Академический Документы
Профессиональный Документы
Культура Документы
Diabetes Effec On Wound Healing
Загружено:
Dennis CobbИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Diabetes Effec On Wound Healing
Загружено:
Dennis CobbАвторское право:
Доступные форматы
p41-47w45_ART&SCIENCE 11/07/2011 10:51 Page 41
art & science diabetes
&
Diabetes and its effects on wound healing
Sharp A, Clark J (2011) Diabetes and its effects on wound healing. Nursing Standard. 25, 45, 41-47. Date of acceptance: October 1 2010.
Summary
This article discusses the reasons why wounds in people with diabetes take longer to heal and are more susceptible to complications. The physiology of the wound healing process, and how this is affected by diabetes, is outlined. The article also explains why wounds in patients with diabetes are more prone to infection and discusses preventive measures.
Authors
Ailsa Sharp, lecturer in adult nursing, Edinburgh Napier University, and Jane Clark, clinical support manager, Systagenix Wound Management, Gatwick, Surrey. Email: a.sharp@napier.ac.uk
Keywords
Diabetes, infection control, wound care, wound healing These keywords are based on subject headings from the British Nursing Index. All articles are subject to external double-blind peer review and checked for plagiarism using automated software. For author and research article guidelines visit the Nursing Standard home page at www.nursing-standard.co.uk. For related articles visit our online archive and search using the keywords.
DIABETES UK estimate that 2.6 million people in the UK were known to have diabetes in 2009, with up to half a million being undiagnosed (Diabetes UK 2010). By 2025 it is estimated that four million people in the UK will have been diagnosed with diabetes (Diabetes UK 2010). Wounds can and do heal in patients with diabetes, but healing may take longer because the process is impaired (Falanga 2005). A non-healing wound is prone to complications, such as infection and trauma, which can further delay the healing process. This can have a significant negative effect on patients and their families and carers (Armstrong et al 2008), with increased patient morbidity and mortality and the economic consequences of being unable to work. One prospective study looking at quality of life showed a reduction in general health, physical functioning, physical role and vitality in patients with active foot ulceration (Ahroni and NURSING STANDARD
Boyko 2000). Nabuurs-Franssen et al (2005) showed that wound healing resulted in an improvement in patients quality of life. Diabetes mellitus is a disease that affects a persons ability to control their blood glucose levels, either because their body does not produce enough insulin or because their cells do not respond to insulin (insulin resistance) (Tortora and Derrickson 2007). Insulin is the hormone that regulates the uptake of glucose from the blood into most cells, but primarily muscle and fat cells (Dunning 2009). High blood sugar produces the classic symptoms of polyuria (frequent urination), polydipsia (excessive thirst), weight loss and lethargy. In response to rising blood glucose levels, beta cells found in the islets of Langerhans in the pancreas release insulin into the blood. This process typically happens after eating (Shier et al 2010). Insulin enables other cells in the body to absorb glucose, which is then metabolised to produce energy and glycogen. If not enough insulin is released into the bloodstream, or if the cells do not respond to the insulin being released, this results in a build-up of glucose in the bloodstream. Diabetes mellitus predisposes patients to chronic complications affecting several organs of the body, including the eye, blood vessels, kidneys and the nervous system (Ahmed 2005). It can also have a significant effect on wound healing. More than half of patients who have had a non-traumatic limb amputation have diabetes, and in a high number of cases the amputation was preceded by an ulcer or non-healing wound (Novak 2010). Intermittent claudication (cramping pain in the calf and leg muscles caused by an inadequate blood supply to the affected muscles), absent pedal pulses and ischaemic gangrene are more prevalent in people with diabetes. Diabetic foot ulcers (Figure 1) affect up to one quarter of all people with diabetes (Dunning 2009). This statistic should make wound prevention and good wound care in patients with diabetes a priority in health care. july 13 :: vol 25 no 45 :: 2011 41
p41-47w45_ART&SCIENCE 11/07/2011 10:51 Page 42
art & science diabetes
Type 1 and type 2 diabetes
There are two types of diabetes mellitus: type 1 and type 2 (Table 1). Type 1 diabetes is an autoimmune disorder in which the pancreas cannot produce insulin because the body destroys the beta cells, halting insulin secretion (Shier et al 2010). About 15% of people with diabetes have type 1 diabetes (McIntosh 2006). Symptoms usually begin before the age of 20 years, and by the time symptoms appear, 80-90% of the beta cells will have been destroyed (Tortora and Derrickson 2007).
&
FIGURE 1 Diabetic foot ulcer
If type 1 diabetes is left untreated, protein and fat will be used as an energy source instead of glucose. This results in the production of ketone bodies from fatty acid metabolism in the liver. Build up of ketone bodies lowers the pH of body fluids, resulting in diabetic ketoacidosis. This is a medical emergency and can lead to diabetic coma and death (Shier et al 2010). Type 2 diabetes develops when the body can still produce some insulin, but not enough, or when the insulin that is produced does not work effectively (known as insulin resistance). Type 2 diabetes accounts for 85% of all people with diabetes. Symptoms usually appear in people aged 40 years or more (Dunning 2009). However, it is also becoming more common in children, adolescents and young people of all ethnicities, possibly as a result of increased prevalence of obesity (Dunning 2009). Stumvoll et al (2005) suggested that the incidence of type 2 diabetes is increasing as a result of lifestyle factors such as obesity, lack of exercise and over-consumption of sugary food and drink. Type 2 diabetes is managed with a healthy diet and increased physical activity. However, medication and/or insulin is often also required.
Predisposing factors to wound development
Although wounds can affect anyone in the general population, those with diabetes have specific risk factors which make foot ulceration a particular risk. More than 100 people with diabetes have a toe or foot amputated in the UK each week; those with diabetes are 15 times more likely to have an amputation than those without (National Diabetes Support Team 2006) Identifying and taking action on risk factors that are known to cause wounds in people with diabetes may reduce their incidence and potential for loss of limb, and can also help reduce the time it takes for these wounds to heal. It is estimated
MEDISCAN
TABLE 1 Comparison of type 1 and type 2 diabetes
Type 1 diabetes Type 2 diabetes
4 Affects 15% of people with diabetes. 4 Characterised by a complete lack of insulin
production.
4 Affects 85% of people with diabetes. 4 Characterised by a relative lack of insulin production,
as a result of beta cell failure, and insulin resistance.
4 Usually affects the younger population aged
under 30 years, but can present at any age.
4 Usually affects older people aged over 40 years,
but is becoming more common in younger people.
4 Genetic predisposition not always present. 4 It is an autoimmune condition. 4 Symptoms appear rapidly.
(Adapted from McIntosh 2006)
4 Genetic predisposition can be a cause. 4 Lifestyle factors increase the risk of developing
symptoms.
4 Symptoms appear gradually.
42 july 13 :: vol 25 no 45 :: 2011
NURSING STANDARD
p41-47w45_ART&SCIENCE 11/07/2011 10:51 Page 43
that 34% of patients with diabetes who develop foot ulceration present each year with a recurrence of the ulcer (Dunning 2009). The following factors contribute to the formation and impaired healing of foot ulcers in people with diabetes (International Working Group on the Diabetic Foot 1999, Reiber et al 1999): 4 Neuropathy (leading to structural foot problems and Charcots joint). 4 Peripheral vascular disease. 4 Minor trauma. 4 History of a previous ulcer. 4 Socioeconomic status. Neuropathy Peripheral neuropathy is the cause of foot ulcers in 90% of cases (Driver et al 2007). In sensory neuropathy patients do not feel pain or discomfort to alert them to an injury. Sensory neuropathy is thought to contribute to the development of Charcots joint damaged, swollen and deformed joints resulting from repeated minor injuries of which the patient is unaware (Figure 2). The formation of Charcots joint can lead to motor neuropathy arching of the foot and clawing of the toes which alters the pressure points of the feet and causes calluses, resulting in the formation of foot ulcers at the new pressure points (Shaw and Boulton 1995, Levin 2002, Falanga 2005). Autonomic neuropathy can result in reduced sweating, which can cause the dry skin and fissures commonly seen in patients with diabetes (Meeking et al 2006). These cracks provide an entry point for bacterial and fungal infections. Fungal foot infection has been implicated as a risk factor for developing lower limb cellulitis (Bristow and Spruce 2009). Swabs are often taken TABLE 2 Risk factors for foot ulcer formation
Risk factor Neuropathy: Outcome
for bacterial culture and sensitivity in patients with cellulitis, but checking for fungal infections should also be considered. Previous ulceration, notably when linked with poor glycaemic control, smoking, alcohol consumption, self-neglect and peripheral neuropathy, increases the chance of recurrence (McIntosh 2006). Peripheral vascular disease Peripheral vascular disease occurs twice as often in people with diabetes compared with the non-diabetic population (Falanga 2005), and can occur at a younger age and progress faster than in people without diabetes (Shaw and Boulton 1995, Shaw and Boulton 2001). It has been suggested that vascular disease alone is not a common cause of ulceration; however, in conjunction with other risk factors, any minor trauma can lead to ulceration (Boulton 2006). Red blood cells consist of haemoglobin solution contained in a flexible membrane (Shin and Ku 2005), which allows red blood cells to pass through narrow capillaries. However, FIGURE 2 Charcots foot
4 Sensory 4 Motor 4 Autonomic
Peripheral vascular disease:
Reduced or absent sensation signalling damage to the tissues. Altered gait, claw toes or high arch, resulting in change in pressure points, callus development and Charcots joint (also a result of sensory neuropathy). Reduced sweating, causing cracks and fissures in the tissue, which increases potential for infection.
4 Atherosclerosis 4 Higher blood viscosity 4 Glycoslyated haemoglobin 4 Thickened basement membrane NURSING STANDARD
Narrowed lumen with reduced blood supply. Stasis of blood in small vessels. Less oxygen released to tissues. Reduced diffusion of nutrients and oxygen.
july 13 :: vol 25 no 45 :: 2011 43
WELLCOME IMAGES
p41-47w45_ART&SCIENCE 11/07/2011 10:51 Page 44
art & science diabetes
in diabetes these red blood cells are less deformable, causing vascular complications (Brown et al 1995). A higher blood viscosity caused by increased blood glucose levels results in blood becoming stagnant in the small blood vessels (Morain and Colen 1990). Glycosylated haemoglobin has a higher affinity for oxygen, which reduces the availability of oxygen for the tissues (Stadelmann et al 1998). Peripheral arterial disease is caused by the presence of atherosclerosis, in which fatty deposits accumulate and form plaques within the arteries that occlude the lumen over time. Calcification of the peripheral arteries, particularly the distal tibial vessels, is also common in patients with diabetes (McIntosh 2006). This can lead to stroke and cardiovascular disease, which in turn causes reduced mobility, and hence a greater risk of ulceration.
&
FIGURE 3 Normal stages of wound healing
Haemostasis Haemorrhage Platelet activation Complement cascade Blood clotting Haemostasis
An additional observation in people with diabetes is a thickening of the basement membrane of capillaries, known as diabetic microangiopathy. This is thought to be more prevalent in the feet because of high capillary pressures (Falanga 2005) and is linked to poor delivery of oxygen and nutrients to the tissues (Table 2). Minor trauma Traumatic damage to the tissues is often the cause of a wound. A minor trauma may cause a wound in anyone, but in those with diabetes the healing process may be compromised resulting in an ongoing chronic wound. The protective elements of sensation may be absent so the damage is unnoticed or not caught as early as it could have been. When the gait is altered pressure points build up leading to callus formation that can obscure an ulcer, increasing the risk of developing ulceration (Foster and Edmonds 2001). Recurrence of ulceration Recurrence of ulceration has been identified as an issue with 40% of those with either a new ulcer or a recurrent ulcer appearing within four months of the initial ulcer healing (Pound et al 2005). Studies suggest this is related to poor self-care and control, smoking, high alcohol consumption and peripheral neuropathy (McIntosh 2006). Socio-economic status Socio-economic status or deprivation is linked to high levels of obesity, inactivity, smoking, a poor diet and high blood pressure (Diabetes UK 2010). These factors are linked to both developing diabetes and the potential to develop complications of diabetes for those already diagnosed.
Compromised wound healing
The aim of wound healing is to reduce blood loss and prevent pathogens from entering the body (Doughty and Sparks-Defriese 2007). The stages of normal wound healing are illustrated in Figure 3. As already stated, in patients with diabetes, wounds can and do heal, but the process is impaired so may take longer (Falanga 2005). A non-healing wound is prone to complications, which can further delay the healing process. Complications that can delay wound healing are (Stadelmann et al 1998, Menke et al 2007): 4 Functional limitations, including alteration in gait and difficulty in walking. 4 Infection, including cellulitis, abscesses and osteomyelitis. 4 Gangrene and septicaemia. 4 Marjolins ulcer: carcinoma that develops within a chronic ulcer, usually a venous ulcer in the ankle region. Haemostasis is the first stage in wound healing. Following a breach in the skin and disruption NURSING STANDARD
Inflammation Cell recruitment Phagocytosis Debridement
Proliferation Release of cytokines Cell growth and activation Neovascularisation Granulation tissue formation
Maturation Wound contraction Closure Dissolution of granulation tissue Remodelling
44 july 13 :: vol 25 no 45 :: 2011
p41-47w45_ART&SCIENCE 11/07/2011 10:51 Page 45
of local blood vessels, vasoconstriction and coagulation with a platelet plug take place (Falanga 2005). However, if the area is poorly supplied with blood this process can be delayed, potentially allowing invading organisms to enter the body. The platelets release a wide range of growth factors that recruit cells to the damaged area and start the wound healing process. Reduced oxygen supply to the tissues accounts for some of the problems associated with wound healing in diabetes. Hypoxia occurs as a result of vascular changes. Hypoxia also has a role in wound infection as it affects the ability of neutrophils and macrophages to function and so allows infection to spread quickly in the diabetic wound (Falanga 2005). In some instances, hypoxia can be the cause of the wound in the first place, for example in acute arterial occlusion. Hypoxia plays a part in stimulating angiogenesis the development of new blood vessels and fibroblast proliferation in the early stages of the healing process (Stadelmann et al 1998). However, if oxygen levels do not improve with new blood vessels supplying oxygenated blood to the wound bed, then fibroblasts cannot produce collagen, resulting in impaired healing (Hunt and Pai 1972). The inflammatory phase of wound healing is impaired in people with diabetes because there is a reduced number of leucocytes at the wound site as a result of a narrowing of the blood vessels (Lioupis 2005, Kidman 2008). It has also been suggested that the phagocytic ability of leucocytes is impaired (Lioupis 2005). Kidman (2008) suggested that inflammatory cytokines remain in the diabetic wound much longer than normal to compensate for the reduced leucocyte activity, thereby perpetuating and prolonging the inflammatory phase, resulting in suppression of granulation tissue formation. During the early stages of inflammation, neutrophils in the wound site prevent microbial TABLE 3
contamination that could result in infection (Adamson 2009). Proteases and proteins are released into the wound bed (Davis 2008), which is normally a therapeutic process as proteases are needed to remove damaged components of tissue destruction and allow cell migration. The inflammatory phase is usually short lived; however, if the inflammatory phase is prolonged by poor control of proteases, the effect on wound healing can be considerable. Over time these proteases can cause oedema and local damage by destroying the new extracellular matrix (Falanga 2005). During the proliferative stage in normal wound healing, angiogenesis produces new vascular tissue to support the fibroblasts producing collagen for the extracellular matrix. However, in the patient with diabetes, this proliferation of tissue can be compromised. Proliferation follows the inflammatory phase, and can be compromised because the cytokine (or chemical messenger) profile of the wound bed is altered in diabetes. Because of the high numbers of inflammatory components, including tumour necrosis factor alpha, there is a reduction in the factors that promote proliferation (for example, platelet-derived growth factor) with pro-inflammatory cytokines dominating the proliferative cytokines. There is also a suggestion that fibroblasts are less responsive to growth factors in ulcers in people with diabetes (Loot et al 2002) and the tensile strength of collagen is poorer, with a tendency to break (Lioupis 2005). The result is slower production of matrix in the wound bed as proliferative activity is suppressed (Lobmann et al 2002). Essentially the inflammatory processes are poorly regulated in patients with diabetes, promoting continued inflammation and delay of the proliferative stage of healing (Table 3).
Impaired wound healing in patients with diabetes
Normal wound healing Haemostasis Inflammation Infection Proliferation Impairment in diabetes Increased risk of infection. Poor vascular supply. Slow recruitment of neutrophils. Persistent inflammation. Hyperglycaemia encourages bacterial growth. Slow and ineffective neutrophil and macrophage activity. Reduced tensile strength of collagen. Reduced collagen deposition. Reduced fibroblast activity. Reduced tensile strength of collagen. Risk of ulcer recurrence as a result of weakened area of scar tissue.
Maturation
NURSING STANDARD
july 13 :: vol 25 no 45 :: 2011 45
p41-47w45_ART&SCIENCE 11/07/2011 10:51 Page 46
art & science diabetes
Wound infection
Hyperglycaemia is responsible for the development of wound infections in people with diabetes. McIntosh (2009) and Lipsky and Berendt (2006) suggested that bacteria thrive on the increased glucose available in the bloodstream, and that at the same time the high glucose concentration inhibits neutrophil action, leading to a proliferation of bacteria and infection. Cellulitis, abscesses and osteomyelitis ensue. Classic signs of infection pain, heat, redness and swelling are often absent or diminished. This is attributed to neuropathy and ischaemia, which impair the normal inflammatory response (Edmonds and Foster 2006). Necrosis and sloughy tissue are often problematic in the diabetic wound (McIntosh 2006), with frequent manual debridement necessary in all diabetic wounds (Figure 4). The presence of this debris in the wound bed can be a reservoir for bacteria and toxins, increasing the risk of wound infection (Knig et al 2005). Acute surgical wounds are also problematic in patients
&
FIGURE 4 Infected foot ulcer
with diabetes with an increased risk of infection and associated complication rates compared with non-diabetic patients (Zerr et al 1997, Talbot 2005). Talbot (2005) proposed that it is not simply glycaemic control that increases the risk of surgical site infection in cardiothoracic patients; obesity is a known surgical site infection risk and 90% of all patients newly diagnosed with type 2 diabetes are overweight. Carriage of Staphylococcus aureus has also been shown to increase the risk of staphylococcal surgical site
References
Adamson R (2009) Role of the macrophages in normal wound healing: an overview. Journal of Wound Care. 18, 8, 349-351. Ahmed N (2005) Advanced glycation endproducts: role in pathology of diabetic complications. Diabetes Research and Clinical Practice. 67, 1, 3-21. Ahroni JH, Boyko EJ (2000) Responsiveness of the SF-36 among veterans with diabetes mellitus. Journal of Diabetes and its Complications. 14, 1, 31-39. Armstrong D, Lavery A, Wrobel J, Vileikyte L (2008) Quality of life in healing diabetic wounds: does the end justify the means? Journal of Foot and Ankle Surgery. 47, 4, 278-282. Boulton AJM (2006) The pathway to ulceration: aetiopathogenesis. In Boulton AJM, Cavanagh PR, Rayman G (Eds) The Foot in Diabetes. Fourth edition. John Wiley & Sons, Chichester. 51-67. Boyko EJ, Lipsky BA, Sandoval R et al (1989) NIDDM and the prevalence of nasal staphylococcus aureus colonization. San Luis Valley Diabetes Study. Diabetes Care. 12, 189-192. Bristow IR, Spruce MC (2009) Fungal foot infection, cellulitis and diabetes: a review. Diabetes Medicine. 26, 5, 548-551. Brown CD, Ghali HS, Zhao Z, Thomas LL, Friedman EA (2005) Association of reduced red blood cell deformability and diabetic nephropathy. Kidney International. 67, 1, 295-300 Davis P (2008) The immunology of wound healing: the body as a battlefield. Wound Healing Science. 4, 4, 54-69. Diabetes UK (2010) Diabetes in the UK 2010: Key Statistics on Diabetes. www.diabetes.org.uk/Documents/Reports/ Diabetes_in_the_UK_2010.pdf (Last accessed: June 23 2011.) Doughty DB, Sparks-Defriese B (2007) Wound healing physiology. In Bryant RA, Nix DP (Eds) Acute and Chronic Wounds: Current Management Concepts. Mosby, St Louis MO. 56-81. Driver VR, Landowski MA, Madsen JL (2007) Neuropathic wounds: the diabetic wound. In Bryant RA, Nix DP (Eds) Acute and Chronic Wounds: Current Management Concepts. Mosby, St Louis MO. 307-336. Dunning T (2009) Care of People with Diabetes: A Manual of Nursing Practice. Third edition. Wiley-Blackwell, Chichester. Edmonds ME, Foster AV (2006) ABC of wound healing. Diabetic foot ulcers. British Medical Journal. 332, 7538, 407-410. Falanga V (2005) Wound healing and its impairment in the diabetic foot. The Lancet. 366, 9498, 1736-1743. Hunt TK, Pai MP (1972) The effect of variant ambient oxygen tensions on wound metabolism and collagen synthesis. Surgery Gynaecology and Obstetrics. 135, 4, 561-567. International Working Group on the Diabetic Foot (1999) International Consensus on the Diabetic Foot. International Working Group on the Diabetic Foot, Amsterdam. Kidman K (2008) Tissue repair and regeneration: the effects of diabetes on wound healing. Diabetic Foot Journal. 11, 2, 73-79. Knig M, Vanscheidt W, Augustin M, Kapp H (2005) Enzymatic versus autolytic debridement of chronic leg ulcers: a prospective randomised trial. Journal of Wound Care. 14, 7, 320-323. Levin ME (2002) Management of the diabetic foot: preventing amputation. Southern Medical Journal. 95, 1, 10-20. Lioupis C (2005) Effects of diabetes mellitus on wound healing: an update. Journal of Wound Care. 14, 2, 84-86. Lipsky BA, Berendt AR (2006) Infection of the foot in persons with diabetes: epidemiology, pathophysiology, microbiology, clinical presentation and approach to therapy. In The Foot in Diabetes. Fourth edition. Wiley & Sons, Chichester. 159-168. Lobmann R, Ambrosch A, Schultz G et al (2002) Expression of matrix-metalloproteinases and their inhibitors in the wounds of diabetic and
46 july 13 :: vol 25 no 45 :: 2011
NURSING STANDARD
SCIENCE PHOTO LIBRARY
p41-47w45_ART&SCIENCE 11/07/2011 10:51 Page 47
infections. S. aureus, considered one of the more important pathogens (Lipsky and Berendt 2006), is frequently found in the nose of diabetic patients (Boyko et al 1989, Stanaway et al 2007) and therefore increases the likelihood of surgical site infection (Talbot 2005). Pre-operative skin preparation may have a role in reducing post-operative infection in these patients.
Management of diabetic wounds
People with diabetes should be encouraged to manage their blood glucose to minimise the potential damage that can result from raised blood glucose levels. Providing advice on what constitutes a healthy diet and encouraging physical activity are advocated to help patients control blood glucose levels and minimise complications (Nair 2007). Smoking cessation is recommended to reduce the risk of vascular disease, as is weight loss in people who are obese (Stumvoll et al 2005). Management of wounds in the patient with diabetes is frequently the responsibility of a multidisciplinary team. Patients with foot ulceration, because of the recognised risk of amputation, should be referred to the specialist
foot team, a multidisciplinary team focusing on the foot in diabetes (McIntosh 2006). However, any wound can potentially be a problem if the patient has diabetes. Effective wound care is vital and this starts with thorough assessment. There are several wound assessment tools available and they should assist the practitioner in choosing the most appropriate wound care practices. The concept of wound bed preparation preparing the wound bed to be in the best possible condition to support healing is the basis of most modern wound care (Watret 2005). Debridement is a fundamental aspect of wound management: removal of necrotic material is essential to allow healing to take place and reduce the risk of infection. Managing moisture levels in a wound can be difficult, especially if the wound is in the inflammatory stage of healing when there is likely to be increased levels of exudate.
Conclusion
Wound healing is usually a well organised and complex series of events which can be impaired in the presence of a chronic illness such as diabetes. An understanding of the wound healing process and the effects of diabetes on this process are essential to promote effective wound healing NS
non-diabetic patients. Diabetologia. 45, 7, 1011-1016. Loot MA, Kenter SB, Au FL et al (2002) Fibroblasts derived from chronic diabetic ulcers differ in their response to stimulation with ECF, IGF-I, bFGF and PDVGF-AB compared to controls. European Journal of Cell Biology. 81, 3, 153-60. McIntosh C (2006) Diabetic Foot Ulcers: An Educational Booklet. Wounds UK Publishing, Aberdeen. McIntosh C (2009) Managing diabetic foot ulceration: review of best practice. Wound Essentials. 4, 102-111 . Meeking D, Holland E, Land D (2006) Diabetes and foot disease. In Shaw KM, Cummings MH (Eds) Diabetes: Chronic Complications. Wiley, Chichester. 47-78. Menke NB, Ward KR, Witten TM, Bonchev DG, Diegelmann RF (2007) Impaired wound healing. Clinics in Dermatology. 25, 1, 19-25. Morain WD, Colen LB (1990) Wound healing in diabetes mellitus. Clinics in Plastic Surgery. 17, 3, 493-501. Nabuurs-Franssen MH, Huijberts MS, Nieuwenhuijzen Kruseman AC, Willems J, Schaper NC (2005) Health-related quality of life of diabetic foot ulcer patients and their caregivers. Diabetologia. 48, 9, 1906-1910.
Nair M (2007) Nursing management of the person with diabetes mellitus. Part 2. British Journal of Nursing. 16, 4, 232-235. National Diabetes Support Team (2006) Diabetic Foot Guide. www.diabetes.nhs.uk/ document.php?o=196 (Last accessed: June 23 2011.) Novak M (2010) Diabetes mellitus. In Nettina SM (Ed) Manual of Nursing Practice. Lippincott Williams & Wilkins, Wolters Kluwer, London. 944-969. Pound N, Chipchase S, Treece K, Game F, Jeffcoate W (2005) Ulcer free survival following management of foot ulcers in diabetes. Diabetic Medicine. 22, 10, 1306-1309. Reiber GE, Vileikyte L, Boyko EJ et al (1999) Causal pathways for incident lower-extremity ulcers in patients with diabetes from two settings. Diabetes Care. 22, 1, 157-162. Shaw JE, Boulton AJM (1995) The Charcot foot. Foot. 5, 65-70. Shaw JE, Boulton AJM (2001) The diabetic foot. In Beard JD, Gaines PA (eds) Vascular and Endovascular Surgery. Second edition. WB Saunders, London. 105-126. Shier D, Butler J, Lewis R (2010) Holes Anatomy and Physiology. Twelfth edition. McGraw-Hill, Boston MA. Shin S, Ku Y (2005) Hemorheology and clinical application: association of
impairment of red blood cell deformability and diabetic nephropathy. Korea-Australia Rheology Journal. 17, 3, 117-123. Stadelmann WK, Digenis AG, Tobin GR (1998) Impediments to wound healing. American Journal of Surgery. 176, Suppl 2a, 39s-47s. Stanaway S et al (2007) Methicillin-resistant Staphylococcus aureus (MRSA) isolation from diabetic foot ulcers correlates with nasal MRSA carriage. Diabetes Research and Clinical Practice. 75, 1, 47-50. Stumvoll M, Goldstein BJ, van Haeften TW (2005) Type 2 diabetes: principles of pathogenesis and therapy. The Lancet. 365, 9467, 1333-1346. Talbot TR (2005) Diabetes mellitus and cardiothoracic surgical site infections. American Journal of Infection Control. 33, 6, 353-359. Tortora GJ, Derrickson B (2007) Introduction to the Human Body: The Essentials of Anatomy and Physiology. Seventh edition. Wiley, New York NY. Watret L (2005) Wound bed preparation and the diabetic foot. Diabetic Foot. 8, 1, 18-26. Zerr KJ, Furnary AP, Grunkemeier GL et al (1997) Glucose control lowers the risk of wound infection in diabetics after open heart operations. Annals of Thoracic Surgery. 63, 2, 356-361.
NURSING STANDARD
july 13 :: vol 25 no 45 :: 2011 47
Reproduced with permission of the copyright owner. Further reproduction prohibited without permission.
Вам также может понравиться
- A Simple Guide to Sternum Disorders, Diagnosis, Treatment and Related ConditionsОт EverandA Simple Guide to Sternum Disorders, Diagnosis, Treatment and Related ConditionsОценок пока нет
- Fractures and Dislocations, A Simple Guide To The Condition, Diagnosis, Treatment And Improvised TreatmentОт EverandFractures and Dislocations, A Simple Guide To The Condition, Diagnosis, Treatment And Improvised TreatmentОценок пока нет
- Amputation-Dr N K BeheraДокумент8 страницAmputation-Dr N K BeheraSheel GuptaОценок пока нет
- Juvenile Rheumatoid ArthritisДокумент3 страницыJuvenile Rheumatoid ArthritisYnos Sta TeresaОценок пока нет
- Study On Pressure UlcerДокумент219 страницStudy On Pressure UlcerThein Ko Oo100% (1)
- Clavicle FractureДокумент6 страницClavicle FractureYbis LizarzaburuОценок пока нет
- Psoriatic ArthritisДокумент12 страницPsoriatic ArthritisSelvia RosadiОценок пока нет
- Diabetes Mellitus Type 2Документ16 страницDiabetes Mellitus Type 2MTs MIFDAОценок пока нет
- Post Natal CareДокумент15 страницPost Natal CareDaphneyОценок пока нет
- Lab ValuesДокумент6 страницLab ValuesdnllkzaОценок пока нет
- Effects of Aging On The Digestive SystemДокумент3 страницыEffects of Aging On The Digestive SystemShereen Manabilang100% (2)
- Preoperative Assessment of Diabetic PatientsДокумент2 страницыPreoperative Assessment of Diabetic PatientsShilpa Pradhan100% (1)
- Orthopedic Splints and Traction TechniquesДокумент26 страницOrthopedic Splints and Traction TechniquesArun C RajОценок пока нет
- BioethicsCasesEEI 316232215 PDFДокумент38 страницBioethicsCasesEEI 316232215 PDFAman UllahОценок пока нет
- DYSTROPHYДокумент15 страницDYSTROPHYleeyan2wenty6Оценок пока нет
- Polio: A Brief History and Overview of the DiseaseДокумент13 страницPolio: A Brief History and Overview of the DiseaseMumin Farah100% (1)
- Shoulder Case Study 1Документ4 страницыShoulder Case Study 1superhoofy718667% (3)
- OSTEOMYELITISДокумент14 страницOSTEOMYELITISKristine Alejandro0% (1)
- 2016 The American Society of Shoulder and ElbowДокумент15 страниц2016 The American Society of Shoulder and ElbowDiego De Farias Diehl100% (1)
- Narrative PathophysiologyДокумент18 страницNarrative PathophysiologyNica Georgelle Maniego SamonteОценок пока нет
- Shoulder Case Study 2Документ5 страницShoulder Case Study 2superhoofy7186Оценок пока нет
- Ethical Issues in Palliative CareДокумент18 страницEthical Issues in Palliative CareDinesh DОценок пока нет
- TRACTION LavlyДокумент9 страницTRACTION Lavlylabsky_evol100% (1)
- 2 Acute Myocardial InfarctionДокумент15 страниц2 Acute Myocardial InfarctionpauchanmnlОценок пока нет
- Nutrition For Older Adults - M.SC - DAN - 2016Документ59 страницNutrition For Older Adults - M.SC - DAN - 2016Ria KumarОценок пока нет
- Rhabdomyolysis: - Striated - Muscle - BreakdownДокумент45 страницRhabdomyolysis: - Striated - Muscle - BreakdownHelmi Ismunandar100% (1)
- Managing Fall Risk in an 84-Year-Old Asian MaleДокумент4 страницыManaging Fall Risk in an 84-Year-Old Asian Malesavvy_as_98-1Оценок пока нет
- Frozen ShoulderДокумент18 страницFrozen Shoulderhemnath rajendranОценок пока нет
- OsteoarthritisДокумент4 страницыOsteoarthritisDharti PatelОценок пока нет
- SNAKE BITE MEDICAL MANAGEMENT CrebonДокумент33 страницыSNAKE BITE MEDICAL MANAGEMENT Crebonbayu riko100% (1)
- Bicipital TendinitisДокумент19 страницBicipital TendinitisRonak PatelОценок пока нет
- Modifiable and Non-Modifiable Risk Factors for Aortic AneurysmДокумент5 страницModifiable and Non-Modifiable Risk Factors for Aortic AneurysmJanine Gerunda100% (1)
- Assessment of The Peripheral Vascular SystemДокумент17 страницAssessment of The Peripheral Vascular SystemgrailbadОценок пока нет
- GoutДокумент5 страницGoutDe Sesto Rhys Carlo100% (2)
- Anemia 130809044630 Phpapp01Документ21 страницаAnemia 130809044630 Phpapp01Siddharth Das100% (1)
- Juvenile Arthritis Symptoms, Causes, TreatmentsДокумент8 страницJuvenile Arthritis Symptoms, Causes, TreatmentsDhanNie CenitaОценок пока нет
- Drug StudyДокумент8 страницDrug Studysarah1217Оценок пока нет
- Types and Treatment of FracturesДокумент68 страницTypes and Treatment of FracturesokaciaОценок пока нет
- Log Rolling TechniqueДокумент2 страницыLog Rolling TechniqueRajaОценок пока нет
- Management of diabetic ketoacidosis: principles of management in the first hourДокумент13 страницManagement of diabetic ketoacidosis: principles of management in the first hourAzim Abd RazakОценок пока нет
- Active Leg Exercises: Sitting Range of MotionДокумент3 страницыActive Leg Exercises: Sitting Range of MotionfrnildegaОценок пока нет
- Heart Valve DiseaseДокумент8 страницHeart Valve DiseaseMundhir Al-Khusaibi100% (1)
- Summary of Key BLS Components For Adults Children and InfantДокумент26 страницSummary of Key BLS Components For Adults Children and Infantjulesubayubay5428Оценок пока нет
- Essential Guide to Orthopedic BracesДокумент44 страницыEssential Guide to Orthopedic BracesAlex Delos SantosОценок пока нет
- Range of Motion Assessment PDFДокумент71 страницаRange of Motion Assessment PDFMohan Krishabi100% (1)
- Food and Drug InteractionsДокумент4 страницыFood and Drug InteractionsClararida RiawanОценок пока нет
- Scoliosis: Aka: Idiopathic Scoliosis, Adolescent ScoliosisДокумент12 страницScoliosis: Aka: Idiopathic Scoliosis, Adolescent ScoliosisLei Coloma SissonОценок пока нет
- ValiumДокумент1 страницаValiumKatie McPeekОценок пока нет
- HypertensionДокумент19 страницHypertensionmr_coolz282344Оценок пока нет
- Osteoporosis Case ReportДокумент21 страницаOsteoporosis Case ReportJewenson SalvadorОценок пока нет
- Duchenne Muscular Dystrophy: Causes, Symptoms & TreatmentsДокумент18 страницDuchenne Muscular Dystrophy: Causes, Symptoms & TreatmentsLusi MunawarohОценок пока нет
- Open FractureДокумент9 страницOpen FractureAnnyl LaurelОценок пока нет
- DiabetesДокумент25 страницDiabetesKoRnflakes100% (2)
- Stump CareДокумент7 страницStump CareirtazakazmiОценок пока нет
- Wound CareДокумент17 страницWound Caredlneisha6183% (6)
- GBS Management, Medications and Nursing ConsiderationsДокумент4 страницыGBS Management, Medications and Nursing Considerationssouledg3100% (1)
- نسخة Lecture - PAIN Assessment & ManagementДокумент52 страницыنسخة Lecture - PAIN Assessment & Managementjsoal100% (1)
- Avascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsОт EverandAvascular Necrosis, A Simple Guide To The Condition, Diagnosis, Treatment And Related ConditionsРейтинг: 4 из 5 звезд4/5 (2)
- Cellular Endocrinology in Health and DiseaseОт EverandCellular Endocrinology in Health and DiseaseAlfredo Ulloa-AguirreОценок пока нет
- Tugas Individu Anggun PDFДокумент6 страницTugas Individu Anggun PDFAnggun PermatasariОценок пока нет
- Transient Ischemic PDFДокумент8 страницTransient Ischemic PDFDennis CobbОценок пока нет
- Treatment of Sternal Wound Infections After Open-Heart SurgeryДокумент6 страницTreatment of Sternal Wound Infections After Open-Heart SurgeryDennis CobbОценок пока нет
- Managing mediastinitis after cardiac surgeryДокумент4 страницыManaging mediastinitis after cardiac surgeryDennis CobbОценок пока нет
- Liver Cirrhosis PDFДокумент9 страницLiver Cirrhosis PDFDennis CobbОценок пока нет
- Autonomy of Nurse PDFДокумент8 страницAutonomy of Nurse PDFDennis CobbОценок пока нет
- Content 8902 PDFДокумент6 страницContent 8902 PDFabdulОценок пока нет
- User Training AED ProДокумент46 страницUser Training AED ProDennis CobbОценок пока нет
- Trend Management Patient of Transposition Great ArteryДокумент3 страницыTrend Management Patient of Transposition Great ArteryDennis CobbОценок пока нет
- Fluid Afterload After CabgДокумент6 страницFluid Afterload After CabgDennis CobbОценок пока нет
- Assessment Constipation PDFДокумент6 страницAssessment Constipation PDFDennis CobbОценок пока нет
- ArdsДокумент7 страницArdsIpar DayОценок пока нет
- Arf Post CabgДокумент19 страницArf Post CabgDennis CobbОценок пока нет
- Assessment Constipation PDFДокумент6 страницAssessment Constipation PDFDennis CobbОценок пока нет
- APGARДокумент1 страницаAPGARblazegomezОценок пока нет
- Post Cardiac ComplicationsДокумент6 страницPost Cardiac ComplicationsGull GillОценок пока нет
- Avian InfluenzaДокумент6 страницAvian InfluenzaDennis CobbОценок пока нет
- Early Postopcare After Cardiac Surgery PDFДокумент23 страницыEarly Postopcare After Cardiac Surgery PDFDennis CobbОценок пока нет
- Heart NotesДокумент13 страницHeart NotesDennis CobbОценок пока нет
- Cardiac ArrhythmiaДокумент5 страницCardiac ArrhythmiaDennis CobbОценок пока нет
- Respiration Disorder PDFДокумент14 страницRespiration Disorder PDFDennis CobbОценок пока нет
- Avian InfluenzaДокумент6 страницAvian InfluenzaDennis CobbОценок пока нет
- Autonomy of Nurse PDFДокумент8 страницAutonomy of Nurse PDFDennis CobbОценок пока нет
- Cognitive Impairment PDFДокумент4 страницыCognitive Impairment PDFDennis CobbОценок пока нет
- Capillary Blood GlucoseДокумент4 страницыCapillary Blood GlucoseDennis CobbОценок пока нет
- Best Practice in The Use of SpirometryДокумент6 страницBest Practice in The Use of SpirometryDennis CobbОценок пока нет
- CPR Nurse LawДокумент6 страницCPR Nurse LawIpar DayОценок пока нет
- Marfan's Syndrome Signs and Symptoms: EtiologyДокумент3 страницыMarfan's Syndrome Signs and Symptoms: EtiologyDennis CobbОценок пока нет
- Atrial FibrilationДокумент10 страницAtrial FibrilationDennis CobbОценок пока нет
- Avian InfluenzaДокумент6 страницAvian InfluenzaDennis CobbОценок пока нет
- 18-93 Mini Project Final ReportДокумент26 страниц18-93 Mini Project Final ReportKP REDDYОценок пока нет
- Saccharomyces Boulardii What Makes It Tick As Successful ProbioticДокумент16 страницSaccharomyces Boulardii What Makes It Tick As Successful ProbioticMonserrat Garduño Fonseca100% (1)
- Pharmacotherapy of MigraineДокумент74 страницыPharmacotherapy of MigraineAvin GupthaОценок пока нет
- AutacoidsДокумент103 страницыAutacoidsKamran Ali100% (1)
- Neet Solution Oct 2020 PDFДокумент202 страницыNeet Solution Oct 2020 PDFarjunkvОценок пока нет
- Chapter 24:: Allergic Contact Dermatitis:: Jake E. Turrentine, Michael P. SheehanДокумент19 страницChapter 24:: Allergic Contact Dermatitis:: Jake E. Turrentine, Michael P. SheehanInke LubisОценок пока нет
- Synovitis in Osteoarthritis: Current Understanding With Therapeutic ImplicationsДокумент9 страницSynovitis in Osteoarthritis: Current Understanding With Therapeutic ImplicationsSalsabila HasnaОценок пока нет
- Journal of Bodywork & Movement TherapiesДокумент10 страницJournal of Bodywork & Movement TherapiesCarol MansurОценок пока нет
- Asthma Thesis StatementДокумент4 страницыAsthma Thesis Statementfjnev0hc100% (2)
- Nutrition For Injury Recovery Infographic PrinterДокумент5 страницNutrition For Injury Recovery Infographic PrinterClau DinuОценок пока нет
- Curier Nr4.indd PDFДокумент58 страницCurier Nr4.indd PDFCristinaCaprosОценок пока нет
- Þ" Hospital: Clinical and Scientific Rationale For The "MATH Treatment Protocol For COVID-19Документ22 страницыÞ" Hospital: Clinical and Scientific Rationale For The "MATH Treatment Protocol For COVID-19Doménica SánchezОценок пока нет
- Classification of Periodontal Diseases PerioДокумент42 страницыClassification of Periodontal Diseases PerioFourthMolar.comОценок пока нет
- Acute and Chronic InflammationДокумент6 страницAcute and Chronic Inflammationangeloudebuyan191Оценок пока нет
- Antimicrobial Activity of Alo e V e Ra (L.) Burm. F. Against Pathogenic MicroorganismsДокумент8 страницAntimicrobial Activity of Alo e V e Ra (L.) Burm. F. Against Pathogenic MicroorganismsBea NufuarОценок пока нет
- (Psychology of Emotions, Motivations and Actions) Leandro Cavalcanti (Ed.), Sofia Azevedo (Ed.) - Psychology of Stress - New Research-Nova Science Publishers (2013)Документ214 страниц(Psychology of Emotions, Motivations and Actions) Leandro Cavalcanti (Ed.), Sofia Azevedo (Ed.) - Psychology of Stress - New Research-Nova Science Publishers (2013)Jesus Jimenez100% (1)
- European Journal of Pharmacology: Alexander V SirotkinДокумент7 страницEuropean Journal of Pharmacology: Alexander V SirotkinNut. Ana Gabriela Cruz ArellanoОценок пока нет
- Uterine Fibroid PDFДокумент12 страницUterine Fibroid PDFAlpascaFirdausОценок пока нет
- CANCER IMMUNOLOGY TITLEДокумент31 страницаCANCER IMMUNOLOGY TITLEAbdul FarooqОценок пока нет
- Sputum Exam GuideДокумент36 страницSputum Exam GuideSari Bunga Mastina0% (1)
- Lecture Outline: See Separate Powerpoint Slides For All Figures and Tables Pre-Inserted Into Powerpoint Without NotesДокумент60 страницLecture Outline: See Separate Powerpoint Slides For All Figures and Tables Pre-Inserted Into Powerpoint Without NotessyafiqahОценок пока нет
- Vidradhi in B Hat-Trayī A Critical Review of LiteratureДокумент8 страницVidradhi in B Hat-Trayī A Critical Review of LiteratureInternational Journal of Innovative Science and Research TechnologyОценок пока нет
- Full Download Test Bank For Comprehensive Radiographic Pathology 6th Edition by Eisenberg PDF Full ChapterДокумент36 страницFull Download Test Bank For Comprehensive Radiographic Pathology 6th Edition by Eisenberg PDF Full Chapterdiesnongolgothatsczx100% (13)
- SBMPTN Bahasa Inggris: Anti-inflammatory Foods May Help Reduce InflammationДокумент8 страницSBMPTN Bahasa Inggris: Anti-inflammatory Foods May Help Reduce InflammationADITAPA OFFICIALОценок пока нет
- Rickettsia, Mycoplasma. Fungi, ProtozoaДокумент4 страницыRickettsia, Mycoplasma. Fungi, ProtozoaVincent ReyesОценок пока нет
- Non Specific HostДокумент46 страницNon Specific HostAdrian BautistaОценок пока нет
- Pedia Allergic DisordersДокумент4 страницыPedia Allergic Disordersmia liaОценок пока нет
- 11805001Документ2 страницы11805001Aniket DubeyОценок пока нет
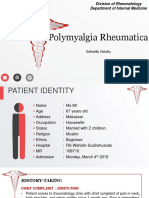
- Polymyalgia RheumaticaДокумент23 страницыPolymyalgia RheumaticaGabriella TungadiОценок пока нет
- CRP - TestДокумент5 страницCRP - TestAhmed AhmedОценок пока нет