Академический Документы
Профессиональный Документы
Культура Документы
Surgical Adult Critical Care Ref Sheet
Загружено:
sgod34Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Surgical Adult Critical Care Ref Sheet
Загружено:
sgod34Авторское право:
Доступные форматы
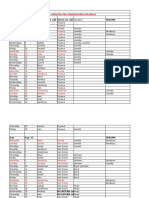
WHMC-BAMC ADULT CRITICAL CARE REFERENCE SHEET 2006
ICU QA CHECKLIST (as applicable): Hand-Washing-Infection Control-Universal Precautions? DVT prophylaxis/US screening? GI ulcer prophylaxis? VT 6 ml/kg PBW + Pplat30[ARDS]? Daily breathing trials [FiO20.5, PEEP8]? Xigris if sepsis+APACHE>25? Monitor platelets on heparin [HIT]? Glucose 80-110? Nutrition? EPO? Spine-cleared? HOB 30-45? Skin care? Lines-tubes tips+duration? Antibiotic duration? Paralysis/sedation breaks? PT/OT consult? Restraint orders? Advance directive? Transfer planning [intermed care, rehab-SNF]? Social services? Family updated daily? IV ANESTHETICS SINGLE AGENT ANESTHETIC SEDATION Induction Maintenance Loading dose Maintenance mcg/kg/min mcg/kg mcg/kg/min Thiopental (Pentothal) 3 - 6 mg/kg ( 1 mg/kg elderly,BP) useful if ICP; caution BP 2000 - 4000 Propofol (Diprivan) 1.5 - 2.5 mg/kg 100-300 5-10 mg over 10 secs start 5, 5 Q 5 min to max 100 (BP, TG, kcal, Zn) Ketamine (Ketalar) 1- 3mg/kg useful if hypovolemia or asthma; caution if BP, HR, AMI, ICP Dexmedetomidine (Precedex) (avoid CHF or > 24 hrs) 1 mcg/kg ABW over 10 min 0.2-0.7 mcg/kg/h Etomidate (Amidate) 0.2 - 0.4 mg/kg useful if BP; muscle movements blunted by Fentanyl 50 100 mcg, adrenal? Morphine 1- 3 mg/kg 50 200 30 - 150 Fentanyl 30 -100 mcg/kg 0.1 - 0.3 1-5 0.01- 0.03 SEDATIVES Midazolam (Versed) 50 - 200 mcg/kg 0.25 - 1.5 20 - 100 0.25 - 1.0 Lorazepam (Ativan) [for seizures: 0.1 mg/kg @ 2 mg/min] 1-2 mg IV/IM Q 1-4 h Diazepam (Valium) 2 -10 mg IV/IM Q 4-6 h Haloperidol (Haldol) acute delerium: 1 5 mg IV; double dose Q 20 min till calm; give total dose required BID IV or PO [monitor: QT, V tach, NMS] NEUROMUSCULAR BLOCKERS Intubating dose Typical load Maintenance Metabolism Succinylcholine (Anectine) 1-1.5 mg/kg 100 mg/70 kg NR pseudocholinesterase Avoid: K, hemiplegia, guillain-barre, crush (bradycardia with repeat dosing) Rocuronium (Zemuron) 0.45 - 0.6 mg/kg 40 mg/70 kg 10 - 15 mcg/kg/min liver Vecuronium (Norcuron) 0.08 - 0.1 mg/kg 7 mg/70 kg (avoid long term) 0.06 - 2 mcg/kg/min liver Cisatricurium (Nimbex) 0.15 - 0.2 mg/kg 10 mg/70 kg (preferred if long term) 2 - 3 mcg/kg/min Hoffman elimination Rapacuronium 1.5 mg/kg 100mg/70 kg (inject over 1 5 sec; onset 60 sec, duration 15 min) infusion not rec AUTONOMIC/CARDIOVASCULAR DRUGS IV loading dose IV Infusion Dilution Final Duration Notes (mcg/kg/min) (in 250 ml) Conc. (IV) Phenylephrine 50-100 mcg 0.15 - 0.7 20 mg 80 mcg/ml 5 - 20 min useful if HR Norepinephrine (Levophed) NR 0.05 - 0.5 8 mg 32 mcg/ml 2 - 10 min (phentolamine for extravasation) Epinephrine 0.3 - 0.5 mg 0.01 - 0.3 30 mg 120 mcg/ml 5 - 10 min Dopamine NR 5 - 20 400 mg 1600 mcg/ml < 10 min Dobutamine NR 2 - 30 250 mg 1000 mcg/ ml < 10 min Vasopressin (40 units Q 3min X2 for VF,PEA) 0.01-0.04 U/min for refractory shock < 20-30 min Milrinone (Primacor) 50 mcg/kg IV (load, 10 min) 0.25-0.75 mcg/kg/min (mix 20 mg in 100 ml NS); t 1/2 2 hr; renal cleared, ppt with lasix or bumex Nesiritide (hBNP,Natrecor) 2 mcg/kg (60 secs) then 0.01 mcg/kg/min infusion X 48 hrs; use: severe CHF; caution: BP (reduce dose 30%) Nitroprusside (Nipride) NR 0.1-10 50 mg 200 mcg/ml < 10 min acidosis; thiocyanate levels Nicardipine 50 ml/hr (5 mg/hr) increase 25 ml/hr (2.5 mg/hr) Q 5 (max 15 mg/hr higher OK?) Fenoldopam 0.1 mcg/kg/min (0.1 mcg/kg/min Q 15 min, max is 1.6 mcg/kg/min) note: D1 agonist, ?renal protective, levels on Tylenol Hydralazine 10 mg IV Q 10-15 min (max 50 mg); repeat dose Q 6h; caution: HR, CAD, dissection (useful with B-blocker or clonidine) Esmolol (Brevibloc) 0.5 mg/kg 1 min 50 - 300 2.5 g 10 mg/ml 10 - 20 min Labetalol (Trandate) 10 mg over 1-2 min (double Q 10 min, max 150 mg) infusion: 2 8 mg/hr 2-4 hr [IV is 7:1 beta:alpha] Amiodarone (Cordarone) 150-300mg over 10 min then 1mg/min x6 hr then 0.5mg/min x 18h 50 mg/ml Diltiazem (Cardizem) 0.25/0.35 mg/kg 5 -15 mg/hr 125 mg 500 mcg/ml 1-3 hr Adenosine 6 mg over 1-3 sec, 20 ml NS bolus may repeat 12 mg in 1-2 minX2; effect on theophylline; avoid dipyridamole or wide complex THROMBOLYTIC TX (TPA=ALTEPLASE) TPA (AMI) 15 mg Bolus50 mg over 30 min (0.75 mg/kg) 35 mg over 60min (0.5 mg/kg) (100 mg Total) TPA (PE) 100 mg over 2h TPA (stroke) 0.9 mg/kg (max 90 mg) over 1h (10% as initial bolus); <3h of sx onset; 6% ICH TPA (unclog lines or tubes) 2 mg/2 ml TPA (empyema) 0.1 mg/kg dilute in 50 100 ml saline into chest tube, clamp 1 hr, (repeat daily as needed); serial chest CTs GASTROINTESTINAL HEMATOLOGIC refractory coagulopathy+bleeding (liver, trauma, etc): Octreotide 50 mcg IV bolus then 50 mcg/hr X 5d Procrit (Epo) 600 u/kg (40,000 units) Q week rFVIIa 80-100 mcg/kg (t1/2 2.5 hrs, check PT 1 hr) Ranitidine (prevent GIB on MV) 50 mg IV q 8 hr DDAVP 0.3 mcg/kg IV (for uremic bleeding) Carafate (prevent GIB on MV) 1 gm po QID Estrogen 0.6 mg/kg days 1-5 prior to invasive procedure (for uremic bleeding) Omeprazole (bleeding PUD) 40 mg po BIDX5d Protamine 10-50 mg IV over 10 min. (1mg antagonizes 100 units UF heparin or 1 mg LMWH) Pantoprazole (bleeding PUD) 80 mg IV 8 mg/hrX3d DVT Prophylaxis (serial ultrasound high risk pts)+TEDs, PCDs Neostigmine (pseudobstruction) 2 mg IV over 3 mins Heparin 5000 U SQ BID-TID or Fondaparinux (Arixtra) 2.5mg SQ QD (start >6 h post-op) or ENDOCRINE Enoxaparin (Lovenox) 40mg SQ QD (30 mg if < 45 kg) or 30mg SQ BID (40 mg SC BID if > 150 kg) Insulin 0.1U/kg IV bolus 0.1 U/kg/hr infusion DVT/ PE Treatment (TPA if shock, severe PaO2, IR consult for severe DVT+ catheter-based tx) HC 50 mg IV Q 6h or 100 +10 mg/hr IV [adrenal shock] Heparin 80 unit/kg load , then 18 unit/kg/hr infusion to PTT 72-125 (use nomogram) or Relativeadrenal: shock and < 9 with Cosyntropin Enoxaparin 1mg/kg SQ Q 12hr (max dose 150 mg) (target goal 4 h post- dose: anti-Xa 0.5-1.2 u/ml) or Thyrotoxic: PIPS-PTU,SSKI,Propranolol,Decadron Fondaparinux (Arixtra) 7.5 mg SQ QD (5 mg if < 50 kg, 10 mg if > 100 kg) Myxedema coma: liothyronine (T3) 10-25 mcg IV Q 12 h HIT Type II Tx (monitor platelets on UFH or LMWH)Lepirudin 0.4 mg/kg [max 44 mg] IV bolus 0.15 Diabetes insipidus: DDAVP 1-2 mcg QD-BID SC or IV mg/kg/hr, renal dz or Argatroban no bolus, 210 mcg/kg/min IV , aPTT 1.5-2.5 X [check in 2 hr],liver dz SEPSIS/SEPTIC SHOCK: Early Sepsis Tx Goals : CVP 8-12 [500 ml Q 30 min], ScvO2 > 70%[Hct 30% if ScvO2 <70?], MAP 65-90, antibiotics <4hr XIGRIS 24 mcg/kg/h IV X 4 d [if Apache 25, platelets > 30K, contra: active bleeding, stroke < 3 months, CNS surgery -trauma<2 mo; DC 2 hr prior to invasive proc] REFRACTORY SHOCK consider Hydrocortisone, Vasopressin, Epi, IVIg (for TSS), Calcium, Glucagon (latter two especially if on B-blocker or Ca-blocker) [WHMC/BAMC Adult Critical Care Ref Sheet, Revised Dec 10, 2005, Stephen Derdak, D.O, Pulmonary/Critical Care Medicine 210-292-5235, sderdak@mac.com]
NEUROLOGY SEIZURES: thiamine-glucose- lorazepam-phenytoin- phenobarbial-midazolam-propofol (mech vent+continuous EEG monitoring) Phenytoin 15-20 mg/kg IV load @ 50 mg/min [mix in 0.9NS], then 5 mg/kg IV/PO q 24 hr in 3 divided doses; Corrected level = Phenytoin level / (0.2 x albumin + 0.1) Phenobarbital 15-20 mg/kg IV load up to 300-800 mg IV at 50-75 mg/min IVIg 400 mg/kg days 15 (Guillain-Barre, Myasthenic Crisis) Mannitol 0.5-2.0 g/kg of 20% solution over 30-60 min or 12.5-25 g over 5-10 min Nimodipine 60 mg po Q 4hX 21d (for SAH vasospasm) Spon ICH: stat neuro consult; ? rFVIIa 80 or 160 mcg/kg IV [if sx<3h, GCS >5, no ASCVD hx; mortality 11%,p=0.02, ?risk MI,ischemic stroke 7% vs 2%,p=0.12] Ischemic STROKE: TPA 0.9 mg/kg (max 90 mg) over 1h (10% as initial bolus); [if sx<3 h and not improving+minimal CT findings; repeat CT 24h; 6% risk ICH!] Vasospasm -SAH: TRIPLE H TX: Hypervolemia [CVP 10-12, PCWP 12-18], Hemodilution [Hct 30-35%], Hypertension [20% > baseline or systolic 150-200]; contra: cerebral infarct or edema, ICP; caution: pulmonary edema 17%; IR consult [angioplasty?, intra-arterial papaverine?] NMS:[rigid, dysautonomia, MSDs] bromocriptine 2.5 mg po [2.5-5.0 mg po tid],dantrolene 1mg/kg IV continuous push till symptoms resolved [max 10mg/kg; also for MH], ECT?, amantidine? Lethal Catatonia: ECT, benzodiazepines Adjunctive clearance modalities SS [above sx+seizures, myoclonus, reflexes]: cyproheptadine 4-8 mg PO (max 8 mg QID)+benzodiazepine? MDAC:carbamazepine, phenobarbital, TOXICOLOGY theophylline, dapsone, salicyclates, COCAINE:agitation or SVT (lorazepam), seizures (phenobarb), VT (NaHCO3, Mg), BP (Nipride,NTG, phentolamine) quinine, ext. release or significant Glucagon (Ca++ or B-blocker OD) 3-10 mg IV bolus 2-5 mg/hr [if severe: insulin 0.1-10 u/kg/hr+glucose10-75g/hr] intrahepatic/enteric recirculation Naloxone (Narcan) 0.1-0.4mg IM/IV/SQ q3 min Urinary Alk: salicylates, phenobarb Flumazenil (Romazicon) 0.2 mg/.IV q min up to 1mg max 5 min. or 3 mg max 1 hr Hemodialysis: alcohols, Li+, Fomepizole (methanol, EG OD) 15 mg/kg IV load 10 mg/kg Q 12 hrX48hr15 mg/kg Q 12hr(till methanol,EG< 20) salicylates, theophylline Ethanol (methanol, EG OD) 1g/kg (10 ml/kg) of 10% ethanol (100 mg/ml) IV over 1-2 hr; then 100 mg/kg/hr Hemoperfusion: theophylline, Octreotide (sulfonylurea OD) 40-100 mcg SQ Q 6-12 hr X 2-3 days (monitor glucose 24 hr after DC) + D10W valproate, carbamazepine, Acetylcysteine (Tylenol OD) 140 mg/kg load of 10-20% solution PO or IV then 70 mg/kg q4h x 17 doses phenytoin,procainamide, paraquat Methylene blue (MetHb) 1-2 mg/kg over 5 minutes WBI (PEG 1-2 L/hr): Iron, SR tabs, Li, Activated Charcoal 1 g/kg with sorbitol[ineffective with LMW,Lithium,heavy metals] packers CroFab (snake bite) 4-6 vials [repeat 1 hr if severe]2 vials Q 6 hr X 18 hr Digoxin immune Fab (Digibind) 38mg/vial, # vials = dig level (ng/ml) x wt (kg) / 100 IV over 30 minutes ACID/BASE FORMULAS COMPENSATION RULE OF 80s (last 2 digits pH+PaCO2): 1. Metabolic Acidosis PaCO21.25 mmHg per mEq/L D HCO3 pH + PaCO2 = 80 (pure resp disorder) 2. Metabolic Alkalosis PaCO2 0.75 mmHg per mEq/L D HCO3 pH + PaCO2 < 70 (met acidosis) 3. Respiratory Acidosis (PaCO2> 45): Acute:HCO3 1 mEq/L per 10 mm PaCO2 pH + PaCO2 > 90 (met alkalosis) Chronic:HCO3 4 mEq/L per 10 mm PaCO2 4. Respiratory Alkalosis (PaCO2< 35): Acute:HCO3 2 mEq/L per 10 mm PaCO2 Chronic:HCO3 4 mEq/L per 10 mm PaCO2 RENAL FORMULAS: **HIGH RISK FOR CONTRAST NEPHROPATHY? PO hydrate+ H2O gain or loss = 0.6Xkg-0.6Xkg x Na/140 1. Mucomyst 600 mg PO bid X 4 doses -start 24 h pre-contrast Free H2O Deficit (L) = 0.6 kg x (Na /140 1) 50% over 8 hours then remainder over 16 hours plus 0.9NS 1 ml/kg/hr 12 hr pre 6 hr post OR Potassium Deficit (mEq) = 370 mEq for each 1 mEq fall in serum K [pH 0.1K 0.6] 2. NaHCO3 (3 amps in D5W) 3 ml/kg 1 hr pre+1 ml/kg/hr 6hr post HCO3 deficit (mEq)= 0.5 kg (Desired HCO3 - measured HCO3) Replace 50% then recheck Osmolality (calculated) = 2 Na + (BUN/2.8) + (Glucose/18) + (EtOH level/4.6) normal gap < 10 mOsm [glucose 100Na 1.35] CH2O=Uvolume X ([UNa + UK]/ P Na Hi-Dose Diuretic: Lasix 100 mg IV20 mg/h (double Q 12-24 h, max 160 mg/hr; Cl- >95) or torsemide 20 mg IV/PO (200 mg/d) HEMODYNAMIC FORMULAS Normal * CI = *CO/BSA 2.8-4.2 l min- 1 m-2 [false low COTDwith TR, false high COTD with cardiac shunts] SV = CO/HR 60-90 ml/beat MAP = DP + 1/3 (SBP - DBP) 80-120 mm Hg SVR = [(MAP - CVP) / CO] x 80 900-1400 dynes-cm-sec3 SVRI =[(MAP - CVP)/CI 1900-2400 dynes-cm-m3 PVR = [(MPAP - PAOP)/CO] x 80 100-250 dynes-cm-sec3 [Echo estimate of PAs y s=4V2+RAP] PVRI =[(MPAP - PAOP)/CI] x 80 45-225 dynes-cm-sec3 ALVEOLAR OXYGEN TENSION = (Pb - PH20) FiO2- PaCO2/0.8 PAO2-PaO2 < 15 mmHg ARTERIAL OXYGEN CONTENT: CaO2 = (SaO2) (Hb x 1.34) + PaO2 (0.0031) 21 ml 100 ml- 1 VENOUS OXYGEN CONTENT: CvO2 = (SvO2) (Hb x 1.34) + PvO2 (0.0031) 15 ml 100 ml- 1 PHYSIOLOGIC DEAD SPACE (BOHR): Vd/Vt = (PaCO2 - PECO2)/PaCO2 < 0.33 FICK EQUATION: CO=VO2/(CaO2-CvO2) x 10 3.5-5.5 L/min OXYGEN CONSUMPTION: VO2 = CO (CaO2 -Cvo2) x 10 225-275 ml/min (3.5 ml/kg/min; 125 ml/min/m2) OXYGEN DELIVERY: DO2= CO(CaO2) x 10 1000 ml min- 1 OXYGEN EXTRACTION RATIO: O2ER = VO2/DO2 22-30% OXYGENATION INDEX: OI = [(Mean Airway Pressure)(FiO2)]/PaO2 <10 normal: > 30 HFOV or ECMO CEREBRAL PERFUSION PRESSURE: CPP= MAP-ICP > 80 mmHg [normal ICP<10 mm Hg; start tx if ICP>20 or CPP< 60 or SjO2<55%] NUTRITION-METABOLIC CALCULATIONS Weir Equation: REE = 5.68 VO2 + 1.59 VCO2 - 2.17 Nu Modified Weir: REE = 7 x VO2 REE(kcal) = 25-30 kcal/kg/d H2O Maintenance = 30-35 ml/kg/d CHO = 4 cal/gm, protein = 4 cal/g , fat = 9 cal/g Non-protein kcal ratio =CHO:FAT 60-70:30-40 N2 Balance = (Total protein intake (g) / 6.25) - (UUN + 4g) Protein required: 1-1.5 g/kg/d PBW(kg) Male = 50 + 2.3 [height (in) 60] PBW(kg) Female = 45.5 + 2.3 [height (in) 60] height=crown-heel or arm span/1.06 MECHANICAL VENTILATION initial settings [then use ARDS Algorithms for CV, APRV, HFOV] 1. (CV) Volume-control (for ARDS) VT 6 ml/kg PBW, I:E 1:2-1:1, PEEP 10, Pplat 30, RR 15 35 , Flow triggering 1-3 L/min (see PBW formulas above) 2. (CV) Pressure-control (for ARDS) Ppeak 30-40 (target VT 6 mg/kg PBW), I:E 1:2-2:1, PEEP 10, RR 12 35 3. APRV/BiLevel (for severe ARDS) Phi 3035, Plo 0, Thi 4.5, Tlow 0.80.4 (adjust Tlow to 40% PEFR; monitor VT,VE,autoPEEP), ATC on, no paralytics OR 4. HFOV (3100B if >35kg) mPaw 34 ,DP 90, Hz 7 [if pH<7.25 cm H2O cuff-leak+Hz 6-5-4-3], IT%=33, BF 40 L/min [start if Pplat >30, Phi>35+ FiO2>70%] 5. (CV) Volume-control (for severe COPD,asthma) VT 6 ml/kg PBW, I:E 1:3-8, no PEEP, Pplat 30 (monitor iPEEP, Ppeak-Pplat), RR 12 Notes: 1. Severe ARDS (P/F < 100, OI > 30) for CV modes may PEEP to max 24 (but keep Pplat 30), may I:E to 2:1, measure bladder pressure [=abdomen] 2. Severe ARDS consider prone positioning, recruiting maneuvers (CPAP 40-45-50 cm H2O X 40-60 secs), rarely iNO (5 ppm, daily dose re-titration) 3. Conventional Ventilation: PaCO2X VT (or VE or rate) = desired PaCO2 X new VT (or new VE or new rate) 4. Weaning: daily breathing trials when FiO250% and PEEP8 cm H2O; consider extubation to BiPAP for appropriate candidates (e.g. COPD) 5. Consider BiPaP or IPV for non-intubated patients with muscle weakness [VC<15 ml/kg, MIP<30]prone to atelectasis (e.g. spine, chest wall injury) 6. No HME: VE>10, T<32,thick-copius secretions, prior ETT block, BPF, cuff-leak, frequent MDI or aerosols, difficult triggering -weaning (severe COPD) [WHMC/BAMC Adult Critical Care Ref Sheet, Revised Dec 10, 2005, Stephen Derdak, D.O, Pulmonary/Critical Care Medicine 210-292-5235, sderdak@mac.com]
Вам также может понравиться
- Common ICU DripsДокумент1 страницаCommon ICU DripsSunshine Willis100% (2)
- SA Anesthesia Drug Dosages 2022Документ3 страницыSA Anesthesia Drug Dosages 2022KRLITHIU Borja100% (1)
- Critical Care Survival GuideДокумент2 страницыCritical Care Survival Guidetringalama100% (4)
- Vasopressors and InotropesДокумент4 страницыVasopressors and InotropesSdОценок пока нет
- Drug Cheat SheetДокумент2 страницыDrug Cheat SheetThomas Hart IIIОценок пока нет
- FLASH CardsДокумент3 страницыFLASH Cardsclarheena100% (2)
- Critical Care Intravenous DrugsДокумент1 страницаCritical Care Intravenous DrugsMarynel Dixie Izon Brao90% (10)
- Fluid and Electrolyte Balance in ICUДокумент46 страницFluid and Electrolyte Balance in ICUtapas_kbОценок пока нет
- Critical Care Medication Infusion ChartДокумент2 страницыCritical Care Medication Infusion ChartEgi Munandar100% (1)
- Criticalcaredrugs PDFДокумент2 страницыCriticalcaredrugs PDFtomywekaОценок пока нет
- CCRN-PCCN Review GastrointestinalДокумент23 страницыCCRN-PCCN Review GastrointestinalGiovanni MictilОценок пока нет
- Icu Nurse SheetДокумент1 страницаIcu Nurse SheetJan MarcusОценок пока нет
- ICU HandbookДокумент146 страницICU HandbookBulent InanОценок пока нет
- ICU Cheat SheetДокумент2 страницыICU Cheat SheetPrescilla Randazzo100% (1)
- Resident Hernia LectureДокумент106 страницResident Hernia Lecturesgod34Оценок пока нет
- Example of Completed Form: Admit Dx/Chief Complaint/Hx Current ILLNESS: - Bowel Obstruction RespiratoryДокумент3 страницыExample of Completed Form: Admit Dx/Chief Complaint/Hx Current ILLNESS: - Bowel Obstruction RespiratoryJosephОценок пока нет
- Hemodynamic Drug InfusionsДокумент45 страницHemodynamic Drug InfusionsDawit MucheОценок пока нет
- Pediatric Anesthesia Drug DosagesДокумент3 страницыPediatric Anesthesia Drug Dosageslhalam80% (5)
- CCU Clinical GuidelinesДокумент63 страницыCCU Clinical GuidelinesHAMMYER ALROKHAMIОценок пока нет
- EVD PosterДокумент1 страницаEVD PosterDwie 'keonk' UnisaspalaОценок пока нет
- ICU Drips: Stephanie Sanderson, RN, MSN, CNS, CCNS, CCRN Medical Cardiac ICU-UNMHДокумент32 страницыICU Drips: Stephanie Sanderson, RN, MSN, CNS, CCNS, CCRN Medical Cardiac ICU-UNMHNicole Adkins100% (1)
- Drugs in Cardiac EnmergenciesДокумент94 страницыDrugs in Cardiac EnmergenciesVijayan VelayudhanОценок пока нет
- Riker ABSITE ReviewДокумент36 страницRiker ABSITE Reviewsgod34Оценок пока нет
- Drug Infusion Guide For SORT PDFДокумент5 страницDrug Infusion Guide For SORT PDFAli HasanОценок пока нет
- ACLS Algorithms Adult 2010 Revised May 31 2011Документ12 страницACLS Algorithms Adult 2010 Revised May 31 2011arturschander3614Оценок пока нет
- Absite Review VascularДокумент183 страницыAbsite Review Vascularsgod34Оценок пока нет
- ICU Progress NoteДокумент7 страницICU Progress NoteDiana Hylton100% (1)
- MN105613 PICU2022 Book ProofДокумент60 страницMN105613 PICU2022 Book ProofErwin Dela GanaОценок пока нет
- Admitting OrdersДокумент4 страницыAdmitting OrdersRommel OliverasОценок пока нет
- Management of Patients With Dysrhythmias and Conduction ProblemsДокумент29 страницManagement of Patients With Dysrhythmias and Conduction ProblemsYlanni Coritana100% (1)
- Anaesthetic Drug Crib Sheet-8 PDFДокумент1 страницаAnaesthetic Drug Crib Sheet-8 PDFRicky Andhika Pratama100% (1)
- ACLS Drugs&Drips Final PDFДокумент6 страницACLS Drugs&Drips Final PDFmesrianti_rubenОценок пока нет
- ICE DrugsДокумент2 страницыICE DrugsRichelle FrondaОценок пока нет
- 6 PacuДокумент15 страниц6 PacuFarrukh Ali KhanОценок пока нет
- ICU Registered Nurse Resume Brick RedДокумент2 страницыICU Registered Nurse Resume Brick RedAngelОценок пока нет
- Paediatric Critical Care Infusions Intubation DrugsДокумент2 страницыPaediatric Critical Care Infusions Intubation DrugsА. Сосорбарам100% (1)
- Critical Care Drug Reference SheetДокумент12 страницCritical Care Drug Reference SheetYanina CoxОценок пока нет
- RN Surival Guide With Blanks v5Документ61 страницаRN Surival Guide With Blanks v5api-620640264Оценок пока нет
- Dosage CalculationsДокумент39 страницDosage Calculationssalak9462900% (1)
- Drug Card Emergency DepartmentДокумент2 страницыDrug Card Emergency Departmentdrmohdtanveer100% (3)
- Drug Name Onset Concentration Dosing Instructions Drug Class How To TitrateДокумент1 страницаDrug Name Onset Concentration Dosing Instructions Drug Class How To Titrateje hanОценок пока нет
- ACLS PharmacologyДокумент5 страницACLS PharmacologyKuruva MallikarjunaОценок пока нет
- Emergency Lecture PDFДокумент57 страницEmergency Lecture PDFDuane Liloc100% (1)
- Resuscitation MedicationДокумент1 страницаResuscitation MedicationDen SinyoОценок пока нет
- Modul EKGДокумент101 страницаModul EKGAjeng Dwik01Оценок пока нет
- Sedation in IcuДокумент2 страницыSedation in Icumathurarun2000Оценок пока нет
- HW InotropesДокумент3 страницыHW InotropesNatalie YeohОценок пока нет
- Intravenous Anesthetic AgentsДокумент23 страницыIntravenous Anesthetic Agentsdrhiwaomer100% (7)
- DRIPSДокумент7 страницDRIPSKim Alvarez100% (2)
- Anasthetic DrugsДокумент62 страницыAnasthetic DrugsMilda InayahОценок пока нет
- Necrotizing Otitis 2022Документ20 страницNecrotizing Otitis 2022asmashОценок пока нет
- Cardiac MedicationsДокумент8 страницCardiac Medicationsangeline totaram100% (2)
- Venous DiseaseДокумент50 страницVenous Diseasesgod34Оценок пока нет
- C-Section Room Setup:: OB Rotation NotesДокумент5 страницC-Section Room Setup:: OB Rotation NotesEricОценок пока нет
- Modes of Mechanical VentilationДокумент4 страницыModes of Mechanical Ventilationsgod34100% (1)
- Critical Care Drugs 2Документ23 страницыCritical Care Drugs 2Asri Ernadi100% (1)
- Arterial Lines in PACU: Presented by Autum Jacobs RN, BSNДокумент34 страницыArterial Lines in PACU: Presented by Autum Jacobs RN, BSNinuko1212Оценок пока нет
- Practice Standards For The Emergency Nurse Specialist. CENA, 2014Документ16 страницPractice Standards For The Emergency Nurse Specialist. CENA, 2014Cristobal Alejandro Falado SantanderОценок пока нет
- Shock Study GuideДокумент8 страницShock Study GuideMadameb1Оценок пока нет
- Acls Course HandoutsДокумент8 страницAcls Course HandoutsRoxas CedrickОценок пока нет
- Nursing Care of PlanДокумент16 страницNursing Care of PlanDbyОценок пока нет
- Hemodynamics For The Bedside Nurse 1CEUДокумент7 страницHemodynamics For The Bedside Nurse 1CEURN333100% (1)
- NURSING CARE OF ADULTS II: Passbooks Study GuideОт EverandNURSING CARE OF ADULTS II: Passbooks Study GuideОценок пока нет
- Nutrition Support: Sean P Harbison MDДокумент42 страницыNutrition Support: Sean P Harbison MDsgod34Оценок пока нет
- Surgery Preround Template SkeletonДокумент2 страницыSurgery Preround Template Skeletonsgod34Оценок пока нет
- NOAC ChartДокумент2 страницыNOAC Chartsgod34Оценок пока нет
- Master Schedule 10-22Документ65 страницMaster Schedule 10-22sgod34Оценок пока нет
- Veins More DistensibleДокумент27 страницVeins More Distensiblesgod34Оценок пока нет
- Colon CAДокумент16 страницColon CAsgod34Оценок пока нет
- 7 MedEd Vascular Jonny Hodgkinson 12.11.12 1Документ35 страниц7 MedEd Vascular Jonny Hodgkinson 12.11.12 1sgod34Оценок пока нет
- Endoscopy TechniqueДокумент8 страницEndoscopy Techniquesgod34Оценок пока нет
- Anast Bleed MMДокумент17 страницAnast Bleed MMsgod34Оценок пока нет
- HD Monitoring ColoradoДокумент28 страницHD Monitoring Coloradosgod34Оценок пока нет