Академический Документы
Профессиональный Документы
Культура Документы
Informed Consent 1
Загружено:
Edah HumaidahИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Informed Consent 1
Загружено:
Edah HumaidahАвторское право:
Доступные форматы
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 1 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent Prepared by: Medical Staff Administrative Committee
Authorized by:
Original Signed by the Medical Director, University Hospitals Executive Director, University Hospital Executive Director, University Hospital East
POLICY The Ohio State University Hospitals respect the patient's right to be informed of surgical or medical procedures which are to be rendered and the patient's right to accept or refuse such surgical or medical procedure. Being consistent with quality patient care, informed consent must be obtained and documented pursuant to this policy before proceeding with surgical and medical procedures, except in emergency situations as defined below. This policy applies to all surgical and medical procedures that involve material risk to the patient, irrespective of their repetitive nature. Some items require informed consent by law or regulatory standard such as HIV testing and blood/blood product administration. A complete list of procedures requiring informed consent has been approved by the Medical Staff and is available on OneSource under the Clinical Care tab.
PROCEDURE
1.OBTAINING INFORMED CONSENT a. The attending physician performing or supervising the surgical or medical procedure, or his/her designee, shall be responsible for obtaining informed consent.
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 2 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent b. For obtaining informed consent, an attending physicians designee is defined as follows: i. A member of the Limited Staff (e.g., intern, resident or fellow) familiar with the specific procedure for which consent is being obtained; ii. A licensed independent practitioner (LIP) with hospital privileges to perform the specific procedure for which consent is being obtained. An LIP with order-writing authority may also get informed consent for HIV testing and blood/blood product administration; iii. Registered nurses permitted to place PICC lines as a part of their job duties are responsible for obtaining informed consent for that procedure after it is ordered by a physician or an LIP with order-writing authority. Registered nurses are not permitted to obtain informed consent for any other procedure or indication. c. The individual obtaining consent must be familiar with both the patient and the surgical or medical procedure for which informed consent is being obtained, and must be capable of accurately answering questions regarding the procedure and its associated risks, benefits and alternatives for that patient. d. Medical students may not obtain informed consent for any procedure or other indication. 2. MECHANISMS OF DOCUMENTING INFORMED CONSENT Informed consent must be documented by one of the following mechanisms: a. A completed Hospitals Informed Consent Form or other hospitalapproved Consent Form signed by the patient; b. A completed Informed Consent form supplied by the physician signed by the patient; c. A written Informed Consent note in the progress notes signed by the patient; d. A written Informed Consent form or progress note signed by the patients legal representative;
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 3 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent e. In urgent situations, informed consent may be received by phone from a patients legal representative if that representative is unable to come to the hospital and unable to sign a faxed consent form. Consent received by phone from a patients legal representative should be confirmed by a witness who also speaks to the legal representative. The details of the phone consent should be documented in the progress notes and should be signed by the person obtaining the consent and by the witness. 3. REQUIREMENTS FOR INFORMED CONSENT a. Consent must be obtained at a time when the patient is fully capable of understanding the procedure so that he/she can make an informed decision regarding consent. For example, informed consent should never be obtained after a patient has received medication for conscious sedation or anesthesia. For multi-stage procedures or when multiple tests requiring consent are contemplated to be done on the same day, informed consent for all parts of the procedure(s) should occur prior to the patient receiving any sedation. b. During the informed consent discussion, the following should be discussed with the patient: i. A description of the proposed procedure, including the anesthesia to be used if applicable; ii. The indications for the proposed procedure; iii. Material risks and benefits for the patient related to the procedure and anesthesia if applicable, including the likelihood of each, based on the available clinical evidence, as informed by the responsible practitioners clinical judgment. Material risks could include risks with a high degree of likelihood but a low degree of severity, as well as those with a very low degree of likelihood but high degree of severity; iv. Treatment alternatives, including the attendant material risks and benefits; v. The probable consequences of declining recommended or alternative therapies; vi. Who will conduct the surgical intervention and administer the anesthesia if applicable; vii. Whether physicians other than the attending physician, including but not limited to residents and fellows, will be performing significant tasks related to the surgery or procedure; viii. If students, residents and/or fellows will perform
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 4 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent significant parts of the surgery/procedure under the supervision of the physician performing the procedure or surgery, the informed consent discussion with the patient or the patients legal representative is encouraged to include the following: 1. That students, residents and/or fellows will perform portions of the procedure, based on their availability and level of competence; 2. That it will be decided at the time of the surgery/procedure which students, residents and/or fellows will participate and their manner or participation, and that this will depend on the availability of students, residents and/or fellows with the necessary competence; the knowledge the attending physician has of the students, residents and fellows skill set; and the patients condition; 3. Whether, based on the residents and/or fellows level of competence, the attending physician is reasonably expected not to be present in the same room for some or all of the tasks performed by residents and fellows.
ix. Whether qualified medical practitioners who are not
physicians (e.g., CRNAs, nurse practitioners, RN first assistants, physician assistants, etc.) will perform significant parts of the surgery or administer the anesthesia and if so, the types of tasks each type of practitioner will carry out. The types of tasks such practitioners will be performing will only be tasks within their scope of practice for which they have been granted privileges.
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 5 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent c. The patient should be given an opportunity to ask questions and to have them answered to the patients or their legal representatives satisfaction. d. Documentation of the informed consent must be completed prior to the procedure. Documentation according the details of Section 4 of this policy should be in the patients medical record as evidence that consent has been obtained. 4. DOCUMENTATION OF INFORMED CONSENT FOR PROCEDURES/SURGERIES a. Properly executed informed consent documentation for a surgery, procedure or other treatment requiring informed consent must contain at least the following: i. The name of the hospital where the procedure, surgery, or treatment is to take place; ii. The name of the patient or, when appropriate, the name of the patients legal representative; iii. The name, nature and purpose of the surgical or medical procedure; iv. A statement that the procedure, surgery or treatment, including the anticipated benefits, material risks and alternative therapies, was explained to the patient or the patients legal representative; v. Name(s) of the attending physician(s) performing or supervising the surgery, procedure, or treatment requiring informed consent. For PICC lines, the name of the RN performing the procedure will suffice; vi. Acknowledgement by the person giving consent that the procedure was explained to them, that they had an opportunity to ask questions, and that questions have been answered to the satisfaction of the patient or the patients legal representative; vii. The signature of the patient or his/her representative. The acquisition of both the patient's consent and the consent of his/her representative is acceptable; viii. Date and time the consent form was signed by the patient or the patients legal representative. b. Optional items may be included in the documentation for informed consent, including but not limited to: i. Name and signature of the practitioner who conducted the informed consent discussion with the patient;
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 6 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent ii. Date, time and signature of the person witnessing the patient or the patients legal representative signing the consent form; iii. Listing of the specific material risks of the procedure, surgery, or treatment that were discussed with the patient. 5. SPECIAL NON-PROCEDURAL CIRCUMSTANCES REQUIRING INFORMED CONSENT a. HIV Testing i. Informed consent for HIV testing is required by Ohio law except in certain circumstances described in OSU Hospitals Policy 3-11. ii. The hospital-approved HIV Informed Consent Form should be used when possible to gain informed consent for HIV testing. Alternatively, a note in the progress note section outlining the informed consent that is signed by the person obtaining consent and the patient will suffice. iii. A copy of the signed consent form should be placed in the patients chart. b. Blood and Blood Product Administration i. Informed consent is required prior to the initial transfusion of blood or any blood product. 1. For inpatients, subsequent administrations of the same blood and/or blood product(s) covered under the original consent during the same admission do not require additional informed consent unless there is a significant change in the risks, benefits or alternatives for the patient in receiving the transfusion. 2. For outpatients, informed consent for blood or blood product administration will have a maximum duration of 12 months. During that period, if there is a significant change in the risks, benefits or alternatives for the patient in receiving the transfusion, the consent process should be redone. 3. In the inpatient or outpatient setting, the patient or their legal representative may withdraw their consent for subsequent transfusions at any time after the initial informed consent is given. ii. Initial informed consent must be obtained by the attending physician or a designee as outlined in Section 1.b above.
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 7 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent iii. A hospital-approved, pre-printed blood and blood product informed consent form should be used when possible for consent for blood or blood product administration. Prior to an initial transfusion, this form must be completed and signed by the patient and the individual obtaining informed consent. Alternatively, a note in the progress note section outlining the informed consent that is signed by the person obtaining consent and the patient will suffice. iv. For both inpatients and outpatients, confirmation that a current, signed informed consent form is in the chart must be done by the nursing staff as a part of the patient identification process prior to the initial and any subsequent transfusions. c. Research, Clinical Trials, Investigational Drugs: Informed consent must be obtained and documented prior to enrolling any patient in a research project or clinical trial or prior to treatment with any investigational drugs as required by applicable University Institutional Review Board (IRB) and Office of Responsible Research Practices (ORRP) policies. d. Sterilization: Informed consent for sterilization procedures must be obtained using the hospital-approved consent form for sterilization or an equivalent form containing the required information. For Medicaid patients, the informed consent process for sterilization must be completed at least 30 days prior to the procedure. e. Transplant and Living Donor Patients i. For transplant patients, the informed consent process must inform the patient regarding, at a minimum, each of the following items: 1. The evaluation process; 2. The surgical procedure contemplated for the patient; 3. Alternative treatments; 4. Potential medical or psychological risks; 5. National and transplant center-specific outcomes for the transplant procedure that is contemplated for the patient from the most recent SRTR center-specific report including but not limited to: a. The transplant centers observed and expected 1year patient and graft survival rate; b. The national 1 year patient and graft survival
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 8 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent rate; c. Notification about all Medicare outcome requirements not being met by the transplant center; 6. Organ donor risk factors that could affect the success of the graft or the health of the patient, including but not limited to the donors history, condition or age of the organs being used; 7. The risk of the organ recipient to contract HIV or other infectious diseases if the disease cannot be detected in an infected donor;
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 9 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent 8. The recipients right to refuse transplantation; 9. The fact that if the recipients transplant is not performed in a Medicare-approved transplant center it could affect the transplant recipients ability to have his/her drugs paid for under Medicare Part B. ii. For living donors, the informed consent process for all prospective living donors must include, at a minimum, the following items: 1. All aspects of living donation including potential outcomes from living donation; 2. The fact that communication between the donor and the transplant center will remain confidential; 3. The evaluation process for living donation; 4. The surgical procedure, including post-operative treatment, contemplated for the patient; 5. The availability of alternative treatments for the transplant recipient; 6. The potential medical or psychosocial risks to the donor; 7. The national and transplant center-specific outcomes for recipients and the national and center-specific outcomes for living donors for the procedure contemplated for the patient; 8. The possibility that future health problems related to the donation may not be covered by the donors insurance and that the donors ability to obtain health, disability, or life insurance might be affected; 9. The donors right to opt out of donation at any time during the donation process;
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 10 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent 10. The fact that if a transplant is not provided in a Medicare-approved transplant center, it could affect the transplant recipients ability to have his/her drugs paid for under Medicare Part B. 6. HOSPITAL STAFF PARTICIPATION a. Responsibility for obtaining informed consent from the patient and the appropriate documentation of informed consent rests with the attending physician with the exception of PICC lines as noted above. The attending physician may delegate this responsibility only to the designees outlined in Section 1.b above. b. Hospital staff members (including all nurses and other employees) may participate in the informed consent process by witnessing the patient's, the patient's representative, or physician's signature regarding informed consent. c. If any staff member has actual knowledge that a patient has not given informed consent or desires to cancel a prior consent, they should report that fact first to the attending physician or his designee, and then to their supervisor. No applicable procedure shall commence without evidence of informed consent. 7. MEDICAL EMERGENCIES a. Informed consent is not required in emergency situations. Consent in an emergency will be implied as allowed by law. This rule applies only in cases where a physician must act immediately and the patient is incapable of expressing such consent. b. To constitute an "emergency," the threat must be immediate to protect the life, limb, or health of the patient. c. The physician must show the need for proceeding without informed consent by documenting in the medical record the reasonable and diligent efforts as time allows to acquire consent from the next of kin or legal representative; and the immediacy and magnitude of the threat to the patient if the medical or surgical procedure were not immediately done.
Number: 03-27 First Effective: March 15, 1993 Last Revised: August 10, 2007 Page: 11 of 11
UNIVERSITY HOSPITALS POLICY AND PROCEDURE MANUAL
Title: Informed Consent 8. INCAPACITY. For guidance regarding obtaining informed consent for patients that lack capacity, including minors, please see Policy 3-18, Consent for Inpatient and Emergency Department Treatment. 9. REFUSAL OF CARE a. A competent adult patient or the patient's representative may refuse or may voluntarily withdraw informed consent. Such a request should be honored. b. In such a case, the physician should write in the medical record a statement of the circumstances under which the refusal or withdrawal occurred. The physician is to explain the consequences of refusal to the patient. c. If a patient lacks capacity and the next of kin refuses treatment essential to the patient's life or health, any health care provider may consult Hospital Legal Services. RELATED HOSPITAL POLICIES AND PROCEDURES 03-24 Do-Not-Resuscitate Orders 03-18 Consent for Inpatient and Emergency Department Care and Treatment 03-11 Management of Human Immunodeficiency Virus Infection in the Healthcare Facility 03-26 Advance Directives RELATED CMS RULES AND REGULATIONS FROM THE FEDERAL REGISTER: 42CFR 482.24(c)(2)(v) Requirement for documentation of informed consent in the medical record 42CFR 482.51(b)(2) Requirements for documentation of informed consent prior to surgical procedures 42CFR 482.102 Conditions of participation related to patient and living donor rights for transplant centers
Вам также может понравиться
- ICU Construction EssentialsДокумент91 страницаICU Construction EssentialsShimmering MoonОценок пока нет
- Leadership & MGTДокумент128 страницLeadership & MGTmutegeki nathanОценок пока нет
- FR Dur I Ski'ta - S: SK Ti 25-f $kifiДокумент6 страницFR Dur I Ski'ta - S: SK Ti 25-f $kifijerayne50% (2)
- Missing Persons Policy SummaryДокумент16 страницMissing Persons Policy SummaryAgnieszka WaligóraОценок пока нет
- Ed Assessment Tool SampleДокумент28 страницEd Assessment Tool SampleAnonymous ibmeej9Оценок пока нет
- Healthcare Environmental Services A Complete Guide - 2020 EditionОт EverandHealthcare Environmental Services A Complete Guide - 2020 EditionОценок пока нет
- Administrative Policy for Hospital AdmissionsДокумент8 страницAdministrative Policy for Hospital AdmissionsHAMMYER ALROKHAMIОценок пока нет
- TRIAGE POLICIES JuvyДокумент6 страницTRIAGE POLICIES JuvyCuyapo Infirmary Lying-In HospitalОценок пока нет
- Emergency CodesДокумент23 страницыEmergency CodesJennifer B. GarciaОценок пока нет
- Hospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsОт EverandHospitalist Program Toolkit: A Comprehensive Guide to Implementation of Successful Hospitalist ProgramsОценок пока нет
- Toledo Code Blue PolicyДокумент4 страницыToledo Code Blue PolicySt SОценок пока нет
- Nursing Services Manual AIIMSДокумент91 страницаNursing Services Manual AIIMSpraveenjenaОценок пока нет
- 001 Admission APP MED 001Документ7 страниц001 Admission APP MED 001HAMMYER ALROKHAMIОценок пока нет
- Cardio & PulmoДокумент64 страницыCardio & PulmoAnonymous bgB7IhОценок пока нет
- Surgical Site Marking PolicyДокумент11 страницSurgical Site Marking PolicymiraОценок пока нет
- Blood Transfusions - TGH Policies & ProceduresДокумент4 страницыBlood Transfusions - TGH Policies & ProceduresMark Anthony FranciscoОценок пока нет
- JD Ward Clerk Job DescriptionДокумент2 страницыJD Ward Clerk Job DescriptionMD Luthfy LubisОценок пока нет
- Nursing Skill RevisionДокумент1 страницаNursing Skill RevisionMichelle TseОценок пока нет
- PACU Discharge CriteriaДокумент1 страницаPACU Discharge CriteriaTarquin Tomada100% (2)
- Scripps Hospital Patient Visitor Policy PDFДокумент2 страницыScripps Hospital Patient Visitor Policy PDFcode4saleОценок пока нет
- Nss 505 Medical Surgical Nursing Critical Care I Teacher - Co .KeДокумент171 страницаNss 505 Medical Surgical Nursing Critical Care I Teacher - Co .Kebirhanu Ayenew AnleyОценок пока нет
- Duties and Responsibilities of An RN: Lpns CnasДокумент4 страницыDuties and Responsibilities of An RN: Lpns CnasSPTDОценок пока нет
- IV Complications Signs, Prevention, TreatmentДокумент6 страницIV Complications Signs, Prevention, TreatmentMercicae AОценок пока нет
- Procedure Manual HospitalДокумент196 страницProcedure Manual HospitalMarian StrihaОценок пока нет
- Liabilities of HospitalsДокумент36 страницLiabilities of HospitalsMJ Carreon100% (1)
- Recovery Room NurseДокумент5 страницRecovery Room NurseChristin 'Kirei' AndoloОценок пока нет
- How To Move The Patient From The Bed To The Wheelchair How To Move The Patient From The Bed To The WheelchairДокумент9 страницHow To Move The Patient From The Bed To The Wheelchair How To Move The Patient From The Bed To The WheelchairAfniy ApriliaОценок пока нет
- Patient Safety Organization A Complete Guide - 2020 EditionОт EverandPatient Safety Organization A Complete Guide - 2020 EditionОценок пока нет
- Clinical Services Plan TTM SamoaДокумент69 страницClinical Services Plan TTM SamoajohnkornieОценок пока нет
- A&E Triage SystemДокумент5 страницA&E Triage SystemArnel AlmutiahОценок пока нет
- 2 Critical Care UnitДокумент59 страниц2 Critical Care UnitPALMA , JULIA A.Оценок пока нет
- Out Patient DepartmentДокумент5 страницOut Patient DepartmentShikhaОценок пока нет
- Western Australian Patient Identification Policy PDFДокумент14 страницWestern Australian Patient Identification Policy PDFpuspadiniaОценок пока нет
- CLCGP030 Theatre Operating List Session Scheduling PolicyДокумент19 страницCLCGP030 Theatre Operating List Session Scheduling PolicyJeffy PuruggananОценок пока нет
- Emergency Drugs (LEAD)Документ8 страницEmergency Drugs (LEAD)RayePrudenteОценок пока нет
- The COAT & Review Approach: How to recognise and manage unwell patientsОт EverandThe COAT & Review Approach: How to recognise and manage unwell patientsРейтинг: 5 из 5 звезд5/5 (1)
- IV Cannulation ChecklistДокумент2 страницыIV Cannulation ChecklistDo0odi AlharbiОценок пока нет
- Arero Primary Hospital Triage Protocol Nov 2022Документ4 страницыArero Primary Hospital Triage Protocol Nov 2022sami ketemaОценок пока нет
- TransitionДокумент13 страницTransitionDonna NituraОценок пока нет
- ISBAR Communication ToolДокумент16 страницISBAR Communication ToolTni JolieОценок пока нет
- Nurse Bob's MICU/CCU Survival Guide Critical Care Concepts General Nursing Requirements of The Intensive Care PatientДокумент7 страницNurse Bob's MICU/CCU Survival Guide Critical Care Concepts General Nursing Requirements of The Intensive Care Patientlil' princessОценок пока нет
- Critical Transport GuidelinesДокумент22 страницыCritical Transport GuidelinesFadil RamadhanОценок пока нет
- DR, OR, WardДокумент14 страницDR, OR, WardjanОценок пока нет
- Manual For EndosДокумент19 страницManual For EndosVarsha MalikОценок пока нет
- Oral Care in ICUДокумент8 страницOral Care in ICUYani Va-Rhy100% (1)
- Delivery InstrumentsДокумент1 страницаDelivery InstrumentsKristine Dianne San BuenaventuraОценок пока нет
- Acute Nutrition PolicyДокумент79 страницAcute Nutrition PolicyyohaneskoОценок пока нет
- Equipments in Icu: Mr. Amol Temkar Asso. Prof College of NursingДокумент46 страницEquipments in Icu: Mr. Amol Temkar Asso. Prof College of NursingAmol TemkarОценок пока нет
- Today Admissions Discharge FON Sem-1 2021Документ25 страницToday Admissions Discharge FON Sem-1 2021zakiralihussaini786Оценок пока нет
- Guide to Measuring Vital SignsДокумент32 страницыGuide to Measuring Vital SignsJacqueline de AsisОценок пока нет
- prehospital-EMS-COVID-19-recommendations - 4.4Документ19 страницprehospital-EMS-COVID-19-recommendations - 4.4MEONEОценок пока нет
- KPI Discussion Paper 3Документ22 страницыKPI Discussion Paper 3Manager HR Hijaz Hospital100% (1)
- Police Hospital PolicyДокумент3 страницыPolice Hospital PolicyThe Salt Lake TribuneОценок пока нет
- Clinical Guidelines For Management of HTNДокумент6 страницClinical Guidelines For Management of HTNChaturangaNSenerath100% (1)
- Transfer Using Gait Belt PDFДокумент2 страницыTransfer Using Gait Belt PDFJasonJejametОценок пока нет
- 1 - 10 - 209case Report-Methanol Intoxication Complicated With Acute Pancreatitis Alcoholic Ketoacidosis and Intracranial HemorrhageДокумент3 страницы1 - 10 - 209case Report-Methanol Intoxication Complicated With Acute Pancreatitis Alcoholic Ketoacidosis and Intracranial HemorrhageEdah HumaidahОценок пока нет
- Prevalens 2014 FranceДокумент9 страницPrevalens 2014 FranceEdah HumaidahОценок пока нет
- Immune Thrombocitopeni PurpuraДокумент8 страницImmune Thrombocitopeni PurpuraEdah HumaidahОценок пока нет
- Lynne Graham Damiano S Return by Lynne Graham PDFДокумент90 страницLynne Graham Damiano S Return by Lynne Graham PDFEdah Humaidah88% (16)
- Angela Aki TegamiДокумент5 страницAngela Aki TegamiEdah HumaidahОценок пока нет
- Jurnal Karies Gigi Pada AnakДокумент11 страницJurnal Karies Gigi Pada AnakYock HeadShooter0% (1)
- SympathiДокумент2 страницыSympathiEdah HumaidahОценок пока нет
- Laporan Kasus Kegawatdaruratan Intoksikasi Metanol: Oleh: Edah HumaidahДокумент1 страницаLaporan Kasus Kegawatdaruratan Intoksikasi Metanol: Oleh: Edah HumaidahEdah HumaidahОценок пока нет
- Angela Aki TegamiДокумент5 страницAngela Aki TegamiEdah HumaidahОценок пока нет
- 2011 ITP Pocket GuideДокумент8 страниц2011 ITP Pocket GuidevtОценок пока нет
- International Headache Classification III ICHD III 2013 Beta 1Документ180 страницInternational Headache Classification III ICHD III 2013 Beta 1Fityan Aulia RahmanОценок пока нет
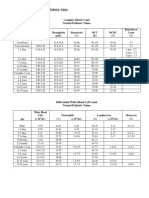
- 30a2131 Complete Blood Count Normal Pediatric Values PDFДокумент1 страница30a2131 Complete Blood Count Normal Pediatric Values PDFReziel Basilan Manalo100% (2)
- Vascular Trauma and Its ManagementДокумент5 страницVascular Trauma and Its ManagementEdah HumaidahОценок пока нет
- International Headache Classification III ICHD III 2013 Beta 1Документ180 страницInternational Headache Classification III ICHD III 2013 Beta 1Fityan Aulia RahmanОценок пока нет
- F.3 Ocd 072012Документ17 страницF.3 Ocd 072012Edah Humaidah100% (1)
- Epidemiology and Outcome of Vascular Trauma at A British Major Trauma CentreДокумент7 страницEpidemiology and Outcome of Vascular Trauma at A British Major Trauma CentreEdah HumaidahОценок пока нет
- Whatyouneed 09 1Документ24 страницыWhatyouneed 09 1Edah HumaidahОценок пока нет
- Existing Trauma and Critical Care Scoring SystemsДокумент8 страницExisting Trauma and Critical Care Scoring SystemsEdah HumaidahОценок пока нет
- Anesthesia For LaparosДокумент12 страницAnesthesia For LaparosEdah HumaidahОценок пока нет
- Hellp Syndr, SibaiДокумент21 страницаHellp Syndr, SibaiMohamed MukhrizОценок пока нет
- WhenДокумент3 страницыWhenEdah HumaidahОценок пока нет
- Penelitian LepraДокумент13 страницPenelitian LepraEdah HumaidahОценок пока нет
- Acute Diare WHO 2005Документ50 страницAcute Diare WHO 2005Boby Abdul RahmanОценок пока нет
- Steroid LepraДокумент20 страницSteroid LepraEdah HumaidahОценок пока нет
- Acute Diare WHO 2005Документ50 страницAcute Diare WHO 2005Boby Abdul RahmanОценок пока нет
- Institutional Biosafety Committee: Role of TheДокумент14 страницInstitutional Biosafety Committee: Role of TheSyeda Wardah NoorОценок пока нет
- Metabolic Stress PDFДокумент30 страницMetabolic Stress PDFNurul Latifa MuhammadОценок пока нет
- Henrietta Lacks: Dr. Roz Iasillo Trinity High School River Forest, ILДокумент13 страницHenrietta Lacks: Dr. Roz Iasillo Trinity High School River Forest, ILRoz IasilloОценок пока нет
- Chapter 17 Reproductive SystemДокумент15 страницChapter 17 Reproductive SystemJurugo GodfreyОценок пока нет
- Knee Osteoarthritis A Review of LiteratureДокумент8 страницKnee Osteoarthritis A Review of LiteratureKurnia Elka VidyarniОценок пока нет
- Examination of Bacterial Contamination in Blood ComponentsДокумент21 страницаExamination of Bacterial Contamination in Blood ComponentsCik KahadiОценок пока нет
- Pre-Eclampsia and EclampsiaДокумент21 страницаPre-Eclampsia and EclampsiaTamratKelelegn100% (1)
- Smoking and Hypertension - UpToDateДокумент25 страницSmoking and Hypertension - UpToDatemehdi.chlif4374Оценок пока нет
- A Glossary of Anesthetic Jargon .8Документ4 страницыA Glossary of Anesthetic Jargon .8TonyОценок пока нет
- Case Pre 2Документ11 страницCase Pre 2Juviely PremacioОценок пока нет
- Tinnitus Today December 1998 Vol 23, No 4Документ29 страницTinnitus Today December 1998 Vol 23, No 4American Tinnitus AssociationОценок пока нет
- Mudlark CPI Medical Care Report Oct 09Документ8 страницMudlark CPI Medical Care Report Oct 09MudlarkResearchОценок пока нет
- Parenteral Nutrition CalculationsДокумент62 страницыParenteral Nutrition CalculationsaqeelaadnanОценок пока нет
- Evmlu Uganda.2020Документ124 страницыEvmlu Uganda.2020ALINOMUGASHA EMMANUELОценок пока нет
- Postnatal Care at The Health Post and in The CommunityДокумент23 страницыPostnatal Care at The Health Post and in The CommunityGreggy Francisco LaraОценок пока нет
- Standard Surgical Attire Surgical ScrubДокумент20 страницStandard Surgical Attire Surgical ScrubzekkipianoОценок пока нет
- MENSTRUAL HYGIENE KNOWLEDGE AMONG STUDENTSДокумент11 страницMENSTRUAL HYGIENE KNOWLEDGE AMONG STUDENTSElsa Christy GumayОценок пока нет
- Empagliflozin Metformin HCL: Jardiance Duo®Документ2 страницыEmpagliflozin Metformin HCL: Jardiance Duo®Lord Carlo CabangalОценок пока нет
- HIV Drug ChartДокумент5 страницHIV Drug Chartalejandroo_26Оценок пока нет
- Nursing Fundamentals Exam ReviewДокумент10 страницNursing Fundamentals Exam ReviewAlain CheryОценок пока нет
- Anaesthetic Considerations for Day Care SurgeryДокумент8 страницAnaesthetic Considerations for Day Care SurgerySirisha Ckv100% (1)
- Comorbidities of Hearing Loss and The Implications of Multimorbidity For Audiological Care. Hearing Research - 10.1016:j.heares.2018.06.008Документ12 страницComorbidities of Hearing Loss and The Implications of Multimorbidity For Audiological Care. Hearing Research - 10.1016:j.heares.2018.06.008ALEIRAMGONZALEZОценок пока нет
- MrdicДокумент18 страницMrdicpapa0011Оценок пока нет
- EphedraДокумент9 страницEphedraapi-367367047Оценок пока нет
- Olimpiada Engleza 2017 CL A 8A PDFДокумент4 страницыOlimpiada Engleza 2017 CL A 8A PDFAnthony AdamsОценок пока нет
- Introduction to Pakistan's National Essential Drug ListДокумент16 страницIntroduction to Pakistan's National Essential Drug ListUmair MazharОценок пока нет
- Discharge PlanДокумент4 страницыDischarge PlanPaul Loujin LeeОценок пока нет
- Kanker Payudara: Dr. Dian Andriani, SPKK, M.Biomed, MarsДокумент31 страницаKanker Payudara: Dr. Dian Andriani, SPKK, M.Biomed, Marsdian andriani ratna dewiОценок пока нет
- Legal and Ethical Issues in Psychiatric NursingДокумент38 страницLegal and Ethical Issues in Psychiatric NursingElizabeth McKee100% (2)
- Data Peserta Gartheting LT 3aumst Final 2022Документ11 страницData Peserta Gartheting LT 3aumst Final 2022Doni IrawanОценок пока нет