Академический Документы
Профессиональный Документы
Культура Документы
4th Lecture (NCM106 CA I) Care of Clients in Cellular Aberrations, ABC, Emergency and Disaster Nursing
Загружено:
Kamx Mohammed100%(3)100% нашли этот документ полезным (3 голоса)
506 просмотров14 страниц1. The document discusses cellular aberrations and the cell cycle. It describes the four phases of the cell cycle - G1, S, G2, and M phase - and notes a fifth phase, G0, as a resting phase.
2. Oncology nursing is described as caring for cancer patients through the wide range of physical, emotional, social, and spiritual crises that arise. Nurses must support patients using standards of practice and the nursing process.
3. Cellular aberrations, or cancers, are characterized by abnormal cell growth and the potential to spread, or metastasize. The term cancer refers to diseases where cells grow and spread unrestrained.
Исходное описание:
:)
Авторское право
© Attribution Non-Commercial (BY-NC)
Доступные форматы
PDF, TXT или читайте онлайн в Scribd
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документ1. The document discusses cellular aberrations and the cell cycle. It describes the four phases of the cell cycle - G1, S, G2, and M phase - and notes a fifth phase, G0, as a resting phase.
2. Oncology nursing is described as caring for cancer patients through the wide range of physical, emotional, social, and spiritual crises that arise. Nurses must support patients using standards of practice and the nursing process.
3. Cellular aberrations, or cancers, are characterized by abnormal cell growth and the potential to spread, or metastasize. The term cancer refers to diseases where cells grow and spread unrestrained.
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
100%(3)100% нашли этот документ полезным (3 голоса)
506 просмотров14 страниц4th Lecture (NCM106 CA I) Care of Clients in Cellular Aberrations, ABC, Emergency and Disaster Nursing
Загружено:
Kamx Mohammed1. The document discusses cellular aberrations and the cell cycle. It describes the four phases of the cell cycle - G1, S, G2, and M phase - and notes a fifth phase, G0, as a resting phase.
2. Oncology nursing is described as caring for cancer patients through the wide range of physical, emotional, social, and spiritual crises that arise. Nurses must support patients using standards of practice and the nursing process.
3. Cellular aberrations, or cancers, are characterized by abnormal cell growth and the potential to spread, or metastasize. The term cancer refers to diseases where cells grow and spread unrestrained.
Авторское право:
Attribution Non-Commercial (BY-NC)
Доступные форматы
Скачайте в формате PDF, TXT или читайте онлайн в Scribd
Вы находитесь на странице: 1из 14
jcmendiola_Achievers 2013
Care of Clients in Cellular Aberrations,
Acute Biologic Crisis (ABC), Emergency and Disaster Nursing
(NCM106)
Cellular Aberration I
Cellular Aberration
- Basic structural and functional unit of an organism
Cell Cycle
- Is a coordinated sequence of events resulting in duplication of
DNA and division into 2 daughter cell
4 Phases of the Cell Cycle
1. G1 / Gap Phase
Lasts from hours to days / longer
RNA and Protein synthesis occurs in preparation for DNA replication
2. S Phase / Synthesis Phase
Lasts from 10 20 hours
DNA replication in preparation for division
3. G2 / Gap 2
Ranges from 2 10 hours
DNA synthesis while RNA and Protein synthesis continues
4. M Phase / Mitosis Phase
Lasts from 30 60 minutes
Cell division occurs
After mitosis the daughter cells enter the G1 Phase and begin the reproductive cycle again
5. G0 / Resting Phase
Is activity to reenter the cell cycle in response to various stimuli that signal for cell renewal
CELL CYCLE
Oncology Nursing
- Field of specialty
- Nurse must be equipped to support patient and
family through a wide range of physical, emotional,
social, cultural and spiritual crises
- Provide realistic support to those receiving nursing
care and use standards of practice and nursing
process as basis of care
Cellular Aberration
- A group of disorders characterized by abnormal cell growth and the ability to metastasize with potential in
killing the host
- The term cancer refers to the group of diseases in which cells grow and spread unrestrained throughout
the body
- Derived from the Latin word crab which means Cancer
- Synonymous with neoplasm
LOOKY
HERE
1. Introduction on Cellular
Aberration
2. Multistage Theory of
Oncogenesis
3. Tumor Invasion and Metastasis
4. Primary Prevention and Control
5. Secondary Prevention and Early
Detection
6. Staging
7. Chemotherapy
jcmendiola_Achievers 2013
INCIDENCE and EPIDEMICS
Male Female
Most Common Cause of Death Most Common Cause of Death
Prostate Cancer
(33%)
Lung Cancer
(31%)
Breast Cancer
(32%)
Lung Cancer
(27%)
Lung Cancer
(13%)
Prostate Cancer
(10%)
Lung Cancer
(12%)
Breast Cancer
(15%)
Colorectal Cancer
(10%)
Colorectal Cancer
(10%)
Colorectal Cancer
(11%)
Colorectal Cancer
(10%)
Bladder Cancer
(7%)
Pancreatic Cancer
(5%)
Endometrial Cancer
(6%)
Ovarian Cancer
(6%)
Cutaneous Melanoma
(5%)
Leukemia
(4%)
Non-Hodgkins Lymphoma
(4%)
Pancreatic Cancer
(6%)
TOP 5 Cancer Incidences by Site and Sex
Male Female
1. Prostate 1. Breast
2. Lungs 2. Lungs
3. Colon 3. Colon
4. Urinary Tract 4. Uterus
5. Leukemia 5. Leukemia and Lymphoma
Women Men
- Breast Cancer followed by lung
and colon and rectum
- High incidence of cancer of the lung and bladder
- Most common neoplasm aged 20 34; testicular Cancer
Etiologic Agent
1. Viruses and Bacteria
Oncogenic viruses
Prolonged / frequent viral infections may cause breakdown of the immune system / overwhelm the
immune system
2. Chemical Carcinogens
Act by causing cellular mutation / alterations in cell enzymes and protein
E.g. Industrial compounds vinyl chloride, polycyclic aromatic hydrocarbons, fertilizers, weed
killers, dyes and drugs
3. Physical Agents
Radiation X-ray / radioactive isotopes and sunlight / UV Rays
Physical Irritation/ trauma Pipe smoking, multiple deliveries, ragged tooth, irritation of the
tongue, overuse of any organ / body part
4. Hormonal Agents
Estrogen as replacement therapy incidence of vaginal and cervical adenocarcinoma
Estrogen, diethylstilbestrol (DES)
5. Genetics and Familial Factors
Oncogene When exposed to carcinogens Changes in the cell structure Becomes
malignant
Predisposing Factors
1. Age Older individuals exposed to carcinogens longer develop immune system alterations
2. Sex
Women = Breast, Uterus, Cervix Cancer
Men = Prostate, Lung Cancer
3. Occupation E.g. Chemical factory worker, radiology department personnel
4. Hereditary Greater risk with positive family history
jcmendiola_Achievers 2013
Urban Versus Rural Incidence
- Common among URBAN DWELLERS than RURAL RESIDENCES
(Greater exposure to carcinogens)
- Geographic Distribution
o Cancer in stomach Japan
o Breast Cancer US; due to environmental diet, ethnic customs and types of pollution
5. Psychological Stress
Depression, grieving, anger, aggression, despair or life stresses decreases immune competence
(Affects hypothalamus and pituitary gland)
Immunodeficiency may spurt the growth and proliferation of Cancer cells
6. Precancerous Lesions
o May undergo transfer into cancer lesion and tumor
o E.g. Pigmented moles, burn scars, senile keratosis, leukoplakia, benign polyps, adenoma of the
colon / stomach fibrocystic disease of the breast
7. Obesity
Studies have linked obesity to breast and colorectal Cancer
Factors to Consider
MR JUAN DELA CRUZ
Etiology
- Carcinogens The process of transferring a
normal cell into cancerous cell which
consists of 3 Stages
1) Initiation (Carcinogen)
2) Promotion, repeated exposure to promote agents (Carcinogen)
3) Progression ( Malignancy behavior)
D Drugs
E Educational Attainment
L Living Conditions
A Ask family History
C Culture
R Radiation Therapy
U Ur Activity
Z Zex
M Marital Status
R Race
J Job
U Ur Life Style
A Age
N Nutrition
jcmendiola_Achievers 2013
Multistage Theory of Oncogenesis
1. Cellular Transformation and Pre-agent Theory
+ Conceptualize that normal cells may be transformed into cancer cells due to exposure to etiologic
agents
2. Failure of the Prime Resource Theory
+ Advocates that all individuals possess cancer cells, however the cancer cells are recognized by the
immune system so the cancer cells undergo destruction
+ Failure of the immune response system leads to inability to destroy the cancer cells
TERMS
1. Cell Proliferation
Is the process whereby cells divide and bear offspring, it normally is regulated so that the number
of cells that are actively dividing is equal to the number of dying / being shed
2. Differentiation
Is the process whereby proliferative cells are transformed into different and more specialized cell
types, as they proliferate it determines what a cells looks like, and how it functions, how long it
will live
3. Apoptosis
It is the process of programmed death of unwanted cells
BENIGN GROWTH PATTERN
1. Hypertrophy
In cell size resulting in an in organ size!
2. Hyperplasia
A reversible in the number of cells in an organ or tissue in response to a specific growth stimulus
3. Metaplasia
Conversion of one cell type to another cell type not usually found in the involved tissue
4. Dysplasia
Characterized by abnormal changes in the size, shape, or organization of cells
Reversible when stimulus is removed
jcmendiola_Achievers 2013
5. Anaplasia
Disorganized irregular cells that have no structure and have loss of differentiation, the result is
almost malignant
CLASSIFICATIONS OF TUMORS
1. Benign
+ Are tumors designated by attaching the suffix oma to the cells of organ
+ E.g. Fibroma, Chondroma,, Osteoma
2. Malignant
+ Tumors that are capable of spreading by invasion and metastasis
+ E.g. Fibrosarcoma, Chondrosarcoma
CATEGORIES OF MALIGNANT NEOPLASMS
1. Carcinogens Growth from epithelial cells, usually solid tumors
2. Sarcoma Arise from muscle, bone, fat and connective tissue, may be solid
3. Lymphoma Arise from lymphoid tissues
4. Leukemia and Myeloma Grows from blood forming organs
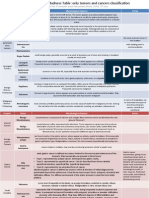
Nomenclature of Tumors
Tissue of Organ Benign Malignant
Connective tissue and derivatives Fibroma
Lipoma
Chondroma
Osteoma
Fibrosarcoma
Liposarcoma
Chondrosarcoma
Osteogenic Sarcoma
Blood Vessels Hemangioma Angiosarcoma
Lymphatic Vessels Lympangioma Lymphangiosarcoma
Brain Meningioma Invasive Meningioma
Hematopoietic Cells Leukemia
Lymphatics Malignant lymph***
Smooth Muscles Leiomyoma Leiomyosarcoma
Stratified Muscles Rhabdomyoma Rhabdomyomasarcoma
Epithelial Tumors
Stratified Squamous Squamous cell papilloma Squamous cell carcinoma
Basal Cells Basal Cells carcinoma
Liver Cells Liver cell adenoma Hepatocellular Carcinoma
Placental epithelium
(Trophoblast)
Hydatidiform Mole
Tumor Invasion and Metastasis
Invasion
Occurs when cancer cells infiltrate adjacent tissues surrounding the neoplasm
Metastasis
Occurs when malignant cells travel through the blood / lymph and invade other tissues and organs
to form a secondary tumor
Types of Metastasis
Extension and Invasion
1. Lymphatic Spread
2. Seeding of body cavities and surfaces
3. Hematogenous spread
Spread of cancer cells from a primary tumor to distant sites
Break away
Only malignant cells has the capability
Lymph, blood, serosal seeding
jcmendiola_Achievers 2013
Comparison of the Characteristics of Benign and Malignant Neoplasms
Characteristics Benign Malignant
Speed of Growth Slow growth
Grows by expansion
Aggressive growth; rapid cell
division and growth
Mode of Growth Localizes and encapsulation Establishes new site malignant
lesion
Cellular Characteristics Well-differentiated Invade surrounding tissues
Metastasis It does not metastasize
No tissue damage
With poor cellular differentation
Prognosis Very good prognosis
Does not cause death, unless
localization affects vital functions
Malignant Cells Mitosis
o Mitosis Multiple daughter cells that may / may not resemble the parent, multiply mitotic spindles
1. Larger, grows more rapidly than normal cells
2. Cells not as cohesive, irregular pattern of expansion
3. Larger, more prominent nucleus
4. Lack characteristic pattern of organization of host cells
5. Anaplastic = Lack of differentiated cell characteristics specific function
Malignant Cells Growth
1. Invade adjacent tissues
2. Proliferation in response to abnormal stimulus
3. Grow in adverse condition such as lack of nutrients
4. Do not exhibit contact-inhibition
5. Cell birth exceeds cell death
6. Loss of cell control as a result of cell membrane changes
7. Growth rate, erratic
8. Able to break off cells that migrate through blood stream / lympati** seed to distant sites and grow in other
sites
Malignant Cells Function
1. Senseless, no useful purpose
2. Do not contribute to the well-being of the host, parasitic
3. If the cells function at all, they do not function normally may cause damage
Malignant Cells
1. Develop antigens completely different from a normal cell
2. Chromosomal aberrations occur as a cell matures
3. Has a more prominent and simplified metabolic enzyme pattern
4. Invasive and spreads
5. Grow in presence of necrosis and inflammatory cells such as lymphocytes and macrophages
6. Exhibit periods of latency that vary from tumor to tumor
7. Have own blood supply and suppository stoma (Angiogenesis factory 2 cm in diameter)
jcmendiola_Achievers 2013
Primary Prevention and Control
WARNING SIGNS OF CANCER (CAUUUTIONALF)
C Change in bowel / bladder habits
A A sore that does not heal
U Unusual bleeding / discharge
U Unexplained sudden weight loss
U Unexplained anemia
T Thickening / lump in the breast or elsewhere
I Indigestion or difficulty in swallowing
O Obvious change in wart / mole
B Nagging cough / hoarseness
A Anemia
L Loss of weight
F Fever of unknown origin
Screening
1. Familial and environmental history
2. Physical Examination
3. Evaluation of laboratory findings and test findings
4. Screening methods
Brest
Monthly BSE = all women ages 20 and above 1 week after menses
Mammography every year from age 40 years old
Colon and Rectum
Fecal occult blood test every year beginning at age 50
Proctosigmoidoscopy every 3- 5 years after 50 years old following 2 negative annual
exams
Uterus
Yearly pelvic examination and PAP Smear test for sexually active girls and any woman
over 18 or less often for 3 consecutive negative results
An endometrial sample at menopause for high risk women
Prostate
Digital Rectal Exam (DRE) yearly beginning at age 50
Prostate-Specific Antigen (PSA) test yearly beginning at age 50
Secondary Prevention and Early Detection
NON INVASIVE DIAGNOSTIC PROCEDURES
^ Diagnostic Imaging Methods
Important in the diagnosis and staging of cancer
Used to guide the surgeon to the appropriate area for biopsy
Use of this modality is guided by physical examination
Clinical instruction through collaboration with the radiology specialist
^ X-RAY
Sites speaks
View the dynamic function of an organ
^ Mammography
Used to screen for malignancies of the breast
Should be conducted with clinical findings
^ CT Scan
Obtain images from various angles through the body such as lungs, soft tissue, blood vessels
Preferred method for diagnosis, liver, kidney and pancreatic cancer
10 Steps for Cancer
Prevention and Protective
Factors
1. Increase consumption of fresh
vegetables
2. Increase fiber intake
3. Increase Vitamin A
4. Increase Vitamin C
5. Practice weight control
6. Decrease dietary fat and
7. Decrease salt
8. Stop cigarette smoking
9. Decrease alcohol intake /
substance abuse
10. Void overexposure to sun
jcmendiola_Achievers 2013
^ MRI
Preferred imaging technique for soft tissue structures, hematologic imaging, vascular imaging and
avascular necrosis
Not exposed to radiation
INVASIVE DIAGNOSTIC PROCEDURE
* Histologic / Cytologic Examination
o For malignant tissues to be identified by name, grade and stage
o Morphologic feature of the cells are examined
3 Basic Methods of Specimen Collection
1. Exfoliation from an epithelial surface (pap smear) or bronchial washing
2. Aspiration of fluid from body cavities or blood
3. Needle suction aspiration of solid tumor
* Direct Visualization
1. Sigmoidoscopy (Viewing the sigmoid colon by use of fiberoptic flexible sigmoidoscopes
2. Cystoscopy (Viewing the urethra and bladder)
3. Endoscopy (Viewing of the upper GIT)
4. Bronchoscopy (Inspection of the tracheobronchial tree
LABORATORY STUDIES
Tumor Markers
Biochemical substances synthesized and released by tumor cells
May be protein products exerted by cancer cells, released in response to the presence of cancer
cells or other conditions
Used to aid in the diagnosis of cancer to determine recurrence or identify regression of a known malignancy
TUMOR MARKER DESCRIPTION
1. Oncofetal Antigen Present in fetal tissue normally suppressed after birth
2. Hormones Present in considerable amount
High levels in hormone-secreting malignancies
3. Isoenzymes Elevated levels can promote hyperplasia of the tissue (Prostate acid
phosphatase)
4. Tissue-Specific Protein Narrows down the type of malignancy that can be increased in
hyperplastic disorders
5. Prostate-Specific Antigen Useful in evaluating response to treatment, recurrent surgery / radiation
therapy
Elevated in prostate cancer, can be elevated in BPH in older men, should
be accompanied with DRE
6. S-100 Found in melanoma cells
Elevated means METASTATIC MELANOMA
7. Thyroglobulin Protein made by the thyroid gland
Removal of the entire gland with or without radiation therapy
Rise in thyroglobulin levels indicate cancer recurrence
8. Estrogen and Progesterone
Receptors
Once diagnosed, breast cancer tissue become tested for the presence of
E and P receptors
Provides an indication of the aggressiveness of the cancer and how
likely the cancer will respond to specific types of endocrine therapy
9. Ca 15 3 and Ca 27 29 Specific for BREAST CANCER
Found in the blood of an affected patient
Ca 27 29 test is MORE sensitive than Ca 15 3
10. Carcinoembryonic Antigen
(CEA)
and Ca 19 9
Elevated in ADVANCED COLORECTAL CANCER
CEA level before surgery POORER PROGNOSIS
11. Human Chorionic
Gonadotropin (HCG) and
Alpha-fetoprotein (AFP)
With germ cell ovarian tumors in men with non-seminomatous
TESTICULAR CANCER = Elevated HCG and AFP
Proportionately to the size of tumors
AFP levels may also be increased in CHRONIC HEPATITIS
jcmendiola_Achievers 2013
12. Beta-2-Microglobulin (B2M) Elevated in periods with multiple myeloma with chronic lymphocytic
leukemia, kidney disease
13. HER-2 / NEU Elevated in one-thirds of persons diagnosed with breast cancer
Laboratory Tests
- Complete Blood Count (CBC)
- Blood Chemistry
) Serum electrolytes
) ALT Alanine Aminotransferase
) AST Aspartate Aminotransferase
) LDH For liver metastases
) CEA For colon cancer
STAGING
Done during the pre-treatment phase
After surgical resection
Recurrence after disease free interval
STAGING TUMOR
Tumor TNM Staging System
T0 No end of primary tumor
Tis Carcinoma in situ
T1, T2, T3, T4 Progressive increase in tumor size and involvement
Tx Tumor cannot be assessed
STAGES
Stage I The tumor is small, local, detected early
Stage II The tumor is somewhat larger and has started to spread to nearby lymph nodes
Stage III The tumor has spread to nearby lymph nodes
Stage IV Cancer has spread to other parts of the body and is generally in an advanced stage
STAGING NODE
N0 Regional lymph nodes
N1, N2, N3 degree of demonstrable abnormality of regional lymph nodes
Nx Regional lymph nodes cannot be assessed clinically
STAGING METASTASIS
M0 No evidence of distant metastasis
M1, M2, M3 Ascending degree of distant metastasis, including metastasis to different lymph nodes
GRADING
Gx Grade cannot be assessed
G1 Well differentiated
G2 Moderately well-differentiated
G3 and G4 Poorly to very poorly differentiated
Poorer differentiation poorer prognosis
Classification, Grading and Stages
TNM Classification
T Extent of primary tumor
Tx Cannot be adequately assessed
T0 No evidence of primary tumor
Tis Tumor in situ 0 localized; no spread
T1 4 prognosis, increase in size
1.5 cm < 2: 6-9 cm
3:10-15 cm 4:15 cm >
jcmendiola_Achievers 2013
STAGES
0 Benign state
I Spread to nearby tissue
II 2 5 cm sometimes involve lymph
III Greater than 5 cm spread advanced spread to connective tissue
IV Metastasis
Grading of Tumor
Grade I Well differentiated
Grade II Moderately well differentiated
Grade III Poorly differentiated
Grade IV Undifferentiated
CHEMOTHERAPY
E A systematic mode of treatment that uses cytotoxins and chemicals to effectively CURE (Leukemia,
Lymphomas, some solid tumors)
Tumor size
Adjunct to surgery / radiation
Prevent / treat suspected metastasis
E Most effective when the tumor is small and cell replication is rapid
E Individualized to the patient and is often prescribed according to the patients calculated body surface area
and type of cancer
E Example:
Acute Lymphocytic Leukemia (ALL)
Uses DVPA
Daunorubicin Given days 1 3
Vincristine Given days 1, 8, 15 and 22
Prednisone Given days 11 28
Asparaginase Given days 17 28
Given in cycles with rest periods (especially if with toxic effects) until disease goes to remission
Chemotherapy Cell Cycle
- Used to disrupt the cell cycle in various phases in specific protocols that are given over varying periods of
time
Cell Kill Hypothesis
1. Several doses of chemotherapy are necessary
2. Each exposure kills: 20% - 99% depending on dosage
3. Repeated exposure targets even those in G0 and leads to regression
4. 100% eradication of tumor cells IMPOSSIBLE
5. But the goal is: To reduce the amount that can be destroyed by the immune system
Factors Crucial to the Rate of Normal / Malignant Tissues
1. Cell Cycle Timing: Amount of time required for cells to remove from one mitosis to the next
2. Growth Fraction: Ratio of dividing cells to resting cells, fraction of cycling cells in the entire cell
population
3. Rate of Cell Loss: Fracture of cell die or leaves
Route of Chemotherapy
1. Oral Hodgkins Lymphoma, Leukemia (Maintenance phase), Lung Cancer
2. Intravenous Leukemia,
3. Intra-arterial Hepatic tumors, head and neck cancer
4. Intracavity Ovarian cancer
New RESEARCH!
Use of chemotherapy based on
CIRCARDIAN RHYTHMS
E.g. Colon Cancer
jcmendiola_Achievers 2013
5. Intraperitoneal Brain tumors
6. Intraventricular Brain tumor
7. Intravesical Bladder tumors
OBJECTIVES:
- To destroy all malignant tumor cells without excessive destruction of normal cells
- To control growth if cure is no longer possible
- Used as adjunct therapy
CONTRAINDICATIONS
* Infection: Anti-tumor drugs are immunosuppressive
* Recent surgery: Drugs may retard healing process
* Impaired renal / Hepatic Function: Drugs are nephrotoxic and hepatotoxic
* Recent Radiation Therapy: Immunosuppressive
* Pregnancy: Drugs may cause congenital defects
* Bone Marrow Depression: Drugs may aggravate the condition, WBC must be within normal levels
Safe Handling of Chemotherapeutic Agents
- Wear mask, gloves and back-closing gown
- Skin contact with drugs must be washed immediately with soap and water. Eye must be flushed
immediately with copious amount of water
- Sterile / Alcohol Wet cotton pledgets should be used, wrapped around the neck of the ampule / vial
when breaking and withdrawing the drug
- Expel air bubbles or wet cotton
- Vent vials to reduce internal pressure after mixing
- Wipe external surface of syringe and IV bottles
- Avoid self-inoculation by needle stab
- Clearly label the hanging IV bottle with antineoplastic chemotherapy
- Contaminated needles and syringes must be disposed in a clearly marked special container leak-proof or
puncture proof
- Dispose half-empty ampules, vials, IV bottles by putting them into plastic bags sealed and then into
another plastic bag or box, clearly marked before placing for removal. Label as Hazardous Wastes
- Handwashing should be done before and after removal of gloves
- Trained personnel only should be involved in use of drugs
Effects of Chemotherapeutic Drugs
Tissues normally affected are:
1. Mucous Membranes
Mouth, tongue, esophagus, stomach, intestine and rectum
Results in anorexia, loss of taste, aversion to food, Erythema,
painful ulceration of GIT, NV, diarrhea
2. Hair Cells
Alopecia
3. Bone Marrow Depression
Affects: Granulocytes, lymphocytes, thrombocytes, erythrocytes
Impaired ability to respond to infection, blood clot and severe
anemia
4. Organ
Heart, lungs, bladder, kidney
Due to specific agents
E.g. Cardiac toxicity (Doxorubicin)
Pneumocystis (Bleomycin)
Effects of CHEMO DRUGS
1. Combined medication
therapy is used to
enhance tumor cell
kill
2. Synergistic actions of
drugs will prevent the
development of drug
resistance
3. Combats resistance of
cells to
chemotherapeutic
agents
jcmendiola_Achievers 2013
Classification of Chemotherapeutic Drugs
Related to the cell cycle
1. Cycle Specific Agents
They are specific to certain phases of the cell cycle
Destroy cells that are actively reproducing
Most affects there in the S Phase of interfering with DNA and RNA synthesis
M Phase (Vinca / Plant Alkaloids: Halt spindle function)
2. Cycle Non-Specific Agents
Act independently of the cell cycle place
Usually have prolonged effects or cells leading to cell death and damage
Classifications of Drugs
1. Alkylating Agents
Contains alkyl groups which binds to DNA and prevents replication and mitosis
Cell Cycle non-Specific
Effective against many types of cancer, including acute and chronic leukemia, solid tumors
Common Side Effects
- Bone marrow suppression
- N/V
- Alopecia
- Sterility
- Cystic cyclophosphamide
- Stomatitis
- Renal Toxicity (Cisplastin)
E.g.
Bisulfiram (Bisulflex)
Cyclophosphamide (Cytoxan)
Chlorambucil (Leukeran)
Cisplastin (Planitol-AQ)
Nursing Implications:
Maintain good hydration
Administer anti-emetics prior to chemotherapy
Monitor WBC, Uric Acid
Assess for possible infection
Discuss concerns for hair loss
2. Nitrosoureas
Similar to the alkylating agent
ONLY CHEMODRUG THAT CAN CROSS THE BLOOD BRAIN BARRIER (BBB)
[Important for Central Nervous System diseases]
Side Effects:
Delayed cumulative myelosuppression (In 3 5 weeks) especially thrombocytopenia;
N/V
Nursing Implications:
Maintain good hydration
Administer anti-emetics prior to chemotherapy
Monitor WBC, Uric Acid
Assess for possible infection
Discuss concerns for hair loss
3. Anti Metabolites
Interferes with the biosynthesis of metabolism or nucleic acid needed for RNA and DNA synthesis
Cell specific (Best in S Phase)
Used to treat acute leukemia, breast cancer, head and neck cancer, lung cancer, and osteosarcoma
Side Effects:
Bone Marrow suppression (Anemia, leukopenia)
jcmendiola_Achievers 2013
Stomatitis
N/V
Alopecia
Hepatitis and renal dysfunction
E.g.
Methotrexate
- Lethal in high doses, must give antidote (Leucovorin) within 24 36 hours after
initiation of therapy
- 5-Flurouracil (5-FU)
- Cytarabine (Depocyt, Tarabine)
- 5-Azacytidine
Side Effects
N/V
Diarrhea
Bone Marrow suppression: Reaches NADIR in 1 2
weeks; with leukopenia being most severe
Renal toxicity (Methotrexate)
Hepatotoxicity
Nursing Implications
Monitor CBC, WBC, Uric acid
Assess oral mucus membranes
Assess for infection, bleeding
Provide oral care
Administer anti-emetics PRN
Discuss concern for hair loss
Evaluate hydration and nutritional status
4. Antitumor Antibiotics
Inhibit RNA synthesis and bind DNA causing fragmentation; interfere with DNA repair
These drugs bind to almost everything they contact and kill cells
Main toxic effect is cardiac muscle toxicity (Limits the amount and duration of treatment)
Side Effects are the same with other anti-Cancer drugs
E.g.
Doxorubicin (Adriamycin)
Bleomycin (Blenoxane)
Dactinomycin (Cosmegen)
Nursing Implications
Monitor ECG, CBC
Assess for bleeding
Assess for hydration and nutritional status
Check for fever 36 hours after administration
Administer anti-emetic PRN
5. Plant Alkaloids
Two main Groups (From natural products)
1. Vinca Alkaloids Mitosis phase, inhibit mitotic tubular formation (spindle); inhibit DNA
and protein synthesis
2. Etoposide (VP-16) or Mitotic Inhibitors All phases; causes breaks in DNA and
metaphase arrest
E.g.
1. Vincristine (Oncovin)
Vinblastin (Velban)
2. Etoposide (Toposar)
Teniposide (Venom)
Side Effect:
Hypotension (Too rapid IV administration), muscle weakness, areflexia, constipation,
N/V, alopecia
Nursing Implications:
NADIR Is the lowest level of
a red blood cell count while a
patient is undergoing
chemotherapy
jcmendiola_Achievers 2013
Assess neuromuscular functions
Monitor CBC, GI function
Manage constipation
Hydration
Discuss concerns for hair loss
6. Hormonal Agents
Alter the deviate / environment to depress / prevent cell proliferation
Corticosteroids (e.g. Prednisone: Mostly used in CA therapy; G1 Phase)
E.g.
Androgen, estrogen, anti-androgens, anti-estrogens
Side Effects
N/V
Hyperglycemia
Hypertension
Weight gain; gynecomastia
Mood changes
Cessation of menstruation
Acne, alopecia
Nursing Interventions for Chemical Side Effects
GI System = N/V, diarrhea, constipation
Administer anti-emetics to relieve N/V
Replace fluids and electrolyte losses, low fiber diet to relieve diarrhea
fluid intake and fibers in diet to prevent / relieve constipation
Integumentary System
Pruritus; urticaria and systemic signs
- Provide good skin care
Stomatitis
- Provide good oral care, avoid HOT and SPICY food
Alopecia
- Reassure that it is temporary, wear wigs / hats
Skin Pigmentation
- Inform that it is temporary
Nail changes (Grow normally after chemotherapy)
Hematopoietic System
Anemia
- Frequent rest periods, eat foods high in Iron!
Neutropenia
- Protect from infection
- Avoid people with infection
Thrombocytopenia
- Protect from trauma
- Avoid ASA
Genito-Urinary System
Hemorrhagic Cystitis
- Provide 2 3 L of fluids per day
Urine color changes
- Reassure that it is harmless
Вам также может понравиться
- Oncology NursingДокумент7 страницOncology NursingDiana Laura Lei100% (1)
- Medical-Surgical Nursing 2 Prepared by Dr. Peña and Dr. CabigonДокумент9 страницMedical-Surgical Nursing 2 Prepared by Dr. Peña and Dr. CabigonZOОценок пока нет
- B. Pathophysiology: Clinical Aspects of Cancer DiagnosisДокумент10 страницB. Pathophysiology: Clinical Aspects of Cancer DiagnosisAbigael Patricia GutierrezОценок пока нет
- Prepared By: Anna Marie M. Montalban, RN, Us-RnДокумент71 страницаPrepared By: Anna Marie M. Montalban, RN, Us-RnPrecai Permangil100% (2)
- Management of Tuberculosis: A guide for clinicians (eBook edition)От EverandManagement of Tuberculosis: A guide for clinicians (eBook edition)Оценок пока нет
- Oncology Handouts PDFДокумент21 страницаOncology Handouts PDFPhilip Simangan100% (1)
- Introduction To Oncology NursingДокумент35 страницIntroduction To Oncology NursingDesh Deepak100% (1)
- Breast Cancer Case Study: Answers For LifeДокумент4 страницыBreast Cancer Case Study: Answers For LifeFaye Mie VelascoОценок пока нет
- MEDSURG MERGED (Cellular Abber + Cancer Manage)Документ34 страницыMEDSURG MERGED (Cellular Abber + Cancer Manage)Leslie CruzОценок пока нет
- Case Study Cervical Cancer InterviewДокумент4 страницыCase Study Cervical Cancer InterviewLYNDON MENDIOLAОценок пока нет
- Lecture Handouts Oncology NursingДокумент12 страницLecture Handouts Oncology NursingTiffany Luv AdriasОценок пока нет
- NCM 106 Cellular-AberrationДокумент6 страницNCM 106 Cellular-AberrationJoanne TolopiaОценок пока нет
- MEDSURG - Cellular AberrationДокумент10 страницMEDSURG - Cellular AberrationLeslie CruzОценок пока нет
- NCM 104 Cellular Aberration Lecture 2007Документ104 страницыNCM 104 Cellular Aberration Lecture 2007api-378278992% (26)
- NCM 106 Cellular AberrasionДокумент11 страницNCM 106 Cellular AberrasionArika Vista-Mamigo100% (3)
- My Courses: Dashboard RMC Cap 2 Prelim Medical Surgical Nursing 4 Post Test 1Документ10 страницMy Courses: Dashboard RMC Cap 2 Prelim Medical Surgical Nursing 4 Post Test 1Fraylle AbongОценок пока нет
- Oncologic NursingДокумент132 страницыOncologic Nursingɹǝʍdןnos100% (10)
- Maternal and Child Health Nursing Key TermsДокумент3 страницыMaternal and Child Health Nursing Key TermsQuennie UmaliОценок пока нет
- Introduction To TransplantationДокумент3 страницыIntroduction To TransplantationGerardLumОценок пока нет
- Oncology Nursing Handouts 1Документ8 страницOncology Nursing Handouts 1pauchanmnlОценок пока нет
- Oncology Nursing Part 1 2Документ51 страницаOncology Nursing Part 1 2fleur harrisonОценок пока нет
- Sample Exam On Community Health Nursing (Communicable Diseases)Документ3 страницыSample Exam On Community Health Nursing (Communicable Diseases)John Eldrin LaureanoОценок пока нет
- Cellular AberrationsДокумент10 страницCellular AberrationsWilbert Antonino CabanbanОценок пока нет
- Lung CancerДокумент7 страницLung CancerClarinda RondainОценок пока нет
- Group 8: Parik Rabasto Patel, D Patel, J Raghuwanshi Regis Moleta Moreno NaromalДокумент35 страницGroup 8: Parik Rabasto Patel, D Patel, J Raghuwanshi Regis Moleta Moreno NaromalDominique RabastoОценок пока нет
- Maternal and Child Health Questions W/ RationaleДокумент15 страницMaternal and Child Health Questions W/ RationaleMaicah ShaneОценок пока нет
- Oncology NursingДокумент10 страницOncology NursingCham Rafaela Conese100% (3)
- Syllabus NCM 104Документ10 страницSyllabus NCM 104ivanguzman860% (1)
- Nursing OncologyДокумент208 страницNursing OncologyfelxhuОценок пока нет
- CancerДокумент14 страницCancerClara De Guzman83% (6)
- Cellular AberrationДокумент71 страницаCellular AberrationKris TejereroОценок пока нет
- Cervical Pathology 4Документ104 страницыCervical Pathology 4Arie PratamaОценок пока нет
- MCN PartographДокумент2 страницыMCN PartographAlec Anon100% (1)
- CANCER NSG QuestionsДокумент43 страницыCANCER NSG QuestionsAnn Michelle Tarrobago83% (6)
- Colorectal CancerДокумент3 страницыColorectal CancerAriane May Rubio50% (2)
- Renal Cell CarcinomaДокумент15 страницRenal Cell Carcinomadger11Оценок пока нет
- Hodgkin'sДокумент35 страницHodgkin'sDorothy Pearl Loyola PalabricaОценок пока нет
- COPARДокумент3 страницыCOPARCecilia TesoreroОценок пока нет
- Lung CancerДокумент22 страницыLung CancermandrakesMD100% (1)
- Ob NotesДокумент16 страницOb Noteslily machan100% (3)
- CD HandoutДокумент20 страницCD HandoutiandameОценок пока нет
- A Case Study On Renal CancerДокумент30 страницA Case Study On Renal CancerAiyish CapunoОценок пока нет
- Hematologic SystemДокумент81 страницаHematologic Systemseigelystic100% (23)
- Cancer Pathophysiology Nursing NotesДокумент8 страницCancer Pathophysiology Nursing Notesgrad_nurse_2015100% (2)
- Pancreatitis: Pancreatitis Is Inflammation in The Pancreas. TheДокумент27 страницPancreatitis: Pancreatitis Is Inflammation in The Pancreas. ThenikkimaxinevaldezОценок пока нет
- NCLEX Review Oncology NursingДокумент8 страницNCLEX Review Oncology NursingJunjun R AquinoОценок пока нет
- Oncology Reviewer 60ptsДокумент10 страницOncology Reviewer 60ptsShirin Forbes AquinoОценок пока нет
- Oral RevalidaДокумент98 страницOral RevalidaJay ArОценок пока нет
- Case Presentation (Oncology)Документ26 страницCase Presentation (Oncology)Froilan FerrerОценок пока нет
- Oncology-Study of Cancer Cellular AbberationДокумент43 страницыOncology-Study of Cancer Cellular AbberationIrwan M. IskoberОценок пока нет
- 2013-Oncology New QuestionsДокумент5 страниц2013-Oncology New QuestionsHarley Justiniani Dela CruzОценок пока нет
- CancerДокумент83 страницыCancersankar100% (1)
- Cellular AberrationДокумент71 страницаCellular AberrationMichael CoronadoОценок пока нет
- AU CA2 Course OutlineДокумент4 страницыAU CA2 Course OutlineYaj Cruzada100% (1)
- Oncology Nursing HandoutsДокумент7 страницOncology Nursing HandoutsShandz de Rosas100% (1)
- Care of The Clients With CancerДокумент78 страницCare of The Clients With Cancercasandra moranteОценок пока нет
- Oncology NursingДокумент12 страницOncology NursingDick Morgan Ferrer80% (5)
- Ncm103 30th Gi IVДокумент6 страницNcm103 30th Gi IVKamx MohammedОценок пока нет
- NCM103 24th F&E IVДокумент5 страницNCM103 24th F&E IVKamx MohammedОценок пока нет
- Ncm103 29th Gi IIIДокумент11 страницNcm103 29th Gi IIIKamx MohammedОценок пока нет
- Ncm103 28th Gi IIДокумент12 страницNcm103 28th Gi IIKamx MohammedОценок пока нет
- NCM103 25th F&E VДокумент6 страницNCM103 25th F&E VKamx MohammedОценок пока нет
- NCM103 23rd F&E IIIДокумент6 страницNCM103 23rd F&E IIIKamx MohammedОценок пока нет
- Ncm103 27th Gi IДокумент10 страницNcm103 27th Gi IKamx MohammedОценок пока нет
- NCM103 26th Acce IДокумент31 страницаNCM103 26th Acce IKamx MohammedОценок пока нет
- NCM103 19th Respi VДокумент5 страницNCM103 19th Respi VKamx MohammedОценок пока нет
- NCM103 20th Respi VIДокумент6 страницNCM103 20th Respi VIKamx MohammedОценок пока нет
- NCM103 21st F&E IДокумент7 страницNCM103 21st F&E IKamx MohammedОценок пока нет
- NCM103 22nd F&E IIДокумент5 страницNCM103 22nd F&E IIKamx MohammedОценок пока нет
- Ncm103 17th Respi IIIДокумент3 страницыNcm103 17th Respi IIIKamx MohammedОценок пока нет
- NCM103 18th Respi IVДокумент6 страницNCM103 18th Respi IVKamx MohammedОценок пока нет
- NCM103 12th Endoc IIДокумент9 страницNCM103 12th Endoc IIKamx MohammedОценок пока нет
- NCM103 11th Endoc IДокумент8 страницNCM103 11th Endoc IKamx MohammedОценок пока нет
- NCM103 14th Endoc IVДокумент9 страницNCM103 14th Endoc IVKamx MohammedОценок пока нет
- NCM103 16th Respi IIДокумент5 страницNCM103 16th Respi IIKamx MohammedОценок пока нет
- NCM103 15th Respi IДокумент10 страницNCM103 15th Respi IKamx MohammedОценок пока нет
- Ncm103 13th Endoc IIIДокумент5 страницNcm103 13th Endoc IIIKamx MohammedОценок пока нет
- Right Sided Heart FailureДокумент5 страницRight Sided Heart FailureKamx MohammedОценок пока нет
- Ncm103 10th Hema IIДокумент8 страницNcm103 10th Hema IIKamx MohammedОценок пока нет
- NCM103 9th Hema IДокумент10 страницNCM103 9th Hema IKamx MohammedОценок пока нет
- Coronary Atherosclerosis: Cardiovascular System: Coronary Vascular Disease Topics Discussed Here AreДокумент6 страницCoronary Atherosclerosis: Cardiovascular System: Coronary Vascular Disease Topics Discussed Here AreKamx MohammedОценок пока нет
- NCM103 2nd Periop IДокумент3 страницыNCM103 2nd Periop IKamx MohammedОценок пока нет
- Ncm103 8th CV IVДокумент5 страницNcm103 8th CV IVKamx Mohammed0% (1)
- NCM103 3rd & 4th Periop II and IIIДокумент5 страницNCM103 3rd & 4th Periop II and IIIKamx MohammedОценок пока нет
- NCM103 5th CV IДокумент7 страницNCM103 5th CV IKamx MohammedОценок пока нет
- NCM103 1st PainДокумент5 страницNCM103 1st PainKamx MohammedОценок пока нет
- NCM103 2nd Periop IДокумент3 страницыNCM103 2nd Periop IKamx MohammedОценок пока нет
- 12 L.straussДокумент5 страниц12 L.straussColectivo RizomaОценок пока нет
- Muscle Atrophy Is The Wasting (Thinning) or Loss of Muscle TissueДокумент2 страницыMuscle Atrophy Is The Wasting (Thinning) or Loss of Muscle TissueJustine Simeon lagunzadОценок пока нет
- Bosniak ClassificationДокумент19 страницBosniak ClassificationGirish Kumar100% (1)
- Pathology Item CardДокумент2 страницыPathology Item CardBir Mohammad SonetОценок пока нет
- What Is Cancer - National Cancer Institute PDFДокумент7 страницWhat Is Cancer - National Cancer Institute PDFAlexis CastilloОценок пока нет
- Tumori Testisa PDFДокумент14 страницTumori Testisa PDFVuk MilutinovićОценок пока нет
- CH 001Документ6 страницCH 001Maaz KhajaОценок пока нет
- CT Applications in Chest PathologyДокумент16 страницCT Applications in Chest PathologyNilanka SandunОценок пока нет
- UI-RADS (Uterus Imaging Reporting and Data System) : April 2019Документ3 страницыUI-RADS (Uterus Imaging Reporting and Data System) : April 2019Jenniffer FlorenciaОценок пока нет
- Cytologic Patterns - Eclinpath PDFДокумент5 страницCytologic Patterns - Eclinpath PDFJD46Оценок пока нет
- Hemangioma - Google SearchДокумент1 страницаHemangioma - Google SearchhapidarrenОценок пока нет
- Septic Arthritis: Briones, Hershey C. BSN - IiiДокумент8 страницSeptic Arthritis: Briones, Hershey C. BSN - IiiHershey Cordero BrionesОценок пока нет
- Benign Mimics of Malignancy On Breast ImagingДокумент35 страницBenign Mimics of Malignancy On Breast Imagingskype72214Оценок пока нет
- 02.22.1 Neoplasia I Final PDFДокумент79 страниц02.22.1 Neoplasia I Final PDFSameeha AbbasОценок пока нет
- Brosur Cusa Clarity KomplitДокумент11 страницBrosur Cusa Clarity KomplitrossiОценок пока нет
- CANCER NSG QuestionsДокумент43 страницыCANCER NSG QuestionsAnn Michelle Tarrobago83% (6)
- Review For The 2° Semester Exam Alessandro Mo6a, UVVG, 3 YearДокумент9 страницReview For The 2° Semester Exam Alessandro Mo6a, UVVG, 3 Yeardjxela89Оценок пока нет
- Tumori Tesuturi MoiДокумент123 страницыTumori Tesuturi MoiOana BarbuОценок пока нет
- 9 Mesenchymal Tumors 2Документ77 страниц9 Mesenchymal Tumors 2Ther Ray100% (1)
- Unusual Large and Abiding Fibroepithelial Polyp in Oral Cavity: A Case ReportДокумент4 страницыUnusual Large and Abiding Fibroepithelial Polyp in Oral Cavity: A Case ReportmuharrimahОценок пока нет
- GENITOGRAPHY (English Version)Документ8 страницGENITOGRAPHY (English Version)Ryesti RahmadheniОценок пока нет
- Kista Ovarii: R6/September 2020Документ100 страницKista Ovarii: R6/September 2020vita_nthОценок пока нет
- Brain Tumor Segmentation and Detection Using Nueral NetworksДокумент9 страницBrain Tumor Segmentation and Detection Using Nueral Networksjoshi manoharОценок пока нет
- RootДокумент119 страницRootเทพนิมิตร สมภักดีОценок пока нет
- Chapter 4 Tissues Glands and MembranesДокумент84 страницыChapter 4 Tissues Glands and MembranesSofia MorenoОценок пока нет
- Epidemiology, Pathology, Clinical Features, and Diagnosis of Meningioma - UpToDateДокумент22 страницыEpidemiology, Pathology, Clinical Features, and Diagnosis of Meningioma - UpToDatewilson kores100% (1)
- Nursing OncologyДокумент131 страницаNursing Oncologyapi-3818438100% (5)
- 1.06 General Pathology - Neoplasia (Part 1) - Dr. Annette SallilasДокумент17 страниц1.06 General Pathology - Neoplasia (Part 1) - Dr. Annette SallilasCherry RahimaОценок пока нет
- A Case Report of Desmoplastic AmeloblastomaДокумент5 страницA Case Report of Desmoplastic AmeloblastomaAndria FadliОценок пока нет
- Benign Lung TumorДокумент16 страницBenign Lung TumorAbdul Mubdi ArdiansarОценок пока нет