Академический Документы
Профессиональный Документы
Культура Документы
Thyroid 9
Загружено:
prelude_t0Исходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Thyroid 9
Загружено:
prelude_t0Авторское право:
Доступные форматы
Clinical Endocrinology (2004) 61, 6174
doi: 10.1111/j.1365-2265.2004.02060.x
Diagnostic value of serum thyroglobulin measurements in the follow-up of differentiated thyroid carcinoma, a structured meta-analysis
Blackwell Publishing, Ltd.
C. F. A. Eustatia-Rutten*, J. W. A. Smit*, J. A. Romijn*, E. P. M. van der Kleij-Corssmit*, A. M. Pereira*, M. P. Stokkel and J. Kievit Departments of *Endocrinology, Nuclear Medicine, Medical Decision Making and Surgery (section Endocrine Surgery), Leiden University Medical Centre, Leiden, the Netherlands
(Received 24 July 2003; returned for revision 5 August 2003; nally revised 23 February 2004; accepted 6 May 2004)
Summary
OBJECTIVE To investigate to what extent thyroid rem-
nant ablation and withdrawal from thyroxine are required to achieve sufcient accuracy of serum thyroglobulin (Tg) measurements as an indicator of tumour recurrence in the follow-up of patients with differentiated thyroid carcinoma. DESIGN AND METHODS We conducted a meta-analysis of the literature from 1975 to 2003 on serum Tg measurements in the follow-up of differentiated thyroid carcinoma. In a computer-based search, we initially found 915 articles that were nally narrowed down to 120.These 120 papers were subjected to strict in /and exclusion criteria, leaving 46 articles (totalling 9094 patients). Data from these articles were extracted in a structured fashion and were grouped according to initial therapy, TSH status, Tg assay method and denition of a gold standard. Original 2 2 tables were pooled by summary receiver operating characteristic curve analysis (sROCa), best estimates of sensitivity and specicity being obtained by the combination of sROCa and Mantel Haenszel odds ratios. RESULTS Despite considerable differences between series in laboratory and clinical methodology, we consistently found higher specicity for Tg measurements after thyroid remnant ablation than after surgery alone. Highest pooled sensitivity 0961 0013 (SE) was found
for immunometric assay (IMA) after thyroid remnant ablation and thyroid hormone withdrawal, at a specicity of 0947 0007. Pooled sensitivity decreased signicantly if ablated patients were tested while on thyroid hormone (0778 0023, at a specicity of 0977 0005). Signicantly decreased pooled specicity was found in patients who did not undergo remnant ablation (sensitivity 0972 0023, at a specicity of 0759 0028). If recombinant human TSH (rhTSH) stimulation was used as a substitute for thyroxine withdrawal, sensitivity remained high (0925 0018) while specicity decreased to 0880 0013. In all analyses, specicity of Tg would decrease when unspecied activity in the thyroid region at scintigraphy was considered benign, whereas sensitivity decreased when such activity was considered malignant. CONCLUSION This study conrms that the best accuracy of Tg-guided follow-up in patients treated for differentiated thyroid carcinoma is obtained if treatment includes remnant ablation, and Tg testing is performed while off thyroxine.
Correspondence: J. W. A. Smit, Department of Endocrinology, C4-R, Leiden University Medical Centre, PO Box 9600, 2300 RC Leiden, the Netherlands. Tel.: + 31 715263082; Fax: + 31 715248136; E-mail: jwasmit@lumc.nl 2004 Blackwell Publishing Ltd
Differentiated thyroid carcinoma has a 10-year survival of 9095% (Hundahl et al., 1998). This favourable prognosis is the result of both the biological properties of most thyroid carcinomas and effective primary therapy. In most patients, initial therapy consists of total thyroidectomy followed by radioiodine ablation of thyroid remnants (Schlumberger, 1998). Although some controversy exists about the routine application of radioiodine ablation of thyroid remnants, this procedure has been adopted by several organizations, including the American Thyroid Association (Singer et al., 1996), the National Cancer Centre Network and the British Thyroid Association (British Thyroid Association, 2002), because of a benecial effect on recurrence and mortality in patients with higher tumour stages or residual tumour (DeGroot et al., 1990; Elgart et al., 1991; Samaan et al., 1992; Taylor et al., 1998; Michal et al., 1999). Despite this overall good prognosis, subgroups of patients are at higher risk for recurrent disease or death (Gilliland et al., 1997; Schlumberger, 1998; Mazzaferri & Kloos, 2001). The purpose of follow-up protocols in thyroid carcinoma is the early detection 61
62 C. F. A. Eustatia-Rutten et al.
of recurrent or metastatic thyroid cancer. Most patients during follow-up have been cured denitely after their initial treatment and as a consequence have a low pretest probability for recurrent disease. Therefore, sensitivity must be adequate to detect the few patients with evident thyroid carcinoma whereas specicity must also be high to avoid unnecessary treatments in patients without recurrent disease. In addition, patient burden should be kept at a minimum. Most follow-up protocols are based on measurements of serum thyroglobulin (Tg) concentrations, both during and after withdrawal from TSH suppressive thyroxine therapy as well as on radioiodine scintigraphies, after withdrawal from thyroxine therapy. The serum Tg concentration reects the mass of benign and/or malignant thyroid tissue present and the magnitude of TSH-receptor stimulation. Although many studies have been published on the diagnostic strategies during follow-up of thyroid carcinoma, uncertainties with respect to Tg measurements remain. In the present study we summarize available evidence on Tg-follow-up accuracy according to modern meta-analytic methods. In the follow-up of patients who have been treated for differentiated thyroid cancer, an important clinical question is whether Tg-testing while on thyroxine provides sufcient accuracy to guide retreatment with 131I. If this is not the case, some form of thyroid metabolism stimulation, such as thyroxine withdrawal, is required to improve test performance, and thus decrease misses of cancer recurrence. Withdrawal from thyroxine therapy is a serious burden for the patient as he/she will suffer from symptoms of hypothyroidism (Dow et al., 1997). This disadvantage may be overcome by the application of recombinant human TSH (rhTSH) (Haugen et al., 1999). In addition, a theoretical disadvantage of thyroid hormone withdrawal is the exposure of the patient to high thyrotrophin concentrations, which may be unfavourable with respect to enhancement of tumour proliferation (Lukinac et al., 1996). In a recent published consensus report (Mazzaferri et al., 2003), based on a meeting of 13 American and two Italian experts, it was recommended that patients in the follow-up of thyroid carcinoma should undergo TSH-stimulated Tg measurements. This advice was based on the analysis of eight retrospective studies on rhTSH and a review of 10 studies, with an overall sensitivity of TSH-stimulated Tg measurements of almost 91%. A second question of the present study is whether this advice still holds when a formal meta-analysis of the literature is performed according to up-to-date methods. In the present study the questions posed above were answered by a formal literature review, followed by a meta-analysis of 46 carefully selected articles on the diagnostic value of Tg measurements in the follow-up of differentiated thyroid carcinoma, which were selected according to strict inclusion criteria from an initial set of 915.
Materials and methods A computer-aided search of MedLine was conducted for articles on humans, written in English and published between January 1975 and November 2003, using the search terms thyroid carcinoma (textword) and thyroglobulin (textword). The last date of data acquisition was December 7, 2003. The search was limited to articles containing abstracts. All abstracts were screened by two independent reviewers (C.F.A.E.-R. and J.W.A.S.), on whether they provided own quantitative data on the diagnostic value of Tg in the follow-up of differentiated thyroid carcinoma, or suggested that such information would be present in the article. Initial judgement differences were resolved by repeated review and consensus. Thus 120 articles remained. Subsequently, these 120 studies were read in full and subjected to criteria for diagnostic tests as recommended by the Cochrane Methods Group on Screening and Diagnostic Tests (www. cochrane.org) and guidelines developed by the Standards for Reporting on Diagnostic Accuracy Group (STARD) (Bossuyt et al., 2003). These criteria include key elements of design, conduct and analytical methods: a description of the study population and the recruitment of patients, a description of the design of the study, a description of the phase of the disease (postoperative, postablative), a description of Tg assays including technique and cut-off values, whether patients were tested during thyroxine therapy (on or off thyroxine) and whether patients with Tg antibodies were excluded and the description of a gold or reference standard. Thus, a total of 74 articles were excluded for one or more reasons as indicated in Appendix 1. In the remaining 46 articles, summarized in Appendix 1, the design of the study was indicated as prospective or retrospective. The description of the study population was veried with regard to age and sex distribution, tumour type, tumour stage and whether the study population contained an unselected cohort of patients or a subgroup of patients with residual tumour or metastases. This was evaluated by calculating the ratio between the number of tumour cases and total patients (prevalence or pretest probability). Based on the prognosis of thyroid carcinoma (Schlumberger et al., 1997; Hundahl et al., 1998), a prevalence of < 02 was considered as in agreement with an unselected study group. The phase in the follow-up (postsurgical or postablative) was registered as well as the time after initial diagnosis. The Tg assay method was registered [radioimmunoassay (RIA) or immunometric assay (IMA), including immunoradiometric assay (IRMA) and immunochemiluminometric assay (ICMA)] the Tg cut-off values recorded, and whether Tg was measured during thyroxine therapy (on), during withdrawal (off) or during rhTSH. When an article contained multiple analyses, such as postsurgical and postablative, on and off thyroxine therapy, all these subseries were registered separately. Series were excluded if the number
2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Diagnostic value of serum Tg measurements in thyroid carcinoma 63
of patients was ve or less, leaving a total of 68 data series out of the 46 articles. The following criteria for active disease (reference standard or gold standard) were found: radioiodine scintigraphy (pathological extrathyroidal accumulation of radioiodine), other radiological examinations [X-ray, ultrasound, computed tomography (CT), magnetic resonance imaging (MRI), positron emission tomography (PET)], histology and follow-up (up to 3 years, considering the generally slow proliferation rate of thyroid carcinoma). A particular problem is the interpretation of thyroid remnants at scintigraphy. Although radioiodine accumulation in the thyroid region after ablation therapy represents benign thyroid tissue in the majority of cases, a nal conclusion can only be drawn when additional criteria are applied to establish the nature of the abnormality, including histology or follow-up data of the patients. Therefore, when activity in the thyroid region was classied as benign thyroid remnants we only maintained this designation when proof of the benign character was given explicitly. In all other cases, activity in the thyroid region was classied as unspecied activity in the thyroid region. The number of cases was determined in each series according to the criteria for active tumour as found in the original article. When radioiodine scintigraphy was used, extrathyroidal activity was considered as proof of tumour. Because, in most articles, no clear criteria were given for the benign or malignant character of activity in the thyroid region, we performed three separate analyses: in the rst analysis, we excluded all patients with as sole nding thyroid region activity; in the second analysis, we considered all unspecied activity in the thyroid region as malignant; and in the third analysis, we considered all thyroid region activity as benign. Sensitivity and specicity in each series were recalculated according to the positive and negative cases found and the number of patients with Tg values above or below the threshold values as used in the original articles. Reported values for sensitivity or specicity as mentioned in the original articles were ignored. A meta-analysis of sensitivity, specicity and positive predictive value was performed by pooling all data from all data series, discriminating between the phase of the study (postsurgical or postablative), whether or not thyroxine treatment was withdrawn or rhTSH was given, Tg assay method and reference standards (scintigraphy only or more methods as well). All original 2 2 tables were imported in a predesigned spreadsheet, and were combined using a three-step method from simple counts, and MantelHaenszel calculations to summary receiver operating characteristic analysis (sROCa). The exact statistical procedure is summarized in Appendix 2. This three-step procedure, combining the advantages of sROCa validity with the point estimate practicality of straight counts and MantelHaenszel odd ratios provided us with the combined estimates of sensitivity and specicity on which we based our comparison of Tg-measurement protocols.
2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Sensitivities, specicities and odds ratios were tested for heterogeneity, using the methods according to http://www.cochrane.org/ software/revman42/User_guide.pdf. Heterogeneity may be explained either by studies using different cut-off levels for essentially the same ROC-curve (which is the reason why we summarize using sROC-methods in the rst place) or by studies reporting from tests summarized by different ROC-curves, or by both. Because discerning between these different causes for heterogeneity is beyond the scope of this paper, we only report observed heterogeneity. Standard errors (SE) and 95% condence intervals were calculated for each variable estimate of sensitivity, specicity or accuracy, as indicated in Appendix 2. Results All studies were retrospective analyses with the exception of Haugen et al. (1999). Criteria for gold standards were often difcult to discern. It was not clear in many studies whether procedures, mentioned as gold standards, were applied in all patients included in the studies. We have to assume that this is not the case in retrospective series for more complicated procedures such as CT or MRI. The distribution of age, sex, tumour type and tumour stage were in accordance with expected frequencies. However, the number of series in which tumour prevalence was > 02 was 35. In seven of these series, it was stated in the text of the article that the patients were indeed selected. In 28 series with a prevalence of > 02, the criteria for patient selection were not mentioned. We grouped the data according to phase of the disease, on or off thyroxine, Tg method and cut-off values, and reference standards, and analysed them as indicated in Appendix 2. Each group was comparable with regard to patient characteristics, follow-up duration and Tg thresholds. Homogeneity analysis in general revealed no signicant heterogeneity. The only case in which signicant heterogeneity was observed was Tg by IMA on thyroxine, when aspecic thyroid region activity at scintigraphy was considered to represent benign thyroid tissue. This is indicated in Fig. 1. As the category of patients without thyroid ablation, on thyroxine, comprised only three studies, data were not pooled. Sensitivity was 1000 and specicity 0750 in Valimaki and Lamberg (1985); however, this study contained only one tumour case. In Ronga et al. (1990), sensitivity and specicity were 0833 and 1000, and in Pacini et al. (1985), sensitivity was 0833, specicity 0921. The clinically most relevant data are the sROCa estimates of Tg sensitivity and specicity for four categories of patients: (a) without ablation off thyroxine, (b) with ablation on thyroxine, (c) with ablation off thyroxine and (d) with ablation, stimulated using rhTSH. For each of these four sets, data were analysed three times, excluding neck activity on 131I scanning (considered default
64 C. F. A. Eustatia-Rutten et al.
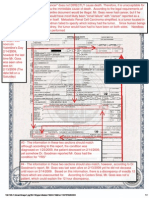
Fig. 1 Receiver operator characteristic (ROC) curves in which the values for sensitivity and specicity of thyroglobulin measurements with IMA are extracted from the individual patient series using summary ROC analyses, as indicated in Materials and Methods. The four sets represent the various Tg-testing protocols. In (a) analyses exclude patients with aspecic activity in the neck region at whole-body scintigraphy as the only abnormality. In (b) neck activity is considered to represent a tumour and in (c) neck activity at scintigraphy is considered to represent benign thyroid remnants. Error bars indicate the size of the 95% condence interval (2 SE of the estimate) around sensitivity and specicity, being depicted in the lower (for sensitivity) and right (for 1-specicity) direction only for the sake of clarity. In (c) heterogeneity was observed in Tg-on.
estimate) (Table 1, Fig. 1a), and interpreting such activity as either malignant or benign thyroid tissue (Fig. 1b,c). Patients without thyroid ablation, during thyroxine withdrawal Twelve series from 10 articles were included in this category. Data are summarized in Table 1a and Fig. 1. The range for
sensitivity was 05001000, for specicity 02141000, when patients with unspecied thyroid region activity were excluded. The studies with remarkably high specicity (Valimaki & Lamberg, 1985; Dadparvar et al., 1995) were limited by the fact that they were small, and contained only few tumour cases. According to Table 1 and Fig. 1, pooled data for sensitivity and specicity according to sROCa revealed a sensitivity of 0972 0023 (SE), and a specicity of 0759 0028 for IMA.
2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Diagnostic value of serum Tg measurements in thyroid carcinoma 65
Table 1 Diagnostic value of serum thyroglobulin measurements during follow-up in differentiated thyroid carcinoma analysed according to summary receiver operator characteristic curve analysis. Patients with aspecic activity in the neck region at scintigraphy were omitted. No heterogeneity was observed in this analysis Time after diagnosis (months, median, range)
Tg method
N* series
N total patients
Tumour prevalence
Gold standard
Tg cut-off (g /l) (median, range)
Sensitivity SE 0926 0033 0928 0033 0972 0023 0839 0029 0801 0037 0778 0023 0869 0021 0877 0022 0961 0013 0925 0018 0909 0021
Specicity SE 0638 0041 0633 0042 0759 0028 0973 0005 0974 0005 0977 0005 0884 0010 0900 0010 0947 0007 0880 0013 0900 0012
Accuracy SE 0668 0033 0659 0034 0874 0020 0920 0008 0931 0008 0933 0007 0861 0009 0878 0010 0952 0006 0859 0012 0872 0012
(a) Patients without thyroid ablation, withdrawn from thyroxine RIA 6 617 039 9 (2 180) All 5 591 041 > SC IMA 6 776 019 All (> SC) (b) Patients with thyroid ablation, during thyroxine RIA 12 1474 014 60 (4 152) 7 1081 014 IMA 9 1613 023 (c) Patients with thyroid ablation, withdrawn from thyroxine RIA 16 1864 020 9 (4 72) 12 1510 020 IMA 12 1602 022 (d) Patients with thyroid ablation, after rhTSH IMA# 7 1148 024 6 988 024 130 (9 252) All > SC All (> SC) All > SC All (> SC) All > SC
4 (110) 5 (110) 4 (115) 6 (224) 5 (324) 2 (110) 3 (127) 3 (127) 3 (110) 1 (12) 1 (12)
*When an article contained multiple analyses all these subseries were registered separately. Prevalence: number of patients with active tumour / total number of patients. Methods used are radioiodine scintigraphy, other imaging techniques (X-ray, ultrasound, CT, MRI, PET), histology and follow-up. > SC, series with scintigraphy as the only gold standard excluded. Data of individual data series are available from the correspondence author on request. #Hangen et al., 1999 = RIA.
Fig. 1b shows that sensitivity dropped to 0710 when thyroid region activity at scintigraphy was considered malignant. When thyroid region activity was considered benign (Fig. 1c), specicity dropped to 0660. Patients with thyroid ablation, on thyroxine Twenty-one series from 18 articles were included in this group. Data are summarized in Table 1b and Fig. 1. The range for sensitivity was 01821000, for specicity 0786 100, when patients with unspecied thyroid region activity were excluded. In the study with the sensitivity of 0182 (Pacini et al., 2003), 27 metastases were only detected after a protocol with rhTSH. According to Table 1 and Fig. 1, pooled data for sensitivity and specicity according to sROCa revealed a sensitivity of 0778 0023 at a specicity of 0977 0005 for IMA. Fig. 1b shows that sensitivity dropped to 0533 when thyroid region activity at scintigraphy was considered malignant. When thyroid region activity was considered benign (Fig. 1c), specicity dropped slightly to 0959. However, IMA revealed signicant heterogeneity in this condition. In all IMA series, tumour presence was established by multiple methods.
2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Patients with thyroid ablation, withdrawn from thyroxine Twenty-eight patient series from 25 articles were included in this group. Data are summarized in Table 1c and Fig. 1. The range for sensitivity was 05201000, for specicity 0167100, when patients with unspecied thyroid region activity were excluded. The study with a sensitivity of 0520 had a relatively high Tg threshold (10 g/ l), and 12 of 25 tumours were missed (Ramanna et al., 1985). Specicity ranged from 0167 to 1000. The value of 0167 was found in a study (Dadparvar et al., 1995) with only 26 patients. According to Table 1 and Fig. 1, pooled data for sensitivity and specicity according to sROCa revealed a sensitivity of 0961 0013 at a specicity of 0947 0007 for IMA. Fig. 1b shows that sensitivity dropped to 0836 when thyroid region activity at scintigraphy was considered malignant. When thyroid region activity was considered benign (Fig. 1c), specicity dropped to 0895. In all IMA series, tumour presence was established by multiple methods. Patients with thyroid ablation and rhTSH stimulation Seven patient series from seven articles were included in this
66 C. F. A. Eustatia-Rutten et al.
group. Data are summarized in Table 1d and Fig. 1. The range for sensitivity was 0778 1000, for specicity 0619 1000, when patients with unspecied thyroid region activity were excluded. According to Table 1 and Fig. 1, pooled data for sensitivity and specicity according to sROCa revealed a sensitivity of 0925 0018 at a specicity of 0880 0013. Fig. 1b shows that sensitivity dropped to 0726 when thyroid region activity at scintigraphy was considered malignant. When thyroid region activity was considered benign (Fig. 1c), specicity dropped to 0841. Discussion The present meta-analysis was performed to assess whether thyroid remnant ablation and /or withdrawal from thyroxine are required to improve the accuracy of serum Tg measurements in the follow-up of patients with thyroid carcinoma. Although most patients are cured after initial therapy, they will usually have follow-up protocols over many years. Despite the universal application of Tg measurements, no consensus exists on the frequency of measurements, the threshold values, and whether Tg should be measured during thyroxine suppression therapy alone and /or during TSH stimulation. Several explanations for this lack of consensus exist. Analytical problems include the lack of universal standardization of the Tg assays, resulting in signicant interassay variability (Feldt-Rasmussen & Schlumberger, 1988; Spencer et al., 1996). The introduction of the Tg standard CRM 457 by the Community Bureau of Reference of the European Union in the 1990s is an important development. In addition, there may be a high intra-assay variability that results in a poor comparability of results obtained within one patient during follow-up. Hook effects may be present that affect IMA methods in particular, and can lead to inappropriately low- or normal-range Tg values in sera with very high Tg concentrations. Results of Tg measurements can be affected by Tg autoantibodies. The incidence of serum Tg antibodies in differentiated thyroid carcinoma is between 15 and 30% (Ericsson et al., 1985). False-positive Tg values due to antibody interference occur by many double-antibody RIA methods; however, falsenegative values may also occur (Ligabue et al., 1993). Recovery studies have shown an underestimation with most IMA methods (Ligabue et al., 1993; Spencer et al., 1998). The exclusion of articles in which Tg antibodies were not accounted for could have inuenced the results of our metaanalysis, as different assays for Tg antibody measurements could have led to different results. Nevertheless, we consider that to exclude studies that did not account for Tg antibodies is the best strategy for this meta-analysis. In our analyses, we have dealt with the differences in Tg methods in several ways. First, we separately analysed series using RIA and IMA. Our main conclusions are based on series
using IMA, but we have shown the RIA results to give a historical perspective. Second, we used the Tg cut-off values that were used in the original articles, assuming that these were based on the properties of the method as used in the original article. Third, series comparing on or off thyroxine were in a number of cases extracted from one article, using the same Tg method. In addition to analytical problems, determination of the diagnostic value of a test method requires a well-designed clinical protocol according to criteria such as those dened by the Cochrane foundation and the STARD group. Critical elements are the selection and denition of the study population, the denition of gold standards and the uniform conductance of reference tests. These criteria can be met best in prospectively designed protocols. One of the problems in retrospective series is the high possibility of selection bias and the nonuniform allocation of patients to reference tests. The selection bias in these articles is reected in the tumour prevalence, which was high in about half of the selected series. Because of the above-described limitations, the performance of a literature study on Tg in differentiated thyroid carcinoma is a complicated exercise. We therefore used strict selection criteria according to the most recent guidelines on diagnostic studies (Cochrane initiative and STARD group), resulting in the exclusion of 74 articles. We grouped the data according to phase of the disease, on or off thyroxine, Tg method and cut-offs, and reference standards, and analysed them using sROCa. We contend that the series on and off thyroxine therapy can be compared because of the patient characteristics, follow-up duration and Tg thresholds. Highest sensitivity was found for IMA-Tg in patients after thyroid remnant ablation and thyroid hormone withdrawal (0961 0013), at a specicity of 0947 0007. The sensitivity for Tg off thyroxine was in line with what was found in the recently published consensus report (Mazzaferri et al., 2003). Low IMATg specicities are found in patients who did not undergo remnant ablation (0759 0028, compared to 0947 0007 in those who did and are off thyroid hormone). This supports the rationale of performing thyroid remnant ablation after surgery for thyroid cancer. The sensitivity for IMA-Tg using rhTSH stimulation was slightly lower (0925 0018). However, the specicity of rhTSH stimulation was lower than after thyroid hormone withdrawal (0880 0013). An estimate of the clinical consequences of using various Tgtesting procedures in a series of 1000 patients, at a prior probability of cancer recurrence being present of 5%, is shown in Table 2. Tg-testing in ablated patients while on thyroxine will result in 11 missed cancers and 22 patients being treated without proven disease according to the reference standards. Withdrawal from thyroxine will reduce the number of missed cancers from 11 to two, at the price of 51 cases of treatment without proven disease. Using rhTSH results in a comparable number of missed
2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Diagnostic value of serum Tg measurements in thyroid carcinoma 67
Table 2 Positive (appropriate treatment of cancer recurrence) and negative (missing cancer recurrence, or subjecting a patient to unnecessary 131Itreatment) clinical consequences in 1000 patients of the use of various Tg-test protocols to guide retreatment with 131I, at a prior probability of recurrence of 005. Numbers of patients, and 95% condence intervals Appropriate treatment No ablation Ablation, on T4 Ablation, off T4 Ablation, rhTSH 49 (47 51) 39 (37 41) 48 (47 49) 46 (44 48) Missed recurrence 1 (03) 11 (912) 2 (13) 4 (26) Treatment without proven disease 229 (176282) 22 (1331) 51 (3765) 114 (89139)
cancers (four), although at the price of a greater number of patients being treated without proven disease. The suggestion that Tg measurements off thyroxine provide optimal diagnostic accuracy is the justication for accepting the disadvantages of thyroid hormone withdrawal. The recent introduction of rhTSH has offered new perspectives for Tg measurement. Although the number of rhTSH studies in our analyses is still limited, our analysis so far suggests that this method offers comparable sensitivity at lower specicity. Decreased test-related morbidity thus comes at the price of more false-positive treatments, increasing treatment costs and discomfort. However, a low specicity can be partly explained by the fact that scintigraphy as the only gold standard has a limited sensitivity for the detection of thyroid carcinoma metastases (19 45% in recent studies) (Mazzaferri & Kloos, 2002; Frasoldati et al., 2003). The consequence of the low sensitivity of scintigraphy as a reference standard is that patients with high Tg values but negative scintigraphy are considered false positives whereas they could very well have a tumour. This problem could contribute to the relative low specicity in the pooled studies on rhTSH: in Haugen et al. (1999), for instance, 32 patients with Tg concentrations above the threshold value after rhTSH had negative scintigraphies. In conclusion, many articles that have been published on the diagnostic value of serum Tg in thyroid carcinoma have methodological shortcomings. However, our analysis conrms that every patient who has undergone thyroid surgery and thyroid remnant ablation should undergo, at least once, Tg-testing while off thyroid hormone, which offers the highest accuracy and thus the most appropriate provision of 131I retreatment. Alternatively, especially in patients who suffer from signicant morbidity when withdrawn from thyroid hormone, rhTSH may be used for Tgtesting. If no indication for disease is present and Tg after stimulation is below the threshold, subsequent Tg measurements can be performed during thyroxine therapy. Tg threshold values should be dened individually within each clinic, based on the available Tg assay method.
References
Aiello, D.P. & Manni, A. (1990) Thyroglobulin measurement vs iodine 2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
131 total-body scan for follow-up of well-differentiated thyroid cancer. Archives of Internal Medicine, 150, 437439. Ain, K.B. (2000) Management of undifferentiated thyroid cancer. Baillieres Best Practice and Research. Clinical Endocrinology and Metabolism, 14, 615629. Almeida-Filho, P., Ravizzini, G.C., Almeida, C. & Borges-Neto, S. (2000) Whole-body Tc-99m sestamibi scintigraphy in the follow-up of differentiated thyroid carcinoma. Clinical Nuclear Medicine, 25, 443446. Alnasi, N.S., Driedger, A.A., Coates, G., Moote, D.J. & Raphael, S.J. (2000) FDG PET of recurrent or metastatic 131I-negative papillary thyroid carcinoma. Journal of Nuclear Medicine, 41, 1010 1015. Altenvoerde, G., Lerch, H., Kuwert, T., Matheja, P., Schafers, M. & Schober, O. (1998) Positron emission tomography with F-18deoxyglucose in patients with differentiated thyroid carcinoma, elevated thyroglobulin levels, and negative iodine scans. Langenbecks Archives of Surgery, 383, 160163. Alzahrani, A.S., Raef, H., Sultan, A., Al Sobhi, S., Ingemansson, S., Ahmed, M. & Al Mahfouz, A. (2002) Impact of cervical lymph node dissection on serum TG and the course of disease in TG-positive, radioactive iodine whole body scan-negative recurrent /persistent papillary thyroid cancer. Journal of Endocrinological Investigation, 25, 526531. Antonelli, A., Miccoli, P., Ferdeghini, M., Di Coscio, G., Alberti, B., Iacconi, P., Baldi, V ., Fallahi, P. & Baschieri, L. (1995) Role of neck ultrasonography in the follow-up of patients operated on for thyroid cancer. Thyroid, 5, 2528. Arslan, N., Ilgan, S., Serdengecti, M., Ozguven, M.A., Bayhan, H., Okuyucu, K. & Gulec, S.A. (2001) Post-surgical ablation of thyroid 131 remnants with high-dose I in patients with differentiated thyroid carcinoma. Nuclear Medicine Communications, 22, 1021 1027. Bachelot, A., Cailleux, A.F., Klain, M., Baudin, E., Ricard, M., Bellon, N., Caillou, B., Travagli, J.P. & Schlumberger, M. (2002) Relationship between tumor burden and serum thyroglobulin level in patients with papillary and follicular thyroid carcinoma. Thyroid, 12, 707 711. Baskin, H.J. (1994) Effect of postoperative 131I treatment on thyroglobulin measurements in the follow-up of patients with thyroid cancer. Thyroid, 4, 239242. Baudin, E., Do, C.C., Cailleux, A.F., Leboulleux, S., Travagli, J.P. & Schlumberger, M. (2003) Positive predictive value of serum thyroglobulin levels, measured during the rst year of follow-up after thyroid hormone withdrawal, in thyroid cancer patients. Journal of Clinical Endocrinology and Metabolism, 88, 11071111. Bednar, J., Nemec, J., Zamrazil, V ., Vana, S., Pohunkova, D. & Rohling, S. (1983) Serum thyroglobulin determinations in patients with differentiated thyroid carcinoma. Nuklearmedizin, 22, 204 211. Bejarano, P.A., Nikiforov, Y.E., Swenson, E.S. & Biddinger, P.W. (2000) Thyroid transcription factor-1, thyroglobulin, cytokeratin 7, and
68 C. F. A. Eustatia-Rutten et al.
cytokeratin 20 in thyroid neoplasms. Applied Immunohistochemistry and Molecular Morphology, 8, 189 194. Black, E.G. & Sheppard, M.C. (1991) Serum thyroglobulin measurements in thyroid cancer: evaluation of false positive results. Clinical Endocrinology (Oxford), 35, 519 520. Black, E.G., Sheppard, M.C. & Hoffenberg, R. (1987) Serial serum thyroglobulin measurements in the management of differentiated thyroid carcinoma. Clinical Endocrinology (Oxford), 27, 115 120. Blahd, W.H., Drickman, M.V ., Porter, C.W., Hill, V .A. & Baumgartner, W.A. (1984) Serum thyroglobulin, a monitor of differentiated thyroid carcinoma in patients receiving thyroid hormone suppression therapy: concise communication. Journal of Nuclear Medicine, 25, 673 676. Bohm, J., Kosma, V .M., Eskelinen, M., Hollmen, S., Niskanen, M., Tulla, H., Alhava, E. & Niskanen, L. (1999) Non-suppressed thyrotropin and elevated thyroglobulin are independent predictors of recurrence in differentiated thyroid carcinoma. European Journal of Endocrinology, 141, 460467. Bossuyt, P.M., Reitsma, J.B., Bruns, D.E., Gatsonis, C.A., Glasziou, P.P., Irwig, L.M., Lijmer, J.G., Moher, D., Rennie, D. & de Vet, H.C. (2003) Towards complete and accurate reporting of studies of diagnostic accuracy: the STARD initiative. The Standards for Reporting of Diagnostic Accuracy Group. Croatian Medical Journal, 44, 635 638. Brandt-Mainz, K., Muller, S.P., Sonnenschein, W. & Bockisch, A. (1998) Technetium-99m-furifosmin in the follow-up of differentiated thyroid carcinoma. Journal of Nuclear Medicine, 39, 1536 1541. Brendel, A.J., Lambert, B., Guyot, M., Jeandot, R., Dubourg, H., Roger, P., Wynchauk, S., Manciet, G. & Lefort, G. (1990) Low levels of serum thyroglobulin after withdrawal of thyroid suppression therapy in the follow up of differentiated thyroid carcinoma. European Journal of Nuclear Medicine, 16, 35 38. British Thyroid Association (2002) Guidelines for the Management of Differentiated Thyroid Cancer in Adults. http:// www.british-thyroidassociation.org/guidelines.htm. Cailleux, A.F., Baudin, E., Travagli, J.P., Ricard, M. & Schlumberger, M. (2000) Is diagnostic iodine-131 scanning useful after total thyroid ablation for differentiated thyroid cancer? Journal of Clinical Endocrinology and Metabolism, 85, 175 178. Carril, J.M., Quirce, R., Serrano, J., Banzo, I., Jimenez-Bonilla, J.F., Tabuenca, O. & Barquin, R.G. (1997) Total-body scintigraphy with thallium-201 and iodine-131 in the follow-up of differentiated thyroid cancer. Journal of Nuclear Medicine, 38, 686 692. Charles, M.A., Dodson, L.E. Jr, Waldeck, N., Hofeldt, F., Ghaed, N., Telepak, R., Ownbey, J. & Burstein, P. (1980) Serum thyroglobulin levels predict total body iodine scan ndings in patients with treated well-differentiated thyroid carcinoma. American Journal of Medicine, 69, 401407. Chung, J.K., So, Y., Lee, J.S., Choi, C.W., Lim, S.M., Lee, D.S., Hong, S.W., Youn, Y.K., Lee, M.C. & Cho, B.Y. (1999) Value of FDG PET in pap131 illary thyroid carcinoma with negative I whole-body scan. Journal of Nuclear Medicine, 40, 986 992. Dadparvar, S., Chevres, A., Tulchinsky, M., Krishna-Badrinath, L., Khan, A.S. & Slizofski, W.J. (1995) Clinical utility of technetium-99m methoxisobutylisonitrile imaging in differentiated thyroid carcinoma: comparison with thallium-201 and iodine-131 Na scintigraphy, and serum thyroglobulin quantitation. European Journal of Nuclear Medicine, 22, 13301338. Dadparvar, S., Krishna, L., Brady, L.W., Slizofski, W.J., Brown, S.J., Chevres, A. & Micaily, B. (1993) The role of iodine-131 and thallium-201 imaging and serum thyroglobulin in the management of differentiated thyroid carcinoma. Cancer, 71, 3767 3773. David, A., Blotta, A., Bondanelli, M., Rossi, R., Roti, E., Braverman, L.E.,
Busutti, L. & degli Uberti, E.C. (2001) Serum thyroglobulin concentrations and 131I whole-body scan results in patients with differentiated thyroid carcinoma after administration of recombinant human thyroidstimulating hormone. Journal of Nuclear Medicine, 42, 14701475. DeGroot, L.J., Kaplan, E.L., McCormick, M. & Straus, F.H. (1990) Natural history, treatment, and course of papillary thyroid carcinoma. Journal of Clinical Endocrinology and Metabolism, 71, 414424. Dietlein, M., Scheidhauer, K., Voth, E., Theissen, P. & Schicha, H. (1997) Fluorine-18 uorodeoxyglucose positron emission tomography and iodine-131 whole-body scintigraphy in the follow-up of differentiated thyroid cancer. European Journal of Nuclear Medicine, 24, 13421348. Dow, K.H., Ferrell, B.R. & Anello, C. (1997) Quality-of-life changes in patients with thyroid cancer after withdrawal of thyroid hormone therapy. Thyroid, 7, 613619. Eber, M., Abecassis, J., Grob, J.C., Ott, G. & Methlin, G. (1980) Immunoradiometric assay for human thyroglobulin and variations in thyroid pathology. Clinica Chimica Acta, 105, 5158. Echenique, R.L., Kasi, L., Haynie, T.P., Glenn, H.J., Samaan, N.A. & Hill, C.S. (1982) Critical evaluation of serum thyroglobulin levels and I-131 scans in post-therapy patients with differentiated thyroid carcinoma: concise communication. Journal of Nuclear Medicine, 23, 235240. Edmonds, C.J. & Willis, C.L. (1988) Serum thyroglobulin in the investigation of patients presenting with metastases. British Journal of Radiology, 61, 317319. Elgart, G.W., Patterson, J.W. & Taylor, R. (1991) Cutaneous metastasis from papillary carcinoma of the thyroid gland. Journal of the American Academy of Dermatology, 25, 404408. Ericsson, U.B., Christensen, S.B. & Thorell, J.I. (1985) A high prevalence of thyroglobulin autoantibodies in adults with and without thyroid disease as measured with a sensitive solid-phase immunosorbent radioassay. Clinical Immunology and Immunopathology, 37, 154 162. Feine, U., Lietzenmayer, R., Hanke, J.P., Held, J., Wohrle, H. & MullerSchauenburg, W. (1996) Fluorine-18-FDG and iodine-131-iodide uptake in thyroid cancer. Journal of Nuclear Medicine, 37, 1468 1472. Feldt-Rasmussen, U. & Schlumberger, M. (1988) European interlaboratory comparison of serum thyroglobulin measurement. Journal of Endocrinological Investigation, 11, 175181. Feldt-Rasmussen, U., Holten, I. & Hansen, H.S. (1983) Inuence of thyroid substitution therapy and thyroid autoantibodies on the value of serum thyroglobulin in recurring thyroid cancer. Cancer, 51, 22402244. Filesi, M., Signore, A., Ventroni, G., Melacrinis, F.F. & Ronga, G. (1998) Role of initial iodine-131 whole-body scan and serum thyroglobulin in differentiated thyroid carcinoma metastases. Journal of Nuclear Medicine, 39, 15421546. Franceschi, M., Kusic, Z., Franceschi, D., Lukinac, L. & Roncevic, S. (1996) Thyroglobulin determination, neck ultrasonography and iodine131 whole-body scintigraphy in differentiated thyroid carcinoma. Journal of Nuclear Medicine, 37, 446451. Frasoldati, A., Pesenti, M., Gallo, M., Caroggio, A., Salvo, D. & Valcavi, R. (2003) Diagnosis of neck recurrences in patients with differentiated thyroid carcinoma. Cancer, 97, 9096. Fridrich, L., Messa, C., Landoni, C., Lucignani, G., Moncayo, R., Kendler, D., Riccabona, G. & Fazio, F. (1997) Whole-body scintigraphy 131 with 99Tcm-MIBI, 18F-FDG and I in patients with metastatic thyroid carcinoma. Nuclear Medicine Communications, 18, 3 9. Frilling, A., Tecklenborg, K., Gorges, R., Weber, F., Clausen, M. & Broelsch, E.C. (2001) Preoperative diagnostic value of [(18)F] uorodeoxyglucose positron emission tomography in patients with radioiodine-negative recurrent well-differentiated thyroid carcinoma. Annals of Surgery, 234, 804811. 2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Diagnostic value of serum Tg measurements in thyroid carcinoma 69
Fugazzola, L., Mihalich, A., Persani, L., Cerutti, N., Reina, M., Bonomi, M., Ponti, E., Mannavola, D., Giammona, E., Vannucchi, G., di Blasio, A.M. & Beck-Peccoz, P. (2002) Highly sensitive serum thyroglobulin and circulating thyroglobulin mRNA evaluations in the management of patients with differentiated thyroid cancer in apparent remission. Journal of Clinical Endocrinology and Metabolism, 87, 32013208. Galligan, J.P., Winship, J., van Doorn, T. & Mortimer, R.H. (1982) A comparison of serum thyroglobulin measurements and whole body 131I scanning in the management of treated differentiated thyroid carcinoma. Australian and New Zealand Journal of Medicine, 12, 248254. Gallowitsch, H.J., Mikosch, P., Kresnik, E., Unterweger, O., Gomez, I. & Lind, P. (1998) Thyroglobulin and low-dose iodine-131 and technetium-99m-tetrofosmin whole-body scintigraphy in differentiated thyroid carcinoma. Journal of Nuclear Medicine, 39, 870 875. Garin, E., Devillers, A., Le Cloirec, J., Bernard, A.M., Lescouarch, J., Herry, J.Y., Reubi, J.C. & Bourguet, P. (1998) Use of indium-111 pentetreotide somatostatin receptor scintigraphy to detect recurrent thyroid carcinoma in patients without detectable iodine uptake. European Journal of Nuclear Medicine, 25, 687 694. Geus-Oei, L.F., Oei, H.Y., Hennemann, G. & Krenning, E.P. (2002) 123 I whole-body scan and thyroglobulin in the Sensitivity of detection of metastases or recurrent differentiated thyroid cancer. European Journal of Nuclear Medicine and Molecular Imaging, 29, 768774. Giammarile, F., Hafdi, Z., Bournaud, C., Janier, M., Houzard, C., Desuzinges, C., Itti, R., Sassolas, G. & Borson-Chazot, F. (2003) Is [18F]2-uoro-2-deoxy-d-glucose (FDG) scintigraphy with non-dedicated positron emission tomography useful in the diagnostic management of suspected metastatic thyroid carcinoma in patients with no detectable radioiodine uptake? European Journal of Endocrinology, 149, 293300. Gilliland, F.D., Hunt, W.C., Morris, D.M. & Key, C.R. (1997) Prognostic factors for thyroid carcinoma. A population-based study of 15 698 cases from the Surveillance, Epidemiology and End Results (SEER) program 19731991. Cancer, 79, 564 573. Girelli, M.E., Busnardo, B., Amerio, R., Casara, D., Betterle, C. & Piccolo, M. (1986) Critical evaluation of serum thyroglobulin (Tg) levels during thyroid hormone suppression therapy versus Tg levels after hormone withdrawal and total body scan: results in 291 patients with thyroid cancer. European Journal of Nuclear Medicine, 11, 333 335. Girelli, M.E., Busnardo, B., Amerio, R., Scotton, G., Casara, D., Betterle, C., Piccolo, M. & Pelizzo, M.R. (1985) Serum thyroglobulin levels in patients with well-differentiated thyroid cancer during suppression therapy: study on 429 patients. European Journal of Nuclear Medicine, 10, 252254. Gorges, R., Kahaly, G., Muller-Brand, J., Macke, H., Roser, H.W. & Bockisch, A. (2001) Radionuclide-labeled somatostatin analogues for diagnostic and therapeutic purposes in nonmedullary thyroid cancer. Thyroid, 11, 647 659. Grant, S., Luttrell, B., Reeve, T., Wiseman, J., Wilmshurst, E., Stiel, J., Donohoe, D., Cooper, R. & Bridgman, M. (1984) Thyroglobulin may be undetectable in the serum of patients with metastatic disease secondary to differentiated thyroid carcinoma. Follow-up of differentiated thyroid carcinoma. Cancer, 54, 1625 1628. Grunwald, F., Menzel, C., Bender, H., Palmedo, H., Willkomm, P., Ruhlmann, J., Franckson, T. & Biersack, H.J. (1997) Comparison of 18FDG-PET with 131iodine and 99mTc-sestamibi scintigraphy in differentiated thyroid cancer. Thyroid, 7, 327 335. Grunwald, F., Kalicke, T., Feine, U., Lietzenmayer, R., Scheidhauer, K., Dietlein, M., Schober, O., Lerch, H., Brandt-Mainz, K., Burchert, W., Hiltermann, G., Cremerius, U. & Biersack, H.J. (1999) Fluorine-18 uorodeoxyglucose positron emission tomography in thyroid cancer: 2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
results of a multicentre study. European Journal of Nuclear Medicine, 26, 15471552. Hall, F.T., Beasley, N.J., Eski, S.J., Witterick, I.J., Walsh, P.G. & Freeman, J.L. (2003) Predictive value of serum thyroglobulin after surgery for thyroid carcinoma. The Laryngoscope, 113, 77 81. Hannequin, P., Liehn, J.C., Delisle, M.J., Deltour, G. & Valeyre, J. (1987) ROC analysis in radioimmunoassay: an application to the interpretation of thyroglobulin measurement in the follow-up of thyroid carcinoma. European Journal of Nuclear Medicine, 13, 203206. Harvey, R.D., Matheson, N.A., Grabowski, P.S. & Rodger, A.B. (1990) Measurement of serum thyroglobulin is of value in detecting tumour recurrence following treatment of differentiated thyroid carcinoma by lobectomy. British Journal of Surgery, 77, 324326. Haugen, B.R., Pacini, F., Reiners, C., Schlumberger, M., Ladenson, P.W., Sherman, S.I., Cooper, D.S., Graham, K.E., Braverman, L.E., Skarulis, M.C., Davies, T.F., DeGroot, L.J., Mazzaferri, E.L., Daniels, G.H., Ross, D.S., Luster, M., Samuels, M.H., Becker, D.V ., Maxon, H.R. III, Cavalieri, R.R., Spencer, C.A., McEllin, K., Weintraub, B.D. & Ridgway, E.C. (1999) A comparison of recombinant human thyrotropin and thyroid hormone withdrawal for the detection of thyroid remnant or cancer. Journal of Clinical Endocrinology and Metabolism, 84, 38773885. Helal, B.O., Merlet, P., Toubert, M.E., Franc, B., Schvartz, C., GauthierKoelesnikov, H., Prigent, A. & Syrota, A. (2001) Clinical impact of (18)F-FDG PET in thyroid carcinoma patients with elevated 131 thyroglobulin levels and negative I scanning results after therapy. Journal of Nuclear Medicine, 42, 14641469. Hsu, C.H., Liu, F.Y., Yen, R.F. & Kao, C.H. (2003) Tc-99m MIBI SPECT in detecting metastatic papillary thyroid carcinoma in patients with elevated human serum thyroglobulin levels but negative I-131 whole body scan. Endocrine Research, 29, 915. Hufner, M., Stumpf, H.P., Grussendorf, M., Hermann, H.J. & Kimmig, B. (1983) A comparison of the effectiveness of 131I whole body scans and plasma Tg determinations in the diagnosis of metastatic differentiated carcinoma of the thyroid: a retrospective study. Acta Endocrinologica (Copenhagen), 104, 327332. Hundahl, S.A., Fleming, I.D., Fremgen, A.M. & Menck, H.R. (1998) A National Cancer Data Base report on 53,856 cases of thyroid carcinoma treated in the U.S., 19851995. Cancer, 83, 2638 2648. Jadvar, H., McDougall, I.R. & Segall, G.M. (1998) Evaluation of suspected recurrent papillary thyroid carcinoma with [18F]uorodeoxyglucose positron emission tomography. Nuclear Medicine Communications, 19, 547554. de Keizer, B., Koppeschaar, H.P., Zelissen, P.M., Lips, C.J., van Rijk, P.P., van Dijk, A. & de Klerk, J.M. (2001) Efcacy of high therapeutic doses of iodine-131 in patients with differentiated thyroid cancer and detectable serum thyroglobulin. European Journal of Nuclear Medicine, 28, 198202. de Klerk, J.M., de Keizer, B., Zelissen, P.M., Lips, C.M. & Koppeschaar, H.P. (2000) Fixed dosage of 131I for remnant ablation in patients with differentiated thyroid carcinoma without pre-ablative diagnostic 131I scintigraphy. Nuclear Medicine Communications, 21, 529 532. Ladenson, P.W. (2000) Recombinant thyrotropin versus thyroid hormone withdrawal in evaluating patients with thyroid carcinoma. Seminars on Nuclear Medicine, 30, 98106. Ladenson, P.W., Braverman, L.E., Mazzaferri, E.L., Brucker-Davis, F., Cooper, D.S., Garber, J.R., Wondisford, F.E., Davies, T.F., DeGroot, L.J., Daniels, G.H., Ross, D.S. & Weintraub, B.D. (1997) Comparison of administration of recombinant human thyrotropin with withdrawal of thyroid hormone for radioactive iodine scanning in patients with thyroid carcinoma. New England Journal of Medicine, 337, 888896.
70 C. F. A. Eustatia-Rutten et al.
Ligabue, A., Poggioli, M.C. & Zacchini, A. (1993) Interference of specic autoantibodies in the assessment of serum thyroglobulin. The Journal of Nuclear Biology and Medicine, 37, 273 279. Lin, K.D., Lin, J.D., Huang, M.J., Huang, H.S., Jeng, L.B., Chao, T.C. & Ho, Y.S. (1997) Clinical presentations and predictive variables of thyroid microcarcinoma with distant metastasis. International Surgery, 82, 378381. Lin, J.D., Kao, P.F., Weng, H.F., Lu, W.T. & Huang, M.J. (1998) Relative value of thallium-201 and iodine-131 scans in the detection of recurrence or distant metastasis of well differentiated thyroid carcinoma. European Journal of Nuclear Medicine, 25, 695 700. Lin, J.D., Hsieh, S.H., Chang, H.Y., Huang, C.C. & Chao, T.C. (2001) Outcome after treatment for papillary thyroid cancer. Head and Neck, 23, 140146. Lindegaard, M.W., Paus, E., Hoie, J., Kullman, G. & Stenwig, A.E. (1988) Thyroglobulin radioimmunoassay and 131I scintigraphy in patients with differentiated thyroid carcinoma. Acta Chirurgica Scandinavica, 154, 141145. Littenberg, B. & Moses, L.E. (1993) Estimating diagnostic accuracy from multiple conicting reports: a new meta-analytic method. Medical Decision Making, 13, 313 321. Lorberboym, M., Murthy, S., Mechanick, J.I., Bergman, D., Morris, J.C. & Kim, C.K. (1996) Thallium-201 and iodine-131 scintigraphy in differentiated thyroid carcinoma. Journal of Nuclear Medicine, 37, 14871491. Lubin, E., Mechlis-Frish, S., Zatz, S., Shimoni, A., Segal, K., Avraham, A., Levy, R. & Feinmesser, R. (1994) Serum thyroglobulin and iodine131 whole-body scan in the diagnosis and assessment of treatment for metastatic differentiated thyroid carcinoma. Journal of Nuclear Medicine, 35, 257262. Lukinac, L., Franceschi, M., Nothig-Hus, D., Lechpammer, S., Tomasic, J., Vranesic, B., Pape, E. & Kusic, Z. (1996) Endogenously labeled 131 thyroid hormones ( I-T3 / T4) in sera of patients with differentiated thyroid carcinoma. Thyroid, 6, 201 206. Mazzaferri, E.L. & Kloos, R.T. (2001) Clinical review 128: current approaches to primary therapy for papillary and follicular thyroid cancer. Journal of Clinical Endocrinology and Metabolism, 86, 1447 1463. Mazzaferri, E.L. & Kloos, R.T. (2002) Is diagnostic iodine-131 scanning with recombinant human TSH useful in the follow-up of differentiated thyroid cancer after thyroid ablation? Journal of Clinical Endocrinology and Metabolism, 87, 1490 1498. Mazzaferri, E.L., Robbins, R.J., Spencer, C.A., Braverman, L.E., Pacini, F., Wartofsky, L., Haugen, B.R., Sherman, S.I., Cooper, D.S., Braunstein, G.D., Lee, S., Davies, T.F., Arafah, B.M., Ladenson, P.W. & Pinchera, A. (2003) A consensus report of the role of serum thyroglobulin as a monitoring method for low-risk patients with papillary thyroid carcinoma. Journal of Clinical Endocrinology and Metabolism, 88, 1433 1441. Meier, C.A., Braverman, L.E., Ebner, S.A., Veronikis, I., Daniels, G.H., Ross, D.S., Deraska, D.J., Davies, T.F., Valentine, M. & DeGroot, L.J.& (1994) Diagnostic use of recombinant human thyrotropin in patients with thyroid carcinoma (phase I / II study). Journal of Clinical Endocrinology and Metabolism, 78, 188 196. Michal, M., Skalova, A., Simpson, R.H., Raslan, W.F., Curik, R., Leivo, I. & Mukensnabl, P. (1999) Cribriform adenocarcinoma of the tongue: a hitherto unrecognized type of adenocarcinoma characteristically occurring in the tongue. Histopathology, 35, 495 501. Mikosch, P., Gallowitsch, H.J., Kresnik, E., Unterweger, O., Gomez, I. & Lind, P. (1999) Comparison of two thyroglobulin immunoradiometric assays on the basis of comprehensive imaging in differentiated thyroid carcinoma. Thyroid, 9, 933 941. Moses, L.E., Shapiro, D. & Littenberg, B. (1993) Combining independent studies of a diagnostic test into a summary ROC curve: data-analytic
approaches and some additional considerations. Statistical Medicine, 12, 12931316. Muller-Gartner, H.W. & Schneider, C. (1988) Clinical evaluation of tumor characteristics predisposing serum thyroglobulin to be undetectable in patients with differentiated thyroid cancer. Cancer, 61, 976 981. Ng, D.C., Sundram, F.X. & Sin, A.E. (2000) 99mTc-sestamibi and 131I whole-body scintigraphy and initial serum thyroglobulin in the management of differentiated thyroid carcinoma. Journal of Nuclear Medicine, 41, 631635. Ng Tang Fui, S.C., Hoffenberg, R., Maisey, M.N. & Black, E.G. (1979) Serum thyroglobulin concentrations and whole-body radioiodine scan in follow-up of differentiated thyroid cancer after thyroid ablation. British Medical Journal, 2, 298300. Oyen, W.J., Verhagen, C., Saris, E., van den Broek, W.J., Pieters, G.F. & Corsten, F.H. (2000) Follow-up regimen of differentiated thyroid carcinoma in thyroidectomized patients after thyroid hormone withdrawal. Journal of Nuclear Medicine, 41, 643646. Pacini, F., Pinchera, A., Giani, C., Grasso, L. & Baschieri, L. (1980) 131 Serum thyroglobulin concentrations and I whole body scans in the diagnosis of metastases from differentiated thyroid carcinoma (after thyroidectomy). Clinical Endocrinology (Oxford), 13, 107110. Pacini, F., Lari, R., Mazzeo, S., Grasso, L., Taddei, D. & Pinchera, A. (1985) Diagnostic value of a single serum thyroglobulin determination on and off thyroid suppressive therapy in the follow-up of patients with differentiated thyroid cancer. Clinical Endocrinology (Oxford), 23, 405 411. Pacini, F., Molinaro, E., Lippi, F., Castagna, M.G., Agate, L., Ceccarelli, C., Taddei, D., Elisei, R., Capezzone, M. & Pinchera, A. (2001) Prediction of disease status by recombinant human TSH-stimulated serum Tg in the postsurgical follow-up of differentiated thyroid carcinoma. Journal of Clinical Endocrinology and Metabolism, 86, 56865690. Pacini, F., Molinaro, E., Castagna, M.G., Agate, L., Elisei, R., Ceccarelli, C., Lippi, F., Taddei, D., Grasso, L. & Pinchera, A. (2003) Recombinant human thyrotropin-stimulated serum thyroglobulin combined with neck ultrasonography has the highest sensitivity in monitoring differentiated thyroid carcinoma. Journal of Clinical Endocrinology and Metabolism, 88, 36683673. Pellegriti, G., Scollo, C., Regalbuto, C., Attard, M., Marozzi, P., Vermiglio, F., Violi, M.A., Cianci, M., Vigneri, R., Pezzino, V . & Squatrito, S. (2003) The diagnostic use of the rhTSH /thyroglobulin test in differentiated thyroid cancer patients with persistent disease and low thyroglobulin levels. Clinical Endocrinology (Oxford), 58, 556561. Pineda, J.D., Lee, T., Ain, K., Reynolds, J.C. & Robbins, J. (1995) Iodine131 therapy for thyroid cancer patients with elevated thyroglobulin and negative diagnostic scan. Journal of Clinical Endocrinology and Metabolism, 80, 14881492. Ramanna, L., Waxman, A.D., Brachman, M.B., Sensel, N., Tanasescu, D.E., Berman, D.S., Catz, B. & Braunstein, G.D. (1985) Correlation of thyroglobulin measurements and radioiodine scans in the follow-up of patients with differentiated thyroid cancer. Cancer, 55, 1525 1529. Ramanna, L., Waxman, A. & Braunstein, G. (1991) Thallium-201 scintigraphy in differentiated thyroid cancer: comparison with radioiodine scintigraphy and serum thyroglobulin determinations. Journal of Nuclear Medicine, 32, 441446. Robbins, R.J., Tuttle, R.M., Sharaf, R.N., Larson, S.M., Robbins, H.K., Ghossein, R.A., Smith, A. & Drucker, W.D. (2001) Preparation by recombinant human thyrotropin or thyroid hormone withdrawal are comparable for the detection of residual differentiated thyroid carcinoma. Journal of Clinical Endocrinology and Metabolism, 86, 619625. Robbins, R.J., Chon, J.T., Fleisher, M., Larson, S.M. & Tuttle, R.M. (2002) Is the serum thyroglobulin response to recombinant human 2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Diagnostic value of serum Tg measurements in thyroid carcinoma 71
thyrotropin sufcient, by itself, to monitor for residual thyroid carcinoma? Journal of Clinical Endocrinology and Metabolism, 87, 32423247. Roelants, V ., Nayer, P.D., Bouckaert, A. & Beckers, C. (1997) The predictive value of serum thyroglobulin in the follow-up of differentiated thyroid cancer. European Journal of Nuclear Medicine, 24, 722727. Ronga, G., Fiorentino, A., Paserio, E., Signore, A., Todino, V ., Tummarello, M.A., Filesi, M. & Baschieri, I. (1990) Can iodine-131 whole-body scan be replaced by thyroglobulin measurement in the post-surgical follow-up of differentiated thyroid carcinoma? Journal of Nuclear Medicine, 31, 1766 1771. Ronga, G., Filesi, M., Ventroni, G., Vestri, A.R. & Signore, A. (1999) Value of the rst serum thyroglobulin level after total thyroidectomy for the diagnosis of metastases from differentiated thyroid carcinoma. European Journal of Nuclear Medicine, 26, 1448 1452. Rubello, D., Girelli, M.E., Casara, D., Piccolo, M., Perin, A. & Busnardo, B. (1990) Usefulness of the combined antithyroglobulin antibodies and thyroglobulin assay in the follow-up of patients with differentiated thyroid cancer. Journal of Endocrinological Investigation, 13, 737742. Rubello, D., Mazzarotto, R. & Casara, D. (2000) The role of technetium99m methoxyisobutylisonitrile scintigraphy in the planning of therapy and follow-up of patients with differentiated thyroid carcinoma after surgery. European Journal of Nuclear Medicine, 27, 431 440. Ruiz-Garcia, J., Ruiz de Almodovar, J.M., Olea, N. & Pedraza, V . (1991) Thyroglobulin level as a predictive factor of tumoral recurrence in differentiated thyroid cancer. Journal of Nuclear Medicine, 32, 395398. Ruter, A., Smeds, S. & Lennquist, S. (1998) Value of serum thyroglobulin measurement in patients operating on for well differentiated thyroid carcinoma. European Journal of Surgery, 164, 665 671. Samaan, N.A., Schultz, P.N., Hickey, R.C., Goepfert, H., Haynie, T.P., Johnston, D.A. & Ordonez, N.G. (1992) The results of various modalities of treatment of well differentiated thyroid carcinomas: a retrospective review of 1599 patients. Journal of Clinical Endocrinology and Metabolism, 75, 714 720. Schirrmeister, H., Buck, A., Guhlmann, A. & Reske, S.N. (2001) Anatomical distribution and sclerotic activity of bone metastases from thyroid cancer assessed with F-18 sodium uoride positron emission tomography. Thyroid, 11, 677 683. Schlumberger, M.J. (1998) Papillary and follicular thyroid carcinoma. New England Journal of Medicine, 338, 297 306. Schlumberger, M., Travagli, J.P., Fragu, P., Gardet, P., Lumbroso, J. & Parmentier, C. (1988) Follow-up of patients with differentiated thyroid carcinoma. Experience at Institut Gustave-Roussy, Villejuif. European Journal of Cancer and Clinical Oncology, 24, 345 350. Schlumberger, M., Fragu, P., Gardet, P., Lumbroso, J., Violot, D. & Parmentier, C. (1991) A new immunoradiometric assay (IRMA) system for thyroglobulin measurement in the follow-up of thyroid cancer patients. European Journal of Nuclear Medicine, 18, 153 157. 131 Schlumberger, M., Mancusi, F., Baudin, E. & Pacini, F. (1997) I therapy for elevated thyroglobulin levels. Thyroid, 7, 273 276. Seabold, J.E., Gurll, N., Schurrer, M.E., Aktay, R. & Kirchner, P.T. (1999) Comparison of 99mTc-methoxyisobutyl isonitrile and 201Tl scintigraphy for detection of residual thyroid cancer after 131I ablative therapy. Journal of Nuclear Medicine, 40, 1434 1440. Shah, D.H., Dandekar, S.R., Jeevanram, R.K., Kumar, A., Sharma, S.M. & Ganatra, R.D. (1981) Serum thyroglobulin differentiated thyroid carcinoma: histological and metastatic classication. Acta Endocrinologica (Copenhagen), 98, 222 226. Shlossberg, A.H., Jacobson, J.C. & Ibbertson, H.K. (1979) Serum thyroglobulin in the diagnosis and management of thyroid carcinoma. Clinical Endocrinology (Oxford), 10, 17 27. Siddiqi, A., Foley, R.R., Britton, K.E., Sibtain, A., Plowman, P.N., 2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Grossman, A.B., Monson, J.P. & Besser, G.M. (2001) The role of 123Idiagnostic imaging in the follow-up of patients with differentiated thyroid carcinoma as compared to 131I-scanning: avoidance of negative therapeutic uptake due to stunning. Clinical Endocrinology (Oxford), 55, 515 521. Singer, P.A., Cooper, D.S., Daniels, G.H., Ladenson, P.W., Greenspan, F.S., Levy, E.G., Braverman, L.E., Clark, O.H., McDougall, I.R., Ain, K.V . & Dorfman, S.G. (1996) Treatment guidelines for patients with thyroid nodules and well-differentiated thyroid cancer. American Thyroid Association. Archives of Internal Medicine, 156, 21652172. Sisson, J.C., Thompson, N.W., Giordano, T.J., England, B.G. & Normolle, D.P. (2000) Serum thyroglobulin levels after thyroxine withdrawal in patients with low risk papillary thyroid carcinoma. Thyroid, 10, 165 169. van Sorge-van Boxtel, R.A., Eck-Smit, B.L. & Goslings, B.M. (1993) Comparison of serum thyroglobulin, 131I and 201Tl scintigraphy in the postoperative follow-up of differentiated thyroid cancer. Nuclear Medicine Communications, 14, 365372. Spencer, C.A., Takeuchi, M. & Kazarosyan, M. (1996) Current status and performance goals for serum thyroglobulin assays. Clinical Chemistry, 42, 164173. Spencer, C.A., Takeuchi, M., Kazarosyan, M., Wang, C.C., Guttler, R.B., Singer, P.A., Fatemi, S., LoPresti, J.S. & Nicoloff, J.T. (1998) Serum thyroglobulin autoantibodies: prevalence, inuence on serum thyroglobulin measurement, and prognostic signicance in patients with differentiated thyroid carcinoma. Journal of Clinical Endocrinology and Metabolism, 83, 11211127. Steyerberg, E.W., Kievit, J., de Mol Van Otterloo, J.C., van Bockel, J.H., Eijkemans, M.J. & Habbema, J.D. (1995) Perioperative mortality of elective abdominal aortic aneurysm surgery. A clinical prediction rule based on literature and individual patient data. Archives of Internal Medicine, 155, 19982004. Sulman, C., Gosselin, P., Carpentier, P. & Lemaire, B. (1984) Value of the estimation of thyroglobulin levels in the surveillance of treated differentiated thyroid carcinoma. Journal of Clinical Chemistry and Clinical Biochemistry, 22, 215218. Taylor, T., Specker, B., Robbins, J., Sperling, M., Ho, M., Ain, K., Bigos, S.T., Brierley, J., Cooper, D., Haugen, B., Hay, I., Hertzberg, V ., Klein, I., Klein, H., Ladenson, P., Nishiyama, R., Ross, D., Sherman, S. & Maxon, H.R. (1998) Outcome after treatment of high-risk papillary and non-Hurthle-cell follicular thyroid carcinoma. Annals of Internal Medicine, 129, 622627. Tenenbaum, F., Schlumberger, M., Bonnin, F., Lumbroso, J., Aubert, B., Benali, H. & Parmentier, C. (1993) Usefulness of technetium-99m hydroxymethylene diphosphonate scans in localizing bone metastases of differentiated thyroid carcinoma. European Journal of Nuclear Medicine, 20, 11681174. van Tol, K.M., Jager, P.L., de Vries, E.G., Piers, D.A., Boezen, H.M., Sluiter, W.J., Dullaart, R.P. & Links, T.P. (2003) Outcome in patients with differentiated thyroid cancer with negative diagnostic whole-body scanning and detectable stimulated thyroglobulin. European Journal of Endocrinology, 148, 589 596. Torlontano, M., Crocetti, U., DAloiso, L., Bontto, N., Di Giorgio, A., Modoni, S., Valle, G., Frusciante, V., Bisceglia, M., Filetti, S., 131 Schlumberger, M. & Trischitta, V . (2003) Serum thyroglobulin and I whole body scan after recombinant human TSH stimulation in the follow-up of low-risk patients with differentiated thyroid cancer. European Journal of Endocrinology, 148, 1924. Tubiana, M., Schlumberger, M., Rougier, P., Laplanche, A., Benhamou, E., Gardet, P., Caillou, B., Travagli, J.P. & Parmentier, C. (1985) Long-term results and prognostic factors in patients with differentiated thyroid carcinoma. Cancer, 55, 794804. Valimaki, M. & Lamberg, B.A. (1985) How to deal with undetectable
72 C. F. A. Eustatia-Rutten et al.
and low measurable serum thyroglobulin levels in the follow-up of patients with differentiated thyroid carcinoma? Acta Endocrinologica (Copenhagen), 110, 487 492. Valli, N., Catargi, B., Ronci, N., Leccia, F., Guyot, M., Roger, P., Ducassou, D. & Tabarin, A. (1999) Evaluation of indium-111 pentetreotide somatostatin receptor scintigraphy to detect recurrent thyroid carcinoma in patients with negative radioiodine scintigraphy. Thyroid, 9, 583589.
Vitale, G., Arianna, L.G., Antonio, C., Francesco, F., Michele, K., Giovanni, S., Marco, S. & Giovanni, L. (2002) The use of recombinant human TSH in the follow-up of differentiated thyroid cancer: experience from a large patient cohort in a single centre. Clinical Endocrinology (Oxford), 56, 247252. Wartofsky, L. (2002) Management of low-risk well-differentiated thyroid cancer based only on thyroglobulin measurement after recombinant human thyrotropin. Thyroid, 12, 583590.
Appendix 1 Articles excluded
Reasons for exclusion Not all patients had total thyroidectomy or information missing Not all patients had radioiodine ablation or information missing References Tubiana et al., 1985; Harvey et al., 1990; Schlumberger et al., 1991; Jadvar et al., 1998 Shlossberg et al., 1979; Shah et al., 1981; Echenique et al., 1982; Tubiana et al., 1985; Black et al., 1987; Schlumberger et al., 1988; Brendel et al., 1990; Black & Sheppard, 1991; Ruiz-Garcia et al., 1991; Dadparvar et al., 1993; Ladenson et al., 1997; Ruter et al., 1998; Ladenson, 2000; Ng et al., 2000; Sisson et al., 2000; Vitale et al., 2002 Dadparvar et al., 1993; Bejarano et al., 2000; Ladenson, 2000 Ng Tang Fui et al., 1979; Eber et al., 1980; Bednar et al., 1983; Schlumberger et al., 1988; Rubello et al., 1990; Grunwald et al., 1997; Ladenson et al., 1997; Roelants et al., 1997; Lin et al., 1998; Almeida-Filho et al., 2000; Fugazzola et al., 2002 Bednar et al., 1983; Feldt-Rasmussen et al., 1983; Edmonds & Willis, 1988; Schlumberger et al., 1991; Meier et al., 1994; Feine et al., 1996; Roelants et al., 1997; Ruter et al., 1998; Grunwald et al., 1999; Seabold et al., 1999; de Klerk et al., 2000; Ng et al., 2000; Rubello et al., 2000; Gorges et al., 2001 Echenique et al., 1982 Tubiana et al., 1985; Lorberboym et al., 1996; Grunwald et al., 1997 Robbins et al., 2001; Schirrmeister et al., 2001; Bachelot et al., 2002; Frasoldati et al., 2003; Lin et al., 1998; Wartofsky, 2002 Pineda et al., 1995; Fridrich et al., 1997; Altenvoerde et al., 1998; Brandt-Mainz et al., 1998; Gallowitsch et al., 1998; Garin et al., 1998; Valli et al., 1999; Ain, 2000; Alnasi et al., 2000; Rubello et al., 2000; Frilling et al., 2001; Helal et al., 2001; Siddiqi et al., 2001; Alzahrani et al., 2002; Vitale et al., 2002; Baudin et al., 2003; Giammarile et al., 2003; Hsu et al., 2003; Pellegriti et al., 2003; van Tol et al., 2003 Pineda et al. 1995; Chung et al., 1999; Seabold et al., 1999 Grunwald et al., 1999; Gorges et al., 2001 Grant et al., 1984; Edmonds & Willis, 1988; Schlumberger et al., 1988; Brendel et al., 1990; Ramanna et al., 1991; Carril et al., 1997; Lin et al., 1998; Almeida-Filho et al., 2000; de Klerk et al., 2000; David et al., 2001; Lin et al., 2001; Fugazzola et al., 2002; Hall et al., 2003
Tg cut-off values not indicated Criteria for tumour missing
Patients with Tg antibodies not excluded or information missing
Adequate TSH levels not indicated Phase in follow-up not indicated clearly Patient selection according to tumour localization Patient selection according to Tg levels
Patient selection according to radioiodine scintigraphy results Tg assay method not indicated Not enough data to perform meta-analyses of Tg sensitivity and specicity
2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Diagnostic value of serum Tg measurements in thyroid carcinoma 73
Articles included
Follow-up stage No ablation No ablation TSH status On thyroxine Off thyroxine References Pacini et al., 1985; Valimaki & Lamberg, 1985; Ronga et al., 1990 Hufner et al., 1983; Pacini et al., 1985; Valimaki & Lamberg, 1985; Lindegaard et al., 1988; Ronga et al., 1990; Tenenbaum et al., 1993; Dadparvar et al., 1995; Filesi et al., 1998; Ronga et al., 1999; Cailleux et al., 2000 Charles et al., 1980; Hufner et al., 1983; Blahd et al., 1984; Sulman et al., 1984; Girelli et al., 1985; Valimaki & Lamberg, 1985; Girelli et al., 1986; Hannequin et al., 1987; Baskin, 1994; Lubin et al., 1994; Franceschi et al., 1996; Dietlein et al., 1997; Bohm et al., 1999; Haugen et al., 1999; Mikosch et al., 1999; David et al., 2001; Geus-Oei et al., 2002; Pacini et al., 2003 Pacini et al., 1980; Galligan et al., 1982; Hufner et al., 1983; Blahd et al., 1984; Valimaki & Lamberg, 1985; Girelli et al., 1986; Hannequin et al. 1987; Muller-Gartner & Schneider, 1988; Aiello & Manni, 1990; van Sorge-van Boxtel RA et al., 1993; Antonelli et al., 1995; Dadparvar et al., 1995; Franceschi et al., 1996; Dietlein et al., 1997; Lin et al., 1997; Gallowitsch et al., 1998; Haugen et al., 1999; Mikosch et al., 1999; Cailleux et al., 2000; Oyen et al., 2000; Arslan et al., 2001; David et al., 2001; de Keizer et al., 2001; Geus-Oei et al., 2002 Haugen et al., 1999; David et al., 2001; Pacini et al., 2001; Mazzaferri & Kloos, 2002; Robbins et al., 2002; Pacini et al., 2003; Torlontano et al., 2003
Ablation
On thyroxine
Ablation
Off thyroxine
Ablation
rhTSH
2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
74 C. F. A. Eustatia-Rutten et al.
Appendix 2 Statistical methods A meta-analysis of sensitivity, specicity and positive predictive value of Tg measurements was performed by pooling all data from all data series, discriminating between the phase of the study (postsurgical or postablative), whether or not thyroxine treatment was withdrawn or rhTSH was given, Tg assay method and reference standards (scintigraphy only or more methods as well). All original 2 2 tables were imported in a predesigned spreadsheet, and were combined using a three-step method from simple counts, and MantelHaenszel calculations to summary receiver operating characteristic analysis (sROCa). First, the respective four cells (TP, FP, FN, FP) of the original 2 2 tables were combined by simple addition, using positive and negative test results analysed as determinants for the presence or absence of thyroid cancer. Aggregated estimates of the positive and negative likelihood ratio (LR) were calculated by straight counts, providing LRposcount and LRnegcount. Second, a MantelHaenszel odds ratio (ORMH) was calculated using traditional methods. From these, Mantel Haenszel estimates of likelihood ratios, were obtained using earlier published formulas (Steyerberg et al., 1995): LRposMH = exp{ln(ORMH )/[1 ln(LRnegcount )/ln(LRposcount )]} and LRnegMH = exp{ln(ORMH)/[(LRposcount )/ln(LRnegcount) 1]}. These likelihoods were then recalculated into MantelHaenszel estimates of sensitivity (SeMH) and specicity (SpMH) according to: SeMH = LRposMH(1 LRnegMH)/(LRposMH LRnegMH ) and SpMH = (LRposMH 1)/(LRposMH LRnegMH)
Third, sROCa was used to obtain best estimates of combined sensitivity and specicity (Littenberg & Moses, 1993; Moses et al., 1993). To this end estimates of b and i were obtained for the regression formula: D = bS + i where D = ln[SesROCa /(1 SesROCa)] ln[SpsROCa /(1 SpsROCa)], S = ln[SesROCa /(1 SesROCa )] ln[SpsROCa /(1 SpsROCa )], b = regression coefcient and I = intercept. From this regression formula, sROCa estimates were obtained for sensitivity and specicity, by solving the combination of formulas and constraints (using the solver-routine of Microsoft Excel) (Littenberg & Moses, 1993; Moses et al., 1993): SesROCa = 1/{1 + 1/(exp[i /(1 b)][(1 SpsROCa) /SPsROCa][(1+b)/(1b )])} SesROCa = SeMHSpsROCa /SpMH and 0 < SesROCa < 1; 0 < SpsROCa < 1 This three-step procedure, combining the advantages of sROCavalidity with the point estimate practicality of straight counts and ORMH, provided us with the combined estimates of sensitivity and specicity on which we based our comparison of Tgmeasurement protocols. Sensitivities, specicities, and odds ratios were tested for heterogeneity, using the methods according to http://www.cochrane.org / software / revman42 / User_guide.pdf. For each variable estimate of sensitivity, specicity or accuracy, standard errors (SE) were calculated using the formula SE = [x(1 x)/n]05, in which x is the variable in question, and n is the total number of patients for this variable. Ninety-ve per cent condence intervals were calculated from 2 SE.
2004 Blackwell Publishing Ltd, Clinical Endocrinology, 61, 6174
Вам также может понравиться
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryОт EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryРейтинг: 3.5 из 5 звезд3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)От EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Рейтинг: 4.5 из 5 звезд4.5/5 (121)
- Never Split the Difference: Negotiating As If Your Life Depended On ItОт EverandNever Split the Difference: Negotiating As If Your Life Depended On ItРейтинг: 4.5 из 5 звезд4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingОт EverandThe Little Book of Hygge: Danish Secrets to Happy LivingРейтинг: 3.5 из 5 звезд3.5/5 (400)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaОт EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaРейтинг: 4.5 из 5 звезд4.5/5 (266)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeОт EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeРейтинг: 4 из 5 звезд4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreОт EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreРейтинг: 4 из 5 звезд4/5 (1091)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyОт EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyРейтинг: 3.5 из 5 звезд3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersОт EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersРейтинг: 4.5 из 5 звезд4.5/5 (345)
- The Emperor of All Maladies: A Biography of CancerОт EverandThe Emperor of All Maladies: A Biography of CancerРейтинг: 4.5 из 5 звезд4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnОт EverandTeam of Rivals: The Political Genius of Abraham LincolnРейтинг: 4.5 из 5 звезд4.5/5 (234)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceОт EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceРейтинг: 4 из 5 звезд4/5 (895)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureОт EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureРейтинг: 4.5 из 5 звезд4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)От EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Рейтинг: 4 из 5 звезд4/5 (98)
- Strategic Scientific and Medical WritingДокумент41 страницаStrategic Scientific and Medical Writingebookecm.itОценок пока нет
- The Unwinding: An Inner History of the New AmericaОт EverandThe Unwinding: An Inner History of the New AmericaРейтинг: 4 из 5 звезд4/5 (45)
- Allopathic Drug Manufacturers 2014-09!09!115229Документ24 страницыAllopathic Drug Manufacturers 2014-09!09!115229zak_bdОценок пока нет
- Accupuncture and Induction of LaborДокумент73 страницыAccupuncture and Induction of LaborMarisela Sereia NagôОценок пока нет
- Esofageal CancerДокумент3 страницыEsofageal CancerNaja HasnandaОценок пока нет
- Sponsorship Letter Template 07Документ1 страницаSponsorship Letter Template 07Aria WibowoОценок пока нет
- Asthma QOLДокумент7 страницAsthma QOLjastevensonОценок пока нет
- Chapter 3 Rationality of DrugsДокумент56 страницChapter 3 Rationality of DrugsS.Srinivasan ('Chinu'); Renu KhannaОценок пока нет
- Interventions For Cutaneous Molluscum ContagiosumДокумент50 страницInterventions For Cutaneous Molluscum ContagiosumRatna Puspa RahayuОценок пока нет
- A Review of Meibography.27Документ10 страницA Review of Meibography.27Luis Fernando SaitoОценок пока нет
- Nonadherence To Medications Among Persons With Bipolar Affective Disorder - A ReviewДокумент9 страницNonadherence To Medications Among Persons With Bipolar Affective Disorder - A ReviewIra DomunОценок пока нет
- Lecture 3 - Formulating A Clinical QuestionДокумент44 страницыLecture 3 - Formulating A Clinical QuestionDiah agung100% (1)
- Activity 1: Parts of PrescriptionДокумент2 страницыActivity 1: Parts of PrescriptionERIKA MARIE BECERRELОценок пока нет
- The Value of Postmarketing Studies: by Timothy Pratt, PHDДокумент3 страницыThe Value of Postmarketing Studies: by Timothy Pratt, PHDAndreea ForalОценок пока нет
- Yrc ReportДокумент2 страницыYrc ReportsamuelapaОценок пока нет
- Chapter 6 Confidence Interval Estimates SolutionДокумент18 страницChapter 6 Confidence Interval Estimates SolutionShrey Mangal92% (12)
- 99 740 Medizin FP E PDFДокумент40 страниц99 740 Medizin FP E PDFPhan AnОценок пока нет
- Joe Batson and The Scripps Research InstituteДокумент1 страницаJoe Batson and The Scripps Research InstituteJoe BatsonОценок пока нет
- Scleroza MultiplaДокумент11 страницScleroza MultiplaNatalia PopioneОценок пока нет
- Kuwat Suk A 2016Документ5 страницKuwat Suk A 2016DenySidiqMulyonoChtОценок пока нет
- NeuroaidДокумент11 страницNeuroaidlindasundaОценок пока нет
- Evidence Based Practice 2Документ19 страницEvidence Based Practice 2reguler1Оценок пока нет
- Michael Goss - Death CertificateДокумент1 страницаMichael Goss - Death CertificateAlex EstradaОценок пока нет
- Quantitative Analysis of Continuous Intravenous Infusions in Pediatric Anesthesia. Safety Implications of Dead Volume, Flow Rates, and Fluid DeliveryДокумент9 страницQuantitative Analysis of Continuous Intravenous Infusions in Pediatric Anesthesia. Safety Implications of Dead Volume, Flow Rates, and Fluid DeliveryDavid Arvizo HuitronОценок пока нет
- Efficacy of Minor Analgesics in Primary Dysmenorrhoea: Systematic ReviewДокумент10 страницEfficacy of Minor Analgesics in Primary Dysmenorrhoea: Systematic Reviewadi saputraОценок пока нет
- Agile Project Manager Healthcare in Raleigh Durham NC Resume Moretta RandleДокумент2 страницыAgile Project Manager Healthcare in Raleigh Durham NC Resume Moretta RandleMorettaRandleОценок пока нет
- Heilsusálfræði GlósurДокумент21 страницаHeilsusálfræði GlósurGuðrún Alma EinarsdóttirОценок пока нет
- Experimental DesignДокумент13 страницExperimental DesignKyrahFaithAquilizan100% (2)
- Exercise Interventions For The Treatment of Chronic Low Back Pain: A Systematic Review and Meta-Analysis of Randomised Controlled TrialsДокумент13 страницExercise Interventions For The Treatment of Chronic Low Back Pain: A Systematic Review and Meta-Analysis of Randomised Controlled TrialsGiovanniОценок пока нет
- 843.full Vitamin D As Supplementary Treatment For TuberculosisДокумент8 страниц843.full Vitamin D As Supplementary Treatment For Tuberculosisadrip234Оценок пока нет
- Prurigo NodularisДокумент5 страницPrurigo NodularisRobith LubisОценок пока нет