Академический Документы
Профессиональный Документы
Культура Документы
Hydatidiform Mole
Загружено:
Irfan HardiИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Hydatidiform Mole
Загружено:
Irfan HardiАвторское право:
Доступные форматы
Background
Gestational trophoblastic disease encompasses several disease processes that originate in the placenta. These include complete and partial moles, placental site trophoblastic tumors, choriocarcinomas, and invasive moles. Almost all women with malignant gestational trophoblastic disease can be cured with preservation of reproductive function. The following discussion is limited to hydatidiform moles (complete and partial).
Pathophysiology
A complete mole contains no fetal tissue. Ninety percent are 46,XX, and 10% are 46,XY.[1, 2] Complete moles can be divided into 2 types:
Androgenetic complete mole o Homozygous These account for 80% of complete moles. Two identical paternal chromosome complements, derived from duplication of the paternal haploid chromosomes. Always female; 46,YY has never been observed. o Heterozygous These account for 20% of complete moles. May be male or female. All chromosomes are of parental origin, most likely due to dispermy. Biparental complete mole: Maternal and paternal genes are present but failure of maternal imprinting causes only the paternal genome to be expressed.[3] o The biparental complete mole is rare. o A recurrent form of biparental mole, which is familial and appears to be inherited as an autosomal recessive trait, has been described. Al-Hussaini describes a series of 5 women with as many as 9 consecutive molar pregnancies.[4, 5] o Mutations in NLRP7 at 19q13.4 have been identified as causative in recurrent molar pregnancies.[6, 7, 8]
With a partial mole, fetal tissue is often present. Fetal erythrocytes and vessels in the villi are a common finding. The chromosomal complement is 69,XXX or 69,XXY.[9] This results from fertilization of a haploid ovum and duplication of the paternal haploid chromosomes or from dispermy. Tetraploidy may also be encountered. As in a complete mole, hyperplastic trophoblastic tissue and swelling of the chorionic villi occur.
Epidemiology
Frequency
United States
By studying elective pregnancy terminations, hydatidiform moles were determined to occur in approximately 1 in 1200 pregnancies.[10] International The reported frequency of hydatidiform mole varies greatly. Some of this variability can be explained by differences in methodology (eg, single hospital vs population studies, identification of cases). The reported frequencies range from 1 in 100 pregnancies in Indonesia to 1 in 200 pregnancies in Mexico to 1 in 5000 pregnancies in Paraguay.[11] The study of pathologic material from first- and second-trimester abortions established a frequency of complete and partial hydatidiform moles in Ireland of 1 per 1945 pregnancies and 1 per 695 pregnancies, respectively.[12]
Mortality/Morbidity
A hydatidiform mole is considered malignant if metastases or destructive invasion of the myometrium (ie, invasive mole) occurs, or when the serum hCG levels plateau or rise during the period of follow-up and an intervening pregnancy is excluded. Malignancy (see eMedicine's article Gestational Trophoblastic Neoplasia) is diagnosed in 15-20% of patients with a complete hydatidiform mole and 2-3% of partial moles.[13, 14] Lung metastases are found in 4-5% of patients with a complete hydatidiform mole and rarely in cases of partial hydatidiform moles.[15,
16]
Race
Differences in the frequency of hydatidiform moles between ethnic groups have been reported internationally.[11, 17] In the United States, comparison of frequency of hydatidiform moles in African Americans and Caucasians have yielded conflicting results.[17] If differences exist, whether they are due to genetic differences or environmental factors is not clear.
Sex
Hydatidiform mole is a disease of pregnancy and therefore a disease of women. See Medscape's Pregnancy Resource Center.
Age
Hydatidiform mole is more common at the extremes of reproductive age. Women in their early teenage or perimenopausal years are most at risk.[18, 19, 20, 11, 17] Women older than 35 years have a 2-fold increase in risk. Women older than 40 years experience a 5- to 10-fold increase in risk compared to younger women. Parity does not affect the risk.
Вам также может понравиться
- Hydatidiform Mole: BackgroundДокумент11 страницHydatidiform Mole: BackgroundIlham TaufanОценок пока нет
- E MedicineДокумент10 страницE MedicineAnggie Pradetya MaharaniОценок пока нет
- Hydatidiform MoleДокумент17 страницHydatidiform MoleRitamariaОценок пока нет
- Molar PregnancyДокумент7 страницMolar PregnancyFelix Valerian HalimОценок пока нет
- Gestational Trophoblastic DiseaseДокумент23 страницыGestational Trophoblastic DiseasemmamloukОценок пока нет
- Molar Pregnancy Is An Abnormal Form ofДокумент26 страницMolar Pregnancy Is An Abnormal Form ofRanjita GhimireОценок пока нет
- CP Hydatidiform MoleДокумент13 страницCP Hydatidiform Molesweetheart_joannieОценок пока нет
- Pci 3.1Документ2 страницыPci 3.1boxclowneraserОценок пока нет
- Gestational Trophoblastic DiseaseДокумент43 страницыGestational Trophoblastic DiseaseHoney May Rollan VicenteОценок пока нет
- Causes: Gestational Trophoblastic Disease ChoriocarcinomaДокумент7 страницCauses: Gestational Trophoblastic Disease ChoriocarcinomajudssalangsangОценок пока нет
- GTD Case StudyДокумент9 страницGTD Case StudyZnarf Izlah Sadanreb100% (1)
- Enf Trofoblastica GestacionalДокумент12 страницEnf Trofoblastica GestacionalVíctor LaraОценок пока нет
- بیماری تروفوبلستیک بارداریДокумент44 страницыبیماری تروفوبلستیک بارداریrazvanОценок пока нет
- Research ArticleДокумент8 страницResearch ArticleJeromeОценок пока нет
- Analysis of Patients With Recurrent Molar Pregnancy in Tertiary Care HospitalДокумент3 страницыAnalysis of Patients With Recurrent Molar Pregnancy in Tertiary Care HospitalAl MubartaОценок пока нет
- Mola Hidatidosa1 PDFДокумент8 страницMola Hidatidosa1 PDFKoas PatoОценок пока нет
- Jurnal Mola HidatidosaДокумент8 страницJurnal Mola HidatidosaDebby SofianaОценок пока нет
- Histological Diagnosis of Hydatidiform Moles: Histological Changes of Complete and Partial Moles AreДокумент8 страницHistological Diagnosis of Hydatidiform Moles: Histological Changes of Complete and Partial Moles AreClareen JuanicoОценок пока нет
- Hydatidiform Mole: AuthorsДокумент7 страницHydatidiform Mole: AuthorsIdo KurniawanОценок пока нет
- Trophoblastic and Pregnancy: DiseasesДокумент6 страницTrophoblastic and Pregnancy: DiseasesKonstantinos PapadakisОценок пока нет
- Gestational Trophoblastic DiseaseДокумент30 страницGestational Trophoblastic DiseaseInstrukcije Seminari100% (1)
- Seminar: Michael J Seckl, Neil J Sebire, Ross S BerkowitzДокумент13 страницSeminar: Michael J Seckl, Neil J Sebire, Ross S BerkowitzFelicia HalimОценок пока нет
- Molar Pregnancy: Presented byДокумент87 страницMolar Pregnancy: Presented bysanjay kashyapОценок пока нет
- Hydatidiform Mole - OverviewДокумент4 страницыHydatidiform Mole - Overviewannmanalad9438Оценок пока нет
- Enf TrofoblasticaДокумент10 страницEnf TrofoblasticaDaniela CovarrubiasОценок пока нет
- Vesicular Mole: Dr. Mohammed Abdalla Egypt, Domiat G. HospitalДокумент32 страницыVesicular Mole: Dr. Mohammed Abdalla Egypt, Domiat G. HospitalPrathibha GuruguriОценок пока нет
- Gestational Trophoblastic Disease (GTD)Документ72 страницыGestational Trophoblastic Disease (GTD)Mohammad BelbahaithОценок пока нет
- OB - Gestational Trophoblastic Disease (JCR)Документ5 страницOB - Gestational Trophoblastic Disease (JCR)gellie gellesОценок пока нет
- Unit 7 - Vesicular MoleДокумент43 страницыUnit 7 - Vesicular MoleN. Siva100% (1)
- Gestational Trophoblastic Disease (Neha Martin Msc. NSG 2nd Year)Документ13 страницGestational Trophoblastic Disease (Neha Martin Msc. NSG 2nd Year)Gunu SinghОценок пока нет
- Vesicular Mole: Dr. Mohammed Abdalla Egypt, Domiat G. HospitalДокумент32 страницыVesicular Mole: Dr. Mohammed Abdalla Egypt, Domiat G. Hospitalmadmax500Оценок пока нет
- 4doc 20221027 Wa0062Документ6 страниц4doc 20221027 Wa0062TUGAS ILMIAHОценок пока нет
- Molarpregnancy 160623022400Документ89 страницMolarpregnancy 160623022400BHAKTI KASHYAPОценок пока нет
- GTD Clinic Guide For CliniciansДокумент23 страницыGTD Clinic Guide For CliniciansesjayemОценок пока нет
- Gestational Trophoblastic NeoplasiaДокумент18 страницGestational Trophoblastic NeoplasiaTanuj sai kumarОценок пока нет
- Vesicular MoleДокумент27 страницVesicular MolePadmaОценок пока нет
- Mola Hidatidosa NcbiДокумент4 страницыMola Hidatidosa NcbiRekno DwiОценок пока нет
- ABORTIONДокумент22 страницыABORTIONcacaОценок пока нет
- 181919-Article Text-463719-1-10-20190115Документ7 страниц181919-Article Text-463719-1-10-20190115Crissan Jejomar AbanesОценок пока нет
- GTD For CIsДокумент82 страницыGTD For CIsDegefaw BikoyОценок пока нет
- Ijgo 13877Документ8 страницIjgo 13877rutujaОценок пока нет
- Chapter 20Документ21 страницаChapter 20M Rama Anshorie100% (1)
- Gestational Trophoblastic Disease WordДокумент3 страницыGestational Trophoblastic Disease WordsahaniОценок пока нет
- An Update On Gestational Trophoblastic DiseaseДокумент9 страницAn Update On Gestational Trophoblastic DiseaseFellita Ratri AОценок пока нет
- Recurrent MiscarriageДокумент6 страницRecurrent MiscarriageuzmajbnОценок пока нет
- Enfermedad Trofoblastica GestacionalДокумент11 страницEnfermedad Trofoblastica GestacionalClaudia Emilce TalaveraОценок пока нет
- Gestational Trophoblastic DiseaseДокумент40 страницGestational Trophoblastic DiseaseAayupta Mohanty100% (2)
- Chapter 4 PathologyДокумент54 страницыChapter 4 Pathologykristinenidoy.mdОценок пока нет
- Gestational Trophoblastic DiseasesДокумент76 страницGestational Trophoblastic DiseasesJhon NegesseОценок пока нет
- Dun 2012Документ16 страницDun 2012Anonymous c4GVTgkvОценок пока нет
- 10.1515 - Med 2019 0098Документ4 страницы10.1515 - Med 2019 0098fansofiuОценок пока нет
- Congenital Cytogenetic Abnormalities - UpToDateДокумент34 страницыCongenital Cytogenetic Abnormalities - UpToDateIzamar RomeroОценок пока нет
- Louise Wilkins-Haug, MD, PHD Deborah Levine, MD Helen V Firth, DM, FRCP, DCH Vanessa A Barss, MD, Facog Contributor Disclosures Peer Review ProcessДокумент10 страницLouise Wilkins-Haug, MD, PHD Deborah Levine, MD Helen V Firth, DM, FRCP, DCH Vanessa A Barss, MD, Facog Contributor Disclosures Peer Review ProcessArienne_Mae_A__6554Оценок пока нет
- First Page PDFДокумент1 страницаFirst Page PDFAmenОценок пока нет
- Diagnosis and Treatment of Gestational Trophoblastic Disease PDFДокумент11 страницDiagnosis and Treatment of Gestational Trophoblastic Disease PDFAlexeySAgОценок пока нет
- Vascular Anomalies in Pediatrics 2012 Surgical Clinics of North AmericaДокумент32 страницыVascular Anomalies in Pediatrics 2012 Surgical Clinics of North AmericaAntonio TovarОценок пока нет
- Chapter 3 EpidemiologyДокумент39 страницChapter 3 Epidemiologykristinenidoy.mdОценок пока нет
- Hydatidiform MoleДокумент10 страницHydatidiform MoleLisa TurnerОценок пока нет
- Research Journal of Obstetrics & Gynecology: ISSN 1994-7925Документ6 страницResearch Journal of Obstetrics & Gynecology: ISSN 1994-7925Mauro Porcel de PeraltaОценок пока нет
- An Interocclusal Recording Method For The Fabrication of Full-Arch Implant-Retained RestorationsДокумент9 страницAn Interocclusal Recording Method For The Fabrication of Full-Arch Implant-Retained RestorationsDr FarhatОценок пока нет
- Post Basic B.SC - Question PapersДокумент55 страницPost Basic B.SC - Question PapersArchana YadavОценок пока нет
- Hokororo J PDFДокумент76 страницHokororo J PDFMutianaUmminyaKhanzaОценок пока нет
- Tiffany Thomas RN ResumeДокумент2 страницыTiffany Thomas RN Resumeapi-283689862Оценок пока нет
- Group 1 Research StemДокумент55 страницGroup 1 Research StemMary AtilloОценок пока нет
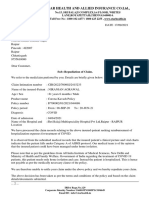
- Star Health and Allied Insurance Co - LTD.Документ2 страницыStar Health and Allied Insurance Co - LTD.AshokОценок пока нет
- Proc Edur e 5 4 3 2 1: Prenatal Check-UpДокумент60 страницProc Edur e 5 4 3 2 1: Prenatal Check-UpCharlie DyОценок пока нет
- Kristal Jade Y. Esquillo: Personal DataДокумент3 страницыKristal Jade Y. Esquillo: Personal DataChristian EsquilloОценок пока нет
- MID1112ra DavaoДокумент32 страницыMID1112ra DavaoNonoyTaclinoОценок пока нет
- Restoration of Body Focussing On NumbersДокумент95 страницRestoration of Body Focussing On Numbersssss87va93% (27)
- Walz Executive Order On Avian Influence Sept. 28, 2022Документ3 страницыWalz Executive Order On Avian Influence Sept. 28, 2022inforumdocsОценок пока нет
- Review of Related Literature: COVID-19Документ17 страницReview of Related Literature: COVID-19Ed Anthony YubacОценок пока нет
- Books For Mrcog Part1Документ2 страницыBooks For Mrcog Part1srini100% (3)
- Epidemiologic Study Designs: Dr. Sunita Dodani Assistant Professor Family Medicine, CHSДокумент23 страницыEpidemiologic Study Designs: Dr. Sunita Dodani Assistant Professor Family Medicine, CHSShubha DavalgiОценок пока нет
- Myers CocktailДокумент15 страницMyers CocktailViladosgirassois Couto PinonОценок пока нет
- Clinical Trial of GenomindДокумент7 страницClinical Trial of GenomindThomas CarswellОценок пока нет
- Brushing Teeth and RecessionДокумент16 страницBrushing Teeth and RecessionWayan SubadiОценок пока нет
- Afast TfastДокумент7 страницAfast TfastEduardo LeónОценок пока нет
- Coc and PopДокумент22 страницыCoc and PopAhmed Mohammed omarОценок пока нет
- Pengalaman Psikososial Pasien Kanker Pay 00bf7b25Документ16 страницPengalaman Psikososial Pasien Kanker Pay 00bf7b25Heru JatmikaОценок пока нет
- Anestesi LaparoskopiДокумент65 страницAnestesi LaparoskopiArief Hariyadi SantosoОценок пока нет
- COPD Case PresentationДокумент15 страницCOPD Case PresentationBola Kwentua29% (7)
- The Recent History of AcupunctureДокумент2 страницыThe Recent History of AcupunctureBhaskaranОценок пока нет
- Shs g12 Peh 3 w1 w2q2 Summative AssessmentДокумент6 страницShs g12 Peh 3 w1 w2q2 Summative AssessmentVERDADERO LevisthoneОценок пока нет
- RRQRQ: 3ttgffihrr National Medical Medical EducationДокумент2 страницыRRQRQ: 3ttgffihrr National Medical Medical EducationF LalramluahpuiaОценок пока нет
- PhRMA Marketing Brochure Influences On Prescribing FINALДокумент12 страницPhRMA Marketing Brochure Influences On Prescribing FINALJalwaz TihamiОценок пока нет
- Nebulization 1Документ3 страницыNebulization 1Shane Aileen AngelesОценок пока нет
- Form 1 - Classroom Level: School Based Deworming Accomplishment Report (1St Round/) ELEMENTARY SY2022-2023Документ12 страницForm 1 - Classroom Level: School Based Deworming Accomplishment Report (1St Round/) ELEMENTARY SY2022-2023Nicko David DaagОценок пока нет
- Enoxaparin - Prescribing, Administration and MonitoringДокумент6 страницEnoxaparin - Prescribing, Administration and MonitoringFaheem AlsabriaОценок пока нет
- Catheter Care Guidelines (By ANZUS)Документ19 страницCatheter Care Guidelines (By ANZUS)cateterdoblejota100% (1)
- Dark Matter and the Dinosaurs: The Astounding Interconnectedness of the UniverseОт EverandDark Matter and the Dinosaurs: The Astounding Interconnectedness of the UniverseРейтинг: 3.5 из 5 звезд3.5/5 (69)
- 10% Human: How Your Body's Microbes Hold the Key to Health and HappinessОт Everand10% Human: How Your Body's Microbes Hold the Key to Health and HappinessРейтинг: 4 из 5 звезд4/5 (33)
- Return of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseОт EverandReturn of the God Hypothesis: Three Scientific Discoveries That Reveal the Mind Behind the UniverseРейтинг: 4.5 из 5 звезд4.5/5 (52)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisОт EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisРейтинг: 3.5 из 5 звезд3.5/5 (2)
- Why We Die: The New Science of Aging and the Quest for ImmortalityОт EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityРейтинг: 4.5 из 5 звезд4.5/5 (6)
- Alex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessОт EverandAlex & Me: How a Scientist and a Parrot Discovered a Hidden World of Animal Intelligence—and Formed a Deep Bond in the ProcessОценок пока нет
- Periodic Tales: A Cultural History of the Elements, from Arsenic to ZincОт EverandPeriodic Tales: A Cultural History of the Elements, from Arsenic to ZincРейтинг: 3.5 из 5 звезд3.5/5 (137)
- The Rise and Fall of the Dinosaurs: A New History of a Lost WorldОт EverandThe Rise and Fall of the Dinosaurs: A New History of a Lost WorldРейтинг: 4 из 5 звезд4/5 (597)
- A Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsОт EverandA Brief History of Intelligence: Evolution, AI, and the Five Breakthroughs That Made Our BrainsРейтинг: 4.5 из 5 звезд4.5/5 (6)
- The Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorОт EverandThe Other Side of Normal: How Biology Is Providing the Clues to Unlock the Secrets of Normal and Abnormal BehaviorОценок пока нет
- Tales from Both Sides of the Brain: A Life in NeuroscienceОт EverandTales from Both Sides of the Brain: A Life in NeuroscienceРейтинг: 3 из 5 звезд3/5 (18)
- Who's in Charge?: Free Will and the Science of the BrainОт EverandWho's in Charge?: Free Will and the Science of the BrainРейтинг: 4 из 5 звезд4/5 (65)
- The Revolutionary Genius of Plants: A New Understanding of Plant Intelligence and BehaviorОт EverandThe Revolutionary Genius of Plants: A New Understanding of Plant Intelligence and BehaviorРейтинг: 4.5 из 5 звезд4.5/5 (138)
- Undeniable: How Biology Confirms Our Intuition That Life Is DesignedОт EverandUndeniable: How Biology Confirms Our Intuition That Life Is DesignedРейтинг: 4 из 5 звезд4/5 (11)
- Gut: the new and revised Sunday Times bestsellerОт EverandGut: the new and revised Sunday Times bestsellerРейтинг: 4 из 5 звезд4/5 (393)
- Good Without God: What a Billion Nonreligious People Do BelieveОт EverandGood Without God: What a Billion Nonreligious People Do BelieveРейтинг: 4 из 5 звезд4/5 (66)
- The Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionОт EverandThe Ancestor's Tale: A Pilgrimage to the Dawn of EvolutionРейтинг: 4 из 5 звезд4/5 (812)
- Water: The Epic Struggle for Wealth, Power, and CivilizationОт EverandWater: The Epic Struggle for Wealth, Power, and CivilizationРейтинг: 3.5 из 5 звезд3.5/5 (37)
- Buddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomОт EverandBuddha's Brain: The Practical Neuroscience of Happiness, Love & WisdomРейтинг: 4 из 5 звезд4/5 (216)
- A Series of Fortunate Events: Chance and the Making of the Planet, Life, and YouОт EverandA Series of Fortunate Events: Chance and the Making of the Planet, Life, and YouРейтинг: 4.5 из 5 звезд4.5/5 (62)
- Moral Tribes: Emotion, Reason, and the Gap Between Us and ThemОт EverandMoral Tribes: Emotion, Reason, and the Gap Between Us and ThemРейтинг: 4.5 из 5 звезд4.5/5 (116)