versus OA comparison of a small number of infective complications might have introduced a signicant alteration to the actual results, with a potential type I statistical error. So et al. [36] nd themselves in a similar situation. In the studies being considered, for OA the conventional approach is described by almost all authors, using a McBurneys, a Gridiron, or a paramedian incision (Table 2). There is some variation in the approach to either primary or secondary closure of the skin wounds. A recent systematic review and meta-analysis of such variation did not show any difference in the postoperative rates of surgical site infection (SSI) between the two closure techniques [39]. Kirshtein et al. [13] and So et al. [36] selectively use secondary closure in patients with a contaminated abdomen, whereas other authors report performing only primary closure. Similar variability appears
to exist in the use of a drain when an intra-abdominal abscess (IAA) is encountered. All of the studies advocated the use of antibiotics in CA, which involves one preoperative dose followed by regular intravenous antibiotics until the patients condition clinically improves and antibiotics are not required. In the absence of a clear care pathway, the decision to stop antibiotic administration becomes subjective and dependent to individual clinicians opinion and may introduce bias within the studies and affect external validity. One of the studies [37] does cite a basis for the cessation of antibiotic treatment, which is the resolution of pyrexia or negative microbiology culture results. The use of a protocol with a xed duration of antibiotic treatment, as reported in the study by Piksun et al. [32], could directly affect one of the study outcomespostoperative length of hospital stay (pLOS), eliminating any potentially signicant pLOS benets gained from LA. In addition, a wide range of broad spectrum antibiotics are used between studies, so it is not possible to achieve direct absolute comparison between study ndings. Assessment of bias risk All the studies appear to be using reasonable statistical tests with Students t-test measurement for continuous normally distributed variables such as operating time and 2 9 2 chi square analysis or Fishers exact test for categorical data [40, 41]. Signicance is tested at 5%. Intention to treat (ITT) analysis is appropriately used in all but four of the studies [13, 3133], introducing attrition bias into these studies [42]. The number of participants in these studies is relatively small and unequal owing to the lack of true randomization between the two operative groups, with the exception of the study by Guller et al., which is based on a stratication sample from a nationwide database [35]. None of the studies uses a power analysis, and therefore the possibility of signicant type II error is present [43]. The lack of randomization and the presence of selection, performance, and measurement bias in all of the studies affect their methodological validity (Table 4). Signicant problems, such as selection bias, absence of patient characteristics, absence of ITT analysis, and absence of any intervention characteristics, would only allow for classication of ndings/conclusions into level 3a to 3a evidence with regard to practice recommendation [18]. Measured outcomes The main outcomes measured for assessing the efcacy of LA against OA in CA in the studies appraised, with shortterm follow-up of up to 45 weeks, are shown on Table 3. All of the studies, although they agreeon the type of
123
World J Surg Table 4 Results of studies risk of bias after critical review Study Center Selection bias BC Katsuno et al. [31] Fukami et al. [12] One Japan One Japan Israel Pokala et al. [29] Yau et al [30] Lin et al. [37] Guller et al. [35] So et al. [36] Piksun et al. [32] One US One Hong Kong One Taiwan [1,000 hospitals U US One Singapore One U U M U M U NM U NM U NM NM M M M M NM M NM NM M M M M U U U U M M M M NM NM NM NM M M NM U C C C B Italy Wullstein et al. [34] One Germany Stoltzing et al. [33] One Germany Khalili et al [44] One US BC baseline characteristics, D diagnosis, ID incomplete data, SM statistical methods, PA power analysis, M met, U unclear, NM not met, A low risk, B moderate risk, C high risk U U NM M M M U M NM M B U NM M U M U M NM U C NM U M M M M U M NM M C U U U M M M U M NM U B NM U U M M M U M NM U C M NM U M NM NM M M M NM M M U U M M NM NM U M B C M D M U Performance Attrition bias bias ID M ITT NM M U Selective Detection Statistical reporting bias bias bias SM M PA NM U B External Overall validity/bias bias
Kirshtein et al. [13] One
Fig. 2 Operative time meta-analysis (all available data)
Fig. 3 Time to oral intake meta-analysis (all available data)
123
World J Surg
outcomes measured, fail to dene these outcomes, allowing for the widespread introduction of detection bias and deciencies in internal and external validity. Important measurement outcomes such as in-hospital and out-ofhospital costs, as well as other life quality issues, such as time to return to normal daily activities and work and cosmesis have not been assessed. In addition, long-term follow-up of patients is lacking, and complications such as hernias and intestinal obstruction lack evaluation. It is important to note the signicant mortality rate of 11% in OA in the study by Stoltzing et al., something that might be attributable to the initial selection bias of the study, which during its initial period required that patients with suspected CA were placed in the OA group. At the same time, the ASA score between LA and OA patients has not been statistically veried for absence of bias in either group. Operating time The lack of an operating time (OT) denition may potentially create internal and external validity problems surrounding this outcome. Most studies suggest that there is no signicant statistical difference in OT between LA
and OA. Four of the studies considered here report signicantly longer OT in LA compared to OA [2931, 37], whereas Fukami et al. [12] report a shorter OT for LA, but with the presence of reduced external validity because only experienced laparoscopic surgeons participated in this study. Meta-analysis of the four studies [31, 36, 37, 44] that report data in mean SD values indicates that OT is longer in LA by 12.8 min (p \ 0.01, 95% CI 8.417.3), but with a signicant statistical heterogeneity of I2 = 86% (Fig. 2). Exclusion of the study by So et al. from the analysis signicantly improves heterogeneity to 36%, but with no signicant change in the nal result (mean OT longer in LA: 21.4 min, 95% CI 15.427.3, p \ 0.01). Conclusions remain the same when only studies with moderate bias (group B) or all studies are included in the analysis (level of evidence 3a). Postoperative analgesia Regarding postoperative analgesia, one of the important advantages of LA, this is measured in four of the studies [12, 31, 36, 37], as the use of intramuscular and per-rectal or oral analgesic use. Three of the studies [12, 31, 36] conclude that there is signicantly less use of postoperative
Fig. 4 Length of hospital stay meta-analysis (all available data)
Fig. 5 Surgical site infection rate meta-analysis (all studies included)
123
World J Surg
Fig. 6 Intra-abdominal abscess rate meta-analysis (all studies included)
analgesia by LA patients. All three of these studies state that analgesia is given as required (PRN), whereas Lin et al. [37] do not dene analgesia use. The use of PRN analgesia may have some drawbacks as it depends on patient understanding and lack of embarrassment with regard to its use, as well as staff being available to administer it. A more objective scoring system for the assessment of postoperative pain would potentially be a more accurate way of measuring this outcome. No data meta-analysis was therefore performed for this outcome. Time to oral intake Time to oral intake (TTOI) is measured in six of the studies [12, 13, 31, 32, 36, 37], and two of the studies report the presence of ileus [29, 33] (Table 4). One variation between studies in this outcome was the measurement by Kirshtein et al. of time to solid oral intake [13] rather than any oral intake. Four of the six studies reporting on TTOI individually report a signicantly shorter TTOI in the LA group. Meta-analysis of data from the three studies [31, 36, 37] providing mean SD values (Fig. 3) shows a signicant difference between the two procedures, with mean difference of TTOI of 0.8 days (p \ 0.01, 95% CI: 0.51.15) shorter for LA and not signicant statistical heterogeneity, both when only group B or all studies are included in the analysis (level of evidence 3a). Length of hospital stay Similarly, length of stay in hospital (LOS) is only dened as postoperative length of stay by Fukami et al. [12] and Kirshtein et al. [13]. Giving results on total length of stay would introducesignicant bias, as preoperative time is not an intervention outcome. Five of the studies [12, 30, 31, 35,
37] individually report LOS as shorter in LA. Four studies providing mean SD values were included in this outcome meta-analysis (Fig. 4), showing a signicantly shorter mean LOS for LA of 1.1 day (p \ 0.01, 95% CI 0.51.6), but with unacceptably high statistical heterogeneity (I2 = 92%), and no change in ndings when only group B studies are included in the analysis (level of evidence 3a). Surgical site infection and intra-abdominal abscess rates The important outcomes of SSI and IAA are measured in all of the identied studies. Unfortunately, the great majority of studies do not explicitly state how the diagnosis was reached in each of these cases. A diagnosis of SSI would more accurately require positive organism culture conrmation rather than just a clinical diagnosis, and IAA diagnosis should be reached via imaging studies. None of the studies include the odds ratio in terms of the rate of each complication, and all of them only report signicance levels. The great majority of studies agree that there is reduced rate of SSI in LA and no signicant difference in IAA rates between LA and CA, whereas So et al. [36] only report a combined reduced incidence in LA. Guller et al. are the only authors to suggest no difference in the rate of SSI between the two procedures. Meta-analysis of the SSI rates reported (Fig. 5) indicates that this complication occurs signicantly less frequently in LA than in OA: OR 0.43 (95% CI 0.340.55) with signicant statistical heterogeneity (I2 = 73%) when all studies are used for the analysis, and OR values of 0.23 (95% CI 0.140.37) when only group B studies are used, with moderate statistical heterogeneity I2 = 61% (level of evidence 3a).
123
World J Surg
Meta-analysis of IAA rates (Fig. 6) shows no signicant difference between the two procedures: OR 1.24 (95% CI 0.841.84), with no statistical heterogeneity when all studies are used and OR 1.02 (95% CI 0.561.86) when only group B studies are used, with no statistical heterogeneity (level of evidence 3a). Conclusions With this systematic review and meta-analysis of reports from the medical literature we have tried to identify the best and most up-to-date evidence in regards to LA and OA in the management of adult patients with CA. Overall the quality of the studies found was intermediate to poor, with heterogeneity achieving only low grades of evidence recommendation. The absence of randomization and blinding and the presence of important methodological aws introduce a number of systematic errors and signicantly reduce the studies rigor. There appears to be a genuine attempt to justify the efcacy of LA in the majority of studies, but their retrospective nature and lack of care pathway standardization decreases their internal and external validity, restricting general interpretation and application of their results. A cautious interpretation of the ndings, having considered all their deciencies, indicates that LA may have a lower incidence of SSI than OA (level 3a evidence). There appears to be no difference with regard to IAA complication rates (level 3a evidence), the main LA drawback, as previously suggested. An important parameter neglected by these studies though is the long-term complications. The reported ndings provide the initial framework for higher level studies on LA versus OA in CA, making it possible to obtain better evidence on the subject and possibly gain a signicant benet from the adoption of a new procedure as the gold standard. Blinded randomized controlled trials comparing LA and OA in CA would be the next step. These are feasible as they have been performed in nCA in the past, comparing the two procedures. Similar studies can be conducted for CA, taking into consideration the problems with current evidence as identied through this review. In current clinical practice LA can be used in CA according to the surgeons discretion and laparoscopic experience. It should, however, be remembered that laparoscopy is a fairly new intervention requiring signicant resources and surgical expertise to reach maximum efciency. Industrialized countries appear to be meeting these technical and surgical criteria, but developing and thirdworld countries may nd a high level of practice difcult to achieve. In those instances conventional OA should be the surgical treatment of choice.
References
1. Rosenberg W, Donald A (1995) Evidence based medicine: an approach to problem solving. BMJ 310:11221126 2. Williams NMA, Everson NW, Jackson D, Johnstone JM (1998) Is the incidence of acute appendicitis really falling? Ann R Coll Surg Engl 80:122124 3. Addiss DG, Shaffer N, Fowler BS, Tauxe RV (1990) The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 132:910925 4. Livingston E, Woodward W, Sarosi GA, Haley RW (2007) Disconnect between incidence of nonperforated and perforated appendicitis. Implications for pathophysiology and management. Ann Surg 245:886892 5. Oliak D, Yamini D, Udani V, Lewis RJ, Vargas H, Arnell T, Stamos M (2007) Can perforated appendicitis be diagnosed preoperatively based on admission factors? J Gastrointest Surg 4:470474 6. Humes DJ, Simpson J (2006) Acute appendicitis. BMJ 333:530534 7. Blomqvist PG, Anderson RE, Granath F, Lambe MP, Ekborn AR (2001) Mortality after appendectomy in Sweden, 19871996. Ann Surg 233:455460 8. McBurney C (1894) The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg 20:38 9. Semm K (1983) Endoscopic appendectomy. Endoscopy 15:5964 10. Sauerland S, Lefering R, Neugebauer EAM (2004) Laparoscopic versus open appendicectomy for suspected appendicitis (review). Cochrane Database of Systematic Reviews Issue 3. Art. No CD001546. doi:10.1002/14651858.CD001546.pub2 11. Pedersen AG, Petersen OB, Wara P, Renning H, Qvist N, Laurberg S (2001) Randomised control trial of laparoscopic versus open appendectomy. Br J Surg 88:200205 12. Fukami Y, Hasegawa H, Sakamoto E, Komatsu S, Hiromatsu T (2007) Value of laparoscopic appendectomy in perforated appendicitis. World J Surg 31:9397 13. Kirshtein B, Bayme M, Domchik S, Mizrahi S, Lantsberg L (2007) Complicated appendicitis: laparoscopic or conventional surgery? World J Surg 31:744749 14. NHS P H R U (2008) Critical Appraisal Skills Programme10 questions to help you make sense of randomised control trials. Accessed 17 January 2009 15. NHS P H R U (2008) Critical Appraisal Skills Programme10 questions to help you make sense of a case control study. Accessed 17 January 2009 16. Higgins JPT, Green S (eds) (2008) Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1 [updated September 2008] The Cochrane Collaboration. www.cochranehandbook.org 17. Centre TNC, Review Manager (RevMan). 2008 The Cochrane Collaboration: Copenhagen 18. Oxford Centre of Evidence Based Medcine (2009) Levels of evidence. Accessed April 2009 19. Sileri P, Gentileschi P, Sica GS, Rossi P, Franceschilli L, Perrone F, Gaspari AL (2008) Abstract: laparoscopic appendectomy for complicated appendicitis. Society for Surgery of the Alimentary Tract 2008 Abstracts T1715:A883 20. Cueto J, DAllemagne B, Vazquez-Frias JA, Gomez S, Delgado F, Trullenque L, Fajardo R, Valencia S, Poggi L, Balli J, Diaz J, Gonzalez R, Mansur JH, Franklin ME (2006) Morbidity of laparoscopic surgery for complicated appendicitis: an international study. Surg Endosc 20:717720 21. Kiriakopoulos A, Tsakayiannis D, Linos D (2006) Laparoscopic management of complicated appendicitis. J Soc Lap Surg 10:453456
123
World J Surg 22. Towgh S, Chen F, Mason R, Katkhouda N, Chan L, Berne T (2006) Laparoscopic appendectomy signicantly reduces length of stay for perforated appendicitis. Surg Endosc 20:495499 23. Mancini GJ, Mancini ML, Nelson HS (2005) Efcacy of laparoscopic appendectomy in appendicitis with peritonitis. Am Surg 71:14 24. Ball CG, Kortbeek JB, Kirkpatrick AW, Mitchell P (2004) Laparoscopic appendectomy for complicated appendicitis: an evaluation of post-operative factors. Surg Endosc 18:969973 25. Johnston AB, Peetz ME (1998) Laparoscopic appendectomy is an acceptable alternative for the treatment of perforated appendicitis. Surg Endosc 12:940943 26. Lachin JM, Matts JP, Wei LJ (1988) Randomisation in clinical trials: conclusions and recommendations. Control Clin Trial 9:365374 27. Schulz KF, Grimes DA (2002) Blinding in randomised trials: hiding who got what. Lancet 359:696700 28. Schulz KF, Grimes DA (2002) Allocation concealment in randomised trials: defending against deciphering. Lancet 359:614 618 29. Pokala N, Sadhasivam S, Kiran RP, Parithivel V (2007) Complicated appendicitisis the laparoscopic approach appropriate? A comparative study with the open approach: Outcome in a community hospital setting. Am Surg 73:737741 30. Yau KK, Siu WT, Tang CN, Yang GPC, Li MKW (2007) Laparoscopic versus open appendectomy for complicated appendicitis. J Am Coll Surg 205:6065 31. Katsuno G, Nagakari K, Yoshikawa S, Sugiyama K, Fukunaga M (2009) Laparoscopic appendectomy for complicated appendicitis: a comparison with open appendectomy. World J Surg 33:208214 32. Piksun G, Kozic D, Rajpal S, Shaftan G, Fogler R (2001) Comparison of laparoscopic, open and converted appendectomy for perforated appendicitis. Surg Endosc 15:660662 33. Stoltzing H, Thon K (2000) Perforated appendicitis: is laparoscopic operation adviseable? Digest Surg 17:610616 34. Wullstein C, Barkhausen S, Gross E (2001) Results of laparoscopic vs conventional appendectomy in complicated appendicitis. Dis Colon Rectum 44:17001705 35. Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks E, Pietrobon P (2004) Laparoscopic versus open appendectomy. Outcomes comparison based on a large administrative database. Ann Surg 239:4352 36. So JBY, Chiong E-C, Chiong E, Cheah W-K, Lomanto D, Goh P, Kum C-K (2002) Laparoscopic appendectomy for perforated appendicitis. World J Surg 26:14851488 37. Lin H-F, Wu J-M, Tseng L-M, Chen K-H, Huang S-H, Lai I-R (2006) Laparoscopic versus open appendectomy for perforated appendicitis. J Gastrointest Surg 10:906910 38. Brewer M (2000) Research design and issues of validity. Cambridge University Press, Cambridge 39. Henry MC, Moss RL (2005) Primary versus delayed wound closure in complicated appendicitis: an international systematic review and meta-analysis. Ped Surg Intern 21:625630 40. Greenwood PE, Nikulin MS (1996) A Guide to Chi-Squared Testing. Wiley, New York 41. Fisher RA (1922) On the interpretation of v2 from contingency tables, and the calculation of P. J R Stat Soc 85:8794 42. Lachin JM (2000) Statistical considerations in the intent-to-treat principle. Control Clin Trial 21:167189 43. Cohen J (1988) Statistical power analysis for the behavioural sciences, 2nd edn. Lawrence Erlbaum Associates, Mahwah 44. Khalili TM, Hiatt JR, Savar A, Lau C, Margulies DR (1999) Perforated appendicitis is not a contraindication to laparoscopy. Am Surg 65:965967
123
Вам также может понравиться
- ATLS 8th, Compendium of Changes PDFДокумент26 страницATLS 8th, Compendium of Changes PDFJuan Carlos SantamariaОценок пока нет
- Aquacel Vs Wet-To-dry GauzeДокумент3 страницыAquacel Vs Wet-To-dry GauzeJuan Carlos SantamariaОценок пока нет
- Effect of Silver Dressings On Fibroblast FunctionДокумент6 страницEffect of Silver Dressings On Fibroblast FunctionJuan Carlos SantamariaОценок пока нет
- Research Article: Single Incision Laparoscopic Surgery For Acute Appendicitis: Feasibility in Pediatric PatientsДокумент3 страницыResearch Article: Single Incision Laparoscopic Surgery For Acute Appendicitis: Feasibility in Pediatric PatientsJuan Carlos SantamariaОценок пока нет
- Acute Appendicitis - A 5-Year Review of Histopathology and Clinical PresentationДокумент4 страницыAcute Appendicitis - A 5-Year Review of Histopathology and Clinical PresentationJuan Carlos SantamariaОценок пока нет
- Article 15Документ5 страницArticle 15Juan Carlos SantamariaОценок пока нет
- Laparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Документ5 страницLaparoscopic Appendectomy For Complicated Appendicitis - An Evaluation of Postoperative Factors.Juan Carlos SantamariaОценок пока нет
- Appendicitis SchwartzДокумент47 страницAppendicitis SchwartzJuan Carlos SantamariaОценок пока нет
- Silver Antimicrobial Dressings in Wound Management PDFДокумент12 страницSilver Antimicrobial Dressings in Wound Management PDFJuan Carlos SantamariaОценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Training in Microvascular Surgery UsingДокумент4 страницыTraining in Microvascular Surgery UsingBob sponjaОценок пока нет
- Larana Inc.: Educational Consultancy ServicesДокумент9 страницLarana Inc.: Educational Consultancy ServicesElo GonçalvesОценок пока нет
- Management Project On Services Hospital in LahoreДокумент20 страницManagement Project On Services Hospital in LahoreReaderОценок пока нет
- @MedicalBooksStore 2013 Abdominal PDFДокумент383 страницы@MedicalBooksStore 2013 Abdominal PDFEmanuel MessiasОценок пока нет
- Surgical Techs Little Black BookДокумент18 страницSurgical Techs Little Black BookMichael Lester100% (5)
- ObwegeserДокумент25 страницObwegeserR KОценок пока нет
- 06 - June RsmiДокумент57 страниц06 - June RsmiJZik SibalОценок пока нет
- Extracted Pages From Cervical Spine Minimally Invasive and Open Surgery 2ED 2022Документ17 страницExtracted Pages From Cervical Spine Minimally Invasive and Open Surgery 2ED 2022Carlos Miglietti100% (1)
- Hinkle PPT CH 17Документ25 страницHinkle PPT CH 17maniz442100% (2)
- Dr. Nasir: Curriculum VitaeДокумент15 страницDr. Nasir: Curriculum VitaeJoshua BoltonОценок пока нет
- Functional Endoscopic Sinus Surgery (Fess) (3) JДокумент20 страницFunctional Endoscopic Sinus Surgery (Fess) (3) JJulianthy SuentoОценок пока нет
- Duties of Circulating NurseДокумент11 страницDuties of Circulating NurseHuemer Uy100% (1)
- Hoegh Fleet v. TuralloДокумент13 страницHoegh Fleet v. TuralloMichael HardingОценок пока нет
- MerinДокумент5 страницMerinFAZEL RAHMANОценок пока нет
- 12 Regional RepresentativesДокумент3 страницы12 Regional RepresentativesplastaukОценок пока нет
- Septoplasty, Rhinoplasty, Septorhinoplasty, Turbinoplasty or TurbinectomyДокумент4 страницыSeptoplasty, Rhinoplasty, Septorhinoplasty, Turbinoplasty or TurbinectomyAldy PratamaОценок пока нет
- Surgical Junior Doctor HandbookДокумент27 страницSurgical Junior Doctor Handbooktalal.fazmin1Оценок пока нет
- Midface Fractures PART IIДокумент64 страницыMidface Fractures PART IIJomi Porinchu100% (1)
- WHO Surgical Safety Checklist: Sign in Sign OutДокумент1 страницаWHO Surgical Safety Checklist: Sign in Sign OutYoevfa Al-FathОценок пока нет
- Alexanders Care of The Patient in Surgery 16th Edition Rothrock Test BankДокумент13 страницAlexanders Care of The Patient in Surgery 16th Edition Rothrock Test BankAlexisLewisbjds100% (63)
- Kahn 2003 The Revelation of Organizational TraumaДокумент17 страницKahn 2003 The Revelation of Organizational Traumanivi99delhiОценок пока нет
- 35.tumorile Benigne - DR - Ouatu ConstantinДокумент29 страниц35.tumorile Benigne - DR - Ouatu Constantinsilviu0mihai_1Оценок пока нет
- AppendexДокумент48 страницAppendexFahmeeda AhmedОценок пока нет
- Trauma Room Checklist February 2022Документ6 страницTrauma Room Checklist February 2022Ben PolegaОценок пока нет
- OSU Orthopaedics Accomplishments Report 2010Документ32 страницыOSU Orthopaedics Accomplishments Report 2010osuorthopaedicsОценок пока нет
- GSTKДокумент5 страницGSTKCristobal Salinas PetersenОценок пока нет
- Yang 2018Документ9 страницYang 2018moncoyaco08Оценок пока нет
- Procedure List With AmountДокумент20 страницProcedure List With AmountMadhavan MadeshsanthoshОценок пока нет
- Etheric Medicine SurgeryДокумент45 страницEtheric Medicine SurgeryAndre3893100% (1)
- Hospital La Comunidad de Santa Rosa: Chapter I: Problem and Its SettingsДокумент15 страницHospital La Comunidad de Santa Rosa: Chapter I: Problem and Its SettingsMeynard MagsinoОценок пока нет