Академический Документы
Профессиональный Документы
Культура Документы
Diabetes - Neuropathy
Загружено:
Isnawan WidyayantoАвторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Diabetes - Neuropathy
Загружено:
Isnawan WidyayantoАвторское право:
Доступные форматы
Diabetic Neuropathy Approximately 60% of Diabetics will develop a form of neuropathy despite tight glucose control on or after 5 years
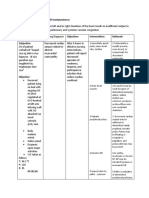
of diagnosis. The occurrence increases to 90% with lack of tight glucose control on or after 5 years of diagnosis. Diabetic Neuropathy may occur in three types of peripheral nerves: Sensory Motor Autonomic Neuropathy can be symmetrical or asymmetrical in nature, and may also affect a single joint or multiple joints. The most common form of neuropathy is symmetrical in nature. The location of neuropathy can occur anywhere along the path of the given nerve; e.g. proximal versus distal. Distal neuropathy is the most common. The most common form of neuropathy involves the lower extremities / feet. Common forms and signs and symptoms of neuropathies include the following Sensory nerves: numbness, tingling, pain, loss of proprioception and vibration Motor nerves: loss of muscle mass, loss of motor function, foot drop Autonomic Nerves: Stomach Intestines Bladder Sexual Organs o bloating, nausea, vomiting o diarrhea, constipation o urinary incontinence, urinary tract infections o erectile dysfunction, vaginal dryness
If diabetic neuropathies of the lower extremities / feet is present, chances are other forms of neuropathy already exist. Consider the following examples when the patient presents with peripheral neuropathy of the feet: the patient complained of bloating and vomiting after eating, gastroparesis could possible be the culprit; the patient has frequent bouts of urinary tract infection, and overflow incontinence, neurogenic bladder could be the possible culprit.
The common problems encountered with diabetic neuropathy of the lower extremities / feet include the following: Skin changes due to the nerves inability to produce oil and lack of moisture control, dryness and flakiness being the most common Calluses are easily formed usually due to improper footwear or an abnormal gait. Calluses need to be addressed because if allowed to deteriorate they will form an open sore. Podiatric services is a vital intervention for calluses. Poor circulation usually demonstrates proximal to distal cooling of the lower extremities. This is a potential problem because a patient may try to warm the feet with water that is too hot or wear socks that may promote falls. We know what poor circulation does to normal wound healing, usually doubling the normal healing process timeframe. Smoking is a huge problem too if poor circulation already exists, usually tripling the normal healing process timeframe. Intermittent claudication is a usual phenomenon.
There is a high correlation with smoking and non-traumatic amputations in the diabetic population. Ulcer formation is a big problem associated with diabetic neuropathy of the lower extremities / feet. Improper care of the web spaces (wetness due to improper drying or using oils and lotions), calluses, abnormal pressure areas on parts of the feet (improper footwear), or traumatic lesions like stepping on a small pebble or sharp objects (usually due to not wearing appropriate footwear). Amputations of toes, the metatarsal area, and/or foot, leads to increased vulnerability to falls due to imbalance and/or impaired mobility. Nailbeds are usually dystrophic (thickened) and mycotic (fungus usually causing yellowing of the nail.) Proper care of nails is essential to preventing ulcerations of surrounding tissue and infections of the nailbeds.
The American Diabetic Association recommends inspecting the feet daily by the patient/caregiver. It is prudent for us to address assessment of the lower extremities if nursing is providing daily skilled nursing visits for insulin administration and/or finger-stick blood sugar analysis. It could be as simple as asking the patient if he/she has pain or numbness, evaluating that proper footwear is present, and assessing proper muscle strength and ambulation of the lower extremities / feet as they see the patient walk. With this in mind, I created the modified integumentary system and possible options for the nurse to choose, relative to assessment parameters that are normally associated with daily nursing interventions. I stayed away from acute situations like moderate to severe pain or burning, ulcers, infections, vomiting, diarrhea, or incontinence because these should be addressed through appropriate NDPs, as they are not normal variations associated with assessment findings of neuropathy. It is also noted that tingling, pain and prickling like sensations may not always be a negative outcome, or evidence of deterioration. Consider this example: The patient has complete numbness, no pain and bilateral foot drop. Vitamin B12 injections are started along with physical therapy. As nerves regenerate at approximately an inch per month, the patient starts developing prickling sensations, and some intermittent pain sensations. In this situation this is a good outcome. Controlling the pain is still important but can controlled with appropriate medications.
Вам также может понравиться
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Serum BDNF Levels in Post Stroke Depression-Li2014Документ7 страницSerum BDNF Levels in Post Stroke Depression-Li2014Isnawan WidyayantoОценок пока нет
- Assessment and Management of Acute Low Back PainДокумент12 страницAssessment and Management of Acute Low Back PainIsnawan WidyayantoОценок пока нет
- LGS MedscapeДокумент14 страницLGS MedscapeIsnawan WidyayantoОценок пока нет
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Evaluation of Homocysteine Level As A RiskДокумент7 страницEvaluation of Homocysteine Level As A RiskIsnawan WidyayantoОценок пока нет
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Serum BDNF Levels in Post Stroke Depression-Li2014Документ9 страницSerum BDNF Levels in Post Stroke Depression-Li2014Isnawan WidyayantoОценок пока нет
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Disorders of The Spinal CordДокумент9 страницDisorders of The Spinal CordIsnawan WidyayantoОценок пока нет
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- Dietary Fiber and CardiovascularДокумент12 страницDietary Fiber and CardiovascularIsnawan WidyayantoОценок пока нет
- Stroke-2015-Guidelines For The Early Management of Patient With Acute Ischemic Stroke Regarding Endovasculat TreatmentДокумент17 страницStroke-2015-Guidelines For The Early Management of Patient With Acute Ischemic Stroke Regarding Endovasculat TreatmentIsnawan WidyayantoОценок пока нет
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Stroke 2013 Qureshi S67 9Документ4 страницыStroke 2013 Qureshi S67 9Isnawan WidyayantoОценок пока нет
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- UNAIDS Global Report 2013 enДокумент198 страницUNAIDS Global Report 2013 enWindy MentariiОценок пока нет
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Effectiveness, TolerabilityДокумент38 страницEffectiveness, TolerabilityIsnawan WidyayantoОценок пока нет
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- Referensi OAДокумент36 страницReferensi OAIsnawan WidyayantoОценок пока нет
- Stroke-2015-Guidelines For The Management of Patients With Unruptured Intracranial AneurysmsДокумент36 страницStroke-2015-Guidelines For The Management of Patients With Unruptured Intracranial AneurysmsIsnawan WidyayantoОценок пока нет
- Core Epidemiological Slides HIV/AIDS Estimates: July 2014Документ11 страницCore Epidemiological Slides HIV/AIDS Estimates: July 2014Isnawan WidyayantoОценок пока нет
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- Tolosa Hunt MedscapeДокумент8 страницTolosa Hunt MedscapeIsnawan WidyayantoОценок пока нет
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Stroke 2006 Tsivgoulis 1913 6Документ5 страницStroke 2006 Tsivgoulis 1913 6Isnawan WidyayantoОценок пока нет
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- Dietary Fiber and Coronary Heart DiseaseДокумент7 страницDietary Fiber and Coronary Heart DiseaseIsnawan WidyayantoОценок пока нет
- Referensi OAДокумент36 страницReferensi OAIsnawan WidyayantoОценок пока нет
- MikrobiologiДокумент11 страницMikrobiologiIsnawan WidyayantoОценок пока нет
- Epilepsy Surgery in Indonesia Achieving Better Result With Limited ResourcesДокумент6 страницEpilepsy Surgery in Indonesia Achieving Better Result With Limited ResourcesIsnawan WidyayantoОценок пока нет
- THS JurnalДокумент7 страницTHS JurnalIsnawan WidyayantoОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Prevention of Varicella: Recommendations of The Advisory Committee On Immunization Practices (ACIP)Документ35 страницPrevention of Varicella: Recommendations of The Advisory Committee On Immunization Practices (ACIP)Isnawan WidyayantoОценок пока нет
- Treatmentofaneurysmalsubarachnoidhemorrhage 090823220241 Phpapp02Документ17 страницTreatmentofaneurysmalsubarachnoidhemorrhage 090823220241 Phpapp02Isnawan WidyayantoОценок пока нет
- Factor Xiii MedscapeДокумент35 страницFactor Xiii MedscapeIsnawan WidyayantoОценок пока нет
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- HopeДокумент21 страницаHopeIsnawan WidyayantoОценок пока нет
- Dr. Retna-New Antiplatelet For Secondary Stroke PreventionДокумент40 страницDr. Retna-New Antiplatelet For Secondary Stroke PreventionIsnawan WidyayantoОценок пока нет
- OsteoarthritisДокумент25 страницOsteoarthritisVidyani AdiningtyasОценок пока нет
- Effectiveness, TolerabilityДокумент38 страницEffectiveness, TolerabilityIsnawan WidyayantoОценок пока нет
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (120)
- American College of Rheumatology 2012 Recommendations For The Use of Nonpharmacologic and Pharmacologic Therapies in Osteoarthritis of The Hand, Hip, and KneeДокумент10 страницAmerican College of Rheumatology 2012 Recommendations For The Use of Nonpharmacologic and Pharmacologic Therapies in Osteoarthritis of The Hand, Hip, and KneeAissyiyah Nur An NisaОценок пока нет
- Sudeep SrivastavaДокумент202 страницыSudeep Srivastavasandeepsrivastava41Оценок пока нет
- Feeding Disorders in ChildrenДокумент65 страницFeeding Disorders in Childrendrhananfathy100% (5)
- Ginjal Polikistik PDFДокумент15 страницGinjal Polikistik PDFAgunkRestuMaulanaОценок пока нет
- Immune Response To Infectious DiseaseДокумент2 страницыImmune Response To Infectious Diseasekiedd_04100% (1)
- CHF NCPДокумент8 страницCHF NCPZy Hallasgo100% (1)
- Droplet InfectionsДокумент11 страницDroplet InfectionsdevОценок пока нет
- Cover LetterДокумент1 страницаCover Letterapi-400385739Оценок пока нет
- Diabetesmeds AcceptablecombДокумент2 страницыDiabetesmeds AcceptablecombCotton LogicОценок пока нет
- HeartburnДокумент76 страницHeartburnRock ArtadiОценок пока нет
- Perineal Urethrostomy PUДокумент2 страницыPerineal Urethrostomy PUclara FОценок пока нет
- Int Endodontic J - 2022 - Shah - Outcomes Reporting in Systematic Reviews On Surgical Endodontics A Scoping Review For TheДокумент22 страницыInt Endodontic J - 2022 - Shah - Outcomes Reporting in Systematic Reviews On Surgical Endodontics A Scoping Review For TheDhiaa AloweadatОценок пока нет
- 5,600 Residents Tested: Case SummaryДокумент3 страницы5,600 Residents Tested: Case SummaryPeterborough ExaminerОценок пока нет
- Comparision US UK Japan RegulationsДокумент5 страницComparision US UK Japan RegulationsProschool HyderabadОценок пока нет
- Antenatal Care: Muhammad Wasil Khan and Ramsha MazharДокумент55 страницAntenatal Care: Muhammad Wasil Khan and Ramsha MazharmarviОценок пока нет
- West African Journal of Medicine: Volume 40, Number 1 January 2023Документ12 страницWest African Journal of Medicine: Volume 40, Number 1 January 2023ThankGod OgbonnaОценок пока нет
- De Baras - Topic and Sentence OutlineДокумент1 страницаDe Baras - Topic and Sentence OutlineMyline Toledo DavadОценок пока нет
- UBYT 2019 Yılı Dergi - ListesiДокумент904 страницыUBYT 2019 Yılı Dergi - ListesicemalОценок пока нет
- Animal Care QP U1Документ12 страницAnimal Care QP U1boho14Оценок пока нет
- The Effect of Mangosteen (Garcinia Mangostana) Rind in The Blood Glucose Levels of Adult Patients With Type 2 Diabetes MellitusДокумент4 страницыThe Effect of Mangosteen (Garcinia Mangostana) Rind in The Blood Glucose Levels of Adult Patients With Type 2 Diabetes MellitusFiqoh Puteri FauziОценок пока нет
- Assignment On DislysisДокумент10 страницAssignment On DislysisSanhati Ghosh Banerjee100% (1)
- MPC-CPN Basics of Toxicology-HДокумент12 страницMPC-CPN Basics of Toxicology-HNahid ParveenОценок пока нет
- A Childbirth Cheat Sheet For Dads-To-be - Baby CenterДокумент3 страницыA Childbirth Cheat Sheet For Dads-To-be - Baby CenterDrhtrth AsdfghsfgОценок пока нет
- 253 Complexes For Biomedis Trinity - DescriptionДокумент74 страницы253 Complexes For Biomedis Trinity - Descriptionjanhendrik4444100% (1)
- Gwen Watego (New)Документ3 страницыGwen Watego (New)Duan Tian0% (1)
- Pediatric Musculoskeletal Summary For Osce ExamДокумент53 страницыPediatric Musculoskeletal Summary For Osce Examopscurly100% (2)
- Patient Delivery Receipt: Product Delivery Location: FacilityДокумент1 страницаPatient Delivery Receipt: Product Delivery Location: FacilityPat Dela CruzОценок пока нет
- NCP EsrdДокумент9 страницNCP EsrdMarisol Dizon100% (1)
- Dermatological Signs in Wilson's DiseaseДокумент4 страницыDermatological Signs in Wilson's DiseaseGingerWiseОценок пока нет
- ArtherosclerosisДокумент23 страницыArtherosclerosistanyagargОценок пока нет
- Allen Part Pedia CaseДокумент3 страницыAllen Part Pedia CasePaul Michael Baguhin0% (1)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeОт EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeРейтинг: 2 из 5 звезд2/5 (1)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОт EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsОценок пока нет
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisОт EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisРейтинг: 4.5 из 5 звезд4.5/5 (42)
- The Age of Magical Overthinking: Notes on Modern IrrationalityОт EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityРейтинг: 4 из 5 звезд4/5 (24)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4 из 5 звезд4/5 (3)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedОт EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedРейтинг: 5 из 5 звезд5/5 (80)