Академический Документы
Профессиональный Документы
Культура Документы
Causes of Metabolic Acidosis
Загружено:
Kimberly Anne SP PadillaИсходное описание:
Авторское право
Доступные форматы
Поделиться этим документом
Поделиться или встроить документ
Этот документ был вам полезен?
Это неприемлемый материал?
Пожаловаться на этот документАвторское право:
Доступные форматы
Causes of Metabolic Acidosis
Загружено:
Kimberly Anne SP PadillaАвторское право:
Доступные форматы
Diabetes mellitus or diabetic ketoacidosis because an insufficient supply of insulin causes increased fat metabolism, leading to an excess Causes
of Metabolic Acidosis accumulation of ketones or other acids; the bicarbonate then ends up being depleted. (and other diseases) An insufficient supply of insulin in a client with metabolic acidosis known as diabetic diabetes mellitus can result in ....? ketoacidosis. 1. Give insulin as prescribed to hasten the movement of serum glucose into the cell, thereby decreasing the concurrent ketosis. 2. When glucose is being properly metabolized, Interventions in diabetes mellitus and diabetic the body will stop converting fats to glucose. ketoacidosis 3. Monitor for circulatory collapse caused by polyuria, which may result from the hyperglycemic state; osmotic diuresis may lead to extracellular volume deficit. ? levels are used to help diagnose diabetes Fasting blood glucose mellitus and hypoglycemia 1. Instruct the client to fast for 8-12 hours before the test Client teaching for fasting glucose testing 2. Instruct a client with diabetes mellitus to withhold morning insulin or oral hypoglycemic medication until after the blood is drawn Glucose, fasting 70-110 Baseline fasting 70-110 mg/dL 30-min fasting 110-170 mg/dL Glucose testing results 60-min fasting 120-170 mg/dL 90-min fasting 100-140 mg/dL 120-min fasting 70-120 mg/dL Glucose, 2-hr postprandial <140 mg/dL If the glucose levels peak at higher than normal at (____________) after injection or ingestion of glucose and are slower than normal to return to 1 and 2 hours fasting levels, then diabetes mellitus is confirmed Glycosylated hemoglobin is blood glucose bound to hemoglobin. Hyperglycemia in clients with diabetes **indicates how well blood glucose levels ? is usually a cause of an increase in the HbA1c have been controlled for the prior 3 to 4 months.** Good control of diabetes: 7% or lower Values of HgbA1C are expressed as a Fair control of diabetes: 7% to 8% percentage of the total hemoglobin Poor control of diabetes: Higher than 8% Used to evaluate insulin resistance and to Diabetes mellitus autoantibody panel identify type 1 diabetes and clients with a
Diet used for clients with diabetes mellitus, hypoglycemia, hyperglycemia, and obesity
Parenteral Nutrition for Diabetic clients
suspected allergy to insulin Carbohydrate-consistent diet The Exchange System for Meal Planning The MyPyramid diet may benefit from receiving a larger percentage of their PN from lipids, which helps control blood glucose levels and lower insulin requirements caused by infused dextrose.
A client with diabetes mellitus usually does not receive (______________) solutions because the dextrose (glucose) solution can increase the blood glucose level. clients with diabetes mellitus are at risk for Candida Albicans- as superficial fungal developing what skin and mucus membrane infection (aka yeast infection) infection? A life-threatening complication of diabetes mellitus that develops when a severe insulin deficiency occurs. Hyperglycemia progresses to ketoacidosis over a period of several hours to diabetic ketoacidosis several days. Acidosis occurs in clients with type 1 diabetes mellitus, persons with undiagnosed diabetes, and persons who stop prescribed treatment for diabetes. A chronic disorder of glucose intolerance and impaired carbohydrate, protein, and lipid diabetes mellitus metabolism caused by a deficiency of insulin or resistance to the action of insulin. A deficiency of effective insulin results in hyperglycemia. Elevated blood glucose level greater than 250 hyperglycemia mg/dL. Extreme hyperglycemia without acidosis. A complication of type 2 diabetes mellitus, which hyperglycemic hyperosmolar nonketotic may result in dehydration or vascular collapse syndrome but does not include the acidosis component of diabetic ketoacidosis. Onset is usually slow, taking from hours to days. Low blood glucose level (lower than 70 mg/dL) hypoglycemia that results from too much insulin, not enough food, or excess activity. A rebound phenomenon that occurs in clients with type 1 diabetes mellitus. Normal or elevated blood glucose levels are present at bedtime; hypoglycemia occurs at about 2 to 3 Somogyi phenomenon AM. Counterregulatory hormones, produced to prevent further hypoglycemia, result in hyperglycemia (evident in the prebreakfast blood glucose level). Treatment includes
job of the Pancreas An absolute or relative deficiency of insulin results in ? Type 1 diabetes mellitus
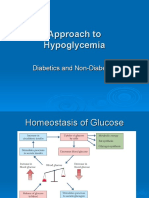
decreasing the evening (predinner or bedtime) dose of intermediate-acting insulin or increasing the bedtime snack. Influences carbohydrate metabolism, indirectly influences fat and protein metabolism, and produces insulin and glucagon hyperglycemia
is a nearly absolute deficiency of insulin; if insulin is not given, fats are metabolized for energy, resulting in ketonemia (acidosis). is a relative lack of insulin or resistance to the action of insulin; usually, insulin is sufficient to Type 2 diabetes mellitus stabilize fat and protein metabolism but not carbohydrate metabolism. the individual has coexisting risk factors for developing type 2 diabetes mellitus; these risk Metabolic syndrome is also known as syndrome factors include abdominal obesity, X hyperglycemia, hypertension, high triglyceride level, and a lowered HDL (high-density lipoprotein) cholesterol level. Diabetes mellitus can lead to chronic health complications that occur in the large and small problems and early death as a result of blood vessels in tissues and organs. coronary artery disease, cardiomyopathy, Macrovascular complications include hypertension, cerebrovascular disease, and peripheral vascular disease. Microvascular complications retinopathy, nephropathy, and neuropathy. a major risk factor for diabetes mellitus obesity a. Polyuria, polydipsia, polyphagia (more common in type 1 diabetes mellitus) b. Hyperglycemia c. Weight loss (common in type 1 diabetes mellitus, rare in type 2 diabetes mellitus) d. Blurred vision assessment e. Slow wound healing f. Vaginal infections g. Weakness and paresthesias h. Signs of inadequate circulation to the feet i. Signs of accelerated atherosclerosis (renal, cerebral, cardiac, peripheral) If the blood glucose level is higher than 250 Instruct the client with diabetes mellitus to mg/dL and urinary ketones (type 1 diabetes monitor the blood glucose level before, during, mellitus) are present, the client is instructed not and after exercising. to exercise until the blood glucose level is closer to normal and urinary ketones are absent. .Oral hypoglycemic medications are prescribed for clients with diabetes mellitus
Medications that cause a decrease in blood glucose levels (increase hypoglycemic effect)
Medications that cause an increase blood glucose levels To prevent a serious reaction, inform the client alcohol taking a sulfonylurea to avoid consuming regular insulin the only insulin that can be administered used in the emergency treatment of diabetic intravenously. ketoacidosis. is loss of subcutaneous fat and appears as slight dimpling or more serious pitting of Lipoatrophy subcutaneous fat; the use of human insulin helps prevent this complication is the development of fibrous fatty masses at Lipohypertrophy the injection site and is caused by repeated use of an injection site a. The client receiving insulin develops immune antibodies that bind the insulin, thereby decreasing the insulin available for use Insulin resistance in the body. b. Treatment consists of administering a purer insulin preparation. results from reduced tissue sensitivity to insulin that usually develops between 5 and 8 AM Dawn phenomenon (prebreakfast hyperglycemia occurs); it may be caused by nocturnal release of growth hormone. a. Normal or elevated blood glucose levels are present at bedtime; hypoglycemia occurs at about 2 to 3 AM, which causes an increase in the production of counterregulatory hormones. Somogyi phenomenon b.B y about 7 AM, in response to the counterregulatory hormones, the blood glucose rebounds significantly to the hyperglycemic range. Hunger Nervousness Palpitations Sweating Mild Hypoglycemia Tachycardia Tremor The client remains fully awake but displays adrenergic symptoms; the blood glucose level is
type 2 when diet and weight control therapy have failed to maintain satisfactory blood glucose levels Aspirin, alcohol, sulfonamides, oral contraceptives, and monoamine oxidase inhibitor Glucocorticoids, thiazide diuretics, and estrogen
Moderate hypoglycemia
Severe Hypoglycemia
Hypoglycemia
Interventions of mild hypo
Interventions: Moderate hypoglycemia
Interventions: Severe hypoglycemia
usually lower than 60 mg/dL Confusion Double vision Drowsiness Emotional changes Headache Impaired coordination Inability to concentrate Irrational or combative behavior Light-headedness Numbness of the lips and tongue Slurred speech The client displays symptoms of worsening hypoglycemia; the blood glucose level is usually lower than 40 mg/dL. Difficulty arousing Disoriented behavior Loss of consciousness Seizures The client displays severe neuroglycopenic symptoms; the blood glucose level is usually lower than 20 mg/dL. occurs when the blood glucose level falls below 70 mg/dL or when the blood glucose level drops rapidly from an elevated level. a. Give 10 to 15 g of a fast-acting simple carbohydrate (Box 54-19). b. Retest the blood glucose level in 15 minutes and repeat the treatment if symptoms do not resolve. c. Once symptoms resolve, a snack containing protein and carbohydrates, such as low-fat milk or cheese and crackers, is recommended unless the client plans to eat a regular meal within 60 minutes. a. Administer 15 to 30 g of a fast-acting simple carbohydrate. b Administer additional food such as low-fat milk or cheese and crackers after 10 to 15 minutes. a. If the client is unconscious and cannot swallow, an injection of glucagon is administered subcutaneously or intramuscularly. b. Administer a second dose in 10 minutes if the client remains unconscious. c. A small meal is given to the client when the client awakens as long as the client is not nauseated.
Diabetic ketoacidosis (DKA)
DKA assessment
DKA treatment
Concern of DKA treatment
Hyperglycemic hyperosmolar nonketotic syndrome (HHNS)
HHS Assessment
HHS Interventions
Diabetic retinopathy
Diabetic retinopathy assessment
Diabetic retinopathy intervention
d. The physician is notified if a severe hypoglycemic reaction occurs. e. Family members need to be instructed about the administration of glucagon. is a life-threatening complication of type 1 diabetes mellitus that develops when a severe insulin deficiency occurs. Ketosis: Kussmaul's respiration, "fruity" breath, nausea, abdominal pain =Dehydration or electrolyte loss: Polyuria, polydipsia, weight loss, dry skin, sunken eyes, soft eyeballs, lethargy, coma Treat dehydration with rapid IV infusions of 0.9% or 0.45% normal saline (NS) as prescribed; dextrose is added to IV fluids (D5NS, or 5% dextrose in 0.45% saline) when the blood glucose level reaches 250 to 300 mg/dL. The potassium level will fall rapidly within the first hour of treatment as the dehydration and the acidosis are treated. Extreme hyperglycemia occurs without ketosis or acidosis The syndrome occurs most often in individuals with type 2 diabetes mellitus. Altered central nervous system function with neurologic symptoms Dehydration or electrolyte loss: Same as for DKA Treatment includes fluid replacement, correction of electrolyte imbalances, and insulin administration. HIE (hydration, Insulin, electrolyte replacement) Chronic and progressive impairment of the retinal circulation that eventually causes hemorrhage a. A change in vision is caused by the rupture of small microaneurysms in retinal blood vessels. b. Blurred vision results from macular edema. c .Sudden loss of vision results from retinal detachment. d. Cataracts result from lens opacity. a. Photocoagulation (laser therapy) may be done to remove hemorrhagic tissue to decrease
scarring and prevent progression of the disease process. b. Vitrectomy may be done to remove vitreous hemorrhages and thus decrease tension on the retina, preventing detachment. c. Cataract removal with lens implantation improves vision. 571. A client is brought to the emergency department in an unresponsive state, and a diagnosis of hyperglycemic hyperosmolar Intravenous infusion of normal saline nonketotic syndrome is made. The nurse would immediately prepare to initiate which of the following anticipated physician's prescriptions? 572. An external insulin pump is prescribed for Gives a small continuous dose of regular a client with diabetes mellitus and the client asks insulin subcutaneously, and the client can selfthe nurse about the functioning of the pump. The administer a bolus with an additional dose from nurse bases the response on the information that the pump before each meal the pump: 573. A client with a diagnosis of diabetic ketoacidosis (DKA) is being treated in an Elevated blood glucose level and low plasma emergency department. Which finding would a bicarbonate level nurse expect to note as confirming this diagnosis? 574. A nurse teaches a client with diabetes mellitus about differentiating between hypoglycemia and ketoacidosis. The client Shakiness demonstrates an understanding of the teaching by stating that a form of glucose should be taken if which of the following symptoms develops? 575. A client with diabetes mellitus demonstrates acute anxiety when first admitted "I will decrease my insulin dose during times of for the treatment of hyperglycemia. The illness." appropriate intervention to decrease the client's anxiety is to: 577. A client is admitted to a hospital with a diagnosis of diabetic ketoacidosis (DKA). The initial blood glucose level was 950 mg/dL. A continuous intravenous infusion of regular insulin is initiated, along with intravenous Intravenous fluids containing 5% dextrose rehydration with normal saline. The serum glucose level is now 240 mg/dL. The nurse would next prepare to administer which of the following? 576. A nurse provides instructions to a client "I will notify my physician if my blood glucose newly diagnosed with type 1 diabetes mellitus. level is higher than 250 mg/dL." The nurse recognizes accurate understanding of
measures to prevent diabetic ketoacidosis when the client states: 578. A nurse is monitoring a client newly diagnosed with diabetes mellitus for signs of complications. Which of the following, if Polyuria exhibited in the client, would indicate hyperglycemia and warrant physician notification? 579. A nurse is preparing a plan of care for a client with diabetes mellitus who has Deficient fluid volume hyperglycemia. The priority nursing diagnosis would be: 580. A home health nurse visits a client with a diagnosis of type 1 diabetes mellitus. The client relates a history of vomiting and diarrhea and tells the nurse that no food has been consumed "I need to stop my insulin." for the last 24 hours. Which additional statement by the client indicates a need for further teaching? 584. A nurse is caring for a client admitted to the emergency department with diabetic Administer regular insulin intravenously. ketoacidosis (DKA). In the acute phase, the priority nursing action is to prepare to: 585. A client with type 1 diabetes mellitus calls the nurse to report recurrent episodes of hypoglycemia with exercising. Which statement "The best time for me to exercise is mid- to late by the client indicates an inadequate afternoon." understanding of the peak action of NPH insulin and exercise? 592. A nurse performs a physical assessment on a client with type 2 diabetes mellitus. Findings include a fasting blood glucose of 120 mg/dL, temperature of 101 F, pulse of 88 beats/min, Temperature respirations of 22 breaths/min, and blood pressure of 100/72 mm Hg. Which finding would be of most concern to the nurse? 593. A nurse is interviewing a client with type 2 diabetes mellitus. Which statement by the client "The medications I'm taking help release the indicates an understanding of the treatment for insulin I already make." this disorder? 595. The nurse is caring for a client who is 2 days postoperative following an abdominal hysterectomy. The client has a history of Obtain a capillary blood glucose level and diabetes mellitus and has been receiving regular perform a focused assessment. insulin according to capillary blood glucose testing four times a day. A carbohydrate-
controlled diet has been prescribed but the client has been complaining of nausea and is not eating. On entering the client's room, the nurse finds the client to be confused and diaphoretic. Which action is appropriate at this time? Insulin increases glucose transport into cells and promotes conversion of glucose to glycogen, decreasing serum glucose levels. stimulate the pancreas to produce more insulin, increase the sensitivity of peripheral receptors to insulin, decrease hepatic glucose output, or delay intestinal absorption of glucose, thus decreasing serum glucose levels. a. Sulfonylureas may be classified as first- or second-generation sulfonylureas. b. Sulfonylureas stimulate the beta cells to produce more insulin. a. May be used alone or in combination with a sulfonylurea b. Suppresses hepatic production of glucose and increases insulin sensitivity c. Side effects: Diarrhea (most common), lactic acidosis (most serious) a.Delay absorption of ingested carbohydrates (sucrose and complex carbohydrates), resulting in smaller increase in blood glucose level after meals. b.Do not increase insulin production c.Can be given alone or in combination with sulfonylureas d.Will not cause hypoglycemia when given alone e.Given with first bite of meal a. Insulin-sensitizing agents that lower blood glucose by decreasing hepatic glucose production and improving target cell response to insulin b. May cause liver toxicity a.Stimulate pancreatic insulin secretion b.Quicker and shorter duration of action; therefore, less chance of hypoglycemia because blood glucose-lowering effect wears off quickly c.Very fast onset of action allows client to take the medication with meals and skip a dose
Oral hypoglycemic agents
Sulfonylureas
Biguanides
Alpha-glucosidase inhibitors
Thiazolidinediones
Meglitinides
Insulin primarily acts
RAPID-ACTING INSULIN SHORT-ACTING INSULIN INTERMEDIATE-ACTING INSULIN LONG-ACTING INSULIN
when a meal is skipped in the liver, muscle, and adipose tissue by attaching to receptors on cellular membranes and facilitating the passage of glucose, potassium, and magnesium 0.25 1-3 3-5 onset peak duration 0.5 2-4 5-7 onset peak duration 1.5 4-12 16-24+ onset peak duration
Вам также может понравиться
- Case Study (NSD - Primi)Документ29 страницCase Study (NSD - Primi)Kimberly Anne SP Padilla82% (11)
- Substance AbuseДокумент45 страницSubstance AbuseKimberly Anne SP Padilla100% (1)
- Concept Map of DMДокумент2 страницыConcept Map of DMLeslie Marie Rendon100% (9)
- Diabetes MellitusДокумент34 страницыDiabetes MellitusKobby AmoahОценок пока нет
- Lec 1Документ9 страницLec 1fbbqbcht6yОценок пока нет
- Management of Diabetis MellitusДокумент24 страницыManagement of Diabetis MellitusTasmia TasnimОценок пока нет
- Classification: LiverДокумент20 страницClassification: LivertermskipopОценок пока нет
- Metabolic Disorders Diabetes HandoutДокумент21 страницаMetabolic Disorders Diabetes HandoutEdelen GaleОценок пока нет
- Hand Out DM Medical Surgical Nursing 2Документ11 страницHand Out DM Medical Surgical Nursing 2Zarlou OtamiasОценок пока нет
- Module 8 Assessment and Management of Patients With DiabetesДокумент44 страницыModule 8 Assessment and Management of Patients With DiabetesBlessed GarcianoОценок пока нет
- 9 Diabetes Mellitus PHYSIOLOGYДокумент22 страницы9 Diabetes Mellitus PHYSIOLOGYEman KhammasОценок пока нет
- Diabetes Mellitus: Dr. Sajid Abbas JaffriДокумент37 страницDiabetes Mellitus: Dr. Sajid Abbas JaffriMaham ZarrinОценок пока нет
- Diabetes: Oral Health TopicsДокумент9 страницDiabetes: Oral Health TopicsAndrei StamateОценок пока нет
- Diabetes Millitus PDFДокумент41 страницаDiabetes Millitus PDFAbdullah BhattiОценок пока нет
- Diabetes ComplicationsДокумент29 страницDiabetes ComplicationsTom ThomasОценок пока нет
- Diabetes For Dentists: DR Jackie Elliott Clinical Lecturer in DiabetesДокумент37 страницDiabetes For Dentists: DR Jackie Elliott Clinical Lecturer in DiabetesKevalChavdaОценок пока нет
- Diabetes Mellitus: Risks FactorsДокумент5 страницDiabetes Mellitus: Risks FactorsAmer Abdulla SachitОценок пока нет
- Diabetes PPT FianlДокумент31 страницаDiabetes PPT FianlUqba MishalОценок пока нет
- 9 - Assessment and Management of Patients With Diabetes MellitusДокумент60 страниц9 - Assessment and Management of Patients With Diabetes Mellitussohaib salamehОценок пока нет
- Type 2 DMДокумент14 страницType 2 DMraffia mehakОценок пока нет
- DIABETES CorrectedДокумент16 страницDIABETES CorrectedBlaise PascalОценок пока нет
- Dysfunction of The Endocrine Pancreas:: Diabetes MellitusДокумент27 страницDysfunction of The Endocrine Pancreas:: Diabetes Mellitushasan ismaelОценок пока нет
- Diabetes Mellitus Diabetes Mellitus, Often Simply Diabetes, Is A Syndrome Characterized by DisorderedДокумент8 страницDiabetes Mellitus Diabetes Mellitus, Often Simply Diabetes, Is A Syndrome Characterized by DisorderedRachel Ann BatayolaОценок пока нет
- Bab IiДокумент8 страницBab IiAdhityaWPutraОценок пока нет
- Welcome To The PresentationДокумент32 страницыWelcome To The PresentationIshaan Arfatur Rahman0% (1)
- Pathophysiology of DiabetesДокумент88 страницPathophysiology of DiabetesCahya SetiyaОценок пока нет
- DM Reporting ZДокумент52 страницыDM Reporting ZZsazsaОценок пока нет
- DiabetesДокумент27 страницDiabetesÑùmãñ MùghãlОценок пока нет
- Diabetes PresentationДокумент32 страницыDiabetes PresentationsgolbariОценок пока нет
- Dental Management of Patients With Diabetes MellitusДокумент8 страницDental Management of Patients With Diabetes Mellitusاحمد سلامОценок пока нет
- Bhs InggrisДокумент13 страницBhs Inggrisciko sisca bintang pamungkhasОценок пока нет
- Diabetes Mellitus DMC 6th SemesterДокумент23 страницыDiabetes Mellitus DMC 6th SemesterHuzaifa CHОценок пока нет
- Hypoglycemia UMYДокумент60 страницHypoglycemia UMYTommy AkromaОценок пока нет
- Komplikasi DMДокумент7 страницKomplikasi DMRhima KemalaОценок пока нет
- Nursing Care Plans For Diabetes MellitusДокумент12 страницNursing Care Plans For Diabetes MellitusPuteri AzmanОценок пока нет
- Diabetes MellitusДокумент31 страницаDiabetes MellitusElenaCondratscribdОценок пока нет
- Chapter 4 Carbohydrate DisorderДокумент26 страницChapter 4 Carbohydrate DisorderNida RidzuanОценок пока нет
- Gastrointestinal SystemДокумент3 страницыGastrointestinal SystemNemr NassarОценок пока нет
- Diabetes MellitusДокумент9 страницDiabetes MellitusCatherine MetraОценок пока нет
- Diabetes Mellitus: (DM)Документ84 страницыDiabetes Mellitus: (DM)Andika HОценок пока нет
- 8 Dayz Hunza and Skardu'Документ8 страниц8 Dayz Hunza and Skardu'Hasnain AliОценок пока нет
- 06.disorder of Carbohydrate MetabolismДокумент47 страниц06.disorder of Carbohydrate MetabolismRizka NizarОценок пока нет
- DM PresentationДокумент28 страницDM PresentationmymommywowОценок пока нет
- HypoglycemiaДокумент68 страницHypoglycemialiaputranti100% (3)
- CBD DMДокумент8 страницCBD DMEtsubdink HailuОценок пока нет
- Diabetes Mellitus: WAHYUDI, S.Farm., AptДокумент31 страницаDiabetes Mellitus: WAHYUDI, S.Farm., AptMayesti FransiskaОценок пока нет
- Drug Study - Regular InsulinДокумент8 страницDrug Study - Regular InsulinRaijenne VersolaОценок пока нет
- Glucose, Part1Документ33 страницыGlucose, Part1SarahОценок пока нет
- Proficiency Testbuilder 4th EditionДокумент27 страницProficiency Testbuilder 4th EditionNgan LeОценок пока нет
- Diabetes MellitusДокумент26 страницDiabetes MellitusKamlesh KishorОценок пока нет
- Lecture 1 Carbohydrate 1Документ39 страницLecture 1 Carbohydrate 1mer12sswОценок пока нет
- Diabetes MellitusДокумент30 страницDiabetes Mellitusurusha vaidyaОценок пока нет
- Blood GlucoseДокумент8 страницBlood Glucoseعبدالرحمن عابدОценок пока нет
- Insulin Secretion and FunctionДокумент8 страницInsulin Secretion and FunctionWendy EscalanteОценок пока нет
- Fear of The Low: What You Need To Know About Hypoglycemia: Stacey A. Seggelke, MS, RN, ACNS-BC, BC-ADM, CDEДокумент6 страницFear of The Low: What You Need To Know About Hypoglycemia: Stacey A. Seggelke, MS, RN, ACNS-BC, BC-ADM, CDEesterОценок пока нет
- Anti Diabetic DrugsДокумент58 страницAnti Diabetic DrugsDaniel WangОценок пока нет
- Diabetes MellitusДокумент44 страницыDiabetes MellituslkristinОценок пока нет
- Acute Complications of Diabetes MellitusДокумент13 страницAcute Complications of Diabetes MellitusMark Christian M. GonzagaОценок пока нет
- Diabetes and It's Oral ManifestationsДокумент28 страницDiabetes and It's Oral ManifestationsYashpreetsingh BhatiaОценок пока нет
- Diabetes and MassageДокумент23 страницыDiabetes and MassagemassagekevinОценок пока нет
- Diabetes ExamДокумент7 страницDiabetes ExambennybuffetОценок пока нет
- Management of Diabetes Mellitus 11Документ25 страницManagement of Diabetes Mellitus 11khalid.zainabОценок пока нет
- Famous Philosopher's Quotes.Документ5 страницFamous Philosopher's Quotes.Kimberly Anne SP PadillaОценок пока нет
- Lab 1-1 CreditДокумент4 страницыLab 1-1 CreditKimberly Anne SP PadillaОценок пока нет
- Endocrine SystemДокумент5 страницEndocrine SystemKimberly Anne SP Padilla100% (2)
- K OnДокумент11 страницK OnKimberly Anne SP PadillaОценок пока нет
- Management of Childhood IllnessesДокумент2 страницыManagement of Childhood IllnessesKimberly Anne SP PadillaОценок пока нет
- Microsoft Word 2007Документ6 страницMicrosoft Word 2007Kimberly Anne SP PadillaОценок пока нет
- Hyperglycemia Algorithm 2Документ1 страницаHyperglycemia Algorithm 2damondouglasОценок пока нет
- Inv. Virtual Conference Ryzodeg-16 JAN 2021 - Final - OKДокумент4 страницыInv. Virtual Conference Ryzodeg-16 JAN 2021 - Final - OKmelyekaОценок пока нет
- Blood Sugar Levels Blood Glucose Charts For Children and AdultsДокумент1 страницаBlood Sugar Levels Blood Glucose Charts For Children and Adultsyvess leyv ignacioОценок пока нет
- Final Atcofliflozin Binder DiabetesДокумент23 страницыFinal Atcofliflozin Binder DiabetesEslamОценок пока нет
- Wan Nurafifah Binti Wan Mohammad Nadzim - hs245 4cДокумент10 страницWan Nurafifah Binti Wan Mohammad Nadzim - hs245 4cMOHD MU'IZZ BIN MOHD SHUKRIОценок пока нет
- Study Guide Blood Glucose MonitoringДокумент4 страницыStudy Guide Blood Glucose MonitoringDan Dan ManaoisОценок пока нет
- Glycemic Targets: American Diabetes AssociationДокумент8 страницGlycemic Targets: American Diabetes AssociationHelenaОценок пока нет
- Steroid Induced Diabetes and Hyperglycaemia Part 2 ManagementДокумент5 страницSteroid Induced Diabetes and Hyperglycaemia Part 2 ManagementAura DiscyacittaОценок пока нет
- Accu Chek - Guide Me Blood Glucose Meter User Manual v2bДокумент140 страницAccu Chek - Guide Me Blood Glucose Meter User Manual v2bWao ZapataОценок пока нет
- RosiglitazoneДокумент2 страницыRosiglitazoneAngelica Alburo PenionОценок пока нет
- BPT GTT & Diabetes MellitusДокумент25 страницBPT GTT & Diabetes MellitusBalajiОценок пока нет
- Diabetes BrochureДокумент3 страницыDiabetes Brochureapi-348372254Оценок пока нет
- 02 Tatalaksana Terapi Insulin - Prof Tri Murti AndayaniДокумент39 страниц02 Tatalaksana Terapi Insulin - Prof Tri Murti AndayaniEndang Wulan SariОценок пока нет
- Path122 Diabetes MellitusДокумент12 страницPath122 Diabetes MellitusGwendolaine PicaОценок пока нет
- 6Документ5 страниц6ρενα μινορεОценок пока нет
- 5405-Article Text-19410-1-10-20211022Документ17 страниц5405-Article Text-19410-1-10-20211022Khairunisa ErsantiОценок пока нет
- 2023 IABO Scientific Paper - TemplateДокумент3 страницы2023 IABO Scientific Paper - TemplateKayla Jihan NamiroОценок пока нет
- Presentation On: Kgmu College of NursingДокумент42 страницыPresentation On: Kgmu College of NursingSweety YadavОценок пока нет
- 2457-Article Text-14907-2-10-20120724Документ6 страниц2457-Article Text-14907-2-10-20120724desi meleniaОценок пока нет
- Ef Ficacy of An Education Program For People With Diabetes and Insulin Pump Treatment (INPUT) : Results From A Randomized Controlled TrialДокумент10 страницEf Ficacy of An Education Program For People With Diabetes and Insulin Pump Treatment (INPUT) : Results From A Randomized Controlled TrialadddОценок пока нет
- Insulin Prod ListДокумент4 страницыInsulin Prod ListSteveEpsteinОценок пока нет
- DiabetesДокумент4 страницыDiabetesNathelyn LaCroixОценок пока нет
- Ada Easd 2018Документ14 страницAda Easd 2018Nimesh ModiОценок пока нет
- Insulin TherapyДокумент23 страницыInsulin Therapymahmoud fuqahaОценок пока нет
- DM GuidelinesДокумент7 страницDM GuidelinesslojnotakОценок пока нет
- Markers of B-Cell Failure Predict Poor Glycemic Response To GLP-1 Receptor Agonist Therapy in Type 2 DiabetesДокумент8 страницMarkers of B-Cell Failure Predict Poor Glycemic Response To GLP-1 Receptor Agonist Therapy in Type 2 DiabetesAnitaFauzziahYusufОценок пока нет
- Inisiasi Insulin DR OctoДокумент47 страницInisiasi Insulin DR Octowulan nurmalasariОценок пока нет
- PEX-04-02 PaldiДокумент4 страницыPEX-04-02 PaldiRivaldy KerenОценок пока нет
- Management of Hyperglycemia in Hospitalized Adult Patients in Non-Critical Care Settings: An Endocrine Society Clinical Practice GuidelineДокумент34 страницыManagement of Hyperglycemia in Hospitalized Adult Patients in Non-Critical Care Settings: An Endocrine Society Clinical Practice Guidelineakash kondapalliОценок пока нет