Академический Документы
Профессиональный Документы
Культура Документы
Intern Guide To Vascular Surgery by Dipen Maun
Загружено:
sgod34Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Intern Guide To Vascular Surgery by Dipen Maun
Загружено:
sgod34Авторское право:
Доступные форматы
Intern Guide to Vascular Surgery by Dipen Maun
The vascular surgery service primarily resides on 7W, 10 East step-down unit and surgical intensive care unit. It is a busy service but an excellent experience. Familiarity with this guide will hopefully ease your anxiety as you embark upon your first call. There are 4 different types of patients that you will commonly see and need to evaluate: 1. The emergency room patient or floor consult 2. Pre-operative patient (usually admitted from the outpatient setting or on the floor) 3. Angiography patient (admitted from the angiography suite either before or after) 4. Post-operative patient Vascular History and Physical Every patient that is seen either on the floor or emergency room should have a full vascular history and physical. Risk factors such as diabetes, coronary artery disease, hypertension, and smoking should be signals for vascular disease. Atrial fibrillation is an important risk factor for embolic phenomena. Also, history of previous vascular surgery (amputations, angiograms, bypass procedures) is a common theme among vascular patients. The vascular physical exam can be approached from head to toe: Neck Palpation for masses. Think about carotid aneurysm or carotid body tumors Auscultation of carotids. Beware of the bruit that is transmitted from the heart. Upper extremity Palpate axillary, brachial and radial pulses Bilateral arm blood pressures. Discrepancy could be a sign of subclavian, axillary stenosis Abdomen Ausculate for bruits. Mesenteric stenosis (celiac or SMA) could have epigastric bruit. Renal artery bruits in the outer quadrants of the abdomen. Palpation: gently palpate for the aorta above the umbilicus (aorta bifurcates at the umbo). Normal aorta should be the width of a thumb. Lower Extremity Inspect: signs of ischemia include: muscle atrophy, hair loss, elevation pallor and dependent rubor, gangrene/ulcers Auscultate: femoral artery bruits suggest pseudoaneurysm, AV fistula Palapation of 4 pulses. It is important that the patient be in the supine position, with the head down (no tensing of muscles). YOU should be relaxed, in the sitting position. 0 1+ 2+ 3+ o o o Grading of arterial pulses Not present Diminished, difficult to palpate Easily palpable aneurysmal Femoral: below the inguinal ligament, 2 fingerbreadths lateral to the tubercle Popliteal: knee slightly flexed, hook the fingertips of both hands around the medial and lateral knee tendons in the popliteal space Posterior tibial (PT): lies in the groove posterior to the medial malleolus
o Dorsalis pedis (DP): mid-dorsum of foot between 1st and 2nd metatarsals Doppler: normal arterial signal should be biphasic. Stenosis or occlusions in arteries can sound low-pitched and monophasic. Ankle-brachial index o Use doppler probe and blood pressure cuff. Cuff placed on the ankle and doppler placed on DP or PT. Cuff is inflated until the signal disappears, then slowly deflated. The pressure when the signal reappears is recorded. Ratio is taken between the ankle and arm pressure. Index 1.0 0.5 to 0.8 < 0.5 >> 1.0 Comment Normal Non threatened limb (claudicators) Threatened limb (rest pain, tissue loss) Calcified, non-compressible in diabetics. Unreliable test. Emergency Room/Floor consult
There are numerous reasons why the ER or floor may consult vascular surgery. It is beyond the scope of this guide to discuss all of them, but there are three entities, which should not be overlooked, blown off or ignored. In all three cases, the chief resident/fellow should be notified immediately. Cold Foot Lower extremity ischemia presents in three different ways: the non-threatened limb (claudicators), the threatened limb (rest pain, non-healing ulcers or gangrene) and acute arterial occlusion. Signs of the latter include the 6Ps: pallor, pulselessness, pain, paralysis, parasthesias, poikilothermia (coolness). Paralysis and sensory loss are late signs and often result in limb loss. Also the time course of the disease suggests urgency: sudden onset, hours to days = acute, whereas weeks to months chronic. History of vascular disease suggests thrombosis of graft or an important collateral. No history of vascular disease suggests embolic etiologies (afib, heart thrombus, shaggy aorta, aneurysm). Whichever the case may be, intervention in the form of operating room or angiography suite should be done promptly in order to prevent limb loss. Hot Foot This is the patient who is diabetic, complaining of pain from days to weeks, may or may not have pulses, high fever and white count, a break in the skin and a tender, erythematous, angry fluctuant foot. This is a surgical emergency as sepsis from this foot/toe abscess can progress rapidly leading to hemodynamic collapse and death. Blood work should be sent right away, rescuscitation started in the emergency room and surgical intervention completed urgently. Ruptured AAA This is a true surgical emergency. It involves the patient with a known abdominal aortic aneurysm or pulsatile mass, complains of pain (abdominal, back or even groin) and signs of hypotension (syncope). This patient needs no further imaging or work-up. As an intern, you should drop everything and your full-undivided attention should be to activate the vascular team immediately (chief resident, fellow and attending), and facilitate this patients delivery to the operating room. A specimen in the blood bank must be sent. Anesthesia and the operating room must be notified immediately, and the patient be transported there at once. A member of the vascular team should be at the bedside at all times. Any delay can result in death.
Pre-operative work-up of a vascular patient History and physical o Full vascular exam as described above o ABIs for lower extremity patients o Stool guiac (before anticoagulation is given) Full list of meds o Halve doses of insulin in diabetics o Be wary of diuretics in patients that are NPO o Stop glucophage for patients receiving contrast Cardiology/PMD o Should be notified o Routine EKG within 7 days of surgery o 2D Echocardiogram to eval left ventricular function when indicated o Pharmacologic stress test to eval reversible ischemia when indicated -Need to be NPO (no caffeine) Renal o Dialysis fellow should be notified for dialysis-dependent patients o Patients should be dialyzed morning of or day before surgery with a documented postdialysis potassium Vein mapping o Bypass patient needs to have upper and lower extremity superficial veins mapped as potential conduits for bypass. o Reinforce lines on arms and legs if fading. Anticoagulation o Heparin should be stopped 6 hrs before start time of surgery o Plavix should be off for 7 days o Aspirin is attending dependent and disease dependent. Needs to be off for 7 days to see no effect in the operating room. o Prophylactic SQ heparin is attending-dependent NPO after midnight CXR within 30 days Lab work o CBC with platelets, Chem 7, PT/PTT within 7 days o Type and hold specimen in the blood bank within 3 days of surgery Informed consent o Health care proxy or next of kin for unconsentable patients o Disposal form for amputee patients Films o Need to print out films for bypass, aorta patients. Use Kenny in radiology Maintenance IVF overnight o Use D5 NS with 20 meq/L at ~ 1 cc/kg o No fluid for dialysis patients o No potassium for renal patients The Angio Patient Pre-Angio (mini pre-op) H&P if being admitted from home
NPO after midnight Renal protection o IV hydration ~1cc/kg except in ESRD patients o Mucomyst 600 mg PO q 12 hrs (2 doses before and 2 doses after) Lab work Type and Screen, CBC, Chem 7, PT/PTT Pulse exam Consent right/left extremity angiogram, possible angioplasty, possible stent
Post-Angio (mini post-op) Bed rest X 6 hrs with frequent vitals checks Post-procedure hydration ~1cc/kg Appropriate diet Groin check o Pulsatile mass/expanding hematoma notify CR/fellow o Hematoma should be marked out and CBC checked o Infection Pulse check o Compare to pre-procedure exam. Interventions could raise intimal flap, cause dissection or embolize debris causing acute ischemia. Do not restart glucophage for 2 days Order routine morning labs Hematocrit and creatinine should be monitored Post-operative patient Carotid Endarterectomy Post-operatively they must remain in a monitored setting (PACU, 10E SDU, SICU). Monitor for signs of cardiopulmonary complication (vitals, oxygen saturation, mental status, urine output, EKG, CXR). There are a few specific things you should check for: Neurological deficits: ipsilateral facial weakness or contralateral extremity weakness May need to be re-explored!!! CN VII: perioral weakness, drooling CN IX: inability to swallow CN X: hoarseness CN XII: deviation of tongue to affected side Wound check: a hematoma can be devastating and cause airway problems BP control: use phenylephrine for SBP <110, or nitroprusside for SBP >160. Blood pressure not controlled could result in stroke Follow morning labs Drains and foley catheter can be taken out the following morning. If everything goes well, patient is discharged on the first post-operative day. Endovascular aortic stent graft Post-operatively they must remain in a monitored setting (PACU, 10E SDU, SICU). Monitor for signs of cardiopulmonary complication (vitals, oxygen saturation, mental status, urine output, EKG, CXR).
They will have two lateral incisions over their groins, which should be examined for hematoma, pulsatile masses or hemorrhage. The extremities should be examined for pulses as limb occlusion, dissections or embolization can cause acute limb ischemia. Most patients are done under spinal anesthesia so foley catheter can be removed once spinal wears off. Patients should be well hydrated as they receive large doses of contrast. Creatinine and hematocrit should be followed. If everything goes well, the patient goes home on the first post-operative day after clearance by the cardiologist.
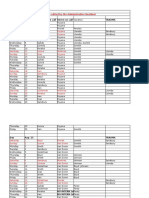
Lower extremity bypass Post-operatively they must remain in a monitored setting (PACU, 10E SDU, SICU). Monitor for signs of cardiopulmonary complication (vitals, oxygen saturation, mental status, urine output, EKG, CXR). Graft thrombosis from technical error usually occurs in first 24 to 48 hours so diligent, frequent vascular checks must be done. Patients are frequently on low dose heparin, so wounds should be examined for hematoma or excessive bleeding. Follow serial hematocrit and creatinine. Physical therapy should start on post-op day #2 (weight bearing status is case based). Dressings should be changed daily. Keep groin wound dry and covered. Coumadin should not be started until amputation/debridement (if necessary) is complete. Early rehab consult. Anti-coagulation Heparin Bolus 5000 Units IV, Drip at 1000 U /hr IV for therapeutic anticoagulation Short half life ~ 60 to 90 minutes Follow PTT (recheck 6 hrs after changing) DVT Prophylaxis 5000 Units SQ Q12 Platelets should be followed early in the course of therapy, watching out for heparininduced thrombocytopenia Heparin protocol (for target PTT 60 - 80) PTT <45 Increase by 200 U/hr, check PTT in 6 hrs PTT 46-59 Increase by 100 U/hr, check PTT in 6 hrs PTT 60-80 No change, recheck PTT in AM PTT 81-100 Decrease by 100 U/hr, check PTT in 6 hrs PTT >110 Decrease by 200 U/hr, check PTT in 6 hrs Low molecular weight heparin Therapuetic: Fragmin 100 Units/kg SQ q12; Lovenox 1 mg/kg SQ q 12 DVT Prophylaxis: Fragmin 5000 Units SQ QD, Lovenox 30mg SQ q12 No PT/PTT checks
Also need to watch for heparin-induced thrombocytopenia Need to stop at least 12 hours prior to procedure Coumadin Inhibits Vit K dep factors (II, VII, IX, X) Delayed effect Usually heparinize concurrently until goal reached Increases PT and PTT, but monitor INR daily until stable dose achieved Reversal with FFP (acute) or Vit K (slow) Disposition There are a few points to make in attempting to get patients discharged or placed into dispositions quickly: Early physical therapy as soon as medically stable. The physical therapist decides whether or not a patient needs acute rehab (rehab consult) or subacute placement (nursing home by social work) Diligent wound care can allow patients to avoid unnecessary amputations, wound debridements or bypass procedures, all of which can prolong hospital stay and increase patient complications Frequent and early discussion with social workers and staying in tune to the patients at home needs eg home physical therapy, visiting nurse, home health aid for assistance with activities of daily living, home IV antibiotics Continuous communication with the nurses, ancillary staff, consulting physicians, primary medical doctor, and attending vascular surgeon. Keeping everyone on the same page is important to avoid suprises. The single most important thing to learn from this guide is never keep information to yourself. Do not be afraid to call your chief resident, fellow or attending at any time. Staying honest and keeping your superiors informed will lead you to a successful vascular surgery rotation.
Вам также может понравиться
- NOAC ChartДокумент2 страницыNOAC Chartsgod34Оценок пока нет
- Espinal STSДокумент2 страницыEspinal STSsgod34Оценок пока нет
- Laparoscopic Peritoneal Entry TechniquesДокумент52 страницыLaparoscopic Peritoneal Entry Techniquessgod34100% (1)
- Nutrition Support: Sean P Harbison MDДокумент42 страницыNutrition Support: Sean P Harbison MDsgod34Оценок пока нет
- Espinal STS PDFДокумент2 страницыEspinal STS PDFsgod34Оценок пока нет
- Nadelman STSДокумент2 страницыNadelman STSsgod34Оценок пока нет
- Abdominal InfectionsДокумент6 страницAbdominal InfectionsPatrico Rillah SetiawanОценок пока нет
- Surgery Preround Template SkeletonДокумент2 страницыSurgery Preround Template Skeletonsgod34Оценок пока нет
- Master Schedule 10-22Документ65 страницMaster Schedule 10-22sgod34Оценок пока нет
- Basic Ventilator y ModesДокумент47 страницBasic Ventilator y ModesAlina VanceaОценок пока нет
- Modes of Mechanical VentilationДокумент4 страницыModes of Mechanical Ventilationsgod34100% (1)
- 2012 KevinSextonMay2 BC Wound HealingДокумент40 страниц2012 KevinSextonMay2 BC Wound HealingYulinda PrimilisaОценок пока нет
- Veins More DistensibleДокумент27 страницVeins More Distensiblesgod34Оценок пока нет
- Resident Rotation Schedule 2015-16 - FinalДокумент14 страницResident Rotation Schedule 2015-16 - Finalsgod34Оценок пока нет
- Venous DiseaseДокумент50 страницVenous Diseasesgod34Оценок пока нет
- HemostasisДокумент38 страницHemostasissgod34100% (1)
- Absite Review VascularДокумент183 страницыAbsite Review Vascularsgod34Оценок пока нет
- Venous Disorder - GodelmanДокумент27 страницVenous Disorder - Godelmansgod34Оценок пока нет
- Lecture 5 Vascular Disorders StudentsДокумент103 страницыLecture 5 Vascular Disorders Studentssgod34Оценок пока нет
- 7 MedEd Vascular Jonny Hodgkinson 12.11.12 1Документ35 страниц7 MedEd Vascular Jonny Hodgkinson 12.11.12 1sgod34Оценок пока нет
- Endoscopy TechniqueДокумент8 страницEndoscopy Techniquesgod34Оценок пока нет
- Fluid Resucitation, 2015Документ44 страницыFluid Resucitation, 2015sgod34Оценок пока нет
- Guidelines Management 2007w Bookmarks PDFДокумент0 страницGuidelines Management 2007w Bookmarks PDFdiaga081Оценок пока нет
- ABX Dosing & RДокумент11 страницABX Dosing & Rsgod34Оценок пока нет
- Colon CAДокумент16 страницColon CAsgod34Оценок пока нет
- General Surgery - DR Tadros - CompressedДокумент164 страницыGeneral Surgery - DR Tadros - Compressedsgod34Оценок пока нет
- Anast Bleed MMДокумент17 страницAnast Bleed MMsgod34Оценок пока нет
- Abnormal LFTs in General PracticeДокумент57 страницAbnormal LFTs in General Practicesgod34Оценок пока нет
- Bile Duct Injuries: Dr. Joe M Das Junior Resident S3 UnitДокумент149 страницBile Duct Injuries: Dr. Joe M Das Junior Resident S3 Unitsgod34Оценок пока нет
- Bile Duct Injuries: Dr. Joe M Das Junior Resident S3 UnitДокумент149 страницBile Duct Injuries: Dr. Joe M Das Junior Resident S3 Unitsgod34Оценок пока нет
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Haematology and Blood Transfusion User HandbookДокумент38 страницHaematology and Blood Transfusion User HandbookARIF AHAMMED P100% (1)
- Coagulation Testing For POCCДокумент77 страницCoagulation Testing For POCCBiniyam AsratОценок пока нет
- Perioperative Medicine PearlsДокумент68 страницPerioperative Medicine PearlsChadi AlraiesОценок пока нет
- 15 Hemoglobin DrabkinДокумент1 страница15 Hemoglobin DrabkinAhmad SaeedОценок пока нет
- Treatment of Infections Associated With Surgical ImplantsДокумент8 страницTreatment of Infections Associated With Surgical ImplantsDiego Bedón AscurraОценок пока нет
- AHCCCS Pharmacy and Therapeutics Committee May 19, 2021Документ247 страницAHCCCS Pharmacy and Therapeutics Committee May 19, 2021hussam mazinОценок пока нет
- Understanding OgdДокумент3 страницыUnderstanding Ogdapi-282091976Оценок пока нет
- Drug Study Vitamin KДокумент3 страницыDrug Study Vitamin KFlorence NightingaleОценок пока нет
- Campomanes NafamostatДокумент8 страницCampomanes NafamostatELSPETH TAMAR CAMPOMANESОценок пока нет
- Thrombin Time - GRP 5Документ14 страницThrombin Time - GRP 5Joyce LeeОценок пока нет
- Serum Vs Plasma: Which Specimen Should You UseДокумент48 страницSerum Vs Plasma: Which Specimen Should You UseTanveerОценок пока нет
- Renal Replacement TherapyДокумент303 страницыRenal Replacement TherapyPaloma Cruz100% (9)
- Acute Stroke Treatment - CPM 8th EdДокумент22 страницыAcute Stroke Treatment - CPM 8th EdSuresh ShresthaОценок пока нет
- Assessment and Management of The Unconscious PatientДокумент6 страницAssessment and Management of The Unconscious PatientRed DevilОценок пока нет
- tPA Ischemic Stroke Protocol Eligibility ChecklistДокумент1 страницаtPA Ischemic Stroke Protocol Eligibility ChecklistMazin Al-TahirОценок пока нет
- CME Quiz 2019 April Issue 7Документ3 страницыCME Quiz 2019 April Issue 7Basil al-hashaikehОценок пока нет
- The Infected Total Knee Arthroplasty: EditorsДокумент186 страницThe Infected Total Knee Arthroplasty: EditorsalvaroОценок пока нет
- KENALOGДокумент4 страницыKENALOGStefan Codrin CriclevitzОценок пока нет
- Coagulants and AnticoagulantsДокумент5 страницCoagulants and AnticoagulantsMuhammad AsifОценок пока нет
- I. P A D: Eripheral Rterial IseaseДокумент8 страницI. P A D: Eripheral Rterial IseasevmdcabanillaОценок пока нет
- Diet Ant PDFДокумент3 страницыDiet Ant PDFAnonymous ZvBtfvОценок пока нет
- Guia Aha Asa Stroke PDFДокумент77 страницGuia Aha Asa Stroke PDFAndrea Cayufilo CarmonaОценок пока нет
- Cardiovascular Drugs (Veterinary Pharmacology)Документ44 страницыCardiovascular Drugs (Veterinary Pharmacology)DR Muhammad Abdul BasitОценок пока нет
- Deep Vein Thrombosis: by Dr. Muhammad Umair ChangДокумент20 страницDeep Vein Thrombosis: by Dr. Muhammad Umair ChangumairОценок пока нет
- Oral-Revalida GДокумент19 страницOral-Revalida GJasmine CorreosОценок пока нет
- PVC Unido ConDuplicadosДокумент1 181 страницаPVC Unido ConDuplicadosJorge Chachaima MarОценок пока нет
- ADC Part 1 - TG Keynotes III v1.0Документ14 страницADC Part 1 - TG Keynotes III v1.0Geethanjali SadasivamОценок пока нет
- Cardiovascular Medications NCLEX Practice QuizДокумент8 страницCardiovascular Medications NCLEX Practice QuizAngie MandeoyaОценок пока нет
- Atrial FibrillationДокумент21 страницаAtrial FibrillationAndrea LombiОценок пока нет
- 2020 Therapeutic Strategies For Thrombosis - New Targets and ApproachesДокумент20 страниц2020 Therapeutic Strategies For Thrombosis - New Targets and ApproachesVladimir BasurtoОценок пока нет