Академический Документы
Профессиональный Документы
Культура Документы
Type 2 DM
Загружено:
Api HrhpОригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Type 2 DM
Загружено:
Api HrhpАвторское право:
Доступные форматы
TYPE 2 DM Insulin resistance and abnormal insulin secretion are central to the development of type 2 DM.
Although controversy remains regarding the primary defect, most studies support the view that insulin resistance precedes insulin secretory defects and that diabetes develops only if insulin secretion becomes inadequate. GENETIC CONSIDERATIONS Type 2 DM has a strong genetic component. Major genes that predispose to this disorder have yet to be identified, but it is clear that the disease is polygenic and multifactorial. Various genetic loci contribute to susceptibility, and environmental factors (such as nutrition and physical activity) further modulate phenotypic expression of the disease. The concordance of type 2 DM in identical twins is between 70 and 90%. Individuals with a parent with type 2 DM have an increased risk of diabetes; if both parents have type 2 DM, the risk approaches 40%. Insulin resistance, as demonstrated by reduced glucose utilization in skeletal muscle, is present in many nondiabetic, first-degree relatives of individuals with type 2 DM. However, definition of the genetic susceptibility remains a challenge because the genetic defect in insulin secretion or action may not manifest itself unless an environmental event or another genetic defect, such as obesity, is superimposed. Mutations in various molecules involved in insulin action (e.g., the insulin receptor and enzymes involved in glucose homeostasis) account for a very small fraction of type 2 DM. Likewise, genetic defects in proteins involved in insulin secretion have not been found in most individuals with type 2 DM. Genome-wide scanning for mutations or polymorphisms associated with type 2 DM is being used in an effort to identify genes associated with type 2 DM. The gene for the protease, calpain 10, is associated with type 2 DMin Hispanic and some other populations. Pathophysiology Type 2 DM is characterized by three pathophysiologic abnormalities: impaired insulin secretion, peripheral insulin resistance, and excessive hepatic glucose production. Obesity, particularly visceral or central (as evidenced by the hip-waist ratio), is very common in type 2 DM. Adipocytes secrete a number of biologic products (leptin, TNF-_, free fatty acids, resistin, and adiponectin) that modulate insulin secretion, insulin action, and body weight and may contribute to the insulin resistance. In the early stages of the disorder, glucose tolerance remains normal, despite insulin resistance, because the pancreatic beta cells compensate by increasing insulin output (Fig.323-6). As insulin resistance and compensatory hyperinsulinemia progress, the pancreatic islets in certain individuals are unable to sustain the hyperinsulinemic state. IGT, characterized by elevations in postprandial glucose, then develops. A further decline in insulin secretion and an increase in hepatic glucose production lead to overt diabetes with fasting hyperglycemia. Ultimately, beta cell failure may ensue. Markers of inflammation such as IL-6 and C-reactive protein are often elevated in type 2 diabetes. Metabolic Abnormalities _ INSULIN RESISTANCE The decreased ability of insulin to act effectively on peripheral target tissues (especially muscleand liver) is a prominent feature of type 2 DM and results from a combination of genetic susceptibility and obesity. Insulin resistance is relative, however, since supernormal levels of circulating insulin will normalize the plasma glucose. Insulin dose-response curves exhibit a rightward shift, indicating reduced sensitivity, and a reduced maximal response, indicating an overall decrease in maximum glucose utilization (30 to 60% lower than normal individuals). Insulin resistance impairs glucose utilization by insulinsensitive tissues and increases hepatic glucose output; both effects contribute to the hyperglycemia. Increased hepatic glucose output predominantly accounts for increased FPG
levels, whereas decreased peripheral glucose usage results in postprandial hyperglycemia. In skeletal muscle, there is a greater impairment in nonoxidative glucose usage (glycogen formation) than in oxidative glucose metabolism through glycolysis. Glucose metabolism in insulin-independent tissues is not altered in type 2 DM. The precise molecular mechanism of insulin resistance in type 2 DM has not been elucidated. Insulin receptor levels and tyrosine kinase activity in skeletal muscle are reduced, but these alterations are most likely secondary to hyperinsulinemia and are not a primary defect. Therefore, postreceptor defects are believed to play the predominant role in insulin resistance (Fig. 323-4). Polymorphisms in IRS-1 may be associated with glucose intolerance, raising the possibility that polymorphisms in various postreceptor molecules may combine to create an insulin-resistant state. The pathogenesis of insulin resistance is currently focused on a PI-3-kinase signaling defect, which reduces translocation of GLUT4 to the plasma membrane, among other abnormalities. Of note, not all insulin signal transduction pathways are resistant to the effects of insulin [e.g., those controlling cell growth and differentiation and using the mitogen-activated protein (MAP) kinase pathway; Fig. 323-4]. Consequently, hyperinsulinemia may increase the insulin action through these pathways, potentially accelerating diabetes-related conditions such as atherosclerosis. Another emerging theory proposes that elevated levels of free fatty acids, a common feature of obesity, may contribute to the pathogenesis of type 2 DM. Free fatty acids can impair glucose utilization in skeletal muscle, promote glucose production by the liver, and impair beta cell function. IMPAIRED INSULIN SECRETION Insulin secretion and sensitivity are interrelated (Fig. 323-6). In type 2 DM, insulin secretion initially increases in response to insulin resistance to maintain normal glucose tolerance. Initially, the insulin secretory defect is mild and selectively involves glucosestimulated insulin secretion. The response to other nonglucose secretagogues, such as arginine, is preserved. Eventually, the insulin secretory defect progresses to a state of grossly inadequate insulin secretion. The reason(s) for the decline in insulin secretory capacity in type 2 DM is unclear. Despite the assumption that a second genetic defectsuperimposed upon insulin resistance leads to beta cell failure, intense genetic investigation has so far excluded mutations in isletcandidate genes. Islet amyloid polypeptide or amylin is cosecreted by the beta cell and likely forms the amyloid fibrillar deposit found in the islets of individuals with long-standing type 2 DM. Whether such islet amyloid deposits are a primary or secondary event is not known. The metabolic environment of diabetes may also negatively impact islet function. For example, chronic hyperglycemia paradoxically impairs islet function (glucose toxicity) and leads to a worsening of hyperglycemia. Improvement in glycemic control is often associated with improved islet function. In addition, elevation of free fatty acid levels (lipotoxicity) and dietary fat may also worsen islet function. INCREASED HEPATIC GLUCOSE PRODUCTION In type 2 DM, insulin resistance in the liver reflects the failure of hyperinsulinemia to suppress gluconeogenesis, which results in fasting hyperglycemia and decreased glycogen storage by the liver in the postprandial state. Increased hepatic glucose production occurs early in the course of diabetes, though likely after the onset of insulin secretory abnormalities and insulin resistance in skeletal muscle. (harrison)
Kasper, Dennis L, et al. Harrisons Principles Of Internal Medicine. 16th Ed. New York: McGraw-Hill. 2001. p.2155-58. Pathophysiology of type 2 diabetes mellitus Type 2 diabetes mellitus is a heterogeneous disorder with varying prevalence among different ethnic groups. In the United States the populations most affected are native Americans, particularly in the desert Southwest, Hispanic-Americans, and Asian-Americans (1). The pathophysiology of type 2 diabetes mellitus is characterized by peripheral insulin resistance, impaired regulation of hepatic glucose production, and declining b-cell function, eventually leading to b-cell failure. The primary events are believed to be an initial deficit in insulin secretion and, in many patients, relative insulin deficiency in association with peripheral insulin resistance (16, 17). The b-cell b-Cell dysfunction is initially characterized by an impairment in the first phase of insulin secretion during glucose stimulation and may antedate the onset of glucose intolerance in type 2 diabetes (18). Initiation of the insulin response depends upon the transmembranous transport of glucose and coupling of glucose to the glucose sensor. The glucose/glucose sensor complex then induces an increase in glucokinase by stabilizing the protein and impairing its degradation. The induction of glucokinase serves as the first step in linking intermediary metabolism with the insulin secretory apparatus. Glucose transport in b-cells of type 2 diabetes patients appears to be greatly reduced, thus shifting the control point for insulin secretion from glucokinase to the glucose transport system (19, 20). This defect is improved by the sulfonylureas (21, 22). Later in the course of the disease, the second phase release of newly synthesized insulin is impaired, an effect that can be reversed, in part at least in some patients, by restoring strict control of glycemia. This secondary phenomenon, termed desensitization or b-cell glucotoxicity, is the result of a paradoxical inhibitory effect of glucose upon insulin release and may be attributable to the accumulation of glycogen within the b-cell as a result of sustained hyperglycemia (23). Other candidates that have been proposed are sorbital accumulation in the b-cell or the nonenzymatic glycation of b-cell proteins. Other defects in b-cell function in type 2 diabetes mellitus include defective glucose potentiation in response to nonglucose insulin secretagogues, asynchronous insulin release, and a decreased conversion of proinsulin to insulin (24, 25). An impairment in first phase insulin secretion may serve as a marker of risk for type 2 diabetes mellitus in family members of individuals with type 2 diabetes mellitus (26 30) and may be seen in patients with prior gestational diabetes (31). However, impaired first phase insulin secretion alone will not cause impaired glucose tolerance. Autoimmune destruction of pancreatic b-cells may be a factor in a small subset of type 2 diabetic patients and has been termed the syndrome of latent autoimmune diabetes in adults. This group may represent as many as 10% of Scandinavian patients with type 2 diabetes and has been identified in the recent United Kingdom study, but has not been well characterized in other populations (46, 30). Glucokinase is absent within the b-cell in some families with maturity-onset diabetes of young (31). However, deficiencies of glucokinase have not been found in other forms of type 2 diabetes (32, 33). In summary, the delay in the first phase of insulin secretion, although of some diagnostic import, does not appear to act independently in the pathogenesis of type 2 diabetes. In some early-onset patients with type 2 diabetes (perhaps as many as 20%) (4, 5), there may be a deficiency in insulin secretion that may or may not be due to autoimmune destruction of the b-cell and is not due to a deficiency in the glucokinase gene. In the great majority of patients with type 2 diabetes (680%), the delay in immediate insulin response is accompanied by a secondary hypersecretory phase of insulin release as a result of either an inherited or acquired defect within the b-cell or a compensatory response to peripheral insulin resistance. Over a
prolonged period of time, perhaps years, insulin secretion gradually declines, possibly as a result of intraislet accumulation of glucose intermediary metabolites (34). In view of the decline in b-cell mass, sulfonylureas appear to serve a diminishing role in the long term management of type 2 diabetes (35). Unanswered is whether amelioration of insulin resistance with earlier detection or newer insulin-sensitizing drugs will retard the progression of b-cell failure, obviating or delaying the need for insulin therapy. Insulin resistance Emanating from the prismatic demonstration by Yalow and Berson of the presence of hyperinsulinism in type 2 diabetes, insulin resistance has been considered to play an integral role in the pathogenesis of the disease (36). Recent critical reviews, however, have questioned the primacy, specificity, and contribution of insulin resistance to the disease state (37, 38). As chronic hyperinsulinemia inhibits both insulin secretion (39) and action (40), and hyperglycemia can impair both the insulin secretory response to glucose (41) as well as cellular insulin sensitivity (42, 43), the precise relation between glucose and insulin level as a surrogate measure of insulin resistance has been questioned. Lean type 2 diabetic patients over 65 yr of age have been found to be as insulin sensitive as their age-matched nondiabetic controls (44). Moreover, in the majority of type 2 diabetic patients who are insulin resistant, obesity is almost invariably present (45, 46). As obesity or an increase in intraabdominal adipose tissue is associated with insulin resistance in the absence of diabetes, it is believed by some that insulin resistance in type 2 diabetes is entirely due to the coexistence of increased adiposity (47). Additionally, insulin resistance is found in hypertension, hyperlipidemia, and ischemic heart disease, entities commonly found in association with diabetes (16, 48, 49), again raising the question as to whether insulin resistance results from different pathogenetic disease processes or is unique to the presence of type 2 diabetes (16, 50, 51). Prospective studies have demonstrated the presence of either insulin deficiency or insulin resistance before the onset of type 2 diabetes (48). Two studies have reported the presence of insulin resistance in nondiabetic relatives of diabetic patients at a time when their glucose tolerance was still normal (52, 53). In addition, first degree relatives of patients with type 2 diabetes have been found to have impaired insulin action upon skeletal muscle glycogen synthesis due to both decreased stimulation of tyrosine kinase activity of the insulin receptor and reduced glycogen synthase activity (54, 55). Other studies in this high risk group have failed to demonstrate insulin resistance, and in the same group, impaired early phase insulin release and loss of normal oscillatory pattern of insulin release have been described (56, 57). Based upon these divergent studies, it is still impossible to dissociate insulin resistance from insulin deficiency in the pathogenesis of type 2 diabetes. However, both entities unequivocally contribute to the fully established disease. The liver The ability of insulin to suppress hepatic glucose production both in the fasting state and postprandially is normal in first degree relatives of type 2 diabetic patients (26). It is the increase in the rate of postprandial glucose production that heralds the evolution of IGT (52). Eventually, both fasting and postprandial glucose production increase as type 2 diabetes progresses. Hepatic insulin resistance is characterized by a marked decrease in glucokinase activity and a catalytic increased conversion of substrates to glucose despite the presence of insulin (53). Thus, the liver in type 2 diabetes is programmed to both overproduce and underuse glucose. The elevated free fatty acid levels found in type 2 diabetes may also play a role in increased hepatic glucose production (50). In addition, recent evidence suggests an important role for the kidney in glucose production via gluconeogenesis, which is unrestrained in the presence of type 2 diabetes (58) CLINICAL REVIEW 102. Type 2 Diabetes Mellitus: Update on Diagnosis, Pathophysiology, and Treatment. RICHARD J. MAHLER AND MICHAEL L. ADLER
Division of Diabetes, Endocrinology, and Metabolism, Cornell University Medical College, New York 0021-972X/99/$03.00/0 Vol. 84, No. 4. The Journal of Clinical Endocrinology & Metabolism Printed in U.S.A. Copyright 1999 by The Endocrine Society 1165-66 Heredity in type 2 diabetes mellitus Although lifestyle and overeating seem to be the triggering pathogenic factors, genetic elements are also involved in the pathogenesis of type 2 diabetes. Positive family history confers a 24 fold increased risk for type 2 diabetes. 15-25% of first-degree relatives of patients with type 2 diabetes develop impaired glucose tolerance or diabetes.15 The lifetime risk (at age 80 years) for type 2 diabetes has been calculated to be 38% if one parent had type 2 diabetes.15 If both parents are affected, the prevalence of type 2 diabetes in the offspring is estimated to approach 60% by the age of 60 years.16 Since dizygotic twins share the environment (both intrauterine and extrauterine) but only 50% of their genes, concordance rates in monozygotic twins in excess of those in dizygotic twins have been used to distinguish genetic from non-genetic contributions. In individuals older than 60 years, concordance rates for diabetes were 35-58% in monozygotic twins, compared with 17-20% in dizygotic twins.17,18 Inclusion of impaired glucose tolerance markedly increased the concordance in monozygotic twins to 88%.19 Nevertheless, concordance rates in monozygotic twins might produce an underestimate of genetic effects, because the monochorionic intrauterine nutrition of monozygotic twins has been shown to result in growth retardation compared with dizygotic twins.32 And low birthweight itself is associated with increased risk of type 2 diabetes later in life. 33,34 Pathophysiology of hyperglycaemia To understand the cellular and molecular mechanisms responsible for type 2 diabetes it is necessary to conceptualise the framework within which glycaemia is controlled. Insulin is the key hormone for regulation of blood glucose and, generally, normoglycaemia is maintained by the balanced interplay between insulin action and insulin secretion. Importantly, the normal pancreatic cell can adapt to changes in insulin action--ie, a decrease in insulin action is accompanied by upregulation of insulin secretion (and vice versa). Figure 2 illustrates the curvilinear relation between normal -cell function and insulin sensitivity.35 Deviation from this hyperbola, such as in the patients with impaired glucose tolerance and type 2 diabetes in figure 2, occurs when -cell function is inadequately low for a specific degree of insulin sensitivity. Thus, -cell dysfunction is a critical component in the pathogenesis of type 2 diabetes. This concept has been verified not only in cross-sectional studies but also longitudinally in Pima Indians progressing from normal to impaired glucose tolerance to type 2 diabetes.36 In people with normal glucose tolerance (NGT) a quasi-hyperbolic relation exists between cell function and insulin sensitivity. With deviation from this hyperbola, deterioration of glucose tolerance (impaired glucose tolerance [IGT], and type 2 diabetes [T2DM]) occurs. However, not only deviation from but also progression along the hyperbola affects glycaemia. When insulin action decreases (as with increasing obesity) the system usually compensates by increasing -cell function. However, at the same time, concentrations of
blood glucose at fasting and 2 h after glucose load will increase mildly.37 This increase may well be small, but over time becomes damaging because of glucose toxicity, and in itself a cause for -cell dysfunction. Thus, even with (theoretically) unlimited -cell reserve, insulin resistance paves the way for hyperglycaemia and type 2 diabetes. Insulin resistance Insulin resistance is said to be present when the biological effects of insulin are less than expected for both glucose disposal in skeletal muscle and suppression of endogenous glucose production primarily in the liver.38 In the fasting state, however, muscle accounts for only a small proportion of glucose disposal (less than 20%) whereas endogenous glucose production is responsible for all the glucose entering the plasma. Endogenous glucose production is accelerated in patients with type 2 diabetes or impaired fasting glucose.39,40 Because this increase occurs in the presence of hyperinsulinaemia, at least in the early and intermediate disease stages, hepatic insulin resistance is the driving force of hyperglycaemia of type 2 diabetes (figure 3).
Insulin secretion from the pancreas normally reduces glucose output by the liver, enhances glucose uptake by skeletal muscle, and suppresses fatty acid release from fat tissue. The various factors shown that contribute to the pathogenesis of type 2 diabetes affect both insulin secretion and insulin action. Decreased insulin secretion will reduce insulin signalling in its target tissues. Insulin resistance pathways affect the action of insulin in each of the major target tissues, leading to increased circulating fatty acids and the hyperglycaemia of diabetes.
In turn, the raised concentrations of glucose and fatty acids in the bloodstream will feed back to worsen both insulin secretion and insulin resistance. Obesity Insulin resistance is strongly associated with obesity and physical inactivity, and several mechanisms mediating this interaction have been identified. A number of circulating hormones, cytokines, and metabolic fuels, such as non-esterified (free) fatty acids (NEFA) originate in the adipocyte and modulate insulin action. An increased mass of stored triglyceride, especially in visceral or deep subcutaneous adipose depots, leads to large adipocytes that are themselves resistant to the ability of insulin to suppress lipolysis. This results in increased release and circulating levels of NEFA and glycerol, both of which aggravate insulin resistance in skeletal muscle and liver (figure 3).41 Excessive fat storage not only in adipocytes but "ectopically" in non-adipose cells also has an important role.42 For example, increased intramyocellular lipids are associated with skeletal muscle insulin resistance under some circumstances.43 The coupling between intrahepatic lipids and hepatic insulin resistance seems to be even tighter.44,45 Insulin receptor knock-out models To understand the contribution of insulin resistance in a particular tissue to whole body glucose homoeostasis, conditional knockouts of the insulin receptor have been created using the Cre-lox system. Among the five conditional insulin receptor knockouts shown in table 3, only liver47 and -cell specific knockouts50 became glucose intolerant whereas, unexpectedly, knockout models specific for muscle46 and fat cells48 did not. These findings clearly support a central role of hepatic insulin resistance in the pathogenesis of type 2 diabetes, and suggest that an adequate insulin signal in the pancreatic cell is needed to maintain its function.
Cellular mechanisms Insulin elicits its pleiotropic metabolic responses by binding to and activating a specific plasma membrane receptor with tyrosine kinase activity.51 Cellular substrates of the insulin receptor kinase, most prominently the insulin receptor substrate (IRS) proteins, are efficiently tyrosine phosphorylated on several sites, which serve as binding scaffolds for various adaptor proteins and lead to the downstream signalling cascade (figure 4).52 Insulin activates a series of lipid and protein kinase enzymes linked to the translocation of glucose transporters to the
cell surface, synthesis of glycogen, protein, mRNAs, and nuclear DNA, which affect cell survival and proliferation. Phosphorylation and dephosphorylation of IRS proteins In states of insulin resistance, one or more of the following molecular mechanisms to block insulin signalling are likely to be involved. The positive effects on downstream responses exerted by tyrosine phosphorylation of the receptor and the IRS proteins are opposed by dephosphorylation of these tyrosine side-chains by cellular protein-tyrosine phosphatases and by protein phosphorylation on serine and threonine residues, which often occur together.53 Phosphotyrosine phosphatase 1B (PTP1B) is widely expressed and has an important role in the negative regulation of insulin signalling.54 Insulin signalling involves binding of insulin to its receptor followed by a cascade of intracellular events, depicted as activation pathways. Negative modulation of insulin action can be mediated via various pathways leading to insulin resistance: various inhibitory triggers affect their respective signal modulators (partly via transcription factors), which lead through deactivating pathways (tyrosine phosphatases, serine kinases, lipid phosphatases and degradation pathways) to inhibitory actions on insulin signalling (activation pathways). Adiponectin has an ameliorating function on glucose metabolism apart from insulin signalling. PKC=protein kinase C. PTEN=phosphatase and tensin homologue. PI=phosphoinositol. Serine/threonine phosphorylation of IRS1 reduces its ability to act as a substrate for the tyrosine kinase activity of the insulin receptor and inhibits its coupling to its major downstream effector systems. Several IRS serine kinases have been identified, including various mitogen-activated protein kinases, c-Jun NH2-terminal kinase, atypical protein kinase C, and phosphatidylinositol 3-kinase, among others.52 Signal downregulation can also occur through internalisation and loss of the insulin receptor from the cell surface and degradation of IRS proteins.55 Members of the suppressor of cytokine signalling (SOCS) family of proteins participate in IRS protein degradation through a ubiquitin-proteosomal pathway (figure 4).56 Role of adipocyte products and inflammation Increased concentrations of NEFA and inflammatory cytokines (eg, tumour necrosis factor alpha [TNFalpha] and interleukin 6) released by expanded visceral adipose tissue adversely affect the insulin signalling cascade.57,58 NEFA inhibit insulin-stimulated glucose metabolism in skeletal muscle and stimulate gluconeogenesis in liver.59,60 They activate cellular kinases, including atypical protein kinase C isoforms by increasing cellular diacylglycerol levels, which can activate the inflammatory kinases inhibitor kappaB kinase (IKK) and c-jun N-terminal kinase, increasing serine/threonine phosphorylation of IRS1 and reducing downstream IRS1 signalling, as previously described.61-63 TNFalpha enhances adipocyte lipolysis, which further increases NEFA, and also elicits its own direct negative effects on insulin signalling pathways.64 Neutralisation of TNFalpha substantially reverses insulin resistance in rodents; however, the magnitude of its involvement in human insulin resistance is not entirely clear.65 The proinflammatory interleukin 6 inhibits the insulin signal by augmenting the expression of SOCS proteins.66,67 Adiponectin
Whereas circulating NEFA and several adipokines are increased in visceral obesity, the concentrations of the adipose-specific protein adiponectin are decreased, reducing its insulinsensitising effects in liver and muscle.57,68 Adiponectin signals via AMP kinase, a stressactivated signalling enzyme implicated in various metabolic responses, including suppression of hepatic gluconeogenesis, glucose uptake in exercising skeletal muscle, fatty acid oxidation, and inhibition of lipolysis, which might explain its beneficial metabolic effects.68-72 AMP kinase has also been implicated in the mechanism of action of metformin,73,74 and possibly of the thiazolidinediones,75 suggesting that it has a role in clinical anti-diabetic responses. NFkappaB and IKK activity A close connection between insulin resistance and classic inflammatory signalling pathways has also recently been identified. Nuclear factor kappaB (NFkappaB) is held in an inactive state in resting conditions by binding to an inhibitory partner, IkappaB.76 Phosphorylation of IkappaB by its kinase (IKK) leads to IkappaB degradation, releasing NFkappaB for translocation to the nucleus where it can affect the transcription of diverse genes involved in the inflammatory response. High doses of salicylates, which block IKK activity,77 can ameliorate hyperglycaemia and insulin resistance in diabetes and obesity.78,79 More importantly, genetic disruption of IKK returned skeletal muscle insulin resistance caused by NEFA to normal, through improvement in IRS1 tyrosine phosphorylation and activation of its downstream signal cascade.80 Overall, this evidence suggests that IKK might be an important target for the development of new therapeutics in insulin resistance, especially in the setting of visceral adiposity. In addition to their effects on insulin signalling, the circulating adipose tissue factors strongly affect vascular endothelial function, linking the increased vascular risk in the metabolic syndrome with mechanisms of cellular insulin resistance.68,81 Adipose secretory factors also recruit and activate inflammatory cells, which can further perpetuate a systemic inflammatory milieu that can strongly affect vascular function and atherogenesis.82 Mitochondrial metabolism The accumulation of ectopic triglyceride in visceral depots (mainly in the liver) has suggested a defect in mitochondrial lipid oxidation in patients with type 2 diabetes, who have impaired oxidative capacity and small mitochondria in skeletal muscle.83 PPARgamma co-activator 1 (PGC1), a transcription factor for genes involved in mitochondrial fatty acid oxidation and ATP synthesis, was decreased in young, lean, insulin-resistant offspring of parents with type 2 diabetes, suggesting that an inherited defect in mitochondrial oxidative phosphorylation could lead to cellular lipid accumulation.84 Gene expression profiling studies have also shown that decreased expression of PGC1 and related gene products could affect mitochondrial function in people with insulin-resistance and type 2 diabetes.85,86 -cell dysfunction Various abnormalities in insulin secretion are present in patients with type 2 diabetes. Basal insulin concentrations may be raised to roughly double the usual value, especially in obese hyperglycaemic patients, but this finding is presumably due to increased plasma glucose. Similarly, after a meal, concentrations of insulin in plasma can appear higher than normal, because of substantially raised plasma glucose. Indeed, hyperglycaemic glucose clamp studies under standardised conditions of identical glycaemia have shown that insulin
secretion is markedly diminished compared with non-diabetic individuals with similar anthropometric characteristics.87 But even before the development of overt hyperglycaemia, which in itself adversely affects -cell function, secretory defects have been shown, for example in individuals with impaired glucose tolerance and impaired fasting glucose.88 Moreover, both normoglycaemic offspring of type 2 diabetic parents and non-diabetic twinsiblings of diabetic patients have reduced insulin secretion.87 Thus, in predisposed individuals, an insulin secretory defect is present, possibly on a genetic basis.89 Obesity, acute illness, or simply ageing might further expose or aggravate the underlying defect, ultimately leading to overt diabetes.87 Type 2 diabetes: principles of pathogenesis and therapy. Michael Stumvoll, Barry J Goldstein, Timon W van Haeften. Lancet, April 9 2005; 365: 1333-46 Reseptor insulin model knock-out Untuk memahami kontribusi resistensi insulin di jaringan tertentu untuk seluruh tubuh glukosa homoeostasis, bersyarat KO dari reseptor insulin telah diciptakan menggunakan Cresistem salmon asap. Di antara kelima bersyarat reseptor insulin KO ditunjukkan dalam tabel 3, hanya liver47 dan -sel knockouts50 tertentu menjadi tidak toleran glukosa sedangkan, secara tak terduga, model KO spesifik untuk muscle46 dan lemak tidak cells48. Temuan ini dengan jelas mendukung peran sentral resistensi insulin hepatik dalam patogenesis diabetes tipe 2, dan menunjukkan bahwa sinyal insulin yang memadai dalam sel pankreas yang dibutuhkan untuk mempertahankan fungsinya. Cellular mekanisme Insulin memunculkan metabolik yang pleiotropic tanggapan dengan cara mengikat dan mengaktifkan reseptor membran plasma spesifik tirosin kinase dengan substrat Seluler activity.51 dari reseptor insulin kinase, yang paling menonjol substrat reseptor insulin (IRS) protein, secara efisien fosforilasi tirosin pada beberapa situs, yang berfungsi sebagai perancah mengikat untuk berbagai adaptor protein dan mengarah ke hilir kaskade sinyal (gambar 4) mengaktifkan insulin ,52 serangkaian lipid dan protein enzim kinase dikaitkan dengan translokasi glukosa transporter ke permukaan sel, sintesis glikogen, protein, mRNA , dan DNA inti, yang mempengaruhi kelangsungan hidup dan proliferasi sel. Fosforilasi dan dephosphorylation dari IRS protein Dalam keadaan resistensi insulin, satu atau lebih hal berikut mekanisme molekuler untuk memblokir sinyal insulin cenderung terlibat. Efek positif hilir tanggapan yang diberikan oleh fosforilasi tirosin pada reseptor dan protein IRS ditentang oleh dephosphorylation ini rantai samping tirosin oleh protein seluler tirosin fosfatase dan oleh fosforilasi protein pada residu serin dan treonin, yang sering terjadi together.53 Phosphotyrosine fosfatase 1B (PTP1B) adalah dinyatakan secara luas dan mempunyai peranan penting dalam regulasi negatif insulin signalling.54 Sinyal insulin melibatkan mengikat insulin ke reseptornya diikuti oleh peristiwa intraselular kaskade, digambarkan sebagai jalur aktivasi. Modulasi negatif insulin tindakan dapat ditengahi melalui berbagai jalur yang mengarah ke resistensi insulin: berbagai
penghambatan memicu mempengaruhi modulator sinyal masing-masing (sebagian melalui faktor transkripsi), yang memimpin melalui jalur menonaktifkan (tirosin fosfatase, serin kinase, fosfatase dan degradasi lipid jalur) untuk tindakan pada insulin penghambatan sinyal (aktivasi jalur). Adiponektin memiliki fungsi ameliorating metabolisme glukosa terpisah dari sinyal insulin. PKC = protein kinase C. PTEN = fosfatase dan tensin homolog. PI = fosfoinositol. Serin / treonin fosforilasi IRS1 mengurangi kemampuannya untuk bertindak sebagai substrat untuk aktivitas kinase tirosin reseptor insulin dan menghambat dengan kopel ke hilir utama sistem efektor. Beberapa kinase serin IRS telah diidentifikasi, termasuk berbagai mitogen-activated protein kinase, c-Jun NH2-terminal kinase, atipikal protein kinase C, dan phosphatidylinositol 3-kinase, antara downregulation Sinyal others.52 juga dapat terjadi melalui internalisation dan hilangnya reseptor insulin dari permukaan sel dan degradasi IRS proteins.55 Anggota penekan dari sinyal sitokin (SOCS) keluarga protein IRS berpartisipasi dalam degradasi protein melalui jalur ubiquitin-proteosomal (gambar 4) .56 Peran produk dan peradangan adipocyte Peningkatan konsentrasi NEFA dan sitokin peradangan (misalnya, tumor nekrosis faktor alfa [TNFalpha] dan interleukin 6) yang dikeluarkan oleh jaringan adiposa viseral diperluas mempengaruhi sinyal insulin cascade.57, 58 NEFA distimulasi insulin menghambat metabolisme glukosa dalam otot rangka dan merangsang glukoneogenesis di liver.59, 60 Mereka mengaktifkan kinase selular, termasuk atipikal protein kinase C isoform dengan meningkatkan tingkat diasilgliserol selular, yang dapat mengaktifkan inflamasi kappaB kinase inhibitor kinase (IKK) dan c-jun N-terminal kinase, meningkatkan serin / treonin fosforilasi IRS1 dan mengurangi sinyal IRS1 hilir, seperti sebelumnya described.61-63 TNFalpha meningkatkan adipocyte lipolysis, yang meningkat lebih lanjut NEFA, dan juga sendiri langsung memunculkan efek negatif pada insulin Netralisasi dari pathways.64 sinyal secara substansial membalikkan TNFalpha resistansi insulin pada tikus, namun besarnya keterlibatannya dalam resistensi insulin manusia tidak sepenuhnya clear.65 properadangan interleukin 6 yang menghambat sinyal insulin oleh peningkatan ekspresi SOCS proteins.66, 67 Adiponektin Sedangkan beredar NEFA dan beberapa adipokines meningkat pada obesitas mendalam, konsentrasi dari protein spesifik adiposa adiponektin yang menurun, mengurangi efek sensitising insulin dalam hati dan muscle.57, 68 adiponectin sinyal melalui AMP kinase, suatu sinyal diaktifkan stres-enzim terlibat dalam berbagai tanggapan metabolik, termasuk penindasan glukoneogenesis hepatik, ambilan glukosa dalam menjalankan otot rangka, oksidasi asam lemak, dan penghambatan lipolysis, yang mungkin menjelaskan menguntungkan metabolisme effects.68-72 AMP kinase juga telah terlibat dalam mekanisme tindakan metformin, 73,74 dan mungkin dari thiazolidinediones, 75 menunjukkan bahwa ia memiliki peran dalam anti-diabetes klinis tanggapan. NFkappaB dan aktivitas IKK
Sebuah hubungan erat antara resistansi insulin dan inflamasi klasik jalur sinyal juga baru-baru ini telah diidentifikasi. Faktor nuklir kappaB (NFkappaB) diadakan di sebuah negara tidak aktif dalam kondisi beristirahat dengan cara mengikat sebuah pasangan penghambatan, IkappaB.76 Fosforilasi IkappaB oleh kinase (IKK) menyebabkan degradasi IkappaB, melepaskan NFkappaB untuk translokasi ke nukleus di mana ia dapat mempengaruhi transkripsi gen beragam yang terlibat dalam respon inflamasi. Salisilat dosis tinggi, yang menghambat aktivitas IKK, 77 dapat memperbaiki hyperglycaemia dan resistensi insulin pada diabetes dan obesity.78, 79 Lebih penting lagi, gangguan genetik IKK kembali otot rangka disebabkan oleh resistansi insulin NEFA normal, melalui perbaikan dalam fosforilasi tirosin dan IRS1 aktivasi dari sinyal hilir cascade.80 Secara keseluruhan, bukti ini menunjukkan bahwa IKK mungkin menjadi sasaran penting untuk pengembangan terapi baru dalam resistensi insulin, terutama dalam penetapan adiposity mendalam. Selain efek pada insulin mereka sinyal, jaringan adiposa yang bersirkulasi faktor sangat mempengaruhi fungsi endotel vaskular, menghubungkan peningkatan risiko vaskuler sindrom metabolik seluler dengan mekanisme insulin resistance.68, 81 adipose faktor sekretorik juga merekrut dan mengaktifkan sel-sel inflamasi, yang selanjutnya dapat melestarikan lingkungan peradangan sistemik yang dapat sangat mempengaruhi fungsi vaskular dan atherogenesis.82 Mitochondrial metabolisme Ektopik akumulasi trigliserida di tempat pengisian mendalam (terutama dalam hati) telah menyarankan sebuah cacat dalam oksidasi lipid mitokondria pada pasien dengan diabetes tipe 2, yang memiliki kapasitas dan cacat oksidatif mitokondria kecil dalam kerangka bersama-muscle.83 PPARgamma penggerak 1 (PGC1) , suatu faktor transkripsi gen mitokondria terlibat dalam oksidasi asam lemak dan sintesis ATP, sedang menurun di muda, ramping, tahan insulin keturunan dari orang tua dengan diabetes tipe 2, menyatakan bahwa cacat yang diturunkan dalam fosforilasi oksidatif mitokondria dapat menyebabkan akumulasi lipid seluler. Ekspresi gen profil 84 penelitian juga menunjukkan bahwa penurunan ekspresi gen PGC1 dan produk terkait dapat mempengaruhi fungsi mitokondria pada orang dengan resistensi insulin dan tipe 2 diabetes.85, 86 -cell disfungsi Berbagai kelainan sekresi insulin hadir pada pasien dengan diabetes tipe 2. Konsentrasi insulin basal dapat dinaikkan untuk kira-kira dua kali lipat nilai biasa, terutama pada pasien obesitas hyperglycaemic, tetapi temuan ini mungkin karena meningkatnya glukosa plasma. Demikian pula, setelah makan, konsentrasi insulin dalam plasma dapat muncul lebih tinggi dari biasanya, karena secara substansial mengangkat glukosa plasma. Memang, penjepit glukosa hyperglycaemic studi di bawah kondisi standar identik glycaemia telah menunjukkan bahwa sekresi insulin berkurang secara mencolok dibandingkan dengan individu nondiabetes yang sama antropometrik characteristics.87 Tapi bahkan sebelum pengembangan terbuka hyperglycaemia, yang dengan sendirinya merugikan mempengaruhi fungsi sel - , sekretorik cacat telah ditunjukkan, misalnya pada individu dengan gangguan dan gangguan toleransi glukosa puasa glucose.88 Selain itu, baik normoglycaemic keturunan diabetes tipe 2 orangtua dan non-diabetes-saudara kembar dari pasien diabetes telah mengurangi insulin
secretion.87 Dengan demikian, dalam cenderung individu, sekresi insulin cacat hadir, mungkin pada basis.89 genetik Obesitas, penyakit akut, atau sekadar penuaan mungkin lebih jauh mengekspos atau memperburuk cacat yang mendasarinya, pada akhirnya menyebabkan terbuka diabetes.87
Вам также может понравиться
- Case Study - Diabetes Mellitus (Nutrition&Dietetics)Документ10 страницCase Study - Diabetes Mellitus (Nutrition&Dietetics)Summer Suarez100% (1)
- Type 2 Diabetes MellitusДокумент19 страницType 2 Diabetes MellitusFelipe Senn Guerrero100% (2)
- Trading Floors WSДокумент86 страницTrading Floors WSAlok Singh100% (3)
- Dharnish ReportДокумент13 страницDharnish Reportdarshan75% (4)
- Referat Type 2 DMДокумент9 страницReferat Type 2 DMAyu Abharina PratiwiОценок пока нет
- Prediction of Type 2 Diabetes: A Natural History PerspectiveДокумент9 страницPrediction of Type 2 Diabetes: A Natural History Perspectiveandree_zz4890Оценок пока нет
- Pathogenesis of Type 2 Diabetes MellitusДокумент44 страницыPathogenesis of Type 2 Diabetes MellitusAsmat BurhanОценок пока нет
- Diabetes 1Документ22 страницыDiabetes 1aparna shamaОценок пока нет
- Case 2Документ23 страницыCase 2EJ CorpusОценок пока нет
- Pathogenesis of Type 2 Diabetes Mellitus - UpToDateДокумент26 страницPathogenesis of Type 2 Diabetes Mellitus - UpToDateMelina AranaОценок пока нет
- Type 2 Diabetes MellitusДокумент24 страницыType 2 Diabetes Mellitusdr. M.F. Romdhoni100% (1)
- Use of Acarbose Medan April 2010Документ14 страницUse of Acarbose Medan April 2010Ibnu WPОценок пока нет
- Molecular Basis of Type 2 DiabetesДокумент22 страницыMolecular Basis of Type 2 DiabetespimpellerОценок пока нет
- LEADING ARTICLE Insulin Resistance As A Predictor of Worsening of Glucose Tolerance in Type 2 DMДокумент6 страницLEADING ARTICLE Insulin Resistance As A Predictor of Worsening of Glucose Tolerance in Type 2 DMEvaPuspitaSariОценок пока нет
- Type 1 Diabetes Mellitus (Type 1 DM) : 1. Describe Patof Insulin PD DMДокумент5 страницType 1 Diabetes Mellitus (Type 1 DM) : 1. Describe Patof Insulin PD DMTheddyon BhenlieОценок пока нет
- Metabolic Changes in Diabetes: R. D. G. Leslie LondonДокумент4 страницыMetabolic Changes in Diabetes: R. D. G. Leslie LondonManuОценок пока нет
- Diabetes IIДокумент3 страницыDiabetes IIbangboomboomОценок пока нет
- Pathogenesis of Type 2 Diabetes Mellitus - UpToDateДокумент38 страницPathogenesis of Type 2 Diabetes Mellitus - UpToDatealinetibes1Оценок пока нет
- 1 Octeto de DefronzoДокумент23 страницы1 Octeto de DefronzoLesli Rodriguez50% (2)
- Pathogenesis and Pathophysiology of Diabetes MellitusДокумент4 страницыPathogenesis and Pathophysiology of Diabetes MellitusIka HabelОценок пока нет
- Review Article: Glucocorticoids and Type 2 Diabetes: From Physiology To PathologyДокумент10 страницReview Article: Glucocorticoids and Type 2 Diabetes: From Physiology To PathologyRengganis PutriОценок пока нет
- Clinical Review 102 Type 2 Diabetes Mellitus: Update On Diagnosis, Pathophysiology, and TreatmentДокумент7 страницClinical Review 102 Type 2 Diabetes Mellitus: Update On Diagnosis, Pathophysiology, and TreatmentWyn AgustinОценок пока нет
- Supplementary Information To Chapter 24: Review: Diabetes MellitusДокумент11 страницSupplementary Information To Chapter 24: Review: Diabetes MellitusAaron JoseОценок пока нет
- Costa Rica GlucoseДокумент91 страницаCosta Rica GlucoseAnthony HarderОценок пока нет
- Articulo Tacticas de Insulina en D2Документ30 страницArticulo Tacticas de Insulina en D2AlderkjОценок пока нет
- Diabetes Mellitus - Type 2 DiabetesДокумент11 страницDiabetes Mellitus - Type 2 DiabetesHafiz IbrahimОценок пока нет
- Livro Robbins PathologyДокумент18 страницLivro Robbins Pathologyernestooliveira50% (2)
- From The Triumvirate To The Ominous Octet: A New Paradigm For The Treatment of Type 2 Diabetes MellitusДокумент26 страницFrom The Triumvirate To The Ominous Octet: A New Paradigm For The Treatment of Type 2 Diabetes MellituselftotalОценок пока нет
- Trerapi Insulin Siip 2Документ10 страницTrerapi Insulin Siip 2Indra YudaОценок пока нет
- Diabetes Mellitus 1Документ16 страницDiabetes Mellitus 1Ajet AsaniОценок пока нет
- Glucose, Part1Документ33 страницыGlucose, Part1SarahОценок пока нет
- Resolving The Paradox of Hepatic Insulin ResistanceДокумент10 страницResolving The Paradox of Hepatic Insulin ResistanceMauro Rojas ZúñigaОценок пока нет
- Pancreatic Hormones and The Treatment of Diabetes MellitusДокумент46 страницPancreatic Hormones and The Treatment of Diabetes MellitusasmaОценок пока нет
- Etiopathogenesis of Type 2 DiabetesДокумент50 страницEtiopathogenesis of Type 2 Diabetesakash kondapalliОценок пока нет
- Pathology Assignment G 4Документ12 страницPathology Assignment G 4Hailat GОценок пока нет
- 二型糖尿病胰岛素分泌功能障碍 代谢异常的作用英文Документ12 страниц二型糖尿病胰岛素分泌功能障碍 代谢异常的作用英文慧吉Оценок пока нет
- Diabetes Diabetes Diabetes: ClassificationДокумент10 страницDiabetes Diabetes Diabetes: ClassificationAjay Pal NattОценок пока нет
- Insulin Resistance.:) DocxДокумент2 страницыInsulin Resistance.:) DocxHerbert Shirov Tendido SecurataОценок пока нет
- GI and Reproductive HormoneДокумент74 страницыGI and Reproductive Hormonepranutan739Оценок пока нет
- Targeting Postprandial HyperglycaemiaДокумент9 страницTargeting Postprandial HyperglycaemiaIbnu WPОценок пока нет
- Diabetes MellitusДокумент19 страницDiabetes MellitusHaleelu Abdul JaleelОценок пока нет
- Pharmacological Management of Type 2 Diabetes Mellitus: Rationale For Rational Use of InsulinДокумент9 страницPharmacological Management of Type 2 Diabetes Mellitus: Rationale For Rational Use of InsulinAditya Rachman Van Der ArjunaqueeОценок пока нет
- DM Report1Документ16 страницDM Report1Wendy EscalanteОценок пока нет
- Pathophysiology ScribdДокумент8 страницPathophysiology ScribdTamil VillardoОценок пока нет
- Hyperglycemia in Critical Illness: A ReviewДокумент11 страницHyperglycemia in Critical Illness: A ReviewSreejith ViswanathanОценок пока нет
- Ally Omary Mwambela MD2Документ10 страницAlly Omary Mwambela MD2Ally OmaryОценок пока нет
- Diagnosis Inggris PDFДокумент10 страницDiagnosis Inggris PDFMuhammad AbiyasaОценок пока нет
- Managemen Pasien Diabetes Mellitus Di Prosthodonsia: Agustin Wulan Suci DДокумент6 страницManagemen Pasien Diabetes Mellitus Di Prosthodonsia: Agustin Wulan Suci DYULYA DWI KARTIKASARIОценок пока нет
- Agustin Wulan PDFДокумент6 страницAgustin Wulan PDFCapaya AntrОценок пока нет
- Managemen Pasien Diabetes Mellitus Di Prosthodonsia: Agustin Wulan Suci DДокумент6 страницManagemen Pasien Diabetes Mellitus Di Prosthodonsia: Agustin Wulan Suci DYULYA DWI KARTIKASARIОценок пока нет
- Diabetes MellitusДокумент26 страницDiabetes Mellitusstrangefruit2483Оценок пока нет
- Dibetes FinalДокумент50 страницDibetes FinalPiyusha SharmaОценок пока нет
- Diabetes Millitus PDFДокумент41 страницаDiabetes Millitus PDFAbdullah BhattiОценок пока нет
- Comprehensive TreatmДокумент13 страницComprehensive TreatmRuki HartawanОценок пока нет
- Bab 2 OkДокумент28 страницBab 2 OknafitrawindriОценок пока нет
- Aims and ObjectivesДокумент13 страницAims and Objectivesmamun183Оценок пока нет
- Hypoglycemia and Hyperglycemia GM Eng 2022Документ3 страницыHypoglycemia and Hyperglycemia GM Eng 2022kabulkabulovich5Оценок пока нет
- Patho DMДокумент2 страницыPatho DMJohn Carlo SamsonОценок пока нет
- Nursing Care Plans For Diabetes MellitusДокумент12 страницNursing Care Plans For Diabetes MellitusPuteri AzmanОценок пока нет
- International Textbook of Diabetes MellitusОт EverandInternational Textbook of Diabetes MellitusR. A. DeFronzoОценок пока нет
- Consent For MTP PDFДокумент4 страницыConsent For MTP PDFMajid SheikhОценок пока нет
- Introduction of BiologyДокумент28 страницIntroduction of BiologyAlfin DestaОценок пока нет
- Restitution of Conjugal RightsДокумент3 страницыRestitution of Conjugal Rightsvalerian fernandesОценок пока нет
- N4 Fortran Codes For Computing The Space-Time Correlations of Turbulent Flow in A ChannelДокумент47 страницN4 Fortran Codes For Computing The Space-Time Correlations of Turbulent Flow in A Channelabhi71127112Оценок пока нет
- Trends in Computer-Based Second Language Assessment Jamieson 2005Документ15 страницTrends in Computer-Based Second Language Assessment Jamieson 2005Oana CarciuОценок пока нет
- M 1.2 RMДокумент16 страницM 1.2 RMk thejeshОценок пока нет
- Comparative and Superlative AdjectivesДокумент11 страницComparative and Superlative AdjectivesUri Leandro MuñozОценок пока нет
- Home DepotДокумент13 страницHome DepotTyfanie PetersenОценок пока нет
- Headache PAINДокумент1 страницаHeadache PAINOmarОценок пока нет
- The World of The GerДокумент302 страницыThe World of The GerMystic Master0% (1)
- Introduction To Qualitative ResearchДокумент19 страницIntroduction To Qualitative ResearchAnonymous LToOBqDОценок пока нет
- Picaresque Novel B. A. Part 1 EnglishДокумент3 страницыPicaresque Novel B. A. Part 1 EnglishIshan KashyapОценок пока нет
- Sonnet 39 ArticleДокумент2 страницыSonnet 39 ArticlelalyitaОценок пока нет
- Absolute Community of Property vs. Conjugal Partnership of GainsДокумент7 страницAbsolute Community of Property vs. Conjugal Partnership of GainsJill LeaОценок пока нет
- Discoid Lupus Erythematosus - Background, Etiology, EpidemiologyДокумент8 страницDiscoid Lupus Erythematosus - Background, Etiology, EpidemiologyJair MathewsОценок пока нет
- MKT202 Ga Su23Документ4 страницыMKT202 Ga Su23Như Nguyễn QuỳnhОценок пока нет
- CS302 - Lab Manual - Week No PDFДокумент8 страницCS302 - Lab Manual - Week No PDFattiqueОценок пока нет
- Film Viewing RomeroДокумент3 страницыFilm Viewing RomeroJenesis MuescoОценок пока нет
- Perceived Impact of Community Policing On Crime Prevention and Public Safety in Ozamiz CityДокумент7 страницPerceived Impact of Community Policing On Crime Prevention and Public Safety in Ozamiz Cityjabezgaming02Оценок пока нет
- IHL 1 BALLB ProjectДокумент16 страницIHL 1 BALLB Projectabcde fghikjОценок пока нет
- Reconceptualising Smart CitiesДокумент80 страницReconceptualising Smart CitiesDevang Parekh100% (1)
- Reading Exercise 2Документ2 страницыReading Exercise 2Park Hanna100% (1)
- E-Tech DLL Blank - Lesson 2-Nov 20-23Документ3 страницыE-Tech DLL Blank - Lesson 2-Nov 20-23Julie Ann SuarezОценок пока нет
- History of English Culture and Literature MidДокумент4 страницыHistory of English Culture and Literature Midfirdasalsa59Оценок пока нет
- FIDP Business Ethics and Social Responsibility PDFДокумент7 страницFIDP Business Ethics and Social Responsibility PDFRachell Mae Bondoc 1Оценок пока нет
- Subordinating Clause - Kelompok 7Документ6 страницSubordinating Clause - Kelompok 7Jon CamОценок пока нет
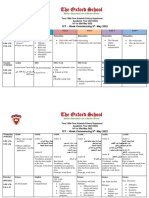
- Term 3 Mid-Term Assessment ScheduleДокумент9 страницTerm 3 Mid-Term Assessment ScheduleRabia MoeedОценок пока нет
- GR 148311-2005-In The Matter of The Adoption of StephanieДокумент8 страницGR 148311-2005-In The Matter of The Adoption of StephanieBogart CalderonОценок пока нет