Академический Документы
Профессиональный Документы
Культура Документы
Anemia in Pregnancy
Загружено:
Shalini ShanmugalingamИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Anemia in Pregnancy
Загружено:
Shalini ShanmugalingamАвторское право:
Доступные форматы
Anaemia in pregnancy
By
Dr Samar K Basu, Senior Consultant (Obst &Gynae) G M Modi Hospital
Definition: Anaemia is defined as reduction in circulating haemoglobin mass below the critical level. The normal haemoglobin (Hb) concentration in the body is between 12-14 grams percent. WHO has accepted up to 11gm percent as the normal haemoglobin level in pregnancy. Therefore any haemoglobin level below 11gm in pregnancy should be considered as anaemia. However in India and most of the other developing countries the lower limit is often accepted as 10 gms percent.
Degree of Anaemia: Anaemia is often classified as mild degree (9-11 gm %), moderate (7-9 gms %), severe (4-7 gm %) and very severe (<4gm %). It is also classified according to Haematocrit (PCV) %.
Incidence: Anaemia in pregnancy is present in very high percentage of pregnant women in India. Exact data is not available about the prevalence of nutritional anaemia. However according to WHO, the prevalence of Anaemia in pregnancy in south East Asia is around 56%. In India incidence of anaemia pregnancy has been noted as high as 40-80%.
Magnitude of the problem: Pregnancy anaemia is one of the important public health problems not only in India but also in most of the south East Asian countries. About 416% of maternal death is due to anaemia. It also increases the maternal morbidity, fetal and neonatal mortality and morbidity significantly.
Anemia in pregnancy is a condition with effects that may be deleterious to mothers and fetuses. Indeed, it is a known risk factor for many maternal and fetal complications.
Maternal risk during Antenatal period: poor weight gain. Pre term labours, PIH, placenta previa, accidental Hg, eclampsia, premature rupture of membrane (PROM) etc. Maternal risk during intranatal period: Dysfunctional labour, intranatal hemorrhage, shock, anesthesia risk, cardiac failure Maternal risk during postnatal period: Postnatal sepsis, sub involution, embolism
Fetal and Neonatal risk: Complications include prematurity, low birth weight, poor Apgar score, fetal distress, neonatal distress requiring prolonged resuscitation, and neonatal anemia due to poor reserve. Infants with anemia have higher prevalence of failure to thrive, poorer intellectual developmental milestones, and higher rates of morbidities and neonatal mortalities than infants without anemia. Moreover, babies whose mothers had AIP during their first trimester in utero experienced higher rates of cardiovascular morbidities and mortalities in their adult lives than babies whose mothers did not have AIP.
Causes: 1) Physiological Pregnancy causes a state of hydraemic plethora. There is
disproportionate increase of plasma volume during pregnancy leading to apparent reduction of RBC, haemoglobin and haematocreit value. Hb is consequently reduced to a varying extent occasionally as low as 80%. The dilution picture is normochromic and normocytic. This is so called physiological anaemia. 2) Acquired- Nutritional a) Iron deficiency anaemia (60%), b) Macrocytic anaemia (10%) due to deficiency of folic acid and/or vitaminB12 c) Dimorphic and protein deficiency anaemia (30%) both due to deficiency of iron and folic acid and /or vitaminB12 d) Protein deficiency due to protein deficiency in extreme malnutrition
Hemolytic or Haemorrhagic (due to acute blood loss,; chronic (hook worm, bleeding piles)
Iron and folate deficiency is by far the most important ateological factor. Haemolytic anaemia may be caused by haemoglobinopathies, drug reaction or infestation with malaria parasites. Risk factors
Sociodemographic factors (age, level of formal education, marital status, areas and cities of residence) Obstetrical factors (gravidity, parity, history of previous preterm or gestational-age deliveries, plurality of pregnancy multiple Or singleton) Small-for-
Behavioral factors (smoking or tobacco usage, alcohol usage, utilization of prenatal care services) Medical conditions (diabetes, renal or cardio-respiratory diseases, chronic hypertension AIP anemia in pregnancy
Clinical presentation:
To start with the pregnant women with anaemia may not have any symptom as the body system get adjusted to reduce haemoglobin mass. However she may represent with vague complain of ill health, fatigue, loss of appetite, digestive upset, dyspnoea, palpitation etc. Clinical examination may reveal pallor, pale nails, koilonychias, pale tongue etc. In severe cases there may be oedema also.
Investigations:
Haemoglobin estimation and study of peripheral smear is good indicator for diagnosis of anaemia. There may be several methods for estimation of Hb. However inspite of limitation of present method of Hb estimation, it is a useful method of diagnosis for anaemia.
Peripheral smear examination is another simple method for diagnosis of anaemia. If the peripheral smear looks pale, there is hypochromia (large central vacuoles) and microcytosis (small deformed red cells). It suggests iron deficiency. In case of megaloblastic anaemia, there would be microcytosis, hyper segmentation of nutrophils and fully haemoglobinised red blood cells. In Haemolytic anaemia there would be poly chromatic cells, stippled cells and target cells. Other special laboratory investigations total iron binding capacity (TIBC), serum feritin (SF), serum folic acid, bone marrow studies are not available every where and expesive.Therefore they are not for routine use to diagnose pregnancy anaemia.
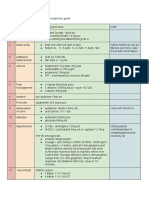
Management:
A pregnant woman requires about 2 to 4.8 mg iron every day. To have it from the dietary sources she must consume 20-48 mg of dietary iron. This is practically impossible in India because of average vegetarian diet does not contain more than 10-15 mg of iron and the phytate content in it further reduces iron absorption. Moreover majority of Indian women enter pregnancy already with iron depleted condition. The iron store is markedly diminished when there is fall in Hb values. Therefore in India there is a need for routine iron supplementation to all pregnant women.
Prophylaxis:
It is advisable to build up iron store before a woman marries and becomes pregnant. This can be achieved by 1) Routine screening for anaemia for adolescent girls form school days 2) Encouraging iron reach foods 3) Fortification of widely consumed food with iron 4) Providing iron supplementation from school days 5) Annual screening for those with risk factors Iron rich foods: Pulses, cereals, jaggery, Beet root, Green leafy vegetables, meat, liver, egg, fish, legumes, dry beans, and iron reached white breads etc.
Oral Iron therapy:
Oral Iron is safe, inexpensive & effective way to administer iron. Oral route should be the route of choice in routine cases. Parenteral route of iron therapy should only be considered when oral route is not possible due to any reason. If all pregnant women receive routine iron and folic acid, it is possible to prevent nutritional anaemia in pregnant women. National nutritional anaemia prophylaxis program advices 60milligrams elemental iron and 500 micrograms of folic acid daily for 100 days to all pregnant women. However it is suggested that 120 milligram of elemental iron and 1 milligram folic acid are the optimum daily doses needed to prevent pregnancy anaemia.The higher dose in Indian women is required as they start pregnancy with low or absent iron stores due to poor nutrition and frequent infection like hook worm and malaria.
How to select the iron salt:
There are many iron preparations available in the market and a clinician is often confused as to which iron preparation should be advised to the patient. Ferrous sulphate is least expensive and best absorbed form of iron. It also allows more elemental iron absorbed per gram administered. If for some reasons this is not tolerated, then ferrous gluconate, fumarate are the next choice for iron therapy. However the iron salt should be selected based on compliance of the patient, tolerance, side effects, clinical situation of the patient and availability of a particular salt. Oral iron must be continued for 3-6 months after haemoglobin has come to normal levels. This helps in building iron stores.
Timing of oral iron intake in relation to food:
It is true that if iron is taken with food there is some reduction in side effect related to GI Tract. However staple Indian diet consists of cereals and cereals contain phytic acid. Phytate reduce iron absorption. Addition of vitamin C in medicine or in the diet enhances iron absorption. If the predictable rise in haemoglobin does not occur after oral iron therapy, one must find out the possible reasons. Some of the reasons area as follows
1. Incorrect diagnosis. 2. Mal-absorption syndrome 3. Presence of chronic infection 4. Loss of iron from the body 5. Lack of patients compliance 6. Ineffective release of iron from a particular preparation
Parenteral Iron:
The indications for parenteral iron therapy are as follows
1. Cannot tolerate side effects of oral iron 2. Suffers from inflammatory bowel disease 3. Patient does not comply 4. Patient near term
The defaulting rate with oral iron therapy in pregnant women is fairly high because of gastrointestinal side effects like nausea, vomiting, diarrhoea and abdominal pain. Sometimes pregnant women present with severe anaemia after 30-32 weeks of pregnancy and in those cases time is an important factor to improve haemoglobin status. In such situations parenteral iron therapy is indicated. Parenteral iron can be given by intramuscular or intravenous route. Iron- sorbitol -citric acid complex (jectofer (1.5ml) 75mg is used for intramuscular route only. On the other hand iron-dextran can
be used both by intramuscular and intravenous route. The main drawback of
intramuscular iron is the pain and staining of the skin at injection site, myalgia, arthralgia and injection abscess. Intravenous route should be reserved for those who do not wish to have frequent intramuscular injections. Iron can be given intravenously at one shot as total dose infusion (TDI). Utmost caution is needed for total dose iron therapy via intravenous route because of severe anaphylactic reaction that may occur.
TDI reaction: Immediate vascular collapse, tachycardia, dyspnoea, cyanosis vomiting, pyrexia etc. Therefore total dose of iron therapy by intravenous route should only be given in a hospital setting where facilities are available to manage severe reaction after iron dextran.
How to calculate TDI: total dose of infusion of iron is calculated as: (15- patient s Hb%) x body weight in Kg x3 =Mg.
Contraindication of parenteral iron therapy: Nephritis, cardio respiratory disease, allergy
Severe anaemia in late pregnancy (after 32 weeks):
These patients should ideally be managed in a hospital setting. They may or may not present with heart failure. However they all need urgent admission and bed rest. They need complete rest with sedation, oxygen. In case, of CCF patient should be given digitalis, diuretics and packed red cells. Packed red cells are preferred choice for severe anaemia in later part of pregnancy. This should be infused along with diuretics. Once the patient is stabilized total dose infusion of iron Dextran may be considered.
Management of endemic infection
Malaria and hook worm infection are major factor causing anaemia in pregnancy due to haemolysis and Chr. Blood loss respectively. Malaria causes low birth wt. babies, parasitaemia in neonates, haemolysis of RBCs and becomes a persistent source of infection. Therefore one should not hesitate to treat malaria in pregnancy. The preferred drug is chloroquine. Malaria prophylaxis should also be given to pregnant women in areas where malaria is endemic. Like wise Albendazole or mebendazole is recommended to all pregnant women after the first trimester of pregnancy. To prevent recurrence, patients should be advised to use footwear, improve sanitation, and personal hygiene.
This document was created with Win2PDF available at http://www.win2pdf.com. The unregistered version of Win2PDF is for evaluation or non-commercial use only.
Вам также может понравиться
- Arm Sling Osce - by DR ShaliniДокумент3 страницыArm Sling Osce - by DR ShaliniShalini ShanmugalingamОценок пока нет
- PaediatricTuina Elisa RossiДокумент7 страницPaediatricTuina Elisa Rossideemoney3100% (1)
- Emotion Code-Body Code Consent AgreementДокумент1 страницаEmotion Code-Body Code Consent Agreementapi-75991446100% (1)
- Preeclampsia, HELLP Syndrome, Eclampsia and other Hypertensive Disorders of PregnancyОт EverandPreeclampsia, HELLP Syndrome, Eclampsia and other Hypertensive Disorders of PregnancyРейтинг: 2 из 5 звезд2/5 (1)
- 2017 - Cabrini Practice OSCE - Station 1 - BurnsДокумент5 страниц2017 - Cabrini Practice OSCE - Station 1 - BurnsShalini ShanmugalingamОценок пока нет
- Anemiain PregnancyДокумент4 страницыAnemiain PregnancyShalini ShanmugalingamОценок пока нет
- Albuterol, Accuneb Drug CardДокумент2 страницыAlbuterol, Accuneb Drug Carddnw876Оценок пока нет
- 09.Project-Hospital Management SystemДокумент37 страниц09.Project-Hospital Management Systemzahidrafique0% (1)
- Anemia in PregnancyДокумент20 страницAnemia in PregnancyMargaretha UsbokoОценок пока нет
- SIM - Anemias of PregnancyДокумент17 страницSIM - Anemias of PregnancyGabrielle EvangelistaОценок пока нет
- Anemia in PregnancyДокумент53 страницыAnemia in PregnancysyafahalimОценок пока нет
- Anemia PregnancyمحاضرةДокумент33 страницыAnemia PregnancyمحاضرةSamia Abu AishiaОценок пока нет
- Pre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandPre-eclampsia, (Pregnancy with Hypertension And Proteinuria) A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОценок пока нет
- Obgyn Anemia in Pregnancy For UG ClassДокумент35 страницObgyn Anemia in Pregnancy For UG ClassimranОценок пока нет
- Anemia in PregnancyДокумент9 страницAnemia in PregnancyKarina Madriaga100% (2)
- Hypertensive Disorder in PregnancyДокумент56 страницHypertensive Disorder in PregnancyESCA GabrielОценок пока нет
- Post Partum HemorrhageДокумент12 страницPost Partum HemorrhageCristinaCaprosОценок пока нет
- Ectopic Pregnancy - CSДокумент14 страницEctopic Pregnancy - CSMASII100% (1)
- Obgyn Anemia in Pregnancy For UG ClassДокумент35 страницObgyn Anemia in Pregnancy For UG ClassMunirathna ChandruОценок пока нет
- Anaemia During PregnancyДокумент21 страницаAnaemia During Pregnancybotet_2306100% (2)
- Anemia in Pregnancy: Rabika Fatima Rabia Saleem Almina RehmanДокумент26 страницAnemia in Pregnancy: Rabika Fatima Rabia Saleem Almina RehmanAlmina Rehman100% (2)
- Abnormal Uterine ActionДокумент48 страницAbnormal Uterine ActionKavya S Mohan0% (1)
- Hyperemesis GravidarumДокумент16 страницHyperemesis GravidarumBabi PanggangОценок пока нет
- Gestational Diabetes MellitusДокумент25 страницGestational Diabetes MellitusMazlina MaidinОценок пока нет
- RH Incompatibil TY: What Is RH Incompatibility?Документ15 страницRH Incompatibil TY: What Is RH Incompatibility?Jannah Marie A. DimaporoОценок пока нет
- OligohydramniosДокумент4 страницыOligohydramniossalamredОценок пока нет
- 260120200anemia in PregnancyДокумент40 страниц260120200anemia in Pregnancyraph faith100% (1)
- GDMДокумент11 страницGDMNikki GarlejoОценок пока нет
- Family PlanningДокумент13 страницFamily PlanningYana PotОценок пока нет
- Pregnancy Induced Hypertension: DefinitionДокумент7 страницPregnancy Induced Hypertension: Definitionkristine hinaresОценок пока нет
- Multiple PregnancyДокумент20 страницMultiple PregnancyNurul Fahmiza TumiranОценок пока нет
- Fetal DistressДокумент33 страницыFetal DistressYara H QaisiОценок пока нет
- MNT I Case Study 1 Anemia in Pregnancy - XhouДокумент18 страницMNT I Case Study 1 Anemia in Pregnancy - Xhouapi-254534492100% (1)
- Placental Abruption PresentationДокумент30 страницPlacental Abruption PresentationNafisat AdepojuОценок пока нет
- Medical and Surgical Complicating PregnancyДокумент70 страницMedical and Surgical Complicating PregnancyGunaОценок пока нет
- Abnormal Labor. BBBB WWPPTXДокумент53 страницыAbnormal Labor. BBBB WWPPTXHamss Ahmed100% (2)
- Meconium Aspiration Syndrome (MAS)Документ12 страницMeconium Aspiration Syndrome (MAS)Angela AmaoОценок пока нет
- Uterine ProlapseДокумент11 страницUterine ProlapseMelDred Cajes BolandoОценок пока нет
- Anemia in PregnancyДокумент7 страницAnemia in PregnancyLenrok AdrianОценок пока нет
- Anaemia in Pregnancy: Dr. Lama MehaisenДокумент11 страницAnaemia in Pregnancy: Dr. Lama MehaisenWendy EvansОценок пока нет
- Hyperemesis Gravidarum PresentationДокумент22 страницыHyperemesis Gravidarum PresentationMaricar Sanson FelicianoОценок пока нет
- Anemia in PregnancyДокумент18 страницAnemia in Pregnancysaagiba100% (1)
- Anemia in PregnancyДокумент34 страницыAnemia in PregnancyHannah Halim100% (1)
- Hydramnios and Premature Rupture of MembranesДокумент5 страницHydramnios and Premature Rupture of Membranessarguss14Оценок пока нет
- Malpresentation and Malposition - BreechДокумент21 страницаMalpresentation and Malposition - BreechNishaThakuri100% (1)
- Infant of Diabetic MotherДокумент17 страницInfant of Diabetic Motheral_humaira91Оценок пока нет
- PIHДокумент18 страницPIHArtyom GranovskiyОценок пока нет
- PREECLAMPSIAДокумент60 страницPREECLAMPSIAMary Grace MasОценок пока нет
- 18 - Oligohydramnios and PolyhydramniosДокумент3 страницы18 - Oligohydramnios and PolyhydramniosSu OoОценок пока нет
- Fetal Well BeingДокумент23 страницыFetal Well BeingKrishnaveni Murugesh100% (1)
- Anemia in PregnancyДокумент79 страницAnemia in Pregnancypat duaОценок пока нет
- Case - Eclampsia FinalДокумент84 страницыCase - Eclampsia FinalKimberley Anne SantosОценок пока нет
- Anemia in PregnancyДокумент14 страницAnemia in PregnancyWern Ching Lee50% (2)
- Pre and Post PregnancyДокумент23 страницыPre and Post PregnancyJitendra ChaudharyОценок пока нет
- NCM - Pregancy Induced HypertensionДокумент5 страницNCM - Pregancy Induced HypertensionZam PamateОценок пока нет
- Hypertension in PregnancyДокумент45 страницHypertension in PregnancyMary Anne Cabalza ApinardoОценок пока нет
- Pre EclampsiaДокумент8 страницPre EclampsiaJamie Agbannawag100% (1)
- Breast Problems After DeviveryДокумент19 страницBreast Problems After DeviverySanthosh.S.UОценок пока нет
- Gestational DiabetesДокумент52 страницыGestational Diabetestammycristobalmd100% (8)
- Normal & Abnormal LabourДокумент5 страницNormal & Abnormal Labourra100% (1)
- Postpartum BluesДокумент6 страницPostpartum BluesmiL_kathrinaОценок пока нет
- Drugs During PregnancyДокумент9 страницDrugs During Pregnancyjeelani saimaОценок пока нет
- Abortion: DEFINITION-Abortion Is The Separation Partial orДокумент77 страницAbortion: DEFINITION-Abortion Is The Separation Partial orPadmaОценок пока нет
- OBG DrugsДокумент30 страницOBG DrugsSANAОценок пока нет
- 19 Myths and Misconceptions About FP - 0Документ3 страницы19 Myths and Misconceptions About FP - 0iammerbinpransisko100% (1)
- Nursing the NeonateОт EverandNursing the NeonateMaggie MeeksОценок пока нет
- History Taking Frcem Osce StationДокумент7 страницHistory Taking Frcem Osce StationShalini Shanmugalingam100% (1)
- Fundoscopy Examination by DR Shalini S.Документ77 страницFundoscopy Examination by DR Shalini S.Shalini ShanmugalingamОценок пока нет
- Gi Emergencies: Jasleen Singh, PGY-5 July 15, 2019Документ51 страницаGi Emergencies: Jasleen Singh, PGY-5 July 15, 2019Shalini ShanmugalingamОценок пока нет
- AsthmaДокумент5 страницAsthmaShalini ShanmugalingamОценок пока нет
- Monash Osce Handbook 2019Документ31 страницаMonash Osce Handbook 2019Shalini Shanmugalingam100% (2)
- Chronic Rhinosinusitis 2012Документ305 страницChronic Rhinosinusitis 2012Sorina StoianОценок пока нет
- Chapter 1-3 FinalДокумент44 страницыChapter 1-3 FinalShalini ShanmugalingamОценок пока нет
- Lampiran 1 Daftar Riwayat HidupДокумент8 страницLampiran 1 Daftar Riwayat HidupShalini ShanmugalingamОценок пока нет
- Ekg TBMДокумент42 страницыEkg TBMShalini ShanmugalingamОценок пока нет
- The Lancet Oct 4, 2003 362, 9390 Proquest Research LibraryДокумент9 страницThe Lancet Oct 4, 2003 362, 9390 Proquest Research LibraryShalini ShanmugalingamОценок пока нет
- Neuro DevelopmentДокумент31 страницаNeuro DevelopmentShalini ShanmugalingamОценок пока нет
- Genetics of AutismДокумент7 страницGenetics of AutismShalini ShanmugalingamОценок пока нет
- Pathophysiology of Angina PectorisДокумент2 страницыPathophysiology of Angina PectorisShalini ShanmugalingamОценок пока нет
- Block 4 Lung PathДокумент31 страницаBlock 4 Lung PathShalini ShanmugalingamОценок пока нет
- Anemia in Pregnancy : Related Risk Factors in Under Developed AreaДокумент4 страницыAnemia in Pregnancy : Related Risk Factors in Under Developed AreaShalini ShanmugalingamОценок пока нет
- Endobronchial Tuberculosis in Children: Dis ChestДокумент21 страницаEndobronchial Tuberculosis in Children: Dis ChestShalini ShanmugalingamОценок пока нет
- Lung CancerДокумент2 страницыLung CancerShalini ShanmugalingamОценок пока нет
- Covid Vaccine Statistics PDFДокумент12 страницCovid Vaccine Statistics PDFNICOLAEОценок пока нет
- Methodology and Project Design 4Документ4 страницыMethodology and Project Design 4api-706947027Оценок пока нет
- Diagram of Pathophysiology CancerДокумент5 страницDiagram of Pathophysiology CancerKristaMaeC.Lazo0% (3)
- Fped 2019 00227Документ7 страницFped 2019 00227Syaifudin LutfiОценок пока нет
- Master Drug ChartДокумент22 страницыMaster Drug ChartMahadhir AkmalОценок пока нет
- b2 CoolДокумент2 страницыb2 CoolGanesh kumarОценок пока нет
- Economic Impact of Medication Nonadherence by Disease Groups: A Systematic ReviewДокумент13 страницEconomic Impact of Medication Nonadherence by Disease Groups: A Systematic ReviewtapsemiОценок пока нет
- Events and Affairs Request Ms Gay BarakoДокумент2 страницыEvents and Affairs Request Ms Gay Barako잔돈Оценок пока нет
- Health Talk TopicsДокумент3 страницыHealth Talk Topicsvarshasharma0562% (13)
- PlagueДокумент31 страницаPlaguelulondon1Оценок пока нет
- Theories of AddictionДокумент30 страницTheories of AddictionAmyOesau100% (1)
- Patient Positioning (Sims, Orthopneic, Dorsal Recumbent) Guide (2020)Документ28 страницPatient Positioning (Sims, Orthopneic, Dorsal Recumbent) Guide (2020)JOSHUA DICHOSO100% (1)
- Irda Non Payable ListДокумент21 страницаIrda Non Payable ListMUKESH SINGHОценок пока нет
- Why Worry About: High Blood Pressure?Документ8 страницWhy Worry About: High Blood Pressure?mattvestrandОценок пока нет
- MK 2866Документ3 страницыMK 2866haydunn55Оценок пока нет
- Leah Cronley ResumeДокумент2 страницыLeah Cronley Resumeapi-343462331Оценок пока нет
- ST George's Outpatient Services Directory & Referral Guide 2010/2011Документ116 страницST George's Outpatient Services Directory & Referral Guide 2010/2011St George's Healthcare NHS TrustОценок пока нет
- Intake and Output PPT - 1Документ44 страницыIntake and Output PPT - 1Prajna TiwariОценок пока нет
- MEDS 1. Diabetic Retinopathy: Practice Essentials, Pathophysiology, EtiologyДокумент14 страницMEDS 1. Diabetic Retinopathy: Practice Essentials, Pathophysiology, EtiologyVivi DeviyanaОценок пока нет
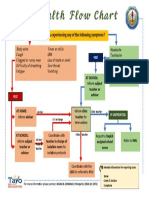
- Health Flow ChartДокумент1 страницаHealth Flow ChartAlex Cainoy JrОценок пока нет
- ProRoot MTA BrochureДокумент12 страницProRoot MTA BrochureAdela FechetaОценок пока нет
- Medtronic Earnings Presentation FY16Q4 FINALДокумент21 страницаMedtronic Earnings Presentation FY16Q4 FINALmedtechyОценок пока нет
- Paper-Organ DonationДокумент7 страницPaper-Organ Donationapi-400417633Оценок пока нет
- Nursing Care of The ElderlyДокумент11 страницNursing Care of The ElderlySpislgal PhilipОценок пока нет
- Adaptive Immunity: Yanne Pradwi EfendiДокумент25 страницAdaptive Immunity: Yanne Pradwi EfendiMelissa Indah SariОценок пока нет
- Surgical Scrubbing Workbook 2020Документ19 страницSurgical Scrubbing Workbook 2020Alistair LauОценок пока нет