Академический Документы
Профессиональный Документы
Культура Документы
Victoria Hospital Resdesign Initiative
Загружено:
Fatima AjmalИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Victoria Hospital Resdesign Initiative
Загружено:
Fatima AjmalАвторское право:
Доступные форматы
Victoria Hospital Redesign Initiative
Case Study Solution
14th March 2013
GROUP NUMBER FIVE FATIMA AJMAL SYED NAUMAN UL HAQ HAQQI NAYYARA RAHMAN
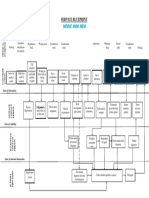
VICTORIA HOSPITAL REDESIGN INITIATIVE Executive Summary and Background: Victoria Hospital was a major hospital in South-Western Ontario. In addition to being a core community health provider, with up to 500,000 patients treated annually from the province and region, it also provided specialized health services, ambulatory care services and was successful in attracting a workforce of highly qualified medical professionals, especially consultants. It pioneered medical research, allocating $7million in research grants per year. Up to 1,100 students benefited from its medical teaching annually, in over 20 disciplines. Collectively, more than 4000 employees provided the bulk of healthcare services that made Victoria Hospital indispensable to the people of South Western Ontario. Together with its Teaching Hospital Arm, extremely healthy doctor: bed ratio (almost 1:1), Victoria Hospital could be seen as an Institutional Pillar of Health Care in Ontario. Unfortunately, this role was not upheld (or valued) universally. Its principal source of fundingthe Provincial Government had been retrenching funding assistance generally, and in particular, sought operational efficiency as a criteria for fund allocation. Though Victoria Hospital had succeeded in balancing its budget for 13 years, this was not enough. Funding continued to decline, its fee structure was unfavorably altered, (thereby losing its benefit as a Teaching Hospital) and its aim to consolidate both wings of the hospital was thwarted. Issues: Ostensibly, Victoria Hospitals issues were fairly obvious: Issue Decreased and declining funding by the government, which was reflective of the overall economic condition of Ontario. Cost restructuring and expansion. This was the product of several internal/external developments: Prior rapid expansion (before 1995-96)Capital outlay carried over Capital expenditure in clinical and technological advancements Delisting of revenue generating health services High internal costs in salaries and wages (70% of the total budget) and this was expected to rise! Teaching benefit replaced by standardized fee. Proposal to consolidate two wings of hospital, at $100 million rejected. If implemented, it would bring savings of $2-4 mill annually. The hospital incurred the highest cost in the province. Business moving to consultants and physicians Government recommendation to move cardiac and neurosurgery to University Teaching Hospital Conventional vertical structure of departmental silos was not working. There was a lack of synergy in teams, a dearth of holistic thinking and needless task duplication and complexity of routine tasks. Lack of consensus between Board of Directors and a lack of cooperation amongst staff regarding strategic realignment. Area/Origin ExternalGovernment Impact Costs
Internal and external
Costs
External Internal External External
Costs and Administration/ Management Costs Revenue and patient (market) base Administration/ Management Administration/ Management Administration/ Management
Internal
Internal
Duplication of acute care teaching services No coordination of city-wide health services.
Internal External
Administration/ Management Administration/ Management
These issues did exist, in fact. But they were symptoms of the real disease, rather than the disease itself. Courses of Alternative Action: The CEO, Dr. Linden Frelick, already reluctant to downsize, was pressed to make some quick changes. He proposed the following three key measures: a) Align organizational structure via inter-disciplinary teams and strategic partnerships for seamless patient care b) Redesign system of production to cut costs, turnaround time and improve service. c) Develop high-revenue generating entrepreneurial strategies Dr Frelick was determined to realize the hospital's vision. He proposed the following steps to achieve his three broad strategic measures : A) Create prototype teams for interdisciplinary function. Based on their success, future teams could be established. B) Establish Financial Task Forces, staffed with middle managers and physicians. Their internal reception and implementation had been lukewarm and half-spirited. The Vice Presidents, who had been made change-leaders were unenthusiastic. They stalled and resisted change. There was also the apprehension that the change management process may take too long. Analysis: Dr Frelick has the right ideas---there is a need to streamline the business, make it flatter, and ensure that those on-board are utilized better. There is a need for intra-preneurial thinking within the hospital. The issue is with the way he is going about it. The problem with prototype teams is that there is still no individual performance measurement system. Hence, there is no way to observe if the silo thinking process has broken or not. It also creates the further problem of free -riding on the team, with physicians delegating tasks to other medical professionals and concentrating on research activities themselves. Two flaws exist with the Financial Task Force Teams too. The first is that they are staffed with middle managers and physicians. i.e. people who are workforce intermediaries. They are not action-driven (like lower level staff); and they lack the authority to take strategic decisions (like upper-level staff). They can make recommendations at best, and as we have seen, the hospital workforce is deeply talented in being able to ignore and override those. The second flaw is that all of whom [Task Force members] were conducting their regular duties in addition to the new challenges of the redesigned initiative. They are not dedicated resources to this initiative. The physicians are already divided between their research and medical practice responsibilities. Now, with a third obligation can we expect to see some real action from them? Dr. Frelick has also concentrated most of the change initiative inward. His attitude towards government funding has been passive and accepting. This is wrong. The hospital already has a very positive record and has given the government no cause for the declining funding. Further, as the case mentions, the
decreased funding was a result of government payments towards elderly care and pensions which typically is the demographic that needs the most healthcare expenditure worldwide. With low federal investment in Ontario, the province needs self-sustaining revenue-generating organizations. And Victoria Hospital is already one of themit is owned by a 130-member corporation. Dr. Frelick needs to promote a more positive image of the hospitaland the aforementioned suggestions make no mention of that. There is a lot of conflict-of-interest at work too. Research is cannibalizing resources that could be spent on treatment. But no alternative action to this has been proposed. Yet there is no evidence that the funding being directed to research contributes to the hospitals direct profitability or not. Perhaps $7 million is too large an amount to direct to research alone, and this could be revised and re-directed to hospital reengineering. There is already a movement towards out-patient and ambulatory-care services in the local health industry. i.e. healthcare is going from brick-and-mortar to click and mortar. So perhaps Dr. Frelick should re-think the need to consolidate both hospital wings, and should either divest of the research wing. Alternatively, the researchers could self-fund the research wing by going on lecture tours, teaching in other areas etc. This would cost less than the current $100 million, and would generate much more than the current saving of $2-4 million per year. A common flaw in the suggestions was that they failed to identify the Act-Actor Gap. The result was that several uninterested stakeholders were brought on board, whereas more interested (and effective) stakeholders were left out. To fulfill full capacity utilization, re-think the role of other medical professionals in the hospital. Big management breakthroughs were coming from nurses, not doctors. Nurses were already active in administration. Patients preferred nurses to physicians, as mentioned in the case. Further, each medical function operated with assistance from 60 service departments. So it was wrong to allocate so much importance and funding to one field in medicine (ie research and consultancy) while downplaying the importance of the rest. In redesigning systems of production, implementing the Patient Care Guidelines And Pathways Effort would bring in the following benefits: Research based recommendations Deliver similar care to patients with similar conditions (cost and resource efficiency and standardization) Made clinicians work together Reduced complexity and duplication Online coordination of clinical information
If implemented, this could break the silo-thinking that prevailed. To make it truly effective, evaluation and management of employees would have to stop being department-specific, and be made team-specific. Currently, physicians were not interested in administration, yet blamed admin for failing inter-disciplinary teams. This would bring in more individual accountability.
Recommendations: The discussion has established that while the hospitals income was declining, the demand for its services was not. People would continue to fall sick, and patients would continue to be under the hospitals care. It was also established that both internal and external inefficiencies were contributing to the escalated costs of the hospital. To counter these, the truest option was not to stop or decrease health service offering, but to redesign it so that it reflected Victoria Hospitals vision of a caring, resource-efficient, progressive and contemporary healthcare organization. This would address its external stakeholders (patients, government, and the competitive scenario). Recommendations must also consider a way of best utilizing and sustaining the hospitals internal stakeholders (physicians, consultants, nurses and other health professionals and the management staff). It was time to evaluate how these internal stakeholders could be best used, and how their contribution could be used to weather the current financial crunch the hospital was undergoing. Recommendation 1 Permit stock options for the Vice Presidents Motive Purpose/Objective Impact Area Required Victoria Hospital is already It will bring in muchCosts and a 130-member company, needed revenue and will Revenue owned and operated by provide a direct incentive Victoria Hospital to the Vice Presidents to Corporation. So the stock contribute more actively to option facility should the hospitals profitability. already exist. No extra-legal It will also make them less legwork required resistant to efficiency measures The local market scenario Full capacity utilization of Management; was towards out-patient consultants Marketing and and ambulatory care Revenue services, which meant that current in-house capacity was idle (i.e. being wasted). To receive fair funding so that the business-processreengineering process can be completed without compromising quality To capitalize on an existing demographic: Government funding was going to pensions, and employee benefit, so this was a very lucrative area A reason Dr Frelicks team and BoD has resisted his suggestions is because he comes across as someone with a soft approach. This abrupt measure would make Cost effective resource allocation Costs; Change Management
Export and aggressively market health/consultancy services to other provinces. The hospital already had a specialty in Womens and Childrens Care, Cardiac, Life support, Cancer Care and Trauma Aggressively promote Victorias services via a marketing campaign, particularly to the public sector. Promote elderly care services, such as physiotherapy and cardiac/orthopedic care
Ability to resist divestment of cardiac unit (as proposed by the government)
Revenue; Marketing
Absorb (or threaten to absorb) staff laid off by other hospitals
Staff laid off by other Cost, Human hospitals would be cheaper Resource to absorb, and it would be easier to replace the current staff
Slash research funding; make it self-sustaining
Move towards preventive care practices (eg gyms, recreation, psychology).
Redesign evaluation criteria for physicians
Move to outpatient services; focus on ambulatory care rather than hospital stay. Patients are increasingly well-informed about treatment alternatives.
10
Increase role of nurses
them sit up If doctors have to pay for their research projects themselves, they will be a lot more interested in medical practice-which will help generate those funds. They will also be interested in choosing projects that have the most immediate relevance to medical practice In the given economic condition, Ontarios leisure industry (clubs, sports centers etc) were likely to have experienced a blow too, so there was a market for a cheaper, healthier avenue of exercise etc. No additional investment needed by Victoria To make them serious about medical practice, evaluation should be functional-team specific, and not department specific This would free resources (bed, ward staff); accede to the patients wish to participate in the treatment plan. It would also diminish the hospitals obligation, since the decision making process closely involve the patient The Regulated Health Professionals Act gives opportunities to 22 medical professional areas
To streamline research; make funding more relevant
Cost, Capacity Utilization; Clinical Innovation
Better resource usage of idle capacity (eg physiotherapy units)
Capacity Utilization; Revenue Generation
Salaries take up 70% of the budget. This is a way of making sure that money is well spent Decreased legal spending; decreased capital expenditure
Cost; Human Resources; Administration
Cost; Marketing
It would be cheaper to appoint/promote nurses in charge of staff management than physicians. It would get better results too
Cost, Capacity Utilization, Human Resources
Вам также может понравиться
- AHA Patient Centered Medical HomeДокумент21 страницаAHA Patient Centered Medical Homein678Оценок пока нет
- Costing Princples and Business Control Systems (Assessement Criteria 1.1)Документ22 страницыCosting Princples and Business Control Systems (Assessement Criteria 1.1)asus13018333% (3)
- Us Cons Mo Strategicchange 110910Документ3 страницыUs Cons Mo Strategicchange 110910Candice H.Оценок пока нет
- Improving Healthy by Getting LeanДокумент3 страницыImproving Healthy by Getting LeanLaura100% (2)
- Paper 5 Review The Literature of Balanced Scorecard and Performance Measurement 1Документ15 страницPaper 5 Review The Literature of Balanced Scorecard and Performance Measurement 1Kepher OnukoОценок пока нет
- Workplace Words and Phrases ArabicДокумент6 страницWorkplace Words and Phrases Arabicshadi alshadafanОценок пока нет
- Critical Analysis of Patient and Family Rights in Jci Accreditation and Cbahi Standards For HospitalsДокумент10 страницCritical Analysis of Patient and Family Rights in Jci Accreditation and Cbahi Standards For HospitalsImpact JournalsОценок пока нет
- ZBB Vs ABB Traditional BudgetingДокумент4 страницыZBB Vs ABB Traditional BudgetingAbhijeet KendoleОценок пока нет
- Tulsa Memorial Hospital, Santa FE Healthcare, Copperline HealthcareДокумент4 страницыTulsa Memorial Hospital, Santa FE Healthcare, Copperline Healthcarealka murarka50% (2)
- Inventing The Professional Association of The Future: Strategic Plan - 2017Документ28 страницInventing The Professional Association of The Future: Strategic Plan - 2017Iván Lech Villaseca DziekonskiОценок пока нет
- Week 2-2Документ8 страницWeek 2-2Marki Mendina100% (1)
- CSIA 360 Project 1 Cybersecurity For OPEN DataДокумент7 страницCSIA 360 Project 1 Cybersecurity For OPEN DataAyesha HanifОценок пока нет
- Stakeholder PresentationДокумент12 страницStakeholder PresentationBRUCE KENNEDYОценок пока нет
- ToolsCorp Corporation's Business PlanДокумент7 страницToolsCorp Corporation's Business PlanericОценок пока нет
- Case Study 2Документ3 страницыCase Study 2JoPaul Prado100% (2)
- Jeneise Mckenzie Resume - Operations Manager - Director of Operations - Business AnalystДокумент2 страницыJeneise Mckenzie Resume - Operations Manager - Director of Operations - Business AnalystMelanieОценок пока нет
- Arnold Palmer Hospital's Supply Chain ManagementДокумент1 страницаArnold Palmer Hospital's Supply Chain ManagementMichelle Ann Wong100% (1)
- Business Intelligence in Health Care IndustryДокумент2 страницыBusiness Intelligence in Health Care IndustrysasiarchieОценок пока нет
- United Healthcare Group SeminarДокумент18 страницUnited Healthcare Group SeminarEhab elhashmyОценок пока нет
- Quality Crest Healthcare ConsultantsДокумент8 страницQuality Crest Healthcare ConsultantsMohammad Muntaz AliОценок пока нет
- Nhs Efficiency Map Updated January 2017Документ14 страницNhs Efficiency Map Updated January 2017TomОценок пока нет
- Asian MedicalДокумент124 страницыAsian MedicalMelanie SamsonaОценок пока нет
- BPR Case HoneywellДокумент31 страницаBPR Case HoneywellFarhan Abdul MalikОценок пока нет
- Fundamental Management: Revenue Cycle Management & Revenue CalculationsДокумент30 страницFundamental Management: Revenue Cycle Management & Revenue Calculationscm senОценок пока нет
- CH 6 - Entry and ContractingДокумент24 страницыCH 6 - Entry and ContractingJawaher Al ShehhiОценок пока нет
- Delivering Cloud-Based Solutions For Hospitals, Physicians, Clinics, Patients, and PopulationДокумент4 страницыDelivering Cloud-Based Solutions For Hospitals, Physicians, Clinics, Patients, and PopulationsomyaОценок пока нет
- Healthcare CFO Operations Leader in Indianapolis IN Resume William Kevin FowlerДокумент3 страницыHealthcare CFO Operations Leader in Indianapolis IN Resume William Kevin FowlerWilliamKevinFowlerОценок пока нет
- E Health Investment StrategyДокумент64 страницыE Health Investment StrategyNetriderTheThechieОценок пока нет
- Cross 1988Документ11 страницCross 1988deltanueveОценок пока нет
- Graded - Final Paper - ShirleneДокумент16 страницGraded - Final Paper - ShirleneS_66713617 SLCОценок пока нет
- Service Blueprint Medical CenterДокумент1 страницаService Blueprint Medical CenterNguyen Le Hoang KimОценок пока нет
- OM 7011 Summer AssignmentДокумент12 страницOM 7011 Summer AssignmentrssarinОценок пока нет
- Refresher-Manacc Term PaperДокумент13 страницRefresher-Manacc Term Papersushi271999Оценок пока нет
- Balanced Scorecard ExamplesДокумент5 страницBalanced Scorecard Examplesapi-3825626100% (1)
- Hospital Management Information System ProjectДокумент4 страницыHospital Management Information System ProjectAlfredo Jimenez CharlesОценок пока нет
- Excel Files For Case 12 - Value PublishinДокумент12 страницExcel Files For Case 12 - Value PublishinGerry RuntukahuОценок пока нет
- DBMS Case Studies CSE IVSemДокумент23 страницыDBMS Case Studies CSE IVSemsatishgwОценок пока нет
- Week 2 Workshop SolutionsДокумент6 страницWeek 2 Workshop SolutionsJenDNg50% (2)
- Microsoft Balanced Scorecard Framework5Документ33 страницыMicrosoft Balanced Scorecard Framework5abcdeОценок пока нет
- Medical Center Marketing PlanДокумент8 страницMedical Center Marketing PlanIan CastroОценок пока нет
- SBE 2 Heuristic Aggregate PlanningДокумент4 страницыSBE 2 Heuristic Aggregate Planning洪億珊Оценок пока нет
- Activity Based Costing and Management Applied in A Hybrid Decision Support System For Order Management 2011 Decision Support SystemsДокумент15 страницActivity Based Costing and Management Applied in A Hybrid Decision Support System For Order Management 2011 Decision Support SystemsLilian BrodescoОценок пока нет
- Strengthen Patient Experience: (Implementation Plan of IDC Program) Domain 1: CommunicationДокумент23 страницыStrengthen Patient Experience: (Implementation Plan of IDC Program) Domain 1: CommunicationRina LestariОценок пока нет
- 200 Hospital BenchmarksДокумент16 страниц200 Hospital BenchmarksMustafa BapaiОценок пока нет
- Quiz 5 SolutionДокумент5 страницQuiz 5 SolutionMichel BanvoОценок пока нет
- Libro - Building A Project-Driven Enterprise - How To Slash Waste and Boost Profits Through Lean Project Management (2002) PDFДокумент384 страницыLibro - Building A Project-Driven Enterprise - How To Slash Waste and Boost Profits Through Lean Project Management (2002) PDFtlatuani1000Оценок пока нет
- 2019 3 15 Qms #2 Assessing Your Healthcare Quality ManagemДокумент47 страниц2019 3 15 Qms #2 Assessing Your Healthcare Quality ManagemHassen TalebОценок пока нет
- 13.SCM - Make Vs BuyДокумент2 страницы13.SCM - Make Vs BuyWah KhaingОценок пока нет
- Education Budget 2019-20 HighlightsДокумент15 страницEducation Budget 2019-20 HighlightsTejasvi TyagiОценок пока нет
- Is your insurance complaint unheard? Contact IRDA for helpДокумент10 страницIs your insurance complaint unheard? Contact IRDA for helpvinaysekharОценок пока нет
- Enlc 553 Business Plan Executive SummaryДокумент3 страницыEnlc 553 Business Plan Executive Summaryapi-407169026Оценок пока нет
- Medical Development PowerPoint TemplateДокумент16 страницMedical Development PowerPoint TemplatesugamОценок пока нет
- 3Q14 Roadmap To ValuationДокумент30 страниц3Q14 Roadmap To ValuationRyan BrookmanОценок пока нет
- 157 28395 EY111 2013 4 2 1 Chap004Документ91 страница157 28395 EY111 2013 4 2 1 Chap004David SelfanyОценок пока нет
- Course Content and Project OutlineДокумент4 страницыCourse Content and Project OutlineYasmine hanyОценок пока нет
- Profit Planning with Three WheelsДокумент28 страницProfit Planning with Three Wheelssiyeni100% (2)
- Research Ibnr Report 2009 PDFДокумент202 страницыResearch Ibnr Report 2009 PDFIotalaseria PutuОценок пока нет
- Case 10 Bennett's Machine Shop Inc PDFДокумент14 страницCase 10 Bennett's Machine Shop Inc PDFFatima AjmalОценок пока нет
- Paging MessagesДокумент51 страницаPaging MessagesFatima AjmalОценок пока нет
- GSM Frequency PlanningДокумент10 страницGSM Frequency PlanningIftikhar AhmadОценок пока нет
- GSM Radio Network PlanningДокумент4 страницыGSM Radio Network PlanningFatima AjmalОценок пока нет
- SH-3 Sea King - History Wars Weapons PDFДокумент2 страницыSH-3 Sea King - History Wars Weapons PDFchelcarОценок пока нет
- Debut Sample Script PDFДокумент9 страницDebut Sample Script PDFmaika cabralОценок пока нет
- The Order of Divine Service FOR Ash Wednesday: (Lutheran Church-Missouri Synod)Документ10 страницThe Order of Divine Service FOR Ash Wednesday: (Lutheran Church-Missouri Synod)Grace Lutheran Church, Little Rock, ArkansasОценок пока нет
- Mathematics: Textbook For Class XIIДокумент14 страницMathematics: Textbook For Class XIIFlowring PetalsОценок пока нет
- Can You Dribble The Ball Like A ProДокумент4 страницыCan You Dribble The Ball Like A ProMaradona MatiusОценок пока нет
- Metocean Design and Operating ConsiderationsДокумент7 страницMetocean Design and Operating ConsiderationsNat Thana AnanОценок пока нет
- 2011 Grade Exam ResultДокумент19 страниц2011 Grade Exam ResultsgbulohcomОценок пока нет
- 1170.2-2011 (+a5)Документ7 страниц1170.2-2011 (+a5)Adam0% (1)
- Mediocrity-The Unwated SinДокумент3 страницыMediocrity-The Unwated SinJay PatelОценок пока нет
- (Part B) APPLICATION LETTER, COVER LETTER, CV, RESUME & JOB INTERVIEW - Google Forms-1Документ10 страниц(Part B) APPLICATION LETTER, COVER LETTER, CV, RESUME & JOB INTERVIEW - Google Forms-1adОценок пока нет
- Narrative On Parents OrientationДокумент2 страницыNarrative On Parents Orientationydieh donaОценок пока нет
- 24 Directions of Feng ShuiДокумент9 страниц24 Directions of Feng Shuitoml88Оценок пока нет
- Battle of Qadisiyyah: Muslims defeat Sassanid PersiansДокумент22 страницыBattle of Qadisiyyah: Muslims defeat Sassanid PersiansMustafeez TaranОценок пока нет
- Multimodal Transport Bill of Lading PDFДокумент3 страницыMultimodal Transport Bill of Lading PDFJulia TombakОценок пока нет
- Ei 22Документ1 страницаEi 22larthОценок пока нет
- PEST Analysis of the Indian Pharmaceutical IndustryДокумент8 страницPEST Analysis of the Indian Pharmaceutical IndustryAnkush GuptaОценок пока нет
- BINUS University: Undergraduate / Master / Doctoral ) International/Regular/Smart Program/Global Class )Документ6 страницBINUS University: Undergraduate / Master / Doctoral ) International/Regular/Smart Program/Global Class )Doughty IncОценок пока нет
- Fe en Accion - Morris VendenДокумент734 страницыFe en Accion - Morris VendenNicolas BertoaОценок пока нет
- EAR Policy KhedaДокумент40 страницEAR Policy KhedaArvind SahaniОценок пока нет
- The Princess AhmadeeДокумент6 страницThe Princess AhmadeeAnnette EdwardsОценок пока нет
- I Am The One Who Would Awaken YouДокумент5 страницI Am The One Who Would Awaken Youtimsmith1081574Оценок пока нет
- Construction Management Guideline (Provisional Edition)Документ97 страницConstruction Management Guideline (Provisional Edition)Kaung Myat HtunОценок пока нет
- Architecture FirmДокумент23 страницыArchitecture Firmdolar buhaОценок пока нет
- Madhuri Economics of Banking Semester 1 ProjectДокумент35 страницMadhuri Economics of Banking Semester 1 ProjectAnaniya TiwariОценок пока нет
- True or FalseДокумент3 страницыTrue or FalseRB AbacaОценок пока нет
- Unit Test: VocabularyДокумент2 страницыUnit Test: VocabularyTrang PhạmОценок пока нет
- Irregular verbs guideДокумент159 страницIrregular verbs guideIrina PadureanuОценок пока нет
- How To Configure User Accounts To Never ExpireДокумент2 страницыHow To Configure User Accounts To Never ExpireAshutosh MayankОценок пока нет
- Meeting Consumers ' Connectivity Needs: A Report From Frontier EconomicsДокумент74 страницыMeeting Consumers ' Connectivity Needs: A Report From Frontier EconomicsjkbuckwalterОценок пока нет
- Addis Ababa University-1Документ18 страницAddis Ababa University-1ASMINO MULUGETA100% (1)