Академический Документы
Профессиональный Документы
Культура Документы
Perspective: Not Just For Women
Загружено:
gloriannelazaroИсходное описание:
Оригинальное название
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Perspective: Not Just For Women
Загружено:
gloriannelazaroАвторское право:
Доступные форматы
OUTLOOK BREAST CANCER
PERSPECTIVE Not just for women
Specific research and treatment of breast cancer in men has been neglected and deserves greater attention, says Valerie Speirs.
differences in tumour biology and treatment outcomes will allow the development of targeted treatments for male breast cancer. Such targeted treatments for female breast cancer have made a huge impact, adding years to womens lives. A 2010 study6 suggests that male breast cancer also has a specific microRNA profile. MicroRNAs are regulatory RNAs that affect the stability and efficiency of the translation of messenger RNA, the intermediate between genes and proteins. Identifying a microRNA-specific signature in male breast cancer could provide further insight into disease pathogenesis, augmenting the results from gene-expression approaches. At present, the treatment of male breast cancer relies heavily on what works for female breast cancer. As the subtle differences between male and female breast cancers become clear, it will be important to plan clinical trials exclusively for male breast cancer patients in order to determine optimal treatments. Building this capacity will allow formal testing of the emerging sex-specific data from gene-expression and microRNA profiling, indicating the potential usefulness of these molecules or signatures as markers of disease outcome or treatment progress. The neglect of male breast cancer, however, extends further than a lack of understanding about its biology. Men with breast cancer are often treated in the same clinic as women; if a patient is accompanied by a woman, many people (staff and patients) assume that he is there in a supporting role, rather than as a patient. Added to the stress of a breast cancer diagnosis, such social and psychological factors can be distressing. Patients or patient advocate groups should campaign to establish men-only breast cancer clinics to help address these issues. Providing information on treatment side effects that is better tailored to the needs of male patients would also help. Finally, given the lack of public awareness, men are less likely than women to report signs of breast cancer, such as lumps in their breast tissue, so the disease is often diagnosed at a later stage when it is harder to treat. More public education is therefore needed for example, through groups like the John W. Nick Foundation in Sebastian, Florida, a charity that promotes male breast cancer awareness so that men know about the risks of breast cancer and the measures they can take to reduce them. Such education is also vital if society is to move away from the idea that breast cancer affects only women. Valerie Speirs is a reader in cellular pathology at Leeds Institute of Molecular Medicine, University of Leeds, UK. e-mail: v.speirs@leeds.ac.uk
1. Ferlay, J. et al. Int. J. Cancer 127, 28932917 (2010). 2. Shaaban, A. M. et al. Breast Cancer Res. Treat. doi:10.1007/s10549-011-1856-9 (18 November 2011). 3. White, J. et al. Breast Cancer Res. 13, 219 (2011). 4. Curtis, C. et al. Nature doi:10.1038/nature10983 (18 April 2012). 5. Johansson, I. et al. Breast Cancer Res. 14, R31 (2012). 6. Lehmann, U. et al. BMC Cancer 10, 109 (2010).
magine a waiting room in a busy clinic. A serious-looking doctor ushers a patient into the consulting room. The patient sits down, and the doctor delivers the sombre news: You have breast cancer. Worldwide, more than 1.3 million women are diagnosed with breast cancer every year1, so this scene is perhaps not uncommon. But this time the patient is a man. He reacts with disbelief: men dont get breast cancer; this must be a mistake. Yet breast cancer affects both men and women, with some 13,000 men being diagnosed each year worldwide. When matched for important prognostic factors (tumour size, grade and lymph-node status), the outcome of male and female breast cancer is similar2. But men are generally diagnosed at a later stage than women, so their survival rates tend to be lower. Male breast cancer is rare, accounting for less than 1% of all breast cancer cases, but its incidence seems to be increasing in Western countries3. With epidemiological studies lacking, the reasons for this increase are unknown. Lifestyle changes over the past two to three decades have been proposed as causes, including the rise in alcohol consumption and obesity, and the decrease in exercise. Most studies of male breast cancer have been restricted to examining small numbers of tissue samples available from histopathology archives, and information about the molecular pathways associated with its biological behaviour has been largely anecdotal. To fill this knowledge gap, in 2007, my team at the University of Leeds established the Male Breast Cancer Consortium: a collaboration with pathologists in Europe and North America to gather samples from hundreds of men with breast cancer. Similarly, following a meeting in Bethesda, Maryland, in 2008, the International Male Breast Cancer Program was launched as a cross-continental effort to pool samples, epidemiological data and clinical information.
THE NEGLECT OF MALE BREAST CANCER EXTENDS FURTHER THAN A LACK OF UNDERSTANDING ABOUT ITS BIOLOGY.
NOT THE SAME
In the past two years, analyses of these large sample collections have shown that, despite superficial similarities in tissue appearance and hormone-receptor expression, male and female breast cancers differ at the molecular level. In November 2011, using hierarchical cluster analysis, my group reported2 subtle differences in hormone-receptor expression in male tumours. In particular, we observed clustering of androgen and oestrogen receptors in male samples and showed that androgen-receptor expression was associated with better overall survival. These differences could open up new avenues for treating male breast cancer, such as androgen-targeting approaches, which have not previously been considered. Molecular (or gene-expression) profiling is also starting to reveal deeper differences. Female breast cancer can now be divided into as many as ten different molecular subgroups, according to a recent paper4. Data published in February 2012 (ref.5) indicate that male breast cancer has two subgroups, both of which seem to differ from the female subgroups. I hope that characterizing these subgroups identifying the
S 6 6 | NAT U R E | VO L 4 8 5 | 3 1 M AY 2 0 1 2
2012 Macmillan Publishers Limited. All rights reserved
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (890)
- Force UsersДокумент64 страницыForce UsersLuftWulf100% (7)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- The Trauma of Freud Controversies in Psychoanalysis PDFДокумент318 страницThe Trauma of Freud Controversies in Psychoanalysis PDFMinuxОценок пока нет
- L o N G e V I T y NotesДокумент24 страницыL o N G e V I T y NotesRajeswara Rao NidasanametlaОценок пока нет
- 1.1.3 Project Execution PlanДокумент7 страниц1.1.3 Project Execution PlanlisahunОценок пока нет
- CH 02Документ20 страницCH 02Pauline Nguyen100% (1)
- A Comparative GrammarДокумент503 страницыA Comparative GrammarXweuis Hekuos KweОценок пока нет
- SaaS Marketing Automation Playbook TeaserДокумент19 страницSaaS Marketing Automation Playbook TeaserValery FenskeОценок пока нет
- 4 5800845248737314443 PDFДокумент457 страниц4 5800845248737314443 PDFNirankar SinghОценок пока нет
- Fourth Assignment.: Summary - Outcome of The ProgramДокумент2 страницыFourth Assignment.: Summary - Outcome of The ProgramHasvdkОценок пока нет
- African American Women's LanguageДокумент30 страницAfrican American Women's LanguageRatih Santi MianawatiОценок пока нет
- Porirua Harbour Patterns and Rates of Sedimentation ReportДокумент65 страницPorirua Harbour Patterns and Rates of Sedimentation ReportPaul MarlowОценок пока нет
- Numark Orbit - VirtualDJ 8 Operation GuideДокумент13 страницNumark Orbit - VirtualDJ 8 Operation GuideCasiLokoОценок пока нет
- Basculas Con MIGO SAPДокумент3 страницыBasculas Con MIGO SAPmizraimОценок пока нет
- Identity Collage RubricДокумент1 страницаIdentity Collage Rubricapi-709145254Оценок пока нет
- Sap Master Data in Materials ManagementДокумент13 страницSap Master Data in Materials Managementedmondo77Оценок пока нет
- Lesson PlanДокумент7 страницLesson Planapi-357536453Оценок пока нет
- Chapter 6Документ17 страницChapter 6Adam KellyОценок пока нет
- Real-Time Temperature Tracking Web ServiceДокумент4 страницыReal-Time Temperature Tracking Web ServiceVirna Uli SamosirОценок пока нет
- Lth-Band Digital Filters Design and PropertiesДокумент2 страницыLth-Band Digital Filters Design and PropertiesHanna AbejoОценок пока нет
- Aneka Cloud IntroductionДокумент36 страницAneka Cloud IntroductionPradeep Kumar Reddy ReddyОценок пока нет
- In The Bedroom Missing Letters in Words Esl WorksheetДокумент2 страницыIn The Bedroom Missing Letters in Words Esl Worksheetgirl_blueeyes89Оценок пока нет
- Seminar ReportДокумент12 страницSeminar ReportNupurОценок пока нет
- Gdot Autoturn User Guide Ds FdsДокумент66 страницGdot Autoturn User Guide Ds FdsMd Didarul AlamОценок пока нет
- Embedded Systems - Fs 2018: Figure 1: Simplified Task States Diagram in FreertosДокумент8 страницEmbedded Systems - Fs 2018: Figure 1: Simplified Task States Diagram in FreertosPhạm Đức HuyОценок пока нет
- Kajo 5 PDFДокумент3 страницыKajo 5 PDFJonathan ChauОценок пока нет
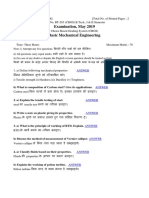
- BT 203 Basic Mechanical Engineering May 2019 PDFДокумент2 страницыBT 203 Basic Mechanical Engineering May 2019 PDFKunta PatleОценок пока нет
- Cisco Callmanager Attendant ConsoleДокумент28 страницCisco Callmanager Attendant ConsoleLuciano Esteban GaeteОценок пока нет
- Methodology of Education Research MCQSДокумент12 страницMethodology of Education Research MCQSRAFIULLAHОценок пока нет
- Integrating Information About The Cost of Carbon Through Activity Based Costing 2012 Journal of Cleaner ProductionДокумент10 страницIntegrating Information About The Cost of Carbon Through Activity Based Costing 2012 Journal of Cleaner ProductionLilian BrodescoОценок пока нет
- Kavindu Final.Документ33 страницыKavindu Final.KavinduKarunarathnaОценок пока нет