Академический Документы
Профессиональный Документы
Культура Документы
Cutaneous Defenses Against Dermatophytes and Yeasts
Загружено:
arsyiadlinaАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Cutaneous Defenses Against Dermatophytes and Yeasts
Загружено:
arsyiadlinaАвторское право:
Доступные форматы
CLINICAL MICROBIOLOGY REVIEWS, July 1995, p. 317335 0893-8512/95/$04.
000 Copyright 1995, American Society for Microbiology
Vol. 8, No. 3
Cutaneous Defenses against Dermatophytes and Yeasts
DAVID K. WAGNER
AND
PETER G. SOHNLE*
Division of Infectious Diseases, Department of Medicine, Medical College of Wisconsin, Milwaukee, Wisconsin 53226, and Medical and Research Services, VA Medical Center, Milwaukee, Wisconsin 53295 OVERVIEW .................................................................................................................................................................318 TYPES OF CUTANEOUS FUNGAL INFECTIONS .............................................................................................318 Cutaneous Candidiasis...........................................................................................................................................318 Dermatophytosis .....................................................................................................................................................319 Tinea (Pityriasis) Versicolor .................................................................................................................................320 Malassezia Folliculitis............................................................................................................................................320 Miscellaneous Supercial Fungal Infections ......................................................................................................320 FACTORS PREDISPOSING TO CUTANEOUS FUNGAL INFECTIONS........................................................321 Cutaneous Candidiasis...........................................................................................................................................321 Dermatophytosis .....................................................................................................................................................321 Tinea Versicolor ......................................................................................................................................................321 Other Cutaneous Fungal Infections .....................................................................................................................321 NONIMMUNOLOGIC CUTANEOUS DEFENSES ..............................................................................................321 Structure of the Skin..............................................................................................................................................321 Keratinization and Epidermal Proliferation.......................................................................................................321 Antifungal Substances............................................................................................................................................321 Unsaturated Transferrin........................................................................................................................................322 THE INFLAMMATORY RESPONSE .....................................................................................................................322 Relationship between Inammation and Chronicity .........................................................................................322 Chemotactic Mechanisms ......................................................................................................................................322 Antifungal Mechanisms of Phagocytic Cells.......................................................................................................322 THE CUTANEOUS IMMUNE SYSTEM ................................................................................................................322 Potential Role in Supercial Fungal Infections .................................................................................................322 Cells with Immunologic Potential in the Skin....................................................................................................323 Epidermal Langerhans cells..............................................................................................................................323 Dermal dendritic cells ........................................................................................................................................323 Epidermal T lymphocytes ..................................................................................................................................323 Keratinocytes .......................................................................................................................................................324 Microvascular endothelial cells ........................................................................................................................324 Interactions between Cutaneous Cells .................................................................................................................324 Langerhans cells and lymphocytes ...................................................................................................................324 Keratinocytes and Langerhans cells ................................................................................................................325 Keratinocytes and lymphocytes.........................................................................................................................325 Keratinocytes and inammatory cells..............................................................................................................325 Microvascular endothelial cells and lymphocytes ..........................................................................................326 Initiation and Expression of Cutaneous Immune Responses...........................................................................326 IMMUNE RESPONSES TO FUNGAL ANTIGENS..............................................................................................326 Cutaneous Candidiasis...........................................................................................................................................326 Dermatophytosis .....................................................................................................................................................327 Tinea Versicolor and Other Supercial Fungal Infections...............................................................................328 MECHANISMS OF IMMUNOLOGIC DEFECTS ................................................................................................328 Cutaneous Candidiasis...........................................................................................................................................328 Dermatophytosis .....................................................................................................................................................329 Tinea Versicolor ......................................................................................................................................................329 IMMUNOLOGIC THERAPY....................................................................................................................................329 Cutaneous Candidiasis...........................................................................................................................................329 Dermatophytosis .....................................................................................................................................................329 Tinea Versicolor ......................................................................................................................................................330 SUMMARY AND CONCLUSIONS..........................................................................................................................330 REFERENCES ............................................................................................................................................................330
Downloaded from cmr.asm.org by on March 19, 2009
* Corresponding author. Phone: (414) 384-2000, ext. 2878. Fax: (414) 383-8010. 317
318
WAGNER AND SOHNLE TABLE 1. Types of cutaneous mycoses and the common responsible pathogens
Type of infection Responsible pathogen(s)
CLIN. MICROBIOL. REV.
TYPES OF CUTANEOUS FUNGAL INFECTIONS Cutaneous Candidiasis Cutaneous candidiasis is an infection of the skin that is generally caused by the yeast Candida albicans and which can be either acute or chronic in nature. Cases of cutaneous candidiasis caused by other Candida species such as C. parapsilosis or C. tropicalis are sometimes seen, but these are rare. C. albicans is part of the normal ora of the gastrointestinal tract rather than of the skin, although it can be found on the skin on occasion. This organism can grow as either yeast cells or lamentous forms, with mixtures of the two phases generally seen in tissue infections. The virulence of C. albicans has been attributed variously to its ability to grow at particular temperatures, its ability to produce lamentous forms, its adherence capabilities, and the activity of its different enzymes. Acute cutaneous candidiasis may present as intertrigo, producing intense erythema, edema, creamy exudate, and satellite pustules within folds of the skin. Other infections may be more chronic, as in the feet where there can be a thick, white layer of infected stratum corneum overlaying the epidermis of the interdigital spaces. Candida paronychia is marked by infections of the periungual skin and the nail itself, resulting in the typical swelling and redness of this type of candida infection. In some cases supercial C. albicans infections may be particularly severe and recalcitrant to treatment, producing the uncommon disorder known as chronic mucocutaneous candidiasis. This condition consists of persistent and recurrent infections of the mucous membranes, skin, and nails, along with a variety of other manifestations. The supercial infections last for years in the affected patients unless they are properly treated; however, deep candida infections are very rare in this situation (141). Oral thrush and candida vaginitis are fairly common in patients with chronic mucocutaneous candidiasis. There is often infection of the esophagus, although further extension into the viscera is unusual. The typical skin lesions are generally red, raised, and hyperkeratotic but usually are not painful. Epidermal neutrophilic microabscesses, which are common in acute cutaneous candidiasis, are rare in the lesions of chronic mucocutaneous candidiasis. Nail involvement can be severe in this condition, producing marked thickening, distortion, and fragmentation of the nails, with chronic swelling of the distal phalanx. The oral thrush and vaginitis in chronic mucocutaneous candidiasis closely resemble the acute mucous membrane infections in other patients, except that they are
Cutaneous candidiasis Candida albicans Dermatophytosis Trichophyton, Microsporum, Epidermophyton spp. Tinea pedis T. rubrum, T. mentagrophytes, E. occosum Tinea cruris E. occosum, T. rubrum, T. mentagrophytes Tinea barbae T. rubrum, T. verrucosum, T. mentagrophytes Tinea unguium T. rubrum, T. mentagrophytes, E. occosum (onychomycosis) Tinea capitis T. tonsurans, T. schoenleini (favus), T. violaceum, M. canis Tinea corporis T. rubrum, T. mentagrophytes, T. concentricum, T. verrucosum, T. tonsurans, M. canis, M. gypseum, E. occosum Tinea versicolor Malassezia furfur (Pityrosporum orbiculare) Malassezia folliculitis Malassezia furfur Tinea nigra Phaeoannellomyces werneckii (Exophialia werneckii) White piedra Trichosporon beigelii Black piedra Piedraia hortae
Downloaded from cmr.asm.org by on March 19, 2009
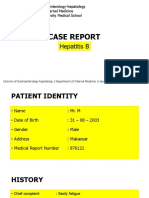
OVERVIEW This review will cover mechanisms of cutaneous defense against supercial mycoses such as cutaneous candidiasis, dermatophytosis, tinea (pityriasis) versicolor, and some related infections. The various individual infections and the organisms causing them are shown in Table 1. In addition, the anatomy of the normal skin is provided in Fig. 1 in order to show the most important cell types and the epidermal cell layers where the infections usually occur. These infections are generally conned to the stratum corneum and cutaneous appendages, in contrast to the subcutaneous mycoses and cutaneous infections associated with deep mycoses. The discussion of defenses against the organisms causing supercial mycoses will be organized to describe the individual infections and predispositions to them, immunologic and nonimmunologic cutaneous defenses, mechanisms of host defense defects in patients with chronic supercial fungal infections, and possibilities for immunologic therapy to correct these defects.
FIG. 1. Anatomy of the normal skin.
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS
319
more chronic in nature. The oral lesions are generally tender and painful. There are a number of other disorders that are associated with the syndrome of chronic mucocutaneous candidiasis (reviewed in references 76 and 147). Especially prominent are certain types of endocrine dysfunction, such as hypoadrenalism, hypoparathyroidism, hypothyroidism, ovarian insufciency, pernicious anemia, and diabetes mellitus. The combination of chronic supercial candidiasis and endocrine hypofunction has been termed the candida endocrinopathy syndrome. Also found in these patients are alopecia totalis, vitiligo, malabsorption, chronic hepatitis, dysplasia of the dental enamel, congenital thymic dysplasia, thymomas, and other infections. Among the latter, chronic dermatophytosis, recurrent bacterial infections, and occasional opportunistic infections such as cryptococcosis, histoplasmosis, and Pneumocystis carinii pneumonia are the most common. In these patients dermatophytosis may cause extensive skin lesions that may be misidentied as cutaneous candidiasis and then perhaps not treated optimally (44). Chronic mucocutaneous candidiasis no doubt represents a group of syndromes with a variety of predisposing or secondary abnormalities in host defense function. Therefore, it may be difcult to describe an immunologic pattern that includes all patients. The most common deciency appears to be one of cell-mediated immune responses against candida antigens, as discussed below, although abnormalities in chemotaxis or phagocytic cell function have also been reported (176, 222, 235, 276, 282). Other host defense mechanisms, such as humoral immunity and the complement system, have generally been found to be normal in these patients (76, 144, 145, 147, 275). Although the supercial infections of chronic mucocutaneous candidiasis are generally not life-threatening, they can be very disguring. Before ketoconazole and other azole antifungal agents became available, the treatment of this condition was quite difcult. Whereas amphotericin B produced prompt clearance of the cutaneous lesions, relapses usually occurred, presumably because of the underlying immunodeciency state. At present, long-term treatment with azole antifungal drugs can produce good results in chronic mucocutaneous candidiasis, although occasional failures have occurred due to the development of resistant strains of C. albicans. Also, endocrine dysfunction, including life-threatening adrenal crises, can develop after presentation of the candidiasis, so these patients need to be followed for this possibility. Patients who present with chronic mucocutaneous candidiasis should also be evaluated for the presence of infection with the human immunodeciency virus and, if presenting as adults, for the possibility of thymoma. Dermatophytosis Dermatophytoses are infections of keratinized structures, such as the nails, hair shafts, and stratum corneum of the skin, by organisms of three genera of fungi termed the dermatophytes. Although they are not part of the normal human skin ora (50), these organisms are particularly well adapted to infecting this location because they can use keratin as a source of nutrients, unlike most other fungal pathogens. The different types of dermatophytosis are classied according to body site, using the word, tinea, followed by a term for the particular body site. The major types of dermatophytosis and the most frequent organisms associated with them are listed in Table 1. The word tinea itself comes from the Roman word for the clothes moth because of the similarity of its effect on wool garments to the shape of the fungal skin infections (2). The degree of inammation produced in the lesions appears to
depend primarily on the particular organism and perhaps also to some extent on the immunological competence of the patient. In any event, the more chronic forms of dermatophytosis are generally associated with less inammation and tend to be produced most often by organisms usually associated with humans (anthropophilic). Those associated with animals (zoophilic) or the soil (geophilic) usually cause much more inammatory infections. Tinea pedis (athletes foot) is probably the most common form of dermatophytosis. This condition is a chronic toe web infection that can be scaly, vesicular, or ulcerative in form and which can sometimes produce hyperkeratosis of the sole of the foot. Secondary gram-negative and mixed bacterial infections may complicate tinea pedis, producing more exudative lesions. Tinea cruris is an expanding dermatophyte infection in the exural areas of the groin and occurs much more frequently in males than in females. Dermatophytosis of the major surface areas of the body is termed tinea corporis. These infections frequently take the classical annular, or ringworm, shape. This type of infection can sometimes be extensive, particularly in patients with some kind of preexisting immunological deciency. In these immunodecient patients the patches are usually nummular instead of annular and are studded with small papules or pustules where the organism has descended into hair follicles. Involvement of the beard area in men, a condition known as tinea barbae, is often caused by zoophilic organisms such as Trichophyton verrucosum. These infections can be highly inammatory because of the organism involved and may also be secondarily infected with bacteria. Tinea unguium is a form of onychomycosis, or fungal infection of the nails, and is most frequently caused by Trichophyton rubrum. Nail infections, particularly of the toenails, are among the most difcult type of dermatophytosis to treat. Infection of the hair and skin on the scalp is called tinea capitis and is more common in children than adults. In some cases a raised, tender mass of inamed tissue, called a kerion, may occur. This situation generally indicates that a spontaneous cure will result. In other cases (black dot ringworm) there may be minimal inammation, but hair loss may occur, with the scattered stumps of broken hairs being left behind in the infected area. Favus (or tinea favosum) is a distinctive type of tinea capitis that lasts for many years and is characterized by the development of extensive, cup-shaped crusts called scutula. The description of the fungal origin of favus in 1837 marked the rst time that a microorganism had been incriminated as causing a human disease (2). Some patients with dermatophytosis develop secondary cutaneous eruptions known as dermatophytids or id reactions. These reactions generally occur at a site distant from the primary dermatophyte infection and may be elicited by skin testing with fungal antigens. They are generally vesicular but can also be papular, eczematous, or urticarial or have the appearance of erythema multiforme. Vesicular dermatophytids are most commonly associated with inammatory dermatophyte infections. It is a characteristic of dermatophytids that the organism can usually not be cultured from them, although it is easily recoverable from the original site of dermatophytosis. Most patients with vesicular dermatophytids can be shown to have delayed hypersensitivity to dermatophyte antigens (96), and some have also been demonstrated to have vigorous lymphocyte transformation responses to these antigens (257). Most patients with urticarial dermatophytids have immediate wheal reactions to dermatophyte antigens. In the past, dermatophytids have been treated effectively with topical corticosteroids (96), but elimination of the infecting fungus is the treatment of choice.
Downloaded from cmr.asm.org by on March 19, 2009
320
WAGNER AND SOHNLE
CLIN. MICROBIOL. REV.
Dermatophytes rarely invade the deep tissues or produce systemic infections, even in severely immunocompromised patients. Infrequently, however, granulomas, draining sinuses, or actual abscesses can be produced by these organisms (72). As discussed below, competition for iron by serum proteins such as transferrin or activation of complement may preclude the dermatophytic fungi from invading deep tissues in most patients, even if they are immunosuppressed. There are two opportunistic fungal organisms, Scytalidium dimidiatum (Hendersonula toruloidea) and Scytalidium hyalinum, that can produce conditions clinically mimicking those caused by the usual dermatophyte species (67). These two organisms appear to be antigenically distinct from the dermatophytes (181). Some cases have apparently been acquired within the United States, but most come from areas in other parts of the world where the organisms are endemic. Because these infections do not respond to conventional antifungal therapy, it is important to identify these pathogens by culture of the infected skin. The treatment of dermatophytosis has improved markedly in recent years with the development of new antifungal agents for topical application or oral administration. The initial approach to most cases of dermatophytosis is to try topical therapy with creams or powders containing specic antifungal agents, including tolnaftate, chlorphenesin, undecylenate, cyclopiroxolamine, and naftane, or an imadozole such as clotrimazole, miconazole, econazole, or ketoconazole. However, certain kinds of dermatophytosis, including widespread infections and those of hair and nails, will often respond poorly to topical therapy and will require prolonged courses of an oral antifungal agent, such as griseofulvin, ketoconazole, itraconazole, uconazole, or terbinane. Tinea (Pityriasis) Versicolor Tinea (pityriasis) versicolor is a chronic supercial fungal infection of the skin, generally affecting the trunk or proximal parts of the extremities, caused by the yeast Malassezia furfur or Pityrosporum orbiculare (81). The organism is lipid requiring and will not grow on most laboratory media unless they are enriched with an appropriate lipid source such as olive oil. The lesions resulting from infection with M. furfur are macules that may coalesce into large, irregular patches characterized by ne (pityriasiform) scaling. Hypopigmentation in the lesions may be due to dicarboxylic acids, such as azelaic acid, that are produced by the fungus and inhibit the tyrosinase that is involved in melanin production (187). Hyperpigmentation may also result, usually stimulated by low-grade inammation. These infections can persist for years unless treated appropriately, although the major symptoms associated with them are cosmetic. On the other hand, pruritus is occasionally produced by the lesions and can be bothersome for some patients. Potassium hydroxide preparations of skin scrapings reveal the typical grapelike clusters of yeast and tangled webs of hyphae of the causative fungus so that a diagnosis of tinea versicolor can be made. By electron microscopy, the organisms of tinea versicolor have been demonstrated to be actually invading the cornied cells of the supercial skin layer, producing a true intracellular infection (178). In some individuals tinea versicolor may be found in unusual patterns. For example, the infection may occasionally be located in sites such as the scalp, genitalia, or exural areas (a condition termed inverse tinea versicolor). Infection on the face has been reported in immunosuppressed patients (121), and in other patients without obvious underlying conditions it may present as intertrigo (140). Tinea versi-
color is more common in adults than in children (71) perhaps because of the greater activity of the sebaceous glands in adults. M. furfur has also been postulated to play a role in certain other diseases, including atopic dermatitis, seborrheic dermatitis, psoriasis, and reticulate papillomatosis (40, 74, 191, 231). Tinea versicolor can be treated topically with lotions or creams containing selenium or sodium thiosulfate or with specic antifungal agents. Sulfur-salicyclic acid shampoo can also be used. Topical treatment is generally successful, although relapses are frequent, either because the patients predisposition to the infection has not been reversed or because the organisms may persist within hair follicles (152). Oral ketoconazole, uconazole, and itraconazole have also been shown to be effective in treating tinea versicolor, although relapses may also occur after these systemic treatments. Malassezia Folliculitis Malassezia folliculitis resembles several other cutaneous infections, including acne vulgaris, the macronodular lesions of disseminated candidiasis in immunosuppressed patients, and the candidal papular folliculitis of heroin addicts (152). It may also be confused with graft-versus-host disease in bone marrow transplant recipients (33). Malassezia folliculitis is caused by M. furfur and tends to infect the same areas as does tinea versicolor: the upper shoulders, back, and chest. As opposed to acne, pustules extend down the arms and down the back to the waist. There are no comedones and the lesions are monotonously monomorphic. The papules begin as an inammation of the hair follicles, instead of the macules typical of tinea versicolor, and may progress to frank pustules. These lesions are generally quite pruritic. The contents of the infected hair follicles include keratinaceous material, amorphous cellular debris, inammatory cells, and the yeast forms (but not the hyphal forms) of the infecting organisms (153, 206). Malassezia folliculitis can be treated with topical antifungal agents and may also respond to 50% propylene glycol in water applied twice a day for 3 weeks (9). If topical therapy fails, malassezia folliculitis can be treated with an oral azole antifungal drug for 2 to 3 weeks. Miscellaneous Supercial Fungal Infections Tinea nigra is a supercial mycosis of the palms that is most often caused by Phaeoannellomyces werneckii (Exophiala werneckii). The lesions are generally dark colored, nonscaling macules that are usually asymptomatic but can be confused with melanomas and perhaps result in unnecessary surgery (195). Tinea nigra is most often seen in tropical or semitropical areas of Central and South America, Africa, and Asia, although some cases do occur in North America. This condition can be treated effectively with either keratinolytic agents or topical imadazoles. White piedra is an asymptomatic fungal infection of the hair shafts that is caused by Trichosporon beigelii. This infection produces light-colored, soft nodules on the hair shafts and may cause the involved hairs to break. Otherwise, this condition appears to be asymptomatic, although the causative fungus can produce serious infections in immunocompromised patients. Cutaneous trichosporonosis and trichosporon onychomycosis have also been reported (82, 138). Black piedra is similar to white piedra in that it is a nodular, generally asymptomatic fungal infection of the hair shafts. It is caused by Piedraia hortae and most commonly affects the scalp hair. Black and white piedra are generally treated by clipping off the affected hairs.
Downloaded from cmr.asm.org by on March 19, 2009
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS
321
FACTORS PREDISPOSING TO CUTANEOUS FUNGAL INFECTIONS Cutaneous Candidiasis A variety of local and systemic factors predispose to supercial fungal infections. Cutaneous candidiasis most frequently occurs when there are warm, moist conditions such as in skin folds, under the diapers of newborns, and in tropical climates or during the summer months. Otherwise, treatment with corticosteroids, cytotoxic agents, broad-spectrum antibiotics, and oral contraceptives all predispose to various forms of candidiasis. Diabetes mellitus (179) and infection with human immunodeciency virus (52, 164, 208) are both strongly associated with supercial candidiasis, although disseminated candidiasis is unusual in these conditions. Genetic predisposition may be important in chronic mucocutaneous candidiasis in that approximately 25% of these patients have relatives with this disease (116, 117). Dermatophytosis Local cutaneous factors appear to be very important in determining whether or not infection will occur after an exposure to the dermatophytic fungi. For example, the warm and moist conditions in the swampy areas of Vietnam were thought to be related to the high incidence of dermatophytosis in combat troops there (28). Also, occlusion over the site appears to enhance susceptibility to experimental dermatophyte infections in humans and other animals (10, 28, 105, 154, 254, 264). Occlusion has been postulated to increase hydration of the underlying skin and emission from the skin of carbon dioxide, which could favor dermatophyte growth (142). A number of medical conditions also appear to predispose patients to chronic dermatophytosis. Most cases of dermatophytosis that persist for long periods in relatively normal persons are caused by Trichophyton rubrum. However, other dermatophytes can cause chronic infections in patients with some underlying disease, such as collagen vascular disease, systemic corticosteroid therapy or Cushings disease, hematologic malignancy, chronic mucocutaneous candidiasis, diabetes mellitus, or atopy (41, 77, 113, 189). Advanced age has also been related to an increased incidence of dermatophytosis (90, 199), and these infections are often asymptomatic (273). Underlying peripheral vascular disease and disorders of keratinization have also been found to be associated with chronic dermatophytosis (113). As discussed below, the chronic infections seem to be related to a higher than expected rate of atopy in the affected individuals. In addition, there is some evidence that susceptibility to chronic dermatophytosis may occur as an inherited trait (114). The best example is tinea imbricata, in which predisposition to the infection has been demonstrated to be transmitted as an autosomal recessive trait (227). Tinea Versicolor Warm climates are strongly associated with an increased incidence of tinea versicolor (167). Since some conjugal cases of tinea versicolor do occur (215), there may be some degree of infectivity of the responsible organism for normal persons. This infection has been reported to be more frequent in steroidtreated patients, those with Cushings disease, those undergoing immunosuppression for renal transplantation, and persons who are severely malnourished (29, 46, 77, 156). Genetic susceptibility has also been postulated for tinea versicolor in that infections in relatives occur at a higher than expected rate (35, 108, 215).
Other Cutaneous Fungal Infections Malassezia folliculitis may develop in immunosuppressed patients (33, 152, 153, 283), although it can also occur in patients with presumably normal immunologic function (9). Experimental infections with Malassezia spp. suggest that certain patients, such as those with seborrheic dermatitis, have a predisposition to this condition (91). Therefore, other host factors, in addition to obvious immunosuppression, may be related to the pathogenesis of this condition. Tinea nigra and both black and white piedra are caused by fungi that are frequently found in the environment. These conditions all seem to be more frequent in warm climates, perhaps because the organisms may be more common there. In addition, Trichosporon beigelii, the cause of white piedra, colonizes a relatively small proportion of hospitalized patients (219). Severely immunocompromised patients may develop life-threatening systemic infections with this organism. NONIMMUNOLOGIC CUTANEOUS DEFENSES Structure of the Skin The physical and chemical structure of the skin represents a form of defense against fungal pathogens. The skin surface is relatively inhospitable to fungal growth because of exposure to UV light, low moisture conditions, and competition from the normal bacterial ora of this site. Therefore, this surface acts as a barrier to the entry of fungi. The stratum corneum is made up of keratin, which most microorganisms cannot use for nutrition. However, C. albicans and the dermatophytes produce keratinases, which hydrolyze this substance and facilitate the growth of these organisms in the stratum corneum itself (188, 266, 284). This very supercial site of infection may protect the infecting organisms from direct contact with at least some of the effector cells of the immune system. Although neutrophils and small numbers of lymphocytes may enter the epidermis, the major inltrates of cell-mediated immune responses are generally conned to the dermis. Keratinization and Epidermal Proliferation The process by which the stratum corneum is continually renewed through keratinization of the epidermal cells may also present a form of defense against organisms infecting this site. The anatomy of the normal skin is shown in Fig. 1. The basal epidermal cells produce continued growth of the epidermis as they undergo continued cell divisions that move the resulting daughter cells (keratinocytes) outward, toward the surface. As they mature these cells lose their nuclei and become attened to form the keratinized cells. This process results in continuous shedding of the stratum corneum, which also may remove infecting fungal microorganisms residing there. Keratinocytes in the periphery of annular dermatophytosis have been found to divide at an increased rate (20). Inammation, including that produced by cell-mediated immune reactions, appears to enhance epidermal proliferation so that rates of transit of epidermal cells towards the stratum corneum are increased (163). A number of studies have demonstrated that epidermal proliferation is important in the defense against supercial mycoses (20, 131, 149, 163, 245). Antifungal Substances Lipids of adult hair contain saturated fatty acids that are fungistatic against Microsporum audouini, formerly a common cause of hair and scalp infections (220). In particular, various
Downloaded from cmr.asm.org by on March 19, 2009
322
WAGNER AND SOHNLE
CLIN. MICROBIOL. REV.
types of sphingosines have recently been found to be active against certain dermatophytes and C. albicans (22). Whereas the sebum of adults may not be signicantly more fungistatic than that from children on a weight-per-weight basis, older individuals appear to produce quantitatively more of this material than do children (151). In addition, fungicidal proteins have been isolated from normal epidermis and could play some role in the defense against cutaneous fungal infections (139). Unsaturated Transferrin In contrast to other fungal pathogens such as C. albicans, M. furfur, and Trichosporun beigelii, the dermatophytic fungi appear to be relatively incapable of causing disseminated disease, except for occasional local abscesses or granulomas in severely immunosuppressed patients. Thus, infections with dermatophytes are generally conned to the keratinized stratum corneum and the cutaneous appendages like the hair and nails. This phenomenon has been related to the presence in the dermis of unsaturated transferrin, which may prevent growth of the organisms in the deeper layers of the skin by competition for iron (143). THE INFLAMMATORY RESPONSE Relationship between Inammation and Chronicity With various kinds of supercial fungal infections there appears to be an inverse relationship between the degree of inammation produced by a particular fungal pathogen and the chronicity of that infection. M. furfur and the anthropophilic dermatophytes, Trichophyton rubrum and Epidermophyton occosum, generally produce little inammation in their cutaneous lesions and frequently cause infections that persist for long periods. On the other hand, many of the geophilic or zoophilic dermatophytes, e.g., Trichophyton verrucosum, produce highly inammatory infections that are usually self-limited. Thus, the local inammatory processes may indeed be involved in the defense against this group of pathogens. Chemotactic Mechanisms Although supercial fungal infections are generally limited to the most supercial layers of the skin or its appendages, some of these infections are highly inammatory. One can observe in the infected skin a variety of gross changes including scaling, vesicles, pustules, annular dermatitis, and severe inammatory reactions (kerions). Microscopically, the lesions are characterized by an accumulation of neutrophils in the infected skin of acute infections or a mononuclear cell inltrate in the dermis of the more chronic ones. The acute inammatory responses may be manifested as epidermal microabscesses. Evidence of epidermal proliferation may also be seen in the chronic infections as hyperkeratosis and parakeratosis. A variety of mechanisms by which inammatory cells are attracted to the sites of cutaneous fungal infections have been described. Trichophyton rubrum and Trichophyton mentagrophytes have both been shown to be capable of activating complement by the alternative pathway to produce chemotactic activity for neutrophils (59, 258). Likewise, C. albicans and M. furfur have been found to activate complement by this pathway (211, 239). Trichophyton mentagrophytes and C. albicans produce low-molecular-weight chemotactic factors analogous to the ones made by growing bacteria (56, 263). On the other hand, Trichophyton rubrum extracts have been shown to destroy chemotactic activity generated from serum (58), perhaps
explaining the minimal degree of inammation usually seen in the lesions produced by this organism. Finally, as discussed more fully below, keratinocytes can generate chemotactic cytokines that could also be responsible for some of the inammation in the lesions of cutaneous fungal infections. Antifungal Mechanisms of Phagocytic Cells Neutrophils and monocytes/macrophages appear to be important in the defense against fungi, including those involved in the cutaneous mycoses. Neutrophils can directly attack pathogens by a variety of microbicidal processes (reviewed in references 218 and 272). Some of these processes depend on microbicidal oxidants, including superoxide, hydrogen peroxide, hypochlorous acid, and monochloramine (106, 269). Alternatively, the neutrophil killing mechanisms may involve nonoxidative granule microbicidal substances, such as cathepsins (62), the defensins (85, 226), bactericidal/permeabilityincreasing protein (279), lactoferrin (5), lysozyme (48), elastase (192), azuricidin (40, 83), and a number of other proteins (118, 177, 234). Most of these substances have been studied primarily for their ability to kill the organisms, although lactoferrin may have both microbistatic and microbicidal effects (6). The neutrophil oxidative mechanisms are capable of killing Trichophyton sp. in vitro (38), suggesting that they could have a role in the defense against dermatophytosis. Macrophages have an additional antimicrobial mechanism by which they can use production of nitric oxide to inhibit growth of ingested fungal pathogens, such as Cryptococcus neoformans (4). This mechanism might be active against the organisms causing supercial fungal infections also. Neutrophils also appear to have signicant growth inhibitory activity in addition to their microbicidal processes. These cells contain large amounts of a calcium and zinc binding protein, called calprotectin, that has potent microbistatic activity against C. albicans and other fungi (174, 185, 250). This protein is released into inammatory exudates as neutrophils die at sites of infection (242) and could supplement other host defenses in the infected skin by controlling growth of C. albicans or other fungi there (174). THE CUTANEOUS IMMUNE SYSTEM Potential Role in Supercial Fungal Infections Since cutaneous fungal infections are more frequent and more severe in patients with immunologic defects, immune responses to fungal antigens would seem to play an important role in the host defense against these infections. Immunologic host defense mechanisms in normal hosts seem to be effective even when the infections are limited to supercial locations such as the stratum corneum (277). A number of studies suggest that the epidermis of the skin represents more than a passive barrier against entry of infecting organisms: i.e., that it also acts as an immunologic organ with some unique elements. In 1983, a hypothesis regarding the skin-associated lymphoid tissue concept, in which the skin acted as an immune surveillance unit (255), was advanced. A variety of cell types are believed to be involved in this cutaneous immune system and will be reviewed below. The mechanisms employed are complex, involving a network of xed or mobile cells interacting either by trafcking of the cells themselves from one site to another or by producing cytokines that inuence the function of other cells. Such skin-initiated immune responses act against a broad spectrum of foreign antigens, including contact allergens, tumors, and transplants, and it is likely that they are also
Downloaded from cmr.asm.org by on March 19, 2009
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS TABLE 2. Major products of Langerhans cells
Product class Productsa
323
active against the fungal pathogens of interest here. Therefore, this system is probably responsible for initiating immune responses that work to eliminate the infecting organisms in the immune host. In addition, such responses may also produce some of the inammation that results in much of the symptomatology of these infections. Cells with Immunologic Potential in the Skin Epidermal Langerhans cells. Langerhans cells, rst discovered by Paul Langerhans in 1868 (252), develop as dendritic cells from bone marrow stem cells and home in to selected tissues. At least ve distinct subsets of dendritic cells have been recognized, including Langerhans cells in epithelial tissues, dendritic cells in peripheral blood or lymph, interdigitating dendritic cells in T-cell-dependent areas of lymphoid tissues, follicular dendritic cells in B-cell-dependent areas, and dermal dendritic cells (19). The bone marrow stem cells are dened as dendritic-Langerhans cell CFU and appear to be a common origin of both macrophages and dendritic cells (155, 212). Peripheral blood dendritic cells account for up to 2% of circulating mononuclear cells and have been shown by transmission electron microscopy to be of three different types (155). Of the three types, the type 2 peripheral blood dendritic cell has an appearance and functional similarity to Langerhans cells, indicating that these cells are precursors of Langerhans cells. Signals for movement into epidermal tissues are not entirely clear but could involve adhesion molecules and lymphokines such as tumor necrosis factor (TNF-) and granulocyte-macrophage colony-stimulating factor (GM-CSF) (43, 155). Epidermal Langerhans cells make up approximately 2 to 5% of the total epidermal cell population (197) and vary in density depending on anatomic location. For example, Langerhans cell density is higher in the epidermis of the head, face, neck, trunk, and limbs than in that of the palms, soles, and genital region (252). These cells have a pronounced dendritic shape and contain rod-shaped organelles of varying length and position, called Birbeck granules, which were rst described in 1961 (26). Birbeck granules are not specic for epidermal Langerhans cells, however, and have been detected in other tissues, including lymph node, thymus, and dermis (252). Freshly isolated Langerhans cells display nonspecic esterase and ATPase activity. They also express a variety of antigenic markers on their surface (reviewed in references 251 and 252). Langerhans cells are the only cells within the normal epidermis to express cluster of differentiation antigen 1a (CD1a), Fc immunoglobulin G (IgG) receptor type II (FcRII/CD32), Fc IgE receptor type I (FcRI), C3bi receptors (CD11b to CD18), and major histocompatibility complex (MHC)-encoded class II antigens. Among these markers, the anti-CD1a labeling appears to be the most reliable one for distinguishing epidermal Langerhans cells. The major products produced by Langerhans cells are summarized in Table 2. The functional signicance of Langerhans cells was rst elucidated in the early 1970s with the observation of the apposition of Langerhans cells and T lymphocytes and the proposal that Langerhans cells might function as antigen-presenting cells (232). Since that time, numerous studies have further elucidated the function of these cells. As antigen-presenting cells, the Langerhans cell would be required to process and present antigens for T-lymphocyte activation. In this regard, there have been a number of observations that support this concept. Similar to other types of antigen-presenting cells, phagocytosis of antigens by Langerhans cells has been demonstrated (248). The Birbeck granules may have an important
Surface markers Adhesion molecules Cytokines
CD1a, FcRII/CD32, FcRI, BP, FcRII/ CD23, CD11b-CD18, CD25, CD40, CD54, CD58, MHC class I, MHC class II LFA-3, ICAM-1, B7 IL-1, IL-6, TNF-
a FcRII/CD32, Fc IgG receptor type II; FcRI, high-afnity receptor for IgE receptor; BP, IgE binding protein; FcRII/CD23, low-afnity receptor for IgE; B7, cell surface molecule B7.
role in the processing of antigens in that there is loss of antigen-processing capacity during culture of these cells, and this loss appears to be associated with the disappearance of Birbeck granules (253). Also, the aspartic proteinase, cathepsin E, appears to play a crucial role in other antigen-processing cells by cleaving proteins and releasing smaller peptides (15), and this enzyme has recently been demonstrated by immunocytochemical stains in the cytoplasmic vesicles (including Birbeck granules) of Langerhans cells (246). Dermal dendritic cells. The dermis contains a population of antigen-presenting cells that constitute one of the ve subsets described above. These cells have dentritic processes, are motile, and express a variety of markers, as shown in Table 3. These include high levels of class II MHC antigen as well as certain proteins involved in adherence of one cell type to another, including intercellular adhesion molecule-1 (ICAM1), leukocyte function antigen-1 (LFA-1), and adhesion molecule B7. All dermal dendritic cells, but not epidermal Langerhans cells, express factor XIIIa in addition to CD1a, although the expression of the latter is weaker than on Langerhans cells. In addition to the above observations, dermal dendritic cells have recently been phenotypically and functionally characterized into three distinct subsets (190). Subset 1 (65 to 70% of total) expresses neither CD1a nor CD14, subset 2 (15 to 20% of total) expresses CD1a but not CD14, and subset 3 (10 to 15% of total) expresses CD14 but not CD1a. The CD14-negative subsets (subsets 1 and 2) are more potent antigen-presenting cells than subset 3 and are as potent as Langerhans cells or blood-derived dendritic cells in allogeneic mixed lymphocyte reactions. These cells may be different from Langerhans cells or they may represent an immature form of these cells (190). In either case, they probably are important in the initiation of immunologic responses in the skin, particularly those involving antigens in the dermis. In this regard it has been shown that in UV B-damaged skin dermal dendritic cells are able to provide an antigen-presenting function and may also confer tolerance (158). However, their role in the afferent phase of immune responses against antigens in the epidermis is unclear at this time. Epidermal T lymphocytes. As discussed above, the lymphoid inltrates characteristic of cutaneous cell-mediated immune responses are generally conned to the dermis of the skin. A
Downloaded from cmr.asm.org by on March 19, 2009
TABLE 3. Major products of dermal dendritic cells
Product class Productsa
Surface markers Adhesion molecules
a
MHC class II, factor XIIIa, subset 1 (CD1a, CD14), subset 2 (CD1a, CD14), subset 3 (CD1a, CD14) ICAM-1, LFA-1, B7
B7, cell surface molecule B7.
324
WAGNER AND SOHNLE TABLE 4. Major products of keratinocytes
Product class Products
a
CLIN. MICROBIOL. REV. TABLE 5. Major products of microvascular endothelial cells
Product class Productsa
Surface markers Adhesion molecules Eicosanoids Cytokines Growth factors Interleukins CSFs
MHC class I, MHC class II ICAM-1, LFA-3, B7 PGE2 bFGF, PDGF AA and B, TGF-, TGF-, TNF- IL-1, IL-3, IL-6, IL-7, IL-8 GM-CSF, G-CSF, M-CSF
Adhesion molecules Cytokines Interleukins CSFs Chemotactic factors
ICAM-1, VCAM-1, P-selectin, E-selectin IL-1, IL-6, IL-8 GM-CSF, G-CSF, M-CSF gro , MCAF
a VCAM, vascular adhesion molecule; G-CSF, granulocyte CSF; M-CSF, macrophage CSF; gro , melanoma growth stimulating factor; MCAF, macrophage chemotactic and activating factor.
a B7, cell surface molecule B7; bFGF, basic broblast growth factor; PDGF, platelet-derived growth factor; PGE2, prostaglandin E2; LTB4, leukotriene B4; G-CSF, granulocyte CSF; M-CSF, macrophage CSF.
majority of the T lymphocytes of normal human skin are located around postcapillary venules beneath the dermal-epidermal junction, whereas less than 5% are present within the epidermis (31). There may be some differences between the two populations of cells. T-lymphocyte antigen receptors are of two types, with most being of the heterodimer phenotype and a small population expressing the heterodimer. In the papillary dermis, up to 80% of T lymphocytes are positive and approximately 7% are positive. In contrast, only 60% of the T lymphocytes in the epidermis are positive, with 18 to 29% being positive. Although these numbers could represent differences in patterns of migration into the epidermis, there does not appear to be a preferential pattern of immigration of the lymphocyte subtypes into the epidermis (31). Sensitized T lymphocytes can be found in the epidermis, with two possibilities accounting for their presence there: (i) through antigenic stimulation of resting T lymphocytes at this site, and (ii) attraction of already sensitized T lymphocytes by chemotactic cytokines. The latter could include members of the interleukin-8 (IL-8) family produced by keratinocytes. Keratinocytes. Keratinocytes not only have an important structural role in forming a physical barrier to foreign antigens and microorganisms but also are important functionally in mediating cutaneous immune reactions. These cells are by far the most numerous in the epidermis, although other cells types, including melanocytes, neuroendocrine Merkel cells, and Langerhans cells, are also found there. The interfollicular epidermis is divided into a series of proliferating units, known as epidermal proliferative units (165, 205). Within an epidermal proliferative unit, there are slow- and fast-cycling basal keratinocytes, which are distinct populations (182, 198) that could possibly have different functions. Other neighboring cells, Langerhans cells, and cells in the dermis appear to have a regulatory effect on keratinocytes and may lead to cellular diversity within the basal layer (198). Keratinocytes secrete a number of soluble factors that are capable of up-regulating and down-regulating immune responses. The major products of these cells are shown in Table 4. Cytokines produced by keratinocytes include a number of growth factors, interleukins, and CSFs (12, 13, 159, 168, 169, 172, 251, 252). The major growth factors produced include basic broblast growth factor, platelet-derived growth factors AA and B, transforming growth factor alpha, transforming growth factor beta, and TNF-. These cells also produce several interleukins, including II-1, IL-3 (also called multi-CSF), IL-6, IL-7, and IL-8, and a number of CSFs, such as GM-CSF, granulocyte CSF, and macrophage CSF. Most of these mediators are not constitutively produced, but their gene expression is up-regulated after a variety of stimuli (251, 252). In addition to the production of soluble factors, keratino-
cytes also express important cell surface molecules, such as MHC and adhesion molecules, suggesting that they may function as immunologic targets. Class I MHC molecules are expressed constitutively on keratinocytes and may represent a target for CD8 cytotoxic T lymphocytes (252). Such a role has been suggested for contact hypersensitivity (267), herpes simplex virus infection (55), graft-versus-host disease and other skin disorders with a lichenoid inltrate, and keratinocyte necrosis (252). Class II MHC molecules are not expressed constitutively but can be induced by gamma interferon (IFN-) (186). Production of the latter is attributed to inltrating T lymphocytes (252). Whereas keratinocytes can express functional peptide-class II complexes, they are apparently unable to process exogenous protein antigens (86). Microvascular endothelial cells. Microvascular endothelial cells are located near the microenvironment where the important cutaneous immunologic reactions occur. Endothelial cells are known to be active participants in a variety of functions, including wound healing, angiogenesis, production of clotting factors, and maintenance of vascular tone. Their role in epidermal immunologic events is not entirely clear, although there is increasing evidence for their participation in this area. Like the keratinocytes, microvascular endothelial cells secrete a number of soluble factors capable of inducing inammation and recruiting leukocytes and express a variety of adhesion molecules. The major products of microvascular endothelial cells are shown in Table 5. The soluble factors include numerous cytokines (IL-1, IL-6, and IL-8), CSFs (granulocyte CSF, macrophage CSF, and GM-CSF), and the chemotactic factors melanoma growth-stimulating factor and macrophage chemotactic and activating factor (193, 260). Adhesion molecules produced by microvascular endothelial cells include ICAM-1, vascular adhesion molecule-1, P-selectin, E-selectin, and others (260). Interactions between Cutaneous Cells Langerhans cells and lymphocytes. After the interaction with a foreign antigen, Langerhans cells migrate to regional lymph nodes, where they interact with T lymphocytes (19). The effect of stimulation of Langerhans cells is to produce enlargement and sheetlike processes (or veils) and loss of Birbeck granules (126). In epidermal cell cultures, ATPase activity and the expression of certain markers (e.g., FcRII) decrease, along with the loss of Birkbeck granules, whereas the surface density of other markers (MHC class I and II antigens, CD25, CD40, CD54, and CD58) increases (251). These cultured Langerhans resemble other lymphoid tissue dendritic cells which are stimulators of T-cell responses (175) and are themselves much better able than resting Langerhans cells to stimulate resting T cells (124). This in vitro phenotypic maturation (reviewed in reference 251) is likely comparable to the in vivo situation inasmuch as increased MHC class II expression con-
Downloaded from cmr.asm.org by on March 19, 2009
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS
325
sistent with acquisition of active antigen-presenting cell function has been observed in contact-sensitized Langerhans cells (54). For proper presentation of antigen and subsequent T-lymphocyte activation and clonal expansion, it is essential to have a proper physical interaction between Langerhans cells and T lymphocytes. The contact between Langerhans cells and the receptor for antigen on T lymphocytes is class II MHC dependent (1). The physical interaction has been shown by electron microscopy to be of two types (49): (i) a glycocalyx-glycocalyx interaction that occurs in relation to protrusions (microvilli) of both cells and may represent the locus for antigen presentation, and (ii) wide and tight areas of close apposition between plasma membranes of both cells. The latter interaction is apparently involved in maintaining adhesiveness between the two cell types. The adhesion molecules LFA-3 and ICAM-1 are expressed on Langerhans cells, whereas the corresponding molecules CD2 and LFA-1 are expressed on T lymphocytes (270). LFA-1 is a member of the integrin family of adhesionpromoting proteins, while LFA-3, ICAM-1, and CD2 are members of the immunoglobulin superfamily. Interaction of LFA-3 with CD2 and ICAM-1 with LFA-1 may enhance Tlymphocyte activation either by providing unique costimulatory signals or by augmenting T-lymphocyteLangerhans cell interaction (126, 271). Following cellular activation, the expression of all four adhesion molecules has been shown to be increased (270). In addition to the antigen-MHC and adhesion interaction, a second signal, such as IL-1, is required for optimal antigenspecic T-lymphocyte clonal expansion. The second signal is likely delivered to the T lymphocyte through the above-described adhesion molecules (233, 270). These molecules therefore serve the purpose of not only physical adhesion but also delivery of stimulatory signals. Langerhans cells themselves can produce IL-1 as well as other cytokines (IL-6 and TNF-) (68, 169, 252). Recent studies indicate that the Langerhans cell-derived IL-1 may play a critical role as the second signal for T-lymphocyte activation (68, 202). Evidence also suggests that the B7/BB-1 (B7) molecule, known to be expressed on cells such as activated monocytes, is a principal costimulator of T lymphocytes. It has also been shown that B7 is expressed on the cell surface of cultured Langerhans cells and that Langerhans cell B7 costimulates the proliferation of resting allogeneic CD4 T lymphocytes (261). The interaction of Langerhans cells and naive CD4 T lymphocytes results in the generation of Th1 effector cells. The latter can release the cytokine IL-2, leading to expansion of the T-lymphocyte clone. When activated hapten-specic CD4 T lymphocytes are stimulated in vitro for several cycles with hapten-modied Langerhans cells, IL-4-secreting Th2 effector cells are produced (111). IL-4 has previously been reported to induce the secretion of IgE in activated B cells (47). Langerhans cells could therefore have a role in atopic reactions when there is constant exposure to antigenic stimulation. Among the surface receptors described above on Langerhans cells is the IgE receptor. Actually, three distinct IgEbinding structures of Langerhans cells have been demonstrated, including the low-afnity receptor for IgE (FcRII/ CD23), the IgE-binding protein (BP), and the high-afnity receptor for IgE (FcRI) (24, 25). IgE molecules play a central role in immediate hypersensitivity reactions, and the description of IgE receptors on Langerhans cells, a well-known participant in T-lymphocyte reactions, demonstrates a unique link between these two types of immune response. Although the functional role of the IgE receptors on Langerhans cells has not been well elucidated, it is possible that they may participate
in defense mechanisms against parasites and/or immune reactions to allergens (25). There is some evidence that Langerhans cells may be involved in the down-regulation of immune responses through their soluble IgG receptors. These cells produce the Fc IgG receptor type II (FcRII/CD32), which may inhibit the binding of immune complexes to FcR cells and therefore participate in suppression of immune responses (7). The fate of Langerhans cells after they stimulate T lymphocytes is unclear. They may serve as targets of natural killer cells (or cytotoxic T cells) and be destroyed after stimulating T lymphocytes. Alternatively, the observation that up to 1% of thoracic duct cells are dendritic would seem to suggest survival and recirculation of these cells (19). Keratinocytes and Langerhans cells. Some of the cytokines produced by keratinocytes (IL-1, GM-CSF, and TNF-) have the potential to inuence the maturation of dendritic cells (217) and therefore could differentially modify the ability of Langerhans cells to respond to antigens. This effect on Langerhans cells may be different in regard to primary or secondary immune responses (94). Therefore, contact hypersensitivity might require not only antigen uptake by Langerhans cells but also antigen-induced cytokine expression by keratinocytes. Keratinocytes have also recently been shown to adhere to Langerhans cells through the expression of E-cadherin on the latter (268). This adhesion may enhance the functional interactions between these two cell types. Keratinocytes and lymphocytes. Although the functional role of class II-expressing keratinocytes in human epidermis is unclear, there is evidence that they may have a role in developing tolerance to certain antigens. When keratinocytes are used as accessory cells, there is a preferential initial production of IL-2 and IL-4 from stimulated lymphocytes and a specic lack of IFN- production. Restimulation induces only IL-4, which is a Th2 cytokine that has been suggested to be important in the maintenance of tolerance to self-antigens (92). Keratinocytes are able to induce nonresponsiveness (tolerance) to subsequent antigen-specic stimulation of T-helper cell clones in vitro (11), and transient hyporesponsiveness to contact allergens has been demonstrated after injection of these keratinocytes into naive mice (87). The potential exists, therefore, for keratinocytes to be involved in selective hyporesponsiveness to microbial antigens in certain cases of chronic cutaneous infections when cell-mediated immune reactions to the infecting organisms appear to be diminished. Keratinocytes, like Langerhans cells, express cell surface adhesion molecules ICAM-1, LFA-3, and B7 (61, 66, 80). ICAM-1 expression is increased by IFN- (66). These adhesion molecules are important, as described above, for appropriate contact of Langerhans cells to T lymphocytes and subsequent T-lymphocyte clonal expansion. In a similar way, these molecules are probably integral to keratinocyte and lymphocyte interactions. Keratinocytes and inammatory cells. Keratinocytes may also enhance inammation through cytokine effects on various kinds of inammatory cells. For instance, macrophage chemotactic and activating factor is produced by keratinocytes in response to IFN- (13). Other cytokines produced by these cells, such as IL-8, are chemotactic for both neutrophils and lymphocytes (12, 169), and keratinocyte-derived IL-7 has been demonstrated to be a growth factor for epidermal T cells (168). In addition to these effects on other cells of the immune system, keratinocytes can themselves respond to keratinocytederived cytokines by dividing and then migrating over a wound surface to form a new epidermis (172). Keratinocytes also generate products of arachidonic acid
Downloaded from cmr.asm.org by on March 19, 2009
326
WAGNER AND SOHNLE
CLIN. MICROBIOL. REV.
metabolism, called eicosanoids, which may inuence inammatory reactions in the skin and whose synthesis appears to be enhanced by IL-1 produced by the keratinocytes themselves (203). One of these products, prostaglandin E2 increases vascular permeability and could promote the inux of inammatory cells into the skin. Prostaglandin E2, however, is primarily involved in down-regulating immune responses, including Tand B-cell proliferation and suppression of IL-1 production by mononuclear phagocytes (93, 252). Another arachadonic acid metabolism product, leukotriene B4, is a potent mediator of leukocyte chemotaxis that may be generated by keratinocytes through an leukotriene A4 hydrolase found in the cytoplasm of these cells (123). Microvascular endothelial cells and lymphocytes. Whereas microvascular endothelial cells have been shown to produce numerous cytokines and adhesion molecules, their specic role in inammatory events is not clear. However, one of the adhesion molecules produced, P-selectin, has been shown to mediate binding of a variety of other cell types, including neutrophils (88), T lymphocytes (180), and natural killer cells (180). This molecule is not constitutively produced but is induced by histamine or thrombin (88). Similarly, E-selectin is produced by microvascular endothelial cells only after induction by cytokines (21) and has been shown to bind memory T lymphocytes (230). ICAM-1 is constitutively expressed on endothelial cells, but the expression can be increased by a number of cytokines, including IL-, TNF-, and IFN- (65, 259). This molecule probably plays a role in binding of lymphocytes to the endothelial cells. The expression of these specic adhesion molecules and the production of proinammatory soluble factors suggest that these microvascular endothelial cells are active participants in cutaneous immunologic trafcking. Their specic involvement probably reects the types of soluble mediators and/or adhesion molecules produced. Initiation and Expression of Cutaneous Immune Responses According to the skin-associated lymphoid tissue concept described in 1983, the skin contains an immune surveillance system consisting of antigen-presenting Langerhans cells, cytokine-producing keratinocytes, epidermotropic T lymphocytes, and draining peripheral lymph nodes. Much work has been done since that time to conrm and expand this concept. In the working hypothesis proposed for mechanisms and pathways involved in these cutaneous immune responses (251, 252), foreign antigens entering the epidermis are rst ingested and processed by Langerhans cells so that the antigenic fragment is complexed to MHC-encoded antigens. Concomitantly, there is antigen-induced enhancement of cytokine production of keratinocytes, leading to activation of the Langerhans cells. Within a short time, the antigen-processing Langerhans cells leave the epidermis, enter the dermal lymphatics, and migrate as veiled cells to the draining lymph nodes. Here they present the antigen-MHC complex on their surface to the proper receptors on resting T lymphocytes and elicit an antigen-specic response in these cells. Through a second signal (IL-1 and/or B7) produced by the Langerhans cells, there is T-lymphocyte stimulation and subsequent clonal expansion. The resulting T-lymphocyte blasts then migrate back to the dermis and epidermis by homing to cytokine-activated microvascular endothelial cells in this area. Once in this location, the T lymphocytes can be further stimulated by other antigen-presenting cells to undergo continued clonal expansion and generation of effector cells that can help to eliminate the pathogenic microorganisms. Other aspects of this immune surveillance mechanism, which are continuing to be elucidated, include the dermal dendritic
cells as antigen-presenting cells, keratinocytes as antigen-presenting cells, and the role of epidermal T lymphocytes in the cutaneous immune response. Each of these cell types may have other less well-dened roles in the above-described immune pathway, or they may play a more or less prominent role against a particular type of infection or other antigenic insult to the skin. The exact role of each cell type in producing immune responses against the organisms causing cutaneous mycoses have not yet been dened, although it is very likely that the immune surveillance mechanism described above is heavily involved in the defense against this type of infection. IMMUNE RESPONSES TO FUNGAL ANTIGENS Cutaneous Candidiasis Inoculation into the skin of viable C. albicans yeast cells in mice has been shown to elicit cell-mediated immune responses to various antigens of this organism (183). Experimental cutaneous candidiasis also sensitizes the infected animals so that a second infection is cleared more rapidly than is the initial one in both guinea pigs (243) and mice (280). Clearance of the organism in these experimental infections appears to be mediated at least in part by a vigorous epidermal proliferative response associated with cell-mediated immune responses to the antigens of the organisms (243, 245). On the other hand, a certain degree of epidermal proliferation occurs in the infected skin of immunosuppressed mice, suggesting that other factors are also involved (244). Depending on environmental conditions, C. albicans can grow in either yeast or lamentous forms, with the latter being postulated to be more invasive. Therefore, it is possible that phase-specic immune responses could develop to antigens that are different between the two phases. Indeed, specic antigens that are not present on yeast cells have been found on the surface of cultured hyphal forms (256). In addition, it has been found that antibodies in sera from some patients with candidiasis react only with germinating C. albicans, whereas those from normal individuals react preferentially with yeast cells (119). Antibody against C. albicans is often found in high titers in human patients with chronic mucocutaneous candidiasis (8, 57, 145, 176, 265, 275). Whereas an occasional patient with this condition lacks anti-candida antibodies in either serum (45, 117) or saliva (160), most seem to have intact humoral immunity to C. albicans (8). Also, the patients who have been reported to have abnormal antibody production appear to be indistinguishable from other patients with chronic mucocutaneous candidiasis, so the signicance of these abnormalities is uncertain. More specic tests of B-cell function may show abnormalities in patients with this condition in that Schick tests have been reported to be abnormal in some patients (36), and in vitro antibody production to candida mannan by cells from patients with active candida infection was found to be decient in another study (64). Patients with the hyper-IgE syndrome often have chronic supercial C. albicans infections along with elevated levels of IgE antibodies to this organism (18, 224). Most noninfected humans have evidence of cell-mediated immunity to C. albicans, as demonstrated by skin testing (75, 228), in vitro lymphocyte stimulation (23, 89), and lymphokine production (23, 241). On the other hand, patients with chronic mucocutaneous candidiasis often demonstrate signicant immunologic defects in cell-mediated immune responses to C. albicans antigens, as discussed below. Even so, the pattern of immunologic abnormalities does not correlate very well with other manifestations of chronic mucocutaneous candidiasis.
Downloaded from cmr.asm.org by on March 19, 2009
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS
327
Also, since some uninfected relatives of patients with this condition also have diminished responsiveness to Candida antigens (221), this abnormality cannot entirely explain why the patients are susceptible to the fungal infections. Dermatophytosis Most of the early animal work with experimental dermatophytosis involved guinea pigs and generally demonstrated that some kind of immunity, either local or systemic, resulted from a previous infection. In one study generalized immunity was demonstrated after experimental dermatophyte infections in that the course of a second infection was accelerated at a different site (104). In contrast, other workers found that the accelerated response to a second infection was greatest at the site of the rst infection, suggesting some form of local immunity (30, 60, 207). Memory cells in the healed skin at the site of a rst infection have been demonstrated after experimental Trichophyton mentagrophytes infectious in guinea pigs (207). In rats and mice, the success of experimental dermatophyte inoculation appears to be dependent on the stage of hair and skin growth cycles, so that immunity to reinfection may not be as easy to demonstrate as it is with guinea pigs (150). In cattle, a previous infection appears to afford partial immunity to a second infection at the same site as well as at different sites (161). Because dermatophytosis in cattle is an important economic problem in some countries, and because these infections represent potential sources of human dermatophytosis, attempts have been made to produce vaccines against Trichophyton verrucosum for veterinary use. One of these, a live vaccine (LTF130) based on a less virulent strain of the organism, appears to show considerable promise for controlling infections with wildtype strains of this organism (225). The ndings concerning immunity to experimental dermatophytic infections in humans parallel those in animals in that there is generally some indication of increased resistance, even though it may be only local in nature (60, 104, 130, 149). Although the results of various studies on experimental dermatophyte infections in humans have differed somewhat from one to another, in general it appears that this immunity is not complete and is probably less than that found in animals (96, 154). The cell wall of the dermatophytes is made up primarily of chitin and glucan in addition to the glycopeptides which represent the major antigens of these organisms. The dermatophytes, like other fungi, have a very complicated antigenic makeup. Antigenic substances of the dermatophytes may be glycopeptides, peptides, or carbohydrates, and the individual types of antigens may elicit different types of responses (14, 184). In addition, the keratinase of Trichophyton mentagrophytes may be an important antigen not only because it elicits strong delayed hypersensitivity responses but also because antibodies that inhibit the proteolytic activity of this enzyme are produced (97). Extracts of various dermatophyte species have usually been found to contain a mixture of antigens that are either species specic or broadly cross-reactive with those of other dermatophytes (98, 101) or those of other fungi (213). This phenomenon may relate to the susceptibility of atopic patients to chronic dermatophytosis because these patients may develop immediate hypersensitivity to airborne molds that cross-reacts with the dermatophyte antigens, and this immediate hypersensitivity may later interfere with the development of delayed responses to these antigens (127, 133). Cross-reactivity between penicillin and dermatophyte antigens has also been postulated as a possible cause of penicillin hypersensitivity in pa-
tients who have never received this drug before (201). Similar cross-reactivity between the antigens of Trichophyton rubrum and those of epidermal cells could also be a factor in the development of inammatory responses in dermatophytosis (120, 200). Even though dermatophyte infections are very supercial in location, they do appear to sensitize the host to the antigens of the infecting organisms. In fact, low levels of antibody against Trichophyton rubrum have been found in uninfected humans by using an enzyme-linked immunosorbent assay (ELISA), although it is possible that such antibodies represent cross-reactivity with other microorganisms (240). Also, rabbits inoculated with Trichophyton verrucosum have been shown to develop precipitins against extracts of the organisms; however, the titers of these antibodies do not seem to correlate with susceptibility to reinfection (51). Complement-xing antibodies to dermatophyte antigens have been found in the sera of experimentally infected guinea pigs and naturally infected horses (32). Humoral immunity has been demonstrated in human dermatophytosis, using a variety of techniques such as ELISAs, complement xation, immunodiffusion, and agglutination. Although precipitins are produced relatively infrequently (99, 115), more sensitive methods may show antibody against the infecting organism in larger numbers of patients with dermatophytosis (100, 137, 196). However, whereas antibody titers to extracts of the organisms have been shown to generally be elevated in patients with dermatophytosis, some of these patients may have low titers that are not different from those in control subjects (99, 137). Immediate hypersensitivity to dermatophyte antigens has been well documented in dermatophytosis. In fact, this process may be involved in the pathogenesis of this condition, as suggested from evidence that this type of response may interfere with the development of a protective delayed hypersensitivity response. In patients with dermatophytosis, both immediate hypersensitivity to dermatophyte antigens and a higher than expected incidence of atopy have been found in a number of studies (113, 125, 129). It is not clear if chronic dermatophytosis stimulates IgE production or if this condition tends to develop in persons who are already atopic (127). A frequent pattern seen in these patients is the presence of immediate, but not delayed, hypersensitivity to trichophytin (110, 112, 122, 134). However, many patients with chronic dermatophytosis neither are atopic nor manifest immediate hypersensitivity to trichophytin, indicating that other factors must also be involved in producing susceptibility to this type of infection. Also, in one patient with Cushings disease and widespread, chronic dermatophytosis, treatment of the underlying disease by adrenalectomy resulted in restoration of a positive delayed trichophytin skin test and appeared to improve the patients cutaneous infections, even though the patient continued to manifest strong immediate hypersensitivity to trichophyton antigens (69). Therefore, it would appear in this case that the immediate hypersensitivity reactions were unrelated to decient host defense in the patient before treatment. Delayed hypersensitivity responses to intradermal injections of trichophytin are fairly common in the normal population (107, 194, 281). Because trichophytin can be obtained commercially, it can be used as one of a battery of delayed hypersensitivity skin tests to assess immunological competence. However, since only 30% or so of normal subjects will have a positive delayed response to this antigen, it is not particularly useful for this purpose. Although these responses are probably due to prior episodes of self-limited dermatophytosis, it is also
Downloaded from cmr.asm.org by on March 19, 2009
328
WAGNER AND SOHNLE
CLIN. MICROBIOL. REV.
possible that cross-reactivity with another organism is responsible. Experimental dermatophyte infections in animals do appear to result in cell-mediated immunity to the antigens of the infecting organism (53, 103, 157). In guinea pigs with experimental Trichophyton mentagrophytes infections, maximal erythema in the infected skin has been demonstrated to occur at the time the animals developed cell-mediated immunity to trichophytin, as manifested by delayed hypersensitivity skin test responses and positive in vitro lymphocyte transformation responses (157). Similar ndings have been reported in cattle experimentally infected with Trichophyton verrucosum (162). In the latter system delayed hypersensitivity reactions in the infected skin appeared to promote clearance of the infection by increasing the rate of desquamation of the stratum corneum (163). In humans, the type and duration of dermatophytosis appear to be important factors in determining whether or not delayed hypersensitivity to trichophytin will be present. Positive delayed hypersensitivity responses to trichophytin have been found to be more frequent in patients with acute dermatophytosis caused by Trichophyton mentagrophytes than in patients with chronic infections caused by Trichophyton rubrum (110, 129, 135). In children with tinea capitis, positive delayed skin tests to trichophytin were found in one study to be present in 15 of 16 of those with highly inammatory infections (kerions) but in none of 36 with minimally inammatory (black dot) infections (210). Patients with chronic dermatophytosis are generally fairly healthy and have been found to have only a mild depression in their ability to develop delayed hypersensitivity skin test responses to antigens unrelated to trichophytin (247). Cell-mediated immunity to trichophytin appears to be important in the defense against dermatophytosis in that studies of experimental infections in humans have demonstrated that patients with positive delayed trichophytin skin tests are more resistant to inoculation with Trichophyton mentagrophytes than are those with negative skin tests (132). Cell-mediated immunity to dermatophyte antigens has been demonstrated by in vitro lymphocyte transformation assays in both animals and humans. Guinea pigs with experimental Trichophyton mentagrophytes infections develop this type of response approximately 9 to 11 days after inoculation with the fungus (103, 157). In human patients with dermatophytosis, positive in vitro lymphocyte transformation to trichophytin has also been found in a number of studies (110, 115, 136, 249, 257). The in vitro response usually correlates with the presence of a positive delayed skin test to trichophytin, although a few patients with chronic Trichophyton rubrum infections have been found to have negative skin tests along with positive in vitro lymphocyte transformation responses (136). This nding suggests some kind of local suppression of the skin test response, as discussed below. The cellular inltrates of dermatophytosis have been analyzed, and the majority of inltrating cells have been found to be helper T lymphocytes (262). Tinea Versicolor and Other Supercial Fungal Infections Serum antibody to M. furfur has been found in a large percentage of normal persons who do not show evidence of infection with this organism (3, 57, 70, 240). This antibody is predominantly of the IgG class, although there are also some IgM and IgA antibodies (240). Titers have been shown to be lower in children under 5 years of age, perhaps because they are less likely to be colonized with M. furfur and therefore not yet sensitized (17). In elderly individuals the titers have also been found to be reduced (16, 240), and this decrease can perhaps
be related to decreased numbers of the organism on the skin of older individuals (16). Antibody titers have also been compared in homosexual men who were either seropositive or seronegative for the human immunodeciency virus, but the titers were not found to be different between the two groups (109). Humoral responses to M. furfur have been shown to be either slightly elevated in patients with tinea versicolor compared with controls in one study (57) or approximately equivalent in another study (73). In malassezia folliculitis, IgG antibodies against this organism were found to be markedly higher in the patients than in healthy subjects, although immediate hypersensitivity to the antigens of this organism seemed to be lacking when prick tests were done with an M. furfur extract (16). Antibody to trichosporon antigens has been shown by an immunoblot technique to be present not only in patients with invasive Trichosporon beigelii infections but also in uninfected controls (170). In addition, both IgG and IgA antibodies against this organism have been demonstrated by an indirect immunouorescence technique in the vaginal washings from three women with asymptomatic carriage of Trichosporon beigeli (209). In that study, washings from women having vaginitis caused by other organisms generally had low titers against trichosporon. Trichosporon also has been shown to share antigens with Cryptococcus neoformans, and the latex agglutination tests for cryptococcal antigen may be positive in patients with disseminated trichosporon infections (173). Cell-mediated immunity to malassezia antigens has been demonstrated by lymphocyte transformation and lymphokine assays in a majority of uninfected human subjects, whereas tinea versicolor patients appear to have decient lymphokine production and weaker lymphocyte transformation responses to these antigens (236, 238). On the other hand, proportions of B and T lymphocytes, subsets of T lymphocytes, and lymphocyte transformation responses against nonspecic mitogens and unrelated antigens appear to be normal in tinea versicolor patients (223, 236). MECHANISMS OF IMMUNOLOGIC DEFECTS Cutaneous Candidiasis In human patients with chronic mucocutaneous candidiasis the most common immunologic abnormalities found are defects in cell-mediated immunity (76, 117, 145, 147, 275). These defects fall into three general groups: (i) anergy to all antigens tested, (ii) unresponsiveness to candida antigens only, and (c) normal responses to all antigens, including those from candida. For example, in one study, 10 of 26 patients appeared to have normal cell-mediated immunity to candida antigens (275). However, other patients appear to have signicant abnormalities in lymphocyte function, with some having complete anergy to a battery of recall antigens and negative in vitro lymphocyte proliferation responses to mitogens and all antigens (147). Serum inhibitors appear to account for some of the immunologic defects in patients with chronic mucocutaneous candidiasis (34, 148, 274, 275). Sometimes the defects disappear after antifungal therapy (63, 146, 274). Parenteral administration of viable C. albicans yeast cells or extracts of this organism to experimental animals can result in suppression of cell-mediated immunity (42, 214, 216). Carbohydrate antigens from C. albicans, primarily mannans, have been shown to persist in the sera of patients with chronic mucocutaneous candidiasis and suppress lymphocyte proliferation responses of cells from con-
Downloaded from cmr.asm.org by on March 19, 2009
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS
329
trol subjects (78). Defective handling of mannan by monocytes from patients with chronic mucocutaneous candidiasis has been postulated as the reason why this substance accumulates in the sera of these patients (79). Mannan-derived oligosaccharides from C. albicans can inhibit in vitro lymphocyte proliferation induced by candida antigens (204). Therefore, catabolism of mannan in vivo may generate immunoinhibitory oligosaccharides that cause the defects in cell-mediated immunity in some patients with chronic mucocutaneous candidiasis. However, other patients with this syndrome probably have immunologic abnormalities due to other mechanisms, and still others have no demonstrable immunologic abnormalities at all and may be susceptible to chronic supercial C. albicans infections for other reasons. Dermatophytosis Suppression of lymphocyte blastogenic responses has been related to potentially immunosuppressive serum factors in acute Trichophyton mentagrophytes infections produced experimentally in animals (37, 102). Studies with human patients also suggest that serum factors may be involved in suppression of cell-mediated immunity to fungal antigens in chronic dermatophytosis (39, 229, 278). A mannan component of Trichophyton rubrum has been shown to be immunosuppressive of in vitro lymphocyte function (27), perhaps because it preferentially binds to monocytes (95). It has also been suggested that the lack of inammation in Trichophyton rubrum infections may be due to dermatophyte-derived lymphocyte inhibitory factors acting locally rather than systemically (171). As discussed above, local antagonism between immediate and delayed hypersensitivity is another possible mechanism of immunosuppression in dermatophytosis (128). Most patients with chronic dermatophytosis have relatively normal cell-mediated immunity to nonspecic mitogens and antigens other than trichophytin (110, 115, 122, 247), indicating that they are relatively intact immunologically. Subjects with immediate hypersensitivity to trichophytin have been found to be more easily infected experimentally with Trichophyton mentagrophytes than are those without this type of response (132). Also, production of an immediate skin test response to trichophytin by passive transfer has been shown to block delayed reactions in patients who previously had only the delayed response (166). Delayed hypersensitivity reactions to trichophytin could be uncovered in some patients with chronic dermatophytosis by suppressing immediate reactions to this antigen via injections of antihistamines into the site (131). Therefore, it is possible that an IgE response in some patients with chronic dermatophytosis may inhibit the development of protective cell-mediated immune responses to dermatophyte antigens. Tinea Versicolor Like patients with chronic dermatophytosis, most patients with tinea versicolor have relatively normal immune systems and respond well against nonspecic mitogens and nonmalassezia antigens. The cells inltrating the infected skin of patients with tinea versicolor and malassezia folliculitis have been characterized as predominantly helper-inducer rather than suppressor-cytotoxic cells by staining with monoclonal antibodies (73, 223). Tinea versicolor patients have been found to have weaker lymphokine responses (236) and a statistically signicant reduction in lymphocyte transformation responses to malassezia antigens compared with uninfected subjects (238); the diminished blastogenic response appears to be related to a decrease in the number of cells initially responding to this antigen (238).
As a possible explanation for the relatively modest degree of inammation present in the lesions of tinea versicolor, the relative antigenicity of this organism has been compared with that of C. albicans, which produces highly inammatory lesions, and found to be markedly less by a number of assays (237). Therefore, two possible reasons for the minimal inammation in tinea versicolor are a reduction in the responsiveness of lymphokine-producing cells of these patients to malassezia antigens and a relative lack of antigenic material in the organism itself. IMMUNOLOGIC THERAPY Cutaneous Candidiasis A variety of treatments aimed at restoring immune function have been tried in patients with chronic mucocutaneous candidiasis (76, 147); these treatments have involved thymic transplantation, thymic hormone replacement, infusion of leukocytes from normal donors, bone marrow transplantation, and administration of transfer factor from candida skin test-positive donors. Of these various therapies, the combination of transfer factor administration with specic antifungal therapy probably has given the best results (147). However, the mechanism of action of transfer factor remains undened, and its use in restoring immunologic function is still considered experimental. At present, antifungal therapy with oral azole agents remains the standard therapy for chronic mucocutaneous candidiasis. Even so, this therapy is unsatisfactory for some patients because of intolerance or the development of resistant C. albicans strains. Therefore, some form of immunological reconstitution might be benecial. A variety of immunomodulatory agents, including interleukins, interferons, CSFs, monoclonal antibodies, and synthetic immunomodulators, have been used to treat other conditions associated with depressed immunological function (84), and it is possible that in the future some of these agents may prove useful as adjunctive therapy for patients with chronic mucocutaneous candidiasis or other chronic supercial fungal infections. Dermatophytosis A useful live vaccine (LTF-130) against Trichophyton verrucosum, the major cause of cattle ringworm, has been developed and has been successful in reducing the infections in cattle herds in the Soviet Union and some European countries (225). However, the use of vaccines against this type of infection is much more difcult in humans. Dermatophytosis has generally not been considered a serious enough disease to warrant largescale immunization programs in children. Therefore, the types of human patients who have been given vaccine in the past include those with intractable, chronic dermatophytosis and those with signicant dermatophytid reactions. This type of therapy has not been particularly effective and has been supplanted in recent years by the use of antifungal drugs. The situation in patients with chronic dermatophytosis is quite different from that in animals that have never been infected with a dermatophyte or sensitized to the antigens of these organisms. In the human patients who are infected at the time of treatment, an inadequate immune response is most likely due to dysfunction of some element of the immune system rather than to lack of primary exposure to the antigens involved; this type of immune dysfunction would generally not be expected to respond to additional amounts of the antigen. Attempts have also been made to treat dermatophytid reactions with
Downloaded from cmr.asm.org by on March 19, 2009
330
WAGNER AND SOHNLE
CLIN. MICROBIOL. REV.
as effectors of macrophage-mediated cytostasis. Infect. Immun. 59:2291 2296. Arnold, R. R., M. Brewer, and J. J. Gauthier. 1980. Bactericidal activity of human lactoferrin: sensitivity of a variety of microorganisms. Infect. Immun. 23:893898. Arnold, R. R., J. E. Russell, W. J. Champion, and J. J. Gauthier. 1981. Bactericidal activity of human lactoferrin: inuence of physical conditions and metabolic state of the target microorganism. Infect. Immun. 32:655 660. Astier, A., H. de la Salle, C. De La Salle, T. Bieber, M. E. Esposito-Farese, M. Freund, and J. P. Cazenave. 1994. Human epidermal Langerhans cells secrete a soluble receptor for IgG, (Fc gamma R II/CD32), that inhibits the binding of immune complexes to Fc gamma R cells. J. Immunol. 152: 201212. Axelsen, N. H., C. H. Kirkpatrick, and R. H. Buckley. 1974. Precipitins to Candida albicans in chronic mucocutaneous candidiasis studied by crossed immunoelectrophoresis with intermediate gels. Clin. Exp. Immunol. 17: 385394. Back, O., J. Faergemann, and R. Hornqvist. 1985. Pityrosporum folliculitis: a common disease of the young and middle-aged. J. Am. Acad. Dermatol. 12:5661. Baer, R. L., S. A. Rosenthal, and D. Furnari. 1955. Survival of dermatophytes applied on the feet. J. Invest. Dermatol. 24:619622. Bal, V., A. McIndoe, G. Denton, D. Hudson, G. Lombardi, J. Lamb, and R. Lechler. 1990. Antigen presentation by keratinocytes induces tolerance in human T cells. Eur. J. Immunol. 20:18931897. Barker, J. N. W. N., M. L. Jones, R. S. Mitra, E. Crockett-Torabe, J. C. Fantone, S. L. Kunkel, J. S. Warren, V. M. Dixit, and B. J. Nickoloff. 1991. Modulation of keratinocyte-derived interleukin-8 which is chemotactic for neutrophils and T lymphocytes. Am. J. Pathol. 139:869876. Barker, J. N. W. N., M. L. Jones, C. L. Swenson, V. Sarma, R. S. Mitra, P. A. Ward, K. J. Johnson, J. C. Fantone, V. M. Dixit, and B. J. Nickoloff. 1991. Monocyte chemotaxis and activating factor production by keratinocytes in response to IFN-. J. Immunol. 146:11921197. Barker, S. A., C. N. D. Cruickshank, J. H. Morris, and S. R. Wood. 1962. The isolation of trichophytin glycopeptide and its structure in relationship to the immediate and delayed hypersensitivity reactions. Immunology 5:627632. Bennet, K., R. Levine, J. S. Ellis, R. J. Peanaski, I. M. Samloff, J. Kay, and B. M. Chain. 1992. Antigen processing for presentation by class II major histocompatibility complex requires cleavage by cathepsin E. Eur. J. Immunol. 22:15191524. Bergbrant, I. M., and J. Faergemann. 1988. Variations of Pityrosporum orbiculare in middle-aged and elderly individuals. Acta Dermato Venereol. 68:537540. Bergbrant, I. M., S. Johansson, D. Robbins, A. Scheynius, J. Faergemann, and T. Soderstrom. 1991. An immunological study in patients with seborrheic dermatitis. Clin. Exp. Dermatol. 16:331338. Berger, M., C. H. Kirkpatrick, P. K. Goldsmith, and J. I. Gallin. 1980. IgE antibodies to Staphylococcus aureus and Candida albicans in patients with the syndrome of hyperimmunoglobulin E and recurrent infections. J. Immunol. 125:24372443. Bergstresser, P. R., P. D. Cruz, Jr., J. Y. Niederkorn, and A. Takashima. 1992. Third International Workshop on Langerhans cells: discussion overview. J. Invest. Dermatol. 99:1S4S. Berk, S. H., N. S. Penneys, and G. D. Weinstein. 1976. Epidermal activity in annular dermatophytosis. Arch. Dermatol. 112:485488. Bevilacqua, M. P., J. S. Pober, D. L. Mendrick, R. S. Cotran, and M. A. Gimbrone, Jr. 1987. Identication of an inducible endothelial-leukocyte adhesion molecule. Proc. Natl. Acad. Sci. USA 84:92389242. Bibel, D. J., R. Aly, S. Shah, and H. R. Shineeld. 1993. Sphingosines: antimicrobial barriers of the skin. Acta Dermato Venereol. 73:407411. Bice, D. E., M. Lopez, H. Rothschild, and J. Salvaggio. 1974. Comparison of Candida delayed hypersensitivity skin test size with lymphocyte transformation, migration inhibitory factor production and antibody titer. Int. Arch. Allergy Appl. Immunol. 47:5462. Bieber, T. 1992. IgE-binding molecules on human Langerhans cells. Acta Dermato Venereol. Suppl. 176:5457. Bieber, T., H. de la Salle, C. de la Salle, D. Hanau, and A. Wollenberg. 1992. Expression of the high afnity receptor for IgE (FcR1) on human Langerhans cells: The end of a dogma. J. Invest. Dermatol. 99:10S11S. Birbeck, M. S., A. S. Breathnach, and J. D. Everall. 1961. An electron microscope study of basal melanocytes and high-level clear cells (Langerhans cells) in vitiligo. J. Invest. Dermatol. 37:5164. Blake, J. S., M. V. Dahl, M. J. Herron, and R. D. Nelson. 1991. An immunoinhibitory cell wall glycoprotein (mannan) from Trichophyton rubrum. J. Invest. Dermatol. 96:657661. Blank, H., D. Taplin, and N. Zaias. 1969. Cutaneous Trichophyton mentagrophytes infections in Vietnam. Arch. Dermatol. 99:135144. Boardman, C. R., and F. D. Malkinson. 1962. Tinea versicolor in steroidtreated patients. Arch. Dermatol. 85:8492. Bonk, A. F., L. Friedman, and V. J. Derbes. 1962. Experimental dermato-
trichophytin immunotherapy. Because patients with these reactions usually have strong delayed hypersensitivity to dermatophyte antigens, attempts to desensitize them by injections of trichophytin make some sense immunologically. However, as with therapy of the infection itself, dermatophytid eruptions are probably best treated with appropriate antifungal therapy. Other immunomodulatory methods might have some potential in the treatment of patients with chronic and intractable dermatophytosis. Suppression of immediate reactions to dermatophyte antigens could possibly benet this type of patient, provided the immediate reactions were indeed suppressing a protective delayed hypersensitivity response. Treatment with oral cimetidine did partially suppress immediate hypersensitivity to trichophytin in patients with chronic dermatophytosis but did not restore the delayed hypersensitivity responses (112). Also, because the infection itself may directly suppress cellmediated immunity to the antigens of the infecting organism, it is possible that successful antifungal therapy by itself could restore the protective immunological responses and perhaps prevent future relapses. Finally, specic immunological therapy to restore immune function in patients with chronic dermatophytosis might be benecial in those in whom antifungal therapy is either ineffective or not tolerated. However, as with chronic mucocutaneous candidiasis, such immunological therapy is experimental at the present time. Tinea Versicolor Because of the lack of serious effects of this infection and the high degree of sensitivity of M. furfur to available antifungal agents, it would seem unlikely that immunological therapy would be of much benet to patients with this condition. SUMMARY AND CONCLUSIONS Predispositions to the supercial mycoses include warmth and moisture, natural or iatrogenic immunosuppression, and perhaps some degree of inherited susceptibility. Some of these infections elicit a greater inammatory response than others, and the noninammatory ones are generally more chronic. The immune system is involved in the defense against these infections, and cell-mediated immunity appears to be particularly important. The mechanisms involved in generating immunologic reactions in the skin are complex, with epidermal Langerhans cells, other dendritic cells, lymphocytes, microvascular endothelial cells, and the keratinocytes themselves all participating in one way or another. A variety of defects in the immunologic responses to the supercial mycoses have been described. In some cases the defects may be preexistent, whereas in others the infection itself may interfere with protective cell-mediated immune responses against the organisms. A number of different mechanisms may underlie these immunologic defects and lead to the development of chronic supercial fungal infections in individual patients. Although the immunologic defects appear to be involved in the chronicity of certain types of cutaneous fungal infections, treatment of these defects remains experimental at the present time.
1. 2. 3. 4. REFERENCES Aiba, S., and S. I. Katz. 1991. The ability of cultured Langerhans cells to process and present protein antigens is MHC-dependent. J. Immunol. 146: 24792487. Ajello, L. 1974. Natural history of the dermatophytes and related fungi. Mycopathol. Mycol. Appl. 53:93110. Alexander, S. 1967. Loss of hair and dandruff. Br. J. Dermatol. 79:549 552. Alspaugh, J. A., and D. L. Granger. 1991. Inhibition of Cryptococcus neoformans replication by nitrogen oxides supports the role of these molecules
5. 6.
7.
8.
9. 10. 11. 12.
Downloaded from cmr.asm.org by on March 19, 2009
13.
14.
15.
16. 17. 18.
19.
20. 21.
22. 23.
24. 25.
26.
27.
28. 29. 30.
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS
331
phytosis. J. Invest. Dermatol. 39:281286. 31. Bos, J. D., M. B. M. Teunissen, I. Cairo, S. R. Krieg, M. L. Kapsenberg, P. K. Das, and J. Borst. 1990. T-cell receptor bearing cells in normal human skin. J. Invest. Dermatol. 94:3742. 32. Brocq-Rousseu, P., A. Urbain, and J. Barotte. 1927. Etude des teignes du cheval et de limmunite dans les teignes experimentales. Ann. Inst. Pasteur Paris 41:513551. 33. Bull, J. A., L. A. Lum, J. G. Caya, C. R. Chitambar, P. S. Ritch, T. Anderson, and R. C. Ash. 1988. Pityrosporum folliculitis after bone marrow transplantationclinical observations in ve patients. Ann. Intern. Med. 108:560563. 34. Burford-Mason, A. P., R. C. Matthews, and J. R. B. Williams. 1987. Transient abrogation of immunosuppression in a patient with chronic mucocutaneous candidiasis following vaccination with Candida albicans. J. Infect. 14:147157. 35. Burke, R. C. 1961. Tinea versicolor: susceptibility factors and experimental infection in human beings. J. Invest. Dermatol. 36:389401. 36. Cahill, L. T., E. Ainbender, and P. R. Glade. 1974. Chronic mucocutaneous candidiasis: T cell deciency associated with B cell dysfunction in man. Cell. Immunol. 14:215225. 37. Calderon, R. A. 1989. Immunoregulation of dermatophytosis. Crit. Rev. Microbiol. 16:339368. 38. Calderon, R. A., and R. J. Hay. 1987. Fungicidal activity of human neutrophils and monocytes on dermatophytic fungi, Trichophyton quinckeanum and Trichophyton rubrum. Immunology 61:289295. 39. Calderon, R. A., R. J. Hay, and G. I. Shennan. 1987. Circulating antigens and antibodies in human and mouse dermatophytosis: use of monoclonal antibody to phosphorylcholine-like epitopes. J. Gen. Microbiol. 133:2699 2705. 40. Campanelli, D., P. A. Detmers, C. F. Nathan, and J. E. Gabay. 1990. Azuricidin and a homologous serine protease from neutrophils. Differential antimicrobial and proteolytic properties. J. Clin. Invest. 85:904915. 41. Canizares, O., H. Shatin, and A. J. Kellert. 1959. Cushings syndrome and dermatomycosis. Arch. Dermatol. 80:705712. 42. Carrow, E. W., and J. E. Domer. 1985. Immunoregulation in experimental murine candidiasis: specic suppression induced by Candida albicans cell wall glycoprotein. Infect. Immun. 49:172181. 43. Caux, C., C. Dezutter-Dambuyant, D. Schmitt, and J. Banchereau. 1992. GM-CSF and TNF- cooperate in the generation of dendritic Langerhans cells. Nature (London) 360:258261. 44. Chappler, R. R., H. I. Maibach, M. K. A. Conant, and R. Aly. 1978. Mucocutaneous candidiasis or mucocutaneous microbiosis. JAMA 239: 428429. 45. Chipps, B. E., F. T. Saulsbury, S. H. Hsu, W. T. Hughes, and J. A. Winkelstein. 1979. Non-candidal infections in children with chronic mucocutaneous candidiasis. Johns Hopkins Med. J. 144:175179. 46. Chugh, K. S., S. C. Sharma, V. Singh, V. Sakhuja, V. Jha, and K. L. Gupta. 1994. Spectrum of dermatological lesions in renal allograft recipients in a tropical environment. Dermatology 188:108112. 47. Coffman, R. L., J. Ohara, M. Bond, J. Carty, A. Zlotnik, and W. E. Paul. 1986. B cell stimulatory factor 1 enhances the IgE-response of lipopolysaccharide-activated B cells. J. Immunol. 136:45384545. 48. Collins, M. S., and D. Pappagianis. 1974. Inhibition by lysozyme of growth of the spherule phase of Coccidioides immitis in vitro. Infect. Immun. 10:616623. 49. Concha, M., A. Vidal, G. Garces, C. D. Figueroa, and I. Caorsi. 1993. Physical interaction between Langerhans cells and T lymphocytes during antigen presentation in vitro. J. Invest. Dermatol. 100:429434. 50. Cornbleet, T. 1926. Cultures from the skin of apparently normal feet. Arch. Dermatol. 13:670671. 51. Cox, W. A., and J. Moore. 1968. Experimental Trichophyton verrucosum infections in laboratory animals. J. Comp. Pathol. 78:3541. 52. Crosby, D. L., T. G. Berger, J. T. Woosley, and S. D. Resnick. 1991. Dermatophytosis mimicking Kaposis sarcoma in human immunodeciency virus disease. Dermatologica 182:135137. 53. Cruickshank, C. N. D., M. D. Trotter, and S. R. Wood. 1960. Studies on trichophytin sensitivity. J. Invest. Dermatol. 35:219223. 54. Cumberbatch, M., S. J. Gould, S. W. Peters, and I. Kimber. 1991. MHC class II expression by Langerhans cells and lymph node dendritic cells: possible evidence for maturation of Langerhans cells following contact sensitization. Immunology 74:414419. 55. Cunningham, A. L., and J. R. Noble. 1989. Role of keratinocytes in human recurrent herpetic lesions. Ability to present herpes simplex virus antigen and act as targets for T-lymphocyte cytotoxicity in vitro. J. Clin. Invest. 83:490496. 56. Cutler, J. E. 1977. Chemotactic factor produced by Candida albicans. Infect. Immun. 18:568573. 57. DaMert, G. J., C. H. Kirkpatrick, and P. G. Sohnle. 1980. Comparison of antibody responses in chronic mucocutaneous candidiasis and tinea versicolor. Int. Arch. Allergy Appl. Immunol. 63:97104. 58. Davies, R. R., and F. Zaini. 1984. Enzymatic activities of Trichophyton rubrum and the chemotaxis of polymorphonuclear leucocytes. Sabouraudia 22:235241.
59. Davies, R. R., and F. Zaini. 1984. Trichophyton rubrum and the chemotaxis of polymorphonuclear leucocytes. Sabouraudia 22:6571. 60. DeLamater, E. D., and R. W. Benham. 1938. Experimental studies with the dermatophytes. II. Immunity and hypersensitivity produced in laboratory animals. J. Invest. Dermatol. 1:469488. 61. DePanlis, G. D., G. C. Manara, C. Ferrari, and C. Torresani. 1991. Adhesion molecules on the plasma membrane of epidermal cells. III. Keratinocytes and Langerhans cells constitutively express the lymphocyte function-associated antigen 3. J. Invest. Dermatol. 96:512517. 62. Drazin, R. E., and R. I. Lehrer. 1977. Fungicidal properties of a chymotrypsin-like cationic protein from human neutrophils: adsorption to Candida parapsilosis. Infect. Immun. 17:382388. 63. Drouhet, E., and B. Dupont. 1980. Chronic mucocutaneous candidiasis and other supercial and systemic mycoses successfully treated with ketoconazole. Rev. Infect. Dis. 2:606619. 64. Durandy, A., A. Fischer, F. Le Deist, E. Drouhet, and C. Griscelli. 1987. Mannan-specic and mannan-induced T-cell suppressive activity in patients with chronic mucocutaneous candidiasis. J. Clin. Immunol. 7:400409. 65. Dustin, M. L., R. Rothlein, A. K. Bhan, C. A. Dinarello, and T. A. Springer. 1986. Induction by IL-1 and interferon gamma: tissue distribution, biochemistry, and function of a natural adherence molecule (ICAM-1). J. Immunol. 137:245254. 66. Dustin, M. L., K. H. Singer, D. T. Tuck, and T. A. Springer. 1988. Adhesion of T-lymphoblasts to epidermal keratinocytes is regulated by interferon and is mediated by intercellular adhesion molecule 1 (ICAM-1). J. Exp. Med. 167:13231340. 67. Elewski, B. E., and D. L. Greer. 1991. Hendersonula toruloidea and Scytalidium hyalinum. Review and update. Arch. Dermatol. 127:10411044. 68. Enk, A. H., V. L. Angeloni, M. C. Udey, and S. I. Katz. 1993. An essential role for Langerhans cell-derived IL-1 in the initiation of primary immune response in skin. J. Immunol. 150:36983704. 69. Espiritu, B. R., A. Szpindor-Watson, H. J. Zeitz, and L. L. Thomas. 1988. IgE-mediated sensitivity to Trichophyton rubrum in a patient with chronic dermatophytosis and Cushings syndrome. J. Allergy Clin. Immunol. 81: 847851. 70. Faergemann, J. 1983. Antibodies to Pityrosporum orbiculare in patients with tinea versicolor and controls of various ages. J. Invest. Dermatol. 80:133 135. 71. Faergemann, J., and T. Fredriksson. 1980. Age incidence of Pityrosporum orbiculare on human skin. Acta Dermato Venereol. 60:531533. 72. Faergemann, J., H. Gisslen, E. Dahlberg, J. Westin, and G. Roupe. 1989. Trichophyton rubrum abscesses in immunocompromised patients. Acta Dermato Venereol. 69:244247. 73. Faergemann, J., S. Johansson, O. Back, and A. Scheynius. 1986. An immunologic and cultural study of Pityrosporum folliculitis. J. Am. Acad. Dermatol. 14:429433. 74. Faergemann, J., and H. I. Maibach. 1984. The Pityrosporon yeaststheir role as pathogens. Int. J. Dermatol. 23:463465. 75. Ferguson, A. C., H. E. Kershnar, W. K. Collin, and E. R. Stiehm. 1977. Correlation of cutaneous hypersensitivity with lymphocyte response to Candida albicans. Am. J. Clin. Pathol. 68:499504. 76. Filler, S. G., and J. E. Edwards, Jr. 1993. Chronic mucocutaneous candidiasis, p. 117133. In J. W. Murphy, H. Friedman, and M. Bendinelli (ed.), Fungal infections and immune responses. Plenum Press, New York. 77. Findling, J. W., J. N. Tyrrell, D. C. Aron, P. A. Fitzgerald, C. W. Young, and P. G. Sohnle. 1981. Fungal infections in Cushings syndrome. Ann. Intern. Med. 95:392. 78. Fischer, A. J., J. J. Ballet, and C. Griscelli. 1987. Specic inhibition of the in vitro Candida induced lymphocyte proliferation by polysaccharide antigens present in the serum of patients with chronic mucocutaneous candidiasis. J. Clin. Invest. 62:10051013. 79. Fischer, A. J., L. Pichat, M. Audinot, and C. Griscelli. 1982. Defective handling of mannan by monocytes in patients with chronic mucocutaneous candidiasis resulting in a specic cellular unresponsiveness. Clin. Exp. Immunol. 47:653660. 80. Fleming, T. E., W. S. Mirando, U. Trefzer, K. A. Tubesing, and C. A. Elmets. 1993. In situ expression of a B7-like adhesion molecule on keratinocytes from human epidermis. J. Invest. Dermatol. 101:754758. 81. Fredriksson, T., and J. Faergemann. 1984. Semanticstinea versus pityriasis versicolor and Pityrosporum orbiculare versus Malassezia furfur. Which is proper? Int. J. Dermatol. 23:110111. 82. Fusaro, R. M., and N. G. Miller. 1984. Onychomycosis caused by Trichosporon beigelii. J. Am. Acad. Dermatol. 11:747749. 83. Gabay, J. E., J. M. Heiple, Z. A. Cohn, and C. F. Nathan. 1986. Subcellular location and properties of bactericidal factors from human neutrophils. J. Exp. Med. 164:14071421. 84. Galbraith, G. M. P. 1988. Therapeutic immunomodulation. Dermatol. Clin. 6:561568. 85. Ganz, T., M. E. Selsted, D. Szklarek, S. S. L. Harwig, K. Dahler, D. F. Bainton, and R. I. Lehrer. 1985. Defensins: natural peptide antibiotics of human neutrophils. J. Clin. Invest. 76:14271435. 86. Gaspari, A., and S. I. Katz. 1988. Induction and functional characterization
Downloaded from cmr.asm.org by on March 19, 2009
332
WAGNER AND SOHNLE
of class II MHC (Ia) antigens on murine keratinocytes. J. Immunol. 140: 29562963. Gaspari, A. A., and S. I. Katz. 1991. Induction of in vivo hyporesponsiveness to contact allergens by hapten-modied Ia keratinocytes. J. Immunol. 147:41554161. Geng, J. G., M. P. Bevilacqua, K. L. Moore, T. M. McIntyre, S. M. Prescott, J. M. Kim, G. A. Bliss, G. A. Zimmerman, and R. P. McEver. 1990. Rapid neutrophil adhesion to activated endothelium mediated by GMP-140. Nature (London) 343:757760. Gettner, S. M. M., and D. W. R. Mackenzie. 1981. Responses of human peripheral lymphocytes to soluble and insoluble antigens of Candida albicans. J. Med. Microbiol. 14:333340. Gilchrest, B. A. 1979. Some gerontologic considerations in the practice of dermatology. Arch. Dermatol. 155:13431346. Goodeld, M. J. D., E. M. Saihan, and J. Crowley. 1987. Experimental folliculitis with Pityrosporum orbiculare: the inuence of host response. Acta. Dermato Venereol. 67:445447. Goodman, R. E., F. Nestle, Y. M. Naidu, J. M. Green, C. B. Thompson, B. J. Nickoloff, and L. A. Turka. 1994. Keratinocyte-derived T cell costimulation induces preferential production of IL-2 and IL-4, but not IFN-. J. Immunol. 152:51895198. Goodwin, J. S. 1980. Prostaglandin regulation of mitogenesis. Cell. Immunol. 52:239240. Grabbe, S., S. Bruvers, and R. D. Granstein. 1992. Effects of immunomodulatory cytokines on the presentation of tumor-associated antigens by epidermal Langerhans cells. J. Invest. Dermatol. 99:66S68S. Grando, S. A., B. S. Hostager, M. J. Herron, M. V. Dahl, and R. D. Nelson. 1992. Binding of Trichophyton rubrum mannan to human monocytes in vitro. J. Invest. Dermatol. 98:876880. Grappel, S. F., C. T. Bishop, and F. Blank. 1974. Immunology of dermatophytes and dermatophytosis. Bacteriol. Rev. 38:222250. Grappel, S. F., and F. Blank. 1972. Role of keratinases in dermatophytosis. I. Immune responses of guinea pigs infected with Trichophyton mentagrophytes and guinea pigs immunized with keratinases. Dermatologica 145: 245255. Grappel, S. F., F. Blank, and C. T. Bishop. 1968. Immunological studies on dermatophytes. III. Further analyses of the reactivities of neutral polysaccharides with rabbit antisera to Microsporum quinckeanum, Trichophyton schoenleini, Trichophyton rubrum, Trichophyton interdigitale, and Trichophyton granulosum. J. Bacteriol. 96:7075. Grappel, S. F., F. Blank, and C. T. Bishop. 1971. Circulating antibodies in human favus. Dermatologica 143:271276. Grappel, S. F., F. Blank, and C. T. Bishop. 1972. Circulating antibodies in dermatophytosis. Dermatologica 144:111. Grappel, S. F., C. A. Buscavage, F. Blank, and C. T. Bishop. 1970. Comparative serological reactivities of twenty-seven polysaccharides from nine species of dermatophytes. Sabouraudia 8:116125. Green, F., and E. Balish. 1979. Suppression of in vitro lymphocyte transformation during an experimental dermatophyte infection. Infect. Immun. 26:554562. Green, F., and E. Balish. 1980. Trichophyton mentagrophytes dermatophytosis in germfree guinea pigs. J. Invest. Dermatol. 75:476480. Greenbaum, S. S. 1924. Immunity in ringworm infections. I. Active acquired immunity with a note on complement xation tests in supercial ringworm infections. Arch. Dermatol. 10:279288. Greenberg, J. H., R. D. King, S. Krebs, and R. Field. 1976. A quantitative dermatophyte infection model in the guinea pig: a parallel to the quantitated human infection model. J. Invest. Dermatol. 67:704708. Grisham, M. B., M. M. Jefferson, D. F. Melton, and E. L. Thomas. 1983. Chlorination of exogenous amines by isolated neutrophils. Ammonia dependent bactericidal, cytotoxic, and cytolytic activities of the chloramines. J. Biol. Chem. 258:1040410413. Grossman, J., J. Baum, J. Gluckman, J. Fusner, and J. J. Condemi. 1975. The effect of aging and acute illness on delayed hypersensitivity. J. Allergy Clin. Immunol. 55:268275. Hafez, M., and S. El-Shamy. 1985. Genetic susceptibility in pityriasis versicolor. Dermatologica 171:8688. Hakansson, C., J. Faergemann, and G. B. Lowhagen. 1988. Studies on the lipophilic yeast Pityrosporum ovale in HIV-seropositive and HIV-seronegative homosexual men. Acta Dermato Venereol. 68:422426. Hanin, J. M., L. F. Ray, and W. C. Lobitz. 1974. Immunological reactivity in dermatophytosis. Br. J. Dermatol. 90:18. Hauser, C. 1992. The interaction between Langerhans cells and CD4 T cells. J. Dermatol. 19:722725. Hay, R. J. 1979. Failure of treatment in chronic dermatophyte infections. Postgrad. Med. J. 55:608610. Hay, R. J. 1982. Chronic dermatophyte infections. I. Clinical and mycological features. Br. J. Dermatol. 106:17. Hay, R. J. 1992. Genetic susceptibility to dermatophytosis. Eur. J. Epidemiol. 8:346349. Hay, R. J., and G. Shennan. 1982. Chronic dermatophyte infections. II. Antibody and cell-mediated immune responses. Br. J. Dermatol. 106:191198.
CLIN. MICROBIOL. REV.
116. Hermans, P. E., J. A. Ulrich, and H. Markowitz. 1969. Chronic mucocutaneous candidiasis as a surface expression of deep-seated abnormalities. Am. J. Med. 47:503519. 117. Herrod, H. G. 1990. Chronic mucocutaneous candidiasis in childhood and complications of non-Candida infection: a report of the pediatric immunodeciency study group. J. Pediatr. 116:377382. 118. Hirsch, J. G. 1956. Phagocytin: a bactericidal substance from polymorphonuclear leucocytes. J. Exp. Med. 103:589611. 119. Ho, Y., M. Ng, and C. T. Huang. 1979. Antibodies to germinating and yeast cells of Candida albicans in human and rabbit sera. J. Clin. Pathol. 32:399 405. 120. Hopfer, R. L., S. F. Grappel, and F. Blank. 1975. Antibodies with afnity for epithelial tissue in chronic dermatophytosis. Dermatologica 151:135143. 121. Hughes, B. R. 1988. Tinea versicolor in immunosuppressed patients. J. Am. Acad. Dermatol. 19:357358. 122. Hunziker, N., and R. Brun. 1980. Lack of delayed reaction in presence of cell-mediated immunity in trichophytin hypersensitivity. Arch. Dermatol. 116:12661268. 123. Ikai, K., H. Okano, Y. Horiguchi, and Y. Sakamoto. 1994. Leukotriene A4 hydrolase in human skin. J. Invest. Dermatol. 102:253257. 124. Inaba, K., G. Schuler, M. D. Witmer, J. Valinsky, B. Atassi, and R. M. Steinman. 1986. Immunologic properties of puried epidermal Langerhans cells. Distinct requirements for stimulation of unprimed and sensitized T lymphocytes. J. Exp. Med. 164:605613. 125. Jillson, O. F., and M. Huppert. 1949. The immediate wheal and 2448 hour tuberculin type edematous reactions to trichophytin. J. Invest. Dermatol. 12:179185. 126. Johnson, J. G., and M. K. Jenkins. 1992. Co-stimulatory functions of antigen-presenting cells. J. Invest. Dermatol. 99:62S65S. 127. Jones, H. E. 1980. The atopic-dermatophytosis syndrome. Acta Dermato Venereol. Suppl. 92:8185. 128. Jones, H. E. 1993. Immune response and host resistance of humans to dermatophyte infections. J. Am. Acad. Dermatol. 28:S12S18. 129. Jones, H. E., J. H. Reinhardt, and M. G. Rinaldi. 1973. A clinical, mycological, and immunological survey for dermatophytosis. Arch. Dermatol. 108:6165. 130. Jones, H. E., J. H. Reinhardt, and M. G. Rinaldi. 1974. Acquired immunity to the dermatophytes. Arch. Dermatol. 109:840847. 131. Jones, H. E., J. H. Reinhardt, and M. G. Rinaldi. 1974. Immunologic susceptibility to chronic dermatophytosis. Arch. Dermatol. 110:213220. 132. Jones, H. E., J. H. Reinhardt, and M. G. Rinaldi. 1974. Model dermatophytosis in naturally-infected subjects. Arch. Dermatol. 110:369374. 133. Jones, H. E., M. G. Rinaldi, H. Chai, and G. Kahn. 1973. Apparent crossreactivity of airborne molds and the dermatophyte fungi. J. Allergy Clin. Immunol. 53:346351. 134. Kaaman, T. 1978. The clinical signicance of cutaneous reactions to trichophytin in dermatophytosis. Acta Dermato Venereol. 58:139143. 135. Kaaman, T. 1981. Cell-mediated reactivity in dermatophytosis: differences in skin responses to puried trichophytin in tinea pedis and tinea cruris. Acta Dermato Venereol. 61:119123. 136. Kaaman, T., B. Petrini, and S. Wasserman. 1979. In vivo and in vitro immune responses to trichophytin in dermatophytosis. Acta Dermato Venereol. 59:229233. 137. Kaaman, T., L. V. von Stedingk, M. von Stedingk, and J. Wasserman. 1981. ELISA-determined serological reactivity against puried trichophytin in dermatophytosis. Acta Dermato Venereol. 61:313317. 138. Kamalan, A., G. Senthamilselvi, K. Ajithadas, and A. S. Thambiah. 1988. Cutaneous trichosporosis. Mycopathology 101:167175. 139. Kashima, M., H. Takahashi, M. Shimozuma, W. L. Epstein, and K. Fukuyama. 1989. Candidacidal activities of proteins partially puried from rat epidermis. Infect. Immun. 57:186190. 140. Katoh, T., S. Kagawa, and M. Ishimoto. 1988. Malassezia intertrigo, a new clinical entity. Mycoses 31:558562. 141. Kauffman, C. A., M. J. Shea, and P. T. Frame. 1981. Invasive fungal infections in patients with chronic mucocutaneous candidiasis. Arch. Intern. Med. 141:10761078. 142. King, R. D., R. L. Cunico, H. I. Maibach, J. H. Greenberg, M. L. West, and J. C. Jeppsen. 1978. The effect of occlusion on carbon dioxide emission from human skin. Acta Dermato Venereol. 58:135138. 143. King, R. D., H. A. Khan, J. C. Foye, J. H. Greenberg, and H. E. Jones. 1975. Transferrin, iron, and dermatophytes. I. Serum dermatophyte inhibitory component denitively identied as unsaturated transferrin. J. Lab. Clin. Med. 86:204212. 144. Kirkpatrick, C. H. 1984. Host defense against fungal infections. Am. J. Med. 77(Suppl. 4D):112. 145. Kirkpatrick, C. H., R. R. Rich, and J. E. Bennett. 1971. Chronic mucocutaneous candidiasis: model building in cellular immunity. Ann. Intern. Med. 74:955978. 146. Kirkpatrick, C. H., and T. K. Smith. 1974. Chronic mucocutaneous candidiasis: immunologic and antibiotic therapy. Ann. Intern. Med. 80:310320. 147. Kirkpatrick, C. H., and P. G. Sohnle. 1981. Chronic mucocutaneous candidiasis, p. 495514. In B. Safai and R. A. Good (ed.), Immunodermatology.
87. 88.
89. 90. 91. 92.
93. 94. 95. 96. 97.
Downloaded from cmr.asm.org by on March 19, 2009
98.
99. 100. 101. 102. 103. 104.
105.
106.
107.
108. 109.
110. 111. 112. 113. 114. 115.
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS
333
Plenum Press, New York. 148. Kirkpatrick, C. H., and D. B. Windhorst. 1979. Mucocutaneous candidiasis and thymoma. Am. J. Med. 66:939945. 149. Kligman, A. M. 1952. The pathogenesis of tinea capitis due to Microsporum audouini and Microsporum canis. J. Invest. Dermatol. 18:231246. 150. Kligman, A. M. 1956. Pathophysiology of ringworm infections in animals with skin cycles. J. Invest. Dermatol. 27:171185. 151. Kligman, A. M., and D. Ginsberg. 1950. Immunity of the adult scalp to infection with Microsporum audouini. J. Invest. Dermatol. 14:345356. 152. Klotz, S. A. 1989. Malassezia furfur. Infect. Dis. Clin. North Am. 3:5364. 153. Klotz, S. A., D. J. Drutz, M. Huppert, and J. E. Johnson. 1982. Pityrosporum folliculitis: its potential for confusion with skin lesions of systemic candidiasis. Arch. Intern. Med. 142:21262129. 154. Knight, A. G. 1972. A review of experimental human fungus infections. J. Invest. Dermatol. 59:354358. 155. Knight, S. C., A. Stagg, S. Hill, P. Fryer, and S. Grifths. 1992. Development and function of dendritic cells in health and diseases. J. Invest. Dermatol. 99:33S38S. 156. Koranda, F. C., E. M. Dehmel, G. Kahn, and I. Penn. 1974. Cutaneous complications in immunosuppressed renal homograft recipients. JAMA 229:419424. 157. Krebs, S., J. Greenberg, and K. Jesrani. 1977. Temporal correlation of lymphocyte blastogenesis, skin test responses, and erythema during dermatophyte infections. Clin. Exp. Immunol. 27:526530. 158. Kurimoto, I., M. Arana, and J. W. Streilein. 1994. Role of dermal cells from normal and ultraviolet B-damaged skin in induction of contact hypersensitivity and tolerance. J. Immunol. 152:33173323. 159. Kutsch, C. L., D. A. Norris, and W. P. Arend. 1993. Tumor necrosis factor- induces interleukin-1 and interleukin-1 receptor antagonist production by cultured human keratinocytes. J. Invest. Dermatol. 101:7985. 160. Lehner, T. J., M. A. Wilton, and L. Ivanyi. 1972. Immunodeciencies in chronic mucocutaneous candidiasis. Immunology 22:775787. 161. Lepper, A. W. D. 1972. Experimental bovine Trichophyton verrucosum infection. Preliminary clinical, immunological, and histological observations in primarily infected and reinoculated cattle. Rev. Vet. Sci. 13:105115. 162. Lepper, A. W. D. 1974. Experimental bovine Trichophyton verrucosum infection. The cellular responses in primary lesions of the skin resulting from surface or intradermal inoculation. Res. Vet. Sci. 16:287298. 163. Lepper, A. W. D., and H. S. Anger. 1976. Experimental bovine Trichophyton verrucosum infection. Comparison of the rate of epidermal cell proliferation and keratinization in non-infected and reinoculated cattle. Res. Vet. Sci. 20:117121. 164. Lowinger-Seoane, M., J. M. Torres-Rodriguez, N. Madrenys-Brunet, S. Aregall-Fuste, and P. Saballs. 1992. Extensive dermatophytoses caused by Trichophyton mentagrophytes and Microsporum canis in a patient with AIDS. Mycopathology 120:143146. 165. Mackenzie, J. C. 1970. Relationship between mitosis and the structure of the stratum corneum in mouse epidermis. Nature (London) 226:653655. 166. Marcussen, P. V. 1937. Relationship of the urticarial to the inammatory reaction to trichophytin. Arch. Dermatol. 36:494514. 167. Marples, M. J. 1950. The incidence of certain skin diseases in Western Samoa: a preliminary study. Trans. R. Soc. Med. Hyg. 44:319332. 168. Matsue, H., P. R. Bergstresser, and A. Takashima. 1993. Keratinocytederived IL-7 serves as a growth factor for dendritic epidermal T cells in mice. J. Immunol. 151:60126019. 169. Matsue, H., P. D. Cruz, Jr., P. R. Bergstresser, and A. Takashima. 1992. Cytokine expression by epidermal cell subpopulations. J. Invest. Dermatol. 99:42S45S. 170. Matthews, R. C., J. P. Burnie, A. Fox, M. Woods, and S. Tabaqchali. 1986. Immunoblot analysis of the serological response in invasive Trichosporon beigelii and Blastoschizomyces capitus infections. J. Clin. Microbiol. 23:395 397. 171. McGregor, J. M., A. J. Hamilton, and R. J. Hay. 1992. Possible mechanisms of immune modulation in chronic dermatophytoses: an in vitro study. Br. J. Dermatol. 127:233238. 172. McKay, I. A., and I. M. Leigh. 1991. Epidermal cytokines and their roles in cutaneous wound healing. Br. J. Dermatol. 124:513518. 173. McManus, E. J., M. J. Bozdech, and J. M. Jones. 1985. Role of the latex agglutination test for cryptococcal antigen in diagnosing disseminated infections with Trichosporon beigelii. J. Infect. Dis. 151:11671169. 174. McNamara, M. P., J. H. Wiessner, C. Collins-Lech, B. L. Hahn, and P. G. Sohnle. 1988. Neutrophil death as a defense mechanism against Candida albicans infections. Lancet ii:11631165. 175. Metaly, J. P., E. Pure, and R. M. Steinman. 1989. Control of the immune response at a level of antigen-presenting cells: a comparison of the function of dendritic cells and B-lymphocytes. Adv. Immunol. 47:45116. 176. Mobacken, H., L. Lindholm, and S. Olling. 1977. Decient neutrophil function in a patient with chronic mucocutaneous candidiasis, thymoma and myasthenia gravis. Acta Dermato Venereol. 57:335339. 177. Modrzakowski, M. C., M. H. Cooney, L. E. Martin, and J. K. Spitznagel. 1979. Bactericidal activity of fractionated granule contents from human polymorphonuclear leukocytes. Infect. Immun. 23:587591.
178. Montes, L. F. 1970. Systemic abnormalities and the intracellular site of infections of the stratum corneum. JAMA 213:14691472. 179. Montes, L. F. 1992. Candidiasis, p. 913923. In S. L. Moschella and H. J. Hurley (ed.), Dermatology, 3rd ed. W. B. Saunders, Co., Philadelphia. 180. Moore, K. L., and L. F. Thompson. 1992. P-selectin (CD-62) binds to subpopulations of human memory T lymphocytes and natural killer cells. Biochem. Biophys. Res. Commun. 186:173181. 181. Moore, M. K., and R. J. Hay. 1986. Circulating antibodies and antigenic cross-reactivity in Hendersonula toruloidea and Scytalidium hyalinum infections. Br. J. Dermatol. 115:435445. 182. Morris, R. J., S. M. Fischer, and T. J. Slaga. 1985. Evidence that the centrally and peripherally located cells in the murine epidermal proliferative unit are two distinct cell populations. J. Invest. Dermatol. 84:277281. 183. Moser, S. A., J. E. Domer, and F. J. Mather. 1980. Experimental murine candidiasis: cell-mediated immunity after cutaneous challenge. Infect. Immun. 27:140149. 184. Moser, S. A., and J. D. Pollack. 1978. Isolation of glycopeptides with skin test activity from dermatophytes. Infect. Immun. 19:10311046. 185. Murthy, A. R. K., R. I. Lehrer, S. S. L. Harwig, and K. T. Miyasaki. 1993. In vitro candidastatic properties of the human neutrophil calprotectin complex. J. Immunol. 151:62916301. 186. Nathan, C. F., G. Kaplan, W. R. Lewis, A. Nusrat, M. D. Witmer, S. A. Sherwin, C. K. Job, C. R. Horowitz, R. M. Steinman, and Z. A. Cohn. 1986. Local and systemic effects of intradermal recombinant interferon- in patients with lepromatous leprosy. N. Engl. J. Med. 315:615. 187. Nazzaro-Porro, M., and S. Passi. 1978. Identication of tyrosinase inhibitors in cultures of Pityrosporum. J. Invest. Dermatol. 71:205208. 188. Negi, M., R. Tsuboi, T. Matsui, and H. Ogawa. 1984. Isolation and characterization of proteinase from Candida albicans: substrate specicity. J. Invest. Dermatol. 83:3236. 189. Nelson, M., and K. J. McNiece. 1959. Recurrent Cushings syndrome with Trichophyton rubrum infection. Arch. Dermatol. 80:700704. 190. Nestle, F. O., X.-G. Zheng, C. B. Thompson, L. A. Turka, and B. J. Nickoloff. 1993. Characterization of dermal dendritic cells obtained from normal human skin reveals phenotypic and functionally distinct subsets. J. Immunol. 151:65356545. 191. Nordvall, S. L., L. Lindgren, S. G. O. Johansson, S. Johansson, and B. Petrini. 1992. IgE antibodies to Pityrosporum orbiculare and Staphylococcus aureus in patients with very high serum total IgE. Clin. Exp. Immunol. 22:756761. 192. Odeberg, H., and I. Olsson. 1976. Microbicidal mechanisms of human granulocytes: synergistic effects of granulocyte elastase and myeloperoxidase or chymotrypsin-like cationic protein. Infect. Immun. 14:12761283. 193. Oppenheim, J. J., C. O. C. Zachariae, N. Mukaida, and K. Matsushima. 1991. Properties of the novel proinammatory supergene intercrine cytokine family. Annu. Rev. Immunol. 9:617648. 194. Palmer, D. L., and W. P. Reed. 1974. Delayed hypersensitivity skin testing. I. Response rates in a hospitalized population. J. Infect. Dis. 130:132137. 195. Palmer, S. R., J. W. Bass, R. Mandojana, and R. R. Wittler. 1989. Tinea nigra palmaris and plantaris: a black fungus producing black spots on the palms and soles. Pediatr. Infect. Dis. J. 8:4850. 196. Papini, M., and S. Simonetti. 1985. Humoral immunouorescent antibodies in subjects with dermatophytosis. Mykosen 28:419429. 197. Parker, F. 1988. Skin diseases, p. 23002353. In J. B. Wyngaarden and L. D. Smith (ed.), Cecil textbook of medicine, 18th ed. W. B. Saunders Co., Philadelphia. 198. Parkinson, E. K. 1992. Epidermal keratinocyte stem cells: their maintenance and regulation. Semin. Cell Biol. 3:435444. 199. Peachey, R. D. G., and M. P. English. 1974. An outbreak of Trichophyton rubrum infection in a geriatric hospital. Br. J. Dermatol. 4:389398. 200. Peck, S. M., K. E. Osserman, and A. H. Rule. 1972. Intercellular antibodies: presence in a Trichophyton rubrum infection. J. Invest. Dermatol. 58:133 138. 201. Peck, S. M., S. Siegel, and R. Bergamini. 1947. Immunologic relationships of the antibiotics and trichophytin. Clinical observations and animal experiments. J. Invest. Dermatol. 9:165185. 202. Peguet-Navarro, J., C. Dalbiez-Gauthier, C. Dezutter-Dambuyant, and D. Schmitt. 1993. Dissection of human Langerhans cells allostimulatory function: the need for an activation step for full development of accessory function. Eur. J. Immunol. 23:376382. 203. Pentland, A. P., and M. G. Mahoney. 1990. Keratinocyte prostaglandin synthesis is enhanced by IL-1. J. Invest. Dermatol. 94:4346. 204. Podzorski, R. P., G. R. Gray, and R. D. Nelson. 1990. Different effects of native Candida albicans mannan and mannan-derived oligosaccharides on antigen-stimulated lymphoproliferation in vitro. J. Immunol. 144:707716. 205. Potten, C. S. 1974. The epidermal proliferative unit: the possible role of the central basal cell. Cell Tissue Kinet. 7:7788. 206. Potter, B. S., C. F. Burgoon, Jr., and W. C. Johnson. 1973. Pityrosporum folliculitisreport of seven cases and review of the Pityrosporum organism relative to cutaneous disease. Arch. Dermatol. 107:388391. 207. Poulain, D., G. Tronchin, A. Vernes, M. Delabre, and J. Biguet. 1980. Experimental study of resistance to infection by Trichophyton mentagro-
Downloaded from cmr.asm.org by on March 19, 2009
334
WAGNER AND SOHNLE
phytes: demonstration of memory skin cells. J. Invest. Dermatol. 74:205 209. Prose, N. S. 1992. Cutaneous manifestations of pediatric HIV infection. Pediatr. Dermatol. 9:326328. Quindos, G., J. Schneider, M. Alvarez, J. Ponton, and R. Cisterna. 1989. Antibodies against Trichosporon beigelii in vaginal washings from asymptomatic women. J. Med. Microbiol. 28:223225. Rasmussen, J. E., and A. R. Ahmed. 1978. Trichophytin reactions in children with tinea capitis. Arch. Dermatol. 114:371372. Ray, T. L., and K. D. Wuepper. 1976. Activation of the alternative (properdin) pathway of complement by Candida albicans and related species. J. Invest. Dermatol. 67:700703. Reid, C. D. L., P. R. Fryer, C. Clifford, A. Kirk, J. Tikerpae, and S. C. Knight. 1990. Identication of hematopoietic progenitors of macrophages and dendritic Langerhans cells (DL-CFU) in human bone marrow and peripheral blood. Blood 76:11391149. Reyes, E. C., and L. Friedman. 1966. Concerning the specicity of dermatophyte-reacting antibody in human and experimental animal sera. J. Invest. Dermatol. 47:2734. Rivas, V., and T. J. Rogers. 1983. Studies on the cellular nature of Candida albicans-induced suppression. J. Immunol. 130:376379. Roberts, S. O. B. 1969. Pityriasis versicolor: a clinical and mycological investigation. Br. J. Dermatol. 81:315326. Rogers, T. J., and E. Balish. 1978. Suppression of lymphocyte blastogenesis by Candida albicans. Clin. Immunol. Immunopathol. 10:298305. Romani, N., E. Kampgen, F. Koch, C. Heuer, and G. Schuler. 1990. Dendritic cell production of cytokines and responses to cytokines. Int. Rev. Immunol. 6:151161. Root, R. K., and M. S. Cohen. 1981. The microbicidal mechanisms of human neutrophils and eosinophils. Rev. Infect. Dis. 3:565598. Rose, H. D., and V. P. Kurup. 1977. Colonization of hospitalized patients with yeast-like organisms. Sabouraudia 15:251256. Rothman, S., A. Smiljanic, A. L. Shapiro, and A. W. Weitkamp. 1947. The spontaneous cure of tinea capitis in puberty. J. Invest. Dermatol. 8:8198. Rothschild, H., M. Wilson, M. Lopez, J. Salvaggio, and D. Bice. 1976. An immunological investigation of a family with chronic mucocutaneous candidiasis. Int. Arch. Allergy Appl. Immunol. 52:291296. Rycroft, R. J. G., H. Valdimarsson, L. H. Bannister, and R. S. Wells. 1976. Chronic mucocutaneous candidiasis of late onset, thymoma and myopathy. A report of four cases. Clin. Exp. Dermatol. 1:5974. Scheynius, A., J. Faergemann, U. Forsum, and O. Sjoberg. 1984. Phenotypic characterization in situ of inammatory cells in pityriasis (tinea) versicolor. Acta Dermato Venereol. 64:473479. Schmitt, C., and J. J. Ballet. 1983. Serum IgE and IgG antibodies to tetanus toxoid and candidin in immunodecient children with the hyper-IgE syndrome. J. Clin. Immunol. 3:178183. Segal, E. 1989. Vaccines for the management of dermatophyte and supercial yeast infections. Curr. Top. Med. Mycol. 3:3649. Selsted, M. E., S. S. Harwig, T. Ganz, J. W. Schilling, and R. I. Lehrer. 1985. Primary structures of three human neutrophil defensins. J. Clin. Invest. 76:14361439. Serjeantson, S., and G. Lawrence. 1977. Autosomal recessive inheritance of susceptibility to tinea imbricata. Lancet i:1315. Shannon, D. C., G. Johnson, F. S. Rosen, and K. F. Austen. 1966. Cellular reactivity to Candida albicans antigen. N. Engl. J. Med. 275:690693. Sherwin, W. K., T. H. Ross, C. M. Rosenthal, and J. W. Petrozzi. 1979. An immunosuppressive serum factor in widespread cutaneous dermatophytosis. Arch. Dermatol. 115:600604. Shimizu, Y., S. Shaw, N. Graber, T. V. Gopal, K. J. Horgan, G. A. Van Seventer, and W. Newman. 1991. Activation-independent binding of human memory T cells to adhesion molecule ELAM-1. Nature (London) 349:799 802. Shuster, S. 1984. The etiology of dandruff and the mode of action of therapeutic agents. Br. J. Dermatol. 111:235242. Silverberg, I. 1973. Apposition of mononuclear cells to Langerhans cells in contact allergic reactions. Acta Dermato Venereol. 53:112. Simon, J. C., P. D. Cruz, Jr., R. E. Tigelaar, R. D. Sontheimer, and P. R. Bergstresser. 1991. Adhesion molecules CD11a, CD18, and ICAM-1 on human epidermal Langerhans cells serve a functional role in the activation of alloreactive T cells. J. Invest. Dermatol. 96:148151. Skarnes, R. C., and D. W. Watson. 1956. Characterization of leukin: an antibacterial factor from leucocytes active against gram-positive pathogens. J. Exp. Med. 104:829845. Snyderman, R., L. C. Altman, A. Frankel, and R. K. M. Blaese. 1973. Defective mononuclear leukocyte chemotaxis: a previously unrecognized immune dysfunction. Ann. Intern. Med. 78:509513. Sohnle, P. G., and C. Collins-Lech. 1978. Cell-mediated immunity to Pityrosporum orbiculare in tinea versicolor. J. Clin. Invest. 62:4553. Sohnle, P. G., and C. Collins-Lech. 1980. Relative antigenicity of Pityrosporum orbiculare and Candida albicans. J. Invest. Dermatol. 75:279283. Sohnle, P. G., and C. Collins-Lech. 1982. Analysis of the lymphocyte transformation response to Pityrosporum orbiculare in patients with tinea versi-
CLIN. MICROBIOL. REV.
color. Clin. Exp. Immunol. 49:559564. 239. Sohnle, P. G., and C. Collins-Lech. 1983. Activation of complement by Pityrosporum orbiculare. J. Invest. Dermatol. 80:9397. 240. Sohnle, P. G., C. Collins-Lech, and K. E. Huhta. 1983. Class-specic antibodies in young and aged humans against organisms producing supercial fungal infections. Br. J. Dermatol. 108:6976. 241. Sohnle, P. G., C. Collins-Lech, and K. E. Huhta. 1983. Kinetics of lymphokine production by lymphocytes from elderly humans. Gerontology 29:169 175. 242. Sohnle, P. G., C. Collins-Lech, and J. H. Wiessner. 1991. The zinc-reversible antimicrobial activity of neutrophil lysates and abscess uid supernatants. J. Infect. Dis. 164:137142. 243. Sohnle, P. G., M. M. Frank, and C. H. Kirkpatrick. 1976. Mechanisms involved in elimination of organisms from experimental cutaneous Candida albicans infection in guinea pigs. J. Immunol. 117:523530. 244. Sohnle, P. G., and B. L. Hahn. 1989. Epidermal proliferation and the neutrophilic inltrates of experimental cutaneous candidiasis in mice. Arch. Dermatol. Res. 281:279283. 245. Sohnle, P. G., and C. H. Kirkpatrick. 1978. Epidermal proliferation in the defense against cutaneous candidiasis. J. Invest. Dermatol. 70:130133. 246. Solcia, E., M. Paulli, E. Silini, R. Fiocca, G. Finzi, S. Kindl, E. Boveri, F. Bosi, M. Cornaggia, C. Capella, and I. M. Samloff. 1993. Cathepsin E in antigen-presenting Langerhans and interdigitating reticulum cells. Its possible role in antigen processing. Eur. J. Histochem. 37:1926. 247. Sorensen, G., and H. E. Jones. 1976. Immediate and delayed hypersensitivity in chronic dermatophytosis. Arch. Dermatol. 112:4042. 248. Sousa, C. R., P. D. Stahl, and J. M. Austyn. 1993. Phagocytosis of antigens by Langerhans cells in vitro. J. Exp. Med. 178:509519. 249. Stahl, D., and E. Svejgaard. 1982. Lymphocyte transformation in vitro in acute dermatophytosis: a follow-up study. Acta Dermato Venereol. 62:289 293. 250. Steinbakk, M., C. F. Naess-Andresen, E. Lingass, I. Dale, P. Brandtzaeg, and M. K. Fagerhol. 1990. Antimicrobial actions of calcium binding leucocyte L1 protein, calprotectin. Lancet 336:763765. 251. Stingl, G. 1993. This skin: initiation and target site of immune responses. Recent Results Cancer Res. 128:4557. 252. Stingl, G., C. Hauser, and K. Wolff. 1993. The epidermis: an immunologic microenvironment, p. 172197. In T. B. Fitzpatrick, A. Z. Eisen, K. Wolff, I. M. Freedberg, and K. F. Austen (ed.), Dermatology in general medicine, 4th ed. McGraw-Hill, New York. 253. Stossel, H., F. Koch, E. Kampgen, P. Stoger, A. Lenz, C. Heuer, N. Romani, and G. Schuler. 1990. Disappearance of certain acidic organelles (endosomes and Langerhans cell granules) accompanies loss of antigen processing capacity upon culture of epidermal Langerhans cells. J. Exp. Med. 172:14711482. 254. Strauss, J. S., and A. M. Kligman. 1957. An experimental study of tinea pedis and onychomycosis of the foot. Arch. Dermatol. 76:7079. 255. Streilein, J. W. 1983. Skin-associated lymphoid tissues (SALT): origins and functions. J. Invest. Dermatol. 80:12S16S. 256. Sundstrom, P. M., and G. E. Kenny. 1984. Characterization of antigens specic to the surface of germ tubes of Candida albicans by immunouorescence. Infect. Immun. 43:850855. 257. Svejgaard, E., M. Thomsen, N. Morling, and A. H. Christiansen. 1976. Lymphocyte transformation in vitro in dermatophytosis. Acta Pathol. Microbiol. Scand. Sect. C 84:511519. 258. Swan, J. W., M. A. Dahl, P. A. Coppo, and D. E. Hammerschmidt. 1983. Complement activation by Trichophyton rubrum. J. Invest. Dermatol. 80: 156158. 259. Swerlick, R. A., E. Garcia-Gonzalez, Y. Kubota, Y. Xu, and T. J. Lawley. 1991. Studies of the modulation of MHC antigen and cell adhesion molecule expression on human dermal microvascular endothelial cells. J. Invest. Dermatol. 97:190196. 260. Swerlick, R. A., and T. J. Lawley. 1993. Role of microvascular endothelial cells in inammation. J. Invest. Dermatol. 100:111S115S. 261. Symington, F. W., W. Brady, and P. S. Linsley. 1993. Expression and function of B7 on human epidermal Langerhans cells. J. Immunol. 150: 12861295. 262. Szepes, E., M. Magyarlaki, Z. Battyani, and I. Schneider. 1993. Immunohistological characterization of the cellular inltrate in dermatophytosis. Mycoses 36:203206. 263. Tagami, H., N. Natsume, T. Aoshima, F. Inoue, S. Suehisa, and M. Yamada. 1982. Analysis of transepidermal leucocyte chemotaxis in experimental dermatophytosis in guinea pigs. Arch. Dermatol. Res. 273:205217. 264. Tagami, H., S. Watanabe, and S. Ofugi. 1973. Trichophytin contact sensitivity in guinea pigs with experimental dermatophytosis induced by a new inoculation method. J. Invest. Dermatol. 61:237241. 265. Takeya, K., K. Nomoto, T. Matsumoto, T. Miyake, and K. Himeno. 1976. Chronic mucocutaneous candidiasis accompanied by enhanced antibody production. Clin. Exp. Immunol. 25:497500. 266. Takiuchi, I., D. Higuchi, Y. Sei, and M. Koga. 1982. Isolation of an extracellular proteinase (keratinase) from Microsporum canis. Sabouraudia 20: 281288.
208. 209. 210. 211. 212.
213. 214. 215. 216. 217. 218. 219. 220. 221. 222. 223. 224. 225. 226.
Downloaded from cmr.asm.org by on March 19, 2009
227. 228. 229.
230.
231. 232. 233.
234.
235.
236. 237. 238.
VOL. 8, 1995
CUTANEOUS DEFENSES AGAINST DERMATOPHYTES AND YEASTS
335
267. Tamaki, K., H. Fujiwara, R. B. Levy, G. M. Shearer, and S. I. Katz. 1981. Hapten specic TNP-reactive cytotoxic effector cells using epidermal cells as targets. J. Invest. Dermatol. 77:225229. 268. Tang, A., M. Amagai, L. G. Granger, J. R. Stanley, and M. C. Udey. 1993. Adhesion of epidermal Langerhans cells to keratinocytes mediated by Ecadherin. Nature (London) 361:8285. 269. Test, S. T., M. B. Lampert, P. J. Ossanna, J. G. Thoene, and S. J. Weiss. 1984. Generation of nitrogen-chlorine oxidants by human phagocytes. J. Clin. Invest. 74:13411349. 270. Teunissen, M. B. M. 1992. Functional role of adhesion molecules LFA-3 and ICAM-1 on cultured human epidermal Langerhans cells in antigenspecic T-cell activation. J. Invest. Dermatol. 99:77S79S. 271. Teunissen, M. B. M., H. A. H. Rongen, and J. D. Bos. 1994. Function of adhesion molecules lymphocyte function associated antigen-3 and intercellular adhesion molecule-1 on human epidermal Langerhans cells in antigen-specic T cell activation. J. Immunol. 152:34003409. 272. Thomas, E. L., R. I. Lehrer, and R. F. Rest. 1988. Human neutrophil antimicrobial activity. Rev. Infect. Dis. 10(Suppl. 2):S450S456. 273. Tindall, J. P., and J. G. Smith. 1963. Skin lesions of the aged and their association with internal changes. J. Am. Med. 186:10391042. 274. Twomey, J. T., C. C. Waddel, S. Krantz, R. OReilly, P. LEsperance, and R. A. Good. 1975. Chronic mucocutaneous candidiasis with macrophage dysfunction, a plasma inhibitor and coexistent aplastic anemia. J. Lab. Clin. Med. 85:968977. 275. Valdimarsson, H., J. M. Higgs, R. S. Wells, M. Yamamura, J. R. Hobbs, and P. J. L. Holt. 1973. Immune abnormalities associated with chronic mucocutaneous candidiasis. Cell Immunol. 6:34861.
276. Van der Meer, J. W. M., P. C. J. Leijh, M. Van den Barselaar, and R. Van Furth. 1978. Functions of phagocytic cells in chronic mucocutaneous candidiasis. Br. Med. J. 1:147148. 277. Wagner, D. K., and P. G. Sohnle. Cutaneous defense mechanisms against fungi. In P. H. Jacobs and L. Nall (ed.), Selected topics in medical mycology, in press. Marcel Dekker, Inc., New York. 278. Walters, B. A. J., J. E. D. Chick, and W. J. Halliday. 1974. Cell-mediated immunity and serum blocking factors in patients with chronic dermatophyte infections. Int. Arch. Allergy Appl. Immunol. 46:849857. 279. Weiss, J., P. Elsbach, I. Olsson, and H. Odeberg. 1978. Purication and characterization of a potent bactericidal and membrane active protein from the granules of human polymorphonuclear leukocytes. J. Biol. Chem. 253: 26642672. 280. Wilson, B. D., and P. G. Sohnle. 1986. Participation of neutrophils and cell-mediated immunity in the defense against experimental cutaneous candidiasis in mice. Am. J. Pathol. 123:241249. 281. Wood, S. R., and C. N. D. Cruickshank. 1962. The relationship between trichophytin sensitivity and fungal infection. Br. J. Dermatol. 74:329335. 282. Yamazaki, M., K. Yasui, H. Kawaii, Y. Miyagawa, A. Komiyama, and T. Akstanl. 1984. A monocyte disorder in siblings with chronic candidiasis. Am. J. Dis. Child. 138:192196. 283. Yohn, J. J., J. Lucas, and C. Camisa. 1985. Malassezia folliculitis in immunocompromised patients. Cutis 35:536538. 284. Yu, R. J., S. R. Harmon, and F. Blank. 1968. Isolation and purication of an extracellular keratinase of Trichophyton mentagrophytes. J. Bacteriol. 96:14351436.
Downloaded from cmr.asm.org by on March 19, 2009
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Case Investigation Form Coronavirus Disease (COVID-19) : (Check All That Apply, Refer To Appendix 2)Документ4 страницыCase Investigation Form Coronavirus Disease (COVID-19) : (Check All That Apply, Refer To Appendix 2)john dave rougel ManzanoОценок пока нет
- Basic ImmunologyДокумент9 страницBasic Immunologyarsyiadlina100% (1)
- Allergic Rhinitis Educational Leaflet 2006Документ2 страницыAllergic Rhinitis Educational Leaflet 2006arsyiadlinaОценок пока нет
- Infectious DiseasesДокумент30 страницInfectious DiseasesMuhammad Ikhlas YasinОценок пока нет
- Basic ImmunologyДокумент9 страницBasic Immunologyarsyiadlina100% (1)
- Allergic Rhinitis - University of MichiganДокумент12 страницAllergic Rhinitis - University of MichiganarsyiadlinaОценок пока нет
- Jpn. J. Clin. Oncol. 1998 Watanabe 559 62Документ4 страницыJpn. J. Clin. Oncol. 1998 Watanabe 559 62arsyiadlinaОценок пока нет
- Poster Miini ERYTRODERMA EC Suspect Eruption DrugДокумент21 страницаPoster Miini ERYTRODERMA EC Suspect Eruption DrugarsyiadlinaОценок пока нет
- Higher Algebra - Hall & KnightДокумент593 страницыHigher Algebra - Hall & KnightRam Gollamudi100% (2)
- Practice TestДокумент2 страницыPractice TestMinh Châu NguyễnОценок пока нет
- Case Report: Hepatitis BДокумент34 страницыCase Report: Hepatitis Bdewi sartikaОценок пока нет
- Chronic MegacolonДокумент3 страницыChronic Megacolondrnareshkumar3281Оценок пока нет
- Jubilant Life Sciences Research Report PDFДокумент50 страницJubilant Life Sciences Research Report PDFAbhiroop DasОценок пока нет
- Journal Reading - Myringitis - Elisabeth PattyДокумент14 страницJournal Reading - Myringitis - Elisabeth PattyLipatOla123Оценок пока нет
- Jurnal 2Документ8 страницJurnal 2AnggunbokingsОценок пока нет
- OTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Документ10 страницOTC and PRESCRIPTION DRUGS Ppt. (TANTICO)Ladyfair TanticoОценок пока нет
- The Effects of Exercise On The Nervous SystemДокумент2 страницыThe Effects of Exercise On The Nervous SystemramadanОценок пока нет
- The Uses and Limitations of The Fetal Biophysical Profile.Документ18 страницThe Uses and Limitations of The Fetal Biophysical Profile.Diego Ortecho100% (1)
- Essentials of Diagnosis, Treatment, and Application of Cardiac and Peripheral Vascular DiseasesДокумент295 страницEssentials of Diagnosis, Treatment, and Application of Cardiac and Peripheral Vascular DiseasesMichael BrunetОценок пока нет
- The Bipolar Affective Disorder Dimension Scale (BADDS) - A Dimensional Scale For Rating Lifetime Psychopathology in Bipolar Spectrum DisordersДокумент11 страницThe Bipolar Affective Disorder Dimension Scale (BADDS) - A Dimensional Scale For Rating Lifetime Psychopathology in Bipolar Spectrum DisordersDM YazdaniОценок пока нет
- Hypertension HistoryДокумент2 страницыHypertension HistorybassamОценок пока нет
- Helping Psychiatry Residents Cope With Patient SuicideДокумент5 страницHelping Psychiatry Residents Cope With Patient SuicidedrguillermomedinaОценок пока нет
- How Do I Know If My Activities Are of Moderate To Vigorous Intensity?Документ2 страницыHow Do I Know If My Activities Are of Moderate To Vigorous Intensity?Balsc Bals BalscОценок пока нет
- Lecture 3 PsychopharmacologyДокумент99 страницLecture 3 PsychopharmacologyPavan chowdaryОценок пока нет
- Hospitalization and Its Effect For Patient - UNTAD 2011 PDFДокумент26 страницHospitalization and Its Effect For Patient - UNTAD 2011 PDFRiris SutrisnoОценок пока нет
- Gynera: Coated TabletsДокумент67 страницGynera: Coated TabletsOdeke VascoОценок пока нет
- Abnormal Urinalysis Children-Tadulako2015Документ33 страницыAbnormal Urinalysis Children-Tadulako2015Yeyen Hastriam AkramОценок пока нет
- Maklumat Vaksinasi: Vaccination DetailsДокумент2 страницыMaklumat Vaksinasi: Vaccination DetailsNORFADHLI ARIFОценок пока нет
- IleusДокумент10 страницIleusChyndi DamiОценок пока нет
- Refresher Course: Preboard Examination Nursing Practice III: Care of Clients With Physiologic and Psychosocial Alterations (Part A)Документ9 страницRefresher Course: Preboard Examination Nursing Practice III: Care of Clients With Physiologic and Psychosocial Alterations (Part A)Jastine Sabornido0% (1)
- Isid Guide Ipc in The Radiology DepartmentДокумент24 страницыIsid Guide Ipc in The Radiology DepartmentYennitaSatumalayОценок пока нет
- Participant Final Exam Answer Sheet: Emergency First Response Primary Care (CPR)Документ2 страницыParticipant Final Exam Answer Sheet: Emergency First Response Primary Care (CPR)Zirak Maan HussamiОценок пока нет
- B Auch Muller 2015Документ7 страницB Auch Muller 2015AdityaОценок пока нет
- (Lecture 4) Vice, Drug Education and ControlДокумент25 страниц(Lecture 4) Vice, Drug Education and ControlJohnpatrick DejesusОценок пока нет
- Oncology Scope of ServicesДокумент2 страницыOncology Scope of ServicesJaisurya SharmaОценок пока нет
- Bisphosphonate Treatment Break Guidance June 2017Документ2 страницыBisphosphonate Treatment Break Guidance June 2017Usman Zafar QaziОценок пока нет
- Getting The Most Out of The Fit Note GP GuidanceДокумент28 страницGetting The Most Out of The Fit Note GP GuidanceLaurensia Erlina NataliaОценок пока нет
- Blood CirculationДокумент42 страницыBlood CirculationAshu kumar100% (1)