Академический Документы
Профессиональный Документы
Культура Документы
N121 Antidiabetics
Загружено:
forminskoИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
N121 Antidiabetics
Загружено:
forminskoАвторское право:
Доступные форматы
ANTIDIABETICS Diabetes Mellitus Chronic disease of deficient glucose metabolism Insufficient insulin secretion from beta cells Impaired
red insulin use Major Symptoms: (3 Ps) o Polyuria increased urination o Polydipsia increased thirst o Polyphagia increased hunger Types: o Type I Diabetes (insulin-dependent DM) o Type II (non-insulin-dependent DM) Insulin Resistance Body tissues do not respond to the action of insulin o Insulin receptors are unresponsive o Insulin receptors are deficient in numbers INSULIN Is released from the beta cells of the islets of Langerhans in the pancreas Insulin release responds to an increase in blood glucose Function: o Promotes uptake of glucose, amino acids, and fatty acids o Converts to glycogen for future glucose needed in liver and muscle Actions: o Promotes use of glucose by body cells, stores glucose as glycogen in muscle cells Uses: o To reduce blood glucose Interactions: o Increased Hypoglycemia when mixed with: aspirin, oral anticoagulants, alcohol, oral hypoglycemic, BBs, TCAs, MAOIs, and tetracyclines o Decreased Hypoglycemia when mixed with thiazides, glucocorticoids, oral contraceptives, thyroid drugs, and smoking Side Effects: o Hypoglycemia (Low Blood Sugar) Wet Symptoms Headache, dizziness, confusion, slurred speech Nervousness, anxiety, agitation Tremors, uncoordination, sweating, tachycardia, seizures o Hyperglycemia (High Blood Sugar) Dry Symptoms Extreme thirst, dry mucous membranes Poor skin turgor, polyuria, fruity breath Fatigue, tachycardia, Kussmaul respirations o Lipodystrophy o Somogyi Effect o Dawn Phenomenon o Insulin Shock o Diabetic Ketoacidosis (DKA) Insulins: Manage hyperglycemia by promoting cellular glucose uptake and metabolism Vary by peak, onset, and duration of action Recombinant DNA (human) is now the standard source (but pork sources are still available) Type I Diabetes MANDATORY Type II Diabetes MAY BE NEEDED
Administration of Insulin Regular insulin may be used alone or in combinations with longer acting insulin such as NPH Given in the AM before breakfast, and several times a day All insulin may be given subQ 45-90 degree angle ONLY Regular Insulin may be given IV (usually only happens in the ICU or ER) Antidiabetic Agents Types of Insulin o Rapid Acting (Humalog) o Short Acting (Humulin R, Novolin R) o Intermediate Acting (Humulin N, Novolin N) o Long Acting (Ultralente) o Very Long Acting (Lantus) o Combination/Mixed (Humulin 70/30), (Novolin 70/30), (Humulin 50/50)
CATEGORIES OF INSULIN
Time Course RAPID ACTING Agent Lispro (Hulalog) Aspart (Novolog) SHORT ACTING INTERMEDIATE ACTING LONG ACTING (UL) VERY LONG ACTING (VLA) Regular (CZI) (Humulin R, Novolin R) NPH or Lente (Humulin N, or Novolin N) Ultra-lente (UL) Lantus (Glargine) Levemir (Detemir) NPH/reg 70/30 NPH/reg 50/50 NPH/reg 75/25 Onset 5-15 min 5-15 min 30 min Peak 30-90 min 1-3 hours 2-4 hours Duration 2-4 hours 3-5 hours 6-8 hours Indications RAPID REDUCTIONS of BLOOD GLUCOSE Usually administered 20-30 min ac (Before Meals) Usually taken after food
1-2 hours
6-12 hours
18-24 hours
6-8 hours 1 hour
12-16 hours No Peak
20-30 hours 24 hours Used primarily to control fasting blood glucose levels
1-2 hours 30 min 30 min 5-15 min
6-8 hours 4-8 hours 4-8 hours 30 min to 6 hours
12-24 hours 22-24 hours 24 hours 20-24 hours Prevents HYPOglycemia; Controls HYPERglycemia
COMBINATION THERAPY (Pre-Mixed)
Combination Insulins Types: o Humulin 70/30, Novolin 70/30 o Humulin 50/50 o Humalog Mix 75/25 Forms: o Vials o Pre-filled disposable pens Regular Insulin o Can be mixed with protamine or zinc insulin in the same syringe; alters absorption rate
Calculating the Unit Amount for Premixed Insulin (HOW TO TEACH THE PATIENT) The labeled numbers on the insulin vials (70/30) contain the percentage. The first # will always represent NPH, the second # will always represent regular insulin o Ex 70/30 = 70 % NPH, 30% Regular To find out how much of each agent is in the percentage you take the ordered # of units to be administered and multiply it by the percentage of each number. o Ex The physician orders 30 units of 70/30 NPH 30 x 0.7 = 21 units of NPH 30 x 0.3 = 9 units of regular 21 + 9 = 30 units TOTAL INSULIN ADMINISTRATION Nursing Interventions: o Monitor VS and blood glucose levels o Instruct client to report hypoglycemia and hyperglycemia o Encourage compliance with diet, insulin, and exercise o Advice client to wear medic-alert bracelet o Teach client how to check their blood glucose o Teach client how to administer insulin Sliding-Scale Insulin Coverage o Adjusted doses dependent on individual blood glucose o Usually done before eating and before bedtime o Usually uses rapid or short acting insulin Methods of Insulin Administration o Insulin Pumps Types: Implantable (internal) Portable (External) e.g. CSII ONLY regular insulin is used Advantages/ Helps to: Decrease the risk of hypoglycemic reaction Maintain glucose (glycemic) control Lessen long-term diabetic complications Has been shown to benefit Type I DM o Insulin Pen Injectors Types: Pre-filled Reusable Advantages: Increased compliance with insulin regimen Convenience Portability (e.g. can be used at work, or while traveling) Less injection pain Disadvantages: Expensive o Insulin Jet Injectors Shoots insulin without a needle directly through the skin into the fatty tissue May cause bruising, stinging, pain & burning Not indicated for children or older adults VERY EXPENSIVE o Oral inhaled insulin Exubera Available in 1 or 3mg dry powder blister packets. Insert into a handheld oral inhaler for administration. 1mg delivers approximately 3mg of insulin 3mg delivers approximately 8mg of insulin Indicated for Type I or Type II DM Contraindicated for COPD pts and those who have smoked within last 6 months
exenatide (Byetta) o Incretin mimetic Injectable (comes in a pre-filled pen injector) Action: improves beta cell responsiveness and enhances insulin secretion in proper amounts Prevents the liver from making excess glucose when not needed Delays gastric emptying Reduces appetite pramlinitide (Symlin) o Injectable o Suppresses glucagon secretion o Delays gastric emptying o Reduces appetite Incretin Modifier o sitagliptin (Januvia) o Use: Treats Type II DM (ONLY) o Action: Increases insulin secretion Decreases glucagon secretion to reduce glucose production o Tablet Form: Sitagliptin, metformin 50/500mg (Janumet) sitagliptin 50mg/metformin 500 mg
PATIENT TEACHING How to administer accurately Diet modifications Sick days Exercise Testing for blood glucose Storage of insulin Disposal of used needles and syringes Teach Insulin Facts o S/S of hypoglycemia & hyperglycemia o Testing o Nutrition o SC/SQ sites o Insulin administration o Drug interactions General Teaching o Instruct client to immediately report symptoms of hypoglycemic (insulin) reaction: headache, nervousness, sweating, tremors, rapid pulse; and symptoms of a hyperglycemic reaction (diabetic acidosis): thirst, increased urine output, sweet fruity breath odor. o Advise client that hypoglycemic reactions are more likely to occur during the peak action time. Most diabetics know whether they are having a hypoglycemic reaction, but some have a higher tolerance to low blood glucose and can have a severe hypoglycemic reaction without realizing it. o Explain that orange juice, sugar-containing drinks, and hard candy may be used when a hypoglycemic reaction begins. o Teach family members to administer glucagon by injection if client has a hypoglycemic reaction and cannot drink sugar-containing fluid. o Inform client that certain herbs may interact with insulin and certain oral anti-diabetic drugs. A hypo- or hyperglycemic effect might occur. o Instruct the client about the necessity for compliance with the prescribed insulin therapy and diet. HbA 1C provides the most accurate picture of optimal diabetic control. o Advise the client to carry a MedicAlert card, tag, or bracelet indicating the health problem and insulin dosage.
Self-administration teaching o Direct client how to check blood glucose with a glucometer. o Instruct client in the care of insulin container and syringes. Inform client taking NPH insulin with regular insulin that the regular insulin (CLEAR) should be drawn up before the NPH insulin (CLOUDY). Diet Teaching o Advise client taking insulin to eat the prescribed diet on a consistent schedule. Diet information may be obtained from the American Diabetes Association or a nutritionist.
INSULIN STORAGE Storage of insulin o Keep in refrigerator o Remove from refrigerator 30 minutes before injection o Avoid storing insulin in direct sunlight or at high temperatures o DO NOT: Place in the freezer Place in direct sunlight or high temperature o Unopened Insulin Vials Refrigeration until needed o Open Insulin Vials Stored at Room Temp last 30 days or 1 month Its less irritating to tissues when injected at room temp Stored in Refrigerator last 3 months (BUT FOR TESTING 1 MONTH IS THE LIMIT!!!) Lose their strength after approx. 3 months HERBAL ALERT ANTI-DIABETIC AGENTS HYPOGLYCMIC EFFECT o Chromium o Black Cohosh o Garlic, Bitter Mellon, Aloe & Gymnema o Ginseng o Bilberry HYPERGLYCEMIC EFFECT o Cocoa, rosemary, stinging nettle ORAL ANTIDIABETICS Criteria for Oral Antidiabetic Therapy Onset of DM at age 40 or older DX of diabetes for less than 5 years Normal weight or overweight Fasting BG equal or less than 200 mg/dL Less than 40 units of insulin required per day Normal renal & hepatic function 5 Classes of OHAs (Oral Hypoglycemic Agents) Sulfonylureas (1950) Biguanides (1995) a-glucosidase inhibitors (1995) Glitazones (1997) Meglitinides (1998)
Sulfonylureas (1950) Mechanism of Action: o Stimulates release of insulin from pancreatic islets o Decreases glycogenolysis (breakdown of glycogen) o Decreases gluconeogenesis (synthesis of glucose from molecules that arent carbs, [amino & fatty acids]) o Enhances cellular sensitivity to insulin Examples: o glyburide (Micronase, DiaBeta) o glipizide (Glucotrol) (Glucotrol XL) Target Organ PANCREAS ACTION: Stimulates beta cells to secrete insulin, alters sensitivity of peripheral insulin receptors Lowers HbA1c by 1-2% Used to control hyperglycemia in Type II DM TAKEN w/ food or 30 min before meals CAUTION: Liver or kidney dysfunction, elderly, malnourished, adrenal or pituitary insufficiency INTERACTIONS: Alcohol may cause disulfiram-like reaction Hypoglycemia and anti-coagulants, cimetidine, anticonvulsants, aspirin, NSAIDS, sulfonamides Increases action thiazide diuretics, barbiturates, phenothiazines Decreases action thyroid drugs SIDE EFFECTS: Drowsiness, headache, confusion, visual disturbances Anxiety, hunger, hypoglycemia Tachycardia Seizures, respiratory depression, coma Biguanides (1995) Mechanism of Action: o Decreases the rate of hepatic glucose production o Augments glucose uptake by muscle tissues Examples: o metformin (Glucophage) Target Organ LIVER ACTION: Increases binding of insulin to receptors Improves tissue sensitivity to insulin Increases glucose transport into skeletal muscles & fatty tissues Control hyperglycemia in Type II DM Lowers HbA1c by 1-2% TAKEN with meals INTERACTIONS: Hypoglycemia potentiated by captopril, nifedipine, procainamide, quinidine, digoxin, furosemide, cimetidine, ranitidine, azole antifungals, vancomycin Iodiniated contrast dyes may lead to lactic acidosis or acute kidney failure SIDE EFFECTS: Dizziness, fatigue, headache, agitation, metallic taste, GI distress, lactic acidosis CONTRAINDICATIONS: DKA Alcoholism, binge drinking Kidney Disease Liver Disease CHF o Glucovance (glyburide + metformin) Used for managing Type II DM CONTRAINDICATIONS: Clients with renal insufficiency because of risk of developing lactic acidosis Teach patient to avoid ETOH!!!
Meglitinides (1998) Mechanism of Action: o Stimulates a rapid and short-lived release of insulin from the pancreas Examples: o repaglinide (Prandin) o nateglide (Starlix) Target Organ PANCREAS ACTION: Stimulates release of insulin from pancreatic islets Increases first phase insulin release, glucose driven, lowers after-meal glucose Lowers HbA1c by 0.5-0.7% TAKEN before each of the three meals Glitazones (Thiazolidinediones) (1997) Mechanism of Action: o Decreases peripheral insulin resistance in skeletal muscle without stimulating insulin secretion Examples: o pioglitazone (Actos) o rosiglitazone (Avandia) Target Organ MUSCLE ACTION: Affects insulin receptors by enhancing insulin sensitivity of cells Lowers HbA1c by 1-1.5% TAKEN with or without food Alpha-Glucosidase Inhibitors (1995) Mechanism of Action: o Works on the brush border of the small intestine to slow the breakdown of disaccharides and polysaccharides into monosaccharides; delays subsequent absorption of glucose Examples: o acarbose (Precose) o miglitol (Glyset) TARGET ORGAN INTESTINES ACTION: Inhibits absorption of sugars from GI tract Inhibits upper GI enzymes Lowers HbA1c by 0.5-0.9% SIDE EFFECTS: Flatulence (so this drug has poor compliance) TAKEN with first bite of food NURSING INTERVENTIONS FOR OHAs Monitor VS, BG levels Administer w/ food to minimize GI distress Teach client to eat prescribed diet on schedule Teach client to recognize symptoms of HYPERGLYCEMIA and HYPOGLYCEMIA Encourage drug compliance Advise client to wear MedicAlert tag Warn client to avoid ETOH Teach client the treatment for HYPOGLYCEMIA and HYPERGLYCEMIA Glucagon (Glucagen) Hyperglycemic hormone secreted by the islets of Langerhans in the pancreas ACTION stimulates breakdown of stored glycogen to glucose in liver Used for insulin-induced hypoglycemia Stimulates glycogenolysis (breakdown of glycogen) in the peripheral tissues Stimulates synthesis of glucose Used for emergency treatment of severe hypoglycemia in unconscious clients of those unable to swallow, and in clients receiving insulin shock therapy Client usually responds/ awakens within 5 to 20 minutes of administration
diazoxide (Proglycem) Oral medicine Chemically r/t thiazide diuretics ACTION increases BS by: o Inhibiting insulin release from the beta cells o Stimulates release of epinephrine (Adrenaline) from the adrenal medulla Has a long T Onset of Action: 1 hour Excreted unchanged in the urine Questions: 1. Mr. Gates receives NPH insulin at 7am. When is he most likely to develop a hypoglycemic reaction? a. mid morning b. mid afternoon c. midnight d. next morning 2. What time frame would be most appropriate for administering sliding scale Lispro insulin? a. Within 30 minutes of consuming breakfast b. When the breakfast try is served and ready to eat c. Within 1 hour of obtaining blood glucose measurement d. Within 15 minutes of obtaining blood glucose measurement 3. A client is prescribed metformin (Glucophage). Which of the following is a side effect/adverse effect common to metformin? a. Seizures b. Constipation c. Bitter or metallic taste d. Polyuria and polydipsia
Insulin Peak/ Reaction Times
Hum/Nov Regular NPH Lente Ultralente Lantus 0 4 8 12 16 20 24
Hours After Insulin Injection
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Gestational Diabetes Brochure ENGДокумент2 страницыGestational Diabetes Brochure ENGP Zamora100% (2)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- HAAD ReviewerДокумент35 страницHAAD ReviewerSydRey92% (24)
- g10 Healthsci CmapДокумент6 страницg10 Healthsci Cmapapi-263590842Оценок пока нет
- Diabetes MCQ 011215 PDFДокумент6 страницDiabetes MCQ 011215 PDFRawda Ibrahim100% (2)
- Health Unit Plan Disease UnitДокумент68 страницHealth Unit Plan Disease UnitKelly0% (1)
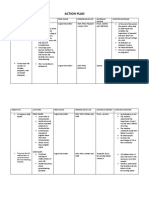
- Action PlanДокумент4 страницыAction PlanJosette Mae Atanacio67% (3)
- Problem Set 1Документ4 страницыProblem Set 1annon55555Оценок пока нет
- Nursing Comps Study GuideДокумент15 страницNursing Comps Study GuideforminskoОценок пока нет
- Common Drugs ChartДокумент15 страницCommon Drugs Chartforminsko100% (1)
- BRM NotesДокумент4 страницыBRM NotesforminskoОценок пока нет
- HypertensionДокумент2 страницыHypertensionforminskoОценок пока нет
- Psychotic DisordersOutlineДокумент6 страницPsychotic DisordersOutlineforminskoОценок пока нет
- Early Hemorrhagic Conditions 20 WeeksДокумент3 страницыEarly Hemorrhagic Conditions 20 WeeksforminskoОценок пока нет
- Shock ChartsДокумент2 страницыShock ChartsforminskoОценок пока нет
- Bulletin of Faculty of Pharmacy, Cairo University: Cynara Scolymus (Artichoke) and Its Efficacy in Management of ObesityДокумент6 страницBulletin of Faculty of Pharmacy, Cairo University: Cynara Scolymus (Artichoke) and Its Efficacy in Management of ObesityArsanОценок пока нет
- The Peptide-Hormone Glucagon-Like Peptide-1 Activates cAMP and Inhibits Growth of Breast Cancer CellsДокумент13 страницThe Peptide-Hormone Glucagon-Like Peptide-1 Activates cAMP and Inhibits Growth of Breast Cancer CellsRidha Surya NugrahaОценок пока нет
- Treatment Strategies in PCOS Patients: OnlineДокумент8 страницTreatment Strategies in PCOS Patients: Onlinenurul hidayahОценок пока нет
- Annotated BibliographyДокумент6 страницAnnotated Bibliographyapi-483637877Оценок пока нет
- Diabetes Melitus: Dr. Ihsanil Husna, SPPDДокумент67 страницDiabetes Melitus: Dr. Ihsanil Husna, SPPDnathan timothyОценок пока нет
- SaudiJOralSci313-2968904 081449Документ9 страницSaudiJOralSci313-2968904 081449EnochDomprehОценок пока нет
- 30 - Toronto Notes 2011 - Common Unit Conversions - Commonly Measured Laboratory Values - Abbreviations - IndexДокумент28 страниц30 - Toronto Notes 2011 - Common Unit Conversions - Commonly Measured Laboratory Values - Abbreviations - IndexRazrin RazakОценок пока нет
- Periodontal MedicineДокумент145 страницPeriodontal MedicineAkash Yss Boddeda67% (3)
- 1608760278Документ384 страницы1608760278Petit Panda100% (3)
- Structured Health Teaching On Proper Nutrition of Common ConditionДокумент11 страницStructured Health Teaching On Proper Nutrition of Common ConditionFry FryОценок пока нет
- Farmakodinamik Obat Anti DiabetesДокумент24 страницыFarmakodinamik Obat Anti DiabetesAsma Somadayo100% (1)
- Diabettes Mellitus and Cognitive ImpairmentsДокумент12 страницDiabettes Mellitus and Cognitive ImpairmentsPutri YunandaОценок пока нет
- InTech-Diabetic Foot and GangreneДокумент25 страницInTech-Diabetic Foot and GangrenePutu Reza Sandhya PratamaОценок пока нет
- Agent Orange ReviewДокумент8 страницAgent Orange Reviewjim912Оценок пока нет
- The GATE Notes: A Graphic Approach To Epidemiology: PrefaceДокумент48 страницThe GATE Notes: A Graphic Approach To Epidemiology: PrefaceSerafim RahadiОценок пока нет
- National Guidelines For GDMДокумент24 страницыNational Guidelines For GDMVijaya LakshmiОценок пока нет
- Interpretation: S03 - FPSC DILSHAD COLONY (C004263143) J-50 Dilshad Colony, DelhiДокумент6 страницInterpretation: S03 - FPSC DILSHAD COLONY (C004263143) J-50 Dilshad Colony, DelhiAll VIDEOS TechОценок пока нет
- IV Insulin - FinalДокумент18 страницIV Insulin - Finaldamondouglas100% (2)
- A-PULMO - (LEE-TAN-CONSTANTINO) - Prelims (TD) B - Pulmo - (Lee-Tan-Constantino) - PrelimsДокумент17 страницA-PULMO - (LEE-TAN-CONSTANTINO) - Prelims (TD) B - Pulmo - (Lee-Tan-Constantino) - PrelimsJohn Paulo CatacutanОценок пока нет
- Biocon AR2011Документ164 страницыBiocon AR2011ruchiwadhawancaОценок пока нет
- Diabetic Gastroparesis Principles and Current Trends in ManagementДокумент42 страницыDiabetic Gastroparesis Principles and Current Trends in ManagementErika AvilaОценок пока нет
- Screening of Antidiabetic Drugs: Presented ByДокумент35 страницScreening of Antidiabetic Drugs: Presented BysharonОценок пока нет
- 22 Little Known Dangers of Magnesium DeficiencyДокумент7 страниц22 Little Known Dangers of Magnesium DeficiencyDianne100% (4)
- EndopthalmitisДокумент106 страницEndopthalmitisGiselle EclarinoОценок пока нет